Professional Documents
Culture Documents
5th Sem - Abnormal Psy-MODULE 4-MG Unvsty - PEPPGUIDE
5th Sem - Abnormal Psy-MODULE 4-MG Unvsty - PEPPGUIDE
Uploaded by
swathy sudheer0 ratings0% found this document useful (0 votes)
9 views10 pagesOriginal Title
5th Sem- Abnormal Psy-MODULE 4-MG Unvsty.PEPPGUIDE
Copyright
© © All Rights Reserved
Available Formats
PDF or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
0 ratings0% found this document useful (0 votes)
9 views10 pages5th Sem - Abnormal Psy-MODULE 4-MG Unvsty - PEPPGUIDE
5th Sem - Abnormal Psy-MODULE 4-MG Unvsty - PEPPGUIDE
Uploaded by
swathy sudheerCopyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
You are on page 1of 10
fear)
PINCUBATION mam
otshing your dreams Guide
M.G
» UNIVERSITY
BSc PSYCHOLOGY
Semester 5
ABNORMAL BEHAVIOUR
, Be,
oo
@
\
Oe
Module 4
OBSESSIVE COMPULSIVE
AND RELATED DISORDERS
www.pepponline.in
Obsessive Compulsive and Related Disorders
DS Re Cameo)
DSM 5 CRITERIA
A. Presence of obsessions, compulsions, or both:
Obsessions are defined by (1) and (2):
1L, Recurrent and persistent thoughts, urges, or images that are experienced, at some time during
the disturbance, as intrusive and unwanted, and that in most individuals cause marked anxiety or
distress.
2. The individual attempts to ignore or suppress such thoughts, urges, or images, or to neutralize
them with some other thought or action (i.e. by performing a compulsion).
Compulsions are defined by (1) and (2)
1. Repetitive behaviors (e.g., hand washing, ordering, checking) or mental acts (e.g., praying,
counting, repeating words silently) that the individual feels driven to perform in response to an
obsession or according to rules that must be applied rigidly.
2. The behaviors or mental acts are aimed at preventing or reducing anxiety or distress, or
preventing some dreaded event or situation; however, these behaviors or mental acts are not
connected in a realistic way with what they are designed to neutralize or-prevent, or are clearly
excessive.
Note: Young children'may notibe able to articulate the aims of these behaviors or mental acts.
B. The obsessions or compulsions are time-consuming (e.g., take more than 1 hour per day) or
cause clinically significant distress or impairment in social, occupational, or other important
areas of functioning,
C. The obsessive-compulsive symptoms are not attributable to the physiological effects of a
substance (¢.g,, a drug of abuse, a medication) or another medical condition.
D. The disturbance is not better explained by the symptoms of another mental disorder (e.g.,
excessive worries, as in generalized anxiety disorder; preoccupation with appearance, as in body
dysmorphic disorder; difficulty discarding or parting with possessions, as in hoarding disorder,
hair pulling, as in trichotillomania [hair-pulling disorder]; skin picking, as in excoriation [skin-
picking] disorder; stereotypies, as in stereotypic movement disorder; ritualized eating behavior,
as in eating disorders; preoccupation with substances or gambling, as in substance-related and
addictive disorders; preoccupation with having an illness, as in illness anxiety disorder; sexual
urges or fantasies, as in paraphilic disorders; impulses, as in disruptive, impulse-control, and
conduct disorders; guilty ruminations, as in major depressive disorder; thought insertion or
delusional preoccupations, as in schizophrenia spectrum and other psychotic disorders; or
repetitive patterns of behavior, as in autism spectrum disorder).
Specify if:
With good or fair insight: The individual recognizes that obsessive-compulsive disorder beliefs
are definitely or probably not true or that they may or may not be true.
With poor insight: The individual thinks obsessive-compulsive disorder beliefs are probably true.
With absent insight/delusional beliefs: The individual is completely convinced that obsessive-
compulsive disorder beliefs are true.
Specify if:
Tic-related: The individual has a current or past history of a tic disorder
BODY DYSMORPHIC DISORDER
Be ae ee Ces eer cur)
‘A Preoccupation with one or more perceived defects or flaws in physical appearance that are not
observable or appear slight to others.
B. At some point during the course of the disorder, the individual has performed repetitive
behaviors (e.g,, mirror checking, excessive grooming, skin picking, reassurance seeking) or
mental acts (e.g., comparing his or her appearance with that of others) in response to the
appearance concerns.
C. The preoccupation causes clinically significant distress or impairment in social, occupational,
or other important areas of functioning,
D. The appearance preoccupation is not better explained by concerns with body fat or weight in
an individual whose symptoms meet diagnostic criteria for an eating disorder
HOARDING DISORDER
A Persistent difficulty disearding or parting with possessions, regardless of their actual value
B This difficulty is due to a perceived need to save the items and to distress associated with
discarding them
C The difficulty discarding possessions results in the accumulation of possessions that congest
and clutter active living areas and substantially compromises their intended use. If living areas
are uncluttered, it is only because of the interventions of third parties (e.g, family members,
cleaners, and authorities)
D The hoarding causes clinically significant distress or impairment in social, occupational, or
other important areas of functioning (including maintaining a safe environment for self and
others)
E The hoarding is not attributable to other medical conditions (e.g., brain injury, cerebrovascular
disease, and Prader-Willi syndrome)
F The hoarding is not better explained by the symptoms of other mental disorders (e.g,
obsessions in obsessive-compulsive disorder, decreased energy in major depressive disorder,
delusions in schizophrenia.or another psychotic disorder, cognitive deficits in major
neurocognitive disorder and restricted interests in autism spectrum disorder
HAIR PULLING DISORDER
oe
ieoreneentr
Rot
TREATMENT
SIGNS & SYMPTOMS: =a
Pesce et ve were
Some enon
a , wonveeonn
ais Srereete
TS se
“© LONG TERM CONSEQUENCES: bahay sti
ean ya eles ee MCU)
‘A. Recurrent pulling out of one's hair resulting in noticeable hair loss.
B. An increasing sense of tension immediately before pulling out the hair or when attempting to
resist the behavior.
C. Pleasure, gratification, or relief when pulling out the hair
D. The disturbance is not better accounted for by another mental disorder and is not due toa
general medical condition (e.g., a dermatological condition)
E, The disturbance causes clinically significant distress or impairment in social, occupational, or
other important areas of functioning,
Causes of trichotillomania
Away of dealing with stress or anxiety
Acchemical imbalance in the brain, similar to Obsessive Compulsive Disorder (OCD)
changes in hormone levels during puberty
For some people, hair pulling can be a type of addiction.
‘The more they pull their hair out, the more they want to keep doing it.
TREATMENT FOR OGD,
Psychotherapy
Exposure and response prevention (ERP)
MEDICATIONS
Fluoxetine (Prozac) for adults and children 7 years and older
Paroxetine (Paxil, Pexeva) for adults only
Sertraline (Zoloft) for adults and children 6 years and older
TREATMENT FOR TRICHOTILLOMANIA
Therapy
‘Types of therapy that may be helpful for trichotillomania include:
Habit Reversal Training, This behavior therapy is the primary treatment for trichotillomania.
‘You learn how to recognize situations where you're likely to pull your hair and how to substitute
other behaviors instead. For example, you might clench your fists to help stop the urge. Other
therapies may be used along with habit reversal training. A variant of this technique, called
decoupling, involves quickly redirecting your hand from your hair to another location.
Cognitive Therapy. This therapy can help you identify and examine distorted beliefs you may
have in relation to hair pulling,
Acceptance and Commitment Therapy. This therapy can help you lear to accept your hair
pulling urges without acting on them.
TREATMENT FOR HOARDING DISORDER
Treatment
Hoarding may persist for a lifetime, but effective treatment can help reduce the need to hold on
to unnecessary items; it can also improve decision-making, stress-reducing, and organizational
skills
‘The primary treatments used to relieve symptoms of hoarding disorder include cognitive
behavioral therapy (CBT) and antidepressant medication, such as selective serotonin
reuptake inhibitors (SSRIs). One or the other, ar both, may be employed. Early clinical trials
suggest that compassion-focused therapy may be moreéffective than CBT alone
fe age) eases
Premier Entrance
Preparation Program
74-l] JOIN
PEPP GUIDE
El WHATSAPP GROUP
SUBSCRIBE
PEPP YOUTUBE
CHANNEL
Download
PEPP Learning App
Fulfill your central university dream
with the!
coaching program in Kerala
For Admission Related Queries:
Call: +91 808925250, +91 8891359553
Visit: www.pepponiine.in
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5814)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Anger ManagementDocument22 pagesAnger Managementswathy sudheerNo ratings yet
- Suicide Prevention and Mental Health PromotionDocument1 pageSuicide Prevention and Mental Health Promotionswathy sudheerNo ratings yet
- TT-1st Sem BSCC CBCSSDocument5 pagesTT-1st Sem BSCC CBCSSswathy sudheerNo ratings yet
- PGNotification2023 24Document1 pagePGNotification2023 24swathy sudheerNo ratings yet
- 3 Existential ApproachDocument10 pages3 Existential Approachswathy sudheerNo ratings yet
- Therapy FamilyDocument14 pagesTherapy Familyswathy sudheerNo ratings yet
- Syllabus M.SC Clinical PsychologyDocument40 pagesSyllabus M.SC Clinical Psychologyswathy sudheerNo ratings yet
- Construction and Standardization of Perceived Parenting Style ScaleDocument4 pagesConstruction and Standardization of Perceived Parenting Style Scaleswathy sudheerNo ratings yet
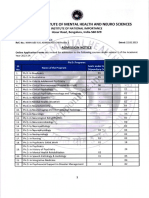
- NIMHANS MPHIL, PHD APPLICATION NOTIFICATION - PeppGuideDocument6 pagesNIMHANS MPHIL, PHD APPLICATION NOTIFICATION - PeppGuideswathy sudheerNo ratings yet
- Unit 2 Cognitive Behaviour Therapies (Including Rational Emotive Therapy)Document19 pagesUnit 2 Cognitive Behaviour Therapies (Including Rational Emotive Therapy)swathy sudheerNo ratings yet
- What Is Psychotherapy?Document11 pagesWhat Is Psychotherapy?swathy sudheerNo ratings yet
- What Is Assertiveness Training?Document3 pagesWhat Is Assertiveness Training?swathy sudheerNo ratings yet
- Multiple Choice Questions - Introduction To Psychology Study GuideDocument8 pagesMultiple Choice Questions - Introduction To Psychology Study Guideswathy sudheerNo ratings yet
- Unit 1 Behaviour Modification Techniques: StructureDocument26 pagesUnit 1 Behaviour Modification Techniques: Structureswathy sudheerNo ratings yet
- After Reading This Chapter, You Would Be Able To:: Some Misuses of Intelligence TestsDocument22 pagesAfter Reading This Chapter, You Would Be Able To:: Some Misuses of Intelligence Testsswathy sudheerNo ratings yet
- List of Fields of Application of Statistics - WikipediaDocument2 pagesList of Fields of Application of Statistics - Wikipediaswathy sudheerNo ratings yet
- Applied Social Psychology Module 3 FinalDocument18 pagesApplied Social Psychology Module 3 Finalswathy sudheerNo ratings yet
- Official Statistics in India The Past and The PresentDocument17 pagesOfficial Statistics in India The Past and The Presentswathy sudheerNo ratings yet
- Applied Social Psychology Module 1Document3 pagesApplied Social Psychology Module 1swathy sudheerNo ratings yet
- Applied Social Psychology Module 2Document5 pagesApplied Social Psychology Module 2swathy sudheerNo ratings yet
- Developmental Psychology On20nov2015 PDFDocument47 pagesDevelopmental Psychology On20nov2015 PDFswathy sudheerNo ratings yet
- L5 PsychometricsDocument4 pagesL5 Psychometricsswathy sudheerNo ratings yet
- Present Status and Challenges of Intellectual Assessment in India - International Journal of School & Educational Psychology - Vol 4, No 4Document5 pagesPresent Status and Challenges of Intellectual Assessment in India - International Journal of School & Educational Psychology - Vol 4, No 4swathy sudheerNo ratings yet