Professional Documents
Culture Documents
APOE and Alzheimer
Uploaded by
KhushCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
APOE and Alzheimer
Uploaded by
KhushCopyright:
Available Formats
Review
APOE and Alzheimer’s disease: advances in genetics,
pathophysiology, and therapeutic approaches
Alberto Serrano-Pozo, Sudeshna Das, Bradley T Hyman
Lancet Neurol 2021; 20: 68–80 The APOE ε4 allele remains the strongest genetic risk factor for sporadic Alzheimer’s disease and the APOE ε2
This online publication has allele the strongest genetic protective factor after multiple large scale genome-wide association studies and genome-
been corrected. The corrected wide association meta-analyses. However, no therapies directed at APOE are currently available. Although initial
version first appeared at
studies causally linked APOE with amyloid-β peptide aggregation and clearance, over the past 5 years our
thelancet.com/neurology on
January 20, 2021 understanding of APOE pathogenesis has expanded beyond amyloid-β peptide-centric mechanisms to tau
Department of Neurology,
neurofibrillary degeneration, microglia and astrocyte responses, and blood–brain barrier disruption. Because all
Massachusetts General these pathological processes can potentially contribute to cognitive impairment, it is important to use this new
Hospital, Boston, MA, USA knowledge to develop therapies directed at APOE. Several therapeutic approaches have been successful in mouse
(A Serrano-Pozo MD, S Das PhD,
models expressing human APOE alleles, including increasing or reducing APOE levels, enhancing its lipidation,
Prof B T Hyman MD);
Massachusetts Alzheimer’s blocking the interactions between APOE and amyloid-β peptide, and genetically switching APOE4 to APOE3 or
Disease Research Center, APOE2 isoforms, but translation to human clinical trials has proven challenging.
Charlestown, MA, USA
(A Serrano-Pozo, S Das,
Prof B T Hyman); and Harvard
Introduction to be effective in mouse models and hold promise for
Medical School, Boston, MA, Even after multiple large-scale genome-wide association translation to human clinical trials. In this Review, we
USA (A Serrano-Pozo, S Das, studies (GWAS) and GWAS meta-analyses1, the ε4 allele of discuss the advances made in genetics, pathophysiology,
Prof B T Hyman) the APOE gene (compared with the most common ε3 and therapeutic approaches related to APOE and
Correspondence to: allele) continues to be the strongest genetic risk factor Alzheimer’s disease.
Prof Bradley T Hyman,
associated with sporadic Alzheimer’s disease since its
Massachusetts Alzheimer’s
Disease Research Center, discovery in 1993. Moreover, the relatively rare APOE ε2 Genetic discoveries related to APOE
Charlestown, MA 02129, USA allele remains by far the strongest genetic protective Over the past 3 years, human genetic studies have
bhyman@mgh.harvard.edu factor against sporadic Alzheimer’s disease (panel 1), suggested risk modifiers that mitigate or increase APOE
empha sising the importance of APOE’s role in ε4-associated Alzheimer’s disease risk, and identified
Alzheimer’s disease pathogenesis. Because Alzheimer’s haplotypes with heterogeneous effects. Understanding the
disease is defined by the accumulation of two hallmark risk variation in APOE ε4 carriers has the potential to shed
pathological protein aggregates: amyloid-β peptide (Aβ) further light on APOE pathobiology and mechanisms of
plaques and neuro fibrillary tangles containing hyper resilience and resistance to Alzheimer’s disease, which
phosphorylated tau, one postulate is that APOE affects could have therapeutic value.
these lesions. Although solid evidence supports this view,
emerging advances are changing our understanding of APOE ε2 homozygosity
APOE involvement in Alzheimer’s disease. First, new In an analysis2 of a US cohort with approximately
genetic modifiers and the APOE local ancestry (ie, the 5000 neuropathologically confirmed Alzheimer’s disease
population-specific genetic variation in the APOE region) and control subjects, APOE ε2 homozygosity was associ
have been associated with a differential APOE ε4-linked ated with much lower odds of Alzheimer’s disease
increased risk of Alzheimer’s disease. Second, although than was APOE ε3 homozygosity (odds ratio [OR] 0·13
APOE modifica tion of Alzheimer’s disease risk has [95% CI 0·05–0·36]), and the APOE ε2ε3 genotype (0·39
been long attributed to its effects on Aβ, systematic [0·30–0·50]). The contrast of APOE ε2 homozygosity
neuropathological examination of large autopsy cohorts versus APOE ε4 homozygosity was even greater (0·004
has suggested that the APOE genotype also correlates with [0·001–0·014]), and APOE ε2 was also associ ated with
the presence and severity of other proteinopathies, milder Alzheimer’s disease neuropathological changes (ie,
pointing to new causal links. Third, technological advances less widespread Aβ plaques and neurofibrillary tangles) in
in the past decade—including mouse models genetically this autopsy cohort. However, these excep tionally low
engineered to express human APOE alleles, virally Alzheimer’s disease ORs in APOE ε2 homozygotes were
mediated gene transfer, proteomics and transcriptomics, not found in the larger clinically defined but neuropathol
patient-derived human-induced pluripotent stem cells, ogically unconfirmed group (23 857 individuals; 10 430 with
plasma, CSF, PET, and MRI biomarkers—have impli probable Alzheimer’s disease and 13 426 cog n
itively
cated APOE in other aspects of Alzheimer’s disease unimpaired), suggest ing a stronger pro tection against
pathophysiology, such as tau-induced neurodegeneration, Alzheimer’s disease neuropathology.
microglial and astrocyte react ions (including neuro
inflammation), and blood–brain barrier disruption. Last, APOE Christchurch mutation
although no APOE-based therapy is yet available, several A single case report27 described an approximately 70-year-
APOE-directed therapeutic approaches have been shown old Colombian woman who, despite carrying a fully
68 www.thelancet.com/neurology Vol 20 January 2021
Review
penetrant autosomal-dominant E280A mutation in
PSEN1, which is linked to familial Alzheimer’s dis
ease, and abundant fibrillar Aβ deposits in her PET scan,
remained cognitively healthy well beyond her expected Panel 1: APOE basic facts
year of symptom onset (age 44 years). After whole exome • Two single nucleotide polymorphisms—rs429358 and
sequencing, it was concluded that a rare homozygous rs7412—define the three alleles of APOE, located in
APOE ε3 Christchurch (R136S) mutation conferred her chromosome 19q13·2: ε2, ε3, and ε4. Relative to the most
resilience to Alzheimer’s disease. Mechanistically, the common APOEε3 homozygous genotype (reference
APOE3 R136S mutation appears to inhibit Aβ oligo group), possessing one APOE ε4 allele increases the risk of
merisation, disrupt APOE binding to low-density lipo developing Alzheimer’s disease by approximately
protein receptor, and interfere with APOE affinity for 3·7 times and being homozygous for the APOE ε4 allele
heparan sul fate proteo
glycans, which are involved in increases the risk up to 12 times, whereas carrying a single
toxic tau uptake by neurons, perhaps explaining the lower APOE ε2 allele reduces the risk by approximately 40%,
than average radioligand uptake observed in her tau and being homozygous for APOEε2 reduces the risk
PET scan.27 even further.2,3
• Besides Alzheimer’s disease risk, the APOE genotype
Other genetic modifiers mainly affects the age of onset of cognitive impairment,
A meta-analysis of 22 studies28 has revealed that with APOEε4 carriers having an earlier age of onset and
KLOTHO-VS heterozygosity—a polymorphism previously APOEε2 carriers a later age of onset than APOEε3
associated with longevity—might attenuate the increased homozygotes. By contrast, the effect of APOE genotype
Alzheimer’s disease risk associated with the APOE ε4 on the rate of cognitive decline after symptom onset
allele, because APOE ε4 carriers older than 60 years with remains controversial, with allele differences typically
KLOTHO-VS heterozygosity had a reduced Alzheimer’s considered not clinically relevant.4
disease risk (OR 0·75 [95% CI 0·67–0·84]; p=7·4×10-⁷), • APOE is a 299-amino acid (MW 34 kDa) secreted
reduced risk of conversion from mild cognitive impair glycoprotein that binds cholesterol and phospholipids
ment to dementia (hazard ratio [HR] 0·64 [95% CI through the C-terminus domain and to its receptors
0·44–0·94]; p=0·02], higher CSF Aβ levels, and lower through the N-terminus domain.5
Aβ PET burden; the results were significant specifically • The three APOE isoforms differ in two amino acid
in the group of individuals aged 60–80 years. A whole residues at positions 112 (Cys in APOE2 and APOE3, and
genome sequencing on a mainland Chinese cohort Arg in APOE4) and 158 (Cys in APOE2, and Arg in APOE3
identified nine potential causal variants in two genes and APOE4), and these polymorphisms cause significant
located in the vicinity of APOE, PVRL2 and APOC1,29 differences across APOE isoforms in both lipid binding
which increased the risk of developing Alzheimer’s disease properties (ie, APOE4 is hypolipidated compared with
independently of the APOE ε4 allele. The risk haplo APOE3 and APOE25,6) and receptor affinities.
types associated with these variants correlated with some • APOE transports lipids packed into HDL-like particles in
Alzheimer’s disease endophenotypes such as worse cogni the brain, or LDL particles in the peripheral blood. APOE
tion, more severe hippocampal atrophy, lower plasma main receptors in the brain are the LRP1, the LDL receptor,
Aβ levels, and higher brain APOE mRNA levels. Another the very LDL receptor, and the apolipoprotein E
analysis of whole genome sequencing data stratified receptor 2, all of which are also Aβ receptors.3,7–9,10
by APOE genotype identified three genes significantly • Lipidation of brain APOE is mediated by ATP-binding
associated with Alzheimer’s disease in APOE ε4 carriers cassette transporters A1 and G1.11–13
only: OR8G5 (p=4·67 × 10–7), IGHV3–7 (p=9·75 × 10–16), and • APOE directly interacts with amyloid β peptide,5,14–17 but
SLC24A3 (p=2·67 × 10–12).30 Conversely, a systematic review there is no solid in-vivo evidence of a direct interaction
investigating the genetic basis of resilience to Alzheimer’s between APOE and tau.18
disease among APOE ε4 homozygotes revealed that • Mouse models to study the effects of APOE isoforms
CASP7 (encoding caspase 7) rs10553596 and SERPINA3 on amyloid β peptide and tau include mice deficient in
(encoding α1-antichymotrypsin) rs4934-A/A polymorph APOE (Apoe knockout) and mice genetically engineered to
isms possibly reduce Alzheimer’s disease risk.31 replace the mouse Apoe with each of the human
APOE alleles (APOE-targeted replacement or knock-in),
Influence of race in APOE-linked Alzheimer’s disease risk crossed with either mice overexpressing one or more
An interaction between race and the effect of APOE geno familial Alzheimer’s disease-linked APP mutations—
type on Alzheimer’s disease risk has long been known, with or without one or more PSEN1 mutations
with African American and Hispanic APOE ε4 carriers (eg, APPV717F, 19,20 APPswePSEN1dE9,21,22 5xFAD,23
having a lower risk than white APOE ε4 carriers, and Asian APPPS1–21)21,24—or mice overexpressing frontotemporal
(ie, Japanese) carriers having the highest ORs.32–34 Studies lobar degeneration-tau-linked MAPT mutations
have found that the local ancestry of APOE (ie, the (eg, MAPTP301S).25,26
population-specific genetic variation within the APOE
www.thelancet.com/neurology Vol 20 January 2021 69
Review
Alzheimer’s disease (ie, mild cognitive impairment and
A Plaque Aβ plaque B Capillary CAA
core Endothelial cell mild-to-moderate dementia).39,40 The APOE ε4 allele has
Anti-APOE
ASOs also been associated with more severe tau pathology as
defined by Braak neurofibrillary tangles stages,2,41 and the
Astrocyte APOE ε2 allele with a lower Braak neurofibrillary tangles
Microglia stage,2,4 independently of their effects on Aβ plaques.
Pericyte Cross-sectional data on tau PET imaging examining
APOE effects on tau radioligand uptake after controlling
ABCA1
and RXR ABCA1 Anti-APOE for Aβ radioligand uptake are conflicting,42,43 but longi
agonists antibodies Unlipidated tudinal combined tau and Aβ PET studies will elucidate
APOE4
C Lipidated this important question.
APOE4
Gene
APOE4 The APOE genotype can also affect the finding of
LRP1
therapy
TREM2 comorbid brain pathologies at autopsy. On one hand,
APOE2
Soluble tau APOE ε4 partly drives (together with ageing) the presence
Neuron Soluble Aβ of Aβ plaques and neurofibrillary tangles in individuals
Neurofibrillary
Aβ fibrils
tangle with other primary neuropathological diagnoses such as
Synapse Tau fibrils
amyotrophic lateral sclerosis, primary tauopathies, and
Figure: Multifaceted effects of APOE in the brain and potential strategies to decrease APOE4 and increase Lewy body diseases.44 On the other hand, in individuals
APOE2 levels
In the healthy brain, APOE is expressed and secreted predominantly by astrocytes, and to a lesser extent by with Alzheimer’s disease the APOE ε4 allele appears
microglia. Most brain APOE is lipidated by the ATP-binding cassettes A1 (ABCA1) and G1 (ABCG1) and lipidated to correlate with the presence and severity of TDP-43
APOE is internalised via APOE receptors such low-density lipoprotein receptor-related protein 1 (LRP1), which is pathology,41,45 Lewy body diseases,46 and possibly cerebrovas
expressed in astrocytes, neurons, vascular smooth muscle cells, endothelial cells, and pericytes. In the Alzheimer’s
cular disease,47 independently of its effects on Aβ plaques
disease brain, astrocytes and microglia react to (A) dense-core Aβ plaques,52 (B) cerebral amyloid angiopathy-
laden arteries and capillaries, and (C) neurofibrillary tangles, activating transcriptional programmes that include and neurofibrillary tangles. Lastly, APOE could be a genetic
APOE mRNA up-regulation in microglia53,54 and down-regulation in astrocytes53,55 and lead to altered lipid risk factor for neurodegenerative diseases other than
metabolism (not shown). APOE directly interacts with both soluble and fibrillar Aβ.3 Relative to APOE3 and Alzheimer’s disease. Indeed, APOE ε4 has been associated
APOE2, APOE4 promotes Aβ seeding and aggregation in oligomers and fibrils14,15,56 and reduces its clearance from
with Lewy body diseases, independently of the Aβ plaque
the interstitial fluid,20 potentially leading to Aβ deposition as dense-core (thioflavin-S positive) amyloid plaques
and cerebral amyloid angiopathy together with APOE.3 This evidence suggests that decreasing APOE (especially and neurofibrillary tangle burdens.48,49,50 Of note, APOE ε4
APOE4) expression or blocking the effects of APOE4 or enhancing the effects APOE2 would be beneficial has been associated with an earlier age of symptom onset
(dashed boxes). Experimental approaches to achieving these outcomes include lowering APOE4 levels with in patients with MAPT-linked or autopsy-proven fronto
isoform-specific antisense oligonucleotides24 or antibodies,57–59 which could also target lipid-poor APOE associated
temporal lobar degeneration-tau indepen dently of its
with plaques.59 Alternatively, APOE4 could be switched to APOE3 or APOE2,60 or APOE2 could be added,6,22 with
gene therapy. Last, APOE lipidation could be enhanced with RXR61–63 and ABCA1 or ABCG113 agonists to improve effects on Aβ plaque burden,51 and with more severe neu
APOE4 receptor-mediated internalisation and lower Aβ in the interstitial fluid. Dashed boxes illustrate the most rodegeneration at post-mortem examination in primary
promising therapeutic approaches. ASO=antisense oligonucleotides. Aβ=amyloid-β peptide. CAA=cerebral tauopathies.25 Paradoxically, APOE ε2 might increase the
amyloid angiopathy. TREM2=triggering receptor expressed in myeloid cells 2. RXR=retinoid X receptor. Adapted
from Servier Medical Art by Servier, which is licensed under a CC BY 3.0 licence.
risk of progressive supranuclear palsy,18 but results are
conflicting.46 The validation and expansion of PET imaging
and CSF biomarkers for other neurodegenerative diseases
region), rather than global ancestry (ie, the population- will help to confirm these correlations between APOE
specific genetic variation in the entire genome) or genotype and non-Alzheimer’s pathologies.
environmental fac tors, explains these inter-racial differ
ences in Alzheimer’s disease risk.35–38 Speci fically, an APOE pathophysiological mechanisms
African local ancestry region surrounding APOE underlies Although traditionally the APOE ε4 allele was represented
the smaller APOE ε4 allele effect on Alzheimer’s disease as a trigger of Aβ accumulation at the top of the sporadic
risk observed in African American and Caribbean Hispanic Alzheimer’s disease amyloid cascade, numerous new data
(from Puerto Rico) popula tions.35,36 Another study of show that the APOE alleles have differential downstream
809 individuals identified a potentially protective African effects in many other pathophysiological processes beyond
ancestral haplotype within APOE defined by the rs769449 Aβ metabolism (figure).
SNP,37 but this was not confirmed in a larger (7997 indi
viduals) study.38 Cellular sources of APOE in brains with and without
Alzheimer’s disease
New pathological correlates of APOE genotype Brain and peripheral pools of APOE are independent from
The classic post-mortem neuropathological correlates of each other because liver transplantation changes APOE
the APOE genotype are a higher Aβ plaque burden and isoforms towards the donor’s in the recipient’s blood but
more severe cerebral amyloid angiopathy in APOE ε4 not CSF,64 and depleting APOE from hepatocytes—its
carriers, and a lower Aβ plaque burden in APOE ε2 main source cell type in the periphery—does not affect
carriers, relative to APOE ε3 homozygotes.4 These differ brain APOE (or Aβ) levels in mice.64 Understanding the
ential effects of APOE alleles have been confirmed by cell types expressing APOE in the brain is relevant because
Aβ PET imaging across preclinical and clinical stages of APOE is a secreted glycoprotein and could have autocrine
70 www.thelancet.com/neurology Vol 20 January 2021
Review
effects on the secreting cell, but also paracrine effects on Aβ metabolism remains debated. On one hand, it has been
neighbouring cells. Although astrocytes are the main proposed that APOE and Aβ direct interaction in the brain
source of APOE in the normal brain, in the Alzheimer’s extracellular space might be negligible in physiological
disease brain reactive astrocytes around Aβ plaques were conditions (ie, Aβ monomers and lipidated APOE), but
reported to be devoid of APOE, whereas Aβ plaque- that both APOE and Aβ can compete for the same
associated microglia express high levels of APOE66 receptors, namely LRP1,16 which is involved in Aβ clearance
(figure). Single nuclei RNA-sequencing studies in human by neurons,7 astrocytes,8 endothelial cells, vascular smooth
Alzheimer’s disease and control brains have confirmed a muscle cells,9 and pericytes.72 On the other hand, there is
down-regulation of APOE expression in reactive astro evidence supporting a direct interaction between APOE
cytes53,55 and an up-regulation in activated microglia.53,54,67 and oligomeric and fibrillar Aβ. First, APOE colocalises
Neuropathological studies also reported APOE staining in with synaptotoxic Aβ oligomers at the synapses in the
pyramidal neurons in neurodegenerating areas such as vicinity of Aβ plaques and leads to synapse loss in an
the hippocampus, but rare colocalisation between APOE isoform-dependent manner (APOE4 more than APOE3).55
and tangles, suggesting little direct interaction between Second, in-vivo experiments in which APOE expression by
APOE and tau.3,67 The presence of APOE in pyramidal neu astrocytes was conditionally deleted, or APOE expression
rons suggested the internalisation of APOE lipoparticles globally silenced with antisense oligonucleotides at differ
from the interstitial space through the APOE receptor ent stages of Aβ deposition, have shown that APOE influ
LRP1 (panel 1, figure),67 which is highly expressed in ences Aβ plaque burden mainly during the seeding phase
neurons among other cell types. Expression of APOE has of Aβ aggregation, but has a lesser effect during the
also been shown in vascular cells from the human brain, exponential growth phase (ie, when fibrillar Aβ deposits
specifically pericytes.68 are already formed).56,24 Third, a subtle difference in tertiary
conformation across APOE isoforms (ie, closer N-terminus
Effects on Aβ and C-terminus in APOE4 vs APOE3 and more open in
The disparate effects of APOE isoforms on Alzheimer’s APOE2) could affect both the affinity of the Aβ and APOE
disease risk was attributed to a differential effect— interaction (higher for APOE4 vs APOE3 and APOE2) and
deleterious for APOE4 and protective for APOE2, with the APOE propensity to enzymatic cleavage in its hinge
respect to APOE3—on both Aβ plaque burden and cere region between the N-terminus and the C-terminus,
bral amyloid angiopathy severity.4 These well established rendering presumably toxic C-terminal frag ments (also
autopsy neuropathological correlates of APOE alleles higher for APOE4 vs APOE3 and APOE2).4,17,58
and the early observation that compact (dense-core, fib
rillar, thioflavin-S-positive), but not diffuse (amorphous, Effects on tau
thioflavin-S-negative), Aβ plaques contain APOE,3 sup Unlike Aβ, there is little overlap between APOE-immuno
ported the idea that APOE interacts with Aβ and pro reactive neurons and neurons that have neurofibrillary
motes its aggregation and deposition in insoluble fibrillar tangles.67 No direct interaction between APOE (primarily
deposits (figure).3 Indeed, genetic deletion and haplo secreted) and the microtubule-associated protein tau
insufficiency of APOE reduces dense-core Aβ plaque bur (primarily intraneuronal and axonal) has been shown in
den in various mouse models of cerebral β amyloidosis.21,69,70 vivo.30 However, studies25,26 in transgenic Apoe knockout or
Of note, APOE deficiency inhibits diffuse Aβ deposits in APOE knock-in mice overexpressing the P301S mutant
some of these models,69 but increases them in others,21 form of tau have shown that the human APOE isoforms
further reinforcing the requirement of APOE for plaque do affect tau downstream pathology. Specifically, APOE4
compaction. When these Aβ-plaque depositing mice were promotes tau-induced neurodegeneration and atrophy
crossed with APOE targeted replacement mice expressing compared with APOE3, whereas APOE2 is protective
human APOE alleles in place of the murine Apoe coding with respect to these outcomes.25 The mechanism under
sequence (knock-in mice; panel 1), APOE4 knock-in mice lying these effects is indirect, mediated by APOE effects
consistently exhibited higher Aβ plaque burden than did on microglia, rather than a direct interaction between
APOE3 knock-in mice, and these APOE3 knock-in mice APOE and tau; transcriptome profiling and cytokine
had higher Aβ plaque burden than did APOE2 knock- measures indicate that APOE4 microglia is primed
in mice,19,20,23 thus recapitulating the allele-specific differ towards a proinflam matory phenotype compared with
ences observed in human post-mortem autopsy and Aβ APOE3, whereas APOE2 exhibits a more homeostatic
PET studies.4,39,40 phenotype.25,75 Of note, LRP1 has been shown to be a
In-vitro and in-vivo studies have shown that, relative to receptor for tau uptake by neurons, and APOE affects the
APOE2 and APOE3, APOE4 promotes the seeding of ability of tau to bind LRP1 (figure), although in vitro all
Aβ peptide into Aβ oligomers, protofibrils, and fibrils,14,15,56 APOE isoforms reduced tau uptake to a similar extent.75
but also inhibits Aβ clearance from the brain prolong Additionally, knocking down neuronal LRP1 reduced
ing its half-life in the interstitial fluid20,56 and inhibiting neuronal tau spreading in mice, but some astrocytes took
its enzymatic degradation.71 The intimate mechanism up the human tau.75 Whether different receptors have
underlying these APOE isoform-driven differences in a role in tau uptake into different cell types remains
www.thelancet.com/neurology Vol 20 January 2021 71
Review
unknown. Moreover, since LRP1 is a recycling receptor haemor rhage and cortical superficial side rosis, cortical
delivered into endosomal or lysosomal compartments, it microinfarcts, and white matter ischaemic changes.
remains not clear how tau escapes to the cytoplasm to APOE ε4 effects on the blood–brain barrier were also
interact with endogenous tau in neurons or to accumulate shown in the first randomised clinical trials with anti-Aβ
as glial fibrillary tangles in astrocytes, but it is plausible monoclonal antibodies,84 which reported a higher inci
that APOE affects tau intra cellular trafficking in an dence of MRI findings (brain oedema, microbleeds, and
isoform-dependent manner.76 cortical superficial siderosis) in the treatment versus pla
cebo groups—collectively termed amyloid-related imag
Effects on glia ing abnormalities.84 Only occasion ally symptomatic
Astrocytes and microglia are known to react to plaques, (eg, headaches, confusion, and seizures), these amyloid-
neurofibrillary tangles, and neurodegeneration. Although related imaging abnormalities are indicative of an
quantitation of reactive (GFAP+) astrocytes and activated increased blood–brain barrier per meability presumably
(IBA1+, CD68+) microglia per Aβ plaque in post-mortem caused by the antibody-mediated Aβ efflux from the brain
sections of the temporal neocortex has shown no dif paren chyma into the blood stream.84 Because amyloid-
ference between APOE ε4 carriers and non-carriers,52 related imaging abnormalities are twice as probable in
transcriptomic studies60,77 have reported that APOE influ APOE ε4 carriers, their occurrence has been attributed to
ences glia reactions. Microglia from APOE4 knock-in a more severe pre-existing cerebral amyloid angiopathy in
mice is primed towards a proinflammatory response APOE ε4 carriers vs APOE ε3 homozygotes.84 Supporting
compared with those from APOE3 knock-in mice77 and this inter pretation, immu no
therapy with an anti-Aβ
APOE ε4 microglia derived from human-induced pluri monoclonal antibody is associated with higher numbers
potent stem cells exhibit a proinflammatory gene expres of cerebral microbleeds in APPswePSEN1dE9 x APOE4
sion programme and impaired Aβ phagocytosis relative to knock-in mice versus APOE3 knock-in and APOE2 knock-
APOE ε3 microglia.60 These APOE-mediated differential in mice.85 A post-mortem quantitative neuropathological
effects on microglia phenotype appear to be at least study86 on individuals who participated in a phase 2
partially mediated by the triggering receptor expressed on anti-Aβ active immunotherapy trial (NCT00021723) also
myeloid cells 2 (TREM2), which is another receptor for showed that Aβ plaque clearance is associated with a
both Aβ and APOE expressed by microglia.78 Loss of func redistribution of Aβ and APOE from plaques to vessels,
tion mutations in TREM2 (eg, R47H, R62H) have been and more severe cerebral amy loid angiopathy-related
associated with a 2–3 times increased risk of developing vasculopathic changes. Pericytes, which are another
Alzheimer’s disease and with less compact Aβ plaques cellular source of APOE,68 are gaining attention for their
that have more neuritic dys trophies, less coverage by implication in cerebral amyloid angiopathy pathogenesis
microglia, and less APOE con tent.79 The Aβ plaque (figure). Pericyte loss resulted in increased cerebral
features of Alzheimer’s disease mouse models deficient in amyloid angiopathy severity and Aβ plaques in a mouse
TREM2 or APOE are phenocopies,21,79 suggesting that model of Aβ deposition.87 Pericytes take up Aβ via LRP1
APOE and TREM2 are both involved in chemotaxis of in an APOE isoform-dependent manner, with APOE4
microglia towards plaques and that plaque-associated interfering with this uptake com pared with APOE3.72
microglia has a neuroprotective role minimising neuritic Human APOE ε4 pericytes express higher levels of APOE
dystrophies. The transcriptomic changes associated with mRNA and protein than APOE ε3 pericytes, resulting in
the conversion from homeostatic to Alzheimer’s disease increased Aβ vascular accumulation.68 Pericytes exposed
microglia require both APOE and TREM2 because genetic to Aβ oligomers con strict capil
laries via endothelin-1
deletion of either in Alzheimer’s disease transgenic mice receptor ETA activation, leading to reduced blood flow.88
precludes such transition,80,81 and TREM2 loss of func APOE4 can also increase blood–brain barrier per
tion mutations partially abrogate the microglia transcrip meability with respect to APOE3 in an Aβ-independent
tomic changes observed in the brains of patients with manner, as shown in APOE4 versus APOE3 knock-in
Alzheimer’s disease.54 Regarding APOE effects on astro mice89,90 and confirmed with dynamic contrast-enhanced
cytes, APOE ε4 human-induced pluripotent stem cell- MRI in the medial temporal lobe of cognitively healthy
derived astrocytes exhibit impaired cholesterol metabolism (clinical dementia rating score 0) and mildly impaired
and Aβ phagocytosis,60 reduced neurotrophic support,82 (clinical dementia rating score 0·5) APOE ε4 carriers
and impaired synaptic pruning,83 relative to APOE ε3 and versus APOE ε3 homozygotes.47 The underlying proposed
APOE ε2 astrocytes. mechanisms include the activation of cyclophilin A, result
ing in increased levels of MMP9 and pericyte injury,90
Effects on blood–brain barrier and disruption of the capillary basement membrane (ie,
Another area of growing interest is the effects of APOE ε4 collagen IV).89
allele on the blood–brain barrier. Traditionally, APOE ε4
had been associated with a more severe cerebral amyloid APOE-based therapeutic opportunities
angiopathy (figure), resulting in a higher risk of lobar Experimental in-vivo studies in Alzheimer’s disease mouse
intracerebral haemorrhage, but also focal subarachnoid models that have a human APOE knock-in background
72 www.thelancet.com/neurology Vol 20 January 2021
Review
have suggested promising approaches to amelio rate Increasing APOE levels and its lipidation
phenotypes related to Alzheimer’s disease (table 1). How Because brain APOE4 is less lipidated and stable than are
ever, there are only a few APOE-directed clinical trials APOE3 and APOE2,5,6 increasing brain APOE levels and
completed or underway (table 2), highlighting a lag in lipidation has been proposed as a therapeutic approach.
therapeutic translation for this target. Genetic deletion of ABCA1 results in poor APOE lipidation
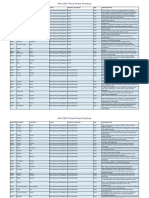
Route Mouse model Age Duration Statistically significant results Comments
Increased APOE levels
Bexarotene61 Oral APPswe/PSEN1dE9 6 and 3, 7, Increased APOE, ABCA1, ABCG1, and Subsequent mouse studies by other
11 months 14, and HDL; reduced soluble or insoluble Aβ groups91–96 yielded mixed results on the
90 days and Aβ plaques; improved memory efficacy of bexarotene on Aβ phenotypes
Bexarotene61 Oral APPPS1‐21 7–8 months 20 days Increased APOE, ABCA1, ABCG1, Subsequent mouse studies by other
and HDL; reduced soluble and groups91 –93 yielded mixed results on the
insoluble Aβ, and Aβ plaques; efficacy of bexarotene on Aβ phenotypes
improved memory
Bexarotene61 Oral Tg2576 12–14 months 3 and Improved social behaviour, olfaction, Subsequent mouse studies by other
9 days and circuit connectivity groups91–93 yielded mixed results on the
efficacy of bexarotene on Aβ phenotypes
CS‐625313 Intraperitoneal APOE3 knock-in; APOE4 2·5 months 6 weeks APOE4 knock-in only: reduced Aβ and ABCA1 agonist derived from
knock-in phosphorylated tau; increased APOE C‐terminus, target engagement
ABCA1, APOE lipidation, APOER2, shown by CS‐6253+ astrocytes in
VGLUT1, and memory immunohistochemistry
Probucol97 Oral Wild-type male rats 26 months 30 days Increased hippocampus APOE, APOE Aged wild-type rats used as a model of
mRNA, HMGCoAR, LRP, and SNAP25; normal cognitive ageing
unchanged cholesterol, LDL receptor,
and synaptophysin; reduced glial
fibrillary acidic protein
Probucol98 Intraperitoneal Wild-type mice, 90 days 2 weeks Reduced plasma cholesterol; Acute intracerebroventricular injection of
intracerebroventricular improved memory and synapses Aβ in wild-type mice is not a faithful
aggregated Aβ 1–40 model of the Alzheimer’s disease scenario
of chronic Aβ accumulation
APOE mimetics
COG141099 Subcutaneous SwDI‐APP/NOS2 knock-out 9 months 3 months Reduced Aβ plaques, phosphorylated SwDI‐APP mice lacking nitric oxide
tau, and interleukin-6 mRNA; synthetase 2 exhibit endogenous tau
improved memory pathology and neuron loss besides
Aβ plaques
COG112100 Intraperitoneal Amyloid-β precursor 1 month 3 months Reduced phosphorylated tau and APP intracellular domain overexpressing
protein intracellular CD45+ and ionised calcium binding mice exhibit microglial activation but no
domain Tg (FeCγ 25 line) adapter molecule-1+ microglia; Aβ plaques
improved neurogenesis
CN‐105101 Subcutaneous APPPS1-21/APOE4 14–18 weeks 40 days Reduced soluble Aβ and Aβ plaques; Greater benefits in young mice
knock-in improved memory (14–18 weeks); for example, improved
CN‐105101 Subcutaneous APPPS1-21/APOE4 25–28 weeks 40 days Unchanged soluble Aβ; improved fear conditioning but not spatial memory
knock-in memory in older mice (25–28 weeks)
Blocking APOE and Aβ interaction
HJ6·3 anti‐APOE Intraperitoneal APPswe/PSEN1dE9 4 months 14 weeks Reduced soluble and insoluble Aβ, Preventative use prior to Aβ plaques
57
antibody Aβ plaques, interferon γ, and very effective compared with therapeutic
interleukin 1α; increased use, microglial activity modulation
CD45+ microglia suggested
HJ6·3 anti‐APOE Intraperitoneal APPswe/PSEN1dE9 7 months 21 weeks Reduced soluble and insoluble Aβ, Therapeutic use after Aβ plaque
antibody58 Aβ plaques, brain APOE, deposition also effective due to inhibition
CD45+ microglia, increased plasma of plaque formation and growth plus
Aβ; improved memory and removal of existing plaques
connectivity; unchanged cerebral
amyloid angiopathy, plasma APOE,
and plasma cholesterol
HAE‐4 anti‐APOE Intracerebroventricular APPPS1‐21/APOE4 2 months 6 weeks Reduced Aβ plaques; unchanged Additionally AAV2/8-mediated expression
antibody59 knock-in insoluble Aβ of HAE‐4 and HAE‐1 anti‐APOE
antibodies via intracerebroventricular
injection at birth reduced Aβ plaque and
insoluble Aβ at age 3·5‐months in a
microglia FcγR1‐dependent manner
(Table 1 continues on next page)
www.thelancet.com/neurology Vol 20 January 2021 73
Review
Route Mouse model Age Duration Statistically significant results Comments
(Continued from previous page)
HAE‐4 anti‐APOE Intraperitoneal APPPS1–21/APOE4 2 months 6 weeks Reduced insoluble Aβ and Aβ Additionally AAV2/8-mediated expression
antibody59 knock-in plaques; unchanged brain soluble of HAE‐4 and HAE‐1 anti‐APOE
and insoluble APOE, plasma APOE, antibodies via intracerebroventricular
and plasma Aβ injection at birth reduced Aβ plaque and
insoluble Aβ at age 3·5 months in a
microglia FcγR1‐dependent manner
Aβ12–28P102 Intraperitoneal APPswe/PSEN1dE9/APOE2 6 months 4 months Reduced soluble and insoluble Aβ, Greater cognitive benefit in APOE4 mice
knock-in; APPswe/ soluble and insoluble APOE, Aβ compared with APOE2 mice because only
PSEN1dE9/APOE4 knock-in plaques, dystrophic neurites, and vehicle‐treated APPswe/PSEN1dE9/
serum cholesterol in both mice; APOE4 knock-in mice (but not
improved memory (only APOE4 APPswe/PSEN1dE9/APOE2 knock-in
knock-in mice); unchanged mice) exhibited impaired cognition
serum APOE
Silencing APOE
Anti‐APOE antisense Intraperitoneal APPPS1–21/APOE3 and Birth 16 weeks Reduced soluble and insoluble Aβ, Reduced Aβ plaque burden when
oligonucleotides24 APPPS1–21/APOE4 Aβ plaques, dystrophic neurites, treated at birth but no change or
knock-in and soluble APOE; unchanged increased when treated at 6 weeks
insoluble APOE suggests preventative rather than
therapeutic use
Anti‐APOE antisense Intracerebroventricular APPPS1‐21/APOE3 and 6 weeks 10 weeks Reduced soluble APOE and Reduced Aβ plaque burden when
oligonucleotides24 APPPS1-21/APOE4 dystrophic neurites; unchanged treated at birth but no change or
knock-in soluble and insoluble Aβ, insoluble increased when treated at 6 weeks
APOE, and CD45+ microglia; suggests preventative rather than
unchanged or increased Aβ plaques therapeutic use
Switching APOE4 to APOE2
AAV4 and APOE2, Intraventricular APPswe/PSEN1dE9 7 months 2 months AAV4-APOE2 vs APOE3: reduced AAV4-mediated expression of APOE2
APOE3, or APOE422 and soluble and insoluble Aβ, Aβ mainly in choroid plexus and
5 months plaques, and dystrophic neurites, ependymal cells via intraventricular
and unchanged plasma Aβ; increased injection can improve Aβ measures in
synapses. AAV4‐APOE4 vs APOE3: aged mice (>12 months old) after
increased soluble and insoluble Aβ, Aβ plaque deposition
Aβ plaques, dystrophic neurites,
and plasma Aβ; reduced synapses
AAV4 and APOE2, Intraventricular Tg2576 16–18 months 3 months AAV4‐APOE2 vs APOE3: AAV4-mediated expression of APOE2
APOE3, or APOE422 reduced interstitial fluid Aβ and mainly in choroid plexus and
oligomeric Aβ, unchanged insoluble ependymal cells via intraventricular
Aβ. AAV4‐APOE4 vs APOE3: injection can improve Aβ measures in
increased interstitial fluid Aβ, aged mice (>12 months old) after
oligomeric Aβ, and insoluble Aβ Aβ plaque deposition
AAV8‐GFAP and Intracerebroventricular APOE3 knock-in and Birth 3 months AAV8-GFAP‐APOE2 vs APOE3: Results suggest that APOE4 is less
APOE2, APOE3, or APOE4 knock-in increased APOE and APOE lipidated and stable than APOE2, and
APOE46 lipidation; reduced mouse Aβ 40 that exogenous expression of APOE4 in
(trend in APOE4 knock-in only); APOE4 carriers could be deleterious by
unchanged APP‐full length, increasing endogenous Aβ, whereas
APP‐CTFs, ABCA1, ABCG1, and expression of APOE2 in APOE4 carriers
Apoe mRNA. AAV8‐GFAP‐APOE4 vs would have opposing beneficial effects
APOE3: increased mouse Aβ 40
(APOE4 knock-in mice only); reduced
APOE lipidation; unchanged APP‐FL,
APP‐CTFs, ABCA1, ABCG1, APOE and
Apoe mRNA.
APPswe=Swedish APP mutation (K670N/M671L). PSEN1dE9=presenilin-1 exon 9 deletion. APPPS1-21=Swedish APP mutation (K670N/M671L) and presenilin-1 L166P mutation. Tg2576=transgenic Swedish
(K670N/M671L) APP mutation overexpressing mice. APOER2=Apolipoprotein E receptor 2. SwDI-APP=Swedish (K670N/M671L), Dutch (E693Q) and Iowa (D694N) APP mutation. AAV4=adeno-associated virus
type-4. AAV8=Adeno-associated virus type-8. APP-FL=APP full length; APPswePSEN1dE9=Swedish APP mutation (K670N/M671L) and presenilin-1 exon 9 deletion; FcγR1=Fc gamma receptor-1.
AAV2/8=Adeno-associated virus type 2/8. APOER2=APOE receptor 2.
Table 1: Summary of APOE-directed therapeutic approaches tested in Alzheimer’s disease mouse models
and increased Aβ plaque burden,11 whereas ABCA1 over cause a rapid reduction of Aβ plaque burden and restora
expression reduces Aβ deposition.12 ABCA1 and ABCG1 tion of cognitive functioning in Alzheimer’s disease
expression is induced by the stimulation of the reti mouse models by inducing ABCA1 and ABCG1 expres
noid X receptor. Bexarotene is a US Food and Drug sion, enhancing APOE lipidation, and increasing APOE
Administration approved retinoid X receptor agonist for levels (table 1).61 This result was, at least partly, replicated
use in cutaneous T-cell lymphoma and was reported to by some investigators but not others, and led to examine
91–96
74 www.thelancet.com/neurology Vol 20 January 2021
Review
Rationale Status Design Phase Participants Dose, route, and Primary Secondary outcomes Results
duration outcome
Bexarotene62 Increase Completed Randomised 1b Young,healthy 225 mg twice daily Newly Fractional clearance Poor bexarotene
APOE levels double‐blind, participants (aged orally for 5 days generated Aβ rate of Aβ from CNS brain penetration
placebo‐ 21–49 years) with in CSF (stable (stable isotope (not detectable in
controlled trial APOE ε3 isotope labelling kinetics) >95% CSF samples),
homozygosity labelling 25% increase in CSF
kinetics) APOE levels, non
significant (p=0·054)
increase in newly
synthesised APOE,
no change in
Aβ synthesis or
clearance levels
Bexarotene63 Increase Completed Randomised, 2 Participants with 150 mg twice daily Aβ burden in Cognition (Mini Mental Significant reduction
APOE levels double-blind, moderate Alzheimer’s orally for 4 weeks amyloid PET State Examination, in Aβ burden only in
placebo‐ disease (Mini Mental imaging Alzheimer’s Disease APOE ε4 non‐carriers
controlled trial State Examination; Assessment which correlated
range 10–20) with Scale-Cognitive with increased serum
positive baseline subscale, clinical Aβ 42 levels,
amyloid PET scan dementia rating scale), increased triglyceride
behaviour plasma level in
(Neuropsychiatric bexarotene group,
Inventory), Activities of no efficacy in
Daily Living, serum clinical outcomes
Aβ 40/42
Probucol Increase Completed Open label, 1/2 Cognitively healthy Initial 600 mg once Plasma No outcomes reported Not available
(NCT02707458) APOE levels dose finding participants at risk of daily orally, then probucol, CSF (study not published)
trial Alzheimer’s disease individualised, 1 year and plasma
by family history of follow‐up APOE levels
CN‐105 APOE Recruiting Randomised, 2 Adults aged ≥60 who 0·1 mg/kg vs Safety CSF cytokine levels, Not available
(NCT03802396) mimetic double-blind, are having major 0·5 mg/kg vs change in cognition, (study ongoing)
placebo‐ surgery 1 mg/kg incidence of
controlled trial intravenously every postoperative delirium
6 h for 4 days and
6 weeks of follow‐up
Gene therapy Switch Recruiting Open label, 1 Symptomatic Single intracisternal Safety Maximum dose Not available
(AAVrh.10hPOE2 APOE4 to dose ranging participants (any injection 8 × 10¹⁰ tolerated (study is ongoing)
vector; APOE2 trial stage), APOEε4 genome copies per kg
NCT03634007) homozygotes, vs 2·5 × 10¹¹ genome
positive copies per kg vs
CSF biomarkers, or 8 × 10¹¹ genome
amyloid PET scan copies per kg, and
2 years of follow-up
Aβ=amyloid β.
Table 2: Early development of APOE-directed therapeutic approaches in human clinical trials
bexarotene for Alzheimer’s disease in human clinical APOE lipidation without changing brain APOE levels, in
trials. A phase 1b proof-of-mechanism trial62 in young APOE4 but not APOE3 knock-in mice.13 These effects
(21–49 years) volunteers revealed poor penetration of correlated with a reduction of hippo campal Aβ and
bexarotene in the CNS according to its plasma versus CSF phosphorylated tau and improved learning and memory in
levels. Bexarotene was able to increase CSF APOE levels APOE4 knock-in mice.13
by 25%, although it had no effects on CSF Aβ levels as Probucol, the now abandoned non-statin lipid-lowering
measured by stable isotope labelling kinetics (table 2). In a drug, has been shown to counteract hippocampal synaptic
proof of concept, double-blind, placebo-controlled clinical loss and cognitive impairment in Aβ-injected wild-type
trial63 in 20 patients with moderate Alzheimer’s disease mice,98 increase APOE and LRP1 levels in the hippocampus
(Mini Mental State Examination range was 10–20; table 2), of aged rats97 and, while results from a phase 1/2 clini
bexarotene 150 mg twice daily for 4 weeks was associated cal trial (NCT02707458) are awaited, might also increase
with a significant reduction in Aβ PET bur den and a CSF APOE levels in humans (table 2).103
proportional increase in serum Aβ42 levels but, contrary to
the prediction, only in APOE ε4 non-carriers. Blocking APOE and Aβ interaction
A derived from the C-terminus of APOE, CS-6253, has Another therapeutic strategy is to interfere with the APOE
been shown to increase ABCA1 levels and, subsequently, and Aβ interaction, because this is thought to stabilise
www.thelancet.com/neurology Vol 20 January 2021 75
Review
toxic oligomeric and fibrillar Aβ species existing within Lowering APOE levels
and around Aβ plaques.14,15,56,73 This strategy has been Lowering brain APOE levels has also been proposed as a
achieved in Alzheimer’s disease mouse models with both therapy because Apoe genetic deletion or haploinsuf
monoclonal anti-APOE antibodies and small molecules ficiency reduces Aβ deposition in mouse models of
that act as Aβ mimetics. cerebral β-amyloidosis69,70,21 and rescues neurodegenera
Chronic intraperitoneal administration of an anti-APOE tion induced by tau in tauopathy mouse models.25 Addi
monoclonal antibody (HJ6·3) to APPswePSEN1dE9 trans tionally, null mutations in the APOE gene do not seem to
genic mice led to a statistically significant reduction of have adverse effects on cognition in humans, although
insoluble Aβ levels and Aβ plaque burden, and APOE they are associated with familial dysbetalipoproteinemia
levels in the brain, which correlated with improved learn (also known as type III hyperlipoproteinemia).104 One way
ing and memory and higher cortical network connectivity of reducing brain APOE levels is increasing the expres
in the resting state.57,58 While the Aβ plaque reduction was sion of its receptors. Over-expression of LDLR reduced
larger when administered before plaque deposition, Aβ plaque deposition105 due to increased efflux of Aβ from
in older mice with substantial plaque deposition this the brain through the blood–brain barrier.10 A more specific
antibody appears to prevent the formation of new plaques approach is to silence APOE expression with specific anti
and clear the smallest previously existing plaques by sense oligonucleotides. In APPPS1-21 x APOE3 knock-in
binding APOE within them.57,58 Of note, systemic treat mouse and APPPS1-21 x APOE4 knock-in mice, a reduction
ment with this anti-APOE antibody increased plasma in soluble APOE concentrations by half with anti-APOE
Aβ levels, but did not have systemic (ie, unchanged plasma antisense oligonucleotides resulted in lower soluble and
cholesterol and APOE levels) or local (ie, cerebral amyloid insoluble Aβ levels and lower total and dense-core plaque
angiopathy did not worsen) adverse side-effects.57,58 burden when adminis tered intracerebroventricularly at
Another anti-APOE monoclonal antibody specific for non- birth, but did not change much these Aβ measures
lipidated APOE (HAE-4) reduced the plaque burden in when applied at the onset of Aβ plaque deposition (ie,
APPPS1-21 x APOE4 knock-in mice through microglia- 6 weeks in this mouse model).24 However, both treatments
mediated clearance, without affecting the levels of plasma resulted in fewer plaque-associated dystrophic neurites,
APOE, which is mostly lipidated.59 Therefore, anti-APOE suggesting less neuronal toxicity of existing plaques
immunotherapy has promise for testing in future trials. and some beneficial effect of APOE reduction on micro
Aβ12–28P, a small peptide corresponding to the APOE- glia and astrocyte responses to plaques, and lending
binding motif within Aβ except for a Val18Pro substitution, support for testing in patients with Alzheimer’s disease in
reduced soluble and insoluble Aβ levels and Aβ plaque clinical trials.
burden in APPswePSEN1dE9 x APOE4 knock-in mice and
APPswePSEN1dE9 x APOE3 knock-in mice and improved Genetic switch of APOE isoforms
memory deficits in APPswePSEN1dE9 x APOE4 knock-in Gene therapy has become a reality in several diseases,
mice.102 Moreover, Aβ12–28P reduced soluble and insoluble including neurodegenerative diseases such as spinal
APOE levels and the deposition of APOE into Aβ plaques. muscular atrophy. The application of CRISPR-Cas9 edit
Of note, this improve ment was not due to an active ing technology to switch APOE alleles has been success
immunisation effect, because these mice did not generate ful in a dish with neurons and glial cells derived from
antibodies against this Aβ fragment.102 Aβ12–28P efficacy human-induced pluripotent stem cells,60 but remains
remains to be tested in clinical trials. to be shown in APOE knock-in mice. However, the
application of gene therapy to express APOE ε2 and
APOE mimetics increase APOE2 levels in APOE ε4 carriers (or even
Another approach is to use APOE N-terminal frag APOE ε3 homozygotes) has become feasible and the first
ments that include its receptor-binding motif, so called phase 1 clinical trial with this approach has been initi
APOE mimetics. Chronic subcutaneous administration of ated (NCT03634007; table 2). In mice, intraventricular
CN-105, a pentapeptide corresponding to the recep tor transfer of human APOE alleles with an adeno-associated
binding face of APOE, reduced both soluble Aβ and Aβ virus type-4 leads to sustained expression of human
plaque burden and improved cognition in APPS1-21 x APOE in the choroid plexus and ependymal cell lining,
APOE4 knock-in mice before plaque deposition, but not that diffuses to the brain parenchyma reaching a con
after this.101 CN-105 is being tested to prevent delirium after centration of 10% of mouse endogenous APOE.22 Adeno-
major surgery in a phase 2 clinical trial (NCT03802396; associated virus type-4-mediated delivery and expression
table 2). APOE mimetics spanning the APOE recep of APOE ε2 in 7-month-old APPswePSEN1dE9 mice
tor binding motif such as COG1410 (12 amino acids) and (ie, after Aβ plaque deposition) resulted in reduced
COG112 (34 amino acids) have also been shown to soluble and insoluble Aβ levels and enhanced plaque
ameliorate Aβ levels and Aβ plaque burden, tau hyper clearance, whereas delivery of APOE ε4 had the opposite
phosphorylation, and neuroinflammation in various effects.22 Plasma Aβ40 concentrations were decreased in
Alzheimer’s disease mouse models,99,100 but have not been the APOE ε3 and APOE ε4 treated mice versus APOE ε2
tested in human clinical trials. treated mice,22 suggesting a reduced efflux from brain
76 www.thelancet.com/neurology Vol 20 January 2021
Review
Panel 2: Areas of uncertainty and research priorities Search strategy and selection criteria
• Possible differential independent effects of APOE alleles We searched PubMed for articles in English published between
on Alzheimer’s disease progression through preclinical Jan 1, 1993, and May 15, 2020, using the search terms
and clinical stages with longitudinal multimodal imaging, “APOE AND Alzheimer’s disease”, “APOE AND blood-brain
CSF, and plasma or serum biomarkers barrier”, “APOE AND Lewy body disease”, “APOE AND
• Influence of genetic modifiers of APOE-linked Alzheimer’s alpha-synuclein”, “APOE AND TAR DNA-binding protein 43”,
disease risk, including the intimate mechanisms of local “APOE AND tau”, “APOE AND microglia”, “APOE AND
ancestry, interaction with longevity genetic astrocytes”, “APOE AND TREM2”, “APOE AND
polymorphisms such as KLOTHO-VS heterozygosity, and immunotherapy”, and “APOE AND gene therapy”. Only human,
APOE mutations such as R136S (Christchurch), mouse model, and human-induced pluripotent stem-cell
as plausible substrates of resistance or resilience to studies were reviewed. In-vitro studies using recombinant
Alzheimer’s disease APOE and synthetic or recombinant Aβ or tau species and
• Possible Aβ-independent mechanisms of APOE on tau in-cellulo studies using cultured cell lines or primary neuron,
seeding and propagation through neuronal circuits astrocyte, or microglial cultures were excluded. The final
• Influence of APOE genotype on other neurodegenerative reference list was generated on the basis of relevance and
proteinopathies, such as primary tauopathies originality with regard to the topics covered in this Review.
(eg, Pick´s disease, progressive supranuclear palsy, and
corticobasal degeneration), TDP-43 proteinopathies
(amyotrophic lateral sclerosis, frontotemporal lobar APOE4 levels and to increase APOE2 levels in the brain
degeneration-TDP-43), and α-synucleinopathies hold the greatest promise (table 2).6,22,24,57,58,59 Against this
(Parkinson’s disease, dementia with Lewy bodies, multiple remarkable momentum, there remains a paucity in trans
system atrophy), as well as on other neurological lation of APOE-based therapies to human clinical trials,
disorders in which the blood–brain barrier or the immune especially when compared with the expedited cases of
system play a substantial role anti-Aβ and anti-tau immunotherapies (table 2).84,86 What
• Autocrine versus paracrine effects of APOE on each brain are the hurdles slowing APOE-based drug development
cell type (astrocytes, microglia, neurons, programmes down? First, further development of small
oligodendrocytes, vascular smooth muscle cells, molecules that reliably change APOE4 conformation to
endothelial cells, and pericytes). APOE3 or APOE2 has proven to be difficult because the
• In-vivo applications of gene therapy, including genetic variable degree of lipidation of APOE might influence its
editing of APOE alleles with CRISPR-Cas9 technology and tertiary conformation.5 Second, the new data implicating a
strategies for viral vector delivery to specific brain variety of non-Aβ and non-tau targets in APOE patho
cell types physiology raises new questions, such as determining
what the best downstream therapeutic target should be
and monitoring the consequences of target engagement.
to plasma through the brain–blood barrier, relative to Third, there are some unique problems related to APOE
APOE ε2 treated mice. Monitoring of Aβ plaque growth separate peripheral (liver generated) and CNS pools and
by in-vivo multiphoton microscopy in living mice showed its inability to cross the blood–brain barrier.64,65 This means
a significant effect on plaque growth rate, slower in that affecting CNS APOE (levels, isoforms, or interac
APOE ε2 treated mice and faster in APOE ε4 treated tions) will require drugs with adequate blood–brain
mice.22 Moreover, APOE ε2 ameliorated plaque-associated barrier penetration. Moreover, potential systemic off-target
dystrophic neurites and synapse loss, which were more adverse effects of some of these approaches should be
severe in APOE ε4 treated mice. Similarly, intracere carefully considered: rare APOE ε2 homozygotes and
broventricular AAV8-mediated astrocyte-specific expres Christchurch mutation carriers,106 and even more rare
sion of human APOE ε2 in APOE4 knock-in mice from individuals with homozygous APOE null mutations104
birth increased APOE lipidation and decreased endog suffer from type III hyperlipoproteinemia resulting in
enous murine Aβ, whereas APOE ε4 delivery had opposite accelerated atherosclerosis; in fact, APOE2 knock-in and
deleterious effects.6 Apoe knockout mice are widely used to model athero
sclerosis. Therefore, gene therapies to lower APOE levels
Conclusions and future directions or switch APOE4 to APOE2 should probably be targeted
New insights in genetic modifiers, neuropathological and specifically to the CNS (ie, via direct injection or with
gene expression correlates, and pathophysiological mech viral capsids that penetrate the blood–brain barrier and
anisms in different brain cell types are broadening our appropriate promoters), which poses its own challenges.
understanding of the implications of APOE in Alzheimer’s Notwithstanding all these barriers, the risk and pro
disease and offering previously unforeseeable oppor tective profiles of APOE genotype in human populations
tunities for therapeutic and preventive interventions. across the globe reinforce the robustness of the effects of
Because of this mounting evidence, strategies to lower subtle variations in this gene, and encourage the field
www.thelancet.com/neurology Vol 20 January 2021 77
Review
to redouble its efforts at further understanding the 15 Hori Y, Hashimoto T, Nomoto H, Hyman BT, Iwatsubo T. Role of
pathophysiology of APOE effects in Alzheimer’s disease apolipoprotein E in β-amyloidogenesis: isoform-specific effects on
protofibril to fibril conversion of aβ in vitro and brain Aβ deposition
(panel 2), and its attempts at translating that knowledge in vivo. J Biol Chem 2015; 290: 15163–74.
into therapeutics. 16 Verghese PB, Castellano JM, Garai K, et al. ApoE influences
amyloid-β (Aβ) clearance despite minimal apoE/Aβ association in
Contributors physiological conditions. Proc Natl Acad Sci USA 2013;
AS-P and SD did the literature search and wrote the manuscript. 110: E1807–16.
BTH reviewed and edited the manuscript. 17 Kara E, Marks JD, Roe AD, et al. A flow cytometry-based in vitro
Declaration of interests assay reveals that formation of apolipoprotein E (ApoE)-amyloid β
BTH receives research funds from AbbVie and F Prime; received complexes depends on ApoE isoform and cell type. J Biol Chem
consultant or science advisory boards honoraria from Arvinas, Biogen, 2018; 293: 13247–56.
Cell Signaling Technology, US Department of Justice, Dewpoint 18 Zhao N, Liu C-C, Van Ingelgom AJ, et al. APOE ε2 is associated
Therapeutics, and Novartis; has a family member who works for with increased tau pathology in primary tauopathy. Nat Commun
2018; 9: 4388.
Novartis and they own Novartis stocks; serves on the Board of Dewpoint
19 Holtzman DM, Bales KR, Tenkova T, et al. Apolipoprotein E
Therapeutics and owns stock; and is funded by the US National Institute
isoform-dependent amyloid deposition and neuritic degeneration in
on Aging (1R01AG047644–01) and the US National Institute of
a mouse model of Alzheimer’s disease. Proc Natl Acad Sci USA
Neurological Disorders and Stroke (U01NS111671–01). AS-P is funded by 2000; 97: 2892–97.
the US National Institute on Aging (K08AG064039) and the Alzheimer’s
20 Castellano JM, Kim J, Stewart FR, et al. Human apoE isoforms
Association (AACF-17–524184). SD is funded by the US National differentially regulate brain amyloid-β peptide clearance.
Institute on Aging (P30AG062421). Sci Transl Med 2011; 3: 89ra57.
Acknowledgments 21 Ulrich JD, Ulland TK, Mahan TE, et al. ApoE facilitates the
We want to thank Ayush Noori, Neurology Department, Massachusetts microglial response to amyloid plaque pathology. J Exp Med 2018;
General Hospital, Boston, MA, USA for his invaluable help preparing 215: 1047–58.
the figure. The funder of the study had no role in data interpretation or 22 Hudry E, Dashkoff J, Roe AD, et al. Gene transfer of human Apoe
writing of the report. isoforms results in differential modulation of amyloid deposition
and neurotoxicity in mouse brain. Sci Transl Med 2013; 5: 212ra161.
References 23 Youmans KL, Tai LM, Nwabuisi-Heath E, et al. APOE4-specific
1 Kunkle BW, Grenier-Boley B, Sims R, et al. Genetic meta-analysis of changes in Aβ accumulation in a new transgenic mouse model of
diagnosed Alzheimer’s disease identifies new risk loci and Alzheimer disease. J Biol Chem 2012; 287: 41774–86.
implicates Aβ, tau, immunity and lipid processing. Nat Genet 2019; 24 Huynh TV, Liao F, Francis CM, et al. Age-dependent effects of
51: 414–30. apoE reduction using antisense oligonucleotides in a model of
2 Reiman EM, Arboleda-Velasquez JF, Quiroz YT, et al. Exceptionally β-amyloidosis. Neuron 2017; 96: 1013–23.e4.
low likelihood of Alzheimer’s dementia in APOE2 homozygotes 25 Shi Y, Yamada K, Liddelow SA, et al. ApoE4 markedly exacerbates
from a 5,000-person neuropathological study. Nat Commun 2020; tau-mediated neurodegeneration in a mouse model of tauopathy.
11: 667. Nature 2017; 549: 523–27.
3 Rebeck GW, Reiter JS, Strickland DK, Hyman BT. Apolipoprotein E 26 Shi Y, Manis M, Long J, et al. Microglia drive APOE-dependent
in sporadic Alzheimer’s disease: allelic variation and receptor neurodegeneration in a tauopathy mouse model. J Exp Med 2019;
interactions. Neuron 1993; 11: 575–80. 216: 2546–61.
4 Serrano-Pozo A, Qian J, Monsell SE, Betensky RA, Hyman BT. 27 Arboleda-Velasquez JF, Lopera F, O’Hare M, et al. Resistance to
APOEε2 is associated with milder clinical and pathological autosomal dominant Alzheimer’s disease in an APOE3
Alzheimer disease. Ann Neurol 2015; 77: 917–29. Christchurch homozygote: a case report. Nat Med 2019; 25: 1680–83.
5 Jones PB, Adams KW, Rozkalne A, et al. Apolipoprotein E: isoform 28 Belloy ME, Napolioni V, Han SS, Le Guen Y, Greicius MD,
specific differences in tertiary structure and interaction with Alzheimer’s Disease Neuroimaging Initiative. Association of
amyloid-β in human Alzheimer brain. PLoS One 2011; 6: e14586. klotho-vs heterozygosity with risk of Alzheimer disease in
6 Hu J, Liu C-C, Chen X-F, Zhang Y-W, Xu H, Bu G. Opposing effects individuals who carry APOE4. JAMA Neurol 2020; 77: 849–62.
of viral mediated brain expression of apolipoprotein E2 (apoE2) and 29 Zhou X, Chen Y, Mok KY, et al. Non-coding variability at the APOE
apoE4 on apoE lipidation and Aβ metabolism in apoE4-targeted locus contributes to the Alzheimer’s risk. Nat Commun 2019;
replacement mice. Mol Neurodegener 2015; 10: 6. 10: 3310.
7 Kanekiyo T, Cirrito JR, Liu C-C, et al. Neuronal clearance of 30 Ma Y, Jun GR, Zhang X, et al. Analysis of whole-exome sequencing
amyloid-β by endocytic receptor LRP1. J Neurosci 2013; 33: 19276–83. data for Alzheimer disease stratified by APOE genotype.
8 Liu C-C, Hu J, Zhao N, et al. Astrocytic LRP1 mediates brain JAMA Neurol 2019; 76:1099–1108.
Aβ clearance and impacts amyloid deposition. J Neurosci 2017; 31 Huq AJ, Fransquet P, Laws SM, et al. Genetic resilience to
37: 4023–31. Alzheimer’s disease in APOE ε4 homozygotes: a systematic review.
9 Kanekiyo T, Liu C-C, Shinohara M, Li J, Bu G. LRP1 in brain Alzheimers Dement 2019; 15: 1612–23.
vascular smooth muscle cells mediates local clearance of 32 Farrer LA, Cupples LA, Haines JL, et al. Effects of age, sex, and
Alzheimer’s amyloid-β. J Neurosci 2012; 32: 16458–65. ethnicity on the association between apolipoprotein E genotype and
10 Castellano JM, Deane R, Gottesdiener AJ, et al. Low-density Alzheimer disease. A meta-analysis. JAMA 1997; 278: 1349–56.
lipoprotein receptor overexpression enhances the rate of 33 Tang MX, Stern Y, Marder K, et al. The APOE-epsilon4 allele and
brain-to-blood Aβ clearance in a mouse model of β-amyloidosis. the risk of Alzheimer disease among African Americans, whites,
Proc Natl Acad Sci USA 2012; 109: 15502–07. and Hispanics. JAMA 1998; 279: 751–55.
11 Wahrle SE, Jiang H, Parsadanian M, et al. Deletion of Abca1 34 Evans DA, Bennett DA, Wilson RS, et al. Incidence of Alzheimer
increases Aβ deposition in the PDAPP transgenic mouse model of disease in a biracial urban community: relation to apolipoprotein E
Alzheimer disease. J Biol Chem 2005; 280: 43236–42. allele status. Arch Neurol 2003; 60: 185–89.
12 Wahrle SE, Jiang H, Parsadanian M, et al. Overexpression of 35 Rajabli F, Feliciano BE, Celis K, et al. Ancestral origin of ApoE ε4
ABCA1 reduces amyloid deposition in the PDAPP mouse model of Alzheimer disease risk in Puerto Rican and African American
Alzheimer disease. J Clin Invest 2008; 118: 671–82. populations. PLoS Genet 2018; 14: e1007791.
13 Boehm-Cagan A, Bar R, Liraz O, Bielicki JK, Johansson JO, 36 Blue EE, Horimoto ARVR, Mukherjee S, Wijsman EM,
Michaelson DM. ABCA1 agonist eeverses the ApoE4-driven Thornton TA. Local ancestry at APOE modifies Alzheimer’s disease
cognitive and brain pathologies. J Alzheimers Dis 2016; 54: 1219–33. risk in Caribbean Hispanics. Alzheimers Dement 2019; 15: 1524–32.
14 Hashimoto T, Serrano-Pozo A, Hori Y, et al. Apolipoprotein E, 37 Babenko VN, Afonnikov DA, Ignatieva EV, Klimov AV, Gusev FE,
especially apolipoprotein E4, increases the oligomerization of Rogaev EI. Haplotype analysis of APOE intragenic SNPs.
amyloid β peptide. J Neurosci 2012; 32: 15181–92. BMC Neurosci 2018; 19 (suppl 1): 16.
78 www.thelancet.com/neurology Vol 20 January 2021
Review
38 Mezlini AM, Magdamo C, Merrill E, et al. Characterizing clinical 61 Cramer PE, Cirrito JR, Wesson DW, et al. ApoE-directed
and neuropathological traits of APOE haplotypes in African therapeutics rapidly clear β-amyloid and reverse deficits in
Americans and Europeans. J Alzheimers Dis JAD 2020; 78: 467–77. AD mouse models. Science 2012; 335: 1503–06.
39 Jansen WJ, Ossenkoppele R, Knol DL, et al. Prevalence of cerebral 62 Ghosal K, Haag M, Verghese PB, et al. A randomized controlled study
amyloid pathology in persons without dementia: a meta-analysis. to evaluate the effect of bexarotene on amyloid-β and apolipoprotein E
JAMA 2015; 313: 1924–38. metabolism in healthy subjects. Alzheimers Dement 2016; 2: 110–20.
40 Ossenkoppele R, Jansen WJ, Rabinovici GD, et al. Prevalence of 63 Cummings JL, Zhong K, Kinney JW, et al. Double-blind,
amyloid PET positivity in dementia syndromes: a meta-analysis. placebo-controlled, proof-of-concept trial of bexarotene Xin
JAMA 2015; 313: 1939–49. moderate Alzheimer’s disease. Alzheimers Res Ther 2016; 8: 4.
41 Wennberg AM, Tosakulwong N, Lesnick TG, et al. Association of 64 Linton MF, Gish R, Hubl ST, et al. Phenotypes of apolipoprotein B
apolipoprotein E ε4 with transactive response DNA-binding and apolipoprotein E after liver transplantation. J Clin Invest 1991;
protein 43. JAMA Neurol 2018; 75: 1347–54. 88: 270–81.
42 Ramanan VK, Castillo AM, Knopman DS, et al. Association of 65 Huynh TV, Wang C, Tran AC, et al. Lack of hepatic apoE does not
apolipoprotein E ε4, educational level, and sex with tau deposition influence early Aβ deposition: observations from a new APOE
and tau-mediated metabolic dysfunction in older adults. knock-in model. Mol Neurodegener 2019; 14: 37.
JAMA Netw Open 2019; 2: e1913909. 66 Uchihara T, Duyckaerts C, He Y, et al. ApoE immunoreactivity and
43 Therriault J, Benedet AL, Pascoal TA, et al. Association of microglial cells in Alzheimer’s disease brain. Neurosci Lett 1995;
apolipoprotein E ε4 with medial temporal tau independent of 195: 5–8.
amyloid-β. JAMA Neurol 2020; 77: 470–79. 67 Han SH, Hulette C, Saunders AM, et al. Apolipoprotein E is present
44 Robinson JL, Lee EB, Xie SX, et al. Neurodegenerative disease in hippocampal neurons without neurofibrillary tangles in
concomitant proteinopathies are prevalent, age-related and Alzheimer’s disease and in age-matched controls. Exp Neurol 1994;
APOE4-associated. Brain 2018; 141: 2181–93. 128: 13–26.
45 Yang H-S, Yu L, White CC, et al. Evaluation of TDP-43 68 Blanchard JW, Bula M, Davila-Velderrain J, et al. Reconstruction of
proteinopathy and hippocampal sclerosis in relation to APOE ε4 the human blood-brain barrier in vitro reveals a pathogenic
haplotype status: a community-based cohort study. Lancet Neurol mechanism of APOE4 in pericytes. Nat Med 2020; 26: 952–63.
2018; 17: 773–81. 69 Holtzman DM, Fagan AM, Mackey B, et al. Apolipoprotein E
46 Sabir MS, Blauwendraat C, Ahmed S, et al. Assessment of APOE facilitates neuritic and cerebrovascular plaque formation in an
in atypical parkinsonism syndromes. Neurobiol Dis 2019; Alzheimer’s disease model. Ann Neurol 2000; 47: 739–47.
127: 142–46. 70 Kim J, Jiang H, Park S, et al. Haploinsufficiency of human APOE
47 Montagne A, Nation DA, Sagare AP, et al. APOE4 leads to blood- reduces amyloid deposition in a mouse model of amyloid-β
brain barrier dysfunction predicting cognitive decline. Nature 2020; amyloidosis. J Neurosci 2011; 31: 18007–12.
581: 71–76. 71 Deane R, Sagare A, Hamm K, et al. ApoE isoform-specific
48 Tsuang D, Leverenz JB, Lopez OL, et al. APOE ε4 increases risk for disruption of amyloid β peptide clearance from mouse brain.
dementia in pure synucleinopathies. JAMA Neurol 2013; 70: 223–28. J Clin Invest 2008; 118: 4002–13.
49 Dickson DW, Heckman MG, Murray ME, et al. APOE ε4 is 72 Ma Q, Zhao Z, Sagare AP, et al. Blood-brain barrier-associated
associated with severity of Lewy body pathology independent of pericytes internalize and clear aggregated amyloid-β42 by
Alzheimer pathology. Neurology 2018; 91: e1182–95. LRP1-dependent apolipoprotein E isoform-specific mechanism.
50 Prokopenko I, Miyakawa G, Zheng B, et al. Alzheimer’s disease Mol Neurodegener 2018; 13: 57.
pathology explains association between dementia with Lewy bodies 73 Koffie RM, Hashimoto T, Tai H-C, et al. Apolipoprotein E4 effects in
and APOE-ε4/TOMM40 long poly-T repeat allele variants. Alzheimer’s disease are mediated by synaptotoxic oligomeric
Alzheimers Dement (N Y) 2019; 5: 814–24. amyloid-β. Brain 2012; 135: 2155–68.
51 Koriath C, Lashley T, Taylor W, et al. ApoE4 lowers age at onset in 74 Kara E, Marks JD, Fan Z, et al. Isoform- and cell type-specific structure
patients with frontotemporal dementia and tauopathy independent of apolipoprotein E lipoparticles as revealed by a novel Forster
of amyloid-β copathology. Alzheimers Dement (Amst) 2019; resonance energy transfer assay. J Biol Chem 2017; 292: 14720–29.
11: 277–80. 75 Rauch JN, Luna G, Guzman E, et al. LRP1 is a master regulator of
52 Serrano-Pozo A, Betensky RA, Frosch MP, Hyman BT. Plaque- tau uptake and spread. Nature 2020; 580: 381–85.
associated local toxicity increases over the clinical course of 76 Xian X, Pohlkamp T, Durakoglugil MS, et al. Reversal of
Alzheimer disease. Am J Pathol 2016; 186: 375–84. ApoE4-induced recycling block as a novel prevention approach for
53 Mathys H, Davila-Velderrain J, Peng Z, et al. Single-cell Alzheimer’s disease. eLife 2018; 7: e40048.
transcriptomic analysis of Alzheimer’s disease. Nature 2019; 77 Zhao N, Ren Y, Yamazaki Y, et al. Alzheimer’s risk factors age,
570: 332–37. APOE genotype, and sex drive distinct molecular pathways.
54 Zhou Y, Song WM, Andhey PS, et al. Human and mouse Neuron 2020; 6: 727–42.
single-nucleus transcriptomics reveal TREM2-dependent and 78 Atagi Y, Liu C-C, Painter MM, et al. Apolipoprotein E is a ligand for
TREM2-independent cellular responses in Alzheimer’s disease. triggering receptor expressed on myeloid cells 2 (TREM2).
Nat Med 2020; 26: 131–42. J Biol Chem 2015; 290: 26043–50.
55 Grubman A, Chew G, Ouyang JF, et al. A single-cell atlas of 79 Parhizkar S, Arzberger T, Brendel M, et al. Loss of TREM2 function
entorhinal cortex from individuals with Alzheimer’s disease reveals increases amyloid seeding but reduces plaque-associated ApoE.
cell-type-specific gene expression regulation. Nat Neurosci 2019; Nat Neurosci 2019; 22: 191–204.
22: 2087–97. 80 Keren-Shaul H, Spinrad A, Weiner A, et al. A unique microglia type
56 Liu C-C, Zhao N, Fu Y, et al. ApoE4 accelerates early seeding of associated with restricting development of Alzheimer’s disease.
amyloid pathology. Neuron 2017; 96: 1024–1032.e3. Cell 2017; 169: 1276–1290.
57 Kim J, Eltorai AEM, Jiang H, et al. Anti-apoE immunotherapy 81 Krasemann S, Madore C, Cialic R, et al. The TREM2-APOE pathway
inhibits amyloid accumulation in a transgenic mouse model of drives the transcriptional phenotype of dysfunctional microglia in
Aβ amyloidosis. J Exp Med 2012; 209: 2149–56. neurodegenerative diseases. Immunity 2017; 47: 566–581.
58 Liao F, Hori Y, Hudry E, et al. Anti-ApoE antibody given after plaque 82 Zhao J, Davis MD, Martens YA, et al. APOE ε4/ε4 diminishes
onset decreases Aβ accumulation and improves brain function in a neurotrophic function of human iPSC-derived astrocytes.
mouse model of Aβ amyloidosis. J Neurosci 2014; 34: 7281–92. Hum Mol Genet 2017; 26: 2690–700.
59 Liao F, Li A, Xiong M, et al. Targeting of nonlipidated, aggregated 83 Chung W-S, Verghese PB, Chakraborty C, et al. Novel allele-
apoE with antibodies inhibits amyloid accumulation. J Clin Invest dependent role for APOE in controlling the rate of synapse pruning
2018; 128: 2144–55. by astrocytes. Proc Natl Acad Sci USA 2016; 113: 10186–91.
60 Lin Y-T, Seo J, Gao F, et al. APOE4 causes widespread molecular 84 Sperling R, Salloway S, Brooks DJ, et al. Amyloid-related imaging
and cellular alterations associated with Alzheimer’s disease abnormalities in patients with Alzheimer’s disease treated with
phenotypes in human iPSC-derived brain cell types. Neuron 2018; bapineuzumab: a retrospective analysis. Lancet Neurol 2012;
98: 1141–1154. 11: 241–49.
www.thelancet.com/neurology Vol 20 January 2021 79
Review
85 Pankiewicz JE, Baquero-Buitrago J, Sanchez S, et al. APOE 97 Champagne D, Pearson D, Dea D, Rochford J, Poirier J.
genotype differentially modulates effects of anti-Aβ, passive The cholesterol-lowering drug probucol increases apolipoprotein E
immunization in APP transgenic mice. Mol Neurodegener 2017; production in the hippocampus of aged rats: implications for
12: 12. Alzheimer’s disease. Neuroscience 2003; 121: 99–110.
86 Sakai K, Boche D, Carare R, et al. Aβ immunotherapy for 98 Santos DB, Peres KC, Ribeiro RP, et al. Probucol, a lipid-lowering
Alzheimer’s disease: effects on apoE and cerebral vasculopathy. drug, prevents cognitive and hippocampal synaptic impairments
Acta Neuropathol 2014; 128: 777–89. induced by amyloid β peptide in mice. Exp Neurol 2012; 233: 767–75.
87 Sagare AP, Bell RD, Zhao Z, et al. Pericyte loss influences 99 Vitek MP, Christensen DJ, Wilcock D, et al. APOE-mimetic
Alzheimer-like neurodegeneration in mice. Nat Commun 2013; peptides reduce behavioral deficits, plaques and tangles in
4: 2932. Alzheimer’s disease transgenics. Neurodegener Dis 2012; 10: 122–26.
88 Nortley R, Korte N, Izquierdo P, et al. Amyloid β oligomers 100 Ghosal K, Stathopoulos A, Thomas D, Phenis D, Vitek MP,
constrict human capillaries in Alzheimer’s disease via signaling to Pimplikar SW. The apolipoprotein-E-mimetic COG112 protects
pericytes. Science 2019; 365: eaav9518. amyloid precursor protein intracellular domain-overexpressing
89 Yamazaki Y, Shinohara M, Yamazaki A, et al. ApoE animals from Alzheimer’s disease-like pathological features.
(Apolipoprotein E) in brain pericytes regulates endothelial function Neurodegener Dis 2013; 12: 51–58.
in an isoform-dependent manner by modulating basement 101 Krishnamurthy K, Cantillana V, Wang H, et al. ApoE mimetic
membrane components. Arterioscler Thromb Vasc Biol 2020; improves pathology and memory in a model of Alzheimer’s disease.
40: 128–44. Brain Res 2020; 1733: 146685.
90 Bell RD, Winkler EA, Singh I, et al. Apolipoprotein E controls 102 Pankiewicz JE, Guridi M, Kim J, et al. Blocking the apoE/Aβ
cerebrovascular integrity via cyclophilin A. Nature 2012; 485: 512–16. interaction ameliorates Aβ-related pathology in APOE ε2 and
91 Fitz NF, Cronican AA, Lefterov I, Koldamova R. Comment on ε4 targeted replacement Alzheimer model mice.
ApoE-directed therapeutics rapidly clear β-amyloid and reverse Acta Neuropathol Commun 2014; 2: 75.
deficits in AD mouse models. Science 2013; 340: 924. 103 Poirier J, Miron J, Picard C, et al. Apolipoprotein E and lipid
92 Muñoz-Cabrera JM, Sandoval-Hernández AG, Niño A, et al. homeostasis in the etiology and treatment of sporadic Alzheimer’s
Bexarotene therapy ameliorates behavioral deficits and induces disease. Neurobiol Aging 2014; 35 (suppl 2): S3–10.
functional and molecular changes in very-old Triple Transgenic 104 Mak ACY, Pullinger CR, Tang LF, et al. Effects of the absence of
Mice model of Alzheimer´s disease. PLoS One 2019; 14: e0223578. apolipoprotein E on lipoproteins, neurocognitive function, and
93 Tai LM, Koster KP, Luo J, et al. Amyloid-β pathology and APOE retinal function. JAMA Neurol 2014; 71: 1228–36.
genotype modulate retinoid X receptor agonist activity in vivo. 105 Kim J, Castellano JM, Jiang H, et al. Overexpression of low-density
J Biol Chem 2014; 289: 30238–55. lipoprotein receptor in the brain markedly inhibits amyloid
94 Price AR, Xu G, Siemienski ZB, et al. Comment on ApoE-directed deposition and increases extracellular A β clearance. Neuron 2009;
therapeutics rapidly clear β-amyloid and reverse deficits in AD 64: 632–44.
mouse models. Science 2013; 340: 924–d. 106 Pocovi M, Cenarro A, Civeira F, et al. Incomplete dominance of
95 Tesseur I, Lo AC, Roberfroid A, et al .Comment on ApoE-directed type III hyperlipoproteinemia is associated with the rare
therapeutics rapidly clear β-amyloid and reverse deficits in AD apolipoprotein E2 (Arg136-->Ser) variant in multigenerational
mouse models. Science 2013; 340: 924–d. pedigree studies. Atherosclerosis 1996; 122: 33–46.
96 Veeraraghavalu K, Zhang C, Miller S, et al. Comment on
ApoE-directed therapeutics rapidly clear β-amyloid and reverse © 2020 Elsevier Ltd. All rights reserved.
deficits in AD mouse models. Science 2013; 340: 924–d.
80 www.thelancet.com/neurology Vol 20 January 2021
You might also like
- Journal Pre-Proof: Neurobiology of DiseaseDocument20 pagesJournal Pre-Proof: Neurobiology of DiseaseChristina MountakiNo ratings yet
- ApoE2 Mitigate Disease Related Phenotypes 2021Document18 pagesApoE2 Mitigate Disease Related Phenotypes 2021Ram KNo ratings yet
- Fragmentation of Brain Apolipoprotein E (Apoe) and Its Relevance in Alzheimer 'S DiseaseDocument15 pagesFragmentation of Brain Apolipoprotein E (Apoe) and Its Relevance in Alzheimer 'S DiseaseChristina MountakiNo ratings yet
- APOE-amyloid Interaction Therapeutic Targets PDFDocument8 pagesAPOE-amyloid Interaction Therapeutic Targets PDFChristina MountakiNo ratings yet
- NIH Public Access: Author ManuscriptDocument31 pagesNIH Public Access: Author Manuscriptنوره نورNo ratings yet
- Differential ApoE ERKDocument20 pagesDifferential ApoE ERKRam KNo ratings yet
- ApoE2 GT For AD 2023Document43 pagesApoE2 GT For AD 2023Ram KNo ratings yet
- Apolipoprotein E Disease-Specific Effects On Brain Atrophy in Alzheimer's Disease and Frontotemporal DementiaDocument5 pagesApolipoprotein E Disease-Specific Effects On Brain Atrophy in Alzheimer's Disease and Frontotemporal DementiaBlackbeatle63No ratings yet
- Alves Et Al - 2016 - Gene Therapy Strategies For Alzheimer's DiseaseDocument8 pagesAlves Et Al - 2016 - Gene Therapy Strategies For Alzheimer's DiseaseMaria ChenNo ratings yet
- JC4 - 41467 - 2018 - Article - 6783Document11 pagesJC4 - 41467 - 2018 - Article - 6783Roaster AppsNo ratings yet
- Apoe4: An Emerging Therapeutic Target For Alzheimer 'S DiseaseDocument17 pagesApoe4: An Emerging Therapeutic Target For Alzheimer 'S DiseaseACHMAD RIFKY ANSYORINo ratings yet
- MMC 2Document38 pagesMMC 2Amir aliNo ratings yet
- Organoidi Chimerici ADDocument10 pagesOrganoidi Chimerici ADfabiofab4No ratings yet
- A Critical Appraisal of Amyloid-β-targeting Therapies for Alzheimer Disease 2019 ReviewDocument16 pagesA Critical Appraisal of Amyloid-β-targeting Therapies for Alzheimer Disease 2019 Review畏No ratings yet
- De Novo Mutations in YWHAG Cause Early Onset EpilepsyDocument11 pagesDe Novo Mutations in YWHAG Cause Early Onset EpilepsyGiselle Costa Daniel HonoratoNo ratings yet
- Alzheimer PatohDocument27 pagesAlzheimer PatohHenry Leroy Lewis BatresNo ratings yet
- Autism-Spectrum-Disorders-an-Intervention-Approach LAO JIDocument12 pagesAutism-Spectrum-Disorders-an-Intervention-Approach LAO JIErica Alejandra SchumacherNo ratings yet
- Biomedicines 12 00695Document11 pagesBiomedicines 12 00695jamel-shamsNo ratings yet
- Seminar: Kaj Blennow, Mony J de Leon, Henrik ZetterbergDocument17 pagesSeminar: Kaj Blennow, Mony J de Leon, Henrik ZetterbergDanni XNo ratings yet
- No Apparent Association Between Beta-Amyloid Deposition and Apolipoprotein E Genotype in The Non-Demented..Document7 pagesNo Apparent Association Between Beta-Amyloid Deposition and Apolipoprotein E Genotype in The Non-Demented..Qorry AmandaNo ratings yet
- Nihms 1795094Document24 pagesNihms 1795094syedrayyanahmed2003No ratings yet
- Wisdom2011.the Effects of Apolipoprotein E On Non-Impaired Cognitive Functioning - A Meta-AnalysisDocument12 pagesWisdom2011.the Effects of Apolipoprotein E On Non-Impaired Cognitive Functioning - A Meta-AnalysisSu AjaNo ratings yet
- β-amyloid Peptides and Amyloid Plaques in Alzheimer's DiseaseDocument9 pagesβ-amyloid Peptides and Amyloid Plaques in Alzheimer's DiseaseNarcisa MateiNo ratings yet
- Synthesis Paper - AdDocument16 pagesSynthesis Paper - Adapi-463372230No ratings yet
- Jiménez-PSEN1 2008Document4 pagesJiménez-PSEN1 2008Carles de Diego BoguñáNo ratings yet
- Ordovas 2002Document5 pagesOrdovas 2002barti koksNo ratings yet
- Murphy 2010Document13 pagesMurphy 2010Nadia SaiNo ratings yet
- Miller2012-How Are Memories RetrievedDocument10 pagesMiller2012-How Are Memories Retrievediulia andreeaNo ratings yet
- Pharmaco GeneticsDocument8 pagesPharmaco GeneticsArti Tyagita KusumawardhaniNo ratings yet
- Alzheimer's - Alzheimer's Disease - Kaj Blennow, Mony J de Leon, Henrik ZeterbergDocument17 pagesAlzheimer's - Alzheimer's Disease - Kaj Blennow, Mony J de Leon, Henrik ZeterbergCatinean DanielaNo ratings yet
- Genetics of DementiaDocument24 pagesGenetics of DementiaandrevendettaNo ratings yet
- 1 s2.0 S221315821930333X MainDocument12 pages1 s2.0 S221315821930333X MainlivelygirlNo ratings yet
- j.nbd.2020.104795 Journal Pree PrrofDocument40 pagesj.nbd.2020.104795 Journal Pree PrrofRifqi Hamdani PasaribuNo ratings yet
- DAI 2017 - The Genes Associated With Early-Onset Alzheimer's Disease PDFDocument12 pagesDAI 2017 - The Genes Associated With Early-Onset Alzheimer's Disease PDFAlberto HenriqueNo ratings yet
- VIrtual Poster DirectoryDocument94 pagesVIrtual Poster Directoryandrewma123No ratings yet
- Genética Do Autismo: Genetics of AutismDocument3 pagesGenética Do Autismo: Genetics of Autismonurb90No ratings yet
- 33 PDFDocument4 pages33 PDFThelma CastlleNo ratings yet
- Gozes Et Al-2002-Drug Development ResearchDocument7 pagesGozes Et Al-2002-Drug Development Researchancuta.lupaescuNo ratings yet
- The Amyloid-β Pathway in Alzheimer's Disease. Molecular PsychiatryDocument23 pagesThe Amyloid-β Pathway in Alzheimer's Disease. Molecular Psychiatryanggi abNo ratings yet
- Fgf13 Causes Synaptic Excitatory-Inhibitory: Disruption of Imbalance and Genetic Epilepsy and Febrile Seizures PlusDocument16 pagesFgf13 Causes Synaptic Excitatory-Inhibitory: Disruption of Imbalance and Genetic Epilepsy and Febrile Seizures Plushidayatul rahmoNo ratings yet
- The Amyloid Hypothesis of Alzheimer's Disease at 25 YearsDocument14 pagesThe Amyloid Hypothesis of Alzheimer's Disease at 25 YearsNguyễn Thị Thảo NhungNo ratings yet
- What Is It Behind Alzheimer's Disease? A Pathophysiology ReviewDocument8 pagesWhat Is It Behind Alzheimer's Disease? A Pathophysiology ReviewAnonymous 4iaWWhhDU8No ratings yet
- Heterozygous UCHL1 Loss of Function Variants Cause A Neurodeg - 2022 - GeneticsDocument12 pagesHeterozygous UCHL1 Loss of Function Variants Cause A Neurodeg - 2022 - Geneticsronaldquezada038No ratings yet
- 1 s2.0 S0149763421002682 MainDocument21 pages1 s2.0 S0149763421002682 MainAna Catarina De Oliveira Da Silv LaborinhoNo ratings yet
- Epileptic Encephalopathies SYNGAP1Document7 pagesEpileptic Encephalopathies SYNGAP1Saya OtonashiNo ratings yet
- DNA Methylome R-Loop and Clinical Exome ProfilingDocument13 pagesDNA Methylome R-Loop and Clinical Exome ProfilingShopnil SarkarNo ratings yet
- 1 s2.0 S1769721222000313 MainDocument14 pages1 s2.0 S1769721222000313 MainCiarol BorbonNo ratings yet
- Shin - 2019 - AB Oligomers Promote Uptake TauDocument13 pagesShin - 2019 - AB Oligomers Promote Uptake TauTibor SzénásiNo ratings yet
- EE y CMSDocument6 pagesEE y CMSdayanachuquimia95No ratings yet
- A Nelson Aalen Estimate of The Incidence PDFDocument43 pagesA Nelson Aalen Estimate of The Incidence PDFMarcela SalazarNo ratings yet
- Aceves - EOE Unmet Needs 2014 - Dig Dis 2014Document9 pagesAceves - EOE Unmet Needs 2014 - Dig Dis 2014George LucasNo ratings yet
- Familial Alzheimer's Disease: Clinical FeaturesDocument4 pagesFamilial Alzheimer's Disease: Clinical FeaturesChristel Charm FajardoNo ratings yet
- ALSDocument14 pagesALSZé CunhaNo ratings yet
- Ε4 Polymorphism And Cognitive: Apoe-Deficit Among The Elderly Population Of Fernando De NoronhaDocument5 pagesΕ4 Polymorphism And Cognitive: Apoe-Deficit Among The Elderly Population Of Fernando De NoronhafabcardososNo ratings yet
- Pathophysiology of Alzheimer's Disease: Neuroimaging Clinics of North America December 2005Document28 pagesPathophysiology of Alzheimer's Disease: Neuroimaging Clinics of North America December 2005AnisNo ratings yet
- Genetic Overlap Between Autism, Schizophrenia and Bipolar DisorderDocument7 pagesGenetic Overlap Between Autism, Schizophrenia and Bipolar DisorderamarillonoexpectaNo ratings yet
- Alzheimers-Disease-Genetics-Fact-Sheet 0Document8 pagesAlzheimers-Disease-Genetics-Fact-Sheet 0api-285676076No ratings yet
- Yoshiyama 2012Document13 pagesYoshiyama 2012yusufNo ratings yet
- VAN 201 Introduction To Gross AnatomyDocument3 pagesVAN 201 Introduction To Gross AnatomyOsakuni OlaoluwakitanNo ratings yet
- PathogensDocument15 pagesPathogensIsmael CastelanNo ratings yet
- Human Cells Journey: Organ Syste MDocument7 pagesHuman Cells Journey: Organ Syste MArina CucuruzaNo ratings yet
- Pathway, Show The Major Pathway of CSF Flow. Beginning in The Lateral Ventricles, CSF FlowsDocument2 pagesPathway, Show The Major Pathway of CSF Flow. Beginning in The Lateral Ventricles, CSF FlowsMary Scarlette CenaNo ratings yet
- MC1 REVIEWER (Introduction To AnaPhy)Document7 pagesMC1 REVIEWER (Introduction To AnaPhy)Francine Dominique CollantesNo ratings yet
- ENDOCRINOLOGY ReportDocument16 pagesENDOCRINOLOGY ReportConlene PontejoNo ratings yet
- 5 Axillary and Epitrochlear Lymph Node Dissection For MelanomaDocument11 pages5 Axillary and Epitrochlear Lymph Node Dissection For MelanomajuanrangoneNo ratings yet
- Periampullary Carcinoma - Surgical Treatment - NCBI Bookshelf PDFDocument4 pagesPeriampullary Carcinoma - Surgical Treatment - NCBI Bookshelf PDFAsif.N.IqbalNo ratings yet
- Cystic Liver LesionsDocument2 pagesCystic Liver LesionsNatnael GetahunNo ratings yet
- Tarif Harga RADIOLOGI Murni TeguhDocument24 pagesTarif Harga RADIOLOGI Murni Teguhester silalahiNo ratings yet
- Vascular DementiaDocument7 pagesVascular DementiaAAshish singh BhadoriyaNo ratings yet
- Mechanical Ventilation Learning Package: Sharon-Ann Shunker, CNC, Liverpool ICU SWSLHD 2/3/2016Document75 pagesMechanical Ventilation Learning Package: Sharon-Ann Shunker, CNC, Liverpool ICU SWSLHD 2/3/2016Hanni HarahapNo ratings yet
- MID YEAR Assessment - SCIENCE10Document5 pagesMID YEAR Assessment - SCIENCE10anelou guingueNo ratings yet
- Clinicaldistinctionof Cerebralischemiaand Triagingofpatientsinthe EmergencydepartmentDocument13 pagesClinicaldistinctionof Cerebralischemiaand Triagingofpatientsinthe EmergencydepartmentBrunaProençaNo ratings yet
- A Critical Review of Interfaces With The Peripheral Nervous System For The Control of Neuroprostheses and Hybrid Bionic SystemsDocument30 pagesA Critical Review of Interfaces With The Peripheral Nervous System For The Control of Neuroprostheses and Hybrid Bionic SystemsJoao PauloNo ratings yet
- Head Trauma & Management: Dr. Utham Murali. M.S M.B.A. Asso - Prof of Surgery IMS / MSU / MalaysiaDocument48 pagesHead Trauma & Management: Dr. Utham Murali. M.S M.B.A. Asso - Prof of Surgery IMS / MSU / MalaysiaNinaNo ratings yet
- Structures and Functions: Chapter 45: Nursing Assessment: Urinary SystemDocument18 pagesStructures and Functions: Chapter 45: Nursing Assessment: Urinary SystemKennette LimNo ratings yet
- Third Quarter Exam in Science 10Document3 pagesThird Quarter Exam in Science 10Marife GuadalupeNo ratings yet
- Perdev 1st Quater ReviewerDocument4 pagesPerdev 1st Quater ReviewerLala CoronelNo ratings yet
- Pediatric RehabDocument32 pagesPediatric RehabRainy DaysNo ratings yet
- "Assessing Respirations": Prepared By: Marie Cecille Liberty S. VarillaDocument11 pages"Assessing Respirations": Prepared By: Marie Cecille Liberty S. VarillaMarie Cecille Soliven VarillaNo ratings yet
- Memory Unit 10Document41 pagesMemory Unit 10Rabia IsrafilNo ratings yet
- Cushing's SyndromeDocument4 pagesCushing's SyndromeZainab AliNo ratings yet
- Concept Strengthening Sheet (CSS-06) Based On CST-11 & 12 - Zoology-1Document4 pagesConcept Strengthening Sheet (CSS-06) Based On CST-11 & 12 - Zoology-1Rudraksh AhujaNo ratings yet
- Neuro ImagingDocument12 pagesNeuro ImagingToby PearceNo ratings yet
- Eaton County Apparent Drowning Death UnidentifiedDocument5 pagesEaton County Apparent Drowning Death UnidentifiedFergus BurnsNo ratings yet
- Organ System Overview NotesDocument1 pageOrgan System Overview NotesMary Kris Sumampong MalonNo ratings yet
- Respuesta Humana Al EstresDocument10 pagesRespuesta Humana Al EstresmorbreirNo ratings yet
- Chapter 31 Immunologic System IntroductionDocument5 pagesChapter 31 Immunologic System IntroductionStacey100% (2)
- Brain MethsDocument17 pagesBrain MethsBolinho ChuvaNo ratings yet