Professional Documents
Culture Documents
Journal - The Physiology of Intrapartum Fetal Compromise at Term
Uploaded by
bedahfkumiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Journal - The Physiology of Intrapartum Fetal Compromise at Term
Uploaded by
bedahfkumiCopyright:
Available Formats
ajog.
org Expert Reviews
The physiology of intrapartum fetal compromise
at term
Jessica M. Turner, MBChB MRCOG; Murray D. Mitchell, FRCOG DPhil(Oxon);
Sailesh S. Kumar, FRCOG FRANZCOG DPhil(Oxon) CMFM
I n the majority of women, placental
function is sufficient to allow
appropriate growth of the fetus
Uterine contractions in labor result in a 60% reduction in uteroplacental perfusion,
causing transient fetal and placental hypoxia. A healthy term fetus with a normally
throughout pregnancy and to help shield developed placenta is able to accommodate this transient hypoxia by activation of the
it from the hypoxic stresses of labor. In peripheral chemoreflex, resulting in a reduction in oxygen consumption and a central-
some women, depending on the degree ization of oxygenated blood to critical organs, namely the heart, brain, and adrenals.
of placental dysfunction, fetal growth Providing there is adequate time for placental and fetal reperfusion between contrac-
restriction may ensue or intrapartum tions, these fetuses will be able to withstand prolonged periods of intermittent hypoxia
fetal compromise may develop if the and avoid severe hypoxic injury. However, there exists a cohort of fetuses in whom
placenta is not able to meet the extra fetal abnormal placental development in the first half of pregnancy results in failure of
demands required during the last few endovascular invasion of the spiral arteries by the cytotrophoblastic cells and inadequate
weeks of pregnancy or during labor and placental angiogenesis. This produces a high-resistance, low-flow circulation predis-
thereby predispose these infants to hyp- posing to hypoperfusion, hypoxia, reperfusion injury, and oxidative stress within the
oxic insults. If severe enough, these can placenta. Furthermore, this renders the placenta susceptible to fluctuations and
result in emergency operative birth, reduction in uteroplacental perfusion in response to external compression and stimuli (as
death, short-term morbidity, and sig- occurs in labor), further reducing fetal capillary perfusion, placing the fetus at risk of
nificant long-term neurodevelopmental inadequate gas/nutrient exchange. This placental dysfunction predisposes the fetus to
issues. intrapartum fetal compromise. In the absence of a rare catastrophic event, intrapartum
Globally, perinatal hypoxia remains a fetal compromise occurs as a gradual process when there is an inability of the fetal heart
major contributor to stillbirth, hypoxic to respond to the peripheral chemoreflex to maintain cardiac output. This may arise as a
ischemic encephalopathy (HIE), and consequence of placental dysfunction reducing pre-labor myocardial glycogen stores
cerebral palsy; 10% of the global burden necessary for anaerobic metabolism or due to an inadequate placental perfusion be-
of disease is attributable to newborn tween contractions to restore fetal oxygen and nutrient exchange. If the hypoxic insult is
conditions. It is estimated that world- severe enough and long enough, profound multiorgan injury and even death may occur.
wide, 23% of the 4 million neonatal This review provides a detailed synopsis of the events that can result in placental
deaths per year occur because of intra- dysfunction, how this may predispose to intrapartum fetal hypoxia, and what protective
partum complications.1,2 Of newborns mechanisms are in place to avoid hypoxic injury.
who develop HIE, almost 1 million die in
the first month of life and 25% of sur- Key words: fetal hypoxia, hypoxic ischemic encephalopathy, inadequate placentation,
vivors have long-term sequelae such as intrapartum fetal compromise, peripheral chemoreflex, physiology, placental
development
From the Mater Research Institute (Drs Turner
and Kumar) and Faculty of Medicine (Drs Turner cerebral palsy with intrapartum hypoxia, uterine contractions.5 Uterine contrac-
and Kumar), University of Queensland; and
accounting for 1 in 5 cases in term tions reduce uteroplacental perfusion by
Institute of Health and Biomedical Innovation -
Centre for Children’s Health Research, Faculty infants.3 Indeed, the World Health Or- as much as 60%6 and although most
of Health, Queensland University of Technology ganization estimates that disability- fetuses are able to tolerate this reduction
(Dr Mitchell), Brisbane, Queensland, Australia. adjusted life years due to neonatal in placental perfusion, there exists a
Received Feb. 22, 2019; revised June 26, 2019; encephalopathy, birth asphyxia, and cohort that are unable to and are at risk
accepted July 18, 2019. birth trauma are comparable with of hypoxic injury. Fetuses that are unable
J.T. and S.K. acknowledge research support by congenital malformations, type II dia- to withstand these periods of intermit-
the Mater Foundation. betes, and HIV/AIDS (54,400 million).4 tent hypoxia manifest their compromise
Corresponding author: Sailesh Kumar, FRCOG Although rare, unpredictable and in a variety of ways, including heart rate
FRANZCOG DPhil(Oxon) CMFM. sailesh. acute catastrophic events such as abnormalities (decelerations, decrease in
kumar@mater.uq.edu.au
placental abruption, uterine rupture, or beat-to-beat variability etc) and passage
0002-9378/$36.00
ª 2019 Elsevier Inc. All rights reserved.
cord prolapse are associated with a high of meconium in utero. In extreme cases,
https://doi.org/10.1016/j.ajog.2019.07.032 risk of severe fetal hypoxia; 75% of cases if the hypoxic insult is severe enough,
in labor occur gradually as a result of brain injury or death can ensue. This
JANUARY 2020 American Journal of Obstetrics & Gynecology 17
Downloaded for FK UMI Makassar (dosenfkumi01@gmail.com) at University of Muslim Indonesia from ClinicalKey.com by Elsevier on April 14, 2020.
For personal use only. No other uses without permission. Copyright ©2020. Elsevier Inc. All rights reserved.
Expert Reviews ajog.org
review will cover the physiology of the placenta. This occurs through the placental perfusion51 and oxygenation.52
placental development, fetal response to processes of vasculogenesis (differentia- Because of a reduction in uteroplacental
intrapartum hypoxia at term, and some tion of mesenchymal-derived heman- perfusion, intermittent placental hyp-
recent advances in the screening and gioblasts into endothelial cells)27 and oxia, reperfusion injury, and oxidative
identification of vulnerable fetuses. angiogenesis (remodeling and expansion stress occurs, with accelerated tropho-
of existing vessels either by branching or blast apoptosis and enhanced endo-
Placental Development non-branching processes), which are plasmic reticulum stress.53,54 In vitro
Development of the placenta involves 2 modulated by vascular endothelial and in vivo studies have demonstrated
complex but concurrent processes: growth factor in first half of preg- that repeated ischemiaereperfusion
endothelial invasion of the maternal spi- nancy28,29 and placental growth factor events, as seen in labor, result in a sub-
ral arteries by cytotrophoblast (CT) cells (PlGF) after 23 weeks gestation.30,31 stantial decline in placental mRNA
and development of the fetal vascular Failure of endovascular invasion of and PlGF levels, which in turn further
tree. Endothelial invasion initially results the spiral arteries produces a high- activates inflammatory cytokine
in the formation of a trophoblast “plug,” resistance, low-flow circulation that pathways.55e57 Placentae that are at
which results in a relatively hypoxic predisposes to hypoperfusion, hypoxia, greatest risk of ischemiaereperfusion
milieu (oxygen partial pressure [PaO2] reperfusion injury, and oxidative stress injury are those with aberrant conver-
<20 mm Hg) within the intervillous in the placenta.32 This affects placental sion of spiral arteries, resulting in nar-
space.7,8 This hypoxic environment is function through several mechanisms— rower vessels with luminal atherosclerotic
crucial for early regulation of CT prolif- the persistent high-pressure flow deposits and retention of vascular inner-
eration and differentiation.9 The CT plug through the intervillous space (2-3 m/s vation and vasoreactivity.36,58,59
dissipates after 10 weeks of gestation, compared with 10 cm/s in normally
resulting in increased placental blood dilated vessels) results in increased sheer Impact of Labor on the Fetus
flow and PaO2.10 Endovascular invasion stress and damage to the syncytio- Although uterine contractions result in
by the CTs into the wall of the spiral ar- trophoblasts lining the chorionic villi, a decline in fetal PaO2 by approximately
teries involves de-differentiation of thereby compromising the functional 25%,60 the majority of appropriately
adhesion molecules and conversion from capacity of the villi for gas and nutrient grown, healthy, term fetuses are able to
an epithelial to endothelial phenotype.11 exchange.33,34 Failure of spiral artery withstand the effects of this over a
By the late second trimester, the inner conversion renders these vessels suscep- prolonged period of time. Indeed,
third of the myometrial spiral arteries are tible to adrenergic stimulation and normal fetuses can cope with a reduc-
exclusively lined by CTendothelial cells,12 vasoconstriction,35,36 resulting in fluc- tion in PaO2 of up to 50% (from a PaO2
replacing the normal vascular smooth tuations in intervillous PaO2 and above 20 mm Hg to as low as 10e12
muscle with a noncontractile matrix that placental hypoxiaereperfusion injury. mm Hg)61,62 because of their high
is nonresponsive to neuronal and hor- Failure of CT endovascular invasion also myocardial glycogen stores,63,64 the
monal stimuli.13,14 These remodeled results in retention of a “functional presence of vascular shunts, the
vessels dilate 4-fold at their terminal sphincter,” an innervated stricture point increased oxygen affinity of HbF, and
portion,15 into low-resistance, high- at the junction of the uterine mucosa, near-maximal basal cardiac output.65,66
capacitance channels capable of predisposing to hypoxia, reperfusion The cornerstone of the fetal defense
increasing the supply of oxygen and nu- injury, and oxidative stress.37 Aberrant against hypoxic injury lies in the pe-
trients to the fetus to meet its growing development of the fetal vascular tree ripheral chemoreflex, triggered in
demands through gestation.16 This pro- within the placenta, as a consequence response to fetal hypoxia when utero-
cess is mediated by the interplay of several of dysregulation of the angiogenic placental perfusion declines by more
paracrine factors, including vascular and antiangiogenic factors at the than 50%.67,68 This has the sole aim of
endothelial growth factor, soluble fms- maternalefetal interface,38e40 further rapidly reducing oxygen consumption
like tyrosine kinase-1,17,18 and insulin- compromises placental function41e43 and centralizing blood flow to the crit-
like growth factor peptides I and II,19,20 and has been implicated in the devel- ical organs needed for preservation of
which are in turn modulated by opment of preeclampsia, fetal growth life and sensitive to hypoxic injury (the
pregnancy-associated plasma protein restriction (FGR), gestational diabetes brain, heart, and adrenal glands). The
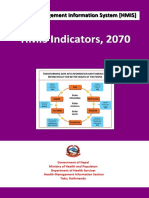
(PAPP-A) produced by trophoblast mellitus, placental abruption, preterm fetal adaptations, including the periph-
cells.21 Low PAPP-A levels are associated labor, and intrapartum fetal compromise eral chemoreflex, to transient hypoxia
with decreased bioavailability of insulin- (IFC).44e49 are summarized in Figure 1.
like growth factor peptides, limiting Acute hypoxemia, detected by
trophoblastic invasion22 and a range of Effect of Uterine Contractions on the carotid body chemoreceptors,
pregnancy disorders associated with Uteroplacental Perfusion stimulates the brain stem to increase
abnormal placentation.23e26 Uterine contractions during term labor both the parasympathetic and sympa-
Concurrent to trophoblast invasion is result in a rise in intrauterine pressure of thetic outflow.69,70 Parasympathetic
the development of new vessels within up to 25e70 mm Hg,50 compromising tone predominates,71 resulting in a
18 American Journal of Obstetrics & Gynecology JANUARY 2020
Downloaded for FK UMI Makassar (dosenfkumi01@gmail.com) at University of Muslim Indonesia from ClinicalKey.com by Elsevier on April 14, 2020.
For personal use only. No other uses without permission. Copyright ©2020. Elsevier Inc. All rights reserved.
ajog.org Expert Reviews
decrease in the fetal heart rate (FHR),
FIGURE 1
prolonging end-diastolic ventricular
filling time, and subsequently end-
Consequences of uterine contractions, fetal adaptions, and effect of
diastolic volume. The greater ventricu-
intrapartum fetal compromise
lar stretch increases sarcomere length,
tension, and contractility (Franke Modulators Uterine Activity
Uterine
Starling mechanism), maintaining fetal Metabolic Hormonal Neuronal
hyperstimulation
Acidosis E2, progesterone, PGE, α1 β2
cardiac output despite the decline in oxytocin, endothelin
FHR.72 In addition, the reduction in "[Ca2]¡ ![Ca2]¡
-
FHR reduces myocardial oxygen con- Uterine CONTRACTION Uterine RELAXATION
UTERINE VESSELS
sumption as well as allowing increased
Compression of uterine Rapid return of
transit time of red cells through tissue arcuate arteries & utero-placental perfusion
beds (including the placenta), thereby utero-placental vessels
permitting increased oxygen extraction
+
-
Rapid return of placental
from HbF and transplacental oxygen gas and waste exchange
PLACENTA 60% reduction in -
transfer to the fetal circulation.73 Intermittent placental utero-placental perfusion Inadequate
hypoxia & reperfusion + endovascular !Fetal and placental
Increased sympathetic outflow induces
invasion hypoxia & acidosis
profound peripheral vasoconstriction,
resulting in hypertension and centrali- "Oxidative stress !Intervillous perfusion
!Transplacental gas Peripheral chemoreflex
zation of blood flow to critical organs as + exchange re-set
well as balancing the parasympathetic Placental ischemia &
apoptosis
effects with a positive chronotropic ef- PATHOLOGICAL MECHANISMS PREDISPOSING TO IFC
fect, leading to a partial recovery in Inadequate/ abberant
!Myocardial
FHR.74,75 Furthermore, peripheral placentation
glycogen stores
vasoconstriction increases the Prior placental damage
e.g. placental abruption Pre-existing
descending aortic pressure, increasing hypoxemia
Insufficient recovery
right ventricular afterload that in turn between contractions
e.g. uterine hyperstimulation or Acidosis
encourages passage of blood from the inadequate placental function
right atrium, through the foramen
ovale, into the left atrium and thereafter FETUS
the left ventricle,76,77 causing an in- !Fetal PaO2
FETAL DECOMPENSATION
crease in blood flow into the ascending
Peripheral chemoreflex triggered !Myocardial responsiveness
aorta and cerebral and coronary
circulations.78,79
!Systemic BP
The initial neuronal triggered pe- "Sympathetic activity "Parasympathetic activity
ripheral vasoconstriction is then main-
!Cerebral Myocardial
tained by humoral factors, including Peripheral vasoconstriction, !FHR perfusion hypoxic damage
adrenal catecholamines, arginine vaso- "PVR & use of CVS shunts
pressin, cortisol, angiotensin II, and
Neuronal Damage
neuropeptide Y,80e84 which prolong the "EDV & CO !Myocardial oxygen
consumption
redistribution of cardiac output, Centralisation of blood flow
(brain, heart and adrenals)
thus maintaining perfusion to critical HYPOXIC ISCHEMIC
"MAP "CBF and cerebral perfusion ENCEPHALOPATHY
organs.
In addition, acute hypoxia stimulates
an increase in plasma adenosine85 and to Illustrated are the effects of uterine contractions upon the uterine vessels, myometrium, placenta,
a lesser extent nitric oxide86,87 and pros- and fetus with a schematic of the peripheral chemo-reflex and the processes/pathologies that
tinoids.88 These potent vasodilators interfere with the fetal protective mechanisms and result in hypoxic injury to the fetus.
further increase cerebral blood flow in- BP, blood pressure; [Ca2þ]I, intracellular calcium; CBF, cerebral blood flow; CO, cardiac output; CVS, cardiovascular system; E2,
estrogen; EDV, end-diastolic volume (cardiac); FHR, fetal heart rate; IFC, intrapartum fetal compromise; MAP, mean arterial pressure;
dependent of the centralization of cardiac PaO2, partial pressure of oxygen; PGE, prostaglandin E2 and F2; PVR, peripheral vascular resistance; ROS, reactive oxygen species.
output,85,89 with adenosine accounting Turner JM. Physiology of intrapartum fetal compromise at term. Am J Obstet Gynecol 2020.
for more than one-half of this increase.90
With uterine relaxation, there is rapid efficiently metabolize lactate (by oxida- These processes allow the autonomic
return of efficient placental gas ex- tion and conversion to nonessential fetal response to be reactivated during
change, restoring fetal PaO2 levels and amino acids and lipids),92,93 rapidly the next contraction, ensuring protec-
removing lactate and carbon dioxide.91 reversing the metabolic acidosis that tion from the repeated hypoxic episodes
In addition, the fetus is able to occurs during the preceding contraction. that characterize labor.74,91
JANUARY 2020 American Journal of Obstetrics & Gynecology 19
Downloaded for FK UMI Makassar (dosenfkumi01@gmail.com) at University of Muslim Indonesia from ClinicalKey.com by Elsevier on April 14, 2020.
For personal use only. No other uses without permission. Copyright ©2020. Elsevier Inc. All rights reserved.
Expert Reviews ajog.org
When and why does IFC occur? myocardial dysfunction progresses with during the reperfusion phase114 due to
It has now clear that fetal decompensa- worsening cerebral and in particular toxicity from reactive oxygen species and
tion in labor occurs because of the in- brain stem hypoxia, the fetal para- excessive stimulation of N-methyl-D-
fant’s inability to respond to the sympathetic response may fail aspartate-type glutamate re-
peripheral chemoreflex to maintain altogether. ceptors.115,116 Indeed, the severity of the
cardiac output.74,94 IFC may occur when The magnitude of the hypoxic insult secondary injury occurring during the
there is inadequate reperfusion time correlates with the fetal response. Sir- reperfusion phase correlates best with
between contractions (eg, during uterine istatidis et al104 demonstrated that the the severity of neurodevelopmental
hyperstimulation) or when there is “brain-sparing” response is only acti- disability at ages 1 and 4 years.117 There
appropriate reperfusion time but sub- vated when fetal PaO2 falls below 37%. is a strong association between hypo-
optimal placental function to allow However, if the PaO2 falls below 30% for tension and hypoxia with fetal injury,
adequate oxygen transfer to the more than 2 minutes, this response fails particularly neuronal damage and fetal
fetus.95,96 altogether and significantly increases the death.113 During hypoxia, blood flow to
Impaired placental development and risk of adverse perinatal outcomes.105 the cerebral hemispheres is reduced,
function renders the fetus vulnerable to whereas perfusion to the basal ganglia,
intrapartum hypoxia through several The impact of intrapartum hypoxic thalamus, and brainstem is increased.118
mechanisms. First, a greater reduction in injury Animal studies have demonstrated that
uteroplacental perfusion occurs for any The fetus adapts to hypoxia by prefer- episodes of intermittent hypoxia
rise in intrauterine pressure due to the entially redistributing its cardiac output, accompanied by recurrent fetal hypo-
smaller surface area of the unconverted mediated by neuroendocrine mecha- tension cause neuronal loss in the
spiral arteries. Consequently, the degree nisms, to its coronary arteries, adrenal “watershed” zones of the brain (the
of fetal hypoxia is greater with each glands (for production of catechol- parasagittal sinus, cerebellar neocortex,
contraction than that which occurs in a amines critical for sustaining circula- and the dorsal horn of the hippocam-
fetus with a normally developed and tion),104 and brain. Occasionally, if the pus).119,120 By comparison, hypoxia
functioning placenta. Furthermore, hypoxic insult is severe or prolonged without hypotension predisposes to
inadequate placental function is associ- enough, these protective mechanisms cerebellar injury.121 Animal studies sug-
ated with the progressive development of fail, and profound multiorgan injury or gest that, even if the total duration of
severe fetal acidosis, even with adequate death can occur. hypoxia is the same, repeated severe ep-
time between contractions, due to an isodes cause greater neurologic injury
inability to correct the impaired gas ex- Hypoxic ischemic encephalopathy. The than a single severe prolonged event.122
change between contractions.97,98 fetal brain is particularly sensitive to This is consistent with recent evidence
Women with pre-labor placental hypoxic injury and oxidative stress due showing that the FHR deceleration area
dysfunction are more likely to develop to its high rate of oxygen consumption, of the cardiotocograph (ie, a composite
IFC. These fetuses are less likely to lack of glucose stores (therefore all of duration and severity) was most
withstand intrapartum hypoxia due to cellular events that are adenosine discriminative of acidemia in term in-
lower glycogen stores before the onset of triphosphate and oxygen dependent fants.123 In addition, the pattern of
labor, limiting their ability to transition rapidly fail), high lipid content neuronal damage is further influenced
to anaerobic metabolism.99 As even (rendering neurons susceptible to lipid by the pre-labor metabolic and growth
short periods of hypoxia can quickly peroxidation in an autocatalytic fashion status of the fetus,124 as well as metabolic
deplete cerebral and cardiac glycogen by triggered by oxidative stress, leading to and nutritional status of the mother.125
up to 80%,64 any limitation in placental structural and function damage),106,107
transfer of nutrients and oxygen renders and relatively low concentrations and Noncerebral consequences of intrapartum
these fetuses vulnerable to IFC and activity of antioxidant enzymes.108,109 hypoxia. After the brain, the renal system
injury. Progressive hypoxia in labor re- HIE is defined as neonatal encephalop- is the most common organ system to be
sults in a further reduction of myocardial athy (cerebral obtundation with injured following severe intrapartum
glycogen stores, impaired cardiac func- disturbed neurological function)110 sec- hypoxia, with up to 64% of hypoxic term
tion,100,101 and, ultimately, profound ondary to systemic hypoxia and reduced infants developing renal dysfunction
systemic hypotension and irreversible cerebral perfusion, resulting in ischemic usually secondary to acute tubular
multiorgan injury.63,64 Cardiac function injury that may be focal or diffuse.111,112 necrosis.126e128 Severely hypoxic infants
is further aggravated by the associated In one study, 51% of neonates with often require dialysis to support renal
systemic hypotension, limiting coronary moderate or severe encephalopathy died function, with an associated mortality
blood flow and causing subendocardial or developed cerebral palsy).113 rate of between 14% and 70%.129,130
myocardial injury.102 Jones et al103 The mechanisms of hypoxic cerebral Between 25% and 50% of hypoxic
recently demonstrated that infants with damage are complex and not entirely infants experience pulmonary compli-
HIE have elevated troponin-T levels, a mediated by the initial hypoxic insult but cations131 and up to 20% require me-
marker of myocardial cell death. As are compounded by injuries occurring chanical ventilation.132 Both hypoxia
20 American Journal of Obstetrics & Gynecology JANUARY 2020
Downloaded for FK UMI Makassar (dosenfkumi01@gmail.com) at University of Muslim Indonesia from ClinicalKey.com by Elsevier on April 14, 2020.
For personal use only. No other uses without permission. Copyright ©2020. Elsevier Inc. All rights reserved.
ajog.org Expert Reviews
and hyperoxia133 (from oxygen therapy thereby potentially missing late-onset hypoxic fetuses.154 Despite these limita-
and ventilation in the neonatal period) growth restriction. tions, it remains the mainstay for intra-
impair alveolar development134 and More recently, the fetal cere- partum fetal monitoring despite having a
predispose to persistent pulmonary hy- broplacental ratio (CPR) (ratio of the false-positive rate as high as 99.8%.155,156
pertension and reactive airway disease, middle cerebral artery pulsatility index to Although the use of intrapartum elec-
which may persist into adulthood.135 the umbilical artery pulsatility index) has tronic FHR monitoring has resulted in a
Cardiac complications occur in up to been proposed as a proxy for intrauterine reduction in the incidence of neonatal
29% of infants with severe intrapartum growth with a low CPR indicative of seizures, there is no improvement in
hypoxia with evidence of myocardial suboptimal fetal growth. A low CPR perinatal death or cerebral palsy rates
ischemia on electrocardiogram seen in (variably defined as <1.0, <5th centile, despite an increase in operative births.155
almost 1 in 5 cases.131 Other organ sys- <10th centile, or <0.67 Multiples of The implementation of CTG monitoring
tems, including hepatic (35%) and Median [MoM])143,144 is associated with use and interpretation guidelines has
gastrointestinal (5%), may be affected. a range of adverse perinatal outcomes, nevertheless reduced the incidence of
More than one-half of infants with HIE including neonatal intensive care admis- HIE.157e160 However, the use of
have multiorgan dysfunction.131,135 sion, acidosis, and emergency operative computerized CTG analysis software has
There are many factors that influence birth for IFC.145,146 However, despite the failed to demonstrate any significant
the severity of neonatal morbidity broad association with adverse outcomes, improvement in maternal or neonatal
following intrauterine hypoxia as well as the predictive utility of the CPR, partic- outcomes compared with standard FHR
our ability to predict the likelihood of ularly in a non-SGA cohort at term, re- monitoring.161,162
hypoxia-related complications.135,136 mains modest, and caution should be Assessment of fetal wellbeing using
137
Low et al demonstrated that exercised before incorporating its routine ST-segment waveform analysis from the
although the range and severity of use into clinical care.147 fetal electrocardiogram163,164 has been
neonatal complications increased with proposed as an adjunct to conventional
the degree of metabolic acidosis, there Biochemical markers. Low PAPP-A levels FHR monitoring. Westgate et al165
was a great deal of heterogeneity between are indicative of failure of trophoblast investigated the use of ST-segment
fetuses, a likely reflection of the nature invasion and placental dysfunction22 and analysis in animal models and demon-
and length of asphyxial event. associated with an increased risk of FGR, strated that although the T/QRS ratio
preeclampsia, intrauterine fetal demise, indicated hypoxic stress, it correlated
Pre-labor identification of the “at-risk” placental abruption, preterm birth, poorly with the severity of fetal hypoxia
fetus emergency cesarean delivery for IFC, or hypotension. Several randomized
There is now evidence that some and neonatal acidosis.24,26 Although low controlled trials and meta-analyses have
apparently normally grown fetuses have maternal PlGF levels in the third produced conflicting results, with the
circulatory changes including cerebral trimester have been shown to be associ- most recent randomized controlled trial
redistribution similar to that seen in ated with IFC and adverse neonatal not demonstrating any improvement in
FGR. These fetuses are particularly outcomes,148,149 the evidence is con- either neonatal outcomes or reduction in
vulnerable to intrapartum hypoxia and flicting with another recent study, sug- operative birth rates.164 A recent obser-
compromise.138e140 gesting that it did not predict cesarean vational study showed that the imple-
Low birth weight at term is a major birth for fetal compromise.150 mentation of intrapartum ST-segment
risk factor for emergency operative birth waveform resulted in a substantial
for IFC, perinatal death, and serious Identification of intrapartum fetal reduction in rates of umbilical artery
neonatal morbidity even in low-risk compromise metabolic acidosis as well as a significant
pregnancies,141 partly due to the pro- Despite concerted efforts to develop ac- reduction in operative birth rates, fetal
portion of small for gestational age curate techniques for the identification blood sampling, and incidence of
(SGA) babies that are growth restricted. of intrapartum fetal hypoxia, to date all neonatal encephalopathy.166
As not all growth-restricted fetuses are techniques currently in clinical practice Fetal pulse oximetry (FPO) was
SGA, parameters other than standard have poor positive predictive values.151 developed as an adjunct to electronic
biometry are required to identify these Reviews of conventional antepartum FHR monitoring, particularly in the
at-risk infants before birth. Cochrane cardiotocography (CTG), computerized context of a nonreassuring FHR pattern.
reviews do not support the use of either FHR analysis, or intermittent ausculta- Fetal PO2 saturations less than 30% are
routine late pregnancy ultrasound or tion have concluded that they do not considered abnormal and corelate with
umbilical artery Doppler assessment in result in improved perinatal out- hypoxic injury.104 In May 2000, the Food
low-risk populations.142 However, these comes.152,153 The CTG has poor char- and Drug Administration granted
reviews are limited by small sample size, acteristics as a test: interpretation is approval for use of FPO167 as an adjunct
use of surrogate outcomes, and most subjective, it has poor intra- and inter- to FHR monitoring based on a single
importantly, ultrasound scans that were observer agreement, and lacks discrimi- randomized controlled trial that showed a
often performed too remote from term, natory power in identifying truly significant reduction in cesarean section
JANUARY 2020 American Journal of Obstetrics & Gynecology 21
Downloaded for FK UMI Makassar (dosenfkumi01@gmail.com) at University of Muslim Indonesia from ClinicalKey.com by Elsevier on April 14, 2020.
For personal use only. No other uses without permission. Copyright ©2020. Elsevier Inc. All rights reserved.
Expert Reviews ajog.org
(CS) for IFC.168 However in 2006, a large, REFERENCES 16. Red-Horse K, Zhou Y, Genbacev O, et al.
multicenter randomized controlled trial Trophoblast differentiation during embryo im-
1. Lawn JE, Blencowe H, Oza S, et al. Every
plantation and formation of the maternal-fetal
demonstrated that FPO as an adjunct to newborn: progress, priorities, and potential
interface. J Clin Invest 2004;114:744–54.
FHR monitoring did not reduce the rate beyond survival. Lancet 2014;384:189–205.
2. Lawn J, Shibuya K, Stein C. No cry at birth: 17. Ahmed A. Angiogenic growth factors in
of CS for any indication.169 An updated pregnancy. In: Aplin JD KP, Schaaps JP,
global estimates of intrapartum stillbirths and
Cochrane review in 2013 of 7 published intrapartum-related neonatal deaths. Bull World Foidart JM, eds. Trophoblast research, early
trials demonstrated that although FPO Health Organ 2005;83:409–17. pregnancy. Vol. 9. New York: University of
3. McIntyre S, Taitz D, Keogh J, Goldsmith S, Rochester Press; 1997. p. 215–58.
did not impact overall CS rates compared
Badawi N, Blair E. A systematic review of risk 18. Ahmed A, Li XF, Dunk C, Whittle MJ,
with FHR monitoring alone, there was a Rushton DI, Rollason T. Colocalisation of
factors for cerebral palsy in children born at term
reduction in CS for IFC.170 vascular endothelial growth factor and its Flt-1
in developed countries. Dev Med Child Neurol
Intrapartum assessment of fetal scalp 2013;55:499–508. receptor in human placenta. Growth Factors
pH or lactate has not resulted in a decline 4. GBD 2017 DALYs and HALE Collaborators. 1995;12:235–43.
in operative birth rates for IFC, neonatal Global, regional, and national disability-adjusted 19. McKinnon T, Chakraborty C, Gleeson LM,
life-years (DALYs) for 359 diseases and injuries Chidiac P, Lala PK. Stimulation of human
acidosis, or adverse neonatal outcomes
and healthy life expectancy (HALE) for 195 extravillous trophoblast migration by IGF-II is
compared with the use of FHR moni- mediated by IGF type 2 receptor involving
countries and territories, 1990-2017: a system-
toring alone. atic analysis for the Global Burden of Disease inhibitory G protein(s) and phosphorylation of
Study 2017. Lancet 2018;392:1859–922. MAPK. J Clin Endocrinol Metab 2001;86:
5. Low JA, Pickersgill H, Killen H, Derrick EJ. 3665–74.
Conclusion The prediction and prevention of intrapartum 20. Lacey H, Haigh T, Westwood M, Aplin JD.
Although the etiology of IFC is multi- fetal asphyxia in term pregnancies. Am J Obstet Mesenchymally-derived insulin-like growth fac-
factorial, placental dysfunction and a Gynecol 2001;184:724–30. tor 1 provides a paracrine stimulus for tropho-
mismatch between its functional ability 6. Janbu T, Nesheim BI. Uterine artery blood blast migration. BMC Dev Biol 2002;2:5.
and the metabolic requirements of fetus velocities during contractions in pregnancy and 21. Bonno M, Oxvig C, Kephart GM, et al.
labour related to intrauterine pressure. Br J Localization of pregnancy-associated plasma
during labor is causative in the majority protein-A and colocalization of pregnancy-
Obstet Gynaecol 1987;94:1150–5.
of cases. Labor is characterized by 7. Jauniaux E, Watson AL, Hempstock J, associated plasma protein-A messenger ribo-
repeated transient episodes of fetal hyp- Bao YP, Skepper JN, Burton GJ. Onset of nucleic acid and eosinophil granule major basic
oxia that, under normal circumstances, maternal arterial blood flow and placental protein messenger ribonucleic acid in placenta.
an appropriately grown fetus with normal oxidative stress. A possible factor in human early Lab Invest 1994;71:560–6.
pregnancy failure. Am J Pathol 2000;157: 22. Qiu Q, Bell M, Lu X, et al. Significance of
or minimal placental dysfunction is able IGFBP-4 in the development of fetal growth re-
2111–22.
to tolerate. However, when there is pre- 8. Burton GJ. Oxygen, the Janus gas; its effects striction. J Clin Endocrinol Metab 2012;97:
existing placental dysfunction, inade- on human placental development and function. E1429–39.
quate uterine relaxation between con- J Anatomy 2009;215:27–35. 23. Johnson MR, Riddle AF, Grudzinskas JG,
tractions, or if the fetus is growth 9. Genbacev O, Zhou Y, Ludlow JW, Sharma V, Collins WP, Nicolaides KH. Reduced
Fisher SJ. Regulation of human placental circulating placental protein concentrations
restricted with suboptimal metabolic re- during the first trimester are associated with
development by oxygen tension. Science
serves, intrapartum fetal hypoxia can 1997;277:1669–72. preterm labour and low birth weight. Hum
ensue. In extreme cases, this can result in 10. Burton GJ, Jauniaux E, Watson AL. Reprod 1993;8:1942–7.
myocardial injury, systemic hypotension, Maternal arterial connections to the placental 24. Smith GC, Shah I, Crossley JA, et al.
cerebral hypoperfusion, and neuronal intervillous space during the first trimester of Pregnancy-associated plasma protein A and
human pregnancy: the Boyd collection revisited. alpha-fetoprotein and prediction of adverse
damage. Neonatal encephalopathy can perinatal outcome. Obstet Gynecol 2006;107:
Am J Obstet Gynecol 1999;181:718–24.
have catastrophic consequences, with 1 in 11. Zhou Y, Fisher SJ, Janatpour M, et al. Hu- 161–6.
2 infants either having significant neuro- man cytotrophoblasts adopt a vascular pheno- 25. Spencer K, Cowans NJ, Nicolaides KH. Low
developmental delay, cerebral palsy, or type as they differentiate. A strategy for levels of maternal serum PAPP-A in the first
death by the age of 2. successful endovascular invasion? J Clin Invest trimester and the risk of pre-eclampsia. Prenat
1997;99:2139–51. Diagn 2008;28:7–10.
The challenges in this field are first, 26. Uccella S, Colombo GF, Bulgheroni CM,
12. Maltepe E, Bakardjiev AI, Fisher SJ. The
the development of a reliable pre-labor placenta: transcriptional, epigenetic, and physi- et al. First-trimester maternal serum screening
test that accurately identifies fetuses at ological integration during development. J Clin and the risk for fetal distress during labor. Am J
risk of intrapartum compromise, second Invest 2010;120:1016–25. Obstet Gynecol 2009;201:166 e161–6.
to develop new or refine current intra- 13. Pijnenborg R, Vercruysse L, Hanssens M. 27. Demir R, Kayisli UA, Cayli S, Huppertz B.
The uterine spiral arteries in human pregnancy: Sequential steps during vasculogenesis and
partum techniques for fetal monitoring, angiogenesis in the very early human placenta.
facts and controversies. Placenta 2006;27:
and finally a prenatal or intrapartum 939–58. Placenta 2006;27:535–9.
treatment that can either prevent the 14. Lyall F. Priming and remodelling of human 28. Cao Y, Linden P, Shima D, Browne F,
development of intrapartum hypoxia or placental bed spiral arteries during pregnancy— Folkman J. In vivo angiogenic activity and hyp-
mitigate some of its perinatal complica- a review. Placenta 2005;26(suppl A):S31–6. oxia induction of heterodimers of placenta
15. Brosens I. A Study of the spiral arteries of the growth factor/vascular endothelial growth fac-
tions. Accompanying these should be tor. J Clin Invest 1996;98:2507–11.
decidua basalis in normotensive and hyperten-
safe intrapartum care provided by sive pregnancies. J Obstet Gynaecol Br Com- 29. Khaliq A, Dunk C, Jiang J, et al. Hypoxia
trained caregivers. - monw 1964;71:222–30. down-regulates placenta growth factor,
22 American Journal of Obstetrics & Gynecology JANUARY 2020
Downloaded for FK UMI Makassar (dosenfkumi01@gmail.com) at University of Muslim Indonesia from ClinicalKey.com by Elsevier on April 14, 2020.
For personal use only. No other uses without permission. Copyright ©2020. Elsevier Inc. All rights reserved.
ajog.org Expert Reviews
whereas fetal growth restriction up-regulates 43. Talbert DG. Uterine flow velocity waveform stress in trophoblast cells from the human
placenta growth factor expression: molecular shape as an indicator of maternal and placental placenta. Placenta 2005;26:210–7.
evidence for "placental hyperoxia" in intrauterine development failure mechanisms: a model- 58. Dunn L, Flatley C, Kumar S. Changes in
growth restriction. Lab Invest 1999;79:151–70. based synthesizing approach. Ultrasound maternal placental growth factor levels during
30. Shore VH, Wang TH, Wang CL, Torry RJ, Obstet Gynecol 1995;6:261–71. term labour. Placenta 2018;61:11–6.
Caudle MR, Torry DS. Vascular endothelial 44. Leung DN, Smith SC, To KF, Sahota DS, 59. Fleischer A, Anyaegbunam AA,
growth factor, placenta growth factor and their Baker PN. Increased placental apoptosis in Schulman H, Farmakides G, Randolph G. Uter-
receptors in isolated human trophoblast. pregnancies complicated by preeclampsia. Am ine and umbilical artery velocimetry during
Placenta 1997;18:657–65. J Obstet Gynecol 2001;184:1249–50. normal labor. Am J Obstet Gynecol 1987;157:
31. Desai J, Holt-Shore V, Torry RJ, Caudle MR, 45. Smith SC, Baker PN, Symonds EM. 40–3.
Torry DS. Signal transduction and biological Increased placental apoptosis in intrauterine 60. Brar HS, Platt LD, DeVore GR, Horenstein J,
function of placenta growth factor in primary growth restriction. Am J Obstet Gynecol Medearis AL. Qualitative assessment of
human trophoblast. Biol Reprod 1999;60: 1997;177:1395–401. maternal uterine and fetal umbilical artery blood
887–92. 46. Fisher SJ. Why is placentation abnormal in flow and resistance in laboring patients by
32. Scifres CM, Nelson DM. Intrauterine growth preeclampsia? Am J Obstet Gynecol 2015;213: Doppler velocimetry. Am J Obstet Gynecol
restriction, human placental development and S115–22. 1988;158:952–6.
trophoblast cell death. J Physiol 2009;587: 47. Ananth CV. Ischemic placental disease: a 61. Jansen CA, Krane EJ, Thomas AL, et al.
3453–8. unifying concept for preeclampsia, intrauterine Continuous variability of fetal PO2 in the chron-
33. Savasan ZA, Goncalves LF, Bahado-Singh growth restriction, and placental abruption. Pa- ically catheterized fetal sheep. Am J Obstet
RO. Second-and third-trimester biochemical per presented at: Seminars in perinatology 2014. Gynecol 1979;134:776–83.
and ultrasound markers predictive of ischemic 48. Fisher SJ, McMaster M, Roberts JM. The 62. Giussani DA, Spencer JAD, Hanson MA.
placental disease. Paper presented at: Seminars placenta in normal pregnancy and preeclamp- Fetal cardiovascular reflex responses to hypo-
in perinatology 2014. sia. In: Taylor RN, Roberts J, Cunningham R, xaemia. Fetal Maternl Med Rev 1994;6:17–37.
34. Burton GJ, Jones CJ. Syncytial knots, Lindheimer M, eds. Chesley’s hypertensive dis- 63. Jensen A, Garnier Y, Berger R. Dynamics of
sprouts, apoptosis, and trophoblast deportation orders of pregnancy, 4th ed. San Diego: Aca- fetal circulatory responses to hypoxia and
from the human placenta. Taiwan J Obstet demic Press; 2015. p. 81–112. asphyxia. Eur J Obstet Gynecol Reprod Biol
Gynecol 2009;48:28–37. 49. Maltepe E, Fisher SJ. Placenta: the 1999;84:155–72.
35. Adamsons K, Mueller-Heubach E, forgotten organ. Annu Rev Cell Dev Biol 64. Dawes GS, Mott JC, Shelley HJ. The
Myers RE. Production of fetal asphyxia in the 2015;31:523–52. importance of cardiac glycogen for the mainte-
rhesus monkey by administration of catechol- 50. Allman AC, Genevier ES, Johnson MR, nance of life in foetal lambs and newborn animals
amines to the mother. Am J Obstet Gynecol Steer PJ. Head-to-cervix force: an important during anoxia. J Physiol 1959;146:516–38.
1971;109:248–62. physiological variable in labour. 1. The temporal 65. Shelley HJ. Glycogen reserves and their
36. Adamsons K, Myers RE. Circulation in the relation between head-to-cervix force and in- changes at birth and in anoxia. Br Med Bull
intervillous space; obstetrical considerations in trauterine pressure during labour. Br J Obstet 1961;17:137–43.
fetal deprivation. In: Gruenwald P, ed. The Gynaecol 1996;103:763–8. 66. Harding R, Bocking AD. Fetal growth and
placenta and its maternal supply line. Effects of 51. Borell U, Fernstroem I, Ohlson L, Wiqvist N. development. Cambridge: Cambridge Univer-
insufficiency on the fetus. Lancaster: Medical Influence of uterine contractions on the utero- sity Press; 2001.
and Technical Publishing Co. Ltd; 1975. p. placental blood flow at term. Am J Obstet 67. Rudolph AM. Distribution and regulation of
158–77. Gynecol 1965;93:44–57. blood flow in the fetal and neonatal lamb. Circ
37. Brosens JJ, Pijnenborg R, Brosens IA. The 52. Sato M, Noguchi J, Mashima M, Tanaka H, Res 1985;57:811–21.
myometrial junctional zone spiral arteries in Hata T. 3D power Doppler ultrasound assess- 68. Ross MG, Jessie M, Amaya K, et al. Corre-
normal and abnormal pregnancies: a review of ment of placental perfusion during uterine lation of arterial fetal base deficit and lactate
the literature. Am J Obstet Gynecol 2002;187: contraction in labor. Placenta 2016;45:32–6. changes with severity of variable heart rate de-
1416–23. 53. Sinding M, Peters DA, Frokjaer JB, celerations in the near-term ovine fetus. Am J
38. Kon K, Fujii S, Kosaka H, Fujiwara T. Nitric Christiansen OB, Uldbjerg N, Sorensen A. Obstet Gynecol 2013;208:285 e281–6.
oxide synthase inhibition by N(G)-nitro-L- Reduced placental oxygenation during subclin- 69. Itskovitz J, LaGamma EF, Rudolph AM.
arginine methyl ester retards vascular sprouting ical uterine contractions as assessed by BOLD Heart rate and blood pressure responses to
in angiogenesis. Microvasc Res 2003;65:2–8. MRI. Placenta 2016;39:16–20. umbilical cord compression in fetal lambs with
39. Fisher SJ. The placental problem: linking 54. Cindrova-Davies T, Yung HW, Johns J, et al. special reference to the mechanism of variable
abnormal cytotrophoblast differentiation to the Oxidative stress, gene expression, and protein deceleration. Am J Obstet Gynecol 1983;147:
maternal symptoms of preeclampsia. Reprod changes induced in the human placenta during 451–7.
Biol Endocrinol 2004;2:53. labor. Am J Pathol 2007;171:1168–79. 70. Itskovitz J, LaGamma EF, Bristow J,
40. Zhou Z, Yang XM, Xie YZ, Yin ZY. Vascular 55. Mizuuchi M, Cindrova-Davies T, Rudolph AM. Cardiovascular responses to
endothelial growth factor gene expression Olovsson M, Charnock-Jones DS, Burton GJ, hypoxemia in sinoaortic-denervated fetal sheep.
regulated by protein kinase C pathway in Yung HW. Placental endoplasmic reticulum Pediatr Res 1991;30:381–5.
endothelial cells during hypoxia. Space Med stress negatively regulates transcription of 71. Giussani DA, Spencer JA, Moore PJ,
Med Eng (Beijing) 2002;15:322–6. placental growth factor via ATF4 and ATF6beta: Bennet L, Hanson MA. Afferent and efferent
41. Rodesch F, Simon P, Donner C, Jauniaux E. implications for the pathophysiology of human components of the cardiovascular reflex re-
Oxygen measurements in endometrial and pregnancy complications. J Pathol 2016;238: sponses to acute hypoxia in term fetal sheep.
trophoblastic tissues during early pregnancy. 550–61. J Physiol 1993;461:431–49.
Obstet Gynecol 1992;80:283–5. 56. Many A, Roberts JM. Increased xanthine 72. Court DJ, Parer JT, Block BS, Llanos AJ.
42. Soothill PW, Nicolaides KH, Rodeck CH, oxidase during labour—implications for oxida- Effects of beta-adrenergic blockade on blood
Campbell S. Effect of gestational age on fetal tive stress. Placenta 1997;18:725–6. flow distribution during hypoxaemia in fetal
and intervillous blood gas and acid-base values 57. Li H, Gu B, Zhang Y, Lewis DF, Wang Y. sheep. J Dev Physiol 1984;6:349–58.
in human pregnancy. Fetal Ther 1986;1: Hypoxia-induced increase in soluble Flt-1 pro- 73. Anderson PA, Glick KL, Killam AP,
168–75. duction correlates with enhanced oxidative Mainwaring RD. The effect of heart rate on in
JANUARY 2020 American Journal of Obstetrics & Gynecology 23
Downloaded for FK UMI Makassar (dosenfkumi01@gmail.com) at University of Muslim Indonesia from ClinicalKey.com by Elsevier on April 14, 2020.
For personal use only. No other uses without permission. Copyright ©2020. Elsevier Inc. All rights reserved.
Expert Reviews ajog.org
utero left ventricular output in the fetal sheep. normoxemia and hypoxemia. Biol Neonate 103. Jones R, Heep A, Odd D. Biochemical and
J Physiol 1986;372:557–73. 1995;68:200–10. clinical predictors of hypoxic-ischemic enceph-
74. Bennet L, Gunn AJ. The fetal heart rate 89. Nishida N, Blood AB, Hunter CJ, et al. Role alopathy after perinatal asphyxia. J Matern Fetal
response to hypoxia: insights from animal of prostanoids in the regulation of cerebral blood Neonatal Med 2018;31:791–6.
models. Clin Perinatol 2009;36:655–72. flow during normoxia and hypoxia in the fetal 104. Siristatidis C, Salamalekis E, Kassanos D,
75. Galinsky R, Jensen EC, Bennet L, et al. sheep. Pediatr Res 2006;60:524–9. Loghis C, Creatsas G. Evaluation of fetal intra-
Sustained sympathetic nervous system support 90. Giussani DA, Gardner DS, Cox DT, partum hypoxia by middle cerebral and umbilical
of arterial blood pressure during repeated brief Fletcher AJ. Purinergic contribution to circula- artery Doppler velocimetry with simultaneous
umbilical cord occlusions in near-term fetal tory, metabolic, and adrenergic responses to cardiotocography and pulse oximetry. Arch
sheep. Am J Physiol Regul Integr Comp Physiol acute hypoxemia in fetal sheep. Am J Physiol Gynecol Obstet 2004;270:265–70.
2014;306:R787–95. Regul Integr Comp Physiol 2001;280:R678–85. 105. Gunn AJ, Maxwell L, De Haan HH, et al.
76. Giussani DA. The fetal brain sparing 91. Park TS, Van Wylen DG, Rubio R, Delayed hypotension and subendocardial injury
response to hypoxia: physiological mecha- Berne RM. Increased brain interstitial fluid after repeated umbilical cord occlusion in near-
nisms. J Physiol 2016;594:1215–30. adenosine concentration during hypoxia in term fetal lambs. Am J Obstet Gynecol
77. Griffin D, Bilardo K, Masini L, et al. Doppler newborn piglet. J Cereb Blood Flow Metab 2000;183:1564–72.
blood flow waveforms in the descending 1987;7:178–83. 106. Bloom SL, Swindle RG, McIntire DD,
thoracic aorta of the human fetus. Br J Obstet 92. Bennet L, Westgate JA, Liu YC, Wassink G, Leveno KJ. Fetal pulse oximetry: duration of
Gynaecol 1984;91:997–1006. Gunn AJ. Fetal acidosis and hypotension during desaturation and intrapartum outcome. Obstet
78. Akalin-Sel T, Nicolaides KH, Peacock J, repeated umbilical cord occlusions are associ- Gynecol 1999;93:1036–40.
Campbell S. Doppler dynamics and their com- ated with enhanced chemoreflex responses in 107. Stockwell BR, Angeli JPF, Bayir H, et al.
plex interrelation with fetal oxygen pressure, near-term fetal sheep. J Appl Physiol (1985) Ferroptosis: a regulated cell death nexus linking
carbon dioxide pressure, and pH in growth- 2005;99:1477–82. metabolism, redox biology, and disease. Cell
retarded fetuses. Obstet Gynecol 1994;84: 93. Carter BS, Moores RR Jr, Teng C, 2017;171:273–85.
439–44. Meschia G, Battaglia FC. Main routes of plasma 108. Cuypers A, Plusquin M, Remans T, et al.
79. Arbeille P, Maulik D, Fignon A, et al. lactate carbon disposal in the midgestation fetal Cadmium stress: an oxidative challenge. Bio-
Assessment of the fetal PO2 changes by cere- lamb. Biol Neonate 1995;67:295–300. metals 2010;23:927–40.
bral and umbilical Doppler on lamb fetuses 94. Bartelds B, Knoester H, Smid GB, et al. 109. Miller SL, Wallace EM, Walker DW. Anti-
during acute hypoxia. Ultrasound Med Biol Perinatal changes in myocardial metabolism in oxidant therapies: a potential role in perinatal
1995;21:861–70. lambs. Circulation 2000;102:926–31. medicine. Neuroendocrinology 2012;96:13–23.
80. Wladimiroff JW, Tonge HM, Stewart PA. 95. Galinsky R, Lear CA, Yamaguchi K, et al. 110. McLean C, Ferriero D. Mechanisms of
Doppler ultrasound assessment of cerebral Cholinergic and beta-adrenergic control of car- hypoxic-ischemic injury in the term infant. Semin
blood flow in the human fetus. Br J Obstet diovascular reflex responses to brief repeated Perinatol 2004;28:425–32.
Gynaecol 1986;93:471–5. asphyxia in term-equivalent fetal sheep. Am J 111. Schendel D. Executive summary: neonatal
81. Broughton Pipkin F, Lumbers ER, Mott JC. Physiol Regul Integr Comp Physiol 2016;311: encephalopathy and neurologic outcome,
Factors influencing plasma renin and angio- R949–56. Report of the American College of Obstetricians
tensin II in the conscious pregnant ewe and its 96. Lear CA, Wassink G, Westgate JA, et al. The and Gynecologists’ task force on neonatal en-
foetus. J Physiol 1974;243:619–36. peripheral chemoreflex: indefatigable guardian cephalopathy. Obstet Gynecol 2014;123:
82. Giussani DA, McGarrigle HH, of fetal physiological adaptation to labour. 896–901.
Spencer JA, Moore PJ, Bennet L, J Physiol 2018;596:5611–23. 112. Cotten CM, Shankaran S. Hypothermia for
Hanson MA. Effect of carotid denervation on 97. Bakker PC, Kurver PH, Kuik DJ, Van hypoxiceischemic encephalopathy. Exp Rev
plasma vasopressin levels during acute hyp- Geijn HP. Elevated uterine activity increases the Obstet Gynecol 2010;5:227–39.
oxia in the late-gestation sheep fetus. risk of fetal acidosis at birth. Am J Obstet 113. Pierrat V, Haouari N, Liska A, et al. Preva-
J Physiol 1994;477:81–7. Gynecol 2007;196:313 e311–6. lence, causes, and outcome at 2 years of age of
83. Jones CT, Robinson RO. Plasma catechol- 98. Simpson KR, James DC. Effects of newborn encephalopathy: population based
amines in foetal and adult sheep. J Physiol oxytocin-induced uterine hyperstimulation dur- study. Arch Dis Child Fetal Neonatal Ed
1975;248:15–33. ing labor on fetal oxygen status and fetal heart 2005;90:F257–61.
84. Fletcher AJ, Edwards CM, Gardner DS, rate patterns. Am J Obstet Gynecol 2008;199: 114. Gunn AJ, Bennet L. Fetal hypoxia insults
Fowden AL, Giussani DA. Neuropeptide Y in the 34 e31–5. and patterns of brain injury: insights from animal
sheep fetus: effects of acute hypoxemia and 99. Wassink G, Bennet L, Davidson JO, models. Clin Perinatol 2009;36:579–93.
dexamethasone during late gestation. Endocri- Westgate JA, Gunn AJ. Pre-existing hypoxia is 115. Choi DW, Rothman SM. The role of gluta-
nology 2000;141:3976–82. associated with greater EEG suppression and mate neurotoxicity in hypoxic-ischemic neuronal
85. Fletcher AJ, Gardner DS, Edwards CM, early onset of evolving seizure activity during death. Annu Rev Neurosci 1990;13:171–82.
Fowden AL, Giussani DA. Development of the brief repeated asphyxia in near-term fetal sheep. 116. Mishra OP, Delivoria-Papadopoulos M.
ovine fetal cardiovascular defense to hypoxemia PLoS One 2013;8:e73895. Cellular mechanisms of hypoxic injury in the
towards full term. Am J Physiol Heart Circ 100. Westgate JA, Wassink G, Bennet L, developing brain. Brain Res Bull 1999;48:
Physiol 2006;291:H3023–34. Gunn AJ. Spontaneous hypoxia in multiple 233–8.
86. Blood AB, Hunter CJ, Power GG. The role of pregnancies is associated with early fetal 117. Roth SC, Baudin J, Cady E, et al. Relation
adenosine in regulation of cerebral blood flow decompensation and enhanced T-wave eleva- of deranged neonatal cerebral oxidative meta-
during hypoxia in the near-term fetal sheep. tion during brief repeated cord occlusion in near- bolism with neurodevelopmental outcome and
J Physiol 2002;543:1015–23. term fetal sheep. Am J Obstet Gynecol head circumference at 4 years. Dev Med Child
87. Thakor AS, Richter HG, Kane AD, et al. 2005;193:1526–33. Neurol 1997;39:718–25.
Redox modulation of the fetal cardiovascular 101. Fisher DJ. Acidaemia reduces cardiac 118. Jensen A, Hohmann M, Kunzel W. Dy-
defence to hypoxaemia. J Physiol 2010;588: output and left ventricular contractility in namic changes in organ blood flow and oxygen
4235–47. conscious lambs. J Dev Physiol 1986;8:23–31. consumption during acute asphyxia in fetal
88. van Bel F, Sola A, Roman C, Rudolph AM. 102. Mott JC. The ability of young mammals to sheep. J Dev Physiol 1987;9:543–59.
Role of nitric oxide in the regulation of the cere- withstand total oxygen lack. Br Med Bull 119. Gunn AJ, Parer JT, Mallard EC,
bral circulation in the lamb fetus during 1961;17:144–8. Williams CE, Gluckman PD. Cerebral histologic
24 American Journal of Obstetrics & Gynecology JANUARY 2020
Downloaded for FK UMI Makassar (dosenfkumi01@gmail.com) at University of Muslim Indonesia from ClinicalKey.com by Elsevier on April 14, 2020.
For personal use only. No other uses without permission. Copyright ©2020. Elsevier Inc. All rights reserved.
ajog.org Expert Reviews
and electrocorticographic changes after asphyxia with metabolic acidosis in the term factor levels and intrapartum fetal compromise.
asphyxia in fetal sheep. Pediatr Res 1992;31: fetus. Am J Obstet Gynecol 1994;170:1081–7. Placenta 2016;48:63–7.
486–91. 136. Parer JT. Effects of fetal asphyxia on brain 150. Ciobanou A, Jabak S, De Castro H, Frei L,
120. Ikeda T, Murata Y, Quilligan EJ, et al. cell structure and function: limits of tolerance. Akolekar R, Nicolaides K. Biomarkers of
Physiologic and histologic changes in near-term Comp Biochem Physiol A Mol Integr Physiol impaired placentation at 35e37 weeks’ gesta-
fetal lambs exposed to asphyxia by partial um- 1998;119:711–6. tion in the prediction of adverse perinatal
bilical cord occlusion. Am J Obstet Gynecol 137. Low JA, Lindsay BG, Derrick EJ. Threshold outcome. Ultrasound Obstet Gynecol 2019;54:
1998;178:24–32. of metabolic acidosis associated with newborn 79–86.
121. de Haan HH, Van Reempts JL, Vles JS, de complications. Am J Obstet Gynecol 1997;177: 151. Low JA. Intrapartum fetal surveillance. Is it
Haan J, Hasaart TH. Effects of asphyxia on the 1391–4. worthwhile? Obstet Gynecol Clin North Am
fetal lamb brain. Am J Obstet Gynecol 138. Sabdia S, Greer RM, Prior T, Kumar S. 1999;26:725–39.
1993;169:1493–501. Predicting intrapartum fetal compromise using 152. Devane D, Lalor JG, Daly S, McGuire W,
122. Mallard EC, Williams CE, Gunn AJ, the fetal cerebro-umbilical ratio. Placenta Smith V. Cardiotocography versus intermittent
Gunning MI, Gluckman PD. Frequent episodes 2015;36:594–8. auscultation of fetal heart on admission to labour
of brief ischemia sensitize the fetal sheep brain to 139. Morales-Rosello J, Khalil A. Fetal cere- ward for assessment of fetal wellbeing.
neuronal loss and induce striatal injury. Pediatr broplacental ratio and adverse perinatal Cochrane Database Syst Rev 2012;(2):
Res 1993;33:61–5. outcome. J Perinatal Med 2016;44:355. CD005122.
123. Cahill AG, Tuuli MG, Stout MJ, López JD, 140. Bligh LN, Alsolai AA, Greer RM, Kumar S. 153. Grivell RM, Alfirevic Z, Gyte G, Devane D.
Macones GA. A prospective cohort study of fetal Cerebroplacental ratio thresholds measured Antenatal cardiotocography for fetal assess-
heart rate monitoring: deceleration area is pre- within 2 weeks before birth and risk of Cesarean ment. Cochrane Database Syst Rev 2010;1:
dictive of fetal acidemia. Am J Obstet Gynecol section for intrapartum fetal compromise and CD007863.
2018;218:523. e521-523. e512. adverse neonatal outcome. Ultrasound Obstet 154. Ayres-de-Campos D, Bernardes J, Costa-
124. Pulgar VM, Zhang J, Massmann GA, Gynecol 2018;52:340–6. Pereira A, Pereira-Leite L. Inconsistencies in
Figueroa JP. Mild chronic hypoxia modifies the 141. Madden JV, Flatley CJ, Kumar S. Term classification by experts of cardiotocograms and
fetal sheep neural and cardiovascular responses small-for-gestational-age infants from low-risk subsequent clinical decision. BJOG 1999;106:
to repeated umbilical cord occlusion. Brain Res women are at significantly greater risk of 1307–10.
2007;1176:18–26. adverse neonatal outcomes. Am J Obstet 155. Alfirevic Z, Devane D, Gyte GML. Contin-
125. Hawkins P, Steyn C, McGarrigle HH, et al. Gynecol 2018;218:525. e521-525. e529. uous cardiotocography (CTG) as a form of
Effect of maternal nutrient restriction in early 142. Bricker L, Medley N, Pratt JJ. Routine ul- electronic fetal monitoring (EFM) for fetal
gestation on responses of the hypothalamic- trasound in late pregnancy (after 24 weeks’ assessment during labour (Review). Cochrane
pituitary-adrenal axis to acute isocapnic hypo- gestation). Cochrane Database Syst Rev Library 2007(4).
xaemia in late gestation fetal sheep. Exp Physiol 2015(6):CD001451. 156. Nelson KB, Dambrosia JM, Ting TY,
2000;85:85–96. 143. Bligh LN, Al Solai A, Greer RM, Kumar S. Grether JK. Uncertain value of electronic fetal
126. Gupta BD, Sharma P, Bagla J, Parakh M, Diagnostic performance of cerebroplacental ra- monitoring in predicting cerebral palsy. N Engl J
Soni JP. Renal failure in asphyxiated neonates. tio thresholds at term for prediction of low Med 1996;334:613–8.
Indian Pediatr 2005;42:928–34. birthweight and adverse intrapartum and 157. ACOG. American College of Obstetri-
127. Perlman JM, Tack ED, Martin T, neonatal outcomes in a term, low-risk popula- cians and Gynecologists Practice Bulletin No.
Shackelford G, Amon E. Acute systemic organ tion. Fetal Diagn Ther 2018;43:191–8. 106: Intrapartum fetal heart rate monitoring:
injury in term infants after asphyxia. Am J Dis 144. DeVore GR. The importance of the cere- nomenclature, interpretation, and general
Child 1989;143:617–20. broplacental ratio in the evaluation of fetal well- management principles. Obstet Gynecol
128. Mohammed LH, Khairy MA, El- being in SGA and AGA fetuses. Am J Obstet 2009;114:192–202.
Hussieny NA, Zaazou MH, Aly RM. Multi-organ Gynecol 2015;213:5–15. 158. NICE. Intrapartum care for healthy women
dysfunction in neonates with hypoxic-ischemic 145. Conde-Agudelo A, Villar J, Kennedy SH, and babies, clinical guideline CG190. 2017.
encephalopathy. Med J Cairo University Papageorghiou AT. Predictive accuracy of cer- 159. RANZCOG. Intrapartum fetal surveillance.
2010;78(2). ebroplacental ratio for adverse perinatal and Available at: https://ranzcog.edu.au/RANZCOG
129. Mathew OP, Jones AS, James E, Bland H, neurodevelopmental outcomes in suspected _SITE/media/RANZCOG-MEDIA/Women%27s
Groshong T. Neonatal renal failure: usefulness of fetal growth restriction: systematic review and %20Health/Statement%20and%20guidelines/
diagnostic indices. Pediatrics 1980;65:57–60. meta-analysis. Ultrasound Obstet Gynecol Clinical-Obstetrics/Intrapartum-Fetal-Surveillance-
130. Ellis EN, Arnold WC. Use of urinary indexes 2018;52:430–41. Guideline-Third-edition-Aug-2014.pdf?ext=.pdf.
in renal failure in the newborn. Am J Dis Child 146. Prior T, Paramasivam G, Bennett P, Accessed August 30, 2019.
1982;136:615–7. Kumar S. Are fetuses that fail to achieve their 160. Byford S, Weaver E, Anstey C. Has the
131. Martin-Ancel A, Garcia-Alix A, Gaya F, growth potential at increased risk of intrapartum incidence of hypoxic ischaemic encephalopathy
Cabanas F, Burgueros M, Quero J. Multiple or- compromise? Ultrasound Obstet Gynecol in Queensland been reduced with improved
gan involvement in perinatal asphyxia. J Pediatr 2015;46:460–4. education in fetal surveillance monitoring? Aust
1995;127:786–93. 147. Kumar S, Figueras F, Ganzevoort W, N Z J Obstet Gynaecol 2014;54:348–53.
132. Massaro D, Massaro GD. Invited review: Turner J, McCowan L. Using cerebroplacental 161. Nunes I, Ayres-de-Campos D,
pulmonary alveoli: formation, the “call for oxy- ratio in non-SGA infants to predict adverse Ugwumadu A, et al. Central fetal monitoring with
gen,” and other regulators. Am J Physiol Lung perinatal outcome: caution is required. Ultra- and without computer analysis: a randomized
Cell Mol Physiol 2002;282:L345–58. sound Obstet Gynecol 2018;52:427–9. controlled trial. Obstet Gynecol 2017;129:
133. Davis RP, Mychaliska GB. Neonatal pul- 148. Sherrell H, Dunn L, Clifton V, Kumar S. 83–90.
monary physiology. Paper presented at: Semi- Systematic review of maternal Placental Growth 162. Brocklehurst P, Field D, Greene K, et al.
nars in pediatric surgery 2013. Factor levels in late pregnancy as a predictor of Computerised interpretation of fetal heart rate
134. Vogel ER, Britt RD Jr, Trinidad MC, et al. adverse intrapartum and perinatal outcomes. during labour (INFANT): a randomised
Perinatal oxygen in the developing lung. Can J Eur J Obstet Gynecol Reprod Biol 2018;225: controlled trial. Lancet 2017;389:1719–29.
Physiol Pharmacol 2014;93:119–27. 26–34. 163. Hokegard KH, Eriksson BO, Kjellmer I,
135. Low JA, Panagiotopoulos C, Derrick EJ. 149. Bligh LN, Greer RM, Kumar S. The rela- Magno R, Rosen KG. Myocardial metabolism
Newborn complications after intrapartum tionship between maternal placental growth in relation to electrocardiographic changes
JANUARY 2020 American Journal of Obstetrics & Gynecology 25
Downloaded for FK UMI Makassar (dosenfkumi01@gmail.com) at University of Muslim Indonesia from ClinicalKey.com by Elsevier on April 14, 2020.
For personal use only. No other uses without permission. Copyright ©2020. Elsevier Inc. All rights reserved.
Expert Reviews ajog.org
and cardiac function during graded hypoxia in 166. Landman AJ, Immink-Duijker ST, 168. Garite TJ, Dildy GA, McNamara H, et al.
the fetal lamb. Acta Physiol Scand 1981;113: Mulder EJ, Koster MP, Xodo S, Visser GH, A multicenter controlled trial of fetal pulse oxim-
1–7. Groenendaal F, Kwee A. Significant reduction etry in the intrapartum management of non-
164. Belfort MA, Saade GR, Thom E, et al. in umbilical artery metabolic acidosis after reassuring fetal heart rate patterns. Am J Obstet
A randomized trial of intrapartum fetal ECG ST- implementation of intrapartum ST waveform Gynecol 2000;183:1049–58.
segment analysis. N Engl J Med 2015;373: analysis of the fetal electrocardiogram. 169. Bloom SL, Spong CY, Thom E, et al. Fetal
632–41. American journal of obstetrics and gynecology pulse oximetry and cesarean delivery. N Engl J
165. Westgate JA, Bennet L, Brabyn C, 2019 Feb 28. Med 2006;355:2195–202.
Williams CE, Gunn AJ. ST waveform changes 167. Food and Drug Administration. Summary 170. East CE, Begg L, Colditz PB, Lau R. Fetal
during repeated umbilical cord occlusions in minutes: meeting of the Obstetrics and Gyne- pulse oximetry for fetal assessment in labour.
near-term fetal sheep. Am J Obstet Gynecol cology Devices Advisory Panel, open session, Cochrane Database Syst Rev 2014(10):
2001;184:743–51. June 9, 2003. In: 2003. CD004075.
26 American Journal of Obstetrics & Gynecology JANUARY 2020
Downloaded for FK UMI Makassar (dosenfkumi01@gmail.com) at University of Muslim Indonesia from ClinicalKey.com by Elsevier on April 14, 2020.
For personal use only. No other uses without permission. Copyright ©2020. Elsevier Inc. All rights reserved.
You might also like
- Castor Oil Packs For Abdominal Adhesions ScarringDocument10 pagesCastor Oil Packs For Abdominal Adhesions ScarringWandarh Rh100% (1)
- 1 s2.0 S2589933323003452 MainDocument10 pages1 s2.0 S2589933323003452 MainimedamNo ratings yet
- Antenatal Care Lesson PlanDocument17 pagesAntenatal Care Lesson PlanAnuradha Maurya80% (15)
- 2015 Wongs Nursing Care of Infants and Children 10 Ed Test BankDocument16 pages2015 Wongs Nursing Care of Infants and Children 10 Ed Test Bankpeggymccallxnpsogirke100% (34)
- The Physiology of Intrapartum Fetal Compromise at Term: Sailesh. Kumar@mater - Uq.edu - AuDocument10 pagesThe Physiology of Intrapartum Fetal Compromise at Term: Sailesh. Kumar@mater - Uq.edu - AuseopyNo ratings yet
- Best Practice & Research Clinical Obstetrics and GynaecologyDocument6 pagesBest Practice & Research Clinical Obstetrics and GynaecologyElena ZepedaNo ratings yet
- Pathophysiological Interpretation of Fetal Heart Rate Tracings in Clinical Practice AJOGDocument23 pagesPathophysiological Interpretation of Fetal Heart Rate Tracings in Clinical Practice AJOGMitsury Jacqueline Flores C.No ratings yet
- Asfixia PerinatalDocument6 pagesAsfixia PerinatalClaudia LópezNo ratings yet
- Endometrial Decidualization: The Primary Driver of Pregnancy HealthDocument20 pagesEndometrial Decidualization: The Primary Driver of Pregnancy HealthSherilinne Quiles LópezNo ratings yet
- Etiology, Clinical Manifestations, and Prediction of Placental AbruptionDocument9 pagesEtiology, Clinical Manifestations, and Prediction of Placental AbruptionKadije OanaNo ratings yet
- Ijms 24 14541Document18 pagesIjms 24 14541Jadilson BorgesNo ratings yet
- AbruptionDocument13 pagesAbruptionAnghelo Aldair Velásquez CarrilloNo ratings yet
- 89 JNMS.2022 89-312Document6 pages89 JNMS.2022 89-312yaritzaalviarezNo ratings yet
- Disproporsi Kepala PanggulDocument14 pagesDisproporsi Kepala PanggulIntan PermataNo ratings yet
- Etiology of Preeclampsia: An UpdateDocument9 pagesEtiology of Preeclampsia: An UpdateSares DaselvaNo ratings yet
- The Placenta: Transcriptional, Epigenetic, and Physiological Integration During DevelopmentDocument10 pagesThe Placenta: Transcriptional, Epigenetic, and Physiological Integration During Developmentpam!!!!No ratings yet
- Acta Obstet Gynecol Scand - 2011 - TIKKANENDocument9 pagesActa Obstet Gynecol Scand - 2011 - TIKKANENsawsanNo ratings yet
- 10 1016@j Ajog 2019 07 010 PDFDocument13 pages10 1016@j Ajog 2019 07 010 PDFDaniel GamarraNo ratings yet
- PIIS000293782200535XDocument17 pagesPIIS000293782200535XnataliaNo ratings yet
- Seminars in Pediatric Surgery: Progress in Anesthesia and Management of The Newborn Surgical PatientDocument5 pagesSeminars in Pediatric Surgery: Progress in Anesthesia and Management of The Newborn Surgical PatientAsif KhanNo ratings yet
- Placenta As Witness 07Document15 pagesPlacenta As Witness 07Vetési OrsolyaNo ratings yet
- Gynec and Obs. Topic Fetal DistressDocument45 pagesGynec and Obs. Topic Fetal DistressRajdeep ParmarNo ratings yet
- AbruptionDocument13 pagesAbruptionMauricio Lopez MejiaNo ratings yet
- Joacp 32 153Document7 pagesJoacp 32 153thresh mainNo ratings yet
- Etiology of Preeclampsia: An UpdateDocument9 pagesEtiology of Preeclampsia: An UpdateRadi PdNo ratings yet
- Eclampsia in The 21st Century: Definition and IncidenceDocument17 pagesEclampsia in The 21st Century: Definition and IncidenceKarilNo ratings yet
- Immunology of PreeclampsiaDocument13 pagesImmunology of PreeclampsiaRohmantuah_Tra_1826No ratings yet
- PIIS0002937820311285Document17 pagesPIIS0002937820311285Jose Francisco Zamora ScottNo ratings yet
- Neonatal Hipoxic IsquemicDocument21 pagesNeonatal Hipoxic IsquemicMariela Nadir Guerreros De VelasquezNo ratings yet
- PlacentaDocument17 pagesPlacentarizka auliaNo ratings yet
- Immunology of EclampsiaDocument10 pagesImmunology of EclampsiaTiara AnggianisaNo ratings yet
- Askep Thypoid FixDocument16 pagesAskep Thypoid FixnilamsaryNo ratings yet
- Jurnal Abrupsio PlasentaDocument13 pagesJurnal Abrupsio Plasentaperussi pranadiptaNo ratings yet
- AmoniakDocument28 pagesAmoniakSulis SipinNo ratings yet
- Romero PDFDocument14 pagesRomero PDFEvertPangkahilaNo ratings yet
- Vaccine: CommentaryDocument11 pagesVaccine: CommentaryCHANNo ratings yet
- Fetal and Neonatal Gene Therapy: Benefits and Pitfalls: ReviewDocument6 pagesFetal and Neonatal Gene Therapy: Benefits and Pitfalls: Reviewbhoopendra chauhanNo ratings yet
- Ijms 22 08622Document24 pagesIjms 22 08622nur aini hidayatinNo ratings yet
- 1471 2393 14 80 PDFDocument5 pages1471 2393 14 80 PDFPaula PebriantyNo ratings yet
- Early Development of The Human Placenta and Pregnancy ComplicationsDocument9 pagesEarly Development of The Human Placenta and Pregnancy ComplicationsSherilinne Quiles LópezNo ratings yet
- Preeclampsia Fisiopatologia 2019Document8 pagesPreeclampsia Fisiopatologia 2019Carlos MirandaNo ratings yet
- MC Allister JPPathophysiologyofcongenitalandneonatalhydrocephalus Sem Fetal Neonat Med 2012Document11 pagesMC Allister JPPathophysiologyofcongenitalandneonatalhydrocephalus Sem Fetal Neonat Med 2012nendaayuwandariNo ratings yet
- Lung MaturityDocument7 pagesLung MaturityAlce Alce EverdienNo ratings yet
- Abruption Associated PrematurityDocument19 pagesAbruption Associated PrematurityFitriyana WinarnoNo ratings yet
- Gestational and Placental DisordersDocument32 pagesGestational and Placental DisordersMcRo UndiNo ratings yet
- Guideline HipertensiDocument7 pagesGuideline HipertensiAgus RiyantoNo ratings yet
- Fetal Surgery Spina BifidaDocument12 pagesFetal Surgery Spina BifidaAvicenna Shafhan ArfiNo ratings yet
- Fetal Asphyxia: S ArulkumaranDocument14 pagesFetal Asphyxia: S ArulkumaranAndrea JIMENEZNo ratings yet
- Estabilizacion de PotrillosDocument6 pagesEstabilizacion de PotrillosCarlos Pedro VillaNo ratings yet
- Abnormal LabourDocument21 pagesAbnormal LabourbetablockersNo ratings yet
- Antioxidant Therapy To Prevent PreeclampsiaDocument8 pagesAntioxidant Therapy To Prevent PreeclampsiaTantonio Tri PutraNo ratings yet
- Cerebral PalsyDocument13 pagesCerebral PalsyNAMA DEPAN NAMA BELAKANGNo ratings yet
- Non-Immune Hydrops Fetalis: Murat YurdakökDocument12 pagesNon-Immune Hydrops Fetalis: Murat YurdakökagitaNo ratings yet
- Artigo 1 PDFDocument9 pagesArtigo 1 PDFLarissa F SNo ratings yet
- 10 1016@j Ogrm 2020 03 006 PDFDocument6 pages10 1016@j Ogrm 2020 03 006 PDFAdriani HartantoNo ratings yet
- Introduction of The Physiological CTG Interpretation & Hypoxia in Labour (HIL) Tool, and Its Incorporation Into A Software Programme: Impact On Perinatal OutcomesDocument8 pagesIntroduction of The Physiological CTG Interpretation & Hypoxia in Labour (HIL) Tool, and Its Incorporation Into A Software Programme: Impact On Perinatal OutcomesMeitsi TeittinenNo ratings yet
- A New Pathophysiological Concept and New Classification of Pre-EclampsiaDocument12 pagesA New Pathophysiological Concept and New Classification of Pre-EclampsiaIstigfarani InNo ratings yet
- 1 s2.0 S0031395503002153 MainDocument21 pages1 s2.0 S0031395503002153 Maindiego bustosNo ratings yet
- Ihsan Ullah ppt05Document44 pagesIhsan Ullah ppt05Ihsan Ullah KhanNo ratings yet
- Congenital Diaphragmatic Hernia: Pathogenesis, Prenatal Diagnosis and Management - Literature ReviewDocument7 pagesCongenital Diaphragmatic Hernia: Pathogenesis, Prenatal Diagnosis and Management - Literature ReviewPritariantiNo ratings yet
- The Placenta and Neurodisability 2nd EditionFrom EverandThe Placenta and Neurodisability 2nd EditionIan CrockerNo ratings yet
- Assessment of The BreastDocument11 pagesAssessment of The BreastSIR ONENo ratings yet
- Assessment of The Postpartum PatientDocument4 pagesAssessment of The Postpartum PatientJanice SnellNo ratings yet
- Anesthesia For Pituitary Lesions: Rialph Engel D. GuiaDocument57 pagesAnesthesia For Pituitary Lesions: Rialph Engel D. GuiaDoc SabNo ratings yet
- IHIMS Indicators BookletDocument36 pagesIHIMS Indicators BookletPurbhuta Bhc health centreNo ratings yet
- Animal CloningDocument13 pagesAnimal Cloningdebanjana2009No ratings yet
- RH Incompatibility New For MDDocument65 pagesRH Incompatibility New For MDMd AtifNo ratings yet
- Factors Contributing To Perineal Tears Among Mothers During LabourDelivery in Kibuku Health Centre IV Kibuku DistrictDocument11 pagesFactors Contributing To Perineal Tears Among Mothers During LabourDelivery in Kibuku Health Centre IV Kibuku DistrictKIU PUBLICATION AND EXTENSIONNo ratings yet
- Impact of A Breastfeeding-Friendly Workplace On An Employed Mother's Intention To Continue Breastfeeding After Returning To WorkDocument7 pagesImpact of A Breastfeeding-Friendly Workplace On An Employed Mother's Intention To Continue Breastfeeding After Returning To WorkMary Rose Estabaya PantojaNo ratings yet
- IV Iron Infusion Vs Oral Iron For Postpartum HemorrhageDocument10 pagesIV Iron Infusion Vs Oral Iron For Postpartum Hemorrhagesunshine bloomNo ratings yet
- Doh ProgramsDocument250 pagesDoh ProgramsEricNo ratings yet
- Practice Guidelines For Obstetric AnesthesiaDocument31 pagesPractice Guidelines For Obstetric AnesthesiaRocio Ayaque AguirreNo ratings yet
- 11.4 Sexual Reproduction: Essential Idea: Sexual Reproduction Involves The Development and Fusion of Haploid GametesDocument34 pages11.4 Sexual Reproduction: Essential Idea: Sexual Reproduction Involves The Development and Fusion of Haploid GametesTshegofatso100% (1)
- Star PackageDocument24 pagesStar PackagePrsdeepNo ratings yet
- CasesDocument37 pagesCasesZakaria FarahNo ratings yet
- Empowering Growing Families With Affordable Fertility TreatmentsDocument9 pagesEmpowering Growing Families With Affordable Fertility TreatmentsOma FertilityNo ratings yet
- Latihan Soal Koding Semester 4Document3 pagesLatihan Soal Koding Semester 4kamilaNo ratings yet
- Lesson 2 Developing The Whole PersonDocument42 pagesLesson 2 Developing The Whole Personthejuluistv llantoNo ratings yet
- SWOT Analysis of The RH LawDocument1 pageSWOT Analysis of The RH LawAsirante LumenNo ratings yet
- Post Cesarean Care For Mothers Attending Arua Regional Referral Hospital Drivers and ChallengesDocument16 pagesPost Cesarean Care For Mothers Attending Arua Regional Referral Hospital Drivers and ChallengesKIU PUBLICATION AND EXTENSIONNo ratings yet
- Garbha & Garbha Sambhava SaamagriDocument12 pagesGarbha & Garbha Sambhava SaamagriManojNo ratings yet
- Prevention of Spontaneous Preterm BirthDocument29 pagesPrevention of Spontaneous Preterm BirthPaola Riveros GilNo ratings yet
- Nutrition in PregnancyDocument5 pagesNutrition in PregnancyCatalin SimionNo ratings yet
- Association of Clinical Features With Obesity and Gonadotropin Levels in Women With Polycystic Ovarian SyndromeDocument4 pagesAssociation of Clinical Features With Obesity and Gonadotropin Levels in Women With Polycystic Ovarian Syndromedoctor wajihaNo ratings yet
- Premarin Drug StudyDocument8 pagesPremarin Drug StudyjanNo ratings yet
- Camel Semen Collection Viscosity and CryopreservatDocument5 pagesCamel Semen Collection Viscosity and Cryopreservatlongjc2690No ratings yet
- Why Not Games - Surial - Bear Folk of The NorthDocument36 pagesWhy Not Games - Surial - Bear Folk of The NorthYiğit ÜnsayNo ratings yet
- Pu500c71230664932610 RLSDocument2 pagesPu500c71230664932610 RLSAbdul MalikNo ratings yet