Professional Documents
Culture Documents
Pharmacology Prelim
Uploaded by
Ivy SantosOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pharmacology Prelim
Uploaded by
Ivy SantosCopyright:
Available Formats
PHARMACOLOGY Egyptians
PRELIM PERIOD ● Archives of remedies on a document known as Erb’s Papyrus in 1500 B.C.
● Pharmacologia sen Manuductio and Materia Medicum
WEEK 1 ● First recorded reference to the word pharmacology
Pharmacology: Early 1800s
● Pharmacology is the study of drugs and its origin, chemical structure, preparation, ● Chemists isolates specific substances from complex mixtures
administration, action, metabolism and excretion. ● Pharmacologists then study their effects in animals
● The study of drugs that alter functions of living organisms. ● Fredrich Serturner (first isolated morphine from opium, injected himself and three
PHARMACY – art of preparing, compounding, and dispensing drugs. It also refers to the other friends with huge doses (100mg))
place where drugs are prepared and dispensed DRUGS - are chemicals that alter physicochemical processes in body cells.
PHARMACIST – a person licensed to prepare and dispense drugs to make up ● They can stimulate or inhibit normal cellular functions.
prescriptions. ● Used interchangeably with medicines.
TERMINOLOGIES: Branches of Pharmacology:
Drug Name - The systematic naming of drug used in Pharmacology >Pharmacodynamics - pharmaco means “medicine” dynamic means “change”.
Oral Medication - preparations are taken by mouth, swallowed with fluid, and absorbed Refers to how a medicine changes the body the branch of pharmacology concerned
via the gastrointestinal tract. with mechanisms of drug action and the relationships between drug concentration and
Parenteral Medication - can be defined as a sterile drug product, suitable for responses in the body.
administration by injection. > Pharmacokinetics - pharmaco means “medicine”, kinetic means “movement or
Ophthalmic Medication - a medication comes in form of drops gel or ointment motion”. The study of drug movement throughout the body. How the body deals with
Topical Medication - a drug suitable for administration applied to a particular body part medications. Actions and side effects of medications in patients.
most often applied to surfaces such as skin and mucous membrane. > Pharmacognosy - the branch of knowledge concerned with medicinal drugs
Otic Medication - drug products used to treat conditions of the external and middle ear. obtained from plants or other natural resources
> Pharmacotherapeutics - the study of the therapeutic uses and effects of drugs.
HISTORY ● Beneficial and adverse effects of drugs.
Babylonians > Pharmacovigilance - the practice of monitoring the effects of medical drugs after they
Earliest surviving “prescriptions” on clay tablets in 3000 B.C. have been licensed for use especially in order to identify and evaluate previously
Chinese unreported adverse reactions.
Recorded the Pen Tsao (Great Herbal) – a 40-volume compendium of plant remedies > Toxicology - the branch of science concerned with the nature, effects, and detection of
dating to 2700 B.C. poisons.the measurement and analysis of potential toxins, intoxicating or banned
substances, and prescription medications present in a person’s body.
DRUG NAMES ● The Chinese recorded the Pen Tsao (Great Herbal), a 40-volume compendium of
> Generic or Nonproprietary Name: name approved by the Medical or Pharmaceutical plant remedies dating to 2700 B.C.
Associations in the original country of manufacture and is adopted by all countries. ● The Egyptians followed in 1500 B.C. by archiving their remedies on a document
● e.g. Paracetamol known as Eber’s Papyrus.
> Brand name or trade name: name given by the manufacturer of the drug ● e.g morphine, colchicine, cocaine - At that time, chemists were making
● e.g. Adol or Panadol or Biogesic remarkable progress, isolating specific substances from complex mixtures, this
> Chemical name: name that describes the atomic or chemical structure enabled scientists to isolate the active agents from scarce natural sources,
● e.g. para-acetylaminophenol ○ ex. morphine.
■ Cocaine from - cocoa leaves
Drug Action b. Animals - Biologic - are agents naturally produced in animal cell, by microorganisms,
Therapeutic effect or by the body itself.
● also referred as the DESIRED EFFECT (primary effect intended) ● e.g. hormones, monoclonal antibodies, natural blood products, Interferons and
Side effect vaccines
● also referred as the SECONDARY EFFECT (unintended effect) others.
● ADVERSE EFFECT (severe side effects) DRUG USES SPECIES
Drug Toxicity Crestor high cholesterol Rats, rabbits, dogs
● Deleterious effects of a drug resulting from over dosage, ingestion of external use Diovan High blood pressure Rats, rabbits
drug, and accumulation on the blood stream Lantus Type 1 & 2 Diabetes Dogs, guinea pigs
Drug Allergy 2. Inorganic compounds
● immunologic reaction to drug ● e.g. Lithium carbonate
Drug Tolerance ○ Cisplatin
● exists in person with unusually low physiologic response to a drug 3. Synthetic
● e.g Ecstasy or Molly - stimulants that mimic the effect of cocaine
Sources of Drugs:
1. Natural sources - DRUG EVALUATION
a. Plants = a series of scientific tests to evaluate the actual therapeutic and toxic effects of
● One of the oldest forms of health care, herbal medicine has been practiced in chemicals
virtually every culture dating to antiquity. STEPS:
● The Babylonians recorded the earliest surviving “prescriptions” on day tablets in PRECLINICAL TRIAL
3000 B.C. = testing done on laboratory performed in animals
= tests efficacy and toxicity, at different doses, it predicts whether the drug will cause PHASE II
harm to humans. > chemicals cleared for limited clinical studies
= do not always reflect the way a human responds, testing may overestimate or > some may not further proceed with the evaluation due to the following criteria
underestimate the actual risk to humans. > less effective than expected
> are too toxic
ORPHAN DRUG > produce unacceptable side effects
= are drugs that have been discovered but are not financially viable and therefore have > have a low benefit-to-risk ratio
not been “adopted” by any drug company > are not as effective as available drugs
= may be useful in treating a rare disease, or they may have potentially dangerous PHASE III
adverse effect > chemicals cleared for large-scale clinical studies
= are often abandoned after preclinical trials or phase I studies. > some chemicals may not advance further in the next phase due to the following criteria:
Criteria: > produce unacceptable side effects
> lack therapeutic activity > produce unexpected responses
> too toxic PHASE IV
> Teratogenic > drugs approved for marketing by FDA
> have a small margin of safety > continues evaluation
● e.g. Zavesca (miglustat), Trisenox (arsenic trioxide injection), Aldurazyme
(Laronidase), Glivec (Imatinib mesylate), Fabrazyme (Agalsidase beta), Ventavis DOSAGE FORMS OF DRUGS: ( Sir include this po, describe, better with pictures )
(iloprost),Litak (cladribine). A. SOLID FORMS
PHASE I 1. TABLET :
> chemicals cleared for human testing, there are significant therapeutic benefits. a. scored.
> testing done on healthy male subjects b. layered.
> companies begin developing a brand name c. enteric-coated.
ORPHAN DRUG d. chewable.
> are chemicals that are discarded Phase I e. sustained released
> will not participate in the next phase 2. CAPSULE :
Criteria: a. soft gel.
> lack therapeutic activity in humans b. hard gel
> too toxic 3. LOZENGES
> produce unacceptable side effects 4. SUPPOSITORY
> teratogenic
B. LIQUID FORMS ✓ OBSERVE THE TEN RIGHTS
1. SYRUP ✓ Right Client
2. SUSPENSION ✓ Right Medication
3. ELIXIR ✓ Right Dose
4. EMULSION ✓ Right Time
5. INHALANTS ✓ Right Route
C. TOPICAL FORMS ✓ Right Client Education
1. CREAM ✓ Right Documentation
2. OINTMENT ✓ Right to Refuse
3. LOTION ✓ Right Assessment
4. PATCH ✓ Right Evaluation
5. GELS
Right client – can be measured by checking the client identification bracelet by having
PRINCIPLES OF DRUG ADMINISTRATION and by having the client state her or his name
MEDICATIONS ● Some client answer to any name or unable to respond, so client identification
✓ Are substances administered for the diagnosis, cure, treatment, or relief of symptom or should verified each time of medication administered
prevention of disease ● In the event of missing identification bracelet, the nurse must verify the client
identity before any drug administration
PRACTICE GUIDELINES
✓ RNs are responsible for own actions, illegible order should be questioned or clarified Right drug – means that the client receives the drug that was prescribed, check at least
✓ RNs should be knowledgeable about the medication three times prior to administration
✓ If the RN is uncertain about the calculation, ask another nurse to double check ● Medication orders may be prescribed by:
✓ What you prepare, you administer ○ Physician
✓ Do not leave medications at bedside ○ Dentist
✓ If the client vomits, report to charge nurse, MD, or both. ○ Podiatrist
✓ When error is made, assess the patient first and report to MD immediately ○ License health care provider such as advance practice registered nurse
✓ Correct identification of the patient: ○ With authority from the state to order medication
✓ ID band or ID bracelet (BEST: Kozier) ● Prescriptions:
✓ Ask the patient’s name ○ Component of drug order
✓ Avoid: calling the client in NAME ○ Date and time the order is written
✓ May answer “YES” to the wrong name ○ Drug name
○ Drug dosage Right documentation – requires that the nurses immediately record the appropriate
○ Route of administration information about drug administered
○ Frequency and duration of administration ● Name of the drug
○ Any special instructions for withholding or adjusting dosage based on ● Dose
nursing assessment, drug effectiveness, or laboratory result ● Route
○ Physician or other health care provider signature or name if TO or VO ● Time and date
○ Signature of license practitioner taking TO or VO ● Nurse initial or signature
● Categories of drug orders: Right to educate – requires that the client received accurate and thorough information
○ Standing about the medication and how it relates to his or her situation
○ One-time ● Client teaching also includes therapeutic purpose, possible side effect of the
○ PRN (as needed) drugs, any dietary restriction or requirements skills administration, and laboratory
○ STAT monitoring
Right time – is the time at which the prescribed dose should be administered Right evaluation – requires that the effectiveness of the medication be determined by
● Daily drug dosages are given at specified time during a day such as the client response to medication
● Twice a day b.i.d Right to refuse – client can and do refuse to take medication
● Three time a day t.i.d ● It is the nurses responsibilities to determine when possible the reason for refusal
● Four times a day q.i.d. and to take reasonable measure to facilitate the client taking the medication
● Every 6hrs q6h
ORAL MEDICATION
Right route – is necessary for adequate or appropriate absorption Most common route
● Common routes are the following: ✓ CONTRAINDICATIONS:
○ Oral ● Client is vomiting
○ Sublingual ● Client with intestinal or gastric suction
○ Buccal ● Unconscious Client
○ Inhalation ● Inability to Swallow
○ Topical ✓ Tablet or Capsules
○ Inhalation ✓ (+) difficulty in swallowing
○ Instillation ✓ Crush and mix with small amount of water
○ Suppository, etc. ✓ Avoid Crushing
Right assessment – requires the appropriate data be collected before administration of ✓ Enteric Coated
drugs ✓ Buccal and Sublingual tablets
✓ Liquid Medication ✓ Ventrogluteal
✓ Mix before pouring ✓ > 1 y/o and adult
✓ Place medication cup on flat surface at eye level ✓ No large nerve or blood vessels
✓ Fill the cup with the desired level using the BOTTOM of the meniscus ✓ Sealed off by bone
✓ Contains less fat than buttocks
PARENTERAL MEDICATION ✓ Vastus Lateralis
✓ Intradermal ✓ Site of choice for 1 y/o and younger
✓ SITE ✓ Infants with fully developed gluteal muscles
✓ Inner lower arm ✓ SITE
✓ Upper chest ✓ Dorsogluteal
✓ Anterior chest ✓ For adults and children with well developed gluteal muscles
✓ Upper back beneath the scapula ✓ CONTRAINDICATED:
✓ Angle : almost parallel to the skin 10 - 15 degrees children under 3 y/o
✓ Gauge: #25, #26, #27 ✓ Increased risk of striking the SCIATIC NERVE
✓ Length: ⅜”, ⅝”, ½” ✓ DELTOID
✓ Max cc: 0.1 to 0.2 ml ✓ Small muscle, very close to the radial nerve and artery
✓ Subcutaneous ✓ Rapid absorption for adults
✓ SITE ✓ Cannot administer more than 1 ml.
✓ Outer aspect of the upper arms ✓ Recommended site for Hepa B vaccine administration
✓ Anterior thighs ✓ RECTUS FEMORIS
✓ Abdomen ✓ Can be used for self administration
✓ Upper back ✓ Disadvantage: causes discomfort
✓ Ventrogluteal ✓ Gauge: #24, 23, 22, 21, 20
✓ Dorsogluteal ✓ Length: 1”, 1 1/2”, 2”
✓ Angle: 45-degrees (1 inch of tissue can be grasped) ✓ Max. cc: 2-5 ml
90-degrees (2 inches of tissue can be grasped) ✓ Angle: 90 degrees
✓ Gauge: #25, #26, #27 ✓ INTRAVENOUS/INTRAVASCULAR
✓ Length: ⅜”, ⅝”, ½” ✓ Gauge: #24, 23, 22, 21, 20
✓ Max cc: 1-3 ml ✓ Length: 1”, 1 ½”, 2”
✓ Intramuscular ✓ Max. cc: Push 10 ml
✓ SITE Infusion: 4L in 24 hrs.
TOPICAL MEDICATIONS ✓ Straighten The Auditory Canal:
✓ Transdermal Patch ● Adult: (>3 y/o): Pull the Pinna UPWARD and BACKWARD
✓ SITE ● Child: (<3 y/o): Pull the Pinna DOWNWARD and BACKWARD
✓ Trunk or lower abdomen ✓ INSTILL THE MEDICATION:
Areas that are: hairless Along the side of the canal
(+) hair (clip, do not shave) ✓ ACTIONS AFTER:
Avoid: cuts, burns, abrasions, distal extremity Gently press the TRAGUS
Insert small piece of cotton fluff loosely
OPHTHALMIC MEDICATIONS ✓ Instruction After:
✓ Preparation: Remain in side-lying for 5 minutes
✓ Clean the eyelid and lashes from inner to outer canthus
✓ Instruction before administration WEEK 2
Look up Pharmacodynamics - is the study of the effect of drugs on the body.
✓ Where and How to Apply: ● Drugs act within the body to mimic the actions of the body’s own chemical
LIQUID: messengers.
● Instill correct number of drops
● Outer third of the lower conjunctival sac Dose-Response Relationship
✓ Instruction after Instillation ● is the body’s physiological response to changes in drug concentration at the site
Do PUNCTAL OCCLUSION for 30 seconds of action.
OINTMENT: Potency – refers to the amount of drug needed to elicit a specific physiologic response to
● Discard the first bead a drug.
● Squeeze 2 cm on the lower conjunctival sac Efficacy – magnitude of effect a drug can cause when exerting its maximal effect.
✓ Instruction after Instillation Maximal efficacy – the point at which increasing a drug dosage no longer increases the
CLOSE but not SQUEEZE the eyelid desired therapeutic response.
OTIC MEDICATIONS TERMINOLOGIES
✓ Preparation: Pharmacodynamics - is the study of the effect of drugs on the body.
✓ Clean the pinna and the meatus of the ear canal Dose-Response Relationship - is the body’s physiological response to changes in drug
✓ Warm the medication: concentration at the site of action.
● In between hands Potency - refers to the amount of drug needed to elicit a specific physiologic response to
● Place in warm water a drug.
Efficacy - magnitude of effect a drug can cause when exerting its maximal effect. Therapeutic dose of a drug – is the dose of a drug that produces a therapeutic response
Maximal efficacy – the point at which increasing a drug dosage no longer increases the in 50% of the population.
desired therapeutic response. Toxic dose of a drug – is the dose that produces a toxic response in 50% of the
Therapeutic Index – (TI) describes the relationship between the therapeutic dose of a population.
drug (ED50) and the toxic dose of a drug (TD50) ● If the ED50 and TD50 are close- drugs have a narrow therapeutic index. require
Therapeutic dose of a drug – is the dose of a drug that produces a therapeutic response close monitoring to ensure patient safety.
in 50% of the population. Onset – is the time it takes for a drug to reach the minimum effective concentration
Toxic dose of a drug – is the dose that produces a toxic response in 50% of the (MEC) after administration.
population. ● Time from drug administration to first observable effect (T0-T1)
Onset – is the time it takes for a drug to reach the minimum effective concentration Peak – occurs when it reaches its highest concentration in the blood/plasma
(MEC) after administration. concentration. T0-T2
Peak – occurs when it reaches its highest concentration in the blood/plasma Duration of action – is the length of time the drug exerts a therapeutic effect. period from
concentration. T0-T2 onset until the drug effect is no longer seen. T1-T3
Duration of action – is the length of time the drug exerts a therapeutic effect.
Trough – lowest plasma concentration. 30 minutes prior to the next infusion. Therapeutic Drug Monitoring
Additive Effect - Two drugs with similar actions are taken for a doubled effect ● Drug concentration can be determined by measuring peak and trough drug levels.
Synergistic- combined effect of two drugs is greater than the sum of the effect of each peak – highest plasma concentration. 30 minutes after infusion.
drug given alone. trough – lowest plasma concentration. 30 minutes prior to the next infusion.
Potentiation- a drug that has no effect enhances the effects of the second drug
Antagonistic- one drug inhibits the effect of another drug Theories of Drug Action
Side Effects - results from the pharmacologic effects of the drug A.Drug-Receptor Interaction
Allergic Reactions - unpredictable adverse drug effects; more serious ● Certain portion of drug molecule (active site) selectively combines with some
Idiosyncratic Reaction - abnormal reactivity to the drug caused by a genetic difference molecular structure (reactive site) on the cell to produce a biologic effect
between the patient and normal individual. Receptor site - drugs act at specific areas on cell membranes; react with certain
Toxicity - the degree to which a drug can be poisonous and thus harmful to the human chemicals to cause an effect within the cell
body. “Lock and Key Theory” - specific chemical (key) approaches a cell membrane and finds
Iatrogenic responses - unintentional responses as a result of medical treatment fit (the lock) at receptor site- affects enzyme system within cell- produce certain effects.
Drug+Receptor=Effect
Parameters of Drug Action
Therapeutic Index – (TI) describes the relationship between the therapeutic dose of a
drug (ED50) and the toxic dose of a drug (TD50)
B. Drug-Enzyme Interaction Categories of Drug Action
● Interferes with enzyme systems that act as catalyst from various chemical 1. Stimulation/Depression
reactions ● Stimulation- increased rate of cell activity/ secretion from the gland T3/T4 for
● If single step in one of enzyme system is blocked- normal function is disrupted hypothyroidism
C. Nonspecific Drug Interaction ● Depression- decreased cell activity and function of a specific organ. Iodine,
● Act by biophysical means that do not affect cellular/enzymatic reactions. propylthiouracil
● drugs do not bind to receptors but instead saturate the water or lipid part of a cell- 2. Replacement- replaces essential body compounds
drug actions occur based on the degree of saturation. Example: Insulin
● Neutralization of stomach acid by antacids. 3. Inhibition/Killing of Organism
D. Selective Toxicity ● Interfere with bacterial cell growth
● Specific action on cellular structures that are unique to the microbe. ● Example: Antibiotics
● All chemotherapeutic agents would act only in one enzyme system needed for life 4. Irritation
of a pathogen or neoplastic cell. Example: Laxative- irritate the inner wall of colon---increased peristalsis---increased
● It is essential to the pathogen but not to the host. defecation
Drug Response Drug-Drug Interaction
Drug Response may be: 1. Additive Effect - 2 drugs with similar actions are taken for a doubled effect 1+1=2
1. Primary- always desirable/physiologic effects ● Ibuprofen + paracetamol= added analgesic effect
2. Secondary- desirable or undesirable ● Codeine with acetaminophen = better pain control
Example: Diphenhydramine (Benadryl) 2. Synergistic - combined effect of 2 drugs is greater than the sum of the effect of each
Primary effect: antihistamine; treat symptoms of allergy drug given alone; 1+1=3
Secondary: Drowsiness ● Aspirin = 30% analgesic effect
● codeine – 30% analgesic effect
Classification of Drug Action ● combination = 90% analgesic effect
1. Rapid- few seconds to minutes 3. Potentiation - a drug that has no effect enhances the effects of the second drug 0+1=2
- IV, SL, Inhalations ● Alcohol enhances the analgesic activity of aspirin.
2. Intermediate- 1-2 hours after administration ● Prozac + Zestril
- IM, SC 4. Antagonistic - one drug inhibits the effect of another drug 1+1=0
3. Delayed/Slow- several hours after administration ● Tetracycline + antacid= decreased absorption of tetracycline
- Oral, rectal ● Charcoal in alkaloidal poisoning
Adverse Drug Effects TERMINOLOGIES
1.Side Effects L = Liberation, the release of the drug from it's dosage form.
● Results from the pharmacologic effects of the drug A = Absorption, the movement of drugs from the site of administration to the blood
● Most common as a result of lack of specificity of action within the therapeutic circulation.
range. D = Distribution, the process by which drug diffuses or is transferred from intravascular
2. Allergic Reactions space to extravascular space (body tissues).
● Unpredictable adverse drug effects; more serious M = Metabolism, the chemical conversion or transformation of drugs into compounds
● Response to patient’s immunological system to the presence of the drug which are easier to eliminate.
● Do not occur unless the patient has been previously exposed to the agent/ E = Excretion, the elimination of unchanged drug or metabolite from the body via renal,
chemical related compound biliary, or pulmonary processes.
3. Idiosyncratic Reaction Processes:
● Occurs when the patient is first exposed to the drug 1. Liberation
● Abnormal reactivity to the drug caused by a genetic difference between the 2. Absorption
patient and normal individual. 3. Distribution
● a patient with G6PD deficiency will have anemia by using antioxidants. 4. Metabolism – biotransformation
4. Toxicity 5. Excretion - elimination
● The degree to which a drug can be poisonous and thus harmful to the human
body. Pharmaceutic Phase (dissolution)
5. Iatrogenic responses ● the 1st phase of drug action.
● Unintentional responses as a result of medical treatment ● In the GI tract, drugs need to be in solution so they can be absorbed.
● Nephrotoxicity; ototoxicity ● disintegrate into small particles to dissolve into a liquid.
WEEK 3 2 phases of Dissolution
PHARMACOKINETICS Disintegration – breakdown into smaller parts
is the process of drug movement throughout the body that is necessary to achieve drug Dissolution – further breakdown into smaller parts in GIT – absorption; dissolve into liquid
action.
When drug is taken by mouth, it undergoes 3 phases: Excipients
1.Pharmaceutic/dissolution ● Tablets are not 100% drug.
2. Pharmacokinetics ● Fillers and inert substances – excipients.
3. Pharmacodynamics ● Allow drug to take on particular size and shape and to enhance drug dissolution.
● Rate of dissolution is the time it takes the drug to disintegrate and dissolve to 2. ABSORPTION
become available for the body to absorb it. ● is the movement of the drug into the bloodstream after administration.
● 80% of drugs are taken by mouth – enteral.
Factors affecting Rate of Dissolution ● Movement of drug molecules from site of administration to circulatory system
● Form of drug ( LIQUID VS. SOLID) – liquids more absorbed than solid, already in Movement of drug particles from GIT to body fluids involve 3 processes:
solution, rapidly available for GI absorption 1. Passive transport
● Gastric ph ( acidic vs. alkaline) – acidic media faster disintegration & absorption Diffusion – drugs move across the cell membrane from an area of higher concentration
● normal gastric pH – 1.5-3.5 to one of lower concentration.
● Age – young & elderly – increase pH decrease absorption 2. Facilitated diffusion –Active transport – requires a carrier such as enzyme or protein to
move the drug against a concentration gradient. Energy is required.
Enteric coated drugs – resist disintegration in gastric acid Disintegration occurs only in 3. Pinocytosis – is the process by which cells carry a drug across their membrane by
alkaline environment ( intestine) Should not be crushed engulfing the drug particles in a vesicle.
Presence of food – interfere with dissolution & absorption, enhance absorption of other
drugs, may be protectants of gastric mucosa. Factors affecting drug absorption
Drug solubility – lipid soluble drugs pass readily through GI membrane, water- soluble
1. LIBERATION drugs need an enzyme or protein
is the first step in the process by which medication enters the body and liberates the Local condition at site of absorption- weak acids less ionized in stomach --Readily pass
active ingredient that has been administered. The pharmaceutical drug must separate through the small intestine.
from the vehicle or the excipient that it was mixed with during manufacture. Some authors Pain/stress/solid foods/fatty or hot foods- slows down gastric emptying time
split the process of liberation into three steps: disintegration, disaggregation and
dissolution. A limiting factor in the adsorption of pharmaceutical drugs is the degree to 3. DISTRIBUTION
which they are ionized, as cell membranes are relatively impermeable to ionized ● process by which drug becomes available to body fluids and tissues.
molecules. ● is the movement of the drug from the circulation to body tissues.
The characteristics of a medication's excipient play a fundamental role in creating a Factors affecting distribution:
suitable environment for the correct absorption of a drug. This can mean that the same 1. Size of the organ
dose of a drug in different forms can have different bioequivalence, as they yield different 2. Blood flow
plasma concentrations and therefore have different therapeutic effects. Dosage forms 3. Solubility- lipid soluble drugs can also cross the blood-brain barrier and enter the
with modified release (such as delayed or extended release) allow this difference to be brain.
usefully applied. Protein Binding
● as drugs are distributed in the plasma --- bind with plasma protein.
● albumin, lipoproteins, alpha-1-acid glycoprotein
4. METABOLISM Other Sites of Metabolism
● or biotransformation is the process by which the body chemically changes drugs 1. Plasma
into a form that can be excreted. 2. Kidneys
● First-pass effect or first-pass metabolism 3. Membranes of intestines
○ GI tract --- intestinal lumen -- liver---some drugs are metabolized to an
inactive form and excreted--- reduced amount of active drug Factors affecting biotransformation
○ liver enzymes – cytochrome P450 system – convert drugs to metabolites. 1. Genetic- some people metabolize drugs rapidly, others more slowly
○ decreased drug metabolism rate will result in excess drug accumulation 2. Physiologic
that can lead to toxicity. 3. Liver disease
○ Drug half-life is the time it takes for the amount of drug in the body to be 4. Infants- decreased rate of metabolism
reduced by half. 5. Elderlies- decreased liver size, blood flow, enzyme production- slows metabolism
Example: 6. Environment- cigarettes may affect the rate of some drugs.
Ibuprofen has a half life of about 2 hours. 7. Stressful environment- prolonged illness, surgery, illness.
● if the patient takes 200 mg, in 2 hours, 50% of the drug will be gone, leaving 100 mg.
● after 2 hours - 50 mg. 5. EXCRETION - ELIMINATION
● after 2 hours – 25 mg - removal of the drug from the body. Drug is changed into inactive form and excreted by
● after 2 hours – 12.5 mg the body.
● after 2 hours – 6.25 mg Routes:
● By knowing the half-life, the time it takes for a drug to reach a steady state ● Kidney- main organ for drug elimination: leave the body through urine
(plateau drug level) can be determined. ● Free or/unbound/water soluble drugs- filtered in the kidney
● it can be achieved when the amount of drug being administered is the same as ● (+) kidney disease- dose must be decreased.
the amount of drug being eliminated. ● kidneys – main route of drug excretion
● a steady state of drug concentration is necessary to achieve optimal therapeutic ● bile, lungs, saliva, sweat and breast milk.
benefit. ● urine pH influences drug excretion.
Half-life/ Elimination half-life (t ½)- time it takes for one half of drug concentration to be ● normal urine pH 4.6-8
eliminated ● acidic urine promotes elimination of weak base drugs.
● Short t1/2= 4-8hrs: given several times a day (ex. Penicillin G) ● alkaline urine promotes elimination of weak acid drugs.
● Long t ½ = >12 hours: given 2x or 1x/day (Ex. Digoxin) ● prerenal, intrarenal and postrenal conditions.
WEEK 4 database established during assessment provides a foundation for subsequent steps in
TERMINOLOGIES the process. Important methods of data collection are the patient interview, medical and
ASSESSMENT: information gathering regarding the current status of a particular patient, drug-use histories, the physical examination, observation of the patient, and laboratory
including evaluation of past history and physical examination; provides a baseline of tests. Two major aspects associated with assessment are the patient’s history (past
information and clues to effectiveness of therapy. illnesses and the current problem) and examination of his or her physical status.
EVALUATION: part of the nursing process; determining the effects of the interventions that
were instituted for the patient and leading to further assessment and intervention. Three reasons for obtaining a drug history
IMPLEMENTATION: actions undertaken to meet a patient’s needs, such as administration ● To evaluate need for medication
of drugs, comfort measures, or patient teaching. ● To obtain current and past use of over-the-counter medication
NURSING: the art of nurturing and administering to the sick, combined with the scientific ● To identify problems related to drug therapy
application of chemistry, anatomy, physiology, biology, nutrition, psychology, and Relies on three sources
pharmacology to the particular clinical situation. ● Primary source: produced by patient
NURSING DIAGNOSIS: statement of an actual or potential problem, based on the ● Secondary sources: relatives, significant others, medical records, lab reports
assessment of a particular clinical situation, which directs needed nursing interventions. ● Tertiary sources: literature to provide background information, diagnostic tests,
NURSING PROCESS: the problem-solving process used to provide efficient nursing care; it diet
involves gathering information, formulating a nursing diagnosis statement, carrying Comprehensive collection of data, including:
out interventions, and evaluating the process. a. History
● The patient’s past experiences and illnesses can influence a drug’s effect.
THE NURSING PROCESS ● This will help to promote safe and effective use of the drug and prevent adverse
● Utilizing steps of nursing process ensures that the interdisciplinary practice of effects, clinically important drug–drug, drug–food, or drug–alternative therapy
pharmacology results in safe, effective, and individualized medication interactions, and medication errors.
administration and outcomes for patients. b. Chronic Conditions
● Although not all nursing theorists completely agree on this process that defines ● Chronic conditions can affect the pharmacokinetics and pharmacodynamics of a
the practice of nursing, most do include certain key elements: assessment, nursing drug. Certain conditions (e.g., renal disease, heart disease, diabetes, chronic lung
diagnosis, implementation, and evaluation. Application of the nursing process with disease) may be contraindications to the use of a drug.
drug therapy ensures that the patient receives the best, safest, most efficient, c. Drug Use
scientifically based, holistic care. ● Prescription drugs, over-the-counter (OTC) drugs, street drugs, alcohol, nicotine,
1. Assessment (gathering information) is the first step of the nursing process. This alternative therapies, and caffeine may have an impact on a drug’s effect.
involves systematic, organized collection of data about the patient. The data must include Patients often neglect to mention OTC drugs or alternative therapies because they
information about physical, intellectual, emotional, social, and environmental factors for do not consider them to be actual drugs or they may be unwilling to admit their
holistic care. These data are used to identify actual and potential health problems. The use to the health care provider.
d. Allergies k. Age
● A patient’s history of allergies can affect drug therapy. Past exposure to a drug or ● The child’s developmental age will influence pharmacokinetics and
other allergens can provoke a future reaction or necessitate the need for cautious pharmacodynamics; the immature liver may not metabolize drugs in the same
use of the drug, food, or animal product. way as in the adult, or the kidneys may not be as efficient as those of an adult. As
e. Level of Education and Understanding patients age, the body undergoes many normal changes that can affect drug
● Gathering information about the patient’s level of understanding about his or her therapy, such as a decreased blood volume, decreased gastrointestinal
condition, illness, or drug therapy helps the nurse to determine where the patient is absorption, reduced blood flow to muscles or skin, and changes in receptor-site
in terms of his or her status and the level of explanation that will be required. responsiveness.
Stress, disease, and environmental factors can all affect a patient’s learning
readiness and ability. 2. Nursing Diagnosis
f. Social Support The nurse analyzes the database to determine actual and potential health problems.
● Patients are being discharged from health care facilities earlier than ever before, These problems may be physiologic, psychologic, or sociologic. Each problem is stated in
often with continuing care needs. Often patients need help at home with care and the form of a nursing diagnosis, which can be defined as an actual or potential health
drug therapy. problem that nurses are qualified and licensed to treat.
g. Financial Supports
● Financial constraints may cause a patient not to follow through with a prescribed A complete nursing diagnosis consists of two statements:
drug regimen. For example, the drug may be too expensive or the patient may lack (1) a statement of the patient's actual or potential health problem, followed by
the means to get to a pharmacy to obtain the drug. In some situations, a less (2) a statement of the problem's probable cause or risk factors.
expensive drug might be appropriate in place of a very expensive drug. Typically, the statements are separated by the phrase related to, as in this example of a
h. Pattern of Health Care drug-associated nursing diagnosis: “noncompliance with the prescribed regimen [the
● Knowing how a patient seeks health care provides the nurse with valuable problem] related to inability to self-administer medication [the cause].”
information to include when preparing the patient’s teaching plan. Information Five Types of Nursing Diagnosis
about patterns of health care also provides insight into conditions that the patient ● Actual: based on human responses and supported by defining characteristics
may have but has not reported or medication use that has not been stated. ● Risk/high-risk: patient may be more susceptible to a particular problem
i. Physical Examination ● Possible: suspected problems requiring additional data
● To determine if any conditions exist that would be contraindications or cautions for ● Wellness: clinical judgment about a transition from one level to a higher level
using the drug and to develop a baseline for evaluating the effectiveness of the ● Syndrome: cluster signs and symptoms to predict certain circumstances or events
drug and the occurrence of any adverse effects.
j. Weight 3. Planning
● A patient’s weight helps to determine whether the recommended drug dose is In the planning step, the nurse delineates specific interventions directed at solving or
appropriate. preventing the problems identified in analysis. The plan must be individualized for each
patient. When creating a care plan, the nurse must define goals, set priorities, identify a. Proper Drug Administration
nursing interventions, and establish criteria for evaluating success. In addition to nursing The nurse must consider seven points, or “rights,” to ensure safe and effective drug
interventions, the plan should include interventions performed by other healthcare administration.
providers. Planning is an ongoing process that must be modified as new data are 1) Right drug and patient,
gathered. 2) Right storage of drug,
Four phases of a nursing care plan 3) Right and most effective route,
a. Setting priorities 4) Right dose,
● Identify problems and prioritize which ones are more important and must be 5) Right preparation,
attended to first, depending on patient needs 6) Right timing, and
b. Developing measurable goal/outcome statements 7) Right recording of administration.
● Write short- and long-term goals for the patient to be followed when providing ● Remembering to review each point before administering a drug will help to
care prevent medication errors and improve patient outcomes.
c. Formulating nursing interventions and
d. Formulating anticipated therapeutic outcomes b. Comfort Measures
● Plan which intervention to use based on anticipated patient behavior A patient is more likely to be compliant with a drug regimen if the effects of the regimen
are not too uncomfortable or overwhelming.
4. Implementation
Involves taking the information gathered and synthesized into nursing diagnoses to plan c. Placebo Effect
the patient care. This process includes setting goals and desired patient outcomes to The anticipation that a drug will be helpful (placebo effect) has proved to have
assure safe and effective drug therapy. These outcomes usually involve ensuring effective tremendous impact on the actual success of drug therapy. For example, a back rub, a
response to drug therapy, minimizing adverse effects, and understanding the drug kind word, and a positive approach may be as beneficial as the drug itself.
regimen.
Nursing actions are suggested d. Managing Adverse Effects
● Dependent actions: performed by a nurse based on health care provider’s orders Such interventions include environmental control (e.g., temperature, light), safety
● Interdependent actions: implemented with the cooperation of a team measures
● Independent actions: provided by nurse by virtue of education and license (e.g., avoiding driving, avoiding the sun, using side rails), and physical comfort measures
(e.g., skin care, laxatives, frequent meals).
Three types of nursing interventions are frequently involved in drug therapy:
a. drug administration
b. provision of comfort measures
c. patient/family education.
e. Lifestyle Adjustment ● FRIED’S RULE:
Some medications and their effects require that a patient make changes in his or her CHILD’s DOSE = ADULT DOSE X AGE IN MONTHS
lifestyle. For example, patients taking diuretics may have to rearrange their day so as to 150
be near toilet facilities when the drug action peaks. Patients taking bisphosphonates will ● DOSE = DESIRED DOSE X QUANTITY
need to plan their morning so they can take the drug on an empty stomach, stay upright STOCK
for at least one-half hour, and plan their first food of the day at least one-half hour after ● CALCULATING INTRAVENOUS FLUID RATE:
taking the drug. RATE = AMOUNT TO BE INFUSED x DROP FACTOR
HOUR OF INFUSION 60 MINUTES / HOUR
f. Patient and Family Education
With patients becoming increasingly responsible for their own care, it is essential that they WEEK 5
have all of the information necessary to ensure safe and effective drug therapy at home. TERMINOLOGIES
In fact, many states now require that patients be given written information. Neurotransmitters
= chemicals in the body acting as messengers
5. Evaluation Sympathetic Nervous System
Evaluation is part of the continuing process of patient care that leads to changes in = a branch of peripheral nervous system involved in preparing the body for stress-related
assessment, diagnosis, and intervention. The patient is continually evaluated for activities
therapeutic response, the occurrence of adverse drug effects, and the occurrence of = “ fight or flight “
drug–drug, drug–food, drug–alternative therapy, or drug–laboratory test interactions. In Parasympathetic Nervous System
some situations, the nurse evaluates the patient simply by reapplying the beginning steps = associated with returning the body to routine, day-to-day operations
of the nursing process and then analyzing for changes, either positive or negative. The = “ rest and digest “
process of evaluation may lead to changes in the nursing interventions being used to Adrenergic
provide better and safer patient care. = means “working on adrenaline (epinephrine) or noradrenaline (norepinephrine) (or on
their receptors)
DRUG CALCULATION: Cholinergics
● CLARK’S RULE: = means “working on acetylcholine or on their receptors
CHILD’s DOSE = ADULT DOSE X WEIGHT IN POUNDS
150 Introduction
● YOUNG’S RULE: Drugs affecting the nervous system alter its functions. A thorough review of the anatomy
CHILD’s DOSE = ADULT DOSE X AGE IN YEARS and physiology of the Central Nervous System and Autonomic System would help
AGE IN YEARS + 12 students understand the mechanisms of actions of drugs. The functional unit, neurons
basic function is impulse transmission which happen by electrical and chemical process.
Electrical transmission of impulses happen by action potential and chemical process PARASYMPATHETIC NERVOUS SYSTEM
make use of neurotransmitters to achieve its functions. Parasympathetic nervous system (PNS) comes from the cranio – sacral outflow of the
peripheral nervous system. Cranial nerve X, IX, VII, III participate in the cranial flow. Majority
Central Nervous System of the PNS comes from cranial nerve X ( Vagus nerve ). This is the only cranial nerves that
Brain & Spinal Cord – very important structure of the CNS is its protective mechanisms extend up to the thorax and abdomen to supply majority of parasympathetic innervation,
that not all chemicals can pass through it, this affects the pharmacodynamics of drugs so a vagal stimulation is synonymous with parasympathetic innervation. Sacral nerves
because some of them cannot penetrate the CNS. One vital protective structure is the also participate in the PNS to supply mostly the effectors in the pelvic area like urinary
Blood Brain Barrier (BBB). This represents therapeutic challenge to drug treatment of brain bladder.
related disorders because a large percentage of drugs are carried bound to plasma
proteins and are unable to cross the brain. The ganglia of the PNS are located near the organ of innervation. The neurons therefore of
the PNS are pre – ganglionic neuron, the neuron from the Cranio – sacral outflow to the
Peripheral Nervous System ganglia and the post – ganglionic neuron, the neuron from the ganglia to the organ of
Autonomic Nervous System & Somatic Nervous System – Synapses made by the innervations. PNS is responsible for “REST AND DIGEST” involuntary responses of the body
peripheral nervous system conduct impulses that is chemical in nature. These
neurotransmitters have specific receptors in the neural membrane to facilitate Impulses transmitted across the synapses of the ganglia are mediated also by the
conduction of nerve impulses. Drugs may act in the nervous system to either stimulate or neurotransmitters.
block the receptors to correct alterations in the nervous functions.
In the PNS, the neurotransmitter is Acetylcholine. Receptors for acetylcholine are located
Neurons conduct impulses by Action Potential, the rapid change in the membrane in the post synaptic neuronal membrane. These receptors are called cholinergic
potential, this happens by movement of sodium into the cells causing depolarization and receptors.
potassium out of the cells to cause repolarization. This movement of ions facilitated by There are 2 types of cholinergic receptors
channels in the cell membranes will be acted upon by drugs to correct changes in the 1. Nicotinic Receptors
nervous system causing disease process. 2. Muscarinic receptors
AUTONOMIC NERVOUS SYSTEM SYMPATHETIC NERVOUS SYSTEM
The division of the peripheral nervous system that supply involuntary muscles, glands and The division of the autonomic nervous system, Sympathetic nervous system (SNS) from
other effectors not innervated by the somatic nervous system. Autonomic nervous system the thoraco- lumbar outflow, spinal nerves from this region send nerve fibers to the
is responsible for all involuntary actions of the body that the person is not aware of. This is sympathetic ganglia located near the CNS, then post ganglionic neurons send
divided into two divisions: innervation to the involuntary muscles and glands and other effectors mostly associated
with involuntary process in the body.
The preganglionic neuron of the SNS is shorter than PNS and the post ganglionic neuron is Most of the effectors are innervated by both sympathetic and parasympathetic and in
longer than PNS. SNS is responsible for “FIGHT OR FLIGHT” involuntary responses of the such case the response of the body is opposite. See examples below:
body. Impulses transmitted across the synapses also are mediated by the Effectors SNS PNS
neurotransmitters. There are two neurotransmitters in the SNS. Acetylcholine and Heart Increase HR Decrease HR
Epinephrine and Norepinephrine ( Catecholamines ) Lungs Bronchodilate Bronchoconstrict
Blood vessels Vasoconstrict Vasodilate
Acetylcholine is released by the preganglionic neurons, while epinephrine and
norepinephrine are the neurotransmitters released by the post ganglionic neurons, except Therefore, if a drug stimulates the receptors for PNS, it is called cholinergic agonist,
for those post ganglionic neurons innervating adrenal medulla, pilo erector muscles, enhancing PNS effect so such drug is also referred to as parasympathomimetic drug. A
sweat glands and some smooth muscles of the blood vessels, they have sympathetic drug that blocks the cholinergic receptors is called cholinergic antagonist, also called
innervations but the neurotransmitter in at the postganglionic neurons is Acetylcholine anticholinergic drugs, inhibiting PNS response and such drug may also be referred to as
parasympatholytic drug
Epinephrine and Norepinephrine may also be called Adrenalin and Noradrenaline
respectively or they are being referred to as catecholamines. Their receptors are called If a drug stimulates receptors for SNS, it is called adrenergic agonist, increasing SNS effect
Adrenergic Receptors. so such drug is also referred to as sympathomimetic drugs. A drug that blocks the
There are 2 types of adrenergic receptors adrenergic receptors decreases SNS responses called adrenergic agonist or it is also
1. Alpha receptors called sympatholytic drugs.
2. Beta receptors
Drugs affecting the Autonomic Nervous System are called Autonomic Drugs Remember, knowing the responses of the PNS and SNS is very important to understand
actions of autonomic drugs, because these drugs would only stimulate or block the
Classifications of Autonomic Drugs receptors.
● Drugs affecting the PNS are called Cholinergic Drugs
● Drugs affecting the SNS are called Adrenergic Drugs Cholinergic drugs – majority of these drugs affect the PNS.
● Direct acting cholinergic agonist – directly stimulates the cholinergic receptors to
In the study of pharmacodynamics, one action of the drugs is its binding with the increase its effects
receptors that may stimulate the receptors (drugs are called agonist) and drugs that ○ Pharmacokinetics: well absorbed with relatively short half – life.
may block the receptors (drugs are called antagonists). If a student is aware of the Metabolism and excretion may occur at the synaptic level but exact
responses of the PNS and SNS, it would be easier to remember drug actions, they would mechanism is unknown
either stimulate the receptors and produce the same effect or block the receptors or ○ Contraindications and Cautions: These drugs enhance parasympathetic
inhibit the effects. effect so must not be given to patients with hypotension, bradycardia or
heart block, intestinal obstruction and urinary retention.
○ Adverse effects: These are related to increase parasympathetic responses ● Neostigmine, Physostigmine, Pyridostigmine – long acting anticholinesterase
such as bradycardia, diarrhea, urinary incontinence. Increase sweating drugs used for therapeutic purposes. The onset of action starts 20 to 30 minutes
may happen because of the acetylcholine present in the sweat glands. and may last for 3 – 6 hours.
○ Drug – Drug interaction: Effects of these drugs maybe increase if
combined with anticholinesterase drugs or the indirect acting cholinergic Alzheimer’s Disease is a degenerative disease of the CNS characterized by loss of
agonists. neurons in the CNS which may slow down impulse transmission across the synapses of
○ Examples the CNS. One important cause of this is explained by loss of acetylcholine receptors in the
1. Bethanechol – indicated for non – obstructive urinary retention like in post synaptic neurons, like myasthenia gravis, less receptors mean lesser impulse
neurogenic bladder transmission. So anticholinesterase drugs that inhibit acetylcholinesterase enzyme will
2. Carbachol – indicated for glaucoma, causing pupillary constriction increase acetylcholine effect and promote impulse transmission in the CNS. Can drugs for
3. Pilocarpine – indicated for glaucoma, causing pupillary constriction myasthenia gravis be used to patients with Alzheimer’s disease? The answer is no simply
● Indirect acting cholinergic agonist – this drug increases acetylcholine effect by because those drugs cannot pass the BBB. Therefore, Alzheimer’s disease will have its own
inhibiting the action of acetylcholinesterase (an enzyme that removes anticholinesterase drugs.
acetylcholine in the synapse. If acetylcholinesterase is not removed in the synaptic
cleft, more acetylcholine stays in the synapse stimulating more receptors, thus Acetylcholinesterase drugs used for Alzheimer’s disease are called Anti Alzheimer’s drugs
enhancing their effects. These drugs are used for treatment of Myasthenia gravis which include
and Alzheimer’s disease ● Rivastigmine
● Donepezil
Myasthenia gravis is an autoimmune disease of the neuromuscular junction (NMJ). This ● Tacrine
is characterized by destruction of cholinergic receptors at the NMJ that will slow down ● Pharmacokinetics: These drugs are well absorbed and distributed in the body. Drugs
impulses going to the skeletal muscles. This disease is characterized by the development for myasthenia do not pass the BBB. The drugs are metabolized in the liver and excreted
of muscle weakness and paralysis. To increase junctional transmission, indirect acting in the urine.
cholinergic agonist inhibits acetylcholinesterase making more acetylcholine present in ● Contraindications and Cautions: The drugs are not given to those with known allergy to
the junction to improve impulse transmission and muscle function. These drugs are also the drugs. The drugs may exacerbate bradycardia, diarrhea and urinary incontinence
called anticholinesterase drugs. ● Adverse effects: Exacerbation of parasympathetic effects may be seen in the patient
such as bradycardia, hypotension and incontinence
Anticholinesterase drugs for Myasthenia gravis include: ● Nursing Considerations
● Edrophonium HCL (Tensilon) – short acting anticholinesterase drug used to ● Properly administer eye medication
diagnose the disease. The action lasts for 10 to 20 minutes. ● Slow IV administration to avoid severe cholinergic effects
● Cholinergic agonist oral preparation must be taken with an empty stomach to
decrease nausea and vomiting
● Closely monitor vital signs and exacerbation of parasympathetic effects ● Scopolamine – use in motion sickness, indicated to decrease secretion, pupil
● Provide safety measures dilation
● Monitor patients with Alzeimer’s disease for progression of the disease. Drugs will ● Adrenergic drugs these drugs act to either stimulate or block the adrenergic receptors
not cure the disease in the SNS
● Monitor patients with Myasthenia gravis for underside or overdose of medication ● Adrenergic agonist – stimulate the receptors to increase sympathetic effect and
● Provide health teaching on the name of drugs, its action and adverse effects to is also referred to as sympathomimetic drugs
promote client’s understanding and compliance ● Adrenergic antagonist – block the receptors to decrease sympathetic effect and
● Provide emotional support and encouragement to help the patient cope with drug is also referred to as sympatholytic drugs
regimen
Adrenergic receptors have 2 types and subtypes. Classification is based on their actual
Cholinergic antagonist also being referred to as anticholinergic drug or locations in the body. Below are some adrenergic receptor sites and their specific
parasympatholytic. The drugs act to block the cholinergic receptors in the PNS. The drugs locations in the body
may also block some cholinergic receptors present in the SNS.
● Pharmacokinetics: The drugs are well absorbed and distributed. Drugs pass the Types of the Adrenergic Receptors
BBB, placenta and breastmilk. The drugs are excreted in the urine. 1. Alpha receptors
● Contraindications and Cautions: The drugs are not given to patients with known a. Alpha 1 receptors
allergy to the drugs. Should not be used in clients with cardiovascular, b. Alpha 2 receptors
gastrointestinal or genitourinary conditions because they may exacerbate 2. Beta receptor
anticholinergic effect add worsen the conditions. Contraindicated in client with a. Beta 1 receptors
glaucoma as the drug may cause pupillary dilation and further increase b. Beta 2 receptors
intraocular pressure. Caution is used to patients with hepatic or urinary Study the table below for some important locations of the receptors
impairment. RECEPTORS LOCATION
● Adverse effects: These are associated with anticholinergic effects of drugs such as Alpha 1 receptors Vascular smooth muscles, iris, visceral smooth muscles
drying of the mouth, constipation, urinary retention, tachycardia, mydriasis. like the urinary bladder and iris
Drowsiness, confusion and insomnia are all related to the CNS effects of Alpha 2 receptors CNS neurons, pancreatic islets
anticholinergic drugs Beta 1 receptors Myocardium, Kidneys, CNS neurons
Examples: Beta 2 receptors Visceral smooth muscles like in the lungs, some vascular
● Atropine – indicated to decrease secretions, treat bradycardia, pylorospams, smooth muscles, CNS neurons
ureteral colic, cause pupil dilation (mydriasis) indicated as preop drug for For the sake of the discussion and the given examples of drugs, the effects of some of
cataract extraction. Use as antidote for cholinergic crisis drugs in particular receptors will be discussed first.
● Dicyclomine – use for hyperactive bowel in adults
Alpha 1 receptors when stimulated will cause vasoconstriction, pupillary dilation and 2. Alpha specific adrenergic agonist – these drugs specifically stimulate only the alpha
closure of urinary bladder sphincter causing urinary retention. receptors and not the beta receptors
● When the receptors are block? What would be the expected effects? ● Pharmacokinetics: these drugs are well absorbed and distributed, reach peak levels in
20 to 45 minutes. These drugs are metabolized in the liver and excreted in the urine
Alpha 2 receptors in the CNS neurons when stimulated will decrease norepinephrine flow ● Contraindications and Cautions: these drugs are not indicated to clients with allergy to
from the CNS to the SNS therefore decreasing sympathetic response. Take note that this is the drugs, those with hypertension and close angle glaucoma. Caution is used in clients
the drug that stimulate adrenergic receptors but decreasing SNS effect because the with cardiovascular disease.
receptors being stimulated are located in the CNS. ● Adverse effects: these are related to the overdose of drugs that may increase
sympathetic effects like hypertension, gastrointestinal depression and genitourinary
Beta 1 receptors in the heart when stimulated will increase heart rate. When we use a effects like urinary retention
drug that blocks the receptor, what is the effect? ● Examples
● Alpha 1 adrenergic agonist – Phenylephrine used for treatment of common colds
Beta 2 are located in the lungs, if we use a drug that stimulates receptors, the effect is and allergy. This drug causes vasoconstriction to lessen congestion in the nose
bronchodilation, what is the effect if we block the receptor? therefore called decongestants.
● Alpha 2 adrenergic agonist – Clonidine better known for its brand name as
Classifications of Adrenergic Agonist Drugs Catapres acting on the CNS neurons to decrease norepinephrine flow. This drug is
1. Alpha and Beta adrenergic drugs ( Sympathomimetic drugs ) – these drugs stimulate indicated for treatment of hypertension.
all adrenergic receptors to enhance their effects. 3. Beta specific adrenergic agonist – these drugs specifically stimulate the beta
● Pharmacokinetics: these drugs are rapidly absorbed, metabolized in the liver and receptors and not the alpha receptors.
excreted in the urine. These drugs may cross the placenta and breastmilk ● Pharmacokinetics: well absorbed and distributed in the body, metabolized in the liver
● Contraindications and Cautions: Should not be given in client with allergy to these and excreted in the urine. The drugs pass the placenta and breastmilk, use in pregnancy
drugs and to patients with pheochromocytoma as the drugs may exacerbate the signs and lactation only if benefits outweigh the risks
and symptoms ● Contraindications and Cautions: The drugs are contraindicated in clients with allergy
● Adverse effects: These are all related to increase SNS response like tachycardia, to the drugs. Caution is used in clients with cardiovascular disease like hypertension and
hypertension, constipation, urinary retention, pupillary dilation tachycardia.
● Examples ● Adverse effects: These are related to the primary effects of drugs which will increase
● Epinephrine – the drug of choice during CPR, indicated for treatment of shock sympathetic effects like hypertension and tachycardia.
● Dobutamine – used for treatment of congestive heart failure ● Examples
● Dopamine – usually given for congestive heart failure and cardiogenic shock ● Isoproterenol – for treatment of cardiogenic shock and heartblock in transplanted
● Norepinephrine – like epinephrine, may be indicated for cardiac arrest heart.
● Salbutamol – for treatment of obstructive respiratory disease like COPD and ● Contraindications and Cautions: The drugs should not be given to clients with
bronchial asthma hypotension and urinary incontinence
● Nursing Considerations ● Adverse effects: related to the primary action of the drug causing vasodilation and
● Avoid sudden withdrawal of the drug because it may cause rebound hypertension, hypotension
arrhythmias and flushing ● Examples
● Monitor vital signs especially blood pressure and heart rate ● Phentolamine – more specific drug hypertension in pheochromocytoma, that will
● Avoid comfort measures including rest and environmental control to decrease have less adverse effects.
CNS irritation.
● Provide adequate health teaching on the name of drug, prescribed dosage, 3. Alpha 1 selective adrenergic antagonist – these drugs block only the alpha receptors,
effects and adverse effects to increase patient’s knowledge and subsequent specific drugs act on the alpha receptors on the blood vessels and urinary bladder to
compliance. case vasodilation for treatment of hypertension and bladder emptying for treatment of
urinary retention. Although some drugs may act in both blood vessels and urinary bladder
● Classifications of Adrenergic Antagonist Drugs (Sympatholytic drugs) at the same time
1. Alpha and Beta adrenergic antagonist – these drugs block all adrenergic receptors ● Pharmacokinetics: drugs are absorbed in the GIT, metabolized in the liver and excreted
● Pharmacokinetics: these drugs are well absorbed and distributed in the body, in the urine.
metabolized in the liver and excreted in the urine and the feces. ● Contraindications and Cautions: Contraindicated in clients with allergy to the drugs.
● Contraindications and Cautions: These drugs should not be given to clients with This may exacerbate hypotension and urinary incontinence. Caution is used to clients
allergy to the drugs. To those with hypotension and bradycardia. Caution is used in clients with cardiovascular disease, gastrointestinal and genitourinary conditions
with cardiovascular disease and obstructive lung disorders ● Adverse effects: related to the sympatholytic effect of drugs causing hypotension and
● Adverse effects: these mainly on the effects of the drugs in the lungs like urinary incontinence.
bronchospasm, blood vessels causing vasodilation and hypotension. ● Examples
● Examples ● Prazosin – indicated for treatment of hypertension
● Carvedilol ● Terazosin – indicated for treatment of hypertension and BPH causing urinary
● Labetalol retention
Both examples maybe indicated to clients with severe hypertension caused by ● Doxazosin – indicated for treatment of hypertension and BPH causing urinary
pheochromocytoma retention
● Alfuzosin indicated for treatment of BPH
2. Alpha adrenergic antagonist – these drugs block only the alpha receptors, specific ● Tamsulosin – indicated for treatment of BPH
drugs act on the alpha 1 and alpha 2 receptors.
● Pharmacokinetics: these drugs are well absorbed and distributed, metabolized in the
liver and excreted in the urine.
4. Beta adrenergic antagonists – these drugs block both beta 1 and beta 2 receptors, ● Avoid comfort measures including rest and environmental control to decrease
particularly affecting both the heart and the lungs, these drugs increase heart rate and CNS irritation.
bronchoconstriction of the lungs ● Provide adequate health teaching on the name of drug, prescribed dosage,
effects and adverse effects to increase patient’s knowledge and subsequent
5. Beta 1 specific adrenergic antagonist these drugs block specifically beta 1 receptors in compliance.
the heart. These drugs are most commonly known as beta blockers. These drugs are
indicated to clients with hypertension, dysrhythmias, angina and use to support cardiac
function in clients with congestive heart failure
● Pharmacokinetics: these drugs are absorbed in the gastrointestinal tract and undergo
hepatic metabolism. The presence of food may increase the bioavailability of some beta
blockers. These drugs are known teratogenic in animals as it passes the placenta and
breast milk
● Contraindications and Cautions: Contraindicated in clients with allergy to the drugs.
Caution should be used in clients with bradycardia and heart block as well on patients
with obstructive lung diseases like COPD and bronchial asthma
● Adverse effects: these are related to the bradycardia and bronchoconstriction effect of
the drug. Gastrointestinal effects like nausea and vomiting, genitourinary symptoms may
be disturbing to clients as well.
● Examples
● Beta adrenergic antagonists or Beta blockers
○ Propranolol
○ Pindolol
● Beta 1 specific adrenergic antagonists or Beta 1 blockers
○ Metoprolol
○ Atenolol
● Nursing considerations
● Avoid sudden withdrawal of the drug because it may cause rebound hypertension,
arrhythmias and flushing
● Monitor vital signs especially blood pressure and heart rate
● Monitor ECG
You might also like
- Nursing2021 Drug Handbook®, 41eDocument73 pagesNursing2021 Drug Handbook®, 41eangel marycor valdezNo ratings yet
- 1.1 Drug Classifications & FormsDocument528 pages1.1 Drug Classifications & FormsMoxie MacadoNo ratings yet
- Pharma Week 1-5Document25 pagesPharma Week 1-5Rachelle CambaNo ratings yet
- Ncma216: BSN 2Nd Year 1St Semester Prelim 2021: Bachelor of Science in Nursing 2YADocument32 pagesNcma216: BSN 2Nd Year 1St Semester Prelim 2021: Bachelor of Science in Nursing 2YAMARIA STEPHANY DELA CRUZ100% (1)
- Cdi 4 Drug Education and Vice Control 2013Document41 pagesCdi 4 Drug Education and Vice Control 2013Jhezzie Gutierrez100% (1)
- Drugs Education and Vice Control QuizDocument5 pagesDrugs Education and Vice Control QuizHEROWIN EDUARDO100% (1)
- Pharmaceutical Inorganic Chemistry (Lecture)Document10 pagesPharmaceutical Inorganic Chemistry (Lecture)yaoi yuriNo ratings yet
- Pharma Week 1-5Document33 pagesPharma Week 1-5Krystel Anne Milan100% (1)
- StructuresDocument7 pagesStructuresFarouk Ramadan100% (1)
- Study Guide-Pharmacology-PrelimDocument20 pagesStudy Guide-Pharmacology-Prelimcath payotNo ratings yet
- Question Bank For Pharmacology - WJP AnsweredDocument55 pagesQuestion Bank For Pharmacology - WJP AnsweredGeorge MoshiNo ratings yet
- PHARMACOLOGY Week 1Document13 pagesPHARMACOLOGY Week 1Bee LeriosNo ratings yet
- Module 1 M PharmaDocument15 pagesModule 1 M PharmaAlphine DalgoNo ratings yet
- Pharmacology Prelim TransesDocument26 pagesPharmacology Prelim TransesShene Claire VigillaNo ratings yet
- What is Pharmacognosy: The Study of Crude DrugsDocument44 pagesWhat is Pharmacognosy: The Study of Crude DrugsShruti RajNo ratings yet
- Pharmacology Chapterwise Year Questions 2nd Yr BdsDocument9 pagesPharmacology Chapterwise Year Questions 2nd Yr Bds76 S.SHRAVAN KUMARNo ratings yet
- CH 1 Pharma Cog Nosy IntroDocument82 pagesCH 1 Pharma Cog Nosy Introuzair khan100% (1)
- Introduction To PharmacologyDocument2 pagesIntroduction To PharmacologyJoy Ann Akia PasigonNo ratings yet
- Pharmacology LectureDocument45 pagesPharmacology LecturebjhilarioNo ratings yet
- Pharmacology - PrelimsDocument9 pagesPharmacology - PrelimsLou KristofferNo ratings yet
- NCM 206 - PharmacologyDocument17 pagesNCM 206 - PharmacologyJonathan RanocoNo ratings yet
- 216 - Pharma First WeekDocument4 pages216 - Pharma First WeekJessielyn FranciscoNo ratings yet
- Ncma216 PrelimDocument44 pagesNcma216 Prelimroldanmarygrace023No ratings yet
- PH CM1 Cu 1 - Basic Concepts in PharmacologyDocument20 pagesPH CM1 Cu 1 - Basic Concepts in Pharmacologyeli pascualNo ratings yet
- Pharma Prelim Cu1 Cu5Document59 pagesPharma Prelim Cu1 Cu5MARIA STEPHANY DELA CRUZNo ratings yet
- Pharmacology: BSN 2-YA-15 - de Leon, Sydney - PRELIM REVIEWER - 2022Document22 pagesPharmacology: BSN 2-YA-15 - de Leon, Sydney - PRELIM REVIEWER - 2022De Leon, Austine Sydney D.No ratings yet
- Introduction Definitions and Sources of DrugsDocument4 pagesIntroduction Definitions and Sources of Drugssindhu mNo ratings yet
- Introduction to the History and Principles of PharmacologyDocument2 pagesIntroduction to the History and Principles of PharmacologyNiacinth LoredoNo ratings yet
- PharmacologyDocument20 pagesPharmacologyKan JiNo ratings yet
- Introduction To Pharmacology: Presented ByDocument23 pagesIntroduction To Pharmacology: Presented BySanghmitra MauryaNo ratings yet
- The History of Pharmacy and Early Drug DevelopmentDocument35 pagesThe History of Pharmacy and Early Drug DevelopmentrenNo ratings yet
- Branches and concepts of pharmacologyDocument15 pagesBranches and concepts of pharmacologyZaira Reine SantosNo ratings yet
- PharmacokineticsDocument7 pagesPharmacokineticsRonica MendozaNo ratings yet
- Pharmacology Fundamental ConceptsDocument84 pagesPharmacology Fundamental Conceptsteaforschool filesNo ratings yet
- 223 NotesDocument36 pages223 NotesNing BalderasNo ratings yet
- Pharmacology BasicsDocument235 pagesPharmacology BasicsLaden SalehNo ratings yet
- Pharmacology ReviewerDocument9 pagesPharmacology ReviewerJeon CookyNo ratings yet
- Wa0001 PDFDocument105 pagesWa0001 PDFAyesha AbdulrahmanNo ratings yet
- Means - Means: Pharmakon GnosisDocument47 pagesMeans - Means: Pharmakon GnosisNasif Abdur RazzaqueNo ratings yet
- PCOLDocument2 pagesPCOLMichelle CasilangNo ratings yet
- Pharmacology IntroductionDocument18 pagesPharmacology IntroductionusamaNo ratings yet
- Quiz 1 PharmaDocument13 pagesQuiz 1 PharmaVanessa May BlancioNo ratings yet
- Pharmacognosy-I: Dr. Wafaa M.A. Alshakh HamedDocument81 pagesPharmacognosy-I: Dr. Wafaa M.A. Alshakh HamedАбу ДжудNo ratings yet
- MM Scope EvolutionDocument53 pagesMM Scope EvolutionSai RevanthNo ratings yet
- PHARMACOLOGYDocument19 pagesPHARMACOLOGYIligan, JamaicahNo ratings yet
- General PharmacologyDocument60 pagesGeneral PharmacologyHAMMADNo ratings yet
- Pharmacology Lab Sources Dosage FormsDocument5 pagesPharmacology Lab Sources Dosage FormsZllison Mae Teodoro MangabatNo ratings yet
- Pharmacology 1 1Document124 pagesPharmacology 1 1danilotinio2No ratings yet
- Unit 2 Pharmacology NotesDocument3 pagesUnit 2 Pharmacology Notessalted fishNo ratings yet
- Genaral Introduction - Pharmacology 16.03.2021Document65 pagesGenaral Introduction - Pharmacology 16.03.2021PHARMACOLOGY SMVMC100% (1)
- Introduction to Pharmacology: Effects of Drugs & Medication AdministrationDocument2 pagesIntroduction to Pharmacology: Effects of Drugs & Medication AdministrationAdri Sinclaire100% (1)
- General Pharmacology 2013Document403 pagesGeneral Pharmacology 2013tareNo ratings yet
- Topic 1 - Introduction To PharmacologyDocument4 pagesTopic 1 - Introduction To PharmacologyReanne Mae AbreraNo ratings yet
- PharmacologyDocument8 pagesPharmacologyJi-Han Abalo ImnidaNo ratings yet
- 01 General Pharmacology History IntroductionDocument10 pages01 General Pharmacology History Introductionpmily100% (1)
- Medication AdministrationDocument298 pagesMedication AdministrationChristille Grace Basa MuchuelasNo ratings yet
- Week 1 Introduction To PharmacologyDocument12 pagesWeek 1 Introduction To PharmacologyDino MicaNo ratings yet
- Pharma 1.2 Introductory Concepts - Dr. GarciaDocument5 pagesPharma 1.2 Introductory Concepts - Dr. GarciaAesthetics MinNo ratings yet
- PharmacologyDocument52 pagesPharmacologyKris Ann Yap-BonillaNo ratings yet
- Ancient Pharmacology History and DevelopmentDocument27 pagesAncient Pharmacology History and DevelopmentMarielle Joy FloraNo ratings yet
- Introduction & Drug Evaluation (Pharmaco)Document72 pagesIntroduction & Drug Evaluation (Pharmaco)Raquel MonsalveNo ratings yet
- Introduction To Nursing PharmacologyDocument5 pagesIntroduction To Nursing PharmacologyJon Adam Bermudez SamatraNo ratings yet
- Pharmacology- The Molecular Dance: Understanding Drug Interactions: Harmony and Chaos: The Symphony of Drug InteractionsFrom EverandPharmacology- The Molecular Dance: Understanding Drug Interactions: Harmony and Chaos: The Symphony of Drug InteractionsNo ratings yet
- Clinical Pharma (CC)Document14 pagesClinical Pharma (CC)Lucas Victor AlmeidaNo ratings yet
- Cc2lab TDM Part1Document3 pagesCc2lab TDM Part1Krisiah Anne HernandezNo ratings yet
- Laporan Obat Bantuan Tahun 2023 (ERA)Document6 pagesLaporan Obat Bantuan Tahun 2023 (ERA)hefikurniasariNo ratings yet
- Office: of The SecretaryDocument15 pagesOffice: of The SecretarySandrea SantosNo ratings yet
- Daftar Pembekalan Farmasi Klinik Prima Medika 2020Document4 pagesDaftar Pembekalan Farmasi Klinik Prima Medika 2020primamedikaNo ratings yet
- Price List September 2022Document61 pagesPrice List September 2022Ade IrawanNo ratings yet
- PQRI - Biosimilar OverviewDocument20 pagesPQRI - Biosimilar OverviewNgoc Sang HuynhNo ratings yet
- B. Pharm Fourth Semester Exam on Medicinal Chemistry IDocument1 pageB. Pharm Fourth Semester Exam on Medicinal Chemistry IMonicaNo ratings yet
- Data Logistik Untuk SO SIHA 2.1 KabKotaDocument34 pagesData Logistik Untuk SO SIHA 2.1 KabKotaTeti HerawatiNo ratings yet
- Price List - updaTED Sep 22 1Document6 pagesPrice List - updaTED Sep 22 1Stamina DaddyNo ratings yet
- 4 MG Drospirenone Only Pill New Data and A Review of The Literature PDFDocument8 pages4 MG Drospirenone Only Pill New Data and A Review of The Literature PDFJuly López LeitonNo ratings yet
- Gharama Za Matibabu PKP Kituo Cha AfyaDocument14 pagesGharama Za Matibabu PKP Kituo Cha AfyashaggyzegratNo ratings yet
- At The Pharmacy: A Dialogue Between A Pharmacist and A CustomerDocument3 pagesAt The Pharmacy: A Dialogue Between A Pharmacist and A CustomerPikm LarashatiNo ratings yet
- Precios Disfarma 04.10.2021Document9 pagesPrecios Disfarma 04.10.2021maxifarmaNo ratings yet
- Daftar Harga ApotikDocument68 pagesDaftar Harga Apotiknuriasni farmasiNo ratings yet
- Siap Print Untuk SimulasiDocument3 pagesSiap Print Untuk SimulasiRossa patria NandaNo ratings yet
- Rifamycins and Anti-Diabetic Agents Drug-Drug InteractionsDocument2 pagesRifamycins and Anti-Diabetic Agents Drug-Drug InteractionsmoniaNo ratings yet
- Lista de Precios 2Document20 pagesLista de Precios 2David GuillenNo ratings yet
- Compare Historic Drug Testing With Contemporary Drug Testing ProtocolsDocument2 pagesCompare Historic Drug Testing With Contemporary Drug Testing ProtocolsDinesha Sudarshani LiyanageNo ratings yet
- Therapeutic Interchange ListDocument29 pagesTherapeutic Interchange ListНазарій ЛавровськийNo ratings yet
- List Obat Kosong Farmasi 171121Document21 pagesList Obat Kosong Farmasi 171121Arif FirmansyahNo ratings yet
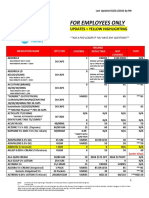
- Employee Only Pricing Sheet 02.11.22Document10 pagesEmployee Only Pricing Sheet 02.11.22rickyNo ratings yet
- Stok19 Apr 21Document92 pagesStok19 Apr 21Rama RakanataNo ratings yet
- Managecare GoldDocument42 pagesManagecare Goldmevi erayaniNo ratings yet