Professional Documents
Culture Documents
10 Year Article NEC
Uploaded by
Precious UncianoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
10 Year Article NEC
Uploaded by
Precious UncianoCopyright:
Available Formats
SERIES Beth Ulrich Cherilyn Hipps Ashlock
Charles Krozek Larissa Marquez Africa
Sean Early Michael L. Carman
Improving Retention, Confidence,
And Competence of New Graduate
Nurses: Results from a 10-Year
Longitudinal Database
1999, CHILDREN’S HOSPITAL evidence of positive outcomes for
I
N
EXECUTIVE SUMMARY Los Angeles (CHLA) found hospitals, new graduates, and
Developing competent and confi-
itself in the position of many patient care that is now provided
dent new graduate nurses who hospitals today; despite much in hospitals across the United
remain with their hospitals is a effort and expense to provide an States. The evolution of the RN
major challenge. inhouse internship for new gradu- residency, the lessons learned
A structured evidence-based RN ate nurses, the results were disap- along the way, and the outcomes
residency was developed and pointing. Turnover was high; 36% achieved are described, and a
implemented in hospitals across of the new graduates hired at model for successfully recruiting,
the United States. CHLA were leaving in less than a onboarding, engaging, and retain-
Outcomes data were collected year and 56% within 2 years. The ing new graduate nurses is pre-
from over 6,000 new graduate resulting cycle of hire-educate- sented.
nurses who completed the RN
replace was negatively impacting
residency over a 10-year period. Background
nursing and patient care. A vision-
The results indicate an accelerat-
ary chief nursing officer, a nursing The nursing shortage – past
ed increase in competence and
self-confidence and a significant education director, and a small and future. When the RN residen-
decrease in turnover intent and group of committed nurses cy began in 1999, the United
actual turnover. embarked on a quest to find a bet- States was at the beginning of the
This study provides persuasive ter way to bring new graduate most recent nursing shortage.
evidence that both new graduate nurses into the profession of nurs- Registered nurse (RN) vacancy
nurses and their organizations ing and into CHLA. Ten years of rates were up across the country
benefit from the implementation development, evaluation, and and enrollments in schools of
of a structured, clinical immersion improvement have resulted in a nursing were down (Buerhaus,
RN residency.
RN residency with documented Auerbach, & Staiger, 2009). In the
BETH ULRICH, EdD, RN, FACHE, FAAN, CHERILYN HIPPS ASHLOCK, MSN, RN, NOTE: The authors reported they are
is Senior Vice President, Versant, Houston, is Director, Versant, Fayetteville, GA. employees of Versant. All Nursing
TX. Economic$ Editorial Board members
LARISSA MARQUEZ AFRICA, MBA, reported no actual or potential conflict of
CHARLES KROZEK, MN, RN, FAAN, is BSN, RN, is Assistant Vice President, interest in relation to this continuing
Managing Partner, Versant, Los Angeles, Versant, Los Angeles, CA. nursing education article.
CA.
MICHAEL L. CARMAN, JD, MBA, AB, is
SEAN EARLY, PhD, is Director, Versant, Managing Partner, Versant, Ithaca, NY.
Los Angeles, CA
NURSING ECONOMIC$/November-December 2010/Vol. 28/No. 6 363
Improving Retention, Confidence, and Competence of New Graduate Nurses:
Results from a 10-Year Longitudinal Database
SERIES
ensuing years, the nursing short- continue to be hard pressed to fit ate influx of appropriately desig-
age persisted and worsened. The everything new graduate nurses nated resources to address the
enrollments in schools of nursing need to begin their careers into the shortages, along with appropriate
increased, but not enough to offset limited time and limited clinical policy changes, it would take
the shortage. It was not until the opportunities available. The readi- many years to yield results” (p. 7).
economic downturn that the ness of new graduates to function RN turnover cost. RN turnover
shortage began to abate. Exper- as RNs continues to be in ques- is costly to organizations in terms
ienced nurses came back into the tion. Del Bueno (2005), in review- of quality of patient care, sustain-
workplace in large numbers and ing 10 years of data for new nurs- ability of the professional nursing
they increased the number of hours es on the performance-based organization, and in both direct
worked. Buerhaus and colleagues development system, found that and indirect financial costs. Jones
(2009) reported that in 2007 and 65%-76% of inexperienced RNs (2008) calculated the replacement
2008, hospital RN employment did not meet the expectations for cost of each new nurse in 2007 as
increased by 243,000, the largest 2- entry-level clinical judgment and $82,000 to $88,000 each. Price
year increase in the last 4 decades. the majority had difficulty trans- Waterhouse Coopers, in 2007, esti-
This influx of nurses coupled with lating knowledge and theory into mated that every percentage point
the negative effect the recession practice. In developing the increase in nurse turnover costs an
had on the economic health of Quality and Safety Education for average hospital about $300,000
many health care organizations Nurses (QSEN) program, Smith, annually. Replacing new graduate
resulted in low RN vacancy rates Cronenwett, and Sherwood (2007) nurses who require additional
in many hospitals and lulled found that neither QSEN faculty resources and non-productive
many hospital executives into and advisory board members or time to onboard can be especially
relaxing their efforts to recruit and queried nursing school faculty costly.
retain RNs. and new graduates felt that quali- In addition, the churn created
Buerhaus (2009) described the ty and safety competencies and by excessive turnover and the
often repeated econometric model their accompanying knowledge, resulting number of newly hired
of RN labor market participation; skills, and attitudes were being staff, part-time staff, and tempo-
when the national unemployment developed by nursing students rary (agency) staff has also been
rate rises, RNs re-enter the labor while in school. identified as a detriment to organ-
market and those already in the Berkow, Virkstis, Stewart, and izations and patients. Duffield,
market increase their work hours. Conway (2008), in a study for the Roche, O’Brien-Pallas, & Catling-
When the unemployment rate Advisory Board Company, sur- Paull (2009) found downstream
declines, RNs withdraw from the veyed nursing school leaders and effects of churn included adverse
labor market. The recent positive hospital nurse executives. When outcomes for patients, lack of con-
economic indicators suggest that asked for their degree of agree- tinuity of care, additional time
such withdrawal will begin to ment with the statement “overall, required to manage employees,
happen again in the near future. In new graduate nurses are fully pre- and loss in staff productivity.
addition, baby boomer nurses are pared to provide safe and effective The need for RN residencies.
closer to aging out of the work- care in the hospital setting,” The need to assure an ongoing
force and the recently enacted 89.9% of the nursing school lead- supply of competent RNs who are
health reform laws are predicted ers agreed versus only 10.4% of prepared to practice in acute care
to increase the demand for health the hospital nurse executives. settings and who will remain in
care and the opportunities and Results from a national survey of those settings requires a change in
need for nurses (Institute of new graduate nurses conducted in how new graduate nurses are tran-
Medicine [IOM], 2010). “Unless 2004-2005 further supported the sitioned into professional nurses.
there is significant progress in existence of a gap in the readiness The National Council of State
expanding the size of the future of new graduate nurses to practice Boards of Nursing (2009) has been
nursing workforce, realizing the (Kovner et al., 2007; Pellico, diligent in developing and docu-
goals of health care reform will be Brewer, & Kovner, 2009). Most menting an evidence base on the
difficult” (Buerhaus et al., 2009, p. recently, Benner, Sutphen, Leonard, need for a transition to practice
w667). The decreased supply of and Day (2010, p. 4) found “a sig- model. In addition, the need for
and increased demand for nurses nificant gap exists between today’s nurse residencies has recently
is a recipe for another even more nursing practice and the educa- been supported by the Carnegie
intense nursing shortage in the tion for that practice, despite some study on nursing education
coming years. considerable strengths in nursing (Benner et al., 2010) and the
Preparing new nurses. While education,” and further noted IOM/RWJF study on the future of
increased enrollment in schools of “Even if nursing and nursing edu- nursing (IOM, 2010).
nursing is positive, the schools cation were to receive an immedi-
364 NURSING ECONOMIC$/November-December 2010/Vol. 28/No. 6
Improving Retention, Confidence, and Competence of New Graduate Nurses:
Results from a 10-Year Longitudinal Database
SERIES
Development of the Versant® RN additional children’s hospitals in classes with case studies, struc-
Residency California participated in the beta tured clinical immersion experi-
The RN residency began in phase of the research. By July ences with team precepting, struc-
1999 as a 1-year pilot with an 2003, 118 new graduates complet- tured mentoring and debriefing/
average of 716 hours of guided ed the residency at the beta sites. self-care sessions, looping to related
clinical experience with a one-on- The results from that phase indi- departments, and competency vali-
one preceptor, a mentor for each cated the RN residency was scala- dation. The initial development of
new graduate, debriefing and self- ble to other hospitals, but it also the RN residency curriculum has
care sessions to discuss issues became clear that deploying the been documented previously
new graduate nurses face and residency on a national basis (Beecroft, Kunzman, Taylor, Devenis,
strategies to deal with them, loop- would require a business model & Guzek, 2004). Briefly, the evi-
ing that involved clinical experi- and the addition of a way to easily dence-based curriculum initially
ences in other areas of the hospital collect, access, and share data was based on Benner’s novice-to-
along the care continuum perti- and information. CHLA created expert framework (Benner, 1984);
nent to the new graduate’s patient Versant® in 2004 and launched a stakeholder interviews including
population, and an average of 225 web-based management system, nurse managers who had hired
hours of classroom time with Voyager®, which included access to and worked with new graduates,
hands-on skills training laborato- the RN residency curriculum com- preceptors who had worked with
ries. The goals of the pilot were to ponents, measurement instru- new graduates, and new graduates
facilitate transition of new gradu- ments, and individual resident in- themselves; and on a standardized
ate nurses to professional RNs, formation on competency achieve- job analysis procedure – the
prepare beginning-level staff nurs- ment and progression toward Develop A CUrriculuM (DACUM)
es who are confident and provide goals. In 2004, the RN residency competency-based analysis (Norton,
competent and safe patent care, was beta tested in general acute 1997). The RN residency contin-
and increase the commitment and care hospitals with successful ues to be based on Benner’s frame-
retention of new graduate nurses results. The RN residency was work, emphasizing the novice to
within the organization (Beecroft, then offered to both childrens hos- expert progression for residents as
Kunzman, & Krozek, 2001). pitals and general acute care hos- well as for preceptors, mentors,
A number of measures were pitals across the United States. debriefers, and subject matter
used to evaluate the pilot. These The development of the RN experts. Additional competency
included self-report and observa- residency was initially treated as a analyses have been completed as
tion instruments whose reliability research endeavor and all partici- new specialties have been added
and validity had been established pating organizations obtained to the RN residency. There is a
previously as well as demographic institutional review board ap- core curriculum for all new gradu-
and evaluation instruments devel- proval prior to implementing the ates and specialty curricula have
oped for the pilot. The pilot, the RN residency. As the RN residen- been developed in medical-surgi-
measures used, and the results cy was deployed in hospitals cal nursing, critical care, emer-
have been described in detail in a throughout the country, the gency nursing, perinatal nursing,
previous publication (Beecroft et research focus continued. Begin- neonatal ICU, perioperative serv-
al., 2001). Results indicated the ning in 2009, with 10 years of evi- ices, and pediatrics. The curricula
graduates of the pilot residency dence-based outcomes showing are reviewed and updated on a
program had equal or better the success of the RN residency, routine basis and more often if
results on all measures when com- Versant moved the RN residency indicated to remain current with
pared to a comparison group of out of traditional research status; practice standards, new clinical
new graduates hired by CHLA in however, essential attributes of the evidence, and feedback from RN
the 2 years prior to implementing research protocol have been residency participants and stake-
the residency. In the following retained. Data collection protocols holders.
year, the pilot was continued with continue to be followed including Clinical immersion. Clinical
an additional 56 graduates and confidentiality of resident res- immersion is vital to the success
some modification of measure- ponses in measurement instru- of new graduates. A critical aspect
ment instruments, notably adding ments and evaluations. Data are of the new graduate’s clinical
direct observations of a sample of only included in the Versant immersion is dedicated precep-
the new graduates in each cohort National Database if they meet tors. Preceptors are educated in
using the Slater Nursing Compe- established criteria. working with new graduates. The
tencies Rating Scale (Wandelt & RN residency began by using the
RN Residency: Overview traditional model of precepting –
Stewart, 1975).
Following the pilot, three Curricula. The Versant RN assigning a preceptor and an alter-
Residency curriculum includes nate preceptor, and using the same
NURSING ECONOMIC$/November-December 2010/Vol. 28/No. 6 365
Improving Retention, Confidence, and Competence of New Graduate Nurses:
Results from a 10-Year Longitudinal Database
SERIES
expert RNs over and over as pre- experience, Beecroft, Santer, Lacy, ager, nurse managers, educators,
ceptors. Within the first year, it Kuntzman, and Dorey (2006) recruiters, and task force subcom-
became apparent the traditional found that when residents met mittee chairpersons oversees the
model was ineffective for resi- with their mentors regularly, guid- RN residency for each organiza-
dents and frustrating for precep- ance and support were provided tion. The RN residency 12-week
tors. Interviews with residents, and resident stress was reduced. start up begins with an all-day
preceptors, and managers, cou- However, the study also found kick-off event which includes a
pled with observations of the first topic areas which needed to be variety of stakeholders and pro-
RN residency cohorts, resulted in improved including commitment, vides an overview of various
a major overhaul of the precepting time, and role inadequacy. As a aspects of the RN residency (such
component of the RN residency result, the mentoring component as mentoring, debriefing, teach-
(Beecroft, Hernandez, & Reid, of the RN residency has been ing), and encourages opportuni-
2008). Team precepting was improved in recent years. ties for engagement and participa-
implemented and has become a Mentoring session topics and tion by many of the organization’s
practice standard of the RN resi- guidelines have been developed. employees (nurses, physicians,
dency. In team precepting, the A new mentoring model, mentor social workers, etc.). The start up
new graduate begins with a novice circles, has been provided as an period includes train-the-trainer
preceptor who has an experience option and has been successfully sessions for all roles, a step-by-
level closer to that of the new implemented by several organiza- step review of all curriculum com-
graduate. As the new graduate tions that provide the RN residen- ponents and competencies, and
gains expertise and knowledge, a cy. In mentor circles, two to three extensive work with the RN resi-
preceptor with more clinical expe- mentors assume responsibility for dency leadership group subcom-
rience takes over. Critical to this a group of residents. Residents mittees. Implementing a struc-
team precepting model is trans- also participate in scheduled, tured RN residency requires the
parency, accountability, and com- facilitated, structured debriefing/ organization to review the compe-
munication between preceptors self-care sessions which provide tencies and knowledge required of
that allows all involved to be up- opportunities for residents to safe- RNs and to review the related
to-date on residents’ strengths, ly voice and share their feelings processes and systems so they can
needs, and individual perform- about their experiences (death of a be effectively communicated to
ance goals. In the Versant RN patient, personal life balance, new graduate nurses. Quality
Residency, this occurs in Voyager, dealing with disruptive behavior). improvement occurs based on
the online RN residency informa- Implementing the Versant RN measurement data and evalua-
tion system. Residency. Implementing the RN tions from each cohort of resi-
As a part of the clinical residency requires the engage- dents and on trends identified
immersion component, each resi- ment and active participation of across multiple cohorts. New
dent rotates or “loops” to other people from throughout the hospi- instructional media and teaching
areas outside of the resident’s tal organization including nurses strategies are developed and in-
home unit during guided clinical in management, education, corporated.
experiences. These structured administrative and direct care Each client organization has a
looping experiences allow the res- roles; hospital administration; Versant Performance and Outcomes
idents to understand what their other health care professionals Manager assigned to it to provide
patients experience in other areas (physicians, pharmacists, social education, guidance, and support
of the hospital and offer them workers); human resource profes- (onsite and via telephone and
opportunities to meet and begin to sionals; etc. This engagement and email) on the implementation,
form relationships with staff in active participation is facilitated management, quality assurance,
these areas. and accomplished through an RN and performance and outcomes
Mentoring and debriefing. residency architecture that delin- measurement of the RN residency.
Providing support to new gradu- eates specific roles as well as Best practice information is dis-
ate nurses through structured structures and systems for the seminated at the annual Versant
mentoring is very important to implementation and ongoing Client Conference and through
their success. Structured mentor- management of the RN residency. webinars and individual organiza-
ing includes scheduled meetings, Each organization designates tion consultation with Versant
guidelines for conducting mentor- an RN residency manager, execu- staff.
ing sessions, and providing specif- tive sponsor, and administrative
ic content as well as discussions support. An RN residency leader- RN Residency Metrics
geared to individual needs. In ship group including the chief Outcomes of the RN residency
evaluating the mentor component nursing officer (CNO) and/or exec- are analyzed using a wide variety
of the RN residency after 6 years of utive sponsor, RN residency man- of metrics including, but not limit-
366 NURSING ECONOMIC$/November-December 2010/Vol. 28/No. 6
Improving Retention, Confidence, and Competence of New Graduate Nurses:
Results from a 10-Year Longitudinal Database
SERIES
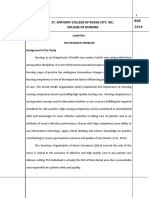
Figure 1.
RN Residency Metrics
Versant RN Residency Metrics
Measurement
Demographics Status Reports Evaluations Other
Instruments
• Competency Assessment Examples: Examples: Examples:
Client Demographics • Work Satisfaction • Competency • Class Evaluations • Focus Group
• Facility • Nurse Satisfaction Completion Reports • End of Residency Summaries
• Comparison Group • Conditions for Work • Class Completion Evaluations • Surveys
Effectiveness Reports • Preceptor Evaluations
• Corwin Nursing Role • Turnover Reports by Residents
Conception - Professional • CNO Reports • Looping Evaluations
RN Resident
Role Subscale • End of Residency • Mentor Evaluations
Demographics
• Group Cohesion Status Report & • Preceptor Evaluations
(i.e. Education, Age, • Leader Empowering
Gender, Referral Development Plan • Debriefer Evaluations
Behaviors Scale • Cross Cohort Reports • SME Evaluations
Source) • Organizational • System Comparison
Commitment Scale
Reports
• Schutzenhofer
Professional Nurse
RN Residency “Role Autonomy Scale
Specific” Demographics • Slater Nursing
(i.e., preceptors, Competencies - Self
mentors debriefers) Report and Observed
• Skills Competency Self
Confidence
• Turnover Intent
ed to, turnover monthly from allow the organization to compare ments have been validated and
months 12 to 60; organization cohorts of residents, and to many have been used in numer-
return on investment; demograph- improve the RN residency. The ous nursing research studies.
ic information; reliable and vali- information can also be used to Feedback on individual resident,
dated measurement instruments; compare RN residency outcomes unit, organization, and health sys-
individual, component, and RN from hospitals within a system. tem performance is provided in
residency evaluations; residency Concepts measured are selected real time via Versant’s web-based
status reports; focus groups; and based on evidence of relationships RN residency management system
surveys (see Figure 1). To measure with outcomes related to individ- (Versant Voyager) and through
new graduate progress within ual new graduates, organizations, periodic data reports that compare
each organization, data are also and patient care. The concepts results of each RN residency
collected from a comparison measured include, but are not lim- cohort to the organization’s com-
group comprising new graduates ited to: parison group, aggregate data, and
employed by the organization 2 • Competency the Versant National Database.
years prior to the implementation • Satisfaction
of the RN residency. Data are col- • Confidence RN Residency Outcomes
lected at specified time points • Empowerment/Autonomy/ Methodology. Analyses per-
throughout each RN residency Role dissonance formed for the Versant National
cohort and up to 60 months after • Group cohesion/Organizational Database included data reduction
the start of each cohort. All data commitment and multiple imputation, correla-
are housed in the Versant National • Turnover intent tion matrix analysis, generation
Database. Measures are selected based and inspection of descriptive sta-
Measurement instruments are on their ability to provide infor- tistics for demographic variables
used to obtain information con- mation related to RN residency as well as each scale and subscale
cerning RN resident progress, to outcomes. Measurement instru- and regression analysis. With two
NURSING ECONOMIC$/November-December 2010/Vol. 28/No. 6 367
Improving Retention, Confidence, and Competence of New Graduate Nurses:
Results from a 10-Year Longitudinal Database
SERIES
Table 1. intention as the outcome variable
Instrument Reliabilities and measurement instrument data
collected as predictor variables
Instrument Cronbach’s alpha with separate analyses performed
Conditions for Work Effectiveness 0.81 for each time period of data collec-
tion (start of program, last week of
Group Cohesion 0.89
program, month 12, month 24,
Leader Empowering Behavior (LEB) Total Scale 0.97 etc.). Logistic regression analysis
LEB Meaning subscale 0.96 was then performed with employ-
ment status (a binary, employed/
LEB Decision subscale 0.94 not employed, categorical vari-
LEB Confidence subscale 0.94 able) as the outcome variable and
Nurse Satisfaction (NS) Total Scale 0.90 the measurement instrument data
as predictor variables. Because of
NS Quality subscale 0.80 loss of cases due to “missingness”
NS Enjoyment subscale 0.87 on one or more of the subscales,
multiple imputation was per-
NS Time to Work subscale 0.78
formed on variables of interest
Organizational Commitment Total Scale 0.89 using SAS 9.2. This form of impu-
Organizational Job (Work) Satisfaction (OJS) Total Scale 0.87 tation provides robust imputed
values for missing data using
OJS Administration subscale 0.79
multi-chain regression-based im-
OJS Interaction subscale 0.81 putation of the data including
OJS Pay subscale 0.88 error term estimates. Identical
regression analyses were run
OJS Professional Status subscale 0.70 using this imputed data set with
OJS Task subscale 0.77 results presented separately from
the raw data set. Using SAS 9.2, a
correlation analysis was per-
Table 2. formed to obtain the five most sig-
Demographics nificant correlations between the
General range of input variables of interest
Comparison Versant – Children’s Acute Care and the outcome variable
Groups All Hospitals Hospitals Turnover Intent (TOI). Reliability
measures were calculated for this
Education
data sample and are shown in
Diploma 2% 1% 1% 1% Table 1.
Associate degree 49% 45% 39% 51% Results. At the 10-year mark,
over 6,000 new graduates com-
Baccalaureate degree 47% 51% 58% 45%
pleted the Versant RN Residency.
Master’s degree 2% 2% 2% 3% The organizations in which they
Age worked ranged from small, rural
hospitals to large health care sys-
Less than 23 years 6% 15% 20% 12% tems with cohort sizes from 4 to
23-30 years 57% 52% 58% 47% 110 residents. The descriptive sta-
23% 21% 16% 26% tistics are provided in Table 2.
31-40 years
Turnover. Turnover was meas-
41-50 years 11% 9% 5% 12% ured monthly from months 12 to
Over 50 years 3% 2% 1% 3% 60. The results are shown in Figure
2. The cumulative turnover rate
for the Versant RN Residency was
7.1% at 12 months, 19.6% at 24
outcome variables of interest, liminary exploratory regression months, 28.6% at 36 months,
employment status and turnover analysis produced a set of signifi- 34.2% at 48 months, and 39.8% at
intention, and a wide range of pos- cant predictor variables for use in 60 months. Of note, the turnover
sible predictor variables of inter- subsequent analyses. Ordinary rates decreased across the 10-year
est, three models of the data were Least Squares regression analysis period as the best practice of hav-
developed and analyzed. Pre- was performed with turnover ing new graduate nurses pass the
368 NURSING ECONOMIC$/November-December 2010/Vol. 28/No. 6
Improving Retention, Confidence, and Competence of New Graduate Nurses:
Results from a 10-Year Longitudinal Database
SERIES
Figure 2. NCLEX prior to starting the RN
Cumulative Turnover residency was identified and pro-
1999-2009 gressively implemented. The turn-
over rate was also found to
60%
decrease with the number of RN
residency cohorts completed with-
in an organization. By the fifth
50% cohort, the overall 12 month
turnover was 4.3%. The turnover
rate for bachelor’s degree graduates
40% was slightly lower than associate
degree graduates at 12 months
30% (6.6% vs. 7.4%), but slightly high-
er in all subsequent years.
A comparison of actual turn-
20% over after implementation of the
Versant RN Residency to the pre-
10% Versant turnover data was also
made, but with caution. Hospitals
who engage Versant are asked to
0 report their new graduate turnover
12 Months 24 Months 36 Months 48 Months 60 Months in the years immediately preced-
ing implementation of the Versant
All Hospitals with Versant RN Residency RN Residency. In the early years of
Children's Hospitals with Versant RN Residency the Versant RN Residency, hospi-
tals were inconsistent in their
General Acute Care Hospitals with Versant RN Residency
internal measurement of new
Pre-Versant New Graduate Turnover graduate turnover; therefore, given
the importance of establishing an
accurate baseline, Versant has im-
plemented standardized reporting
Figure 3. to Versant in recent years. For the
Competency purposes of this study, only the
data from hospitals that reported
Nursing Competencies Rating both 12 and 24 month pre-Versant
Percent of Maximum new graduate turnover were com-
pared to the actual turnover data.
100% The average pre-Versant new grad-
90% uate turnover for these hospitals at
80% 12 months was 27% (with some
70% organizations reporting a 12-
60% month turnover of up to 75%) and
another 30% in months 13 to 24,
50% resulting in an average cumulative
40% turnover of 49% at 24 months (see
30% Figure 2).
20% Competency. Individual com-
10% petencies were validated by pre-
ceptors for each resident. In addi-
0 tion, the Nursing Competencies
Comparison Week 2 End of RN Week 2 End of RN Rating Scale developed by Slater
Group Self Residency Observed Residency
Report Self Report Observed (Wandelt & Stewart, 1975) was
used for resident self-assessment
Children’s Hospitals General Acute Care Hospitals and trained observers performed
observations on a random sample
of nurses from each organization’s
comparison group and on a sam-
ple of residents from each cohort.
NURSING ECONOMIC$/November-December 2010/Vol. 28/No. 6 369
Improving Retention, Confidence, and Competence of New Graduate Nurses:
Results from a 10-Year Longitudinal Database
SERIES
Figure 4. The results from the observations
Nurse Satisfaction are shown in Figure 3. Because the
rating scale allows for the possibil-
ity of some items not being appli-
5.00
cable to or able to be observed in a
specific encounter, the scores are
4.50 reported as a percentage of the
maximum score attainable. In the
4.00 self-assessments, residents rated
themselves higher than the
3.50 observers rated them at both week
2 and at the end of the RN residen-
3.00 cy. Observers found significant
progress from the beginning to the
end of the RN residency. At the
2.50
end of the RN residency, the aver-
age observed rating was equal to
2.00 or higher than the observed rating
of the comparison groups, who
1.50 have an average experience of 17.1
months.
1.00 Satisfaction. Satisfaction was
Total Enjoyment Quality Time to Work measured using both work satis-
faction (also called organizational
End of RN Residency Month 12 Month 24 job satisfaction) and nurse job sat-
isfaction measures (Beecroft et al.,
2001). The Nurse Job Satisfaction
Scale includes elements that are
Figure 5. pertinent to nurses’ work and
Organizational Job Satisfaction includes the subscales of satisfac-
tion with enjoyment, quality, and
5.00 time to work. As shown in Figure
4, the enjoyment subscale is rated
4.50 highest followed by quality and
time to work, with satisfaction
with the latter two increasing in
4.00
stepwise fashion from the end of
the RN residency to months 12
3.50 and month 24.
The Work (Organizational Job)
3.00 Satisfaction Scale includes gener-
al items and includes subscales
2.50 for administration, interaction,
pay, professional, and task (see
Figure 5). Satisfaction with pay is
2.00 rated the lowest and declines pro-
gressively across time.
1.50 Self-confidence. The Skills
Competency Self-Confidence Survey
1.00 is a self-rating completed by the
RN residents at weeks 2, week 16,
the last week of the RN residency,
l
sk
ta
na
Pa
tio
io
To
Ta
ct
oi
and at months 12, 24, and 60. It
tra
ra
si
is
es
te
includes core skills that each resi-
in
In
of
m
Pr
dent is expected to possess at the
Ad
conclusion of the RN residency.
Results are reported as a percent-
End of RN Residency Month 12 Month 24 Month 60
age of maximum score. Because
370 NURSING ECONOMIC$/November-December 2010/Vol. 28/No. 6
Improving Retention, Confidence, and Competence of New Graduate Nurses:
Results from a 10-Year Longitudinal Database
SERIES
Figure 6. the scale includes a broad spec-
Self-Confidence trum of nursing skills, it is not
expected residents will be confi-
Skills Competency Self-Confidence dent in all skills. Results are inter-
Percent of Maximum Score preted in terms of improvement
over time. As can be seen in
100% Figure 6, self-confidence grew
90% across time.
80% Empowerment. Empowerment
is measured using the Leader
70% Empowering Behavior Scale and
60% three subscales of the Conditions
50% for Work Effectiveness measure.
40% The Leader Empowering Behaviors
Scale comprises subscales that
30%
include the degree to which the
20% leader is perceived by the resident
10% as enhancing the meaningfulness
0 of work, fostering participation in
decision making, and expressing
up
16
cy
16
24
60
confidence in high performance.
k
en
ro
ee
th
th
th
As shown in Figure 7, enhancing
ee
G
id
on
on
on
W
es
W
on
the meaningfulness of work was
R
ris
rated lowest at all time points and
pa
R
om
of
expressing confidence was rated
C
d
En
the highest. The resident ratings
Children’s Hospitals General Acute Care Hospitals were very similar to those of the
comparison group.
The Conditions for Work Ef-
fectiveness Questionnaire (CWEQ)
Figure 7. measures nurses’ perceptions of
Leader Empowering Behavior workplace effectiveness. The
questionnaire incorporates specif-
7.00 ic structural factors that influence
work behaviors. Three of the
6.00 CWEQ subscales were measured
and respondents are asked to indi-
5.00 cate what they have now (current-
ly have) and what they would like
4.00
(would like to have) in opportuni-
ty, access to information, and sup-
port. The results are shown in
3.00
Table 3.
Group cohesion and organiza-
2.00
tional commitment. The Group
Cohesion Scale evaluates percep-
1.00 tions of the nursing unit or depart-
Comparison End of RN Month 12 Month 24 ment in terms of productivity, effi-
Group Residency ciency, morale, “belongingness,”
and working together. The Group
Total Meaning Decision Confidence Cohesion Scale asks the respon-
dents’ opinions about the col-
league group (nursing staff) with
whom they work. Each item is
rated on a 1-7 scale. The mean
total Group Cohesion score was
5.77 at the end of the RN residen-
cy, 5.68 at 12 months, and 5.74 at
NURSING ECONOMIC$/November-December 2010/Vol. 28/No. 6 371
Improving Retention, Confidence, and Competence of New Graduate Nurses:
Results from a 10-Year Longitudinal Database
SERIES
Table 3.
Conditions for Work Effectiveness
Versant Comparison End of RN Laschinger (2004) Staff
Group Residency Month 12 Month 24 Nurses - Mean (Range)
Opportunity-Have 3.21 3.34 3.21 3.16 3.29 (2.35-4.14)
Opportunity-Would Like 3.67 3.55 3.62 3.63
Info Access-Have 2.76 2.84 2.87 2.88 2.81 (2.20-3.02)
Info Access-Would Like 3.91 3.93 3.88 3.85
Support-Have 3.06 3.00 3.02 3.05 2.85 (2.21-3.07)
Support-Would Like 3.86 3.89 3.85 3.81
Figure 8. of the RN residency, at month 12,
Turnover Intent and at month 24.
Correlations. As can be seen in
No the spider diagram in Figure 9, a
Do you plan to leave this facility number of significant correlations
within the next year? Maybe were found. Higher levels of satis-
Yes faction significantly correlate with
100% lower intent to leave the facility.
The Work Satisfaction Total Score
90%
and TOI have a 0.36 Pearson corre-
80% lation coefficient (p<0.0001), with
70% two of the subscales of Work
60% Satisfaction - Professional Status
50% (0.37, p<0.0001) and Work Satis-
40% faction - Satisfaction with Pay (0.18,
30% p<0.0001) also demonstrating sig-
nificant correlations. Similarly, the
20%
Nursing Satisfaction Total Score
10% (0.35, p<0.0001) and one of its sub-
0 scales, Enjoyment (0.39, p<0.0001)
Comparison End of RN Month 12 Month 24 Month 60 was also significantly correlated
Group Residency with TOI. Second order (indirect)
correlations of interest were also
identified between the difference
between present and observed sum-
24 months. The Comparison scale. The mean total Organi- mary scores for the Conditions of
Group mean was 5.55. zational Commitment score was Work Effectiveness (CWE) scale
The Organizational Commit- 4.59 at 16 weeks, 4.84 at the end of (have vs. would like to have -
ment Questionnaire is a scale that the RN residency, 4.74 at 12 “Have-Like”) and Work Satisfaction
measures the relative strength of an months, and 4.72 at 24 months. (0.31, p<0.0001) and Nurse
individual’s identification with The Comparison Group mean was Satisfaction (0.31, p< 0.0001)
and involvement in a particular 5.00. scales. The CWE Have-Like gap
organization. Commitment is char- Turnover intent. Turnover also was significantly correlated
acterized as (a) a strong belief in intent is measured by a single item with the Group Cohesion Total
and acceptance of the organiza- which asks “Do you plan to leave Score (0.37, p<0.0001). Larger gaps
tion’s goals and values, (b) a will- this facility in the next year?” and between the work conditions resi-
ingness to exert considerable effort offers a six-point continuum of dents would like to have and what
on behalf of the organization, and responses from “Not at all” to “I they perceive they have correlate
(c) a strong desire to maintain surely do.” Results are shown in with lower levels of satisfaction and
membership in the organization Figure 8. Turnover intent was a group cohesion. The Group
(Porter, Steers, Mowday, & Boulian, meaningful predictor of employ- Cohesion score, in turn, had a
1974). Each item is rated on a 1-7 ment status (p<0.0001) at the end strong correlation (0.53, p<0.0001)
372 NURSING ECONOMIC$/November-December 2010/Vol. 28/No. 6
Improving Retention, Confidence, and Competence of New Graduate Nurses: Results from a 10-Year
Longitudinal Database
SERIES
Figure 9.
Correlations with Turnover Intent and Turnover
Nurse Work
Organizational
Satisfaction Satisfaction
Commitment
Enjoyment Professional
.30* .59*
.07 †
Age .37*
Nurse .35 †
Satisfaction Turnover
Total Intent Turnover
Group .53* Work
Satisfaction
Cohesion
Total
.36*
P < 0.0001
.18*
.37*
.31*
.31*
CWE Work
Have - Satisfaction
Like Pay
Note: * = 0.0001; † = 0.002
with the Work Satisfaction Total laboration between new graduates assuring new graduate competen-
Score. Organizational Commitment and experienced nurses; patient cy to assure patient safety, validat-
was positively correlated with the and physician satisfaction; precep- ed competency decreases the
Nurse Satisfaction Enjoyment sub- tor role definition, engagement, and chance of preventable adverse
scale (0.30, p<0.0001), which in accountability; the quality and the events, thereby decreasing the
turn was positively correlated with number of applicants; and new hospital’s exposure to decreased
Work Satisfaction - Professional graduate engagement and advance- reimbursement and liability
Status (0.59, p<0.0001). Finally, the ment. claims. Accelerating the compe-
age group demographic variable tency and confidence develop-
was significantly correlated with Discussion ment further decreases this expo-
TOI, although with a small correla- The results of this 10-year lon- sure. Hospitals rely on nurses as a
tion coefficient (0.07, p=0.002). gitudinal study of new graduate critical component of error pre-
Organizational impact. In addi- nurses from Versant RN Residency vention. A study by Leape et al.
tion to the metric data collected, a in hospitals across the United (1995) found nurses intercepted
qualitative study on the organiza- States supports its advantages to 86% of all medication errors by
tional impact of the RN residency both the individual new graduates physicians, pharmacists, and oth-
was conducted in 2009. Re- and organizations which have ers who are part of the medication
spondents included CNOs, execu- been reported previously (Dyess & delivery system before the errors
tive sponsors, and RN residency Sherman, 2009; National Council reached the patients. The applica-
managers. The results indicated of State Boards of Nursing, 2009). tion of competence, however,
positive organizational outcomes of Competence development and requires self-confidence. Com-
the RN residency in the areas of self-confidence were accelerated. petence without self-confidence is
improved communication and col- In addition to the basic concept of insufficient. As Bandura (2001, p.
NURSING ECONOMIC$/November-December 2010/Vol. 28/No. 6 373
Improving Retention, Confidence, and Competence of New Graduate Nurses:
Results from a 10-Year Longitudinal Database
SERIES
10) noted in studies of efficacy, new graduate turnover prior to • Performance and outcomes
“Unless people believe they can implementing an RN residency. management.
produce desired results and fore- Equally and perhaps more • Research and development.
stall detrimental ones by their important than decreasing turn- • Continuous improvement.
actions, they have little incentive over costs is adding the value of • A delivery system with a disci-
to act or to persevere in the face of the organizational impact of the plined structural framework to
difficulties.” The acceleration of RN residency. Improvements in manage a fully integrated RN
confidence development in new communication, patient and phy- residency at individual hospital
graduates assures their accelerated sician satisfaction, employee en- and health care system levels.
competence acquisition is applied. gagement, such as those reported Our results support the need
The correlations between to result from the RN residency, for the 18-week clinical immer-
turnover intent and organizational positively impact nurse satisfac- sion component with dedicated
commitment, work satisfaction, tion, patient outcomes, and organ- preceptors. In addition, our expe-
nursing satisfaction, group cohe- ization success (Gallup, 2006; rience and extensive followup of
sion, and conditions for work Kalisch, Curley, & Stefanov, 2007; our RN residents has shown us
effectiveness support the results of Maxfield, Grenny, McMillan, their need for ongoing support
other research (Larrabee et al., Patterson, & Switzler, 2005). and guidance through their first
2003; Nogueras, 2006; Stone et al., year of practice. As a result, we
2006; Tourangeau & Cranley, Lessons Learned will soon begin incorporating
2006). Employee satisfaction has Based on 10 years experience additional structured supportive
also been previously correlated to and evidence for the Versant RN components (mentoring and
customer satisfaction and loyalty, Residency, we found that in order debriefing) throughout the resi-
profitability, productivity, and to achieve successful outcomes on dents’ first year of practice and
safety outcomes (Harter, Schmidt, an individual and organizational developing additional evaluation
& Hayes, 2002). The relationship level, an RN residency must: and coaching activities designed
found in our study between • Define a set of standards based to further focus everyone involved
turnover intent and actual turn- upon an outcomes-validated with residents on their long-term
over is similar to that found by set of competencies. success.
Griffeth, Hom, and Gaertner (2000) • Teach to those standards.
and Harris and Boonthanom (2005). • Monitor and manage adher- Conclusion
Decreasing actual new gradu- ence to those standards. Versant’s mission is to help
ate turnover provided substantial • Objectively evaluate – by use hospitals and health systems
savings to the Versant RN of quantitative and qualitative develop and sustain nursing
Residency hospitals. In one exam- outcomes measures – success organizations. The Versant RN
ple, a general acute care hospital in achieving the demonstrated Residency contributes to this mis-
had a 35% new graduate turnover competencies expected of a sion through facilitating the tran-
rate at 12 months prior to imple- competent nurse. sition of new graduate nurses into
menting the RN residency. The 12- We also identified the key the professional RN role, acceler-
month turnover rate in the first 3 characteristics of a successful RN ating the development of their
years of the RN residency at that residency. competence and confidence, and
hospital was 5.36% (6 of 112 resi- • Structure and standardization. increasing their retention within
dents). Had the previous 35% 12- • An evidence base for content the organization.
month turnover continued, the and RN residency practices. The results of this longitudi-
hospital could have expected to • Educational content manage- nal 10-year study present persua-
lose 39 new graduates – a net loss ment. sive evidence that both new grad-
of 33. Using Jones’ (2008) calcula- • Clinical immersion experience uate nurses and their organiza-
tion of the replacement cost of with dedicated preceptors. tions benefit from the implemen-
each new nurse to be between • Support systems for RN resi- tation of a structured, immersion
$82,000 to $88,000, the cost to the dency roles (preceptors, sub- RN residency that includes class-
hospital for replacing the 36 new ject matter experts) and for res- room instruction, guided opportu-
graduates would have been estimat- idents. nities to develop hands-on mas-
ed to be $2,706,000 to $2,904,000. • Transparency and accountabil- tery of nursing skills, support, pro-
Because the range of new graduate ity. fessional guidance, and engage-
turnover varies from hospital to • Communication. ment of stakeholders. Formal RN
hospital, to effectively measure • Active stakeholder engage- residencies with measured out-
the return on investment related ment and organization-wide comes should become the norm
to turnover, hospitals must have commitment. for all new graduate nurses. $
accurate information on their own • Rigorous evaluations.
374 NURSING ECONOMIC$/November-December 2010/Vol. 28/No. 6
Improving Retention, Confidence, and Competence of New Graduate Nurses:
Results from a 10-Year Longitudinal Database
SERIES
REFERENCES Gallup. (2006). Gallup study: Engaged Maxfield, D., Grenny, J., McMillan, R.,
Bandura, A. (2001). Social cognitive theo- employees inspire company innova- Patterson, K., & Switzler, A. (2005).
ry: An agentic perspective. Annual tion. New York: Author. Retrieved Silence kills: The seven crucial con-
Review of Psychology, 52, 1-26. from http://gmj.gallup.com/content/ versations in healthcare. Provo, UT:
Beecroft, P.C., Kunzman, L., & Krozek, C. 24880/Gallup-Study-Engaged- VitalSmarts. Retrieved from http://
(2001). RN internship: Outcomes of a Employees-Inspire-Company- www.aacn.org/WD/Practice/Docs/
one-year pilot program. Journal of Innovation.aspx PublicPolicy/SilenceKills.pdf
Nursing Administration, 31(12), 575- Griffeth, R.W., Hom, P.W., & Gaertner, S. National Council of State Boards of
582. (2000). A meta-analysis of ante- Nursing. (2009). Transition evidence
Beecroft, P.C., Kunzman, L., Taylor, S., cedents and correlates of employee grid - March 2009. Chicago, IL:
Devenis, E., & Guzek, F. (2004). turnover: Update, moderator tests, Author. Retrieved from www.ncsbn.
Bridging the gap between school and and research implications for the org/Evidence_Grid_2009.pdf
workplace: Developing a new gradu- next millennium. Journal of Manage- Nogueras, D. J. (2006). Occupational com-
ate nurse curriculum. Journal of ment, 26, 463-488. mitment, education, and experience
Nursing Administration, 34(7/8), Harris, K.J., & Boonthanom, R. (2005). as a predictor of intent to leave
338-345. Perceptions of organizational politics the nursing profession. Nursing
Beecroft, P.C., Santner, S., Lacy, M.L., and cooperation as moderators of the Economic$, 24(2), 86-93.
Kunzman, L., & Dorey, F. (2006). New relationship between job strains and Norton R. (1997). DACUM handbook (2nd
graduate nurses’ perceptions of men- intent to turnover. Journal of Manage- ed.). Columbus, OH: The Ohio State
toring: Six-year programme evalua- ment Issues, 17, 26-42. University.
tion. Journal of Advanced Nursing, Harter, J.K., Schmidt, F.L., & Hayes, T.L. Pellico, L.H., Brewer, C.S., & Kovner, C.T.
55(6), 736-747. doi: 10.1111/j.1365- (2002). Business-unit-level relation- (2009). What newly licensed regis-
2648.2006.03964. ship between employee satisfaction, tered nurses have to say about their
Beecroft, P.C., Hernandez, A.M., & Reid, employee engagement, and business first year experience. Nursing
D. (2008). Team preceptorships: A outcomes: A meta-analysis. Journal Outlook, 57(4), 194-203.
new approach for precepting new of Applied Psychology, 87(2), 268- Porter, L.W., Steers, R.M., Mowday, R.T., &
nurses. Journal for Nurses in Staff 279. Boulian, P.V. (1974). Organizational
Development, 24(4), 143-148. Institute of Medicine (IOM). Committee commitment, job satisfaction, and
Benner, P. (1984). From novice to expert: on the Robert Wood Johnson turnover among psychiatric techni-
Excellence and power in clinical nurs- Foundation Initiative on the Future cians. Journal of Applied Psychology,
ing practice. Menlo Park, CA: of Nursing. (2010). The future of 59(5), 603-609.
Addison-Wesley Publishing Company. nursing: Leading change, advocating Price Waterhouse Coopers. (2007). What
Benner, P., Sutphen, M., Leonard, V., & health. Washington, DC: National works: Healing the healthcare
Day, L. (2010). Educating nurses: A Academies Press. Retrieved from staffing shortage. Retrieved from
call for radical transformation. San http://www.nap.edu/catalog.php?rec http://www.pwc.com/us/en/health
Francisco: Jossey-Bass. ord_id=12956 care/publications/what-works-heal
Berkow, S., Virkstis, K., Stewart, J., & Jones, C.B. (2008). Revisiting nurse ing-the-healthcare-staffing-short
Conway, L. (2008). Assessing new turnover costs: Adjusting for infla- age.html
graduate nurse performance. Journal tion. Journal of Nursing Administration, Smith, E.L., Cronenwett, L., & Sherwood,
of Nursing Administration, 38(11), 38(1), 11-18. G. (2007). Current assessments of
468-474. Kalisch, B.J., Curley, M., & Stefanov, S. quality and safety education in nurs-
Buerhaus, P. I. (2009). The shape of the (2007). An intervention to enhance ing. Nursing Outlook, 55(3), 132-137,
recovery: Economic implications for nursing staff teamwork and engage- Stone, P.W., Larson, E.L., Mooney-Kane,
the nursing workforce. Nursing ment. Journal of Nursing Administra- C., Smolowitz, J., Lin, S.X., & Dick,
Economic$, 27(5), 338-340, 336. tion, 37(2), 77-84. A.W. (2006). Organizational climate
Buerhaus, P., Auerbach, D., & Staiger, D. Kovner, C.T., Brewer, C.S., Fairchild, S., and intensive care unit nurses’ inten-
(2009). The recent surge in nurse Poornima, S., Kim, H., & Djukic, M. tion to leave. Critical Care Medicine,
employment: Causes and implica- (2007). Newly licensed RNs’ charac- 34(7), 1907-1912.
tions. Health Affairs (web exclusive), teristics, work attitudes, and inten- Tourangeau, A.E., & Cranley, L.A. (2006).
w657-668. Retrieved from www. tions to work. American Journal of Nurse intention to remain employed:
healthstaff.org/documents/surgein Nursing, 107(9), 58-70. Understanding and strengthening
nurseemployment.pdf Larrabee, J.H., Janney, M.A., Ostrow, C.L., determinants. Journal of Advanced
del Bueno, D.J. (2005). Why can’t new reg- Withrow, M.L., Hobbs Jr., G R., & Nursing, 55(4), 497-509.
istered nurse graduates think like Burant, C. (2003). Predicting regis- Wandelt, M.A., & Stewart, D.S. (1975).
nurses? Nursing Education Perspec- tered nurse job satisfaction and Slater nursing competencies rating
tives, 26(5), 278-282. intent to leave. Journal of Nursing scale. New York: Appleton-Century-
Duffield, C., Roche, M., O’Brien-Pallas, L., Administration, 33(5), 271-283. Crofts.
& Catling-Paull, C. (2009). The impli- Laschinger, H.K.S. (2004). Range of man-
cation of staff ‘churn’ for nurse man- agers’ and staff nurses’ empower- ADDITIONAL READINGS
agers, staff, and patients. Nursing ment scores. Retrieved from http:// Beecroft, P.C., Dorey, F., & Wenten, M.
Economic$, 27(2), 103-110. publish.uwo.ca/~hkl/descriptives.pdf (2007). Turnover intention in new
Dyess, S.M., & Sherman, R.O. (2009). The Leape, L.L., Bates, D.W., Cullen, D.J., graduate nurses: A multivariate
first year of practice: New graduate Cooper, J., Demonaco, H.J., Gallivan, analysis. Journal of Advanced
nurses’ transition and learning needs. T., … for the ADE Prevention Study Nursing, 62(1), 41-52.
The Journal of Continuing Education Group. (1995). Systems analysis of Cronenwett, L., Sherwood, G., Bernsteiner,
in Nursing, 40(9), 403-410. doi:10. adverse drug events. JAMA, 274(1), J., Disch, J., Johnson, J., Mitchell, P.,
3928/00220124-20090824 -03 35-43. … Warren, J. (2007). Quality and safe-
ty education for nurses. Nursing
Outlook, 55, 122-131.
Reprinted from Nursing Economic$, 2010, Volume 28, Number 6, pp. 363-375. Reprinted with permission of the publisher, Jannetti
Publications, Inc., East Holly Avenue, Box 56, Pitman, NJ 08071-0056; (856) 256-2300; FAX (856) 589-7463; Web site:
www.nursingeconomics.net ; For a sample copy of the journal, please contact the publisher.
375
You might also like
- Top 10 Pastoral Interview Questions and AnswersDocument16 pagesTop 10 Pastoral Interview Questions and Answersmaretjonh100% (3)
- 2019 Stryker Culture Book InteractiveDocument79 pages2019 Stryker Culture Book InteractivescubadruNo ratings yet
- Employee Selection - Structure ExerciseDocument11 pagesEmployee Selection - Structure Exerciseshah100% (1)
- Diagnosing Organizational EffectivenessDocument60 pagesDiagnosing Organizational EffectivenessYodhia AntariksaNo ratings yet
- Opening The Doors To The orDocument9 pagesOpening The Doors To The orWanda Juszczuk100% (1)
- DND EconomyDocument3 pagesDND EconomyNHY100% (2)
- Cross Selling and Upselling Strategies of Axis BankDocument70 pagesCross Selling and Upselling Strategies of Axis Banksimranarora200750% (2)
- Lecture Notes - Gens 202 - SUMMARYDocument45 pagesLecture Notes - Gens 202 - SUMMARYebuka75% (4)
- PROF JONA Casey Fink Nurse Retention ArticleDocument9 pagesPROF JONA Casey Fink Nurse Retention ArticleMaryam Teodosio Al JedawyNo ratings yet
- Van Patten 2019Document6 pagesVan Patten 2019Amrinder RandhawaNo ratings yet
- Research Paper PDFDocument11 pagesResearch Paper PDFevaNo ratings yet
- IRamirezNU310M2Credibility of SourcesDocument6 pagesIRamirezNU310M2Credibility of SourcesIvan RamirezNo ratings yet
- 4 AeeDocument6 pages4 AeeAlberto Jr. AndresNo ratings yet
- Running Head: Advanced Clinical Nurse Specialist and Nurse Practitioner RolesDocument19 pagesRunning Head: Advanced Clinical Nurse Specialist and Nurse Practitioner RolesMd. Shahfayet JinnahNo ratings yet
- BrownDocument13 pagesBrownapi-255084253No ratings yet
- Finding Your PlaceDocument11 pagesFinding Your PlacetiniliciousNo ratings yet
- Nursing Quality Indicator Outcomes in Hospitals With A Clinical Nurse Leader: A Scoping Review ProtocolDocument7 pagesNursing Quality Indicator Outcomes in Hospitals With A Clinical Nurse Leader: A Scoping Review ProtocolNYONGKERNo ratings yet
- Nursing Shortages in The OR: Solutions For New Models of EducationDocument23 pagesNursing Shortages in The OR: Solutions For New Models of EducationCham SaponNo ratings yet
- Nursing 1Document5 pagesNursing 1Ray NamuNo ratings yet
- Reed - Reflection Paper Nurs631Document10 pagesReed - Reflection Paper Nurs631api-215994182No ratings yet
- Sample Article 1Document10 pagesSample Article 1Manoj Asanka ManamperiNo ratings yet
- Optimal Nurse Staffing To Improve Quality of Care and Patient OutcomesDocument50 pagesOptimal Nurse Staffing To Improve Quality of Care and Patient OutcomesBen תפילה100% (1)
- Garduate Nurse Perceptions of The Work ExperienceDocument7 pagesGarduate Nurse Perceptions of The Work Experienceshabatat2002No ratings yet
- Novice Nurse Support Group: A Pilot StudyDocument21 pagesNovice Nurse Support Group: A Pilot Studyastor toNo ratings yet
- Nurse Job Satisfaction To Implementation of A Nursing Professional Practice ModelDocument11 pagesNurse Job Satisfaction To Implementation of A Nursing Professional Practice ModelAmeng GosimNo ratings yet
- Motivation For Entry, Occupational Commitment and Intent To Remain: A Survey Regarding Registered Nurse RetentionDocument11 pagesMotivation For Entry, Occupational Commitment and Intent To Remain: A Survey Regarding Registered Nurse RetentionMuhammad Fahrin AzhariNo ratings yet
- Issues in Nursing OrganizationsDocument6 pagesIssues in Nursing Organizationssebast107No ratings yet
- Attending Registered Nurses Evolving Role Perceptions in Clinical Care TeamsDocument8 pagesAttending Registered Nurses Evolving Role Perceptions in Clinical Care TeamsjokoNo ratings yet
- Nursing LeadershipDocument10 pagesNursing LeadershipEloise PateñoNo ratings yet
- Entrevista Linda Aiken Parte 1Document7 pagesEntrevista Linda Aiken Parte 1pirritoleoncitoNo ratings yet
- 4 Understanding The Factors Which Promote Registered Nurses Intent To Stay in Emergency and Critical Care AreasDocument7 pages4 Understanding The Factors Which Promote Registered Nurses Intent To Stay in Emergency and Critical Care Areasroselle portudoNo ratings yet
- New Graduate Nurse Preceptor Program: A Collaborative Approach With AcademiaDocument9 pagesNew Graduate Nurse Preceptor Program: A Collaborative Approach With AcademiaSunil MachambiNo ratings yet
- Health Policy Memo MgenoviaDocument5 pagesHealth Policy Memo Mgenoviaapi-302138606No ratings yet
- A Journey To Leadership: Designing A Nursing Leadership Development ProgramDocument7 pagesA Journey To Leadership: Designing A Nursing Leadership Development ProgramediNo ratings yet
- The Evolving Role of Midwives As Laborists: Original ReviewDocument8 pagesThe Evolving Role of Midwives As Laborists: Original Reviewmnazri98No ratings yet
- AB Nursing Patient Care 11 09Document51 pagesAB Nursing Patient Care 11 09dediNo ratings yet
- Anno Bib Research QuestionDocument3 pagesAnno Bib Research QuestionShawn HartleyNo ratings yet
- The Graduate Nurse ExperienceDocument9 pagesThe Graduate Nurse ExperienceNurmala DewiNo ratings yet
- ValdesDocument6 pagesValdesPrameswari ZahidaNo ratings yet
- Contemporary Nursing PresentationDocument39 pagesContemporary Nursing Presentationapi-443501911No ratings yet
- Nurse Residency Program 1Document5 pagesNurse Residency Program 1api-315956703No ratings yet
- Orientation GuidelinesDocument24 pagesOrientation GuidelinesjitnunNo ratings yet
- NURS402 ResearchPaperDocument11 pagesNURS402 ResearchPaperldhendersonNo ratings yet
- An Evidence-Based ProtocolDocument8 pagesAn Evidence-Based ProtocolKMNo ratings yet
- Admsci 07 00017Document13 pagesAdmsci 07 00017SriMathi Kasi Malini ArmugamNo ratings yet
- Building A Nursing Workforce For The 21St Century: Brenda L. Cleary, PHD, RN, FaanDocument5 pagesBuilding A Nursing Workforce For The 21St Century: Brenda L. Cleary, PHD, RN, FaanRoshan KumarNo ratings yet
- Optimal Allocation of Nursing ResourcesDocument2 pagesOptimal Allocation of Nursing ResourcesReinhold AcacioNo ratings yet
- Will Is 2017Document7 pagesWill Is 2017enfaraujoNo ratings yet
- Running Head: Quality Improvement Project: Nurse To Patient Rati 1Document5 pagesRunning Head: Quality Improvement Project: Nurse To Patient Rati 1api-300602911No ratings yet
- 2PROFE1Document132 pages2PROFE1Selena MarieNo ratings yet
- Zolnierek 2010 Negsafety-1Document10 pagesZolnierek 2010 Negsafety-1robbyNo ratings yet
- 1 s2.0 S155730871200087X MainDocument4 pages1 s2.0 S155730871200087X MainCicilia Ika WNo ratings yet
- Perceptions of Organizational Support and Its Impact On Nurses' Job OutcomesDocument8 pagesPerceptions of Organizational Support and Its Impact On Nurses' Job OutcomesAliza arifNo ratings yet
- TransitionDocument13 pagesTransitionDonna NituraNo ratings yet
- Nurse Practitioner Job Satisfaction: Looking For Successful OutcomesDocument12 pagesNurse Practitioner Job Satisfaction: Looking For Successful OutcomesCorporacion H21No ratings yet
- Extending The Nursing Role in Emergency Departments: Challenges For AustraliaDocument10 pagesExtending The Nursing Role in Emergency Departments: Challenges For AustraliaAnonymous nEQNlgbYQCNo ratings yet
- RC Competency-By-Design Ebook eDocument141 pagesRC Competency-By-Design Ebook ebill jonsNo ratings yet
- 1 PBDocument10 pages1 PBDwi NopriyantoNo ratings yet
- Annotated Bibliography Paper #1 RevisedDocument11 pagesAnnotated Bibliography Paper #1 Revisedpotas abuyaNo ratings yet
- Turnover Among Foreign Nurses in Saudi ArabiaDocument9 pagesTurnover Among Foreign Nurses in Saudi ArabiaNabila SalsabilaNo ratings yet
- High Patient Nurse RatiosDocument2 pagesHigh Patient Nurse Ratiosrachel lorenNo ratings yet
- Wage, Work Environment, and Staffing: Effects On Nurse OutcomesDocument9 pagesWage, Work Environment, and Staffing: Effects On Nurse OutcomesDwi NopriyantoNo ratings yet
- Literature Review - Midwifery EducationDocument8 pagesLiterature Review - Midwifery Educationafdtszfwb100% (1)
- Structured Mentoring StrategiesDocument31 pagesStructured Mentoring Strategiesrandy gallegoNo ratings yet
- Nurses Contributions to Quality Health OutcomesFrom EverandNurses Contributions to Quality Health OutcomesMarianne BaernholdtNo ratings yet
- Nursing Leadership: Scope and Standards of Practice, 3rd editionFrom EverandNursing Leadership: Scope and Standards of Practice, 3rd editionNo ratings yet
- Guide to Medical Education in the Teaching Hospital - 5th EditionFrom EverandGuide to Medical Education in the Teaching Hospital - 5th EditionNo ratings yet
- Developmental Psychology Chapter 1Document7 pagesDevelopmental Psychology Chapter 1Precious UncianoNo ratings yet
- 2804 ArticleText 4316 1 10 20220808Document9 pages2804 ArticleText 4316 1 10 20220808Precious UncianoNo ratings yet
- ACTIVITY INTOLERANCE PostDocument2 pagesACTIVITY INTOLERANCE PostPrecious UncianoNo ratings yet
- Anatomy and PhysiologyDocument2 pagesAnatomy and PhysiologyPrecious UncianoNo ratings yet
- Business Env. in NepalDocument12 pagesBusiness Env. in NepalbgbhattacharyaNo ratings yet
- Part 3C Control and Performance Evaluation 291 QuestionsDocument83 pagesPart 3C Control and Performance Evaluation 291 Questionspanchitoperez2014No ratings yet
- Caregivers For Geriatrics PDFDocument17 pagesCaregivers For Geriatrics PDFMihir AnandNo ratings yet
- Measuring HR Systems - KPMGDocument16 pagesMeasuring HR Systems - KPMGSmetanin2012No ratings yet
- Qip Group 3 - Education and TrainingDocument19 pagesQip Group 3 - Education and Trainingapi-356303021No ratings yet
- Globalization S4Document10 pagesGlobalization S4Emilien MercenierNo ratings yet
- Krystel Smalls Senior Recruiter AIRSDocument2 pagesKrystel Smalls Senior Recruiter AIRSkrystelsmallsNo ratings yet
- Individual Assignment Public Finance and TaxationDocument3 pagesIndividual Assignment Public Finance and TaxationSahal Cabdi AxmedNo ratings yet
- Internship Manual KUSTDocument27 pagesInternship Manual KUSTSaif Bettani KustNo ratings yet
- Statistics of Filipino Children 4th Quarter of 2008 Juvenile DelinquencyDocument119 pagesStatistics of Filipino Children 4th Quarter of 2008 Juvenile DelinquencyalexiaNo ratings yet
- Building ResumeDocument6 pagesBuilding ResumeFallen GodNo ratings yet
- Pre-Arrival Programs For EmploymentDocument4 pagesPre-Arrival Programs For EmploymentSaleem AbdulNo ratings yet
- Project EntrepreNurse BrochureDocument2 pagesProject EntrepreNurse BrochurePhilippineNursingDirectory.comNo ratings yet
- Question 13 Draft FormalDocument4 pagesQuestion 13 Draft FormalFlora InnehNo ratings yet
- HRM531 FinalDocument24 pagesHRM531 FinalroposandyNo ratings yet
- Evaluating The Deming Management Model of Total Quality in ServicesDocument31 pagesEvaluating The Deming Management Model of Total Quality in ServicesKenneth R. HearneNo ratings yet
- Psychological Capital (Psycap) in Nigeria Adaptation of Luthan's Postive Psychological Capital Questionnaire (Pcq-24) For Nigerian SamplesDocument10 pagesPsychological Capital (Psycap) in Nigeria Adaptation of Luthan's Postive Psychological Capital Questionnaire (Pcq-24) For Nigerian SamplesInternational Journal of Advance Study and Research WorkNo ratings yet
- Presentation On:-: Export Sales Organization & Export Sales Man (Recruiting & Training)Document26 pagesPresentation On:-: Export Sales Organization & Export Sales Man (Recruiting & Training)Vivek Kumar SharmaNo ratings yet
- Inspiring WomenDocument12 pagesInspiring WomenRina FitrianiNo ratings yet
- DRE ChecklistDocument1 pageDRE Checklistutreasure23No ratings yet
- Collective BargainingDocument17 pagesCollective Bargainingsubashik100% (1)
- Laws To BDDocument120 pagesLaws To BDSujan SarkerNo ratings yet
- Agriculture Sector in India PDFDocument2 pagesAgriculture Sector in India PDFAnonymous D82fJtjKNo ratings yet