Professional Documents
Culture Documents
Management of Stroke in The Neurocritical Care.7
Management of Stroke in The Neurocritical Care.7
Uploaded by
Bryan ZhengOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Management of Stroke in The Neurocritical Care.7
Management of Stroke in The Neurocritical Care.7
Uploaded by
Bryan ZhengCopyright:
Available Formats
REVIEW ARTICLE
Management of Stroke
in the Neurocritical
C O N T I N UU M A UD I O
I NT E R V I E W A V AI L A B L E
ogM/G3Lw98L4g53y0W25aSbX7CEFzDyuApk/85Hsqz5UhDeRfNPFhkYp95Mer+PxzV9+48F39Z4b5s+Btx/00RefYCHmPbzv2sNN
Care Unit
ONLINE
Downloaded from http://journals.lww.com/continuum by KjfsNO4rm+70wsgqTPXGiE1ivOxovFfe/bXXYpJT6n4lQzg
S U P P L E M E N T AL D I G I T A L
CONTENT (SDC) By Chethan P. Venkatasubba Rao, MD, FNCS; Jose I. Suarez, MD, FNCS, FANA
A VA I L A B L E O N L I N E
ABSTRACT
PURPOSE OF REVIEW: This article provides updated information regarding the
diagnosis and treatment (specifically critical care management) of acute
ischemic stroke. This article also discusses the increased use of
LisNIokjeaJDU on 03/08/2023
thrombolysis and thrombectomy in clinical practice.
RECENT FINDINGS: Stroke is the leading cause of disability in the United States.
CITE AS:
CONTINUUM (MINNEAP MINN) A significant proportion of patients with acute ischemic stroke require
2018;24(6, NEUROCRITICAL CARE): critical care management. Much has changed in the early evaluation and
1658–1682.
treatment of patients presenting with acute ischemic stroke. The
Address correspondence to introduction of embolectomy in large vessel occlusions for up to 24 hours
Dr Chethan P. Venkatasubba Rao, post–symptom onset has resulted in one in every three eligible patients
Baylor College of Medicine, MS
NB 124, One Baylor Plaza,
with acute ischemic stroke with the potential to lead an independent
Houston, TX 77030, lifestyle. These patients increasingly require recognition of complications
cprao@bcm.edu. and initiation of appropriate interventions as well as earlier admission to
RELATIONSHIP DISCLOSURE:
dedicated neurocritical care units to ensure better outcomes.
Dr Venkatasubba Rao has
received personal compensation SUMMARY: This article emphasizes issues related to the management of
as an editorial board member
of Brain Disorders & Therapy. patients with acute ischemic stroke undergoing mechanical thrombectomy
Dr Suarez has received research/ and thrombolysis and addresses the complex physiologic changes
grant support from the National
affecting neurologic and other organ systems.
Institute of Neurological
Disorders and Stroke and
as co-investigator in the
SETPOINT2 (Stroke-related Early
Tracheostomy Versus Prolonged INTRODUCTION
A
Orotracheal Intubation in cute ischemic stroke is a neurologic emergency. A recent report from
Neurocritical Care Trial) study
from the Patient-Centered
the American Heart Association has shown that acute ischemic
Outcomes Research Institute. stroke affects an average of 800,000 people annually in the
Dr Suarez is the current president United States, the majority of whom experience their first event.1
and a member of the board of
directors of the Neurocritical This translates into one person having a stroke every 40 seconds.
Care Society. About 7.2 million Americans older than 20 years of age report having had a stroke,
and the prevalence is estimated to be 2.7%.2 Recent studies have noted that acute
UNLABELED USE OF
PRODUCTS/INVESTIGATIONAL ischemic stroke affects men and women equally overall but has variable influence
USE DISCLOSURE: in different ages and ethnic groups. Acute ischemic stroke has a higher incidence
Drs Venkatasubba Rao and
Suarez report no disclosures.
in American Indians/Alaskan Natives (5.4%), non-Hispanic blacks (4.5%), and
other races and multiracial people (4.7%) compared to non-Hispanic whites (2.5%).3
Acute ischemic stroke remains the number one cause of morbidity and
© 2018 American Academy disability in the United States, costing an unprecedented $33.9 billion, which is
of Neurology. 14% of annual health care expenditure. Several disturbing trends are
1658 DECEMBER 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
noted in stroke epidemiology. Certain models have predicted that by 2030, KEY POINTS
3.4 million more adult Americans will have had a stroke, a staggering 20.5%
● One in every four patients
increase as compared to the prevalence in 2010. This increase is predicted with acute ischemic stroke
to affect Hispanic men by more than 29%. Stroke remains the fifth most common will need critical care
cause of mortality, claiming 133,000 lives annually in the United States. In other intervention.
ogM/G3Lw98L4g53y0W25aSbX7CEFzDyuApk/85Hsqz5UhDeRfNPFhkYp95Mer+PxzV9+48F39Z4b5s+Btx/00RefYCHmPbzv2sNN
words, one person dies every 4 minutes from stroke. Therefore, it is imperative
● Factors predicting critical
that preventive measures and timely administration of thrombolytics,
Downloaded from http://journals.lww.com/continuum by KjfsNO4rm+70wsgqTPXGiE1ivOxovFfe/bXXYpJT6n4lQzg
care admission in patients
thrombectomy, and critical care management are instituted in patients with with acute ischemic stroke
acute ischemic stroke to prevent the resultant morbidity and mortality. include severity of stroke,
age, elevated systolic blood
EPIDEMIOLOGY AND RISK FACTORS FOR INTENSIVE CARE pressure, and
hyperglycemia.
UNIT ADMISSION
It is estimated that only 5% to 7% of all patients with acute ischemic stroke are
treated with IV recombinant tissue plasminogen activator (rtPA) in the
United States. Admission of patients with acute ischemic stroke treated with IV
rtPA or thrombectomy primarily to an intensive care unit (ICU) varies and
LisNIokjeaJDU on 03/08/2023
depends on local health care practices and availability of resources. Specialized
clinical care units designated to manage patients with acute ischemic stroke have
been shown to improve outcomes and reduce the length of hospitalizations.4 The
impact of a neurocritical care unit team in the improvement of outcomes of
patients with traumatic brain injury, spinal cord injury, and neurosurgical
patients is very well established.5,6 However, its impact on patients with acute
ischemic stroke has yet to be systematically studied, but some preliminary
evidence suggests that admission to a neurocritical care unit is associated with
positive effects on this population.5
In this section, the definition of a neurocritical care unit will be limited to
specialized ICUs, which consist of a treatment team led by a neurointensivist
or an intensivist well versed in the treatment of neurologic and neurosurgical
patients who are critically ill; nursing staff trained for neurologic management;
respiratory therapists; pharmacists trained in critical care; and physical,
occupational, and speech therapists in an institution that is committed to
assuring quality of care as specified by their certifying bodies. As mentioned
above, a small proportion of patients with acute ischemic stroke are currently
receiving thrombolytic therapy,7 and because of the lack of screening data, it is
unclear what percentage of them would actually be eligible for thrombectomy
for up to both 8 and 24 hours. However, it is estimated that 24% of all patients
admitted with acute ischemic stroke may need critical care intervention.8
Potential factors that predict the need for critical care intervention include the
following: being African American (odds ratio of 3.8), being male (odds ratio of
3.8), systolic blood pressure values (odds ratio of 1.45 per 10 mm Hg increase),
and National Institutes of Health Stroke Scale (NIHSS) score (odds ratio of
1.09 per 1 point increase in NIHSS) in one study.8 In another study, age,
hyperlipidemia, the presence of extracranial vascular disease, and NIHSS were
found to be independent predictors of critical care needs.9 Separate scores such
as the Intensive Care After Thrombolysis (ICAT) score (TABLE 4-1) and the
Simplified Acute Physiology Score II (SAPS II) (a score using physiological
variables to evaluate the risk of mortality in any given disease state) have been
developed to assess the need for critical care intervention in patients presenting
with acute ischemic stroke. For every 1 point increase in the ICAT score, the
odds of requiring critical care increases 2.22 times. The odds of requiring critical
CONTINUUMJOURNAL.COM 1659
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
MANAGEMENT OF STROKE IN THE NEUROCRITICAL CARE UNIT
care for a patient with an ICAT score of more than 2 was 13 times higher than
for a patient with a score of less than 2. A score of 5 or more predicts critical
care needs with a 94% specificity and 45.8% sensitivity. Factors that can
independently influence the need for critical care in patients with stroke are
summarized in TABLE 4-2.
ogM/G3Lw98L4g53y0W25aSbX7CEFzDyuApk/85Hsqz5UhDeRfNPFhkYp95Mer+PxzV9+48F39Z4b5s+Btx/00RefYCHmPbzv2sNN
INITIAL MANAGEMENT OF ACUTE ISCHEMIC STROKE
Downloaded from http://journals.lww.com/continuum by KjfsNO4rm+70wsgqTPXGiE1ivOxovFfe/bXXYpJT6n4lQzg
Similar to other neurologic emergencies, patients with acute ischemic stroke
should be evaluated and triaged promptly so that they can receive adequate
management. Time is of the essence. The general principles of initial
management include the following:
u Assess circulation and, if needed, perform cardiopulmonary resuscitation per the basic
life support method
u Assess and secure airway and breathing (ventilation)
u Initiate a call for rapid response of a critical care team (obtain help)
LisNIokjeaJDU on 03/08/2023
u Point of care testing for glucose, coagulopathy
u Perform a standardized and complete neurologic assessment (NIHSS, see below).
TABLE 4-1 Determination of the Intensive Care After Thrombolysis Scorea
Intensive Care After
Thrombolysis
Score Component (ICAT) Score Points
Male sex
Yes 0
No 1
Black race
No 0
Yes 1
Systolic blood pressure in mm Hg
<160 0
160–200 2
>200 4
National Institutes of Health Stroke Scale Score
≤6 0
7–12 1
≥13 2
Total Score 0–8
a
Reprinted with permission from Faigle R, et al, Crit Care.8 © 2016 Faigle et al.
1660 DECEMBER 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
u Review vital signs prior to the current neuroemergency
u Review history and list of medications and recent treatments received
u Neuroimaging
u Appropriate laboratory tests
ogM/G3Lw98L4g53y0W25aSbX7CEFzDyuApk/85Hsqz5UhDeRfNPFhkYp95Mer+PxzV9+48F39Z4b5s+Btx/00RefYCHmPbzv2sNN
u Neurosurgical consultation
u Update patient/surrogate regarding the diagnosis and plan of care and clarify agreement
Downloaded from http://journals.lww.com/continuum by KjfsNO4rm+70wsgqTPXGiE1ivOxovFfe/bXXYpJT6n4lQzg
for treatment.
NIHSS is a standardized neurologic assessment of patients and is helpful in
determining the severity of stroke but is heavily weighted toward anterior
circulation and left hemispheric symptoms. Left hemispheric strokes score at
least 4 points more than the opposite hemisphere.10 NIHSS has a limitation as a
bedside assessment tool, and special caution has to be exercised, especially
when performed by untrained personnel.
Thrombolytic and Endovascular Therapies
LisNIokjeaJDU on 03/08/2023
Acute ischemic stroke treatment has experienced a paradigm shift over the last
3 years. Foundations for this progress were laid in 1995, wherein a National
Institute of Neurological Disorders and Stroke–rtPA trial reported benefit in
3-month outcomes with the use of IV rtPA within 3 hours of acute ischemic
stroke symptom onset (SDC 4-1, links.lww.com/CONT/A259).11–22 Using that
protocol for rtPA infusion, one in every 12 patients would be functionally
independent in 3 months post–acute ischemic stroke as compared to patients
without receiving rtPA. Extending that window of thrombolysis between 3 and
4.5 hours in the ECASS III (European Cooperative Acute Stroke Study III),
functional independence was demonstrated in one in 14 patients treated with IV
rtPA as compared to patients not receiving thrombolytics.12
The IST-3 (Third International Stroke Trial) was yet another landmark trial for
enrolling patients older than 80 years, who comprised more than 25% of the
3035 patients enrolled in the study, and tested an extended window of IV
thrombolysis up to 6 hours. The results of this trial must be interpreted
Factors Increasing the Risk of Requiring Critical Care Interventions in TABLE 4-2
Patients With Acute Ischemic Strokea
◆ Age (odds ratio of 1.3 per 10 years)
◆ African American ethnicity (odds ratio of 3.8)
◆ Male sex (odds ratio of 3.8)
◆ Systolic blood pressure (odds ratio of 1.45 for every 10 mm Hg greater than 140 mm Hg)
◆ Hyperglycemia (odds ratio of 1.25 per 50 mg/dL increase in glucose)
◆ National Institutes of Health Stroke Scale (odds ratio of 1.09 per 1 point increase)
◆ Simplified Acute Physiology Score II of greater than 22
◆ Vascular disease affecting non-neurologic locations (ie, peripheral vascular disease)
a
Data from Faigle R, et al, Crit Care.8
CONTINUUMJOURNAL.COM 1661
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
MANAGEMENT OF STROKE IN THE NEUROCRITICAL CARE UNIT
cautiously. While outcome improvement was better when comparing complete
recovery or recovery with minimal symptoms (defined as an Oxford Handicap
Scale score of 0 or 1) in the group treated with rtPA as compared to controls, no
such improvement was seen when the data were analyzed to compare traditional
dependency versus independency (Oxford Handicap Scale score of <3 versus >3)
ogM/G3Lw98L4g53y0W25aSbX7CEFzDyuApk/85Hsqz5UhDeRfNPFhkYp95Mer+PxzV9+48F39Z4b5s+Btx/00RefYCHmPbzv2sNN
in 3-month outcomes.13 Furthermore, the rates of symptomatic intracranial
hemorrhage and other cerebral-related mortality rates were higher in patients
Downloaded from http://journals.lww.com/continuum by KjfsNO4rm+70wsgqTPXGiE1ivOxovFfe/bXXYpJT6n4lQzg
receiving rtPA, and thus the use of IV rtPA is currently limited to up to 4.5 hours
after symptom onset. A Cochrane meta-analysis of 12 trials using rtPA for
acute ischemic stroke demonstrated an odds risk of 0.85 for reducing the
proportion of patients with dependency or death at 3 months.23
It is only recently that rtPA use has been extended beyond the traditional
4.5 hours. In a study led by the WAKE-UP (MRI-Guided Thrombolysis
for Stroke With Unknown Time of Onset) investigators, patients were
selected for thrombolysis based on brain tissue viability as determined by a
diffusion-weighted imaging (DWI) sequence demonstrating ischemia and no
LisNIokjeaJDU on 03/08/2023
visible change in T2 fluid-attenuated inversion recovery (FLAIR) sequence.14
Patients were randomly assigned to either placebo or IV rtPA. Outcomes as
defined by a modified Rankin Scale (mRS) score of 0 or 1 were better in patients
who received rtPA (53.3%) as compared to the group treated with placebo
(41.8%). A higher incidence of hemorrhage was noted in patients receiving rtPA
(4% versus 0.4% in the placebo group), but the overall death or dependency
was still higher in patients receiving placebo (18.3% versus 13.5% in the rtPA-
treated group).14
Large vessel occlusions seem resistant to the effects of IV rtPA and portend a
devastating impact on clinical outcomes. Therefore, interventional strategies for
chemical thrombolysis and mechanical thrombectomy have been developed in a
stepwise evolution to its current stage, the roots of which can be traced to the
PROACT II (Prolyse in Acute Cerebral Thromboembolism II) study.24 Initially,
as seen in the PROACT II study, local thrombolytic delivery alone failed to
provide the anticipated response in perfusion and clinical recovery, which led to
the development of interventional techniques for clot disruption. Of the many
studies investigating this concept, the IMS III (Interventional Management of
Stroke III), MR RESCUE (Mechanical Retrieval and Recanalization of Stroke
Clots Using Embolectomy), and SYNTHESIS Expansion trials evaluated the use
of mechanical embolectomy in patients with acute ischemic stroke but failed to
demonstrate clinical improvement with intervention.25–27
Despite these trials having different methodologies, three universally pervasive
themes likely responsible for the failure of these studies could be identified, namely
poor selection of cases (ie, a significant portion of patients enrolled did not have
intracranial occlusion), unclear definition of parenchymal viability, and, finally,
ineffective embolectomy devices. It comes as no surprise that addressing these
specific issues led to clinically fruitful studies. It was the pragmatically designed
MR CLEAN (Multicenter Randomized Clinical Trial of Endovascular Treatment
for Acute Ischemic Stroke) study that paved the path for future successes of
interventional trials. Patients with middle cerebral artery– or internal carotid
artery–documented occlusions on a CT angiogram were randomly assigned to
conventional treatment or recanalization using mechanical stent retrievers with or
without thrombolysis within 6 hours of symptom onset. Independent outcomes
were seen in one of every seven patients treated with embolectomy.16
1662 DECEMBER 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Similarly, the REVASCAT (Randomized Trial of Revascularization With KEY POINT
Solitaire FR Device Versus Best Medical Therapy in the Treatment of Acute
● Circulation, airway, and
Stroke Due to Anterior Circulation Large Vessel Occlusion Presenting Within breathing stabilization
8 Hours of Symptom Onset)20 and ESCAPE (Endovascular Treatment for Small followed by rapid
Core and Anterior Circulation Proximal Occlusion With Emphasis on Minimizing neurologic assessment,
ogM/G3Lw98L4g53y0W25aSbX7CEFzDyuApk/85Hsqz5UhDeRfNPFhkYp95Mer+PxzV9+48F39Z4b5s+Btx/00RefYCHmPbzv2sNN
CT to Recanalization Times)17 trials evaluated the effect of thrombectomy by neuroimaging, and point of
care testing should be the
using the Alberta Stroke Program Early Computed Tomography Score (ASPECTS)
Downloaded from http://journals.lww.com/continuum by KjfsNO4rm+70wsgqTPXGiE1ivOxovFfe/bXXYpJT6n4lQzg
initial response in the
as a marker of tissue viability and CT angiography/magnetic resonance evaluation of patients
angiography (MRA) confirmation of intracranial occlusion, demonstrating presenting with acute
independent outcomes in one in seven or one in four patients, respectively. The ischemic stroke.
SWIFT-PRIME (Solitaire With the Intention for Thrombectomy as Primary
Endovascular Treatment)19 and EXTEND-IA (Extending the Time for
Thrombolysis in Emergency Neurological Deficits—Intra-arterial)18 trials used
CT perfusion studies to identify infarct core using RAPID software
(iSchemaView, Menlo Park, California), and when recanalized, one in four and
one in three patients, respectively, experienced functional independence.
LisNIokjeaJDU on 03/08/2023
In the immediate past, two trials have extended the traditional windows of
endovascular treatment for up to 24 hours. The DAWN (DWI or CT Perfusion
Assessment With Clinical Mismatch in the Triage of Wake-up and Late
Presenting Strokes Undergoing Neurointervention With Trevo) investigator–led
study evaluated patients who were last seen normal within 24 hours and
evaluated imaging for large vessel occlusion and used the RAPID software to
select patients with specific ischemic core volumes (SDC 4-1, links.lww.com/
CONT/A259).21 One out of every three patients treated experienced functional
independence. The very recently released DEFUSE 3 (Diffusion and pErFUsion
Imaging Evaluation for Understanding Stroke Evolution 3) study used perfusion
criteria to define an infarct volume (ischemic core) of less than 70 mL, a ratio
of volume of ischemic tissue to initial infarct volume of 1.8 or more, and an
absolute volume of potentially reversible ischemia (penumbra) of 15 mL or more.
One in every four patients has the potential to be independent when treated
using this protocol.22
It is only recently that tenecteplase has been used as a thrombolytic agent in
acute ischemic stroke. The EXTEND-IA TNK investigator–led study,
Tenecteplase Versus Alteplase Before Thrombectomy for Ischemic Stroke,
randomly assigned patients with intracranial occlusions who were within
4.5 hours of symptom onset to receive either rtPA or tenecteplase in addition to
thrombectomy.15 They observed that 22% of patients in the tenecteplase group
had more than 50% of occluded vessels reperfused or completely resolved
thrombus as compared to 11% in the group treated with rtPA. Outcomes
indicating independence in clinical function, defined by an mRS score of 2 or less,
was insignificant in both the groups. Both groups had similarly low rates of
symptomatic intracranial hemorrhage. Therefore, although tenecteplase seemed
to provide better brain reperfusion and thrombolysis, tenecteplase did not
seem to result in better clinical outcomes in patients with acute ischemic stroke
and an intracranial occlusion.15
INDICATIONS FOR INTENSIVE CARE UNIT ADMISSION
Patients who undergo thrombolysis and thrombectomy are usually at risk of
developing complications and are typically better served in an ICU and preferably
in the neurocritical care unit. It is reported that about one in four patients with
CONTINUUMJOURNAL.COM 1663
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
MANAGEMENT OF STROKE IN THE NEUROCRITICAL CARE UNIT
acute ischemic stroke post-thrombolysis will need critical care interventions
possible only in an ICU.8 Systemic complications in the setting of acute ischemic
stroke can pose significant secondary brain injury requiring care in a neurocritical
care unit. The following section will address complications in individual organ
systems that indicate admission to a neurocritical care unit (TABLE 4-3).
ogM/G3Lw98L4g53y0W25aSbX7CEFzDyuApk/85Hsqz5UhDeRfNPFhkYp95Mer+PxzV9+48F39Z4b5s+Btx/00RefYCHmPbzv2sNN
Neurologic Indications
Downloaded from http://journals.lww.com/continuum by KjfsNO4rm+70wsgqTPXGiE1ivOxovFfe/bXXYpJT6n4lQzg
Perhaps the most common reasons for admission to the neurocritical care unit are
neurologic indications, which are detailed below.
POST-THROMBOLYSIS/POST-THROMBECTOMY CARE AND HEMODYNAMIC
MONITORING. Because of variable practices across health care systems, patients
with acute ischemic stroke treated with thrombolysis are admitted to either a
dedicated stroke unit or to a neurocritical care unit. Both neurologic and
hemodynamic monitoring remains the mainstay of such admissions.
Management of hemodynamics (systolic blood pressure and diastolic blood
pressure parameters prethrombolysis and post-thrombolysis) should be followed
LisNIokjeaJDU on 03/08/2023
as directed by the American Heart Association guidelines and Brain Attack
Coalition.28,29 Post-thrombolysis, blood pressure should be maintained at less
than 180/105 mm Hg during the first 24 hours. Fluctuating neurologic symptoms
that correlate with hemodynamic changes will need either fluid management or
augmentation using vasopressors. More data are emerging supporting cardiac
output augmentation as more effective in enhancing cerebral perfusion.30 An
infrequent but life-threatening angioedema associated with the use of rtPA needs
aggressive airway management in an ICU setting.
CEREBRAL EDEMA. Cerebral edema is a common complication affecting patients
with acute ischemic stroke. Even in small infarcts, cerebral edema is associated
with a significant secondary brain injury.31 The subgroup of patients who are
at risk of severe life-threatening edema includes patients with posterior
circulation strokes with the involvement of more than 35% of the cerebellar
hemisphere and middle cerebral artery territory infarcts, which have a footprint
of more than 50% involvement of its territory on a CT scan. Clinically, that
usually is representative of any neurologic deficit greater than an NIHSS score of
15, with altered mentation.
SYMPTOMATIC HEMORRHAGIC TRANSFORMATION AND COAGULOPATHY.
Intracranial hemorrhagic transformation following acute ischemic stroke with or
without thrombolysis/thrombectomy has been found to range from 4% to 6%.32
Radiographic changes are classified as types 1 and 2 hemorrhagic infarctions
and types 1 and 2 parenchymal hematomas and extraischemic hematomas.
Hemorrhagic infarctions are petechial hemorrhages that immediately follow an
ischemic infarct and are seen in the first 1 to 2 weeks after an ischemic stroke. A
hemorrhagic infarct is type 1 if the radiographic appearance shows a multifocal
petechial pattern and is type 2 when an appearance of confluent hyperdensity
occurs throughout the infarcted area without a resultant mass effect.
Parenchymal hematomas show a homogenous appearance of hyperdensity and
are type 1 if the hematoma occupies less than one-third of the infarct zone
leading to some mass effect. Parenchymal hematomas are type 2 if the hematoma
involves more than one-third of the infarct zone with significant mass effect or if
it extends beyond the borders of the infarcted brain parenchyma. Extraischemic
1664 DECEMBER 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Indications for Admission to Neurocritical Care Unit in Patients With Acute TABLE 4-3
Ischemic Stroke
Neurologic Indications
ogM/G3Lw98L4g53y0W25aSbX7CEFzDyuApk/85Hsqz5UhDeRfNPFhkYp95Mer+PxzV9+48F39Z4b5s+Btx/00RefYCHmPbzv2sNN
◆ Hemodynamic management
Downloaded from http://journals.lww.com/continuum by KjfsNO4rm+70wsgqTPXGiE1ivOxovFfe/bXXYpJT6n4lQzg
◇ Post-thrombectomy
◇ Post IV thrombolysis
◇ Need for continuous hemodynamic support
◆ Cerebral edema
◇ Cerebellar stroke involving more than 25% to 33% of hemisphere
◇ Involvement of more than 50% of middle cerebral artery territory
◇ Signs of herniation
◆ Hydrocephalus
LisNIokjeaJDU on 03/08/2023
◆ Symptomatic hemorrhagic transformation and coagulopathy
◆ Coma with Glasgow Coma Scale score of <9
◆ Seizures requiring continuous IV medications
Cardiac Indications
◆ Hemodynamic augmentation
◆ Acute myocardial infarction requiring monitoring and hemodynamic support
◆ Cardiac rhythm abnormalities (such as atrial flutter/fibrillation)
◆ Congestive cardiac failure requiring continuous IV infusions
◆ Cardiac mechanical hardware on anticoagulation with moderate to large strokes
Respiratory Indications
◆ Respiratory failure requiring endotracheal intubation and mechanical ventilation
◆ Hypoxic respiratory failure
◆ Hypercarbic respiratory failure
◆ High suspicion of aspiration pneumonia
◆ Central respiratory failure
Infectious Indications
◆ Signs of sepsis or septic shock
Renal Indications
◆ Renal failure requiring renal replacement therapy
IV = intravenous.
CONTINUUMJOURNAL.COM 1665
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
MANAGEMENT OF STROKE IN THE NEUROCRITICAL CARE UNIT
hematomas, however, are areas of confluent hyperdensity that do not overlap
with the infarcted brain parenchyma.
Symptomatic intracranial hemorrhage, defined as any hemorrhage resulting
in a change in clinical status manifested by an NIHSS score increase of 4 points or
more, seems to affect patients with larger ischemic strokes, high systolic blood
ogM/G3Lw98L4g53y0W25aSbX7CEFzDyuApk/85Hsqz5UhDeRfNPFhkYp95Mer+PxzV9+48F39Z4b5s+Btx/00RefYCHmPbzv2sNN
pressure, diabetes mellitus, and, in certain cases, low plasminogen inhibitor
levels in serum, and is seen in less than 2% to 7% of patients. The radiographic
Downloaded from http://journals.lww.com/continuum by KjfsNO4rm+70wsgqTPXGiE1ivOxovFfe/bXXYpJT6n4lQzg
appearance of parenchymal hematoma type 2 is associated with consistently
poorer clinical outcomes and hence needs aggressive management in the
neurocritical care unit.
SEIZURES. Clinical ictal events following acute ischemic stroke are relatively rare
and may occur in about 1.3% of cases.33 Males with an NIHSS score of greater
than 10 are at risk, and the seizures themselves portend an independent poor
outcome (twofold to threefold increase in odds).
Cardiac Indications
LisNIokjeaJDU on 03/08/2023
Patients with acute ischemic stroke are prone to cardiac complications, which
need neurocritical care unit management, as detailed below.
MYOCARDIAL INFARCTION. Acute myocardial infarction is seen in 2% of all
patients with acute ischemic stroke with a cumulative risk over 10 years.34
Myocardial infarction in the setting of acute ischemic stroke is associated with
poor outcomes and increased mortality. Thus, close monitoring of the patients
in the ICU is warranted.
CARDIAC ARRHYTHMIAS. The most common arrhythmias following acute
ischemic stroke include atrial fibrillation and atrial flutter, reported in as many as
10% of patients.35 Rapid ventricular rate in atrial fibrillation requires immediate
management because of the resultant hemodynamic compromise.
CONGESTIVE HEART FAILURE. Left ventricular systolic dysfunction is reported
in as many as 28% of the population with acute ischemic stroke and diastolic
dysfunction in 18%. Congestive heart failure has been recognized as an independent
marker of poor outcomes in patients with ischemic stroke and is associated with
cardiac and pulmonary complications requiring monitoring in the ICU.
Respiratory Indications
Respiratory complications that indicate admission to the neurocritical care unit
are detailed below.
AIRWAY MANAGEMENT. The inability to maintain a patent airway because of
altered mentation seems to be the most common respiratory indication (47%)
for admitting patients with acute ischemic stroke to the neurocritical care unit.
PNEUMONIA. Stroke-associated pneumonia has been variably reported in the
literature with a wide range of 4% to 56% of all patients in the stroke units.36
Dysphagia and altered level of consciousness are partly contributory to pneumonia.
However, an increased incidence of pneumonia compared to similar neurologic
illnesses can be potentially explained by stroke-induced immunodepression.
Pneumonia confers a poor functional outcome and mortality as high as 49% to 60%
in patients with acute ischemic stroke as seen in multiple studies.
1666 DECEMBER 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
MECHANICAL VENTILATION. Approximately 1.3% of all patients with stroke KEY POINTS
undergo mechanical ventilation due to various causes of respiratory failure and
● The main neurologic
experience 40% to 80% mortality. Patients requiring mechanical ventilation reasons for intensive care
have associated poorer outcomes and a longer hospital stay, which could be unit admission in patients
due to the administration of sedatives and analgesics, ventilator-associated with acute ischemic stroke
ogM/G3Lw98L4g53y0W25aSbX7CEFzDyuApk/85Hsqz5UhDeRfNPFhkYp95Mer+PxzV9+48F39Z4b5s+Btx/00RefYCHmPbzv2sNN
pneumonia, or both. Various other miscellaneous complications of the include blood pressure
management
respiratory system occur that result in hypoxic or hypercarbic respiratory failure
Downloaded from http://journals.lww.com/continuum by KjfsNO4rm+70wsgqTPXGiE1ivOxovFfe/bXXYpJT6n4lQzg
post-thrombolysis or
that may be managed with mechanical ventilation or noninvasive modes of post-thrombectomy,
positive breathing, as will be mentioned later, but that require monitoring in the cerebral edema,
neurocritical care unit. symptomatic hemorrhagic
transformation, and
seizures.
Neurocritical Care Unit Triaging
Several predictive models have been created to assess appropriate triaging ● The main cardiac and
of patients with acute ischemic stroke to the neurocritical care unit. Of these, respiratory indications for
the ICAT score is a novel tool that scores based on the ethnicity, age, gender, admission of patients with
acute ischemic stroke to the
the degree of hypertension, and clinical severity of stroke measured by the
neurocritical care unit
LisNIokjeaJDU on 03/08/2023
NIHSS. Current literature suggests that for every point increase in the ICAT include myocardial
score, there is a 2.2-fold higher chance of requiring intervention. An ICAT infarction, cardiac
score of more than 2 has a 13-fold risk of requiring critical care intervention arrhythmias, heart failure,
and hence can potentially be used for triaging patients to the neurocritical inability to maintain the
airway, and the need for
care unit.8 mechanical ventilation.
INTENSIVE CARE UNIT MANAGEMENT
The critical care management of patients with acute ischemic stroke is complex.
An evidence-based approach is presented below, and when no or very little
evidence exists, the authors recommend what they and most other
neurointensivists do in their daily practice. The recommendations for ICU
management of patients with acute ischemic stroke are summarized in TABLE 4-4.
Neurologic Management
Neurologic complications that follow acute ischemic stroke need diligent
management, as is detailed below.
POST-THROMBOLYTIC AND POST-THROMBECTOMY CARE. The care of patients
post-thrombolysis and post-thrombectomy include neuromonitoring as
recommended by the American Heart Association and Brain Attack Coalition
guidelines, which include blood pressure measurement and neurologic
examination every 15 minutes for the first 2 hours after IV rtPA infusion, then
every 30 minutes for the next 6 hours, and subsequently every hour for the next
16 hours.28,29 As part of the neuromonitoring of patients, special attention should
be provided to the airway during or immediately after the IV administration of
rtPA because of the rare but potentially fatal angioedema association with its
administration. Concurrent use of lisinopril has been noted in the majority of
such patients. Changes in neurologic assessment should be emergently evaluated
by a noncontrast head CT scan. In addition, patients who have undergone
embolectomy will need monitoring of angiography access site(s) to assess for the
presence of hematoma and evaluation of peripheral pulses for determination
of distal perfusion. In the event of any hematoma collection, local mechanical
pressure application should be continued followed by correction of
underlying coagulopathy.
CONTINUUMJOURNAL.COM 1667
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
MANAGEMENT OF STROKE IN THE NEUROCRITICAL CARE UNIT
TABLE 4-4 Principles of Critical Care Management in Patients With Acute
Ischemic Stroke
Neurologic Critical Care
ogM/G3Lw98L4g53y0W25aSbX7CEFzDyuApk/85Hsqz5UhDeRfNPFhkYp95Mer+PxzV9+48F39Z4b5s+Btx/00RefYCHmPbzv2sNN
Issues Treatment Principles Treatment Specifics
Downloaded from http://journals.lww.com/continuum by KjfsNO4rm+70wsgqTPXGiE1ivOxovFfe/bXXYpJT6n4lQzg
Post-thrombolytic/ Neuromonitoring
post-thrombectomy
care Hemodynamic management See cardiac, cerebral perfusion control, and
hemorrhagic transformation for specific
management
Dysphagia assessment Nothing by mouth orders in anyone with suspected
dysphagia
Angioedema Diphenhydramine and other histamine 1 receptor
antagonists, corticosteroids
Access site hematoma Local pressure and coagulopathy reversal (see
LisNIokjeaJDU on 03/08/2023
hemorrhagic transformation for specific
management)
Cerebral perfusion Hypertension (for goals <185/110 mm Hg Short-acting injectable agents such as metoprolol,
control prethrombolysis and <180/105 mm Hg labetalol, enalaprilat, and hydralazine, or a
post-thrombolysis) continuous agent such as nicardipine
Vasopressor and inotropic support Epinephrine, norepinephrine, dobutamine, milrinone,
and dopamine
Hemorrhagic Hemodynamic management See hypertension treatment above; blood pressure
transformation parameters should be individualized, but systolic
blood pressure <160 mm Hg per intracerebral
hemorrhage management guidelines should be
followed when possible
Reversal of recombinant tissue Cryoprecipitate 10 U, repeated for goal fibrinogen
plasminogen activator administration level of >150 mg/dL; platelet transfusion 8–10 U, may
also consider recombinant factor VIIa 20–160 mcg/kg;
antifibrinolytic agents, aminocaproic acid 4 g IV first
hour followed by 1 g/h for 8 hours or tranexamic acid
10 mg/kg 3 to 4 times a day
Reversal of coagulopathy Platelet transfusion 8–10 U (for thrombocytopenia of
<100,000/mm3); fresh frozen plasma 12 mL/kg (for
patients on warfarin and especially with implanted
mechanical devices); prothrombin complex
concentrate 25–50 U/kg (based on international
normalized ratio level); vitamin K 10 mg IV (adjunctive
for reversing warfarin); recombinant factor VIIa
20–160 mcg/kg; antifibrinolytic agents, aminocaproic
acid 4 g IV first hour followed by 1 g/h for 8 hours or
tranexamic acid 10 mg/kg 3 to 4 times a day,
idarucizumab and andexanet alfa as needed for
reversal of newer anticoagulants.
IV = intravenous.
1668 DECEMBER 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
HEMODYNAMIC MANAGEMENT. Hemodynamic management of patients with
acute ischemic stroke is perhaps the most common indication for neurocritical
care unit admission. The American Heart Association and the Brain Attack
Coalition recommend that patients post-thrombolysis should be treated with
short-acting agents or continuous drip of medications for a blood pressure
ogM/G3Lw98L4g53y0W25aSbX7CEFzDyuApk/85Hsqz5UhDeRfNPFhkYp95Mer+PxzV9+48F39Z4b5s+Btx/00RefYCHmPbzv2sNN
goal of less than 185/110 mm Hg before thrombolysis and less than 180/
105 mm Hg for at least 24 hours post-thrombolysis. If the patients are not
Downloaded from http://journals.lww.com/continuum by KjfsNO4rm+70wsgqTPXGiE1ivOxovFfe/bXXYpJT6n4lQzg
being thrombolysed, the blood pressure goals should be changed to less than
220/120 mm Hg.28,29
An intact cerebral autoregulation ensures unimpeded cerebral perfusion when
blood pressures fluctuate. Loss of such autoregulatory mechanisms can lead to
either hyperperfusion or worsening of cerebral perfusion. In ischemic strokes,
generally the intracranial pressure remains unchanged in the hyperacute period,
and hence one can surmise that the mean arterial pressure and systemic
pressures are the sole determinants of cerebral perfusion pressures. Therefore,
hemodynamic monitoring becomes a clear priority.
LisNIokjeaJDU on 03/08/2023
Various techniques such as positron emission tomography (PET), transcranial
Doppler, and MRI-based studies have resulted in variable observations. Recently,
dynamic autoregulation has been widely studied with the use of MRI or transcranial
Doppler. (In these studies, a thigh pressure cuff is applied on a lower extremity
and inflated to isolate a significant volume of blood. Cerebral vascular pulse
contours can be measured using transcranial Doppler or special sequences in MRI.
Deflating the thigh pressure cuff augments the cardiac output, which provides an
opportunity to study how the intracranial vasculature can adapt to hemodynamic
changes. With measurements of intracranial vascular flows in two different
hemodynamic states, we can understand cerebrovascular autoregulation.)
In some studies of patients with acute ischemic stroke with large vessel
occlusions, autoregulation has been demonstrated to be severely affected.37
Furthermore, patients with impaired autoregulation in the hemisphere affected
by stroke seemed to have worse outcomes when compared to patients with
preserved autoregulation. Moreover, in studies using concomitant transcranial
Doppler and arterial blood pressure waveform analyses, it is noted that an
impaired autoregulatory index can be appreciated for the first week following
acute ischemic stroke and normalized within the following week.38
Conflicting observations refuting the presence of autoregulatory failure also
are abundant in the literature. Studies evaluating autoregulation using various
modalities have found that although there is a difference between autoregulation
in patients with acute ischemic stroke and normal controls, there appears to be no
clear difference between the affected and unaffected hemispheres in patients
with acute ischemic strokes.39 Several factors are responsible for producing these
variable observations. First, patient selection in individual studies varied widely;
while some focused on moderate to large ischemic infarcts, some clearly defined
large vessel ischemia as the selection criteria. Second, multiple modalities have
been used in the evaluation of autoregulation, which makes it difficult to compare
the studies in an objective manner. Third, within evaluations of an individual
modality, researchers have used different parameters to define autoregulation.
Finally, the studies always compare immediate physiologic outcomes while
standardized long-term clinical outcomes are not reported. Given these
shortcomings, it is not surprising that such a vast difference is seen in the observed
outcomes of cerebral autoregulatory changes in acute ischemic stroke.
CONTINUUMJOURNAL.COM 1669
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
MANAGEMENT OF STROKE IN THE NEUROCRITICAL CARE UNIT
It is important to understand that admission blood pressures have a U-shaped
response in patients with acute ischemic stroke, with poor outcomes occurring
in patients presenting with the lowest and the highest values.40 Clinical trials
have tried to address the safety of reducing blood pressures in the setting of
acute ischemic stroke. The SCAST (Angiotensin-receptor Blocker Candesartan
ogM/G3Lw98L4g53y0W25aSbX7CEFzDyuApk/85Hsqz5UhDeRfNPFhkYp95Mer+PxzV9+48F39Z4b5s+Btx/00RefYCHmPbzv2sNN
for Treatment of Acute Stroke Trial) study evaluated blood pressure
management in acute stroke by randomly allocating patients with acute ischemic
Downloaded from http://journals.lww.com/continuum by KjfsNO4rm+70wsgqTPXGiE1ivOxovFfe/bXXYpJT6n4lQzg
stroke presenting with a systolic blood pressure of greater than 140 mm Hg to
treatment with either candesartan or placebo. Although the blood pressures were
significantly lower in the candesartan group, no significant difference was found
between the groups in mRS at 6 months or in the composite end point of vascular
death, myocardial infarction, or stroke during the first 6 months.41 Similarly, the
COSSACS (Continue or Stop Poststroke Antihypertensives Collaborative Study)
trial enrolled patients with acute ischemic stroke to stop the home regimen of
antihypertensive medications to evaluate the presence of improved outcomes
and better perfusion as manifested by higher blood pressures.42 The trial was
LisNIokjeaJDU on 03/08/2023
underpowered and observed no differences between the groups.
The CATIS (China Antihypertensive Trial in Acute Ischemic Stroke) study
enrolled the intended 4071 participants with acute ischemic stroke who presented
with a systolic blood pressure of 140 mm Hg to 220 mm Hg. CATIS investigators
randomly assigned patients to either an antihypertensive arm, which consisted of
lowering admission blood pressure by 10% to 25% within the first 24 hours after
randomization and a blood pressure goal of less than 140/90 mm Hg within 7 days,
or a complete stopping of all antihypertensive treatment during hospitalization.
The authors reported no difference in the primary outcome of death or an mRS
score of ≥3 at 2 weeks or hospital discharge between treatment arms.43
Another large study, the ENOS (Efficacy of Nitric Oxide in Stroke) clinical
trial, enrolled 4011 patients with ischemic or hemorrhagic stroke with a systolic
blood pressure of 140 mm Hg to 220 mm Hg on admission. The patients were
randomly assigned to either 7 days of transdermal nitrate therapy at 5 mg/d or
placebo. Similar to the other clinical trials, the ENOS investigators reported no
difference in the 90-day mRS score between the treatment arms.44 Currently, it
is recommended to reduce the blood pressure to less than 180/105 mm Hg for
patients with acute ischemic stroke post-thrombolysis.
As mentioned above, mechanical thrombectomy trials have benefited the
landscape of stroke treatment since 2015. With the use of stent retrievers, several
trials have demonstrated outcome improvement by 14% to 36%, which translates
as the total number of patients needed to treat to achieve one person who is
independent at 3 months between 3 and 7.16–21,45 The patients assigned to the
thrombectomy arm had reperfusion (defined as Thrombolysis in Cerebral
Infarction [TICI] grades of 2B to 3) rates of 59% to 88%. This variability in the
reperfusion rates is likely related to the study design, patient selection, treatment
times, study power, and overall different set of the population being analyzed. Of
note, no difference was found in mortality between the treatment groups across
the trials. It is currently unknown whether hemodynamic parameters need to be
changed based on the degree of reperfusion. However, it is important to
individualize blood pressure parameters in patients, especially when there is a
worsening neurologic examination associated with lower blood pressures.
Vasopressors or inotropic agents should be used to improve the neurologic
examination. A trial of an individual agent is recommended initially to assess
1670 DECEMBER 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
neurologic examinations for a set pressure parameter, and readjusting the goals KEY POINTS
or treating agents should be performed dynamically (CASE 4-1).
● Management of
hemodynamics in patients
HEMORRHAGIC TRANSFORMATION. Neurologic worsening in the setting of with fluctuating neurologic
intracranial hemorrhage following acute ischemic stroke is associated with poor symptoms should be
ogM/G3Lw98L4g53y0W25aSbX7CEFzDyuApk/85Hsqz5UhDeRfNPFhkYp95Mer+PxzV9+48F39Z4b5s+Btx/00RefYCHmPbzv2sNN
outcomes and mortality rates of up to 50%, especially in patients with targeted individually and
adjusted for optimum
parenchymal hematoma type 2 (confluent hematoma that involves more than
Downloaded from http://journals.lww.com/continuum by KjfsNO4rm+70wsgqTPXGiE1ivOxovFfe/bXXYpJT6n4lQzg
symptom control.
one-third of infarcted tissue, as detailed above), which represents the majority of
all symptomatic intracranial hemorrhages.46 Most of these hemorrhages occur ● Interpretation of the
within 12 hours following IV thrombolysis, with a median time of 8 hours.47,48 neurologic evaluation of
It is important to point out that neurologic deterioration may not be obvious patients with acute ischemic
stroke with larger deficits
because of the hematoma development in the infarcted tissue. Changes in can be obscured when only
neurologic status are usually heralded by the expansion of the hematoma using the National Institutes
into noninfarcted tissues, mass effect, or extension onto the CSF-filled spaces. of Health Stroke Scale and
Also, neurologic patients who have severe baseline stroke impairment may no other clinical parameters.
not manifest a change in the neurologic status because of the ceiling effect of
LisNIokjeaJDU on 03/08/2023
the clinical examination and NIHSS. Therefore, a low threshold for follow-up
neuroimaging studies should be maintained. Two important factors in
determining the outcomes of symptomatic intracranial hemorrhage are
rapid hemodynamic control and correction of underlying coagulopathy.49
Symptomatic intracranial hemorrhage as a manifestation of cerebral
hyperperfusion has been noted mostly in patients undergoing elective carotid
surgical and endovascular revascularization but has occasionally been reported
after mechanical embolectomy.50 In a meta-analysis involving all factors
influencing the association of hyperperfusion and intracranial hemorrhage in the
setting of carotid reperfusion, patients undergoing carotid endarterectomy had
an increased odds of developing hyperperfusion (odds ratio of 1.4 times) as
compared to patients undergoing carotid stenting.45 Since hyperperfusion
manifests itself as a hemorrhagic stroke, evaluation of the symptomatic
intracranial hemorrhage rates in the embolectomy trials may be helpful to
identify potential patients for stricter hemodynamic control. Symptomatic
intracranial hemorrhage rates in patients treated with embolectomy were not
reported in the EXTEND-IA and the SWIFT-PRIME studies, while REVASCAT
had the same rates as the control group at 1.9%. The ESCAPE study showed a
symptomatic intracranial hemorrhage rate of 3.6%, while MR CLEAN had 7.7%
in those patients treated with embolectomy. Imaging-based selection of patients
who were beyond the traditional 6-hour window for treatment with mechanical
thrombectomy resulted in symptomatic intracranial hemorrhage rates of
6%, despite a mean time of revascularization of 13 hours after the onset of
symptoms. Hemodynamic regulation has the potential to prevent hemorrhagic
transformation. However, it is unclear as to how to individualize parameters to
obtain optimum perfusion and to prevent hyperperfusion that can lead to
hemorrhage. Until further evidence is available, best judgment should be used
to personalize hemodynamic parameters to balance cerebral, systemic, and
cardiac perfusion (CASE 4-2).
Correction of coagulopathy should be individualized based on whether patients
have received IV thrombolysis or active anticoagulant use. In patients who have
received thrombolysis with rtPA, assessment of plasma fibrinogen levels and
correction with IV cryoprecipitate (10 U) for a goal of more than 150 mg/dL should
be initiated at the earliest opportunity, as these steps perhaps have the most benefit
CONTINUUMJOURNAL.COM 1671
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
MANAGEMENT OF STROKE IN THE NEUROCRITICAL CARE UNIT
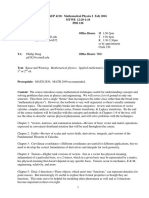
CASE 4-1 A 57-year-old right-handed man presented to the emergency department
for evaluation of left-sided weakness, numbness, and loss of vision he
noticed upon waking after going to bed 4 hours earlier. He had a history of
atrial fibrillation and nonischemic cardiomyopathy and had been
ogM/G3Lw98L4g53y0W25aSbX7CEFzDyuApk/85Hsqz5UhDeRfNPFhkYp95Mer+PxzV9+48F39Z4b5s+Btx/00RefYCHmPbzv2sNN
prescribed dabigatran with unknown compliance.
On examination, he had a left hemiplegia, hemianesthesia, hemineglect,
Downloaded from http://journals.lww.com/continuum by KjfsNO4rm+70wsgqTPXGiE1ivOxovFfe/bXXYpJT6n4lQzg
and left hemianopsia, which yielded a National Institutes of Health Stroke
Scale (NIHSS) score of 13.
Admission head CT showed a hyperdense right middle cerebral artery
sign (FIGURE 4-1A). He underwent thrombectomy with a full Thrombolysis
in Cerebral Infarction (TICI) grade 3 recanalization (FIGURE 4-1B and
FIGURE 4-1C), after which his NIHSS score improved to 3.
During his neurocritical care unit stay, his weakness worsened as his
systolic blood pressure decreased from 170 mm Hg to 110 mm Hg. He was
started on an IV norepinephrine infusion to elevate his systolic blood
LisNIokjeaJDU on 03/08/2023
pressure, after which his neurologic symptoms improved. However, he
experienced pulmonary edema of cardiac origin, for which he received
diuretics, and the norepinephrine infusion was titrated down followed by
dobutamine and milrinone infusions. His hemodynamic status was
monitored using an arterial catheter and attached noninvasive cardiac
output monitor, which allowed for the titration of his medications to
regulate his peripheral vascular resistance and cardiac output. His left
ventricular ejection fraction evaluated by transthoracic echocardiogram
initially was 20%, down from his baseline of 40% to 45%. The patient was
diagnosed with non–ST segment elevation myocardial infarction with
troponinemia, which was treated with an IV heparin drip with a lower
partial thromboplastin time (PTT) goal initially poststroke, in coordination
with the cardiology team.
FIGURE 4-1
Imaging of the patient in CASE 4-1. A, Head CT showing a hyperdense right middle cerebral
artery sign (arrow). B, Cerebral angiogram showing a distal right internal carotid artery
occlusion. C, Cerebral angiogram obtained after thrombectomy demonstrating Thrombolysis
in Cerebral Infarction (TICI) grade 3 recanalization. D, MRI of the brain showing no
abnormalities suggestive of cerebral infarction on diffusion-weighted imaging (DWI).
1672 DECEMBER 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Within the next 2 days, his respiratory and cardiac symptoms
improved, his left ventricular ejection fraction improved to his baseline
values, and his NIHSS score normalized to 0 upon discharge, as
evidenced by lack of any diffusion-weighted image (DWI) changes on his
ogM/G3Lw98L4g53y0W25aSbX7CEFzDyuApk/85Hsqz5UhDeRfNPFhkYp95Mer+PxzV9+48F39Z4b5s+Btx/00RefYCHmPbzv2sNN
MRI (FIGURE 4-1D). He was started on rivaroxaban for compliance issues and
remained symptom free.
Downloaded from http://journals.lww.com/continuum by KjfsNO4rm+70wsgqTPXGiE1ivOxovFfe/bXXYpJT6n4lQzg
This case demonstrates the need for individualization of care, using COMMENT
noninvasive monitoring devices to optimize hemodynamics, and highlights
coordination of management between care teams. The patient was not
eligible for IV recombinant tissue plasminogen activator as his intake of oral
anticoagulants was uncertain and no laboratory test was available to
determine the activity of his anticoagulant. Hence, he was treated with
embolectomy. Despite complete recanalization, subsequent
LisNIokjeaJDU on 03/08/2023
compromised hemodynamics resulted in worsening of his neurologic
deficits. He was initially supported by vasopressors that likely resulted in
congestive cardiac failure due to systolic failure of the left ventricle caused
by increased afterload. He likely developed non–ST segment elevation
myocardial infarction due to Takotsubo cardiomyopathy and pump failure.
Noninvasive cardiac monitoring was used to determine optimum
vasopressor and inotrope dosage to perfuse the brain while not
exacerbating cardiac decompensation.
This case also illustrates cautious use of anticoagulants in the setting
of acute ischemic stroke. In the setting of an acute ischemic stroke,
anticoagulation is usually not recommended. In this case, the patient
developed troponinemia with non–ST elevated myocardial infarction on
ECG, which necessitated the use of anticoagulation. After ensuring the
absence of any parenchymal injury on MRI, the patient was started on a
heparin infusion with lower anticoagulation goals (PTT of 50 to 60 seconds
instead of the standard 60 to 80 seconds). Noninvasive monitoring of
cardiac and neurologic status in patients can be very helpful in optimizing
personalized care for patients who are critically ill.
CONTINUUMJOURNAL.COM 1673
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
MANAGEMENT OF STROKE IN THE NEUROCRITICAL CARE UNIT
CASE 4-2 A 68-year-old man presented to the emergency department with a left
hemiplegia, hemianesthesia, and right gaze preference that began
2 hours before presentation. His head CT was remarkable for a right
middle cerebral artery hyperdense sign. He received IV recombinant
ogM/G3Lw98L4g53y0W25aSbX7CEFzDyuApk/85Hsqz5UhDeRfNPFhkYp95Mer+PxzV9+48F39Z4b5s+Btx/00RefYCHmPbzv2sNN
tissue plasminogen activator (rtPA), and CT angiography demonstrated a
right middle cerebral artery occlusion (FIGURE 4-2A). With a National
Downloaded from http://journals.lww.com/continuum by KjfsNO4rm+70wsgqTPXGiE1ivOxovFfe/bXXYpJT6n4lQzg
Institutes of Health Stroke Scale (NIHSS) score of 12, he underwent
thrombectomy with a resultant Thrombolysis in Cerebral Infarction (TICI)
grade 3 recanalization (FIGURE 4-2B and FIGURE 4-2C).
LisNIokjeaJDU on 03/08/2023
FIGURE 4-2
Imaging of the patient in CASE 4-2. CT angiogram (A) and cerebral angiogram (B) demonstrating
an occlusive thrombus (arrows), and post-thrombectomy cerebral angiogram showing
Thrombolysis in Cerebral Infarction (TICI) grade 3 recanalization (C). Noncontrast head
CTs showing intraparenchymal hemorrhage (D, arrow) and right hemispheric edema, and
after right hemicraniectomy for malignant right hemispheric edema (E).
1674 DECEMBER 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
His NIHSS score worsened to 18 within 4 hours of IV rtPA administration
despite his systolic blood pressure being under control on a nicardipine
drip. A repeat head CT demonstrated intracranial hemorrhage with
worsening edema (FIGURE 4-2D). His systolic blood pressure goal was
ogM/G3Lw98L4g53y0W25aSbX7CEFzDyuApk/85Hsqz5UhDeRfNPFhkYp95Mer+PxzV9+48F39Z4b5s+Btx/00RefYCHmPbzv2sNN
reduced to 160 mm Hg, and he received 10 U of cryoprecipitate. His serum
fibrinogen levels improved from 80 mg/dL to 154 mg/dL. The
Downloaded from http://journals.lww.com/continuum by KjfsNO4rm+70wsgqTPXGiE1ivOxovFfe/bXXYpJT6n4lQzg
cryoprecipitate was used to reverse rtPA activity and to aid in reducing
intracranial hemorrhage expansion in anticipation of possible surgical
intervention.
A neurosurgical consultation was sought, and he underwent
prophylactic hemicraniectomy for cerebral edema (FIGURE 4-2E). Platelet
infusion was initiated during surgery. His hospital stay was remarkable
for new-onset atrial fibrillation with rapid ventricular response that
required rate control and mechanical ventilation support for 1 week
following hemicraniectomy. Three weeks following the hemorrhagic
LisNIokjeaJDU on 03/08/2023
transformation, the patient was started initially on a heparin drip and
eventually transitioned to warfarin. The latter was chosen after
discussion with patient’s family regarding all therapeutic options. He was
extubated after a week of mechanical ventilator support and eventually
was discharged to a skilled nursing facility.
Cranioplasty was performed after 2 months under careful transition
of warfarin to heparin, and he was eventually restarted on oral
anticoagulation with warfarin. Follow-up at 3 months revealed improved
dysarthria and left spastic hemiparesis, but the patient was ambulatory
with the help of a walker.
Thrombolysis and thrombectomy were performed in this patient upon COMMENT
presentation. The hemorrhagic complication associated with rtPA in this
patient was treated with hemodynamic management and coagulopathy
control by administering cryoprecipitate. Malignant cerebral edema was
treated with hemicraniectomy. Atrial fibrillation was detected during the
admission, and careful anticoagulation was initiated with IV heparin and
eventually transitioned to warfarin. The patient was transitioned to
rehabilitation and recovered with moderate disability. Management of
patients with acute ischemic stroke requires a multidisciplinary approach,
and the treatment of each individual complication should be approached
with personalized goals of care.
CONTINUUMJOURNAL.COM 1675
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
MANAGEMENT OF STROKE IN THE NEUROCRITICAL CARE UNIT
of all the treatment options. It is estimated that for every 10 U of cryoprecipitate
administered, plasma fibrinogen levels increase by an average of 55 mg/dL to
60 mg/dL. While interpreting the levels of fibrinogen, it is important to realize
that it is one of the acute phase reactants, and hence a lower level is more
reliable, and a normal level should be considered with healthy skepticism.
ogM/G3Lw98L4g53y0W25aSbX7CEFzDyuApk/85Hsqz5UhDeRfNPFhkYp95Mer+PxzV9+48F39Z4b5s+Btx/00RefYCHmPbzv2sNN
Other treatments that could be considered in the right setting include platelet
transfusion, fresh frozen plasma, prothrombin complex concentrate, activated
Downloaded from http://journals.lww.com/continuum by KjfsNO4rm+70wsgqTPXGiE1ivOxovFfe/bXXYpJT6n4lQzg
factor VII, antifibrinolytic medications, and reversal agents for direct acting
oral anticoagulants. Platelet transfusions of 6 U to 8 U are also usually
recommended based on a theoretic concern of thrombolysis inhibiting platelet
function. Furthermore, platelet transfusions can also be used to correct
thrombocytopenia for platelet counts of less than 100,000/μL. Fresh frozen
plasma contains endogenous procoagulant and anticoagulant proteins that
enhance intrinsic and extrinsic pathways with an end result of converting
fibrinogen to fibrin. Fresh frozen plasma is used at a dose of 12 mL/kg while
treating patients with hemorrhagic complications from rtPA. Prothrombin
LisNIokjeaJDU on 03/08/2023
complex concentrate is a concentrated form of vitamin K–dependent clotting
factors (II, VII, IX, and X) along with proteins C and S. Prothrombin complex
concentrate is the first-line treatment for warfarin-associated intracranial
hemorrhage and is extremely helpful by reducing the volume and time of IV
infusion required to achieve reversal of anticoagulation, which is usually in
30 minutes. Activated factor VII and vitamin K are used as adjuncts to reverse
warfarin. Use of prothrombin complex concentrate and activated factor VII
should be undertaken cautiously in patients with mechanical cardiac supports
and valves. The thrombogenic nature of the reversal agents can result in
mechanical cardiac valve dysfunction and clotting of the lines of mechanical
heart support devices. In such a situation, fresh frozen plasma seems to be an
optimal choice for regulating anticoagulation but presents challenges with
volume expansion and furthering cardiac stresses. Antifibrinolytic agents such
as tranexamic acid and aminocaproic acid can be used sparingly in an attempt to
prevent hematoma expansion. However, these agents also have a tendency to
cause deep vein thrombosis and cardiac and systemic thrombosis and are best
avoided in patients with mechanical heart devices and valves.
Direct-acting oral anticoagulants are increasingly being used in clinical
practice and pose a unique challenge for reversing their actions. As of now, the
agent idarucizumab, which is approved by the US Food and Drug Administration
(FDA), used at 5 g IV dose, is the only medication available to reverse the
effect of dabigatran. Agents such as rivaroxaban, apixaban, and edoxaban have
limited ability to be reversed. A factor X mimic, andexanet alfa, has been studied
and reported to reverse the activity of the direct-acting oral anticoagulants and
is only recently available for clinical use.51 Surgery should be considered after
correcting coagulopathy in selected patients where hematoma may be surgically
accessible by minimally invasive, stereotactic intervention or craniotomy, or for
decompressive hemicraniectomy.
CEREBRAL EDEMA. Cerebral edema is seen in patients with moderate to large
acute ischemic strokes and can independently worsen clinical outcomes.31
Malignant cerebral edema manifesting as a hemispheric syndrome in
combination with altered mental state and impending herniation and death is
seen in 10 to 20 per 100,000 people. It is more frequent in women and younger
1676 DECEMBER 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
patients because of low compensatory intracranial space. Most of the trials KEY POINTS
assessing the prophylactic management of such severe edema have sought
● In patients with acute
surgical treatment with hemicraniectomy, with a minimal flap diameter of 15 cm. ischemic stroke, treatment
A pooled analysis of the clinical trials DECIMAL (Decompressive Craniectomy in of hemorrhagic
Malignant Middle Cerebral Artery Infarction), DESTINY (Decompressive transformation should be
ogM/G3Lw98L4g53y0W25aSbX7CEFzDyuApk/85Hsqz5UhDeRfNPFhkYp95Mer+PxzV9+48F39Z4b5s+Btx/00RefYCHmPbzv2sNN
Surgery for the Treatment of Malignant Infarction of the Middle Cerebral directed toward
hemodynamic control and
Artery), and HAMLET (Hemicraniectomy After Middle Cerebral Artery
Downloaded from http://journals.lww.com/continuum by KjfsNO4rm+70wsgqTPXGiE1ivOxovFfe/bXXYpJT6n4lQzg
coagulopathy reversal.
Infarction With Life-threatening Edema Trial) indicated that performing
hemicraniectomy in patients with malignant cerebral edema reduced mortality ● Recombinant tissue
by 50% and improved outcomes by 16%.52 Improved outcomes are seen plasminogen
mainly in patients younger than 60 years of age who present with an NIHSS activator–related
symptomatic intracranial
score of greater than 15 and evidence of middle cerebral artery infarction hemorrhage should be
involving more than 50% of its territory, and in whom surgery can be performed treated initially with
within 48 hours of symptom onset. While the benefit of hemicraniectomy was cryoprecipitate.
studied in a younger population in these studies, the DESTINY-2 study
● While interpreting the
demonstrated this benefit even in patients older than 60 years of age.53 The levels of fibrinogen, it is
LisNIokjeaJDU on 03/08/2023
concern that a lifesaving hemicraniectomy for prolonged life would leave important to realize that it is
patients with a moderate to severe disability was addressed in a survey where one of the acute phase
health professionals were given the options of treatment with consequent reactants and, hence, a
lower level is more reliable,
outcomes. The majority of the decision makers were agreeable to a
and a normal level should be
hemicraniectomy but were unlikely to accept the resultant quality of life. considered with healthy
After the clinical efficacy was explained, the majority did not consider skepticism.
hemicraniectomy but seemed to accept the resultant dependency.54 Therefore,
discussions with the patient’s next of kin should involve a description of ● Patients with acute
ischemic stroke with a
outcomes to provide clarity to make decisions for care. There is overwhelming National Institutes of Health
practice to perform surgical decompressions of cerebellar stroke. In a study of Stroke Scale score of
patients with cerebellar infarcts involving 25% to 33% of a hemisphere without greater than 15, altered
brainstem strokes, prophylactic suboccipital decompression prevented sensorium, and infarction of
more than 50% of the middle
significant neurologic deterioration.55 cerebral artery territory
should be considered
SEIZURES. Seizures seem to affect around 2% of the acute ischemic stroke for prophylactic
population within 24 hours.56 Initial resuscitation should focus on circulation, hemicraniectomy within
48 hours.
airway, and breathing followed by benzodiazepines such as IV lorazepam or IM
midazolam. The use of loading antiepileptic drugs followed by IV continuous ● Patients with acute
sedative agents for the management of refractory status epilepticus should be ischemic stroke who present
considered along with EEG monitoring.57 For more information, refer to the with cerebellar strokes
involving more than 25%
article “Status Epilepticus, Refractory Status Epilepticus, and Super-refractory
to 33% of a hemisphere
Status Epilepticus” by Sarah E. Nelson, MD, and Panayiotis N. Varelas, MD, should be considered for
PhD, FNCS, FAAN,58 in this issue of Continuum. suboccipital decompressive
craniectomy.
Cardiopulmonary Complications
Myocardial infarction in the setting of acute ischemic stroke needs careful
management. Hemodynamic management should be personalized based on the
systemic, cardiac, and cerebral perfusion needs for that patient. Use of
anticoagulants and antiplatelet agents to treat cardiac and pulmonary thrombotic
episodes should be evaluated based on the volume of the cerebral infarct,
hemorrhagic risks, and cardiac status. Although anticoagulation in patients with
acute ischemic stroke can be associated with increased risk of hemorrhagic
stroke, studies indicate that when initiated between 4 and 14 days, complications
can be minimized.55 Coronary revascularization procedures also should be
CONTINUUMJOURNAL.COM 1677
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
MANAGEMENT OF STROKE IN THE NEUROCRITICAL CARE UNIT
carefully considered as these entail the use of dual antiplatelet agents and
should be carefully coordinated with cardiologists.
Tachyarrhythmias and bradyarrhythmias are frequently seen in patients with
acute ischemic stroke. Atrial fibrillation is commonly seen and is best managed
with rate control aiming for less than 110 beats/min.59 Short-acting IV
ogM/G3Lw98L4g53y0W25aSbX7CEFzDyuApk/85Hsqz5UhDeRfNPFhkYp95Mer+PxzV9+48F39Z4b5s+Btx/00RefYCHmPbzv2sNN
beta-blockers and calcium channel blockers, digoxin and amiodarone, should be
considered. Atropine, cardioselective beta-agonists, and electrical pacing should
Downloaded from http://journals.lww.com/continuum by KjfsNO4rm+70wsgqTPXGiE1ivOxovFfe/bXXYpJT6n4lQzg
be the mainstay of treating bradyarrhythmias. Patients with mechanical implanted
devices pose an immediate need for resumption of anticoagulants, which should
be balanced against the risk of hemorrhagic transformation. Coordinated
management along with an experienced cardiac team is recommended.
Pulmonary complications usually stem from altered mentation and the
inability to protect the airway, aspiration pneumonia, and underlying primary
pulmonary pathology. In the neurocritical care unit, the incidence of pneumonia
in patients with stroke is variably reported between 10% and 56%.36 With the
increasing incidence of obstructive sleep apnea, there has been an increase in
LisNIokjeaJDU on 03/08/2023
the use of noninvasive positive pressure ventilation. In a meta-analysis, no
significant difference in secondary stroke or other vascular morbidity or
mortality was seen in patients treated with noninvasive positive pressure
ventilation, but there seemed to be an overall improvement in the
clinical outcomes.60
Many centers perform routine endotracheal intubation for patients
undergoing mechanical embolectomy. However, post hoc analysis of the MR
CLEAN study demonstrated clearly worse outcomes in the routine use of general
anesthesia in patients undergoing mechanical thrombectomy compared to
patients undergoing conscious sedation.61 In the SIESTA (Sedation Versus
Intubation for Endovascular Stroke Treatment) study, the primary outcome
was defined as a neurologic improvement within 24 hours. In that respect, no
difference was found between patients undergoing general anesthesia and
conscious sedation. However, many complications occurred in the general
anesthesia group, such as delayed extubation, hypothermia, and pneumonia.
Surprisingly, 3-month outcomes as measured by mRS were significantly better
in the general anesthesia group.62
In a case series, as many as 14% of patients with acute ischemic stroke had
respiratory insufficiency requiring mechanical ventilation.63 Furthermore, when
compared to patients without respiratory insufficiency, patients who were
ventilated had 1.4 times higher risk of 1-year mortality. This risk was further
exemplified if the patients were stuporous (2.6 times) or if they had absent
corneal reflexes or ischemic heart disease (3.4 times).64 The authors of this
article discourage the routine use of endotracheal intubation and mechanical
ventilation in the management of patients with acute ischemic stroke.
In patients who are intubated, it is unclear if early tracheostomy can
facilitate early mobilization and enhance early recovery. The SETPOINT2
(Stroke-related Early Tracheostomy Versus Prolonged Orotracheal Intubation
in Neurocritical Care Trial) study is actively enrolling patients to address
this question.65
FUTURE OF ACUTE ISCHEMIC STROKE TREATMENT
This is an exciting time for stroke research as new clinical trials and
observational studies provide new evidence to enhance the treatment options
1678 DECEMBER 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
for patients with acute ischemic stroke. DEFUSE 3 has recently announced a KEY POINTS
favorable outcome in patients selected by imaging criteria for embolectomy
● Short-acting IV agents
when presenting between 6 and 16 hours of symptoms. It is anticipated that should be used to provide
more patients with acute ischemic stroke will be eligible for embolectomy, as optimal hemodynamic
the WAKE-UP (Efficacy and Safety of MRI-Based Thrombolysis in Wake-up management in patients with
ogM/G3Lw98L4g53y0W25aSbX7CEFzDyuApk/85Hsqz5UhDeRfNPFhkYp95Mer+PxzV9+48F39Z4b5s+Btx/00RefYCHmPbzv2sNN
Stroke) and EXTEND (Extending the Time for Thrombolyis in Emergency acute ischemic stroke.
Neurological Deficits [International]) trials address the ability to perform
Downloaded from http://journals.lww.com/continuum by KjfsNO4rm+70wsgqTPXGiE1ivOxovFfe/bXXYpJT6n4lQzg
● Early mobilization in the
mechanical embolectomy in patients with wake-up stroke. Furthermore, intensive care unit should be
studies are ongoing to determine the ability to triage these patients earlier encouraged in patients with
and more accurately by using a mobile stroke unit where initiation of acute ischemic stroke.
thrombolysis can be performed at the site. Expansion of telestroke networks is
● When possible,
also anticipated and thus will certainly rearrange local and regional stroke endotracheal intubation and
systems of care to adapt to new treatment paradigms. Further research general anesthesia
addressing the metabolic demands of patients with acute ischemic stroke via the administration should be
SHINE (Stroke Hyperglycemia Insulin Network Effort) study and early avoided for patients
undergoing mechanical
tracheostomy and mobilization through the SETPOINT2 clinical trial are thrombectomy.
LisNIokjeaJDU on 03/08/2023
anticipated soon.
CONCLUSION
This article is meant to highlight the main points in the critical care management
of patients with acute ischemic stroke and supplement the information in the
Continuum series addressing the management of acute ischemic stroke.66
Significant advances have been made in the treatment of patients with acute
ischemic stroke over the last decade. In 1995, initiation of thrombolysis was once
the only mainstay of treatment. The armamentarium to tackle stroke has taken a
significant step forward with the interventional trials, which have extended the
treatment windows from 4.5 hours through 24 hours. Despite these strides, we
still are left with many unanswered questions in the management of patients
with acute ischemic stroke. Peri-interventional anesthetic and hemodynamic
management still need further clarification. A large population still exists who
are not eligible for thrombectomy or thrombolysis who will need novel treatment
strategies. We are still unsure about the optimal hemodynamic management in
patients with acute ischemic stroke with or without thrombectomy. Clinical
management is driven by the symptom-based response, but no clear
neuromonitoring strategies have been developed to predict neurologic
worsening. A noninvasive measurement such as dynamic autoregulation seems
to have promising potential to intervene prior to neurologic decompensation.
Further research should be conducted to optimize stroke outcomes based on
hemodynamic management.
It is still unclear how to identify patients who will develop symptomatic
intracerebral hemorrhage. The management of such hemorrhages currently is
reflexive use of plasma products without clear evidence for improvement in
outcomes. Especially in patients with mechanical cardiac valves and support
devices, balancing between symptomatic intracranial hemorrhage expansion and
cardiac protection is a tough clinical decision. Clarity for management is very
much desired here.
Cerebral edema has been conventionally managed with osmotherapy and
surgical decompression. Newer approaches to reduce edema formation and
prevent secondary cerebral injury are warranted, especially in patients who
CONTINUUMJOURNAL.COM 1679
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
MANAGEMENT OF STROKE IN THE NEUROCRITICAL CARE UNIT
would not be candidates for either treatment. Furthermore, the burden of
addressing these issues has to be shared by the health care community.
Enrolling patients in trials whenever possible should be actively pursued.
Interest has grown in a collaborative approach between specialties and societies
to address many such issues, and we anticipate that such continued efforts will
ogM/G3Lw98L4g53y0W25aSbX7CEFzDyuApk/85Hsqz5UhDeRfNPFhkYp95Mer+PxzV9+48F39Z4b5s+Btx/00RefYCHmPbzv2sNN
make strides in caring for our patients with stroke.
Downloaded from http://journals.lww.com/continuum by KjfsNO4rm+70wsgqTPXGiE1ivOxovFfe/bXXYpJT6n4lQzg
USEFUL WEBSITE
NEUROCRITICAL CARE SOCIETY: EMERGENCY
NEUROLOGICAL LIFE SUPPORT
Refer to the Emergency Neurological Life Support
website to obtain further information on initial
management of neurologic emergencies.
neurocriticalcare.org/enls
REFERENCES
LisNIokjeaJDU on 03/08/2023
1 Mozaffarian D, Benjamin EJ, Go AS, et al. Heart 10 Lyden P. Using the National Institutes of Health
disease and stroke statistics–2015 update: a Stroke Scale: a cautionary tale. Stroke 2017;48(2):
report from the American Heart Association. 513–519. doi:10.1161/STROKEAHA.116.015434.
Circulation 2015;131(4):e29–e322. doi:10.1161/
11 National Institute of Neurological Disorders and
CIR.0000000000000152.
Stroke rt-PA Stroke Study Group. Tissue
2 Behavioral Risk Factor Surveillance System 2013 plasminogen activator for acute ischemic stroke.
survey data and documentation. Centers for N Engl J Med 1995;333(24):1581–1587. doi:10.1056/
Disease Control and Prevention. cdc.gov/brfss/ NEJM199512143332401.
annual_data/annual_2013.html. Updated June 23,
12 Hacke W, Kaste M, Bluhmki E, et al. Thrombolysis
2014. Accessed October 10, 2018.
with alteplase 3 to 4.5 hours after acute ischemic
3 Writing Group Members, Mozaffarian D, stroke. N Engl J Med 2008;359(13):1317–1329.
Benjamin EJ, et al. Heart Disease and Stroke doi:10.1056/NEJMoa0804656.
Statistics–2016 update: a report from the
13 IST-3 collaborative group, Sandercock P,
American Heart Association. Circulation 2016;133(4):
Wardlaw JM, et al. The benefits and harms of
e38–e360. doi:10.1161/CIR.0000000000000350.
intravenous thrombolysis with recombinant
4 Stroke Unit Trialists’ Collaboration. Organised tissue plasminogen activator within 6 h of acute
inpatient (stroke unit) care for stroke. Cochrane ischaemic stroke (the third international stroke
Database Syst Rev 2013(9):CD000197. trial [IST-3]): a randomised controlled trial.
doi:10.1002/14651858.CD000197.pub3. Lancet 2012;379(9834):2352–2363. doi:10.1016/
S0140-6736(12)60768-5.
5 Bershad EM, Feen ES, Hernandez OH, et al.
Impact of a specialized neurointensive care team 14 Thomalla G, Simonsen CZ, Boutitie F, et al. MRI-
on outcomes of critically ill acute ischemic stroke guided thrombolysis for stroke with unknown
patients. Neurocrit Care 2008;9(3):287–292. time of onset. N Engl J Med 2018;379(7):611–622.
doi:10.1007/s12028-008-9051-5. doi:10.1056/NEJMoa1804355.
6 Kramer AH, Zygun DA. Do neurocritical care units 15 Campbell BCV, Mitchell PJ, Churilov L, et al.
save lives? Measuring the impact of specialized Tenecteplase versus alteplase before
ICUs. Neurocrit Care 2011;14(3):329–333. thrombectomy for ischemic stroke. N Engl J Med
doi:10.1007/s12028-011-9530-y. 2018;378(17):1573–1582. doi:10.1056/NEJMoa1716405.
7 Goldstein LB. IV tPA for acute ischemic stroke: 16 Berkhemer OA, Fransen PS, Beumer D, et al. A
times are changing. Neurology 2016;87(21): randomized trial of intraarterial treatment for
2178–2179. doi:10.1212/WNL.0000000000003366. acute ischemic stroke. N Engl J Med 2015;372(1):
11–20. doi:10.1056/NEJMoa1411587.
8 Faigle R, Marsh EB, Llinas RH, et al. ICAT: a simple
score predicting critical care needs after 17 Goyal M, Demchuk AM, Menon BK, et al.
thrombolysis in stroke patients. Crit Care 2016; Randomized assessment of rapid endovascular
20:26. doi:10.1186/s13054-016-1195-7. treatment of ischemic stroke. N Engl J Med 2015;
372(11):1019–1030. doi:10.1056/NEJMoa1414905.
9 Papamichalis P, Karagiannis S, Dardiotis E, et al.
Predictors of need for critical care support, 18 Campbell BC, Mitchell PJ, Kleinig TJ, et al.
adverse events, and outcome after stroke Endovascular therapy for ischemic stroke with
thrombolysis. J Stroke Cerebrovasc Dis perfusion-imaging selection. N Engl J Med 2015;
2018;27(3):591–598. doi:10.1016/j. 372(11):1009–1018. doi:10.1056/NEJMoa1414792.
jstrokecerebrovasdis.2017.09.042.
1680 DECEMBER 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
19 Saver JL, Goyal M, Bonafe A, et al. Stent-retriever 32 Lansberg MG, Albers GW, Wijman CA.
thrombectomy after intravenous t-PA vs. t-PA Symptomatic intracerebral hemorrhage
alone in stroke. N Engl J Med 2015;372(24): following thrombolytic therapy for acute
2285–2295. doi:10.1056/NEJMoa1415061. ischemic stroke: a review of the risk factors.
Cerebrovasc Dis 2007;24(1):1–10. doi:10.
20 Jovin TG, Chamorro A, Cobo E, et al.
1159/000103110.
Thrombectomy within 8 hours after symptom
ogM/G3Lw98L4g53y0W25aSbX7CEFzDyuApk/85Hsqz5UhDeRfNPFhkYp95Mer+PxzV9+48F39Z4b5s+Btx/00RefYCHmPbzv2sNN
onset in ischemic stroke. N Engl J Med 2015; 33 Xu Y, Hackett ML, Chalmers J, et al. Frequency,
372(24):2296–2306. doi:10.1056/NEJMoa1503780. determinants, and effects of early seizures after
thrombolysis for acute ischemic stroke: the
Downloaded from http://journals.lww.com/continuum by KjfsNO4rm+70wsgqTPXGiE1ivOxovFfe/bXXYpJT6n4lQzg
21 Nogueira RG, Jadhav AP, Haussen DC, et al.
ENCHANTED trial. Neurol Clin Pract 2017;7(4):
Thrombectomy 6 to 24 hours after stroke
324–332. doi:10.1212/CPJ.0000000000000384.
with a mismatch between deficit and infarct.
N Engl J Med 2018;378(1):11–21. doi:10.1056/ 34 Prosser J, MacGregor L, Lees KR, et al. Predictors
NEJMoa1706442. of early cardiac morbidity and mortality after
ischemic stroke. Stroke 2007;38(8):2295–2302.
22 Albers GW, Mark MP, Kemp S, et al.
doi:10.1161/STROKEAHA.106.471813.
Thrombectomy for stroke at 6 to 16 hours with
selection by perfusion imaging. N Engl J Med 35 Wira CR 3rd, Rivers E, Martinez-Capolino C, et al.
2018;378(8):708–718. doi:10.1056/NEJMoa1713973. Cardiac complications in acute ischemic stroke.
West J Emerg Med 2011;12(4):414–420. doi:10.5811/
23 Wardlaw JM, Murray V, Berge E, del Zoppo GJ.
westjem.2011.2.1765.
Thrombolysis for acute ischaemic stroke.
Cochrane Database Syst Rev 2014(7):CD000213. 36 Hannawi Y, Hannawi B, Rao CP, et al. Stroke-
LisNIokjeaJDU on 03/08/2023
doi:10.1002/14651858.CD000213.pub3. associated pneumonia: major advances and
obstacles. Cerebrovasc Dis 2013;35(5):430–443.
24 Furlan A, Higashida R, Wechsler L, et al. Intra-arterial
doi:10.1159/000350199.
prourokinase for acute ischemic stroke. The
PROACT II study: a randomized controlled trial. 37 Reinhard M, Rutsch S, Lambeck J, et al. Dynamic
Prolyse in acute cerebral thromboembolism. cerebral autoregulation associates with infarct
JAMA 1999;282(21):2003–2011. doi:10.1001/ size and outcome after ischemic stroke. Acta
jama.282.21.2003. Neurol Scand 2012;125(3):156–162. doi:10.1111/
j.1600-0404.2011.01515.x.
25 Broderick JP, Palesch YY, Demchuk AM, et al.
Endovascular therapy after intravenous t-PA 38 Petersen NH, Ortega-Gutierrez S, Reccius A, et al.
versus t-PA alone for stroke. N Engl J Med 2013; Dynamic cerebral autoregulation is transiently
368(10):893–903. doi:10.1056/NEJMoa1214300. impaired for one week after large-vessel acute
ischemic stroke. Cerebrovasc Dis 2015;39(2):
26 Ciccone A, Valvassori L, Nichelatti M, et al.
144–150. doi:10.1159/000368595.
Endovascular treatment for acute ischemic
stroke. N Engl J Med 2013;368(10):904–913. 39 Panerai RB, Jara JL, Saeed NP, et al. Dynamic
doi:10.1056/NEJMoa1213701. cerebral autoregulation following acute
ischaemic stroke: comparison of transcranial
27 Kidwell CS, Jahan R, Gornbein J, et al. A trial of
Doppler and magnetic resonance imaging
imaging selection and endovascular treatment
techniques. J Cereb Blood Flow Metab 2016;
for ischemic stroke. N Engl J Med 2013;368(10):
36(12):2194–2202.
914–923. doi:10.1056/NEJMoa1212793.
40 Vemmos KN, Tsivgoulis G, Spengos K, et al.
28 Alberts MJ, Latchaw RE, Jagoda A, et al.
U-shaped relationship between mortality and
Revised and updated recommendations for the
admission blood pressure in patients with acute
establishment of primary stroke centers: a
stroke. J Intern Med 2004;255(2):257–265.
summary statement from the brain attack
doi:10.1046/j.1365-2796.2003.01291.x.
coalition. Stroke 2011;42(9):2651–2665. doi:10.1161/
STROKEAHA.111.615336. 41 Sandset EC, Bath PM, Boysen G, et al. The
angiotensin-receptor blocker candesartan
29 Jauch EC, Saver JL, Adams HP Jr, et al. Guidelines
for treatment of acute stroke (SCAST): a
for the early management of patients with acute
randomised, placebo-controlled, double-blind
ischemic stroke: a guideline for healthcare
trial. Lancet 2011;377(9767):741–750. doi:10.1016/
professionals from the American Heart Association/
S0140-6736(11)60104-9.
American Stroke Association. Stroke 2013;44(3):
870–947. doi:10.1161/STR.0b013e318284056a. 42 Robinson TG, Potter JF, Ford GA, et al. Effects
of antihypertensive treatment after acute
30 Fuhrer H, Reinhard M, Niesen WD. Paradigm
stroke in the Continue or Stop Post-Stroke
change? Cardiac output better associates with
Antihypertensives Collaborative Study
cerebral perfusion than blood pressure in
(COSSACS): a prospective, randomized, open,
ischemic stroke. Front Neurol 2017;8:706.
blinded-endpoint trial. Lancet Neurol 2010;9(8):
doi:10.3389/fneur.2017.00706.
767–775. doi:10.1016/S1474-4422(10)70163-0.
31 Battey TW, Karki M, Singhal AB, et al. Brain edema
43 He J, Zhang Y, Xu T, et al. Effects of immediate
predicts outcome after nonlacunar ischemic
blood pressure reduction on death and major
stroke. Stroke 2014;45(12):3643–3648. doi:10.1161/
disability in patients with acute ischemic stroke:
STROKEAHA.114.006884.
the CATIS randomized clinical trial. JAMA 2014;
311(5):479–489. doi:10.1001/jama.2013.282543.
CONTINUUMJOURNAL.COM 1681
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
MANAGEMENT OF STROKE IN THE NEUROCRITICAL CARE UNIT
44 ENOS Trial Investigators. Efficacy of nitric oxide, 55 Kim MJ, Park SK, Song J, et al. Preventive
with or without continuing antihypertensive suboccipital decompressive craniectomy for
treatment, for management of high blood cerebellar infarction: a retrospective-matched
pressure in acute stroke (ENOS): a partial- case-control study. Stroke 2016;47(10):
factorial randomised controlled trial. Lancet 2565–2573. doi:10.1161/STROKEAHA.116.014078.
2015;385(9968):617–628. doi:10.1016/S0140-
56 Burn J, Dennis M, Bamford J, et al. Epileptic
6736(14)61121-1.
ogM/G3Lw98L4g53y0W25aSbX7CEFzDyuApk/85Hsqz5UhDeRfNPFhkYp95Mer+PxzV9+48F39Z4b5s+Btx/00RefYCHmPbzv2sNN
seizures after a first stroke: the Oxfordshire
45 Galyfos G, Sianou A, Filis K. Cerebral Community Stroke Project. BMJ 1997;315(7122):
hyperperfusion syndrome and intracranial 1582–1587. doi:10.1136/bmj.315.7122.1582.
Downloaded from http://journals.lww.com/continuum by KjfsNO4rm+70wsgqTPXGiE1ivOxovFfe/bXXYpJT6n4lQzg
hemorrhage after carotid endarterectomy or
57 Claassen J, Goldstein JN. Emergency
carotid stenting: a meta-analysis. J Neurol Sci
neurological life support: status epilepticus.
2017;381:74–82. doi:10.1016/j.jns.2017.08.020.
Neurocrit Care 2017;27(suppl 1):152–158.
46 Yaghi S, Willey JZ, Cucchiara B, et al. Treatment doi:10.1007/s12028-017-0460-1.
and outcome of hemorrhagic transformation
58 Nelson SE, Varelas PN. Status epilepticus,
after intravenous alteplase in acute ischemic
refractory status epilepticus, and super-refractory
stroke: a scientific statement for healthcare
status epilepticus. Continuum (Minneap Minn)
professionals from the American Heart
2018;24(6 Neurocritical Care):1683–1707.
Association/American Stroke Association.
Stroke 2017;48(12):e343–e361. doi:10.1161/ 59 Skanes AC, Healey JS, Cairns JA, et al. Focused
STR.0000000000000152. 2012 update of the Canadian Cardiovascular
Society atrial fibrillation guidelines:
47 Gore JM, Sloan M, Price TR, et al. Intracerebral
LisNIokjeaJDU on 03/08/2023
recommendations for stroke prevention and
hemorrhage, cerebral infarction, and subdural
rate/rhythm control. Can J Cardiol 2012;28(2):
hematoma after acute myocardial infarction and
125–136. doi:10.1016/j.cjca.2012.01.021.
thrombolytic therapy in the Thrombolysis in
Myocardial Infarction Study. Thrombolysis in 60 Tsivgoulis G, Alexandrov AV, Katsanos AH,
Myocardial Infarction, phase II, pilot and clinical Barlinn K, Mikulik R, Lambadiari V, et al.
trial. Circulation 1991;83(2):448–459. Noninvasive ventilatory correction in patients
with acute ischemic stroke: a systematic review
48 Yaghi S, Boehme AK, Dibu J, et al. Treatment and
and meta-analysis. Stroke 2017;48(8):2285–2288.
outcome of thrombolysis-related hemorrhage:
doi:10.1161/STROKEAHA.117.017661.
a multicenter retrospective study. JAMA Neurol
2015;72(12):1451–1457. doi:10.1001/jamaneurol. 61 Berkhemer OA, van den Berg LA, Fransen PS,
2015.2371. et al. The effect of anesthetic management
during intra-arterial therapy for acute stroke in
49 Claude Hemphill J 3rd, Lam A. Emergency
MR CLEAN. Neurology 2016;87(7):656–664.
neurological life support: intracerebral
doi:10.1212/WNL.0000000000002976.
hemorrhage. Neurocrit Care 2017;27(suppl 1):
89–101. doi:10.1007/s12028-017-0453-0. 62 Schönenberger S, Uhlmann L, Hacke W, et al.
Effect of conscious sedation vs general
50 Hashimoto T, Matsumoto S, Ando M, et al.
anesthesia on early neurological improvement
Cerebral hyperperfusion syndrome after
among patients with ischemic stroke undergoing
endovascular reperfusion therapy in a
endovascular thrombectomy: a randomized
patient with acute internal carotid artery
clinical trial. JAMA 2016;316(19):1986–1996.
and middle cerebral artery occlusions.
doi:10.1001/jama.2016.16623.
World Neurosurg 2018;110:145–151.
doi:10.1016/j.wneu.2017.11.023. 63 Dziewas R, Ritter M, Schilling M, et al. Pneumonia
in acute stroke patients fed by nasogastric tube.
51 Siegal DM, Curnutte JT, Connolly SJ, et al.
J Neurol Neurosurg Psychiatry 2004;75(6):852–856.
Andexanet alfa for the reversal of factor Xa
inhibitor activity. N Engl J Med 2015;373(25): 64 Santoli F, De Jonghe B, Hayon J, et al. Mechanical
2413–2424. doi:10.1056/NEJMoa1510991. ventilation in patients with acute ischemic
stroke: survival and outcome at one year.
52 Vahedi K. Decompressive hemicraniectomy for
Intensive Care Med 2001;27(7):1141–1146.
malignant hemispheric infarction. Curr Treat
Options Neurol 2009;11(2):113–119. 65 Schönenberger S, Niesen WD, Fuhrer H, et al.
Early tracheostomy in ventilated stroke patients:
53 Jüttler E, Unterberg A, Woitzik J, et al.
study protocol of the international multicentre
Hemicraniectomy in older patients with
randomized trial SETPOINT2 (stroke-related early
extensive middle-cerebral-artery stroke.
tracheostomy vs. prolonged orotracheal
N Engl J Med 2014;370(12):1091–1100.
intubation in neurocritical care trial 2). Int J Stroke
doi:10.1056/NEJMoa1311367.
2016;11(3):368–379. doi:10.1177/1747493015616638.
54 Honeybul S, Ho KM, Blacker DW. ORACLE stroke
66 Coplin WM. Critical care management of acute
study: opinion regarding acceptable outcome
ischemic stroke. Continuum (Minneap Minn)
following decompressive hemicraniectomy for
2012;18(3, Critical Care Neurology):547–559.
ischemic stroke. Neurosurgery 2016;79(2):
doi:10.1212/01.CON.0000415427.53653.1b.
231–236. doi:10.1227/NEU.0000000000001115.
1682 DECEMBER 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5814)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- PS12Document3 pagesPS12Bryan ZhengNo ratings yet
- Chronux Tutorial Slides and MatlabDocument71 pagesChronux Tutorial Slides and MatlabBryan ZhengNo ratings yet
- A Tutorial Review of Functional Connectivity Analysis Methods and Their Interpretational PitfallsDocument23 pagesA Tutorial Review of Functional Connectivity Analysis Methods and Their Interpretational PitfallsBryan ZhengNo ratings yet
- Anne G. Osborn - Diagnostic Cerebral Angiography (1998, LWW)Document445 pagesAnne G. Osborn - Diagnostic Cerebral Angiography (1998, LWW)Bryan ZhengNo ratings yet
- Chronux Tutorial Slides and MatlabDocument71 pagesChronux Tutorial Slides and MatlabBryan ZhengNo ratings yet
- 11 Objectives 16 - SilvaDocument1 page11 Objectives 16 - SilvaBryan ZhengNo ratings yet
- Assignment 9, Phys 2218, Fall 2016Document1 pageAssignment 9, Phys 2218, Fall 2016Bryan ZhengNo ratings yet
- SOC 3750 - 17 FallDocument7 pagesSOC 3750 - 17 FallBryan ZhengNo ratings yet
- Bio G 1440 Sample Questions For Exam 1Document2 pagesBio G 1440 Sample Questions For Exam 1Bryan ZhengNo ratings yet
- Tess EssayDocument4 pagesTess EssayBryan ZhengNo ratings yet
- AEP Syllabus F 2016Document3 pagesAEP Syllabus F 2016Bryan ZhengNo ratings yet
- 2013-2014 PMP SheetDocument1 page2013-2014 PMP SheetBryan ZhengNo ratings yet
- Experiment 4Document3 pagesExperiment 4Bryan ZhengNo ratings yet
- Bryan ZhengDocument1 pageBryan ZhengBryan ZhengNo ratings yet
- Conflict in HamletDocument5 pagesConflict in HamletBryan Zheng100% (2)
- Chapter 1 The Study of ChangeDocument1 pageChapter 1 The Study of ChangeBryan ZhengNo ratings yet