Professional Documents
Culture Documents
Farlow - Treatment Options
Uploaded by
aruesjasOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Farlow - Treatment Options
Uploaded by
aruesjasCopyright:
Available Formats
Review Article
Dement Geriatr Cogn Disord 2008;25:408–422 Accepted: October 10, 2007
Published online: April 3, 2008
DOI: 10.1159/000122962
Treatment Options in Alzheimer’s Disease:
Maximizing Benefit, Managing Expectations
Martin R. Farlow a Michael L. Miller b Vojislav Pejovic b
a Indiana University School of Medicine, Indianapolis, Ind., and b Prescott Medical Communications Group,
Chicago, Ill., USA
Key Words Introduction
Alzheimer’s disease ⴢ Cholinesterase inhibitors ⴢ
Memantine ⴢ Pharmacotherapy ⴢ Combination therapy ⴢ Alzheimer’s disease (AD) is the most common cause
Antioxidants ⴢ Ginkgo biloba of dementia in the elderly, affecting approximately 4.5
million people in the United States alone [1]. As the inci-
dence of AD in the United States and Europe is expected
Abstract to double by the year 2050 [2, 3], developing successful
Alzheimer’s disease (AD) is becoming an increasingly heavy treatments to this complex disease is becoming an ever-
burden on the society of developed countries, and physi- increasing priority.
cians now face the challenge of providing efficient treatment Approved treatments for AD – the cholinesterase in-
regimens to an ever-higher number of individuals affected hibitors (ChEIs) and the N-methyl-D-aspartate (NMDA)
by the disease. Currently approved anti-AD therapies – the receptor antagonist memantine – offer some symptom-
cholinesterase inhibitors and the N-methyl-D -aspartate re- atic relief by targeting the cholinergic and glutamatergic
ceptor antagonist memantine – offer modest symptomatic neurotransmitter systems, respectively [4–9]. Other ther-
relief, which can be enhanced using combination therapy apies, such as statins, vitamin E, Ginkgo biloba extracts,
with both classes of drugs. Additionally, alternative therapies cognitive therapy, and psychological treatments have also
such as nonsteroidal anti-inflammatory drugs, vitamin E, been investigated clinically. Given the relatively limited
selegiline, Ginkgo biloba extracts, estrogens, and statins, as arsenal of currently approved anti-dementia drugs, it is
well as behavioral and lifestyle changes, have been explored vital for physicians to make the best use of available op-
as therapeutic options. Until a therapy is developed that can tions and, when appropriate, combine treatments in or-
prevent or reverse the disease, the optimal goal for effective der to maximize benefit for the patient.
AD management is to develop a treatment regimen that will
yield maximum benefits for individual patients across mul-
tiple domains, including cognition, daily functioning, and Dr. Martin Farlow receives grants from Eli Lilly & Co., Novartis, Ono/
behavior, and to provide realistic expectations for patients Pharmanet, Pfizer, Elan Pharm. He also is consultant for Abbott, Ac-
and caregivers throughout the course of the disease. This re- cera, Adamas, Cephalon Inc., Eisai Pharm, GlaxoSmithKline, Mediva-
view provides a basic overview of approved AD therapies, tion, Memory Pharm., Merck Res. Labs., Neurochem, Novartis, Oc-
discusses some pharmacologic and nonpharmacologic tapharma, Takeda, Toyama, Worldwide Clinical Trials and received
honoraria from Eisai, Forest, Novartis, Pfizer as a member of Speak-
treatment strategies that are currently being investigated, ers’ Bureau.
and offers suggestions for optimizing treatment to fit the Drs. Michael Miller and Vojislav Pejovic work for Prescott Medical
needs of individual patients. Copyright © 2008 S. Karger AG, Basel Communications Group, a contractor of Forest Laboratories, Inc.
© 2008 S. Karger AG, Basel Martin R. Farlow, MD
Department of Neurology, CL 291, Indiana University School of Medicine
Fax +41 61 306 12 34 541 Clinical Drive
E-Mail karger@karger.ch Accessible online at: Indianapolis, IN 46202-5111 (USA)
www.karger.com www.karger.com/dem Tel. +1 317 274 2893, Fax +1 317 274 5873, E-Mail mfarlow@iupui.edu
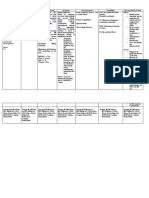
Table 1. Currently approved medications for the treatment of AD [10, 19, 27, 28, 32]
Second-generation ChEIs NMDAR
antagonist
donepezil rivastigmine galantamine memantine
oral transdermal
Dosing once daily twice daily once daily twice or once dailya twice daily
Starting 5 mg/day 3.0 mg/day 4.6 mg/day 8 mg/day 5 mg/day
Maximum 10 mg/day 12 mg/day 9.5 mg/day 24 mg/day 20 mg/day
Titration interval 4 weeks minimum 4 weeks recommended 4 weeks minimum 4 weeks minimum 1-week intervals
Recommended doses 5 and 10 mg/day 6–12 mg/day 9.5 mg/day 16–24 mg/day 20 mg/day
Peak plasma concentration, h 3–5 0.8–1.7 8–16 0.5–1.5 3–7
Effect of food on drug absorption none delays rate and none delays rate but not none
extent of absorption extent of absorption
Hepatic metabolism CYP 2D6 non-hepatic non-hepatic CYP 2D6 primarily
CYP 3A4 CYP 3A4 non-hepatic
Elimination half-life, h ⬃70 1.5 3.4 5–7 60–80
Drug–drug interactions yes none known none known yes none known
See prescribing information for complete details. a See text.
In this review, we discuss approved and investigation- Donepezil (Aricept쏐, Eisai; Pfizer, Inc.) has a long
al treatments for AD, methods for maximizing clinical half-life (approximately 70 h), which allows for once-dai-
benefits, and strategies to effectively manage patient and ly dosing and can be administered in the form of an oral-
caregiver expectations. ly disintegrating tablet [6, 7, 10]. Evidence suggests that
donepezil, in addition to providing cognitive and global
benefits, may be moderately effective at alleviating func-
ChEIs: The First Class of Agents Approved for the tional problems and behavioral changes such as depres-
Treatment of AD1 sion, anxiety, and apathy [6, 7]. As with other ChEIs, the
predominant side effects associated with donepezil are
The first 15 years of AD pharmacotherapy were pri- gastrointestinal (diarrhea, nausea; table 2) [10]. These
marily focused on the widespread degeneration of acetyl- symptoms are most severe during dose escalation, but
choline (ACh)-containing neurons in the brains of affect- may continue during maintenance therapy. Other re-
ed patients. ChEIs were developed with the idea of inhib- ported side effects include anorexia, headaches, muscle
iting acetylcholinesterase (AChE), thereby enhancing cramps, fatigue, syncope, sleep disturbances, and uri-
cholinergic neurotransmission. Tacrine (Cognex쏐, War- nary incontinence [7, 10, 11]. Donepezil is metabolized in
ner-Lambert), the first ChEI approved by the US Food the liver, but a portion of it (17%) is excreted unchanged
and Drug Administration (FDA) for the treatment of in the urine [10, 12]. The 5-mg dose can be given safely to
mild-to-moderate AD, is no longer prescribed due to patients with mild-to-moderate hepatic and renal im-
problems with tolerability and hepatotoxicity. Three sec- pairment [13].
ond-generation ChEIs have been approved by the FDA Rivastigmine (Exelon쏐, Novartis Pharmaceuticals) [6,
for mild-to-moderate AD, with one (donepezil) recently 7, 14] selectively inhibits AChE in the central nervous sys-
receiving approval for the treatment of severe AD. All of tem, and also inhibits butyrylcholinesterase [7, 15]. It has
the ChEIs provide modest but significant improvements been speculated that this additional mechanism may be-
in cognition and global patient functioning and, in spite come important in advanced AD as AChE levels decline
of having different pharmacological profiles (table 1), are [16, 17], but recent measurements of butyrylcholinester-
considered to have similar efficacy [4–7]. ase activity in the synapses of patients with AD challenge
this view [18]. Rivastigmine has a very short half-life in
1
plasma and cerebrospinal fluid (1–2 h), thus requiring
A thorough review of the efficacy data for the ChEIs and memantine is
outside the scope of this article. For complete Phase III registration trials twice-daily dosing [19–21]. Statistically significant bene-
for these drugs, please refer to references 38–40, 54, 176–183. fits of rivastigmine have been observed for cognition,
AD Treatment Options Dement Geriatr Cogn Disord 2008;25:408–422 409
Table 2. Adverse events1 associated with the use of ChEIs and memantine in patients with AD* [10, 19, 27, 28, 32]
Adverse events1 Donepezil Rivastigmine Galantamine Memantine
mild to severe AD oral transdermal
moderate AD
placebo drug placebo drug placebo drug placebo capsule2 patch2 placebo drug placebo drug
355 747 392 501 868 1,189 302 294 291 801 1,040 922 940
Abdominal pain – – – – 6 13 – – – 4 5 – –
Accident 6 7 12 13 9 10 – – – – – – –
Anorexia – – 4 8 3 17 2 9 3 3 9 – –
Anxiety – – – – 3 5 – – – – – – –
Asthenia – – – – 2 6 1 6 2 – – – –
Confusion – – – – 7 8 – – – – – 5 6
Constipation – – – – 4 5 – – – – – 3 5
Depression – – – – 4 6 – – – 5 7 – –
Diarrhea 5 10 4 10 11 19 3 5 6 7 9 – –
Dizziness 6 8 – – 11 21 2 7 2 6 9 5 7
Dyspepsia – – – – 4 9 – – – 2 5 – –
Ecchymosis – – 2 5 – – – – – – – – –
Fatigue 3 5 – – 5 9 – – – 3 5 – –
Headache 9 10 – – 12 17 2 6 3 5 8 3 6
Infection – – 9 11 – – – – – – – – –
Insomnia 6 9 4 5 7 9 – – – 4 5 – –
Malaise – – – – 2 5 – – – – – – –
Muscle cramps 2 6 – – – – – – – – – – –
Nausea 6 11 2 6 12 47 5 23 7 9 24 – –
Pain 8 9 – – – – – – – – – – –
Somnolence – – – – 3 5 – – – – – – –
Urinary tract infection – – – – 6 7 – – – 7 8 – –
Vomiting 3 5 4 8 6 31 3 17 6 4 13 – –
Weight decrease – – – – – – 1 5 3 2 7 – –
* Information taken from Prescribing Information for each drug. 1 Adverse events reported in at least 5% of patients receiving drug
and at a higher frequency than placebo-treated patients (the 10 most frequently occurring adverse events for each drug are indicated
in bold). 2 Capsule: 6 mg/day; patch: 9.5 mg/day.
global function, and activities of daily living (ADLs) [22], metabolism is almost completely (97%) nonhepatic (pri-
and the drug also may improve attention focusing [7]. marily occurring through cholinesterase-mediated hy-
Moreover, a recent study has demonstrated that treatment drolysis) [14], so possibilities of metabolic drug–drug in-
with rivastigmine may delay the onset of behavioral symp- teractions are minimal. In July 2007, the FDA approved a
toms and thus reduce the risk of initiating therapy with transdermal patch delivery system for rivastigmine, which
an antipsychotic [23]. The side effect profile for rivastig- demonstrated similar efficacy but better tolerability than
mine varies with dosing; in clinical trials designed to the oral preparation in a clinical trial [26, 27].
achieve the maximum tolerated dose, up to 50% of indi- Galantamine (RazadyneTM, previously Reminyl쏐, Or-
viduals in higher-dose groups experienced cholinomi- tho-McNeil) [6, 7, 28], in addition to inhibiting AChE,
metic side effects [24]. As with other ChEIs, gastrointesti- allosterically binds nicotinic ACh receptors, thereby
nal side effects associated with rivastigmine are common modulating the effects of ACh [29]. While binding nico-
(vomiting, nausea, diarrhea, anorexia, abdominal pain; tinic ACh receptors could influence neuronal processes,
table 2), but some can be circumvented using a slower the clinical benefit of this mechanism has not been estab-
dose-titration scheme, upwardly titrating monthly rather lished. Traditional dosing is twice daily, and an extended
than every 2 weeks [25]. Other notable side effects include release daily formulation is now available, allowing once
dizziness, headache, and fatigue (table 2). Rivastigmine daily dosing. Galantamine has been shown to provide
410 Dement Geriatr Cogn Disord 2008;25:408–422 Farlow /Miller /Pejovic
some stabilization on measures of global functioning, events are rare. The most commonly reported adverse
cognition, behavior, and ADLs [30], although studies in- events that occur more frequently with memantine than
vestigating its effects on behavior and ADLs have pro- placebo include dizziness, headache, confusion, and con-
duced inconsistent results [30]. Approximately 30% of stipation (table 2) [32]. Memantine is primarily excreted
galantamine is excreted unchanged in urine, whereas the unchanged in urine (48%) [32], although in vitro evi-
rest is metabolized by hepatic enzymes [31]. Dose reduc- dence suggests the possibility of hepatic metabolism as
tion is recommended in patients with moderately im- well [43]. No metabolic interactions with other drugs
paired hepatic or renal function [28]. The most common- have been observed with memantine [32] (table 1). Medi-
ly reported adverse events include nausea, vomiting, cations that alkalize urine may reduce the renal elimina-
diarrhea, anorexia, and dizziness (table 2) [28]. Other re- tion of memantine, and dose reductions are recommend-
ported side effects include depression, headache, and ed for patients with severe renal impairment [32, 44].
weight decrease (table 2). In July 2005, the commercial
name of galantamine was changed from Reminyl to Raza-
dyne, in an effort to avoid confusion and dispensing er- Other Therapeutic Options in AD
rors with the diabetes treatment, Amaryl.
While the ChEIs and memantine have been designed to
affect specific aspects of chemical neurotransmission, oth-
NMDA Receptor Antagonists: The Second Class of er therapies seek to target biochemical stressors, such as
Agents Approved for the Treatment of AD inflammation, oxidation, and the disruption of hormonal
processes, all of which have been implicated in the neuro-
Memantine (Namenda쏐, Forest Laboratories, Inc.) nal loss observed in AD [8]. Some of the many therapies
[32], the first compound approved for patients in the investigated for their potential to prevent the onset, delay
moderate-to-severe stages of AD, is a moderate-affinity, progression, or reverse AD include anti-inflammatory
uncompetitive antagonist of the NMDA receptors drugs, antioxidants, selegiline, G. biloba, estrogen replace-
(NMDARs). Glutamatergic dysfunction can lead to an ex- ment, statins, and compounds designed to inhibit amyloid
cessive influx of calcium ions through NMDARs, leading and tau neuropathology. Currently, efficacy data for each
to neuronal death through mechanisms that are not clear- of these are either largely negative or inconclusive (most
ly understood [33]. Such ‘excitotoxicity’ has been impli- studies of compounds designed to inhibit amyloid or tau
cated in AD [34]. The pharmacological properties of me- neuropathology are preliminary or still in progress).
mantine are believed to prevent NMDAR-mediated exci- It has been hypothesized that inflammation, likely
totoxicity, while permitting normal synaptic activity [35]. caused (at least in part) by amyloid plaques, contributes
The half-life of memantine in plasma is approximately 70 to neuronal damage and eventual loss of synaptic func-
h, which theoretically allows for once-daily dosing; how- tion [45, 46]. Epidemiological studies have demonstrated
ever, the manufacturer, following established procedures, a lower incidence of AD in patients regularly using non-
recommends two daily doses of 10 mg each [32]. steroidal anti-inflammatory drugs (NSAIDs), suggesting
Memantine treatment of patients with moderate-to- that NSAID use may be protective against AD [47]. How-
severe AD has been shown to confer significant benefits ever, prospective trials evaluating NSAID use did not re-
on cognition, ADLs, global outcomes, and behavior (par- veal a symptomatic benefit in patients with AD [48, 49]
ticularly agitation and aggression) when administrated or mild cognitive impairment (MCI) [50, 51], and a trial
either alone or in patients already receiving donepezil [9, investigating a potential preventative role for naproxen
36–40]. Memantine has also been investigated in patients and celecoxib was halted due to concerns over cardiovas-
with mild-to-moderate AD, demonstrating significant cular risks [52].
results on cognition, behavior, and global status in one Another alternative approach involves protection
trial [41]; however, the FDA recently denied approval for against cellular damage caused by oxidative stressors. As
this indication as other trials suggest that memantine markers of oxidative injury are evident in postmortem
may not be efficacious at this stage of the disease [9, 42]. brain tissue of patients with AD [53, 54], it has been sug-
Memantine is safe and well tolerated, and trial discon- gested that oxidative processes are involved in the disease
tinuation rates due to adverse events in memantine-treat- pathogenesis. Antioxidants that have been investigated for
ed patients are comparable to those in placebo groups their potential to reduce the risk of AD include vitamins
[32]. In contrast to the ChEIs, gastrointestinal adverse A, C, and E, coenzyme Q, and selenium [8, 55, 56]. Clinical
AD Treatment Options Dement Geriatr Cogn Disord 2008;25:408–422 411
trials with vitamin E have produced the most consistent Observational studies have revealed a lower incidence
results, suggesting that it may be the most promising anti- of AD in postmenopausal women taking estrogen, sug-
oxidant for delaying the onset or slowing the progression gesting that estrogen may have a protective role in AD
of AD [57, 58]. As a result of these findings, AD treatment [71]. However, recent studies indicate that the combina-
guidelines issued by the American Academy of Neurology tion of estrogen and progestin, or estrogen alone, may in
in 2001 advised considering vitamin E as an adjunctive fact increase the risk for dementia and adversely effect
treatment [24]. However, in a more recently published cognition [72, 73]. Estrogen supplementation has also
large, double-blind, placebo-controlled trial in patients been linked to an increased risk of stroke, cancer, and
with MCI, no advantage for vitamin E over placebo re- other health problems [71, 74, 75]. Consequently, the
garding rate of cognitive decline or disease progression Women’s Health Initiative concluded in 2003 that the
was seen during the 3-year course of the study [59]. Since risks accompanying estrogen-progestin replacement
recent evidence also suggests that high doses of vitamin E therapy outweigh the potential benefits [72]. However, it
(6400 IU/day) may be associated with higher all-cause should be noted that data from a smaller subsequent trial
mortality rates [60], a more comprehensive clinical evalu- suggest that the timing of HRT in respect to the onset of
ation is required before the risk-benefits ratio of vitamin E menopause may be critical: early HRT initiation was as-
supplementation in AD can be determined. sociated with cognitive benefits compared to later initia-
A small number of clinical trials have also indicated tion, whereas later initiation was associated with cogni-
that selegiline, a monoamine oxidase B inhibitor with an- tive decline on the MMSE compared to participants who
tioxidant properties used for treating patients with Par- did not use HRT [76]. While debate continues over other
kinson’s disease [61], may be useful for the treatment of potential benefits of hormone replacement therapy, it is
AD. In a long-term clinical trial, selegiline-treated pa- not currently recommended specifically for the preven-
tients demonstrated significant improvement on the tion or treatment of AD.
Clock Draw Test and on the Mini-Mental Status Exami- Epidemiological evidence has also revealed a decreased
nation (MMSE) [62]. Clinical trial results have also indi- incidence of AD in patients taking the cholesterol-lower-
cated that treatment of AD with either selegiline, vitamin ing drugs known as statins [77], thereby prompting in-
E or both may slow the progression of the disease [58]; vestigation of their utility as an AD therapy [78]. A small
however, a recent Cochrane meta-analysis of 17 trials of prospective, double-blind, placebo-controlled trial of
selegiline for AD found very few significant treatment ef- simvastatin in AD demonstrated a reduced level of -
fects and recommended that no further studies need to amyloid in the cerebrospinal fluid of patients with mild,
be conducted [63]. but not moderate AD [79]. A similar trial found that pa-
G. biloba extract, a popular herbal medication, is wide- tients with AD treated with atorvastatin performed sig-
ly used for its potential cognitive and neuroprotective ef- nificantly better than placebo-treated patients on a mea-
fects [64]. It has also been associated with antioxidant sure of cognition at 6 months (but not 12 months) [80].
properties and inhibition of platelet-activating factor [65]. Despite these results, it is not recommended that statins
While ginkgo has been promoted as a memory enhancer be used specifically for AD treatment. It has been sug-
for a number of years, its efficacy in patients with AD has gested that patients with AD may be overly susceptible to
not been validated by consistent data [66]. Several clinical adverse effects of statins due to pre-existing alterations in
studies have revealed a potential benefit of ginkgo for signal transduction and energy metabolism [81], although
treatment of patients with AD [66–68]; however, a recent this has not been clinically verified. Future studies are
randomized, double-blind, placebo-controlled trial in- expected to clarify the role of cholesterol and cholesterol-
volving 513 patients did not demonstrate significant ef- processing pathways on AD progression and to ascertain
ficacy over placebo [69]. An ongoing prevention trial whether the putative effects of statins in AD are related
aimed at evaluating the potential effect of ginkgo on de- to their lipid-lowering properties. Regardless of age or
laying progression to AD may reveal its utility in prodro- risk of dementia, all individuals are advised to maintain
mal stages of dementia (ClinicalTrials.gov Identifier: cholesterol within recommended levels.
NCT00010803; scheduled completion date: July 2009). Many studies are underway to investigate biochemical
G. biloba extract is generally well-tolerated: previous con- and immunological methods for blocking one or more of
cerns regarding risk of hemorrhage due to inhibition of the steps involved in amyloid and neurofibrillary pathol-
platelet-activating factor [70] have proven to be un- ogy. Such therapeutic approaches may ultimately lead to
founded [69]. additional ways of deterring, preventing, or altering the
412 Dement Geriatr Cogn Disord 2008;25:408–422 Farlow /Miller /Pejovic
progression of AD; however, they will be required to un- sibility is realized, it is important that practicing physi-
dergo rigorous preclinical and clinical evaluation before cians optimize available symptomatic therapies in order
being approved by the FDA. Most of those approaches are to provide the best possible treatment regimen. Clinical
in relatively early stages of development, and it is unlikely issues that may influence the effectiveness of therapy in-
that they will be available for at least a few more years. clude early and efficient diagnosis, behavioral or lifestyle
modifications, patient compliance, and sequential or
Nonpharmacological Approaches combinatorial therapeutic approaches with available
In addition to pharmacological approaches to AD, a drugs.
number of nonpharmacological methods have also been
investigated. Although many of these studies have been Early and Efficient Diagnosis
poorly controlled and not subjected to the same rigorous Pathological changes and neuronal degeneration in
criteria as trials of pharmaceutical agents [82], recent ev- AD begin many years before a clinical diagnosis can be
idence suggests that there may be a role for various types made [88–91]. Since such changes are likely cumulative,
of cognitive training and psychological intervention in diagnosis and intervention at an early, preclinical stage of
the treatment of AD. A meta-analysis [83] showed that the disease can be of paramount importance in preserv-
various cognitive therapy methods may improve or slow ing cognitive function [92].
the rate of decline of cognitive and functional abilities in The first signs of cognitive complaints can indicate a
patients with AD, and that restorative strategies, which syndrome called mild cognitive impairment (MCI) [93,
are designed to restore functioning through repeated 94], which is defined as a ‘cognitive decline greater than
cognitive challenges, are typically more effective than that expected for an individual’s age and education level
compensatory strategies designed to ‘work around’ cog- but that does not interfere notably with activities of daily
nitive deficits [83]. A Cochrane meta-analysis of trials us- life’ [95]. The significance of MCI is well illustrated by an
ing reality orientation, in which patients are regularly observation that 80-year-old patients with MCI can be
presented with cues relating to their environment, also expected to progress to AD at a rate of 12% per year, com-
suggested potentially significant benefits for patients pared to 2% per year for control, age-matched subjects
[84]. More recently, in a trial involving untreated patients [96]. A 2003 conference dedicated to MCI resulted in a
with AD, participants undergoing regular, intensive real- diagnostic algorithm that can be used to identify four
ity orientation and cognitive stimulation demonstrated MCI subtypes [93, 94], one of which, the single-domain
better cognitive performance than the patients in the amnestic MCI (also referred to as ‘amnesic MCI’ or
control group [85]. Such gains may be maintained for sev- ‘aMCI’), is particularly associated with a high probability
eral months after the cessation of the treatment, although of conversion to AD: one study found a conversion rate
data on the persistence of such benefits are sparse [83]. to AD of approximately 49% (over 2.5 years) for patients
Furthermore, psychosocial interventions such as caregiv- with amnestic MCI, compared to approximately 27% for
er support, counseling, education, and environmental patients with nonamnestic forms [97]. The identification
modifications that minimize stressful situations for pa- of factors that best predict the conversion from MCI to
tients with AD have also been shown to minimize both AD is an area of intense research [97–101].
patient behavioral problems [86] and caregiver distress Current expert opinion recommends careful monitor-
(see below) [87]. As a caveat, it should be noted that it is ing of patients who show symptoms of amnestic MCI,
often difficult to ascertain whether the benefits of cogni- since they may have reached a prodromal stage of AD [95,
tive therapy in AD are due to the methods themselves or 102, 103]. Although standard diagnostic tools for demen-
the general stimulation of patients through regular inter- tia, such as the MMSE, may not be sensitive enough to
personal interactions with caregivers, family members, detect memory problems indicative of MCI [95], efforts
and health care professionals [83]. are being made to develop more effective diagnostic tools
[104]. In addition, corroboration and characterization of
patient memory complaints from family members or oth-
Maximizing Benefit er caregivers can help identify individuals at the highest
risk of progressing from MCI to AD [105–108]. Finally,
Ultimately, the hope for a truly revolutionary AD ther- emerging brain imaging techniques hold the promise of
apy lies in the potential of some pipeline compound to an early, accurate, and sensitive detection of the underly-
prevent or delay the onset of the disease. Until this pos- ing AD pathology [109–112], although at this point the
AD Treatment Options Dement Geriatr Cogn Disord 2008;25:408–422 413
cost-effectiveness of these tools is still a matter of conten- [127], coffee [128, 129], curry [130, 131], and fish [132–
tion [113–115]. 134] is associated with a lower risk of AD.
For individuals whose changes in cognitive, function- Activities involving complex cognitive functioning,
al, or behavioral performance indicate progression to- such as reading, participating in board games, or playing
ward AD, there are numerous standard and validated musical instruments, may also help protect against the
evaluation tools for measuring the degree of impairment development of dementia [135]. In addition, regular phys-
and monitoring progression of the disease. The MMSE ical activity has been associated with the maintenance of
and the Clock Drawing Test are most commonly used in healthy brain function, increased neuronal survival, pro-
a clinical setting; however, a recent study comparing 13 tection against neuronal injury, and a reduced risk of de-
screening instruments with an administration time of 10 mentia in cognitively normal elderly persons [136–139].
min or less suggests that the Mini-Cog, the Memory Im- Physical activity has been also associated with improved
pairment Screen, and the General Practitioner Assess- cognitive function in older adults with cognitive impair-
ment of Cognition show potential for widespread clinical ment and dementia, suggesting that exercise may con-
use due to ease of administration and interpretation, pa- tinue to provide benefits even after diagnosis [140]. A re-
tient-friendliness, sensitivity, specificity, and freedom cent review of lifestyle activities suggests that social net-
from factors such as age, education, and language [116]. working, in addition to mental and physical activity, is
A recently developed questionnaire called the St. Louis also important to maintaining cognitive health [141].
University Mental Status Examination, similar to the Therefore, patients should be encouraged to maintain or
MMSE but possibly more sensitive to MCI [117], also initiate healthy lifestyles, including a balanced diet, in-
shows promise for diagnostic purposes, although addi- creased mental and physical activities, and regular social
tional validation is required. With the standardization of contact with peers and family members.
basic clinical evaluation tools, practitioners should be Finally, since patients with AD become increasingly
able to evaluate patients more easily, potentially enabling dependent on caregiver support as the disease progresses,
earlier diagnosis, staging, and treatment initiation. To a caregiver’s own well-being constitutes an important
emphasize the importance of early and accurate diagno- goal of disease management. In a recent study of 406
sis of dementia, an international working group has re- caregivers over 18 years, nursing home placement of pa-
cently proposed new diagnostic criteria for AD that in- tients with AD was delayed by an average of 557 days in
clude neuroimaging, biomarkers, and genetic evidence families that received enhanced caregiver support [142].
[118]. Several studies have shown that many types of interven-
tion (cognitive-behavioral therapy, counseling, daycare,
Patient and Caregiver Lifestyle training of care recipient, and multicomponent interven-
Lifestyle and environmental factors such as diet, edu- tions) can be beneficial for people who care for patients
cation, and occupational complexity have all been inves- with AD [142–147]. Caregiver psychotherapy (counsel-
tigated for correlations to AD [119]. For example, a retro- ing) and psychoeducational techniques such as caregiver
spective analysis of approximately 10,000 participants of stress and anger management, depression management,
a healthcare system in California showed that an in- and programs designed to help the caregiver recognize
creased adiposity (defined as the body mass index of at and minimize stressful situations for patients, have prov-
least 25) in midlife (40–45 years of age) is associated with en particularly effective [86, 87]. Caregivers should be di-
a significantly greater risk of developing AD or vascular rected to educational and support resources, such as the
dementia, in a manner independent of comorbidities Alzheimer’s Association website (http://www.alz.org),
[120, 121]. According to a Swedish study of twins, low which contains a large amount of information about local
education represents a risk factor for dementia indepen- resources, caregiver support, and patient care. The issue
dent of genetic influences [122]. Both of these findings are of caregiver burden has been largely overlooked until re-
mirrored by another Scandinavian study, which showed cently, and deserves the increased attention of healthcare
that future dementia could be significantly predicted by policy makers and physicians alike [148].
high age, low education, hypertension, hypercholesterol-
emia, and obesity [123]. In addition, epidemiological Optimizing Pharmacotherapy: Monotherapy
studies suggest that the regular consumption of food rich Patients with AD often discontinue treatment due to
in antioxidants or -unsaturated fatty acids, such as red side effects, a lack of initial efficacy, or the loss (or per-
wine [124, 125], fruit and vegetable juices [126], green tea ceived loss) of efficacy during treatment [149]. Approxi-
414 Dement Geriatr Cogn Disord 2008;25:408–422 Farlow /Miller /Pejovic
mately 51% of patients newly treated with an AD medica- rent practice suggests that patients should not discontin-
tion discontinue therapy within 4 months of treatment ue ChEI therapy even after they progress to a more severe
initiation [150], suggesting that many patients are not re- stage [155]. Additional studies involving patients with
ceiving optimal benefits from pharmacotherapy. The side mild-to-moderate AD may also help clarify whether me-
effects associated with the use of ChEIs, which are pri- mantine can be effective in treating patients (or a subset
marily gastrointestinal (table 2), continue to provide a of patients) in earlier stages of the disease [9, 41, 42].
significant challenge to patient adherence. Some of these Despite the apparent advantages of beginning therapy
adverse effects can be minimized through a slower dos- as early in the disease process as possible, the ability of
ing scheme (titrating as slowly as every 4–6 weeks) during either the ChEIs or memantine to delay (or modify) dis-
the initial and escalation phases of treatment, or by ad- ease progression, as opposed to merely providing symp-
ministering the medication with food to retard the rapid tomatic relief, remains unproven. The clinical efficacy of
stimulation of the cholinergic system [25] (except in the ChEIs in MCI is also being tested, but neither symptom-
case of donepezil and transdermally delivered rivastig- atic nor disease-modifying effects have been established
mine, for which the rate of absorption is not affected by for the use of these drugs at such an early stage [30, 59,
food [10, 151]). Since side effects associated with meman- 156, 157]. Preclinical studies with memantine are consis-
tine use are less severe and less frequent, tolerability prob- tent with a putative neuroprotective role [158], but this
lems are not a common reason for discontinuance with has yet to be demonstrated in patients. Until more data
this medication [4, 9]. are available, practicing physicians must use their best
As each ChEI has a distinct pharmacokinetic and judgment in determining the point at which pharmaco-
pharmacodynamic profile, switching patients from one therapy is instituted, based on an individual patient’s
ChEI to another is a viable option in patients who have risks and needs.
problems with long-term efficacy or tolerability of their
initial medication [149, 152]. In several studies, approxi- Optimizing Pharmacotherapy: Combination Therapy
mately 50% of patients who previously failed to respond Combination therapy is commonly used in treating
to a ChEI demonstrated stabilization or improvement af- many other diseases, including cancer and HIV. Due to
ter switching to a different ChEI; in addition, a patient’s the complex nature of AD and the distinct mechanisms of
response to one ChEI was not predictive of response to action of the ChEIs, memantine, and alternative treat-
another [5, 149, 152]. In many cases, patients who switch ments, combination therapy may also be effective in AD.
medications are also less likely to experience cholinergic
side effects [149]. The optimal procedure for switching Co-Administration of ChEIs and Memantine
remains to be determined, although some studies and A randomized, double-blind clinical trial of meman-
guidelines suggest that the second drug may be adminis- tine was performed in 404 patients with moderate-to-se-
tered as early as one day after the first has been discon- vere AD who were already receiving stable doses of done-
tinued [149]. In cases of poor tolerability with the initial- pezil [39]. Participants who received both donepezil and
ly prescribed medication, however, a washout period is memantine showed significantly better performance
recommended until side effects resolve [149]. One guide- over those who received donepezil plus placebo in all do-
line suggests cessation of therapy for five half-lives (done- mains assessed, which included measures of cognition,
pezil, 15 days; rivastigmine/galantamine, 2 days) before function (ADLs), behavior, psychiatric disturbance, and
switching [6], although in most cases 1 week is sufficient global condition. While most adverse events in both
[153]. Dose adjustments to the initial treatment should treatment groups were mild or moderate and judged to
always be considered before switching medications, and be unrelated to either study drug, the addition of meman-
a minimum treatment period of 6 months, with realistic tine was associated with a lower incidence of several cho-
treatment expectations (see below), is recommended in linergic adverse events in this study. Participants who re-
cases where a lack of efficacy is perceived [149]. ceived both drugs had a lower frequency of diarrhea, fecal
Traditionally, patients with early-stage (mild-to-mod- incontinence, and discontinuance due to adverse events
erate) AD are prescribed ChEIs, while memantine is in- than those on donepezil alone, although the statistical
dicated for patients in moderate-to-severe stages of the significance of these differences was not addressed in this
disease. These lines are beginning to blur, however. The study [39].
recent approval of donepezil for severe AD [154] will like- Pilot combination studies have also been performed
ly lead to increased ChEI use in late-stage AD, and cur- using memantine and the other ChEIs. A European post-
AD Treatment Options Dement Geriatr Cogn Disord 2008;25:408–422 415
marketing surveillance study demonstrated that meman- results in clinical trials, it would be premature to recom-
tine is well-tolerated in combination with donepezil, riv- mend combining them with standard ChEI or meman-
astigmine, and tacrine [159]. Co-therapy of memantine tine therapy. Although these and other agents may even-
with galantamine in a 6-month prospective cross-sec- tually be deemed effective and safe for patients with AD,
tional study was well-tolerated and resulted in no cogni- additional prospective trials will be required to deter-
tive or functional deterioration during the course of mine their exact role in pharmacotherapy. However, there
treatment, according to caregiver reports [160]. Another is an increasing body of evidence that nonpharmacologi-
recent pilot study investigating the efficacy and tolerabil- cal methods may ultimately become a useful supplement
ity of memantine in patients with mild-to-moderate AD to current pharmacologic treatment. For example, a ran-
receiving stable rivastigmine treatment concluded that domized, controlled, multicenter trial of reality orienta-
the addition of memantine resulted in additional cogni- tion therapy in patients taking donepezil demonstrated
tive benefits and was safe and well-tolerated [161]. A significant improvements for patients receiving both
growing body of evidence suggests that adding meman- treatments over those receiving donepezil alone [169]. As
tine to ChEI therapy may produce additional cognitive, cognitive and behavioral methods pose little risk to pa-
functional, and global benefits, accompanied by a negli- tients and caregivers, and may provide benefits, caregiv-
gible increase in risk of adverse effects. The possibility ers should be encouraged to pursue these alternative
that memantine may also have an effect on improving the strategies if desired. However, more rigorously controlled
tolerability of ChEI treatment [39] merits further investi- long-term studies will be required to determine which of
gation in prospective trials. It should again be noted, these techniques, if any, can provide consistent benefits,
however, that memantine is currently approved for pa- and whether they should become a routine part of stan-
tients with moderate to severe AD, while rivastigmine dard therapy.
and galantamine are currently approved for patients with
mild to moderate AD.
Managing Expectations
Co-Administration of Antidementia Therapy and
Antipsychotics Unrealistic expectations of patients and caregivers can
While co-administration of ChEIs or memantine with negatively impact treatment compliance. When patients
antipsychotics and antidepressants is a standard practice inevitably continue to decline despite therapeutic inter-
for patients with behavioral disturbances in advanced vention, frustration is understandable; however, studies
stages of AD [24], the treatment of behavioral symptoms suggest that the benefits of therapy can be rapidly lost if
with atypical antipsychotics is considered off-label in ge- treatment is discontinued [170], and in most cases even
riatric patients, as these drugs are associated with an in- modest therapeutic effects provide justification for ther-
creased risk of death, falls and cerebrovascular adverse apy maintenance [155]. Open-label extension trials have
events in the elderly [162–164]. In such patients, nonphar- suggested continued benefits for up to 1 year with me-
macologic interventions should be exhausted prior to mantine [171] and for at least 3 years with each of the
prescribing drugs for these symptoms [for a review of ChEIs [172–174]. Patients and caregivers should be aware
many nonpharmacologic options, see 165]. Evidence also that current pharmacotherapy responses are less than
suggests that both memantine and the ChEIs may reduce ideal, and expectations should center on slowing decline
or prevent the emergence of behavioral symptoms in AD or delaying institutionalization rather than overall pa-
patients [37, 166, 167], which may allow patients to either tient improvement. While current treatments for AD
avert or reduce the usage of antipsychotic medications. It may lessen the symptomatic decline of the disease and
has been suggested that AD patients are particularly vul- provide an extension of independence in some cases, they
nerable to antipsychotic-induced cerebral neurotoxicity, cannot be considered disease-modifying or curative.
so diminished antipsychotic use may be of particular rel- Physicians must exercise caution when discussing treat-
evance in this patient population [168]. ments with patients and their caregivers, impressing
upon them that the benefits of current pharmacologic
Co-Administration of Traditional and treatments are rarely seen as an improvement in symp-
Nontraditional Therapies toms, but rather as an extension of patient independence.
As studies regarding the efficacy of agents such as vi- If patients and caregivers understand that a significant
tamin E and G. biloba have not yet produced consistent goal of treatment is to delay the onset of more severe
416 Dement Geriatr Cogn Disord 2008;25:408–422 Farlow /Miller /Pejovic
symptoms or long-term care placement, treatment com- first line of pharmacotherapy for mild-to-moderate AD,
pliance may improve. Providing regular reassessment ev- while memantine and donepezil are both indicated for
ery 6 months is also crucial for tracking both the progres- moderate-to-severe AD. In instances where patients do
sion of the disease and the status of the caregiver [175]. not respond or have tolerability issues with a particular
Physicians should also assist patients and caregivers ChEI, changes in dose titration or switching of ChEIs can
in recognizing that nontraditional treatments, such as be attempted. Combinations involving memantine and
ginkgo, vitamin E, and selegiline, are not yet clinically ChEIs may produce additional benefits to patients with-
validated as efficacious treatments. While some clinical out significantly increasing the risk of side effects, and
evidence supports their use, many of the double-blind future clinical trials may identify other agents that show
placebo-controlled trials to date have been negative. Con- efficacy for AD symptoms when used alone or as a part
tinuing the prescribed treatment – along with a healthy of combination therapy. In principle, therapeutic inter-
diet, exercise (if possible), and regular contact with the vention should occur early in the disease, in order to slow
physician – is the most realistic manner in which patients or prevent symptom progression for as long as possible.
can control the symptoms of their illness. Patients and caregivers must maintain reasonable ex-
pectations regarding pharmacotherapy, and resources
such as support groups and social networking can pro-
Conclusions vide relief for both patients and caregivers. Cognitive and
behavioral therapies may also play a role in improving
The availability of approved pharmacotherapies (sec- patient cognition and function, diminishing caregiver
ond-generation ChEIs and memantine) and the emer- stress, and delaying nursing home placement. As more is
gence of numerous alternative therapies have armed phy- learned about the combinatorial effects of these and oth-
sicians with more treatment options for AD compared to er potential therapeutic options at all stages of AD, the
just over a decade ago, when tacrine was the only avail- ability to significantly impact disease progression may
able therapeutic option. Although prospective trials ex- one day be realized.
amining the role of agents such as NSAIDs, selegiline or
estrogen-progestin combination in the prevention or
treatment of AD have been largely negative, potential Acknowledgments
new therapeutics for AD, including statins and agents
The authors wish to thank Ms. Annalise Nawrocki and Dr.
that combat amyloid deposition and tau hyperphosphor-
Kristen A. Andersen of Prescott Medical Communications Group
ylation, may one day be shown to provide protection for their assistance in the preparation and review of the manu-
against neurodegeneration. However, until new preven- script.
tive or disease-altering medications are approved, physi- Dr. Martin Farlow receives support from the NIH grant P30
cians must optimize the use of available pharmaceutical AG10133.
and behavioral therapies. ChEIs are still the traditional
References
1 Hebert LE, Scherr PA, Bienias JL, Bennett 4 Birks J: Cholinesterase inhibitors for Alz- 6 Cummings JL: Use of cholinesterase inhibi-
DA, Evans DA: Alzheimer disease in the US heimer’s disease. Cochrane Database Syst tors in clinical practice: evidence-based rec-
population: prevalence estimates using the Rev 2006:CD005593. ommendations. Am J Geriatr Psychiatry
2000 census. Arch Neurol 2003; 60: 1119– 5 Burns A, O’Brien J, Auriacombe S, Ballard C, 2003;11:131–145.
1122. Broich K, Bullock R, Feldman H, Ford G, 7 Farlow M: A clinical overview of cholinester-
2 Hebert LE, Beckett LA, Scherr PA, Evans Knapp M, McCaddon A, Iliffe S, Jacova C, ase inhibitors in Alzheimer’s disease. Int
DA: Annual incidence of Alzheimer disease Jones R, Lennon S, McKeith I, Orgogozo JM, Psychogeriatr 2002;14(suppl 1):93–126.
in the United States projected to the years Purandare N, Richardson M, Ritchie C, 8 Farlow MR: Utilizing combination therapy
2000 through 2050. Alzheimer Dis Assoc Thomas A, Warner J, Wilcock G, Wilkinson in the treatment of Alzheimer’s disease. Ex-
Disord 2001;15:169–173. D: Clinical practice with anti-dementia pert Rev Neurotherapeutics 2004; 4: 799–
3 Wancata J, Musalek M, Alexandrowicz R, drugs: a consensus statement from British 808.
Krautgartner M: Number of dementia suf- Association for Psychopharmacology. J Psy- 9 McShane R, Areosa Sastre A, Minakaran N:
ferers in Europe between the years 2000 and chopharmacol 2006;20:732–755. Memantine for dementia. Cochrane Data-
2050. Eur Psychiatry 2003;18:306–313. base Syst Rev 2006:CD003154.
AD Treatment Options Dement Geriatr Cogn Disord 2008;25:408–422 417
10 Aricept쏐: U.S. Prescribing Information. 27 Exelon Patch쏐: U.S. Prescribing Informa- 41 Peskind ER, Potkin SG, Pomara N, Ott BR,
New York, Pfizer, 2006. tion. East Hanover, Novartis, 2007. Graham SM, Olin JT, McDonald S, for the
11 Dunn NR: Adverse effects associated with 28 Razadyne ER: U.S. Prescribing Informa- Memantine MEM-MD-10 Study Group:
the use of donepezil in general practice in tion. Titusville, Ortho-McNeil Neurologics, Memantine treatment in mild to moderate
England. J Psychopharmacol 2000; 14: 406– 2006. Alzheimer disease: a 24-week randomized,
448. 29 Maelicke A, Albuquerque EX: Allosteric controlled trial. Am J Geriatr Psychiatry
12 Tiseo PJ, Perdomo CA, Friedhoff LT: Metab- modulation of nicotinic acetylcholine recep- 2006;14:704–715.
olism and elimination of 14C-donepezil in tors as a treatment strategy for Alzheimer’s 42 Doody RS, Tariot PN, Pfeiffer E, Olin J, Gra-
healthy volunteers: a single-dose study. Br J disease. Eur J Pharmacol 2000;393:165–170. ham SM: Meta-analysis of 6-month meman-
Clin Pharmacol 1998;46(suppl 1):19–24. 30 Loy C, Schneider L: Galantamine for Alz- tine trials in Alzheimer’s disease. Alzheimer
13 Seltzer B: Donepezil: a review. Expert Opin heimer’s disease and mild cognitive impair- Dement 2007;3:7–17.
Drug Metab Toxicol 2005;1:527–536. ment. Cochrane Database Syst Rev 2006: 43 Micuda S, Mundlova L, Anzenbacherova E,
14 Exelon: U.S. Prescribing Information. East CD001747. Anzenbacher P, Chladek J, Fuksa L, Mar-
Hanover, Novartis, 2006. 31 Mannens GS, Snel CA, Hendrickx J, Verhae- tinkova J: Inhibitory effects of memantine
15 Bullock R: The clinical benefits of rivastig- ghe T, Le Jeune L, Bode W, van Beijsterveldt on human cytochrome P450 activities: pre-
mine may reflect its dual inhibitory mode of L, Lavrijsen K, Leempoels J, Van Osselaer N, diction of in vivo drug interactions. Eur J
action: an hypothesis. Int J Clin Pract 2002; Van Peer A, Meuldermans W: The metabo- Clin Pharmacol 2004;60:583–589.
56:206–214. lism and excretion of galantamine in rats, 44 Periclou A, Ventura D, Rao N, Abramowitz
16 Giacobini E: Cholinesterase inhibitors: new dogs, and humans. Drug Metab Dispos 2002; W: Pharmacokinetic study of memantine in
roles and therapeutic alternatives. Pharma- 30:553–563. healthy and renally impaired subjects. Clin
col Res 2004;50:433–440. 32 Namenda쏐: U.S. Prescribing Information. Pharmacol Ther 2006;79:134–143.
17 Giacobini E: Cholinesterases: new roles in St. Louis, Forest Pharmaceuticals, 2006. 45 van Gool WA, Aisen PS, Eikelenboom P:
brain function and in Alzheimer’s disease. 33 Arundine M, Tymianski M: Molecular Anti-inflammatory therapy in Alzheimer’s
Neurochem Res 2003;28:515–522. mechanisms of calcium-dependent neuro- disease: is hope still alive? J Neurol 2003;250:
18 Kuhl DE, Koeppe RA, Snyder SE, Minoshi- degeneration in excitotoxicity. Cell Calcium 788–792.
ma S, Frey KA, Kilbourn MR: In vivo butyr- 2003;34:325–337. 46 McGeer PL, Rogers J, McGeer EG: Inflam-
ylcholinesterase activity is not increased in 34 Danysz W, Parsons C, Möbius HJ, Stöffler A, mation, anti-inflammatory agents and Alz-
Alzheimer’s disease synapses. Ann Neurol Quack G: Neuroprotective and symptomat- heimer disease: the last 12 years. J Alzhei-
2006;59:13–20. ological action of memantine relevant for mers Dis 2006;9:271–276.
19 Exelon쏐: U.S. Prescribing Information. East Alzheimer’s disease – a unified glutamater- 47 in t’ Veld BA, Ruitenberg A, Hofman A,
Hanover, Novartis, 2006. gic hypothesis on the mechanism of action. Launer LJ, van Duijn CM, Stijnen T, Breteler
20 Farlow MR: Update on rivastigmine. Neu- Neurotox Res 1999;2:85–97. MM, Stricker BH: Nonsteroidal antiinflam-
rologist 2003; 9:230–234. 35 Rogawski MA, Wenk GL: The neurophar- matory drugs and the risk of Alzheimer’s
21 Gobburu JV, Tammara V, Lesko L, Jhee SS, macological basis for the use of memantine disease. N Engl J Med 2001;345:1515–1521.
Sramek JJ, Cutler NR, Yuan R: Pharmacoki- in the treatment of Alzheimer’s disease. CNS 48 Zandi PP, Breitner JC: Do NSAIDs prevent
netic-pharmacodynamic modeling of riv- Drug Rev 2003;9:275–308. Alzheimer’s disease? And, if so, why? The
astigmine, a cholinesterase inhibitor, in pa- 36 Cummings JL, Schneider E, Tariot PN, Gra- epidemiological evidence. Neurobiol Aging
tients with Alzheimer’s disease. J Clin ham SM: Behavioral effects of memantine in 2001;22:811–817.
Pharmacol 2001;41:1082–1090. Alzheimer disease patients receiving done- 49 Aisen PS, Schafer KA, Grundman M, Pfeif-
22 Birks J, Grimley Evans J, Iakovidou V, Tso- pezil treatment. Neurology 2006;67:57–63. fer E, Sano M, Davis KL, Farlow MR, Jin S,
laki M: Rivastigmine for Alzheimer’s dis- 37 Gauthier S, Wirth Y, Mobius HJ: Effects of Thomas RG, Thal LJ: Effects of rofecoxib or
ease. Cochrane Database Syst Rev 2000: memantine on behavioural symptoms in naproxen vs. placebo on Alzheimer disease
CD001191. Alzheimer’s disease patients: an analysis of progression: a randomized controlled trial.
23 Suh DC, Arcona S, Thomas SK, Powers C, the Neuropsychiatric Inventory (NPI) data JAMA 2003;289:2819–2826.
Rabinowicz AL, Shin H, Mirski D: Risk of two randomised, controlled studies. Int J 50 Thal LJ, Ferris SH, Kirby L, Block GA, Lines
of antipsychotic drug use in patients with Geriatr Psychiatry 2005;20:459–464. CR, Yuen E, Assaid C, Nessly ML, Norman
Alzheimer’s disease treated with rivastig- 38 Reisberg B, Doody R, Stöffler A, Schmitt F, BA, Baranak CC, Reines SA: A randomized,
mine. Drugs Aging 2004;21:395–403. Ferris S, Möbius HJ: Memantine in moder- double-blind, study of rofecoxib in patients
24 Doody RS, Stevens JC, Beck C, Dubinsky ate-to-severe Alzheimer’s disease. N Engl J with mild cognitive impairment. Neuropsy-
RM, Kaye JA, Gwyther L, Mohs RC, Thal LJ, Med 2003;348:1333–1341. chopharmacology 2005;30:1204–1215.
Whitehouse PJ, DeKosky ST, Cummings JL: 39 Tariot PN, Farlow MR, Grossberg GT, Gra- 51 Jelic V, Kivipelto M, Winblad B: Clinical tri-
Practice parameter: management of demen- ham SM, McDonald S, Gergel I: Memantine als in mild cognitive impairment: lessons for
tia (an evidence-based review). Report of the treatment in patients with moderate to se- the future. J Neurol Neurosurg Psychiatry
Quality Standards Subcommittee of the vere Alzheimer disease already receiving 2006;77:429–438.
American Academy of Neurology. Neurolo- donepezil: a randomized controlled trial. 52 U.S. Food and Drug Administration: FDA
gy 2001;56:1154–1166. JAMA 2004;291:317–324. Issues Public Health Advisory Recommend-
25 Jann MW, Shirley KL, Small GW: Clinical 40 Winblad B, Poritis N: Memantine in severe ing Limited Use of Cox-2 Inhibitors. FDA
pharmacokinetics and pharmacodynamics dementia: results of the M-Best Study (Ben- Talk Paper, December 23. 2004;T04-61.
of cholinesterase inhibitors. Clin Pharmaco- efit and efficacy in severely demented pa- 53 Pratico D, Delanty N: Oxidative injury in
kinet 2002;41:719–739. tients during treatment with memantine). diseases of the central nervous system: focus
26 Winblad B, Cummings JL, et al: IDEAL: a 24 Int J Geriatr Psychiatry 1999;14:135–146. on Alzheimer’s disease. Am J Med 2000;109:
week placebo controlled study of the first 577–585.
transdermal patch in Alzheimer’s disease – 54 Markesbery WR, Carney JM: Oxidative al-
rivastigmine patch versus capsule; presented terations in Alzheimer’s disease. Brain
at the 10th International Congress of Alz- Pathol 1999;9:133–146.
heimer’s and Related Disorders (ICAD), Ma-
drid, Spain, 2006.
418 Dement Geriatr Cogn Disord 2008;25:408–422 Farlow /Miller /Pejovic
55 Nourhashemi F, Gillette-Guyonnet S, 68 Mazza M, Capuano A, Bria P, Mazza S: Gink- 79 Simons M, Schwarzler F, Lutjohann D, von
Andrieu S, Ghisolfi A, Ousset PJ, Grandjean go biloba and donepezil: a comparison in the Bergmann K, Beyreuther K, Dichgans J,
H, Grand A, Pous J, Vellas B, Albarede JL: treatment of Alzheimer’s dementia in a ran- Wormstall H, Hartmann T, Schulz JB: Treat-
Alzheimer disease: protective factors. Am J domized placebo-controlled double-blind ment with simvastatin in normocholester-
Clin Nutr 2000;71:643S–649S. study. Eur J Neurol 2006;13:981–985. olemic patients with Alzheimer’s disease: a
56 Luchsinger JA, Tang MX, Shea S, Mayeux 69 Schneider LS, DeKosky ST, Farlow MR, Tar- 26-week randomized, placebo-controlled,
R: Antioxidant vitamin intake and risk of iot PN, Hoerr R, Kieser M: A randomized, double-blind trial. Ann Neurol 2002; 52:
Alzheimer disease. Arch Neurol 2003; 60: double-blind, placebo-controlled trial of two 346–350.
203–208. doses of Ginkgo biloba extract in dementia of 80 Sparks DL, Sabbagh MN, Connor DJ, Lopez
57 Morris MC, Beckett LA, Scherr PA, Hebert the Alzheimer’s type. Curr Alzheimer Res J, Launer LJ, Browne P, Wasser D, Johnson-
LE, Bennett DA, Field TS, Evans DA: Vita- 2005;2:541–551. Traver S, Lochhead J, Ziolwolski C: Atorva-
min E and vitamin C supplement use and 70 Sierpina V, Wollschlaeger B, Blumenthal M: statin for the treatment of mild to moderate
risk of incident Alzheimer disease. Alzhei- Ginkgo biloba. Am Fam Physician 2003; 68: Alzheimer disease: preliminary results. Arch
mer Dis Assoc Disord 1998;12:121–126. 923–926. Neurol 2005;62:753–757.
58 Sano M, Ernesto C, Thomas RG, Klauber 71 Nelson HD, Humphrey LL, Nygren P, 81 Algotsson A, Winblad B: Patients with Alz-
MR, Schafer K, Grundman M, Woodbury Teutsch SM, Allan JD: Postmenopausal hor- heimer’s disease may be particularly suscep-
P, Growdon J, Cotman CW, Pfeiffer E, mone replacement therapy: scientific review. tible to adverse effects of statins. Dement
Schneider LS, Thal LJ: A controlled trial JAMA 2002;288:872–881. Geriatr Cogn Disord 2004;17:109–116.
of selegiline, alpha-tocopherol, or both as 72 Shumaker SA, Legault C, Thal L, Wallace 82 Yon A, Scogin F: Procedures for identifying
treatment for Alzheimer’s disease. The Alz- RB, Ockene JK, Hendrix SL, Jones BN 3rd, evidence-based psychological treatments for
heimer’s Disease Cooperative Study. N Engl Assaf AR, Jackson RD, Kotchen JM, Was- older adults. Psychol Aging 2007; 22:4–7.
J Med 1997;336:1216–1222. sertheil-Smoller S, Wactawski-Wende J: Es- 83 Sitzer DI, Twamley EW, Jeste DV: Cognitive
59 Petersen RC, Thomas RG, Grundman M, trogen plus progestin and the incidence training in Alzheimer’s disease: a meta-anal-
Bennett D, Doody R, Ferris S, Galasko D, Jin of dementia and mild cognitive impairment ysis of the literature. Acta Psychiatr Scand
S, Kaye J, Levey A, Pfeiffer E, Sano M, van in postmenopausal women: the Women’s 2006;114:75–90.
Dyck CH, Thal LJ: Vitamin E and donepezil Health Initiative Memory Study: a random- 84 Spector A, Orrell M, Davies S, Woods B: Re-
for the treatment of mild cognitive impair- ized controlled trial. JAMA 2003; 289: 2651– ality orientation for dementia. Cochrane Da-
ment. N Engl J Med 2005;352:2379–2388. 2662. tabase Syst Rev 2000:CD001119.
60 Miller ER 3rd, Pastor-Barriuso R, Dalal D, 73 Rapp SR, Espeland MA, Shumaker SA, Hen- 85 Spector A, Thorgrimsen L, Woods B, Royan
Riemersma RA, Appel LJ, Guallar E: Meta- derson VW, Brunner RL, Manson JE, Gass L, Davies S, Butterworth M, Orrell M: Effi-
analysis: high-dosage vitamin E supplemen- ML, Stefanick ML, Lane DS, Hays J, Johnson cacy of an evidence-based cognitive stimula-
tation may increase all-cause mortality. Ann KC, Coker LH, Dailey M, Bowen D: Effect of tion therapy programme for people with de-
Intern Med 2005;142:37–46. estrogen plus progestin on global cognitive mentia: randomised controlled trial. Br J
61 Lange KW, Riederer P, Youdim MB: Bio- function in postmenopausal women: the Psychiatry 2003;183:248–254.
chemical actions of l-deprenyl (selegiline). Women’s Health Initiative Memory Study: a 86 Logsdon RG, McCurry SM, Teri L: Evidence-
Clin Pharmacol Ther 1994;56:734–741. randomized controlled trial. JAMA 2003; based psychological treatments for disrup-
62 Filip V, Kolibas E: Selegiline in the treatment 289:2663–2672. tive behaviors in individuals with dementia.
of Alzheimer’s disease: a long-term random- 74 Chlebowski RT, Hendrix SL, Langer RD, Ste- Psychol Aging 2007;22:28–36.
ized placebo-controlled trial. Czech and Slo- fanick ML, Gass M, Lane D, Rodabough 87 Gallagher-Thompson D, Coon DW: Evi-
vak Senile Dementia of Alzheimer Type RJ, Gilligan MA, Cyr MG, Thomson CA, dence-based psychological treatments for
Study Group. J Psychiatry Neurosci 1999;24: Khandekar J, Petrovitch H, McTiernan A: distress in family caregivers of older adults.
234–243. Influence of estrogen plus progestin on Psychol Aging 2007;22:37–51.
63 Birks J, Flicker L: Selegiline for Alzheimer’s breast cancer and mammography in healthy 88 Gomez-Isla T, Price JL, McKeel DW Jr, Mor-
disease. Cochrane Database Syst Rev 2003: postmenopausal women: the Women’s ris JC, Growdon JH, Hyman BT: Profound
CD000442. Health Initiative Randomized Trial. JAMA loss of layer II entorhinal cortex neurons oc-
64 Wold RS, Lopez ST, Yau CL, Butler LM, 2003;289:3243–3253. curs in very mild Alzheimer’s disease. J Neu-
Pareo-Tubbeh SL, Waters DL, Garry PJ, 75 Wassertheil-Smoller S, Hendrix SL, Lima- rosci 1996;16:4491–4500.
Baumgartner RN: Increasing trends in elder- cher M, Heiss G, Kooperberg C, Baird A, 89 Morris JC, Storandt M, McKeel DW Jr, Rubin
ly persons’ use of nonvitamin, nonmineral Kotchen T, Curb JD, Black H, Rossouw JE, EH, Price JL, Grant EA, Berg L: Cerebral
dietary supplements and concurrent use of Aragaki A, Safford M, Stein E, Laowattana S, amyloid deposition and diffuse plaques in
medications. J Am Diet Assoc 2005;105:54– Mysiw WJ: Effect of estrogen plus progestin ‘normal’ aging: evidence for presymptom-
63. on stroke in postmenopausal women: the atic and very mild Alzheimer’s disease. Neu-
65 Ahlemeyer B, Krieglstein J: Neuroprotective Women’s Health Initiative: a randomized rology 1996; 46:707–719.
effects of Ginkgo biloba extract. Cell Mol Life trial. JAMA 2003;289:2673–2684. 90 Mondadori CR, Buchmann A, Mustovic H,
Sci 2003;60:1779–1792. 76 MacLennan AH, Henderson VW, Paine BJ, Schmidt CF, Boesiger P, Nitsch RM, Hock C,
66 Birks J, Grimley E, van Dongen M: Ginkgo Mathias J, Ramsay EN, Ryan P, Stocks NP, Streffer J, Henke K: Enhanced brain activity
biloba for cognitive impairment and demen- Taylor AW: Hormone therapy, timing of ini- may precede the diagnosis of Alzheimer’s
tia. Cochrane Database Syst Rev 2002; 4: tiation, and cognition in women aged older disease by 30 years. Brain 2006; 129: 2908–
CD003120. than 60 years: the REMEMBER pilot study. 2922.
67 Napryeyenko O, Borzenko I: Ginkgo biloba Menopause 2006;13:28–36. 91 Ingelsson M, Fukumoto H, Newell KL,
special extract in dementia with neuropsy- 77 Miida T, Takahashi A, Tanabe N, Ikeuchi T: Growdon JH, Hedley-Whyte ET, Frosch MP,
chiatric features. A randomised, placebo- Can statin therapy really reduce the risk of Albert MS, Hyman BT, Irizarry MC: Early
controlled, double-blind clinical trial. Arz- Alzheimer’s disease and slow its progres- Abeta accumulation and progressive synap-
neimittelforschung 2007;57:4–11. sion? Curr Opin Lipidol 2005; 16:619–623. tic loss, gliosis, and tangle formation in AD
78 Drachman D: Preventing and treating Alz- brain. Neurology 2004;62:925–931.
heimer’s disease: strategies and prospects.
Exp Rev Neurotherapeut 2003;3:565–569.
AD Treatment Options Dement Geriatr Cogn Disord 2008;25:408–422 419
92 DeKosky S: Early intervention is key to suc- 103 Petersen RC, Doody R, Kurz A, Mohs RC, 117 Tariq SH, Tumosa N, Chibnall JT, Perry
cessful management of Alzheimer disease. Morris JC, Rabins PV, Ritchie K, Rossor M, MH 3rd, Morley JE: Comparison of the
Alzheimer Dis Assoc Disord 2003;17(suppl Thal L, Winblad B: Current concepts in Saint Louis University Mental Status Ex-
4):S99–S104. mild cognitive impairment. Arch Neurol amination and the Mini-Mental State Ex-
93 Winblad B, Palmer K, Kivipelto M, Jelic V, 2001;58:1985–1992. amination for detecting dementia and mild
Fratiglioni L, Wahlund LO, Nordberg A, 104 Daly E, Zaitchik D, Copeland M, Schmah- neurocognitive disorder – a pilot study. Am
Backman L, Albert M, Almkvist O, Arai H, mann J, Gunther J, Albert M: Predicting J Geriatr Psychiatry 2006;14:900–910.
Basun H, Blennow K, de Leon M, DeCarli conversion to Alzheimer disease using 118 Dubois B, Feldman HH, Jacova C, Dekosky
C, Erkinjuntti T, Giacobini E, Graff C, Har- standardized clinical information. Arch ST, Barberger-Gateau P, Cummings J, Dela-
dy J, Jack C, Jorm A, Ritchie K, van Duijn Neurol 2000;57:675–680. courte A, Galasko D, Gauthier S, Jicha G,
C, Visser P, Petersen RC: Mild cognitive im- 105 Garand L, Dew MA, Eazor LR, DeKosky Meguro K, O’Brien J, Pasquier F, Robert P,
pairment – beyond controversies, towards ST, Reynolds CF 3rd: Caregiving burden Rossor M, Salloway S, Stern Y, Visser PJ,
a consensus: report of the International and psychiatric morbidity in spouses of Scheltens P: Research criteria for the diag-
Working Group on Mild Cognitive Impair- persons with mild cognitive impairment. nosis of Alzheimer’s disease: revising the
ment. J Intern Med 2004;256:240–246. Int J Geriatr Psychiatry 2005;20:512–522. NINCDS-ADRDA criteria. Lancet Neurol
94 Petersen RC: Mild cognitive impairment as 106 Ready RE, Ott BR, Grace J: Patient versus 2007;6:734–746.
a diagnostic entity. J Intern Med 2004; 256: informant perspectives of Quality of Life in 119 Gatz M, Prescott CA, Pedersen NL: Life-
183–194. Mild Cognitive Impairment and Alzhei- style risk and delaying factors. Alzheimer
95 Gauthier S, Reisberg B, Zaudig M, Petersen mer’s disease. Int J Geriatr Psychiatry 2004; Dis Assoc Disord 2006;20:S84–S88.
RC, Ritchie K, Broich K, Belleville S, Bro- 19:256–265. 120 Whitmer RA, Gunderson EP, Barrett-Con-
daty H, Bennett D, Chertkow H, Cum- 107 Olazaran J, Muniz R, Reisberg B, Pena-Ca- nor E, Quesenberry CP Jr, Yaffe K: Obesity
mings JL, de Leon M, Feldman H, Ganguli sanova J, del Ser T, Cruz-Jentoft AJ, Serrano in middle age and future risk of dementia:
M, Hampel H, Scheltens P, Tierney MC, P, Navarro E, Garcia de la Rocha ML, Frank a 27 year longitudinal population based
Whitehouse P, Winblad B: Mild cognitive A, Galiano M, Fernandez-Bullido Y, Serra study. BMJ 2005;330:1360.
impairment. Lancet 2006;367:1262–1270. JA, Gonzalez-Salvador MT, Sevilla C: Ben- 121 Whitmer RA, Gunderson EP, Quesenberry
96 Petersen RC, Smith GE, Waring SC, Ivnik efits of cognitive-motor intervention in CP Jr, Zhou J, Yaffe K: Body mass index in
RJ, Tangalos EG, Kokmen E: Mild cognitive MCI and mild to moderate Alzheimer dis- midlife and risk of Alzheimer disease and
impairment: clinical characterization and ease. Neurology 2004;63:2348–2353. vascular dementia. Curr Alzheimer Res
outcome. Arch Neurol 1999;56:303–308. 108 Ready RE, Ott BR, Grace J: Validity of in- 2007;4:103–109.
97 Fischer P, Jungwirth S, Zehetmayer S, formant reports about AD and MCI pa- 122 Gatz M, Mortimer JA, Fratiglioni L, Jo-
Weissgram S, Hoenigschnabl S, Gelpi E, tients’ memory. Alzheimer Dis Assoc Dis- hansson B, Berg S, Andel R, Crowe M, Fiske
Krampla W, Tragl KH: Conversion from ord 2004;18:11–16. A, Reynolds CA, Pedersen NL: Accounting
subtypes of mild cognitive impairment to 109 Scheltens P, Korf ES: Contribution of neu- for the relationship between low education
Alzheimer dementia. Neurology 2007; 68: roimaging in the diagnosis of Alzheimer’s and dementia: a twin study. Physiol Behav
288–291. disease and other dementias. Curr Opin 2007;92:232–237.
98 Tabert MH, Manly JJ, Liu X, Pelton GH, Neurol 2000;13:391–396. 123 Kivipelto M, Ngandu T, Laatikainen T,
Rosenblum S, Jacobs M, Zamora D, Good- 110 Chang CY, Silverman DH: Accuracy of ear- Winblad B, Soininen H, Tuomilehto J: Risk
kind M, Bell K, Stern Y, Devanand DP: ly diagnosis and its impact on the manage- score for the prediction of dementia risk in
Neuropsychological prediction of conver- ment and course of Alzheimer’s disease. 20 years among middle aged people: a lon-
sion to Alzheimer disease in patients with Expert Rev Mol Diagn 2004;4:63–69. gitudinal, population-based study. Lancet
mild cognitive impairment. Arch Gen Psy- 111 Dougall NJ, Bruggink S, Ebmeier KP: Sys- Neurol 2006;5:735–741.
chiatry 2006;63:916–924. tematic review of the diagnostic accuracy of 124 Orgogozo JM, Dartigues JF, Lafont S,
99 Palmer K, Berger AK, Monastero R, Win- 99mTc-HMPAO-SPECT in dementia. Am J Letenneur L, Commenges D, Salamon R,
blad B, Backman L, Fratiglioni L: Predic- Geriatr Psychiatry 2004;12:554–570. Renaud S, Breteler MB: Wine consumption
tors of progression from mild cognitive im- 112 Kantarci K, Jack CR Jr: Neuroimaging in and dementia in the elderly: a prospective
pairment to Alzheimer disease. Neurology Alzheimer disease: an evidence-based re- community study in the Bordeaux area.
2007;68:1596–1602. view. Neuroimaging Clin N Am 2003; 13: Rev Neurol (Paris) 1997;153:185–192.
100 Lopez OL, Kuller LH, Becker JT, Dulberg C, 197–209. 125 Anekonda TS: Resveratrol – a boon for
Sweet RA, Gach HM, Dekosky ST: Incidence 113 Silverman DH, Gambhir SS, Huang HW, treating Alzheimer’s disease? Brain Res
of dementia in mild cognitive impairment in Schwimmer J, Kim S, Small GW, Chodosh Brain Res Rev 2006;52:316–326.
the cardiovascular health study cognition J, Czernin J, Phelps ME: Evaluating early 126 Dai Q, Borenstein AR, Wu Y, Jackson JC,
study. Arch Neurol 2007;64:416–420. dementia with and without assessment of Larson EB: Fruit and vegetable juices and
101 Schonknecht P, Pantel J, Kaiser E, Tho- regional cerebral metabolism by PET: a Alzheimer’s disease: the Kame Project. Am
mann P, Schroder J: Increased tau protein comparison of predicted costs and benefits. J Med 2006;119:751–759.
differentiates mild cognitive impairment J Nucl Med 2002;43:253–266. 127 Rezai-Zadeh K, Shytle D, Sun N, Mori T,
from geriatric depression and predicts con- 114 McMahon PM, Araki SS, Sandberg EA, Hou H, Jeanniton D, Ehrhart J, Townsend
version to dementia. Neurosci Lett 2007; Neumann PJ, Gazelle GS: Cost-effective- K, Zeng J, Morgan D, Hardy J, Town T, Tan
416:39–42. ness of PET in the diagnosis of Alzheimer J: Green tea epigallocatechin-3-gallate
102 Dubois B, Feldman HH, Jacova C, Dekosky disease. Radiology 2003;228: 515–522. (EGCG) modulates amyloid precursor pro-
ST, Barberger-Gateau P, Cummings J, Dela- 115 McMahon PM, Araki SS, Neumann PJ, tein cleavage and reduces cerebral amyloi-
courte A, Galasko D, Gauthier S, Jicha G, Harris GJ, Gazelle GS: Cost-effectiveness of dosis in Alzheimer transgenic mice. J Neu-
Meguro K, O’Brien J, Pasquier F, Robert P, functional imaging tests in the diagnosis of rosci 2005;25:8807–8814.
Rossor M, Salloway S, Stern Y, Visser PJ, Alzheimer disease. Radiology 2000; 217:
Scheltens P: Research criteria for the diag- 58–68.
nosis of Alzheimer’s disease: revising the 116 Lorentz WJ, Scanlan JM, Borson S: Brief
NINCDS-ADRDA criteria. Lancet Neurol screening tests for dementia. Can J Psychia-
2007;6:734–746. try 2002;47:723–733.
420 Dement Geriatr Cogn Disord 2008;25:408–422 Farlow /Miller /Pejovic
128 Arendash GW, Schleif W, Rezai-Zadeh K, 141 Fratiglioni L, Paillard-Borg S, Winblad B: 154 Winblad B, Kilander L, Eriksson S, Mint-
Jackson EK, Zacharia LC, Cracchiolo JR, An active and socially integrated lifestyle in hon L, Batsman S, Wetterholm AL, Jans-
Shippy D, Tan J: Caffeine protects Alzhei- late life might protect against dementia. son-Blixt C, Haglund A: Donepezil in pa-
mer’s mice against cognitive impairment Lancet Neurol 2004;3:343–353. tients with severe Alzheimer’s disease:
and reduces brain beta-amyloid produc- 142 Mittelman MS, Haley WE, Clay OJ, Roth double-blind, parallel-group, placebo-
tion. Neuroscience 2006;142:941–952. DL: Improving caregiver well-being delays controlled study. Lancet 2006; 367: 1057–
129 Lindsay J, Laurin D, Verreault R, Hebert R, nursing home placement of patients with 1065.
Helliwell B, Hill GB, McDowell I: Risk fac- Alzheimer disease. Neurology 2006; 67: 155 Schmitt FA, Wichems CH: A systematic re-
tors for Alzheimer’s disease: a prospective 1592–1599. view of assessment and treatment of mod-
analysis from the Canadian Study of Health 143 Mittelman MS, Roth DL, Haley WE, Zarit erate to severe Alzheimer’s disease. Prim
and Aging. Am J Epidemiol 2002; 156:445– SH: Effects of a caregiver intervention on Care Companion J Clin Psychiatry 2006; 8:
453. negative caregiver appraisals of behavior 158–159.
130 Lim GP, Chu T, Yang F, Beech W, Frautschy problems in patients with Alzheimer’s dis- 156 Feldman HH, Ferris S, Winblad B, Sfikas
SA, Cole GM: The curry spice curcumin re- ease: results of a randomized trial. J Geron- N, Mancione L, He Y, Tekin S, Burns A,
duces oxidative damage and amyloid pa- tol B Psychol Sci Soc Sci 2004; 59:P27–P34. Cummings J, del Ser T, Inzitari D, Orgogo-
thology in an Alzheimer transgenic mouse. 144 Roth DL, Mittelman MS, Clay OJ, Madan zo JM, Sauer H, Scheltens P, Scarpini E,
J Neurosci 2001;21:8370–8377. A, Haley WE: Changes in social support as Herrmann N, Farlow M, Potkin S, Charles
131 Yang F, Lim GP, Begum AN, Ubeda OJ, mediators of the impact of a psychosocial HC, Fox NC, Lane R: Effect of rivastigmine
Simmons MR, Ambegaokar SS, Chen PP, intervention for spouse caregivers of per- on delay to diagnosis of Alzheimer’s dis-
Kayed R, Glabe CG, Frautschy SA, Cole sons with Alzheimer’s disease. Psychol Ag- ease from mild cognitive impairment: the
GM: Curcumin inhibits formation of amy- ing 2005;20:634–644. InDDEx study. Lancet Neurol 2007; 6:501–
loid beta oligomers and fibrils, binds 145 Jang Y, Clay OJ, Roth DL, Haley WE, Mit- 512.
plaques, and reduces amyloid in vivo. J Biol telman MS: Neuroticism and longitudinal 157 Birks J, Flicker L: Donepezil for mild cogni-
Chem 2005;280:5892–5901. change in caregiver depression: impact of a tive impairment. Cochrane Database Syst
132 Morris MC, Evans DA, Bienias JL, Tangney spouse-caregiver intervention program. Rev 2006;3:CD006104.
CC, Bennett DA, Wilson RS, Aggarwal N, Gerontologist 2004; 44:311–317. 158 Lipton SA: Paradigm shift in neuroprotec-
Schneider J: Consumption of fish and n-3 146 Mittelman MS, Roth DL, Coon DW, Haley tion by NMDA receptor blockade: meman-
fatty acids and risk of incident Alzheimer WE: Sustained benefit of supportive inter- tine and beyond. Nat Rev Drug Discov
disease. Arch Neurol 2003;60:940–946. vention for depressive symptoms in care- 2006;5:160–170.
133 Morris MC, Evans DA, Tangney CC, Bien- givers of patients with Alzheimer’s disease. 159 Hartmann S, Mobius HJ: Tolerability of
ias JL, Wilson RS: Fish consumption and Am J Psychiatry 2004;161:850–856. memantine in combination with cholines-
cognitive decline with age in a large com- 147 Belle SH, Burgio L, Burns R, Coon D, Czaja terase inhibitors in dementia therapy. Int
munity study. Arch Neurol 2005; 62: 1849– SJ, Gallagher-Thompson D, Gitlin LN, Clin Psychopharmacol 2003;18:81–85.
1853. Klinger J, Koepke KM, Lee CC, Martin- 160 Pass MD, Shua-Haim JR, Patel P, Smith J:
134 Morris MC, Evans DA, Bienias JL, Tangney dale-Adams J, Nichols L, Schulz R, Stahl S, Safety, tolerability and caregiver’s impres-
CC, Bennett DA, Aggarwal N, Schneider J, Stevens A, Winter L, Zhang S: Enhancing sions of combination therapy with galan-
Wilson RS: Dietary fats and the risk of in- the quality of life of dementia caregivers tamine and memantine for the treatment of
cident Alzheimer disease. Arch Neurol from different ethnic or racial groups: a Alzheimer’s disease (Abstract). Neurobiol
2003;60:194–200. randomized, controlled trial. Ann Intern Aging 2004;25(suppl 2):S210.
135 Verghese J, Lipton RB, Katz MJ, Hall CB, Med 2006;145:727–738. 161 Riepe MW, Adler G, Ibach B, Weinkauf B,
Derby CA, Kuslansky G, Ambrose AF, Sli- 148 Sorensen S, Duberstein P, Gill D, Pinquart Gunay I, Tracik F: Adding memantine to
winski M, Buschke H: Leisure activities and M: Dementia care: mental health effects, rivastigmine therapy in patients with mild-
the risk of dementia in the elderly. N Engl J intervention strategies, and clinical impli- to-moderate Alzheimer’s disease: results of
Med 2003;348:2508–2516. cations. Lancet Neurol 2006;5:961–973. a 12-week, open-label pilot study. Prim
136 Larson EB, Wang L, Bowen JD, McCormick 149 Gauthier S, Emre M, Farlow MR, Bullock R, Care Companion J Clin Psychiatry 2006; 8:
WC, Teri L, Crane P, Kukull W: Exercise is Grossberg GT, Potkin SG: Strategies for 258–263.
associated with reduced risk for incident de- continued successful treatment of Alz- 162 Hien le TT, Cumming RG, Cameron ID,
mentia among persons 65 years of age and heimer’s disease: switching cholinesterase Chen JS, Lord SR, March LM, Schwarz J, Le
older. Ann Intern Med 2006;144:73–81. inhibitors. Curr Med Res Opin 2003; 19: Couteur DG, Sambrook PN: Atypical anti-
137 Cotman CW, Berchtold NC: Exercise: a be- 707–714. psychotic medications and risk of falls in
havioral intervention to enhance brain 150 SDI Alzheimer’s Disease Patient Persisten- residents of aged care facilities. J Am Geri-
health and plasticity. Trends Neurosci cy and Compliance Study (August 2006 atr Soc 2005;53:1290–1295.
2002;25:295–301. Update): NPA, IMS; August 2006. 163 Nelson JC: Increased risk of cerebrovascu-
138 Abbott RD, White LR, Ross GW, Masaki 151 Seltzer B: Donepezil: an update. Expert lar adverse events and death in elderly de-
KH, Curb JD, Petrovitch H: Walking and Opin Pharmacother 2007;8:1011–1023. mented patients treated with atypical anti-
dementia in physically capable elderly men. 152 Emre M: Switching cholinesterase inhibi- psychotics: what’s a clinician to do? J Clin
JAMA 2004;292:1447–1453. tors in patients with Alzheimer’s disease. Psychiatry 2005;66:1071.
139 Weuve J, Kang JH, Manson JE, Breteler Int J Clin Pract Suppl 2002: 64–72. 164 Schneider LS, Tariot PN, Dagerman KS,
MM, Ware JH, Grodstein F: Physical activ- 153 Morris JC, Farlow MR, Ferris SH, Kurz AF, Davis SM, Hsiao JK, Ismail MS, Lebowitz
ity, including walking, and cognitive func- Maelicke A, Rasmusen L, Wilkinson D, Yan BD, Lyketsos CG, Ryan JM, Stroup TS,
tion in older women. JAMA 2004; 292: B: Therapeutic continuity in Alzheimer’s Sultzer DL, Weintraub D, Lieberman JA,
1454–1461. disease: switching patients to galantamine. the CATIE-AD Study Group: Effectiveness
140 Heyn P, Abreu BC, Ottenbacher KJ: The ef- Panel discussion: recommendations for of atypical antipsychotic drugs in patients
fects of exercise training on elderly persons prescribers. Clin Ther 2001; 23(suppl A): with Alzheimer’s disease. N Engl J Med
with cognitive impairment and dementia: a A31–A39. 2006;355:1525–1538.
meta-analysis. Arch Phys Med Rehabil
2004;85: 1694–1704.
AD Treatment Options Dement Geriatr Cogn Disord 2008;25:408–422 421
165 Cummings JL, Frank JC, Cherry D, Kohat- 172 Pirttila T, Wilcock G, Truyen L, Damaraju 178 Corey-Bloom J, Anand J, Veach J: A ran-
su ND, Kemp B, Hewett L, Mittman B: CV: Long-term efficacy and safety of galan- domized trial evaluating the efficacy and
Guidelines for managing Alzheimer’s dis- tamine in patients with mild-to-moderate safety of ENA 713 (rivastigmine tartrate), a
ease. II. Treatment. Am Fam Physician Alzheimer’s disease: multicenter trial. Eur new acetylcholinesterase inhibitor, in pa-
2002;65: 2525–2534. J Neurol 2004;11:734–741. tients with mild to moderately severe Alz-
166 Trinh NH, Hoblyn J, Mohanty S, Yaffe K: 173 Winblad B, Wimo A, Engedal K, Soininen heimer’s disease. International Journal of
Efficacy of cholinesterase inhibitors in the H, Verhey F, Waldemar G, Wetterholm AL, Geriatric Psychopharmacology 1998; 1:55–
treatment of neuropsychiatric symptoms Haglund A, Zhang R, Schindler R: 3-year 65.
and functional impairment in Alzheimer study of donepezil therapy in Alzheimer’s 179 Rosler M, Anand R, Cicin-Sain A, Gauthier
disease: a meta-analysis. JAMA 2003; 289: disease: effects of early and continuous S, Agid Y, Dal-Bianco P, Stahelin HB, Hart-
210–216. therapy. Dement Geriatr Cogn Disord man R, Gharabawi M: Efficacy and safety
167 Grossberg GT: Effect of rivastigmine in the 2006;21:353–363. of rivastigmine in patients with Alzhei-
treatment of behavioral disturbances asso- 174 Farlow MR, Lilly ML: Rivastigmine: an mer’s disease: international randomised
ciated with dementia: review of neuropsy- open-label, observational study of safety controlled trial. BMJ 1999;318:633–638.
chiatric impairment in neuropsychiatric and effectiveness in treating patients with 180 Raskind MA, Peskind ER, Wessel T, Yuan
impairment in Alzheimer’s disease. Curr Alzheimer’s disease for up to 5 years. BMC W: Galantamine in AD: A 6-month ran-
Med Res Opin 2005;21:1631–1639. Geriatr 2005;5:3. domized, placebo-controlled trial with a 6-
168 Bonelli RM, Hofmann P, Aschoff A, Nie- 175 Cummings JL, Frank JC, Cherry D, Kohat- month extension. The Galantamine USA-1
derwieser G, Heuberger C, Jirikowski G, su ND, Kemp B, Hewett L, Mittman B: Study Group. Neurology 2000;54:2261–
Kapfhammer HP: The influence of psycho- Guidelines for managing Alzheimer’s dis- 2268.
tropic drugs on cerebral cell death: female ease. I. Assessment. Am Fam Physician 181 Tariot PN, Solomon PR, Morris JC, Ker-
neurovulnerability to antipsychotics. Int 2002;65: 2263–2272. shaw P, Lilienfeld S, Ding C: A 5-month,
Clin Psychopharmacol 2005; 20:145–149. 176 Rogers SL, Doody RS, Mohs RC, Friedhoff randomized, placebo-controlled trial of
169 Onder G, Zanetti O, Giacobini E, Frisoni LT: Donepezil improves cognition and galantamine in AD. The Galantamine
GB, Bartorelli L, Carbone G, Lambertucci global function in Alzheimer disease: a 15- USA-10 Study Group. Neurology 2000;
P, Silveri MC, Bernabei R: Reality orienta- week, double-blind, placebo-controlled 5:2269–2276
tion therapy combined with cholinesterase study. Donepezil Study Group. Arch Intern 182 Wilcock GK, Lilienfeld S, Gaens E: Efficacy
inhibitors in Alzheimer’s disease: ran- Med 1998;158:1021–1031. and safety of galantamine in patients with
domised controlled trial. Br J Psychiatry 177 Rogers SL, Farlow MR, Doody RS, Mohs R, mild to moderate Alzheimer’s disease: mul-
2005;187:450–455. Friedhoff LT: A 24-week, double-blind, pla- ticentre randomised controlled trial.
170 Doody RS, Geldmacher DS, Gordon B, Per- cebo-controlled trial of donepezil in pa- Galantamine International-1 Study Group.
domo CA, Pratt RD: Open-label, multi- tients with Alzheimer’s disease. Donepezil BMJ 2000;321:1445–1449.
center, phase 3 extension study of the safety Study Group. Neurology 1998;50:136–145. 183 Rockwood K, Mintzer J, Truyen L, Wessel
and efficacy of donepezil in patients with T, Wilkinson D: Effects of a flexible galan-
Alzheimer disease. Arch Neurol 2001; 58: tamine dose in Alzheimer’s disease: a ran-
427–433. domised, controlled trial. J Neurol Neuro-
171 Reisberg B, Doody R, Stoffler A, Schmitt F, surg Psychiatry 2001;7:589–895.
Ferris S, Mobius HJ: A 24-week open-label
extension study of memantine in moderate
to severe Alzheimer disease. Arch Neurol
2006;63:49–54.
422 Dement Geriatr Cogn Disord 2008;25:408–422 Farlow /Miller /Pejovic
Reproduced with permission of the copyright owner. Further reproduction prohibited without permission.
You might also like
- Psychiatry Practice BoostersFrom EverandPsychiatry Practice BoostersJesse KoskeyNo ratings yet
- The Child Medication Fact Book for Psychiatric PracticeFrom EverandThe Child Medication Fact Book for Psychiatric PracticeRating: 5 out of 5 stars5/5 (1)
- Genomic Biomarkers for Pharmaceutical Development: Advancing Personalized Health CareFrom EverandGenomic Biomarkers for Pharmaceutical Development: Advancing Personalized Health CareYihong YaoNo ratings yet
- Cours PharmacoDocument41 pagesCours PharmacoHIBA OUFKIRNo ratings yet
- Mahatme M S Et. Al., 2018Document6 pagesMahatme M S Et. Al., 2018kaniNo ratings yet
- Anti-Aging Therapeutics Volume XIIIFrom EverandAnti-Aging Therapeutics Volume XIIINo ratings yet
- Taiwan Dementia Treatment Guideline: International Journal of GerontologyDocument9 pagesTaiwan Dementia Treatment Guideline: International Journal of GerontologyPei-Hao ChenNo ratings yet
- The Prevention and Treatment of Disease with a Plant-Based Diet Volume 2: Evidence-based articles to guide the physicianFrom EverandThe Prevention and Treatment of Disease with a Plant-Based Diet Volume 2: Evidence-based articles to guide the physicianNo ratings yet
- Dis ContinuationDocument8 pagesDis ContinuationGrace KahonoNo ratings yet
- Habibudin 2014-Pharmacological Management of Obesity Past, Present and FutureDocument10 pagesHabibudin 2014-Pharmacological Management of Obesity Past, Present and FutureMas NuriNo ratings yet
- Efficacy and Safety of Dasotraline in Adults With Binge-Eating Disorder: A Randomized, Placebo-Controlled, Fixed-Dose Clinical TrialDocument10 pagesEfficacy and Safety of Dasotraline in Adults With Binge-Eating Disorder: A Randomized, Placebo-Controlled, Fixed-Dose Clinical TrialNaiana PaulaNo ratings yet
- WNL 2022 201574Document10 pagesWNL 2022 201574triska antonyNo ratings yet
- User's Guide to Natural Therapies for Cancer Prevention and ControlFrom EverandUser's Guide to Natural Therapies for Cancer Prevention and ControlRating: 5 out of 5 stars5/5 (1)
- Cancer Pain Management: Opioid Analgesics, Part 2Document20 pagesCancer Pain Management: Opioid Analgesics, Part 2azkiel fikrieNo ratings yet
- Piracetam Cognitive Vitality For ResearchersDocument13 pagesPiracetam Cognitive Vitality For ResearchersreubenmercadoNo ratings yet
- Persistence and Switching Patterns of Oral Migraine Prophylactic Medications Among Patients With Chronic Migraine: A Retrospective Claims AnalysisDocument16 pagesPersistence and Switching Patterns of Oral Migraine Prophylactic Medications Among Patients With Chronic Migraine: A Retrospective Claims AnalysisAzam alausyNo ratings yet
- Nejme 2301045Document2 pagesNejme 2301045Billy LamNo ratings yet
- Complementary and Alternative Therapies and the Aging Population: An Evidence-Based ApproachFrom EverandComplementary and Alternative Therapies and the Aging Population: An Evidence-Based ApproachRating: 5 out of 5 stars5/5 (1)
- Unzip Your Genes: 5 Choices to Reveal a Radically Radiant YouFrom EverandUnzip Your Genes: 5 Choices to Reveal a Radically Radiant YouNo ratings yet
- Obat Anti EpilepsiDocument23 pagesObat Anti EpilepsiTegar Jati KusumaNo ratings yet
- Pi Is 0149291820302836Document15 pagesPi Is 0149291820302836John SMithNo ratings yet
- AripiprazolDocument15 pagesAripiprazolFabrício de Souza XavierNo ratings yet
- General: Guideline TitleDocument23 pagesGeneral: Guideline TitleAndi NamirahNo ratings yet
- Child Medication Fact Book for Psychiatric Practice, Second EditionFrom EverandChild Medication Fact Book for Psychiatric Practice, Second EditionNo ratings yet
- Psychiatry Practice Boosters, Second Edition: Insights from research to enhance your clinical workFrom EverandPsychiatry Practice Boosters, Second Edition: Insights from research to enhance your clinical workNo ratings yet
- Obesity 2010 ReportDocument13 pagesObesity 2010 ReportAlda LiuNo ratings yet
- Personalized Medicine and Psychiatry - Dream or RealityDocument6 pagesPersonalized Medicine and Psychiatry - Dream or RealityAwais QureshiNo ratings yet
- Literature Review: Parental Refusal of Childhood Vaccinations TonsillectomyDocument2 pagesLiterature Review: Parental Refusal of Childhood Vaccinations TonsillectomyilldoitNo ratings yet
- Adzenys PIDocument25 pagesAdzenys PIVFFanNo ratings yet
- Myrene PostDocument4 pagesMyrene PostMEHATHI SUBASHNo ratings yet
- Hendrix2019 Article PatternsOfHigh-DoseAndLong-TerDocument9 pagesHendrix2019 Article PatternsOfHigh-DoseAndLong-TerOlivia Chandra DeviNo ratings yet
- 3C Wednesday Polypharmacy WallaceDocument13 pages3C Wednesday Polypharmacy WallaceYuliana Eka SintaNo ratings yet
- Medication Fact Book for Psychiatric Practice, Fifth EditionFrom EverandMedication Fact Book for Psychiatric Practice, Fifth EditionNo ratings yet
- The Age of Personalized Medicine: Tailoring Treatment to Your Unique DNAFrom EverandThe Age of Personalized Medicine: Tailoring Treatment to Your Unique DNANo ratings yet
- Antiemetic Drug Use in Children What The.3Document6 pagesAntiemetic Drug Use in Children What The.3Zafitri AsrulNo ratings yet
- Gniadeckietal 2015 BritishjournalofdermatologyDocument9 pagesGniadeckietal 2015 BritishjournalofdermatologyChristman SihiteNo ratings yet
- Daughton - 2009 - Review of ADHD PharmacotherapiesDocument9 pagesDaughton - 2009 - Review of ADHD PharmacotherapiesRene LutherNo ratings yet
- Eptinezumab in Episodic Migraine: A Randomized, Double-Blind, Placebo-Controlled Study (PROMISE-1)Document14 pagesEptinezumab in Episodic Migraine: A Randomized, Double-Blind, Placebo-Controlled Study (PROMISE-1)JUAN MANUEL CERON ALVARADONo ratings yet
- How to Restore Your Health: Practical Steps to Transform Your Mind, Nutrition and LifestyleFrom EverandHow to Restore Your Health: Practical Steps to Transform Your Mind, Nutrition and LifestyleNo ratings yet
- Antidiabetic Activity of Plants ThesisDocument8 pagesAntidiabetic Activity of Plants Thesisygsyoeikd100% (1)
- BIOS LIFE - Utah Trial by Dr. Peter J.E. VerdegemDocument6 pagesBIOS LIFE - Utah Trial by Dr. Peter J.E. VerdegemHisWellnessNo ratings yet
- 1 s2.0 S0002838X21000885Document2 pages1 s2.0 S0002838X21000885henry hernandezNo ratings yet
- LowDog4 AdaptogensDocument34 pagesLowDog4 AdaptogensJoshNo ratings yet
- Innovation in Aging Symposium Highlights ResearchDocument1 pageInnovation in Aging Symposium Highlights ResearchHoang Mai NguyenNo ratings yet
- Dinh Lang Cognitive Vitality For ResearchersDocument7 pagesDinh Lang Cognitive Vitality For ResearchersTuấn Trương NgọcNo ratings yet
- 2013 PavaniDocument11 pages2013 PavaniGopal KrishnaNo ratings yet
- Module 3 Discussion NUR520Document5 pagesModule 3 Discussion NUR52078xh8x8b69No ratings yet
- Deprescribing Tools: A Review of The Types of Tools Available To Aid Deprescribing in Clinical PracticeDocument10 pagesDeprescribing Tools: A Review of The Types of Tools Available To Aid Deprescribing in Clinical PracticeandresadarvegNo ratings yet
- Newsletter - Fall 2022 FinalDocument14 pagesNewsletter - Fall 2022 Finalapi-398712370No ratings yet
- Guideline Summary NGC-6824: FDA Warning/Regulatory AlertDocument8 pagesGuideline Summary NGC-6824: FDA Warning/Regulatory AlertÜnal ZağliNo ratings yet
- Weight Loss Genes - the Genetic Advantage: The genetic advantageFrom EverandWeight Loss Genes - the Genetic Advantage: The genetic advantageNo ratings yet
- Protandim Cognitive Vitality For ResearchersDocument7 pagesProtandim Cognitive Vitality For Researchersierine joy caserialNo ratings yet
- World Happiness ReportDocument170 pagesWorld Happiness ReportmrdanNo ratings yet
- A Foster, 2017 - What Students Know About Child AbuseDocument30 pagesA Foster, 2017 - What Students Know About Child AbusearuesjasNo ratings yet
- Advice of The Wise PDFDocument10 pagesAdvice of The Wise PDFMelissaNo ratings yet
- Pro 43 6 576 PDFDocument10 pagesPro 43 6 576 PDFRaghuNo ratings yet
- Lists of Pharmaceutical Companies in New JerseyDocument23 pagesLists of Pharmaceutical Companies in New JerseyFithrul Mubarok100% (1)
- Quick Reference BWDocument2 pagesQuick Reference BWmcbermudezNo ratings yet
- Apm 20050Document6 pagesApm 20050hnzzn2bymdNo ratings yet
- LiverpoolSedation ManagementDocument9 pagesLiverpoolSedation ManagementTheresia Avila KurniaNo ratings yet
- Bio Pharmaceutics and Pharmacokinetics A Treatise Brahmankar Jaiswal Pharma DostDocument206 pagesBio Pharmaceutics and Pharmacokinetics A Treatise Brahmankar Jaiswal Pharma DostDeviselvam86% (7)
- Manufacturing: Capsule, A Form of Dosage Form in Medication, Are Common in Our Day-To-Day HealthDocument3 pagesManufacturing: Capsule, A Form of Dosage Form in Medication, Are Common in Our Day-To-Day HealthZubair Bashir KhanNo ratings yet
- DiphenhydramineDocument3 pagesDiphenhydramineGwyn RosalesNo ratings yet
- Pengaruh Pemberian Air Rebusan Daun Sirsak (Annona Muricata) Terhadap Penurunan Kadar Glukosa Darah Pada Mencit Diabetes MellitusDocument1 pagePengaruh Pemberian Air Rebusan Daun Sirsak (Annona Muricata) Terhadap Penurunan Kadar Glukosa Darah Pada Mencit Diabetes MellitusAgus StyawanNo ratings yet
- Rko 2023Document16 pagesRko 2023Annita MaretnaNo ratings yet
- Clarithromycin DrugDocument1 pageClarithromycin DrugMatth N. ErejerNo ratings yet
- Daftar Harga Ethical Mei 2015Document130 pagesDaftar Harga Ethical Mei 2015Sopha DwiNo ratings yet
- Dapus CaDocument3 pagesDapus CaAlif RamadhanNo ratings yet
- Thesis StatementDocument3 pagesThesis Statementapi-301334682No ratings yet
- OB FR SE List 2016 03Document40 pagesOB FR SE List 2016 03Christine MarieNo ratings yet
- Intravenous Anaesthetic Agents ExplainedDocument5 pagesIntravenous Anaesthetic Agents ExplainedAlisya NadhilahNo ratings yet
- Phrmaceutical IndustryDocument49 pagesPhrmaceutical IndustryRiddhi PandyaNo ratings yet
- CimetidineDocument3 pagesCimetidineRodolfo Lone UlvenNo ratings yet
- Good Advice: 1. The Flu 2. A Sunburn 3. Sore Muscles 4. Stress 5. InsomniaDocument2 pagesGood Advice: 1. The Flu 2. A Sunburn 3. Sore Muscles 4. Stress 5. InsomniaYusufSaputrooNo ratings yet
- Oral hypoglycemic agents: Biguanides, Sulfonylureas, α-glucosidase inhibitors and moreDocument31 pagesOral hypoglycemic agents: Biguanides, Sulfonylureas, α-glucosidase inhibitors and moreBivek Singh RathoreNo ratings yet
- Acceso Dificil Via Periferica PediatricosDocument5 pagesAcceso Dificil Via Periferica PediatricosGein AgozNo ratings yet
- Clinical Research OverviewDocument40 pagesClinical Research Overviewjyoti100% (1)
- Activity 7 Calculations Involved in Parenteral Therapy: University of Santo TomasDocument3 pagesActivity 7 Calculations Involved in Parenteral Therapy: University of Santo TomasJANNIE BELLE RODRIGUEZ100% (1)
- Schedule 4 Appendix D Drugs (Prescribed Restricted Substances)Document2 pagesSchedule 4 Appendix D Drugs (Prescribed Restricted Substances)GUrpreet SinghNo ratings yet
- Cholinerv - DSDocument2 pagesCholinerv - DSThrinNo ratings yet
- 1 Early Access Application 14 May 2018 PDFDocument2 pages1 Early Access Application 14 May 2018 PDFArdat LiliNo ratings yet
- To C Manual of Icu ProceduresDocument9 pagesTo C Manual of Icu ProceduresVitor SandresNo ratings yet
- Cyclophosphamide Doxorubicin Ver 1.1Document6 pagesCyclophosphamide Doxorubicin Ver 1.1Yudi ApriyantoNo ratings yet
- Laporan Belanja Obat Bulan Januari 2017: No Tanggal Nama Obat Harga Satuan Jumlah BarangDocument16 pagesLaporan Belanja Obat Bulan Januari 2017: No Tanggal Nama Obat Harga Satuan Jumlah Barangcitra husadaNo ratings yet
- Tylenol 500 MGDocument3 pagesTylenol 500 MGENo ratings yet
- Combined Cataract and Glaucoma SurgeryDocument20 pagesCombined Cataract and Glaucoma SurgerymanognaaaaNo ratings yet