Professional Documents
Culture Documents
1 s2.0 S246812532300208X Main
Uploaded by
Piyush malikOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
1 s2.0 S246812532300208X Main
Uploaded by
Piyush malikCopyright:
Available Formats
Articles
Efficacy and safety of upadacitinib maintenance therapy
for moderately to severely active ulcerative colitis in
patients responding to 8 week induction therapy
(U-ACHIEVE Maintenance): overall results from the
randomised, placebo-controlled, double-blind, phase 3
maintenance study
Séverine Vermeire, Silvio Danese, Wen Zhou, Dapo Ilo, Justin Klaff, Gweneth Levy, Xuan Yao, Su Chen, Yuri Sanchez Gonzalez, Xavier Hébuterne,
James O Lindsay, Peter D R Higgins, Qian Cao, Hiroshi Nakase, Jean-Frédéric Colombel, Edward V Loftus Jr, Remo Panaccione
Summary
Lancet Gastroenterol Hepatol Background Upadacitinib is an oral, selective, and reversible JAK inhibitor with demonstrated efficacy in patients with
2023; 8: 976–89 moderately to severely active ulcerative colitis in a phase 2b induction trial, two phase 3 induction trials (U-ACHIEVE
Published Online Induction and U-ACCOMPLISH), and a primary analysis of the first 451 patients entering a subsequent maintenance
September 5, 2023
trial (U-ACHIEVE Maintenance). Here, we present overall results from the entire U-ACHIEVE Maintenance
https://doi.org/10.1016/
S2468-1253(23)00208-X population.
This online publication has
been corrected. The corrected Methods In this randomised, placebo-controlled, double-blind, phase 3 maintenance study done across Europe,
version first appeared at North and South America, Australasia, Africa, and the Asia-Pacific region at 251 clinical centres in 44 countries,
thelancet.com/gastrohep on
patients aged 16–75 years with moderately to severely active ulcerative colitis (adapted Mayo score 5–9, centrally
October 1 1, 2023
assessed endoscopic subscore of 2 or 3) for 90 days or more were randomly assigned (2:1) to double-blind
See Comment page 956
upadacitinib 45 mg once daily or placebo induction therapy in the phase 2b induction trial or two phase 3 induction
Department of
Gastroenterology &
trials. Patients with a clinical response per adapted Mayo score after 8 weeks were randomly reassigned (1:1:1)
Hepatology, University using web-based interactive response technology to 52 week double-blind maintenance therapy with placebo,
Hospital Leuven, Leuven, upadacitinib 15 mg, or upadacitinib 30 mg once daily. Efficacy was analysed at week 52 in the intention-to-treat
Belgium (Prof S Vermeire MD); population, which included all patients randomly reassigned who received at least one dose of study drug. The
Gastroenterology and
Endoscopy, IRCCS Ospedale
primary endpoint was clinical remission per adapted Mayo score. Safety through week 52 was assessed with
San Raffaele and University exposure-adjusted event rates (EAERs; events per 100 patient-years) in upadacitinib 45 mg once daily 8-week
Vita-Salute San Raffaele, Milan, induction responders who were enrolled per protocol for 44-week or 52-week maintenance therapy (ie, the
Italy (Prof S Danese MD); intention-to-treat population plus patients who received up to 44 weeks’ maintenance therapy under earlier protocol
AbbVie, North Chicago, IL, USA
(W Zhou MD, D Ilo MBBS,
amendments) and received at least one dose of study drug. The study is registered with ClinicalTrials.gov,
J Klaff MD, G Levy MD, X Yao PhD, NCT02819635 and is complete.
S Chen PhD,
Y Sanchez Gonzalez PhD); Findings Between Sept 3, 2016, and Jan 14, 2021 987 patients received the upadacitinib 45 mg once daily induction
Department of
Gastroenterology and Clinical
therapy in the phase 2b trial, U-ACHIEVE Induction, or U-ACCOMPLISH. 681 patients with a clinical response to
Nutrition, CHU de Nice, the induction therapy (319 from U-ACHIEVE Induction, 341 from U-ACCOMPLISH, and 21 from the phase 2b
Université Côte d’Azur, Nice, induction trial) received placebo (n=223), upadacitinib 15 mg once daily (n=225), or upadacitinib 30 mg once daily
France (Prof X Hébuterne MD);
(n=233) in U-ACHIEVE Maintenance and were included in this analysis. A greater proportion of patients achieved
Department of
Gastroenterology, The Royal the primary endpoint with upadacitinib 15 mg (40·4%) and 30 mg once daily (53·6%) versus placebo (10·8%;
London Hospital, Barts Health both p<0·0001 vs placebo). For safety, 746 patients were analysed, representing 552·9 patient-years of exposure; the
NHS Trust, London, UK most common grade 3–4 treatment-emergent adverse events were worsening of ulcerative colitis in nine (4%) patients
(Prof J O Lindsay FRCP);
with placebo, and COVID-19 pneumonia and cryptococcal pneumonia in two (1%) patients each with upadacitinib
Department of Internal
Medicine, Division of 30 mg once daily. Higher EAERs of the following treatment-emergent events of special interest were observed with
Gastroenterology, University upadacitinib versus placebo: herpes zoster (6·0 events per 100 patient-years with upadacitinib 15 mg once daily and
of Michigan, Ann Arbor, MI, 7·3 events per 100 patient-years with upadacitinib 30 mg once daily vs none per 100 patient-years with placebo
USA (Prof P D R Higgins MD);
[12 and 16 vs no events, respectively), hepatic disorders (17·0 and 9·2 vs 5·9 events per 100 patient-years
Department of
Gastroenterology, [34 and 20 vs eight events, respectively), creatine phosphokinase elevation (8·0 and 10·1 vs 3·7 events per 100 patient-
Sir Run Shaw Hospital, years [16 and 22 vs five events], respectively), and neutropenia (5·5 and 8·7 vs 5·2 events per 100 patient-years
Zhejiang University School of [11 and 19 vs seven events], respectively). One (<1% of patients) adjudicated major adverse cardiovascular event
Medicine, Hangzhou, China
occurred with placebo and one (<1% of patients) with upadacitinib 30 mg once daily (EAERs 0·7 and 0·5 events per
(Prof Q Cao MD); Department
of Gastroenterology and 100 patient-years, respectively). Two (1% of patients) venous thromboembolic events occurred with upadacitinib
Hepatology, Sapporo Medical 15 mg once daily and two (1% of patients) with upadacitinib 30 mg once daily (EAERs 1·0 and 0·9 events per
976 www.thelancet.com/gastrohep Vol 8 November 2023
Articles
100 patient-years, respectively). All adjudicated major adverse cardiovascular events and venous thromboembolic University School of Medicine,
events with upadacitinib occurred in patients with relevant known risk factors. Sapporo, Japan
(Prof H Nakase MD); Icahn
School of Medicine at
Interpretation Consistent with the primary analysis done among a smaller population, both maintenance doses of Mount Sinai, New York, NY,
upadacitinib showed a positive benefit–risk profile in patients with moderately to severely active ulcerative colitis. USA (Prof J-F Colombel MD);
Upadacitinib represents an effective treatment option for this population, for whom a large unmet need persists. Division of Gastroenterology
and Hepatology, Mayo Clinic
College of Medicine and
Funding AbbVie. Science, Rochester, Minnesota,
USA (Prof E V Loftus Jr MD);
Copyright © 2023 Elsevier Ltd. All rights reserved. Division of Gastroenterology
and Hepatology, University of
Calgary, Calgary, Alberta,
Introduction and was well tolerated.4 Patients in U-ACHIEVE Canada (Prof R Panaccione MD)
Ulcerative colitis is a chronic, idiopathic, relapsing, and Induction, U-ACCOMPLISH, or a phase 2b dose-ranging Correspondence to:
remitting inflammatory bowel disease that results in induction trial (NCT02819635),5 with a clinical response Prof Séverine Vermeire,
mucosal inflammation, which typically extends from the (per adapted Mayo score) after 8 weeks of upadacitinib Department of Gastroenterology
& Hepatology, University
rectum to the proximal colon.1 The estimated incidence 45 mg once daily induction therapy were eligible to be Hospital Leuven, Leuven,
of ulcerative colitis is 1·9–17·2 per 100 000 person-years reassigned randomly to receive 52 weeks of upadacitinib Belgium
in western Europe and 8·8–23·1 per 100 000 person- 15 mg once daily, upadacitinib 30 mg once daily, or severine.vermeire@uzleuven.be
years in North America.2 Hallmark symptoms of placebo maintenance therapy in the U-ACHIEVE
ulcerative colitis include bloody diarrhoea, faecal urgency, Maintenance study (NTC02819635). A prespecified
and abdominal discomfort, which have a substantial primary analysis of the first 8-week induction responders
effect on patients’ quality of life.1 (n=451) who subsequently entered the U-ACHIEVE
Upadacitinib is an oral, selective, and reversible JAK Maintenance study found that upadacitinib 15 mg and
inhibitor.3 In two identical, double-blind, randomised upadacitinib 30 mg once daily showed greater efficacy
clinical trials (U-ACHIEVE Induction [NCT02819635] versus placebo after 52 weeks’ maintenance therapy
and U-ACCOMPLISH [NCT03653026]) of patients with across clinical, endoscopic, histological, and quality of
moderately to severely active ulcerative colitis and an life endpoints, and was well tolerated.4 On the basis of
inadequate response, loss of response, or intolerance to the results of these trials, upadacitinib has been approved
conventional or biological therapy, 8 weeks’ double- for the treatment of adults with moderately to severely
blind induction therapy with upadacitinib 45 mg once active ulcerative colitis in numerous countries.3,6
daily led to a significantly greater proportion of patients Here, we present an updated and final analysis of
achieving clinical remission at week 8 versus placebo, efficacy and safety data from the U-ACHIEVE Maintenance
Research in context
Evidence before this study patients receiving upadacitinib 15 mg once daily or upadacitinib
Upadacitinib is a JAK inhibitor approved for the treatment of 30 mg once daily achieved clinical remission at week 52 versus
moderately to severely active ulcerative colitis. Approval was placebo; both doses were also significantly more efficacious
based on two induction trials and a prespecified analysis of the versus placebo across all secondary clinical, endoscopic, and
first 8-week induction responders (n=451) who entered the histological endpoints. Upadacitinib was well tolerated, and
subsequent maintenance trial. In the induction trials, 8 weeks’ there were no new safety risks identified with upadacitinib
double-blind therapy with upadacitinib 45 mg once daily led to compared with the previous analysis, or other indications for
a significantly greater proportion of patients achieving the which upadacitinib is approved.
primary endpoint of clinical remission per adapted Mayo score
Implications of all the available evidence
at week 8 versus placebo. In the primary analysis of the
The overall results from the entire population enrolled in this
maintenance trial, upadacitinib 15 mg once daily and
phase 3 maintenance study show the favourable benefit–risk
upadacitinib 30 mg once daily showed greater efficacy versus
profile of upadacitinib in patients with moderately to severely
placebo after 52 weeks’ maintenance therapy for the primary
active ulcerative colitis. These results are consistent with
endpoint of clinical remission per adapted Mayo score, as well
those seen in the primary analysis and support the use of
as all assessed secondary clinical, endoscopic, and histological
upadacitinib as a therapeutic option in patients with
endpoints. Upadacitinib was well tolerated in both induction
moderately to severely active ulcerative colitis, for whom a
studies and the primary analysis of the maintenance study.
large unmet need persists.
Added value of this study
In this analysis of a larger population (n=681) than has been
previously analysed, a significantly greater proportion of
www.thelancet.com/gastrohep Vol 8 November 2023 977
Articles
Induction
8-week responders* 8-week responders* 8-week responders*
319 from U-ACHIEVE induction† 341 from U-ACCOMPLISH† 21 from phase 2b induction study
Maintenance
681 patients randomly assigned (1:1:1) in U-ACHIEVE
Maintenance intention-to-treat population‡
223 assigned to placebo 225 assigned to upadacitinib 233 assigned to upadacitinib
15 mg once daily 30 mg once daily
148 discontinued treatment 70 discontinued treatment 49 discontinued treatment
17 adverse events 5 adverse events 14 adverse events
3 withdrew consent 1 withdrew consent 4 withdrew consent
109 lack of efficacy 51 lack of efficacy 18 lack of efficacy
1 lost to follow-up 13 other reasons 1 lost to follow-up
18 other reasons 1 COVID-19 infection
1 COVID-19 logistical
restriction
10 other reasons
75 completed treatment 155 completed treatment 184 completed treatment
Figure 1: Patient disposition in U-ACHIEVE Maintenance
Patient numbers are given for the U-ACHIEVE Maintenance trial intention-to-treat population, defined as upadacitinib 45 mg once daily 8-week induction
responders who were enrolled per protocol for the 52-week maintenance period, and received ≥1 dose of study drug (placebo, upadacitinib 15 mg once daily, and
upadacitinib 30 mg once daily). Bio-IR=inadequate response, loss of response, or intolerance to ≥1 biologic. RBS=rectal bleeding subscore. RR=re-randomised.
*Clinical response was defined as a decrease from baseline in the adapted Mayo score ≥2 points and ≥30% from baseline, plus a decrease in RBS ≥1 or an absolute
RBS ≤1. †Includes patients who were initially randomly assigned to placebo for 8 weeks but did not achieve a clinical response at week 8 and were subsequently
treated with, and had a clinical response to, 8 weeks’ upadacitinib 45 mg once daily. ‡Re-randomisation was stratified by previous bio-IR status (bio-IR or non-bio-IR),
clinical remission status at week 0 of the maintenance trial (yes or no), and corticosteroid use at week 0 of the maintenance trial (yes or no).
study comprising all patients who had a clinical response aged 16–75 years with a confirmed diagnosis of ulcerative
after 8 weeks of induction therapy with upadacitinib colitis for at least 90 days before study entry, active
45 mg once daily and were reassigned randomly to receive disease (defined as an adapted Mayo score of 5–9 and a
maintenance therapy with upadacitinib 15 mg once daily, centrally assessed Mayo endoscopic subscore of 2 or 3),
upadacitinib 30 mg once daily, or placebo for up to and had inadequate response or were intolerant to at
52 weeks in the maintenance phase. This represents a least one oral aminosalicylate, corticosteroid, immuno
larger population (n=681) than has been analysed suppressant, or biological therapy. Key exclusion criteria
previously (n=451),4 and addresses whether the efficacy of included a diagnosis of Crohn’s disease or indeterminate
upadacitinib in the entire trial population is consistent colitis, fulminant colitis, toxic megacolon, disease limited
with that observed in the registrational analysis, as well as to the rectum, active infection, or previous exposure to
whether there are any new safety signals with additional JAK inhibitors. The study protocol, informed consent
upadacitinib exposure. forms, and recruitment materials were approved by the
relevant ethics committees or institutional review boards
Methods of each country before enrolment. The studies were done
Study design and participants in accordance with the International Conference for
Details of the study designs and methodology for the Harmonisation guidelines, Declaration of Helsinki,
phase 2b induction trial,5 the double-blind, randomised, Good Clinical Practice guidelines, and all applicable
placebo-controlled, induction trials (U-ACHIEVE regulations. All patients provided written informed
Induction and U-ACCOMPLISH) and the maintenance consent before screening.
trial (U-ACHIEVE Maintenance) have been previously
published.4 This was a randomised, placebo-controlled, Randomisation and masking
double-blind, phase 3 maintenance study done across In part 1 of the phase 2b induction trial, patients were
Europe, North and South America, Australasia, Africa, randomly assigned 1:1:1:1:1 to receive oral placebo or
and the Asia-Pacific region at 1251 clinical centres in upadacitinib 7·5 mg, 15 mg, 30 mg, or 45 mg once
44 countries. Briefly, patients eligible for induction were daily induction therapy for 8 weeks. In part 2,
978 www.thelancet.com/gastrohep Vol 8 November 2023
Articles
additional patients were randomly assigned 1:1 to oral received double-blind oral upadacitinib 15 mg once daily,
upadacitinib 15 mg once daily or 45 mg once daily. upadacitinib 30 mg once daily, or placebo for an additional
Randomisation was stratified by previous biological 52 weeks in the maintenance trial (44 weeks under earlier
status (patients without inadequate response, loss of protocol amendments assessed for safety only). Patients
response, or intolerance to a biologic [non-bio-IR] or initially randomly assigned to placebo who did not
patients with inadequate response, loss of response, or achieve a clinical response at week 8 were treated with
intolerance to at least one biologic [bio-IR], baseline open-label upadacitinib 45 mg once daily for 8 weeks;
corticosteroid use (yes or no), and baseline adapted responders after 8 weeks’ open-label upadacitinib
Mayo score (≤7 and >7). Study investigators, study site induction therapy were also randomly reassigned into the
personnel, and patients were masked to treatment maintenance trial and analysed in the same population.
allocation throughout the study.5 Only patients with Non-responders after 8 weeks’ upadacitinib 45 mg once
a response to 8 weeks’ upadacitinib 45 mg once daily daily therapy could receive an additional 8 weeks’ open-
are analysed here, to align with the populations label upadacitinib 45 mg once daily therapy (extended
included from the other induction studies. induction) and enter the maintenance trial; these patients
In the phase 3 induction trials, patients were randomly were not analysed as part of the population reported here.
assigned 2:1 to 8-week double-blind induction therapy During induction therapy, doses of concomitant
with oral upadacitinib 45 mg once daily or placebo. ulcerative colitis-related medications including cortico
Randomisation was stratified by previous biological steroids remained stable, but concomitant use of biologics
status (non-bio-IR or bio-IR), baseline corticosteroid use and immunosuppressants (except metho trexate) was
(yes or no), and baseline adapted Mayo score (≤7 or >7). prohibited. From week 0 of the maintenance trial,
Baseline was defined as the last non-missing value corticosteroid use was tapered according to the protocol-
collected on or before the first induction dose. specified schedule (which could be initiated or increased
Patients who achieved a clinical response (defined as at the discretion of the investigator if a patient had new or
a decrease in the adapted Mayo score of at least 2 points worsening symptoms of ulcerative colitis). Rescue
and at least 30% from baseline plus a decrease in rectal therapy could be provided during maintenance to treat
bleeding subscore [RBS] ≥1 or an absolute RBS ≤1) to new or worsening symptoms of ulcerative colitis at
upadacitinib 45 mg once daily at week 8 in the phase 2b the investigator’s discretion. Protocol-permitted rescue
induction study,5 or the phase 3 induction studies,4 were therapies were initiating or increased dosage of cortico
randomly reassigned (1:1:1) to receive double-blind oral steroids, aminosalicylates, methotrexate, or ulcerative
upadacitinib 15 mg once daily, upadacitinib 30 mg once colitis-related antibiotics. However, patients were
daily, or placebo for an additional 52 weeks in the phase 3 considered as non-responders for efficacy assessments
maintenance trial (figure 1). Patients who were initially on or after dose escalation of ulcerative colitis-related
randomised to placebo but did not achieve a clinical medication or initiation of rescue therapy.
response at week 8 were treated with open-label The primary protocol-defined reasons for study drug
upadacitinib 45 mg once daily for 8 weeks; responders after discontinuation included clinically significant abnormal
8 weeks’ open-label upadacitinib induction therapy were laboratory results or adverse events; introduction of
also randomly reassigned into the maintenance trial as prohibited medications or dosages, or non-compliance
described above and analysed in the same population. with study procedures that could have placed the
Random reassignment was stratified by previous bio-IR patient at risk; patient non-compliance with tuberculosis
status (bio-IR or non-bio-IR), clinical remission status at prophylaxis (if applicable) or development of active
week 0 of the maintenance trial (yes or no), and cortico tuberculosis during the study; or serious infections
steroid use at week 0 of the maintenance trial (yes or no). which could not be adequately controlled by anti-infective
All patients were randomly assigned with web-based treatment, malignancy (except for localised non-
interactive response technology using block random melanoma skin cancer or carcinoma in-situ of the cervix),
isation methods. Block randomisation schedules (block gastrointestinal perforation (except for appendicitis or
size of 3) were generated by randomisation specialists mechanical injury), or confirmed diagnosis of deep vein
employed by the sponsor and distributed to the inter thrombosis. Study drug could be interrupted for toxicity
active response technology vendor for patient random management (eg, because of a treatment-emergent
assignment. As previously described, study investigators, adverse event including serious infections, herpes zoster,
study site personnel, and patients were masked to gastrointestinal perforations, cardiovascular events,
treatment allocation throughout the studies.4 The malig nancy and gastrointestinal dysplasia, thrombosis
upadacitinib and placebo tablets were identical in events, electrocardiogram abnormality, or management
appearance to maintain masking. of select laboratory abnormalities). If a patient had signs
or symptoms of and suspicion of COVID-19 infection, or
Procedures a confirmed diagnosis, study drug was interrupted until
Patients who achieved a clinical response to upadacitinib resolution (with no time limit for interruption, providing
45 mg once daily at week 8 in the induction studies4 no permanent discontinuation criteria were met).
www.thelancet.com/gastrohep Vol 8 November 2023 979
Articles
Adapted Mayo score (full Mayo score excluding without friability and Geboes score ≤3·1); mucosal
Physician’s Global Assessment) was assessed at healing (also known as histological–endoscopic mucosal
maintenance baseline and week 52. Endoscopic subscore remission; endoscopic subscore=0 and Geboes score <2);
was calculated on the basis of a centrally reviewed no abdominal pain (mean score of 0 across 3 days); no
endoscopy, with a primary central reader masked to the bowel urgency (mean score of 0 across 3 days); change
site’s endoscopy assessment, and the patient’s clinical from baseline in FACIT-F score; and change from
data and therapy. Stool frequency subscore, RBS, baseline in IBDQ score. Efficacy outcomes were also
abdominal pain, and bowel urgency, assessed at baseline analysed by previous bio-IR status (bio-IR and non-bio-IR)
and week 52, were calculated using mean values reported and reported for patients with inadequate response to
by patients in e-diaries from the most recent 3-day anti-TNF (TNF-IR, defined as inadequate response, loss
consecutive period in the last 10 days; if data were not of response, or intolerance to ≥1 anti-TNF agent).
available for consecutive days, the three most recent A subgroup analysis was done for efficacy endpoints by
non-consecutive days were used. IBD Questionnaire baseline demographics and clinical characteristics (sex
(IBDQ) and Functional Assessment of Chronic Illness [self-reported], age, weight, race [self-reported along with
Therapy—Fatigue (FACIT–F) score were assessed at ethnicity and collected as a standard clinical trial
baseline and week 52. Full details of assessments and demographic], region, disease duration, adapted Mayo
See Online for appendix timings are listed in the appendix (pp 1–2). score, full Mayo score, presence of pancolitis, high-
At the time of the protocol-defined primary analysis, sensitivity C-reactive protein, albumin concentrations,
enrolment of 8-week upadacitinib 45 mg once daily corticosteroid use, aminosalicylate use, bio-IR status,
induction responders into the maintenance trial was previous exposure to anti-TNF agents in non-bio-IR
complete, and 451 patients had either completed the patients, and previous exposure to biologics in non-bio-
study or prematurely ended study participation. Safety IR patients). Point estimates and 95% CIs for treatment
and efficacy data at week 8 of induction therapy, and differences between each upadacitinib dose and placebo
maintenance data at week 52 from these 451 patients are presented.
have been reported previously.4 Additional patients Safety outcomes included treatment-emergent adverse
ongoing in the maintenance at the time of the primary events, defined as any adverse events that began or
analysis are included in this updated and final analysis of worsened in severity on or after the first dose of study
efficacy (post hoc; n=681) and safety (prespecified; n=746) drug in the maintenance trial and within 30 days after
in the maintenance trial, comprising all 8 week induction the last dose for patients who did not participate in the
responders in U-ACHIEVE Maintenance. ongoing long-term extension study, or until first dose of
study drug in the long-term extension study. Adverse
Outcomes events of special interest (AESIs) were prespecified
In the maintenance trial, the primary endpoint was and based on previous studies in patients receiving
clinical remission per adapted Mayo score (SFS ≤1 and upadacitinib for other indications or other JAK
not greater than baseline, RBS=0, and endoscopic inhibitors,5,7,8 and included serious infections, herpes
subscore ≤1 without friability) at week 52 of maintenance. zoster, malignancy excluding non-melanoma skin cancer,
Key secondary endpoints at week 52 were maintenance non-melanoma skin cancer, adjudicated major adverse
of clinical response per adapted Mayo score (decrease ≥2 cardiovascular events (MACEs, defined as cardiovascular
and ≥30% from baseline, plus a decrease in RBS ≥1 or death, nonfatal myocardial infarction, and non-fatal
an absolute RBS ≤1 at week 52, among patients who stroke), and adjudicated venous thromboembolic events
achieved clinical response per adapted Mayo score at the (VTEs, defined as deep vein thrombosis [DVT] and
end of the induction period); maintenance of clinical pulmonary embolism [ fatal and non-fatal]). Safety
remission per adapted Mayo score (clinical remission at outcomes were also analysed by previous bio-IR status
week 52 among patients who achieved clinical remission and reported for anti-TNF-IR patients.
per adapted Mayo score at the end of the induction In November, 2022, the European Medicines
period); corticosteroid-free clinical remission per adapted Agency (EMA) issued recommendations to minimise
Mayo score (clinical remission and corticosteroid-free for the risk of serious side-effects with JAK inhibitors.9,10
≥90 days immediately before week 52 among patients Given the focus of these recommendations on patients
who achieved clinical remission per adapted Mayo with increased risk of MACE, VTE, and malignancy,
score at the end of the induction period); endoscopic we reviewed baseline data, including previous
improvement (endoscopic subscore ≤1 without friability); cardiovascular events (all events in which the Medical
maintenance of endoscopic improvement (endoscopic History Body System or Organ Class [MHBODSYS] was
subscore ≤1 without friability at week 52 among patients cardiac disorders) from the safety population for
who had achieved endoscopic subscore ≤1 without relevant known risk factors for events of these types. In
friability at the end of the induction period); endoscopic addition, full details on all events of MACE, VTE, and
remission (endoscopic subscore =0); histological–endo malignancies (excluding non-melanoma skin cancer)
scopic mucosal improvement (endoscopic subscore ≤1 are provided.
980 www.thelancet.com/gastrohep Vol 8 November 2023
Articles
To characterise further the risk of herpes zoster in this imputation; for this, patients were considered responders
population, herpes zoster rates were analysed by or non-responders at that timepoint on the basis of
geographical region, previous herpes zoster, and previous multiple imputation values.
herpes zoster vaccination. Data collected at or after ulcerative colitis-related
rescue medication were not used for efficacy analysis.
Statistical analysis For binary endpoints, patients who had these events
The protocol-defined sample size calculation for the were considered as not achieving them. For continuous
primary analysis of the first 451 8-week upadacitinib 45 mg endpoints, data were analysed by means of multiple
once daily induction responders has been described imputation incorporating return-to-baseline to handle
previously,4 depicting the pivotal portion of the efficacy visits on, or after, ulcerative colitis-related rescue
evaluation. Additional patients who had not completed the medication use.
study at the time of the primary database lock were Post-hoc analyses of the number needed to treat (NNT)
prespecified for safety analyses only, according to the were done for binary efficacy outcomes in the intention-
protocol. The efficacy analyses comprising all 8-week to-treat population at week 52. NNT was calculated as the
induction responders presented in this paper were inverse of the difference in proportions achieving each
performed post hoc, and results are nominal in nature. outcome with each maintenance dose of upadacitinib
Efficacy analyses were done in the intention-to-treat versus placebo.
population, defined as upadacitinib 45 mg once daily All efficacy analyses on the overall population were
8-week induction responders who were enrolled per adjusted for stratification factors. Subgroup analyses were
protocol for the 52-week maintenance treatment period not adjusted for stratification factors to avoid small sizes
and received at least one dose of study drug (placebo, of stratum within each subgroup–treatment combination.
upadacitinib 15 mg once daily, or upadacitinib For safety, exposure-adjusted event rates (EAERs,
30 mg once daily). The safety analysis population was defined as events per 100 patient-years) and 95% CIs
defined as the upadacitinib 45 mg once daily 8-week were calculated. The 95% CIs were calculated by normal
induction responders who were enrolled per protocol for approximation to the Poisson distribution.
44-week or 52-week maintenance therapy (ie, the intention- Post-hoc analyses of the number needed to harm
to-treat population plus patients who received up to (NNH) were done in the safety population at week 52.
44 weeks’ maintenance therapy under earlier protocol NNH was calculated as the inverse of the difference in
amendments) and received at least one dose of study drug proportions of patients having a treatment-emergent
(placebo, upadacitinib 15 mg once daily, or upadacitinib adverse event with each dose of upadacitinib versus
30 mg once daily). placebo (ie, not exposure adjusted). Negative or positive
Efficacy comparisons between upadacitinib 15 mg once NNH values indicate a lower or higher risk, respectively,
daily versus placebo, and upadacitinib 30 mg once of treatment-emergent adverse events for upadacitinib
daily versus placebo were made by means of the versus placebo; values closest to 1 indicate that the safety
Cochran–Mantel–Haenszel test adjusted by previous risk difference between upadacitinib and placebo is
bio-IR status (bio-IR or non-bio-IR), corticosteroid use at largest (ie, closer to 100%).
week 0 of the maintenance trial (yes or no), and clinical All statistical analyses were done with SAS (version 9.4).
remission status at week 0 of the maintenance trial (yes These studies are registered with ClinicalTrials.gov
or no). Continuous endpoints collected at only one post- (U-ACHIEVE [Induction and Maintenance] NCT02819635;
baseline visit were analysed by means of an analysis of U-ACCOMPLISH NCT03653026).
covariance model. The study was not designed for
statistical comparisons between upadacitinib 15 mg once Role of the funding source
daily and upadacitinib 30 mg once daily, meaning that The funder of the study was involved in the study
any comparisons are descriptive only. design, data collection, data analysis, data interpretation,
The primary approach for handling missing data was writing of the report, and the decision to submit for
non-responder imputation, while incorporating multiple publication.
imputation to handle missing data owing to COVID-19.
This approach categorised any patient who did not have Results
an evaluation during a prespecified visit for any reason Between Sept 3, 2016, and June 14, 2018 (phase 2b
(including initiation of ulcerative colitis-related rescue induction study), Oct 23, 2018, and Sept 7, 2020
medications, lack of efficacy, study drug intolerance, or (U-ACHIEVE Induction), and Dec 6, 2018, and
early discontinuation from the maintenance study to the Jan 14, 2021 (U-ACCOMPLISH), 987 patients received
long-term extension study) as a non-responder for 8-week upadacitinib 45 mg once daily induction therapy.
efficacy assessments at that timepoint. For missing data Of these, 681 (69%) patients achieved a clinical response
owing to COVID-19 infection or logistical restrictions after 8 weeks and were randomly reassigned to
related to the COVID-19 pandemic, under missing at upadacitinib 15 mg once daily (n=225), upadacitinib
random assumptions, data were handled by multiple 30 mg once daily (n=233), or placebo (n=223) for
www.thelancet.com/gastrohep Vol 8 November 2023 981
Articles
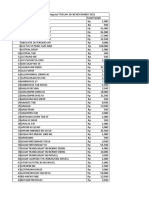
Placebo (n=223) Upadacitinib 15 mg once daily Upadacitinib 30 mg once daily
(n=225) (n=233)
Sex*
Male 123 (55%) 146 (65%) 141 (61%)
Female 100 (45%) 79 (35%) 92 (39%)
Age, years 40·0 (32·0–54·0) 39·0 (30·0–53·0) 42·0 (31·0–55·0)
Age
<18 years 4 (2%) 0 2 (1%)
≥18 – <40 years 103 (46%) 113 (50%) 100 (43%)
≥40 – <65 years 97 (43%) 92 (41%) 110 (47%)
≥65 years 19 (9%) 20 (9%) 21 (9%)
Race†
American Indian or Alaskan Native 1 (<1%) 0 0
Asian 65 (29%) 70 (31%) 74 (32%)
Black or African American 7 (3%) 9 (4%) 6 (3%)
Native Hawaiian or Other Pacific Islander 1 (<1%) 0 1 (<1%)
Multiple 8 (4%) 0 1 (<1%)
White 141 (63%) 146 (65%) 151 (65%)
Ethnicity†
Hispanic or Latinx 15 (7%) 19 (8%) 16 (7%)
Not Hispanic or Latinx 208 (93%) 206 (92%) 217 (93%)
BMI, kg/m² 23·9 (21·2–27·8) 23.8 (21·0–27·6) 24·5 (20·9–28·1)
Disease duration, years 5·9 (2·8–11·3) 6·3 (2·8–12·1) 5·9 (2·7–11·0)
Faecal calprotectin, mg/kg n=195; 1679·0 (658·0–3338·0) n=197; 1707·0 (724·0–3067·0) n=193; 1580·0 (809·0–2913·0)
High-sensitivity C-reactive protein, mg/L 3·9 (1·4–9·2) 3·6 (1·2–9·3) 4·1 (1·2–8·6)
Aminosalicylate use 146 (65%) 160 (71%) 168 (72%)
Methotrexate use 0 2 (1%) 1 (<1%)
Corticosteroid use‡ 84 (38%) 84 (37%) 84 (36%)
Corticosteroid dose, mg/day prednisone equivalent§ n=83; 20·0 (10·0–25·0) n=81; 15·0 (10·0–30·0) n=81; 20·0 (10·0–20·0)
Bio-IR 116 (52%) 109 (48%) 111 (48%)
Number of previous biologics in bio-IR patients
1 45 (39%) 43 (39%) 40 (36%)
≥2 71 (61%) 66 (61%) 71 (64%)
Adapted Mayo score 7·0 (1·2) 6·9 (1·2) n=231; 7·0 (1·3)
≤7 131 (59%) 140 (62%) 137 (59%)
>7 92 (41%) 85 (38%) 94 (41%)
Mayo score endoscopic subscore 2·7 (0 5) 2·7 (0·5) 2·7 (0·5)
Presence of bowel urgency n=215; 201 (93%) n=221; 204 (92%) n=230; 213 (93%)
Presence of abdominal pain n=215; 197 (92%) n=221; 202 (91%) n=230; 202 (88%)
Inflammatory Bowel Disease Questionnaire n=222; 123·0 (98·0–145·0) n=222; 126·5 (102·0–151·0) n=229; 122·0 (97·0–147·0)
total score
Functional Assessment of Chronic Illness n=221; 30·0 (21·0–40·0) n=222; 33·0 (25·0–40·0) n=228; 31·0 (22·0–39·5)
Therapy—Fatigue score
Data are n (%), median (IQR), or mean (SD) for the intention-to-treat population, defined as upadacitinib 45 mg once daily 8-week induction responders who were enrolled
per protocol for the 52-week maintenance treatment period and received ≥1 dose of study drug (placebo, upadacitinib 15 mg once daily, or UPA 30 mg once daily). Baseline
is defined as the last non-missing value collected on or before the first induction dose. Bio-IR=inadequate response, loss of response, or intolerance to ≥1 biologic.
*Self-reported. †Self-reported and collected as a standard clinical trial demographic. ‡Corticosteroid use was tapered from week 0 of the U-ACHIEVE Maintenance study
according to the protocol-specified schedule (which could be adapted based on the discretion of the investigator). §Among patients receiving corticosteroids at baseline.
Two patients (placebo, n=1; upadacitinib 15 mg once daily, n=1) had reported baseline corticosteroid doses substantially greater than the usual maximum administered daily
dose (>80 mg of prednisone or equivalent).
Table 1: Baseline demographics and clinical characteristics (intention-to-treat population; n=681)
52 weeks of maintenance therapy in the U-ACHIEVE included 319 patients from U-ACHIEVE Induction,
Maintenance trial (Dec 14, 2016–Dec 13, 2021) and 341 patients from U-ACCOMPLISH, and 21 patients
included in the 8-week induction responder intention-to- from the phase 2b induction study. Details on the
treat efficacy population (figure 1). These responders numbers of participants from each country are included
982 www.thelancet.com/gastrohep Vol 8 November 2023
Articles
in the appendix (pp 3–8). 746 patients (representing 100
552·9 patient-years of exposure) who achieved a clinical
response after 8 weeks of upadacitinib 45 mg once daily 90
induction therapy were enrolled for 44-week or 52-week
maintenance therapy and were included in the 8-week 80
induction responder safety population (upadacitinib
15 mg once daily, n=250; upadacitinib 30 mg once daily, 70 42·9% (35·4–50·4)*†
n=251; placebo, n=245). The difference between the
53·6%
intention-to-treat and safety populations (n=65) was due to 60
30·1% (22·7–37·4)*†
Patients (%)
patients being enrolled for 44-week maintenance therapy
under earlier protocol amendments (n=61) and site non- 50 40·4%
compliance issues relating to informed consent (n=4).
40
Demographics and clinical characteristics at baseline
of patients entering U-ACHIEVE Maintenance were
30
generally well balanced across treatment groups in the
8-week induction responder intention-to-treat efficacy 20
population (table 1). Across treatment groups, 35–45% 10·8%
of patients were female, and the median age was 10
39·0–42·0 years; patients had a median disease duration
n=223 n=225 n=233
of 5·9–6·3 years and 38–41% of patients had a baseline 0
Placebo Upadacitinib 15 mg Upadacitinib 30 mg
adapted Mayo score greater than 7. Approximately half of once daily once daily
the patients in each treatment group had previously
Week 52 clinical remission
had an inadequate response, loss of response or
intolerance to biologics (48–52%); of these, almost Figure 2: Clinical remission per adapted Mayo score at week 52
two-thirds had received at least two biologics (61–64%). (intention-to-treat population; n=681)
Data are provided for the intention-to-treat population, defined as upadacitinib
A significantly greater proportion of patients in
45 mg once daily 8-week induction responders who were enrolled per protocol
the 8-week induction responder population (n=681) for the 52-week maintenance treatment period and received ≥1 dose of study
achieved clinical remission per adapted Mayo score at drug (placebo, upadacitinib 15 mg once daily, or upadacitinib 30 mg once daily).
week 52 with upadacitinib 15 mg once daily (40·4%) and Results are based on non-responder imputation incorporating multiple
imputations to handle missing data owing to COVID-19 (appendix p 21). The
upadacitinib 30 mg once daily (53·6%) versus placebo
adjusted differences, 95% CI (normal approximation to the binomial distribution)
(10·8%; both p<0·0001; figure 2). A greater proportion of and p value were calculated according to the Cochran–Mantel–Haenszel test
patients who received upadacitinib achieved endoscopic adjusted for strata (corticosteroid use at week 0 [yes or no], clinical remission
improvement than did those who received placebo status at week 0 [yes or no], bio-IR status at baseline [bio-IR or non-bio-IR]).
Bio-IR=inadequate response, loss of response, or intolerance to ≥1 biologic.
(upadacitinib 15 mg once daily 48·5%; upadacitinib
*p<0·0001 vs placebo. †Adjusted difference (95% CI) vs placebo.
30 mg once daily 63·3%; vs 14·1% for placebo; both
p<0·0001); this was also seen with maintenance of
endoscopic improvement (upadacitinib 15 mg once Both upadacitinib 15 mg once daily and 30 mg once
daily 61·2%; upadacitinib 30 mg once daily 71·0%; daily were more efficacious than placebo across all
vs 18·4% for placebo; both p<0·0001), and histologic– subgroups for achievement of the primary endpoint of
endoscopic mucosal improvement (upadacitinib clinical remission per adapted Mayo score when stratified
15 mg once daily 40·5%; upadacitinib 30 mg once by baseline demographics and clinical characteristics,
daily 56·0%; vs 12·3%; both p<0·0001). Achievement of including sex (appendix pp 22–23). Across bio-IR (n=336),
all other clinical, endoscopi c, and histological endpoints non-bio-IR (n=345), and anti-TNF-IR (n=306; 91% of
was also significantly higher with both upadacitinib bio-IR population) subgroups within the 8-week
maintenance doses versus placebo (all p<0·0001; table 2). induction responder population, both upadacitinib
At week 52, a significantly greater proportion of patients 15 mg once daily and 30 mg once daily were more
with upadacitinib achieved no abdominal pain (45·8% for efficacious than placebo after 52 weeks of maintenance
upadacitinib 15 mg once daily and 59·7% for upadacitinib treatment across the primary endpoint of clinical
30 mg once daily, vs 20·6% for placebo; both p<0·0001) remission, and all key secondary endpoints (figure 3;
and no bowel urgency (53·8% for upadacitinib appendix pp 9–10). Upadacitinib 30 mg once daily had
15 mg once daily and 66·9% for upadacitinib 30 mg once numerically better efficacy than upadacitinib 15 mg once
daily, vs 18·4% for placebo; both p<0·0001). Improvements daily across all endpoints in each subgroup, except for
in both FACIT-F and total IBDQ scores were significantly maintenance of endoscopic improvement in the bio-IR
greater with upadacitinib than placebo (p<0·0001; and anti-TNF-IR subgroups. Generally, efficacy was
table 2). Across all analysed efficacy endpoints, outcomes similar in the bio-IR and anti-TNF-IR subgroups
were numerically better with upadacitinib 30 mg once (although this should be interpreted with respect to the
daily than upadacitinib 15 mg once daily (table 2). fact that 91% of the bio-IR population was made up of
www.thelancet.com/gastrohep Vol 8 November 2023 983
Articles
Placebo (n=223) Upadacitinib 15 mg Adjusted difference Upadacitinib 30 mg Adjusted difference
once daily (n=225) vs placebo* once daily (n=233) vs placebo*
Maintenance of clinical response per n=204; 21·5% n=197; 65·6% 43·9† (35·4–52·5) n=217; 77·5% 55·6† (47·8–63·4)
adapted Mayo score
Maintenance of clinical remission per n=85; 18·8% n=76; 53·6% 34·9† (21·2–48·5) n=87; 65·8% 46·9† (34·0–59·8)
adapted Mayo score
Corticosteroid-free clinical remission per n=85; 18·8% n=76; 52·3% 33·7† (20·0–47·3) n=87; 64·6% 45·5† (32·6–58·5)
adapted Mayo score
Endoscopic improvement 14·1% 48·5% 34·4† (26·7–42·1) 63·3% 49·0† (41·4–56·7)
Maintenance of endoscopic improvement n=115; 18·4% n=97; 61·2% 42·2† (30·4–53·9) n=118; 71·0% 51·5† (40·9–62·1)
Endoscopic remission 6·1% 24·9% 18·6† (12·2–25·0) 28·3% 21·9† (15·4–28·5)
Histologic–endoscopic mucosal 12·3% 40·5% 28·5† (21·1–35·9) 56·0% 43·8† (36·1–51·5)
improvement
Mucosal healing 5·1% 18·8% 13·5† (7·8–19·3) 22·6% 17·2† (11·2–23.3)
No abdominal pain 20·6% 45·8% 24·7† (16·5–33·0) 59·7% 38·9† (30·7–47·1)
No bowel urgency 18·4% 53·8% 35·3† (27·3–43·4) 66·9% 48·2† (40·4–56·0)
Change from baseline in Functional 2·6 8·1 5·5† (3·5–7·5) 9·8 7·2† (5·3–9·2)
Assessment of Chronic Illness
Therapy—Fatigue score
Change from baseline in Inflammatory 16·3 48·2 31·8† (23·9–39·8) 59·4 43·1† (35·4–50·8)
Bowel Disease Questionnaire total score
Data are n (%), % adjusted (95% CI), least squares mean, and least squares mean (95% CI). Data are provided for the intention-to-treat population, defined as upadacitinib
45 mg once daily 8-week induction responders who were enrolled per protocol for the 52-week maintenance treatment period and received ≥1 dose of study drug (placebo,
upadacitinib 15 mg once daily, or upadacitinib 30 mg once daily). Baseline is defined as the last non-missing value collected on or before the first induction dose. Results for
categorical endpoints are based on non-responder imputation incorporating multiple imputations to handle missing data owing to COVID-19 (appendix p 21). The adjusted
differences, 95% CI (normal approximation to the binomial distribution within each stratum) and p value were calculated according to the Cochran–Mantel–Haenszel test
adjusted for strata (corticosteroid use at week 0 [yes or no], clinical remission status at week 0 [yes or no], bio-IR status at baseline [bio-IR or non-bio-IR]). Results for
continuous endpoints are based on return-to-baseline multiple imputation; least squares mean, adjusted 95% CI and p values are the synthetic results based on ANCOVA
with baseline, week 0, treatment, and strata (corticosteroid use at week 0 [yes or no], clinical remission status at week 0 [yes or no], bio-IR status at baseline [bio-IR or non-
bio-IR]) in the model using the PROC MIANALYZE procedure. Bio-IR=inadequate response, loss of response, or intolerance to ≥1 biologic. *Adjusted difference in percentage
points for categorical endpoints. †p<0·0001 vs placebo.
Table 2: Key secondary efficacy endpoints at week 52 (intention-to-treat population; n=681)
the anti-TNF-IR population) and was consistent with the of adjudicated gastrointestinal perforation in either
overall 8-week induction responder population (figure 3, upadacitinib group, compared with two cases (1·5 events
appendix pp 9–10). per 100 patient-years) with placebo. EAERs of neutropenia
Calculation of NNT values in the intention-to-treat were 5·2, 5·5, and 8·7 events per 100 patient-years with
population showed greater efficacy at 52 weeks of placebo, upadacitinib 15 mg once daily, and upadacitinib
maintenance therapy for patients treated with either 30 mg once daily, respectively; EAERs of creatine
upadacitinib 15 mg once daily or 30 mg once daily versus phosphokinase elevation were 3·7, 8·0, and 10·1 events
placebo for the primary endpoint of clinical remission per 100 patient-years, respectively.
(NNT 3·4 and 2·4, respectively). Across key secondary Hepatic disorders were more common with upadacitinib
efficacy endpoints, NNT values ranged between 15 mg once daily and upadacitinib 30 mg once daily versus
2·3 and 7·5 for upadacitinib 15 mg once daily and placebo, with EAERs of 17·0 and 9·2 versus 5·9 events
1·8–5·9 for upadacitinib 30 mg once daily (appendix per 100 patient-years, respectively. Of the 31 patients
pp 24–25). receiving upadacitinib treatment with any event of
EAERs for any treatment-emergent adverse event, hepatic disorder, the most frequent events were elevated
either serious or leading to discontinuation were alanine aminotransferase (seven events with upadacitinib
numerically higher with placebo than either upadacitinib 15 mg once daily and seven events with upadacitinib
dose; no deaths were reported (table 3). For AESIs, the 30 mg once daily) and elevated aspartate aminotransferase
EAERs of serious infection were 5·9, 5·0, and 3·2 events (nine events with upadacitinib 15 mg once daily and
per 100 patient-years with placebo, upadacitinib five events with upadacitinib 30 mg once daily).
15 mg once daily, and upadacitinib 30 mg once daily, One non-serious case of drug-induced liver injury led to
respectively (table 3). Herpes zoster was reported only discontinuation of upadacitinib. There were no confirmed
with upadacitinib in a dose-dependent manner cases of Hy’s law.
(upadacitinib 15 mg once daily 6·0 events per There was one malignancy (excluding non-melanoma
100 patient-years; upadacitinib 30 mg once daily skin cancer) with placebo, one with upadacitinib
7·3 events per 100 patient-years). There were no cases 15 mg once daily, and two with upadacitinib 30 mg once
984 www.thelancet.com/gastrohep Vol 8 November 2023
Articles
100 UPA 15 mg once daily Overall
UPA 30 mg once daily Non-bio-IR
Bio-IR
Anti-TNF-IR
80
Response rate difference vs placebo (%)
60
40
20
0
Clinical remission Maintenance of Corticosteroid-free Endoscopic Endoscopic remission Histological–endoscopic Mucosal healing
clinical response clinical remission improvement mucosal improvement
Figure 3: Efficacy at week 52 in subgroups by biological status (intention-to-treat population)
The efficacy analysis was done in the non-bio-IR, bio-IR, and anti-TNF-IR subgroups of the intention-to-treat population (upadacitinib 45 mg once daily 8-week induction responders who were
enrolled per protocol for the 52-week maintenance treatment period and received ≥1 dose of study drug [placebo, upadacitinib 15 mg once daily, or upadacitinib 30 mg once daily]). Results are based
on non-responder imputation incorporating multiple imputations to handle missing data owing to COVID-19. For the overall population, adjusted differences, 95% CI (normal approximation to the
binomial distribution within each stratum) and p value were calculated according to the Cochran–Mantel–Haenszel test adjusted for strata (corticosteroid use at week 0 [yes or no], clinical remission
status at week 0 [yes or no], bio-IR status at baseline [bio-IR or non-bio-IR]). For the subgroup data, unadjusted differences are shown with 95% CI calculated by means of normal approximation to the
binomial distribution. Anti-TNF=anti-tumour necrosis factor. Anti-TNF-IR=inadequate response, loss of response, or intolerance to ≥1 TNF inhibitor. Bio-IR=inadequate response, loss of response, or
intolerance to ≥1 biologic.
daily (0·7, 0·5, and 0·9 events per 100 patient-years, (n=53; 7%), hypertension (n=111; 15%), diabetes
respectively). There was one adjudicated MACE with (n=43; 6%), current or former tobacco use (n=305;
placebo and one with upadacitinib 30 mg once daily 41%), and low concentrations of high-density lipo
(0·7 and 0·5 events per 100 patient-years, respectively); protein cholesterol (n=102; 14%; appendix p 13).
there were no cases with upadacitinib 15 mg once daily. Additionally, five (1%) patients had previous VTE.
There were no cases of adjudicated VTE with placebo, Assessment of the upadacitinib-treated patients who
two cases with upadacitinib 15 mg once daily, and had an adjudicated MACE (one [<1%] of 501 patients) or
two with upadacitinib 30 mg once daily (1·0 and 0·9 events VTE (four [1%] of 501 patients) during maintenance
per 100 patient-years for upadacitinib 15 mg once daily, therapy showed that all had at least one known risk
and upadacitinib 30 mg once daily, respectively). factor (see appendix pp 14–16 for details of these events
Across treatment groups, the EAERs of any and relevant known risk factors). There were
treatment-emergent adverse event, either serious or two adjudicated MACEs: one acute myocardial infarc
leading to discontinuation, and AESIs were generally tion in a placebo-treated patient and one subarachnoid
similar between each of the bio-IR, non-bio-IR, and haemorrhage in a patient receiving upadacitinib
anti-TNF-IR subgroups and were similar to the overall 30 mg once daily. Four patients had adjudicated VTE:
population, except for lower EAERs of any treatment- two patients receiving upadacitinib 15 mg once daily had
emergent adverse event across treatments in the a pulmonary embolism (both had mild disease [adapted
non-bio-IR subgroup (appendix pp 11–12). Mayo score ≤7] at the time of the event) and two patients
To investigate the safety of upadacitinib in patients at receiving upadacitinib 30 mg once daily had a deep vein
higher risk of MACE, VTE, and malignancies, data thrombosis (one with mild disease at the time of the
from the safety population were reviewed for known event and one with severe [adapted Mayo score >7]).
baseline risk factors that might increase the risk of None of the female patients who had a MACE or VTE
these events. Given that advanced age is a known risk reported use of concomitant oral contraception or
factor for cardiovascular events and VTE, it is of note hormone replacement therapy. Four (1% of patients)
that 243 (33%) of 746 patients in the safety population malignancies (excluding non-melanoma skin cancer)
were aged at least 50 years and 65 (9%) were 65 years or were reported, all of which were considered serious; of
older. The safety population also included a substantial these, three occurred in upadacitinib-treated patients,
proportion of patients with one or more known one invasive breast carcinoma in the upadacitinib
cardiovascular risk factor at baseline (n=417; 56%), 15 mg once daily group, one adenocarcinoma of the
including at least one previous cardiovascular event colon and one small cell carcinoma of the prostate in the
www.thelancet.com/gastrohep Vol 8 November 2023 985
Articles
Placebo (n=245) Upadacitinib 15 mg Upadacitinib 30 mg
135·0 patient-years once daily (n=250) once daily (n=251)
199·4 patient-years 218·5 patient-years
Event
Any treatment-emergent adverse event 674 (499·4, 461·7–537·1) 626 (313·9, 289·3–338·5) 691 (316·2, 292·7–339·8)
Serious treatment-emergent adverse events 28 (20·7, 13·1–28·4) 24 (12·0, 7·2–16·8) 22 (10·1, 5·9–14·3)
Treatment-emergent adverse events leading to discontinuation 26 (19·3, 11·9–26·7) 11 (5·5, 2·3–8·8) 19 (8·7, 4·8–12·6)
Treatment-emergent adverse events leading to death 0 0 0
Adverse event of special interest
Serious infection 8 (5·9, 1·8–10·0) 10 (5·0, 1·9–8·1) 7 (3·2, 0·8–5·6)
Opportunistic infection (excluding tuberculosis and herpes zoster) 2 (1·5, 0·0–3·5) 2 (1·0, 0·0–2·4) 2 (0·9, 0·0–2·2)
Herpes zoster 0 12 (6·0, 2·6–9·4) 16 (7·3, 3·7–10·9)
Malignancy (excluding non-melanoma skin cancer) 1 (0·7, 0·0–2·2) 1 (0·5, 0·0–1·5) 2 (0·9, 0·0–2·2)
Non-melanoma skin cancer 0 0 3 (1·4, 0·0–2·9)
Renal dysfunction 1 (0·7, 0·0–2·2) 1 (0·5, 0·0–1·5) 1 (0·5, 0·0–1·4)
Hepatic disorder 8 (5·9, 1·8–10·0) 34 (17·0, 11·3–22·8) 20 (9·2, 5·1–13·2)
Adjudicated gastrointestinal perforation 2 (1·5, 0·0–3·5) 0 0
Adjudicated major adverse cardiovascular event* 1 (0·7, 0·0–2·2) 0 1 (0·5, 0·0–1·4)
Adjudicated venous thromboembolic event† 0 2 (1·0, 0·0–2·4) 2 (0·9, 0·0–2·2)
Anaemia 19 (14·1, 7·7–20·4) 12 (6·0, 2·6–9·4) 10 (4·6, 1·7–7·4)
Neutropenia 7 (5·2, 1·3–9·0) 11 (5·5, 2·3–8·8) 19 (8·7, 4·8–12·6)
Lymphopenia 5 (3·7, 0·5–7·0) 10 (5·0, 1·9–8·1) 7 (3·2, 0·8–5·6)
Creatine phosphokinase elevation 5 (3·7, 0·5–7·0) 16 (8·0, 4·1–12·0) 22 (10·1, 5·9–14·3)
Data are events (events per 100 patient-years; 95% CI). Data are from the safety population, defined as the upadacitinib 45 mg once daily 8-week induction responders
per protocol for 44-week or 52-week maintenance therapy, and received ≥1 dose of study drug (placebo, upadacitinib 15 mg once daily, and upadacitinib 30 mg once daily).
The 95% CIs were calculated by normal approximation to the Poisson distribution, so 95% CIs were not calculated for event rates of 0. *Defined as cardiovascular death,
nonfatal myocardial infarction, and non-fatal stroke. †Defined as deep vein thrombosis and pulmonary embolism (fatal and non-fatal).
Table 3: Treatment-emergent adverse events and adverse events of special interest over 52 weeks (safety population; n=746)
upadacitinib 30 mg once daily group. All three patients cases were reported in Latin America, although few
had at least one relevant known risk factor, and a time upadacitinib-treated patients were included from that
to onset from the first upadacitinib dose within region (upadacitinib 15 mg once daily n=9; upadacitinib
approximately 1 year. No malignancies (excluding non- 30 mg once daily n=10). Less than 5% (n=24) of patients
melanoma skin cancer) with upadacitinib were in this study were vaccinated against herpes zoster or
considered by the investigator as having a reasonable had previous history of herpes zoster (appendix p 13),
possibility of being related to upadacitinib treatment making it difficult to assess the effect of these factors on
(appendix pp 14–16). the incidence of herpes zoster. For patients treated with
Most events of herpes zoster involved a single upadacitinib, two herpes zoster events occurred among
dermatome and were not serious. Of the cases with more 17 patients with previous vaccination, and four events
extensive dermatomal involvement, there were two cases occurred among the 15 patients with previous history of
of herpes zoster with unilateral involvement of multiple herpes zoster (appendix p 17).
dermatomes in the upadacitinib 15 mg once daily group Overall, calculation of NNH showed generally similar
and five cases in the upadacitinib 30 mg once daily safety at 52 weeks for patients treated with upadacitinib
group. In addition, in the upadacitinib 30 mg once daily 15 mg once daily or upadacitinib 30 mg once daily versus
group, there were two cases of disseminated herpes placebo, with no risk differences in overall or serious
zoster with cutaneous involvement only (ie, without treatment-emergent adverse events (appendix pp 18–20).
central nervous system involvement) and one case of There was a lower risk of treatment-emergent adverse
herpes zoster with meningoencephalopathic involve events leading to discontinuation with upadacitinib
ment. No events had lung or liver involvement. EAERs of 15 mg once daily versus placebo (NNH –16·1). Higher
herpes zoster in upadacitinib-treated patients varied by risks were seen for upadacitinib 15 mg once daily and
geographical region, with the highest rates seen in upadacitinib 30 mg once daily versus placebo for herpes
western Europe and Oceania for upadacitinib 15 mg zoster (NNH 21·2 and 17·8, respectively), as well as
once daily (12·3 events per 100 patient-years) and Japan hepatic disorders with upadacitinib 15 mg once daily
for upadacitinib 30 mg once daily (14·9 events (NNH 20·8) and neutropenia with upadacitinib
per 100 patient-years; appendix p 17). No herpes zoster 30 mg once daily (NNH 25·6; appendix pp 18–20).
986 www.thelancet.com/gastrohep Vol 8 November 2023
Articles
Discussion immunosuppression (2021). Current recommendations
In this final efficacy analysis of 681 patients with state that patients are brought up to date with all relevant
moderately to severely active ulcerative colitis who achieved immunisations, including prophylactic herpes zoster
clinical response after 8 weeks of induction treatment with vaccinations, before initiating advanced therapies,
upadacitinib 45 mg once daily, both maintenance doses including upadacitinib.15,16
(upadacitinib 15 mg once daily and 30 mg once daily) In November, 2022, the EMA issued recommendations
showed efficacy across the primary endpoint of clinical to minimise the risk of serious side-effects with JAK
remission and all key secondary endpoints assessed at inhibitors, particularly relating to MACEs, VTEs, and
week 52. Both upadacitinib maintenance doses were well malignancy, based on potential safety issues reported
tolerated up to week 52 with no new safety signals in ORAL Surveillance.9–11 Consequently, the EMA
observed. Efficacy results and the safety profile of recommends that JAK inhibitors should only be used
upadacitinib for the entire patient population were when no suitable alternatives are available in patients at
consistent with those previously reported by Danese and higher risk of MACE or malignancy, patients aged
colleagues4 in the smaller primary registrational study 65 years or older, and current or former long-term
analysis of the first 451 patients randomly assigned into the smokers, and should be used cautiously in patients
maintenance trial. with known risk factors for VTE. Clinicians prescribing
In this analysis, significantly higher proportions of JAK inhibitors to patients with these risk factors are
patients achieved clinical remission with upadacitinib advised to assess the suitability of alternative treatments
15 mg once daily and upadacitinib 30 mg once daily and make individual benefit–risk assessments for their
compared with placebo, with similar proportions patients. Regarding the posology of upadacitinib, it is
reported as in the primary analysis.4 Similar proportions recommended to use upadacitinib 15 mg once daily for
of patients achieved clinical remission in subgroup patients at high risk of MACE, VTE, or malignancy
analyses of baseline demographics and clinical charac whenever possible, and to use the lowest effective dose
teristics. The proportions of patients achieving key to maintain response.
secondary efficacy endpoints with both upadacitinib No dose-dependent risk for MACE, VTE, or malignancy
maintenance doses were also consistent with those excluding non-melanoma skin cancer has been observed
previously reported4 and, for some endpoints, were in the indications for which upadacitinib is approved,14
numerically higher in this final, larger analysis. Although including for patients with ulcerative colitis in the
both upadacitinib maintenance doses (15 mg once daily current analysis. In this study, despite a substantial
and 30 mg once daily) showed efficacy, numerically proportion of the population sharing characteristics with
greater efficacy was seen with the higher dose across all patients in ORAL Surveillance (ie, aged ≥50 years with
assessed endpoints, both in the current analysis and the one or more known baseline risk factor for cardiovascular
primary analysis.4 However, these comparisons are events), there were few cases of adjudicated MACE, VTE,
descriptive in nature given that the study was not or malignancy (excluding non-melanoma skin cancer).
designed to statistically compare upadacitinib doses. Furthermore, all upadacitinib-treated patients with
Consistent with other approved upadacitinib an adjudicated MACE or VTE had more than one known
indications,12–14 dose dependence was observed for AESIs risk factor. No malignancies were considered by the
of neutropenia, creatine phosphokinase elevations, and investigator as having a reasonable possibility of being
herpes zoster. Alanine aminotransferase and aspartate related to upadacitinib treatment and, given the long
aminotransferase elevations were more common with latency time in the development of solid tumours
upadacitinib than with placebo, with more events (≥4 years),17,18 the relatively short times between receipt
observed in patients receiving upadacitinib 15 mg once of first upadacitinib dose and time to onset of the
daily than with upadacitinib 30 mg once daily. In this event (within approximately 1 year) suggests temporal
analysis, non-melanoma skin cancer was observed only implausibility for upadacitinib in the oncogenesis of the
in patients receiving upadacitinib 30 mg once daily malignancies reported. The long-term safety of
(two out of three cases in patients ≥70 years old), with no upadacitinib will continue to be evaluated by means
cases in patients receiving upadacitinib 15 mg once of data from the ongoing U-ACTIVATE long-term
daily or placebo. Most events of herpes zoster involved a extension study (NCT03006068), as well as from other
single dermatome and were non-serious. Of note, few postmarketing safety commitments by the sponsor.
patients (3%) in the trial had been vaccinated against Although patients were eligible for enrolment in the
herpes zoster. This was because most patients in the trial U-ACHIEVE Maintenance trial with treatment failure in
were younger than 60 years at baseline, and U-ACHIEVE at least one type of conventional or biological therapy,
Induction and U-ACCOMPLISH started in close almost half of patients (49%) in the intention-to-treat
proximity to approval of the vaccine in patients aged population had an inadequate response to biologic therapy
50 to 60 years (2017 onwards depending on region), (primarily anti-TNFs). Inadequate response or intolerance
and before the vaccine was approved for patients between to at least one anti-TNF agent is a label-specified
the ages of 18 and 50 years with increased risk of prerequisite for treatment in some countries where
www.thelancet.com/gastrohep Vol 8 November 2023 987
Articles
upadacitinib is approved; therefore, it is likely that many Allergan (Warner Chilcott), Atlantic Healthcare, Bristol-Myers Squibb,
patients initiating upadacitinib in real-world practice have Celgene, Celltrion, Eli Lilly, Ferring Pharmaceuticals, Gilead, GSK,
Janssen, MSD, Napp, Pfizer, Shire, Takeda, and Vifor Pharma; has
had an inadequate response or intolerance to biologics received speaker fees and sponsorship for academic meetings from
(including anti-TNFs), meaning that understanding the AbbVie, Allergan (Warner Chilcott), Ferring Pharmaceuticals, Janssen,
efficacy and safety of upadacitinib in these patients is MSD, Napp, Norgine, Pfizer, Shire, Tillotts Pharma, and Takeda; and has
important. In this analysis, the efficacy and safety profile received investigator-led research grants from AbbVie, Gilead, Pfizer,
Shire, and Takeda. PDRH has received grants from AbbVie, the Crohn’s &
of upadacitinib in patients who had had an inadequate Colitis Foundation, the National Institutes of Health, and Takeda; and has
response, loss of response or intolerance to biologics served as a consultant for Eli Lilly, the Gastrointestinal Health Foundation,
(including anti-TNFs) and those who had not had an Imedex, Pfizer, Takeda, and Vindico Medical Education. QC declares no
inadequate response, loss of response or intolerance to competing interests. HN has received support from AbbVie, Celgene
Corporation, Daiichi Sankyo, EA Pharma, Janssen Pharmaceutical,
biologics generally reflected the overall population. JIMRO, Kissei Pharmaceutical, Kyorin Pharmaceutical, Mitsubishi
The main limitation of this analysis is that some Tanabe Pharma, Mochida Pharmaceutical, Nippon Kayaku, Pfizer, Takeda,
analyses were post hoc; results from these should be and Zeria Pharmaceutical; as well as grants for commissioned or joint
interpreted with respect to the study design. In addition, research from Boehringer Ingelheim, Bristol Myers Squibb, and Hoya
Group Pentax Medical. J-FC has received personal fees from AbbVie,
further data on upadacitinib beyond 52 weeks’ treatment Amgen, Boehringer Ingelheim, Celgene, Celltrion, Enterome, Ferring,
are warranted. Genentech, Janssen–Johnson & Johnson, MedImmune, Merck, Pfizer,
In conclusion, in patients with moderately to severely Protagonist, PPM Services, Second Genome, Seres, Shire, Takeda, and
active ulcerative colitis who responded to 8 weeks’ Theradiag; has received grant support from AbbVie, Janssen, Johnson &
Johnson, and Takeda; and holds stock options in Genfit and Intestinal
upadacitinib 45 mg once daily induction therapy, both Biotech Development. EVL has received consulting fees from AbbVie,
upadacitinib maintenance doses were significantly Alvotech, Amgen, Arena, Avalo Therapeutics, BMS, Boehringer
more efficacious than placebo for achieving important Ingelheim, Calibr, Celgene, Celltrion Healthcare, Eli Lilly, Fresenius Kabi,
clinical, endoscopic, and histological outcomes, while Genentech, Gilead, GlaxoSmithKline, Gossamer Bio, Iota Biosciences,
Iterative Scopes, Janssen, KLS Diagnostics, Morphic Therapeutics, Ono
maintaining an acceptable safety profile with no new Pharma, Pfizer, Protagonist, Scipher Medicine, Sun Pharma, Surrozen,
safety risks in the full trial population over 52 weeks. Takeda, and UCB; has served as an advisory board participant for Eli Lilly
The favourable benefit–risk profile of both maintenance and Morphic; has received research support from AbbVie, BMS,
Celgene/Receptos, Genentech, Gilead, Gossamer Bio, Janssen,
doses in this analysis was consistent with that observed
Pfizer, Takeda, Theravance, and UCB; and holds stock in Exact Sciences.
in the primary analysis of a smaller patient population. RP has received consulting fees, speaker fees, and research support from
Overall, these findings support the use of upadacitinib as Abbott, AbbVie, Alimentiv (formerly Robarts Clinical Trials), Amgen,
a therapeutic option for treating patients with moderately Arena Pharmaceuticals, AstraZeneca, BMS, Boehringer Ingelheim,
Celgene, Celltrion, Cosmos Pharmaceuticals, Eisai, Élan, Eli Lilly, Ferring,
to severely active ulcerative colitis, for whom a large
Galapagos, Genentech, Gilead, GlaxoSmithKline, Janssen, Merck, Mylan,
unmet need persists. Oppilan Pharma, Pandion Pharma, Pfizer, Progenity, Protagonist
Contributors Therapeutics, Roche, Sandoz, Satisfai Health, Schering-Plough, Shire,
SV, SD, XH, JOL, PDRH, QC, HN, J-FC, EVL, and RP participated in Sublimity Therapeutics, Takeda, Theravance, and UCB.
data acquisition. SV, SD, WZ, YSG, PDRH, J-FC, and RP participated in Data sharing
study design. WZ, DI, JK, GL, XY, SC, YSG, and RP assessed and verified AbbVie is committed to responsible data sharing regarding the clinical
the data. XY, SC, and RP participated in statistical analysis. All authors trials that it sponsors. Sharing includes access to anonymised,
had access to relevant data and participated in data interpretation, individual, and trial-level data (analysis datasets), and other information
critically reviewed the manuscript, and provided final approval for (eg, protocols, clinical study reports, and analyses plans), as long as the
publication. No honoraria or payments were made for authorship. trials are not part of an ongoing or planned regulatory submission, and
Declaration of interests accepting requests for clinical trial data for unlicensed products and
SV has received grants from AbbVie, Galapagos, Johnson & Johnson, indications. These clinical trial data can be requested by any qualified
Pfizer, and Takeda; and consulting or speaking fees from AbbVie, Abivax, researchers who engage in rigorous independent scientific research and
Alimentiv (formerly Robarts Clinical Trials), Arena Pharmaceuticals, will be provided following review and approval of a research proposal
Avaxia, Boehringer Ingelheim, Celgene, Dr Falk Pharma, Ferring, and statistical analysis plan and execution of a data sharing statement.
Galapagos, Genentech-Roche, Gilead, Hospira, Janssen, MSD, Data requests can be submitted at any time after approval in the USA
Mundipharma, Pfizer, Prodigest, Progenity, Prometheus, Second and Europe and acceptance for publication, and the data will be
Genome, Shire, Takeda, Theravance, and Tillotts Pharma. SD has received accessible for 12 months, with possible extensions considered. Further
consultancy fees from Boehringer Ingelheim, Celgene, Celltrion, Eli Lilly, instructions can be provided by the corresponding author, on request.
Enthera, Ferring Pharmaceuticals, Gilead, Hospira, Janssen, Johnson & Acknowledgments
Johnson, MSD, Mundipharma, Mylan, Pfizer, Roche, Sandoz, Sublimity AbbVie and the authors thank the participants, study sites, and
Therapeutics, Takeda, TiGenix, UCB, and Vifor. WZ is a former employee investigators who participated in this clinical trial. AbbVie funded this
of AbbVie and may hold AbbVie stock or stock options. DI, JK, GL, XY, study and participated in the study design, research, analysis, data
SC, and YSG are full-time employees of AbbVie and may hold AbbVie collection, interpretation of data, and the review and approval of the
stock or stock options. XH reports clinical research funding from AbbVie, publication. Medical writing assistance was provided by Fraser Harris,
Abivax, Alphasigma, Arena, Gilead, Eli Lilly, Enterome, Fresenius-Kabi, on behalf of 2 the Nth (Cheshire, UK), and was funded by AbbVie.
Janssen, InDex Pharmaceuticals, Pfizer, Prometheus Biosciences,
Sangamo, Takeda, and Theravance; serving on advisory boards for References
AbbVie, Abivax, Boehringer Ingelheim, Celltrion, Fresenius-Kabi, 1 Ungaro R, Mehandru S, Allen PB, Peyrin-Biroulet L, Colombel JF.
Galapagos, Janssen, Nestlé Health Sciences, Nordic Pharma, and Viatris; Ulcerative colitis. Lancet 2017; 389: 1756–70.
and participating in lectures and educational activities for AbbVie, 2 Ng SC, Shi HY, Hamidi N, et al. Worldwide incidence and
Amgen, Celltrion, Fresenius-Kabi, Janssen, MSD, Nordic Pharma, Nestlé prevalence of inflammatory bowel disease in the 21st century:
a systematic review of population-based studies. Lancet 2017;
Health Sciences, Nutricia, Pfizer, Tillotts, Takeda, and Viatris. JOL has
390: 2769–78.
served as a consultant and an advisory board participant for AbbVie,
988 www.thelancet.com/gastrohep Vol 8 November 2023
Articles
3 US FDA Prescribing Information. RINVOQ (upadacitinib). 12 Simpson EL, Papp KA, Blauvelt A, et al. Efficacy and safety of
October, 2022. https://www.rxabbvie.com/pdf/rinvoq_pi.pdf upadacitinib in patients with moderate to severe atopic
(accessed March 10, 2023). dermatitis: analysis of follow-up data from the Measure Up 1 and
4 Danese S, Vermeire S, Zhou W, et al. Upadacitinib as induction and Measure Up 2 randomized clinical trials. JAMA Dermatol 2022;
maintenance therapy for moderately to severely active ulcerative 158: 404–13.
colitis: results from three phase 3, multicentre, double-blind, 13 Cohen SB, van Vollenhoven RF, Winthrop KL, et al. Safety profile of
randomised trials. Lancet 2022; 399: 2113–28. upadacitinib in rheumatoid arthritis: integrated analysis from the
5 Sandborn WJ, Ghosh S, Panes J, et al. Efficacy of upadacitinib in SELECT phase III clinical programme. Ann Rheum Dis 2021;
a randomized trial of patients with active ulcerative colitis. 80: 304–11.
Gastroenterology 2020; 158: 2139–49. 14 Burmester GR, Cohen SB, Winthrop KL, et al. Safety profile of
6 Rinvoq. Summary of product characteristics. EMA. 2022. upadacitinib over 15 000 patient-years across rheumatoid arthritis,
https://www.ema.europa.eu/en/documents/product-information/ psoriatic arthritis, ankylosing spondylitis and atopic dermatitis.
rinvoq-epar-product-information_en.pdf (accessed Sept 15, 2022). RMD Open 2023; 9: E002735.
7 Boland BS, Sandborn WJ, Chang JT. Update on Janus kinase 15 Centers for Disease Control and Prevention. Shingrix
antagonists in inflammatory bowel disease. recommendations. cdc.gov/vaccines/vpd/shingles/hcp/Shingrix/
Gastroenterol Clin North Am 2014; 43: 603–17. recommendations.html# (accessed Dec 14, 2022).
8 Danese S, Argollo M, Le Berre C, Peyrin-Biroulet L. JAK selectivity 16 Anderson TC, Masters NB, Guo A, et al. Use of recombinant zoster
for inflammatory bowel disease treatment: does it clinically matter? vaccine in immunocompromised adults aged ≥19 years:
Gut 2019; 68: 1893–99. recommendations of the Advisory Committee on Immunization
9 European Medicines Agency. EMA confirms measures to minimise Practices—United States, 2022. MMWR Morb Mortal Wkly Rep
risk of serious side effects with Janus kinase inhibitors for chronic 2022; 71: 80–84.
inflammatory disorders. 2022. https://www.ema.europa.eu/en/ 17 Howard J. Minimum latency & types or categories of cancer.
news/ema-confirms-measures-minimise-risk-serious-side-effects- https://www.cdc.gov/wtc/pdfs/policies/wtchpminlatcancer2014-
janus-kinase-inhibitors-chronic (accessed Nov 11, 2022). 11-07-508.pdf (accessed Aug 21, 2023).
10 European Medicines Agency. Janus kinase inhibitors (JAKi). 2022. 18 Frost G. The latency period of mesothelioma among a cohort of
https://www.ema.europa.eu/en/medicines/human/referrals/janus- British asbestos workers (1978-2005). Br J Cancer 2013;
kinase-inhibitors-jaki (accessed Feb 21, 2023). 109: 1965–73.
11 Ytterberg SR, Bhatt DL, Mikuls TR, et al. Cardiovascular and cancer
risk with tofacitinib in rheumatoid arthritis. N Engl J Med 2022;
386: 316–26.
www.thelancet.com/gastrohep Vol 8 November 2023 989
You might also like
- Tofacitinib As Induction and Maintenance Therapy For Ulcerative ColitisDocument14 pagesTofacitinib As Induction and Maintenance Therapy For Ulcerative Colitismichal ben meronNo ratings yet
- Avelumab Plus Axitinib Versus Sunitinib For Advanced Renal-Cell CarcinomaDocument13 pagesAvelumab Plus Axitinib Versus Sunitinib For Advanced Renal-Cell CarcinomaCarlos Rodolfo SinibaldiNo ratings yet
- Ulcerative ColitisDocument8 pagesUlcerative Colitisfidah12012000No ratings yet
- Sepsis y SNDocument7 pagesSepsis y SNAdela FuentesNo ratings yet
- Clinical Outcomes of Esophagogastroduodenoscopy In.27Document6 pagesClinical Outcomes of Esophagogastroduodenoscopy In.27Agung KaryawinaraNo ratings yet
- Proktitis 1Document2 pagesProktitis 1adi chandraNo ratings yet
- FDA Approves Lilly's Omvoh - (Mirikizumab-Mrkz), A First-in-Class Treatment For Adults With Moderately To Severely Active Ulcerative ColitisDocument4 pagesFDA Approves Lilly's Omvoh - (Mirikizumab-Mrkz), A First-in-Class Treatment For Adults With Moderately To Severely Active Ulcerative ColitisOscar OrtegaNo ratings yet
- Alimentary TractDocument8 pagesAlimentary Tractgrace liwantoNo ratings yet
- Tumour-Agnostic Efficacy and Safety of Selpercatinib in Patients With RET Fusion-Positive Solid Tumours Other Than Lung or Thyroid Tumours (LIBRETTO-001)Document13 pagesTumour-Agnostic Efficacy and Safety of Selpercatinib in Patients With RET Fusion-Positive Solid Tumours Other Than Lung or Thyroid Tumours (LIBRETTO-001)Milan JovicNo ratings yet
- KavanaughDocument11 pagesKavanaughluis moralesNo ratings yet
- Guselkumab in Patients With Active PsA Who Were Biologic-naive or Had Previously Received TNFα DISCOVER-1Document11 pagesGuselkumab in Patients With Active PsA Who Were Biologic-naive or Had Previously Received TNFα DISCOVER-1Edmundo RomanoNo ratings yet
- Enteral Feedings in Hospitalized Patients: Early Versus Delayed Enteral NutritionDocument7 pagesEnteral Feedings in Hospitalized Patients: Early Versus Delayed Enteral NutritionokipashaNo ratings yet
- Adenoma y CA GastricoDocument8 pagesAdenoma y CA GastricoJhon Jaime CarvajalNo ratings yet
- Efficacy and Safety of Abatacept in Lupus Nephritis: A Twelve-Month, Randomized, Double-Blind StudyDocument11 pagesEfficacy and Safety of Abatacept in Lupus Nephritis: A Twelve-Month, Randomized, Double-Blind StudyAndreea AdaNo ratings yet
- Clinical-Liver, Pancreas, and Biliary TractDocument8 pagesClinical-Liver, Pancreas, and Biliary TractKirsten HartmanNo ratings yet
- Palliative Stenting With or Without Radiotherapy For Inoperable Esophageal CarcinomaDocument7 pagesPalliative Stenting With or Without Radiotherapy For Inoperable Esophageal CarcinomaBella StevannyNo ratings yet
- 467 2020 Article 4774Document10 pages467 2020 Article 4774javifarez1No ratings yet
- Ne en WhippleDocument9 pagesNe en WhippleOscar VillacresNo ratings yet
- ContentServer 8Document7 pagesContentServer 8Fitra PahlevyNo ratings yet
- Clinical NutritionDocument12 pagesClinical NutritionBagus Candra BuanaNo ratings yet
- A Prospective Randomized Controlled Trial On The Value of Prophylactic Supplementation Pral NutritionDocument7 pagesA Prospective Randomized Controlled Trial On The Value of Prophylactic Supplementation Pral NutritionOkky IrawanNo ratings yet
- Paper 26Document4 pagesPaper 26fundj22No ratings yet
- Iihyuyu6756e54tw5w3553w5et6yfug5757 Jgut75Document6 pagesIihyuyu6756e54tw5w3553w5et6yfug5757 Jgut75RIBNo ratings yet
- 01 HepatogastroDocument3 pages01 Hepatogastroyacine26No ratings yet
- Jon Ker 2018Document8 pagesJon Ker 2018WilliamYañezRojasNo ratings yet
- A Randomized Controlled Trial of Probiotics For Clostridium Dif Cile Infection in AdultsDocument4 pagesA Randomized Controlled Trial of Probiotics For Clostridium Dif Cile Infection in Adults林新中No ratings yet
- 10 1016@j Ejogrb 2015 09 020Document5 pages10 1016@j Ejogrb 2015 09 020samuel tapia pardoNo ratings yet
- PIIS014067361261900XDocument10 pagesPIIS014067361261900X呂鍇東No ratings yet
- Timing of Oral Intake After Esophagectomy A Narrative Review ofDocument19 pagesTiming of Oral Intake After Esophagectomy A Narrative Review ofAna RosiNo ratings yet
- Top Trials in Gastroenterology & HepatologyFrom EverandTop Trials in Gastroenterology & HepatologyRating: 4.5 out of 5 stars4.5/5 (7)
- 9 ErDocument13 pages9 Ermartin Ignacio Zapata LaguadoNo ratings yet
- Essah 2011Document6 pagesEssah 2011ThormmmNo ratings yet
- Tele The Ruthr AbotuDocument5 pagesTele The Ruthr AbotukhanjanNo ratings yet
- Effects of Specific Nutrients On Immune Modulation in PatientsDocument7 pagesEffects of Specific Nutrients On Immune Modulation in Patientsusuario101122No ratings yet
- Enteral Nutrition in The Critically Ill Marik PDFDocument8 pagesEnteral Nutrition in The Critically Ill Marik PDFCami Cuevas VergaraNo ratings yet
- Oral Vancomycin Induces and Maintains Remission of Ulcerative Colitis in The Subset of Patients With Associated Primary Sclerosing Cholangitis PDFDocument2 pagesOral Vancomycin Induces and Maintains Remission of Ulcerative Colitis in The Subset of Patients With Associated Primary Sclerosing Cholangitis PDFAnonymous tlsoBJiNo ratings yet
- Trastuzumab Deruxtecan (DS-8201a) in Patients With Advanced HER2-positive Gastric Cancer: A Dose-Expansion, Phase 1 StudyDocument10 pagesTrastuzumab Deruxtecan (DS-8201a) in Patients With Advanced HER2-positive Gastric Cancer: A Dose-Expansion, Phase 1 Studybawoji1763No ratings yet
- EchografyDocument6 pagesEchografyMiha ElaNo ratings yet
- 1 s2.0 S0140673623009662 MainDocument14 pages1 s2.0 S0140673623009662 MainKesia MaldonadoNo ratings yet
- Critical Apprisal of A Prospective StudyDocument7 pagesCritical Apprisal of A Prospective StudyVK LabasanNo ratings yet
- Pi Is 0016508520300184Document12 pagesPi Is 0016508520300184ntnquynhproNo ratings yet
- 65 Stenoza GDDDocument7 pages65 Stenoza GDDGabriela MilitaruNo ratings yet
- Mbizzarri,+9 1 Case Fish+Protein ProiettiDocument10 pagesMbizzarri,+9 1 Case Fish+Protein ProiettibaliardoforcaNo ratings yet
- Preoperative Nutritional Support in Cancer Patients With No Clinical Signs of Malnutrition - Prospective Randomized Controlled TrialDocument6 pagesPreoperative Nutritional Support in Cancer Patients With No Clinical Signs of Malnutrition - Prospective Randomized Controlled TrialtttttNo ratings yet
- 11 JCO-2005-Ravasco-1431-8Document8 pages11 JCO-2005-Ravasco-1431-8Samuel Kyei-BoatengNo ratings yet
- Digestive PDFDocument10 pagesDigestive PDFRahmat AgungNo ratings yet
- Intestinal Ultrasound Detects An Increased Diameter and Submucosal Layer Thickness in The Appendix of Patients With Ulcerative Colitis Compared To Healthy Controls - A Prospective Cohort StudyDocument9 pagesIntestinal Ultrasound Detects An Increased Diameter and Submucosal Layer Thickness in The Appendix of Patients With Ulcerative Colitis Compared To Healthy Controls - A Prospective Cohort StudyСергей СадовниковNo ratings yet
- PIIS2405456922002619Document7 pagesPIIS2405456922002619Oriol Colet GuitertNo ratings yet
- Sucralfate Therapy in NSAID Bleeding Gastropathy: Background & Aims: A Randomized, Double-Blind, PlaceDocument6 pagesSucralfate Therapy in NSAID Bleeding Gastropathy: Background & Aims: A Randomized, Double-Blind, PlaceDewi nur thohidahNo ratings yet
- 15 Original ArticleDocument4 pages15 Original ArticleNayan ChaudhariNo ratings yet
- Fonc 11 693386Document9 pagesFonc 11 693386Luana FerreiraNo ratings yet
- Fecal Calprotectin and Lactoferrin As Predictors of Relapse in Patients With Quiescent Ulcerative Colitis During Maintenance TherapyDocument7 pagesFecal Calprotectin and Lactoferrin As Predictors of Relapse in Patients With Quiescent Ulcerative Colitis During Maintenance TherapyLuis Gerardo Alcalá GonzálezNo ratings yet
- Magic TrailDocument10 pagesMagic Trailchootu509No ratings yet
- 5 NGTDocument9 pages5 NGTPipit PitalokaNo ratings yet
- CreonDocument12 pagesCreonNikola StojsicNo ratings yet
- ACG Clinical Guideline: Management of Acute PancreatitisDocument8 pagesACG Clinical Guideline: Management of Acute PancreatitisNick ANo ratings yet
- Song 2018Document7 pagesSong 2018Jonathan RyanNo ratings yet
- Jo Howard Long TermDocument11 pagesJo Howard Long TermKuliah Semester 4No ratings yet
- Effect of Antibiotic Prophylaxis On Acute Necrotizing Pancreatitis: Results of A Randomized Controlled TrialDocument7 pagesEffect of Antibiotic Prophylaxis On Acute Necrotizing Pancreatitis: Results of A Randomized Controlled TrialKirsten HartmanNo ratings yet
- Pharmacokinetic & Pharmacodynamic AbbreviationsDocument2 pagesPharmacokinetic & Pharmacodynamic Abbreviationspharmacysmile8049No ratings yet
- Drug Therapy MonitoringDocument48 pagesDrug Therapy MonitoringPooja agarwalNo ratings yet
- Myasthenia Gravis, Megacolon and Narrow Angle Glaucoma, Hypersensitivity To HNBB and Other Components of The ProductDocument3 pagesMyasthenia Gravis, Megacolon and Narrow Angle Glaucoma, Hypersensitivity To HNBB and Other Components of The ProductGwyn RosalesNo ratings yet
- Laporan Stock OpnameDocument138 pagesLaporan Stock OpnameAnggunia DeaNo ratings yet
- Color Code Anesthesia PDFDocument6 pagesColor Code Anesthesia PDFYusnia Gulfa MaharaniNo ratings yet
- Adrenocortical SteroidsDocument10 pagesAdrenocortical SteroidsAyu Laisitawati FirlafinzaNo ratings yet
- Ophthalmic Drug Delivery SystemsDocument749 pagesOphthalmic Drug Delivery Systemskulbhushan singh100% (2)
- Sedative HypnoticsDocument70 pagesSedative Hypnoticshystexi caaaleNo ratings yet
- Obat - Obat Tertentu: Dextromethorphan HBRDocument2 pagesObat - Obat Tertentu: Dextromethorphan HBRgo3nawanNo ratings yet
- Pengadaan Obat 22 Mei 2021Document209 pagesPengadaan Obat 22 Mei 2021Aristha Novyra PutriNo ratings yet
- Equations Sheet - v2Document9 pagesEquations Sheet - v2angelamnsr100% (1)
- PF 2002 Vol 28 Issues 1 3Document1,166 pagesPF 2002 Vol 28 Issues 1 3Alexandra EnacheNo ratings yet
- Adult Critical Care IV Medication Infusion Sheet PDFDocument2 pagesAdult Critical Care IV Medication Infusion Sheet PDFihtisham1No ratings yet
- CRO and Sponsor - Integrated Application FormDocument42 pagesCRO and Sponsor - Integrated Application FormVillaruelJasperNo ratings yet
- 17 Etest-Pricing v16 PDFDocument2 pages17 Etest-Pricing v16 PDFRapBoy TrinhNo ratings yet
- No Nama Barang Total TuslahDocument11 pagesNo Nama Barang Total TuslahPenunjang Medis Rs PMCNo ratings yet
- For NursingDocument13 pagesFor NursingAmparo VillamilNo ratings yet
- The Chemistry of PoppiesDocument1 pageThe Chemistry of PoppiesShruti SinghalNo ratings yet
- Clinical Pharmacy Book ReviewDocument4 pagesClinical Pharmacy Book Reviewsaman7752No ratings yet
- Tufts Pharmacology Flashcards - QuizletDocument66 pagesTufts Pharmacology Flashcards - QuizletDENTAL REVIEWER ONLYNo ratings yet
- Daftar Obat Yang Di Pesan: NO Nama Obat Jumlah HargaDocument4 pagesDaftar Obat Yang Di Pesan: NO Nama Obat Jumlah HargaalmuliasyahNo ratings yet
- Biowaiver Monographs For Immediate-Release Solid Oral Dosage Forms: KetoprofenDocument11 pagesBiowaiver Monographs For Immediate-Release Solid Oral Dosage Forms: KetoprofendyanNo ratings yet
- Directory NPADocument1,934 pagesDirectory NPAAnonymous qWY12CYlmNo ratings yet
- Lesson Plan in Consumer ChemDocument5 pagesLesson Plan in Consumer ChemJessie M. Indolos0% (1)
- Kampar Creditor Update 31.07.2021Document5,271 pagesKampar Creditor Update 31.07.2021gracious pharmacy 2No ratings yet
- Cisplatin Etoposide (Intravenous)Document7 pagesCisplatin Etoposide (Intravenous)Nurul Kamilah SadliNo ratings yet
- Spesialit Obat Vitamin & Mineral-1Document36 pagesSpesialit Obat Vitamin & Mineral-1yuni panda100% (1)
- Drugs Society and Human Behavior 18Th Edition Carl L Hart Full ChapterDocument67 pagesDrugs Society and Human Behavior 18Th Edition Carl L Hart Full Chapterebony.blanchard211100% (9)
- Drugs Used To Treat Substance Use DIsordersDocument21 pagesDrugs Used To Treat Substance Use DIsordersYsa LuisNo ratings yet
- Adobe Scan 20 Dec 2023Document1 pageAdobe Scan 20 Dec 2023Sculeac EvelinaNo ratings yet