Professional Documents
Culture Documents
Korean COMPASS-31 PD and MSA
Korean COMPASS-31 PD and MSA
Uploaded by
Margareth HildariaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Korean COMPASS-31 PD and MSA
Korean COMPASS-31 PD and MSA
Uploaded by
Margareth HildariaCopyright:
Available Formats
RESEARCH ARTICLE
The composite autonomic symptom scale 31
is a useful screening tool for patients with
Parkinsonism
Younsoo Kim1☯, Jin Myoung Seok2☯, Jongkyu Park3, Kun-Hyun Kim4,5, Ju-Hong Min4,5,
Jin Whan Cho4,5, Suyeon Park6, Hyun-jin Kim4, Byoung Joon Kim4,5*, Jinyoung Youn4,5*
1 Department of Neurology, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine,
Changwon, Korea, 2 Department of Neurology, Soonchunhyang University Cheonan Hospital,
Soonchunhyang University College of Medicine, Cheonan, Korea, 3 Department of Neurology,
Soonchunhyang University, Gumi, Korea, 4 Department of Neurology, Samsung Medical Center,
a1111111111 Sungkyunkwan University School of Medicine, Seoul, Korea, 5 Neuroscience Center, Samsung Medical
Center, Seoul, Korea, 6 Department of Biostatistics, Soonchunhyang University Seoul Hospital,
a1111111111
Soonchunhyang University College of Medicine, Seoul, Korea
a1111111111
a1111111111 ☯ These authors contributed equally to this work.
a1111111111 * genian@skku.edu (JY); bjkim@skku.edu (BK)
Abstract
OPEN ACCESS
Differentiation of multiple system atrophy with predominant parkinsonism (MSA-P) and
Citation: Kim Y, Seok JM, Park J, Kim K-H, Min J- Parkinson’s disease (PD) is important, but an effective tool for differentiation has not been
H, Cho JW, et al. (2017) The composite autonomic
identified. We investigated the efficacy of the composite autonomic symptom scale 31
symptom scale 31 is a useful screening tool for
patients with Parkinsonism. PLoS ONE 12(7): (COMPASS 31) questionnaire as a tool for evaluating autonomic function in parkinsonism
e0180744. https://doi.org/10.1371/journal. patients. In this study, we enrolled drug-naïve patients with MSA-P and PD, and adminis-
pone.0180744
tered the COMPASS-31 and an objective autonomic dysfunction test (AFT). Demographic
Editor: Pedro Gonzalez-Alegre, University of and clinical data, including parkinsonism and autonomic dysfunction, were compared
Pennsylvania Perelman School of Medicine,
between the two groups. Additionally, we determined the optimal COMPASS 31 cut-off
UNITED STATES
score to differentiate MSA-P from PD for use as a screening tool. In this study, 27 MSA-P
Received: February 25, 2017
patients and 41 PD patients were recruited. The total COMPASS 31 score was well corre-
Accepted: June 20, 2017 lated with the objective AFT results. When we compared the COMPASS 31 score between
Published: July 6, 2017 the two groups, MSA-P patients showed higher total scores and sub-scores in the ortho-
static intolerance, gastrointestinal, and bladder domains compared with PD patients. Simi-
Copyright: © 2017 Kim et al. This is an open
access article distributed under the terms of the larly, MSA-P patients had more abnormalities in expiration to inspiration ratio, Valsalva ratio
Creative Commons Attribution License, which and pressure recovery time than PD patients in objective AFT. With 13.25 as the cut-off
permits unrestricted use, distribution, and
score for diagnosis of MSA-P, the total COMPASS-31 score demonstrated high sensitivity
reproduction in any medium, provided the original
author and source are credited. (92.6%) and moderate specificity (51.2%) with an area under the curve of 0.765. Based on
our results, the COMPASS 31 is an effective tool for evaluation of autonomic function in
Data Availability Statement: All relevant data are
within the paper and its Supporting Information patients with parkinsonism. The COMPASS-31 could be used as a sensitive and convenient
files. screening tool, especially for the differentiation between MSA-P and PD.
Funding: This study did not receive any specific
grant from funding agencies in the public,
commercial, or not-for-profit sectors.
Competing interests: The authors have declared
that no competing interests exist.
PLOS ONE | https://doi.org/10.1371/journal.pone.0180744 July 6, 2017 1 / 10
COMPASS 31 for differentiation of MSA and PD
Introduction
Multiple system atrophy with predominant parkinsonism (MSA-P) and Parkinson’s disease
(PD) are different in terms of disease progression and survival. Nevertheless, because MSA-P
and PD share similar motor symptoms, differential diagnosis at an early stage is difficult.
Although autonomic dysfunction is a characteristic symptom of MSA [1], autonomic function
is also commonly involved in PD even from an early stage [2, 3]. Therefore, precise evaluation
of autonomic dysfunction is important for diagnosis in patients with parkinsonism. Previous
studies have used an objective autonomic function test (AFT) for differentiation of MSA-P in
patients with parkinsonism, but optimal evaluation of autonomic dysfunction in patients with
parkinsonism is still controversial [4–8]. Additionally, questionnaires on autonomic dysfunc-
tion could easily be assessed in the clinic, but only a few studies have investigated the clinical
implications of these scales in patients with parkinsonism [7, 8].
The composite autonomic symptom scale 31 (COMPASS 31) questionnaire is a self-rating
questionnaire evaluating six domains of autonomic function: orthostatic intolerance, vasomo-
tor, secretomotor, gastrointestinal, bladder, and pupillomotor domains [9]. The COMPASS 31
has already been reported as a useful tool for the evaluation of autonomic dysfunction in vari-
ous neurologic diseases such as multiple sclerosis, polyneuropathy, and fibromyalgia [10–12].
However, only one previous study has used the COMPASS 31 in MSA and PD patients [7].
This study did not divide MSA patients into predominant subtypes or use the COMPASS 31
for the differential diagnosis of MSA.
In addition, previous studies enrolled PD and MSA-P patients irrespective of dopami-
nergic medications, thus failing to eliminate the possible confounding effects of such [4–8].
Because dopaminergic medications have various effects on both parkinsonism and auto-
nomic symptoms in patients with parkinsonism [13], the confounding effects due to medi-
cations should be minimized when comparing clinical features between patients with MSA-
P and PD.
In this study, we investigated the diagnostic significance of the COMPASS 31 score in
patients with parkinsonism by comparing the total score and domain scores between drug-
naïve patients with MSA-P and PD, and determining the correlation between COMPASS 31
score and AFT results.
Methods
Subjects
This study was approved by the Institutional Review Board of Samsung Medical Center, Seoul,
Korea and all enrolled subjects provided written informed consent. We recruited drug-naïve
patients with PD and probable MSA-P from January 2015 to October 2015 from the move-
ment disorders clinic at Samsung Medical Center. PD was diagnosed based on the UK Brain
Bank Criteria for PD [14], and 18F-FP-CIT positron emission tomography (PET). Probable
MSA-P was determined based on the Second Consensus diagnostic criteria for MSA [1]. Sub-
jects with structural brain lesions, other known neurodegenerative diseases, cognitive
impairment (mini-mental status examination score of < 26 or fulfillment of DSM-IV criteria
for dementia), psychiatric disorders requiring medication, malignancy, or musculo-skeletal
problems mimicking parkinsonism were excluded. In addition, we also excluded subjects with
medical conditions which could affect AFT results including diabetes mellitus or cardiac
arrhythmia. Demographic and clinical data were collected for all patients. Motor symptoms
were evaluated with the Unified Parkinson’s Disease Rating Scale (UPDRS) part 3 and by
Hoehn and Yahr stage [15].
PLOS ONE | https://doi.org/10.1371/journal.pone.0180744 July 6, 2017 2 / 10
COMPASS 31 for differentiation of MSA and PD
Autonomic symptom questionnaire
All enrolled subjects received the COMPASS 31, which is a questionnaire of autonomic symp-
toms and consists of six domains: orthostatic intolerance, vasomotor, secretomotor, gastroin-
testinal, bladder and pupillomotor [9]. The six domain scores sum to a total COMPASS 31
score of 0 to 100, and a higher COMPASS 31 score indicates more severe autonomic
symptoms.
Autonomic function test
All enrolled subjects discontinued medications that could affect the AFT results at least 24
hours before the AFT, and refrained from drinking coffee or tea and smoking on the day of
the test. Both MSA-P and PD patients underwent our standardized autonomic test battery
which included heart rate response to deep breathing (HRDB), the Valsalva maneuver, blood
pressure and heart rate response to head-up tilt test (HUT), and sympathetic skin response
(SSR). Continuous BP monitoring using the Finometer1 (FMS, Amsterdam, the Nether-
lands), and ECG and respiratory movements were obtained during the HRDB test, Valsalva
maneuver, and HUT.
The HRDB test was performed with the patient in a supine position. Patients were asked to
breathe deeply by repeatedly inhaling for 5 seconds and exhaling for 5 seconds for 1 minute at
a rate of 6 breaths per minute. The difference in heart rate between the end of expiration, end
of inspiration and the expiration to inspiration ratio (E:I ratio) were calculated to evaluate car-
diovagal function.
The Valsalva maneuver was performed with the patient in a supine position. The patient
breathed into a mouthpiece connected to a manometer with an expiratory pressure of 40
mmHg for 15 seconds. Pressure recovery time (PRT) and Valsalva ratio were measured for the
assessment of adrenergic and cardiovagal functions, respectively; PRT was defined as the time
interval from the bottom of phase III to the complete return of systolic blood pressure to base-
line during the Valsalva maneuver [16]. The Valsalva ratio was calculated by dividing the max-
imum heart rate by the lowest heart rate during the maneuver [17].
HUT was performed on patients after 30 minutes of resting in a supine position on an elec-
trically driven tilt table. Patients were tilted up to 70 degrees for 10 minutes while their blood
pressure, heart rate, and the presence of any discomfort, chest pain, dyspnea, dizziness, or syn-
cope was monitored. The presence of orthostatic hypotension (OH) was evaluated as an adren-
ergic function parameter, which was defined as a fall of at least 30 mmHg in systolic blood
pressure and/or a 15 mmHg fall in diastolic blood pressure within two to five minutes of HUT
[17].
Sudomotor function was assessed with SSR. SSR was recorded from the palm of the hand
and sole of the foot using a Nicolet Viking IV electromyography machine (Nicolet Biomedical,
Madison, WI, USA) according to a previously reported protocol [18]. The SSR was considered
abnormal if at least one of the two limb responses was absent in five serial stimulation trials
[19].
Statistical analyses
All data were presented as medians and interquartile ranges (IQR). Demographic and clinical
data were compared between groups using the Student t-test or Mann-Whitney U-test for con-
tinuous variables, and Pearson’s χ2 or Fisher’s exact test for categorical variables. To determine
the relationship between COMPASS 31 score and AFT results, we performed Spearman’s cor-
relation analysis. Receiver operating characteristic (ROC) curve analysis was performed to
establish the optimal cut-off value for the differentiation of MSA-P from PD. A p-value < 0.05
PLOS ONE | https://doi.org/10.1371/journal.pone.0180744 July 6, 2017 3 / 10
COMPASS 31 for differentiation of MSA and PD
was considered significant. Statistical analyses were performed with a commercially available
software package (PASW version 18.0; SPSS Inc., Chicago, IL, USA).
Results
Patient groups
We recruited 41 patients with idiopathic PD and 27 patients with probable MSA-P. Demo-
graphic and clinical details of the enrolled subjects are presented in Table 1. There was no dif-
ference between the two groups in demographic data and parkinsonism. Even though MSA-P
patients showed higher Hoehn and Yahr stage comparing with PD patients, there was no sta-
tistical significance.
Correlation between COMPASS 31 and objective AFT scores
To investigate the efficacy of using the COMPASS 31 for evaluation of autonomic dysfunction
in patients with parkinsonism, we performed correlation analyses between COMPASS 31
score and objective AFT results. The total COMPASS 31 score was well-correlated with all
objective AFT results, including the E:I ratio, Valsalva ratio, PRT, SSR and OH (S1 Table and
S1 Fig). Among the sub-scores of the COMPASS 31, the gastrointestinal domain sub-score
was also significantly correlated with all parameters of the objective AFT. Among the objective
AFT results, SSR were significantly correlated with the sub-scores of all domains of the COM-
PASS 31, except for the secretomotor and pupillomotor domains.
Comparison of the COMPASS 31 and objective AFT between MSA-P
and PD patients
MSA-P patients demonstrated more autonomic involvement than PD patients in both COM-
PASS 31 score and objective AFT results (Table 2). In terms of the COMPASS 31, higher total
score and sub-scores for orthostatic intolerance, gastrointestinal, and bladder domains were
seen in MSA-P patients compared with PD patients (Fig 1). Similarly, MSA-P patients showed
more diffuse and severe autonomic dysfunction than PD patients for E:I ratio, Valsalva ratio,
PRT, OH, and SSR among objective AFT parameters.
Sensitivity and specificity of COMPASS 31 for the diagnosis of MSA-P
The sensitivity and specificity of COMPASS 31 total score for discriminating MSA-P from PD
(Fig 2 and S2 Table) were 92.6% (75.7–99.1 for 95% CI) and 51.2% (35.1–67.1 for 95% CI),
respectively. The area under the curve (AUC) was 0.765 (0.654–0.877 for 95% CI) with a cut-
off score of 13.25. In addition, the sub-score for the bladder domain showed a high specificity
Table 1. Demographic and clinical characteristics of enrolled subjects with PD and MSA-P.
PD (n = 41) MSA-P (n = 27) p-value
Male/female, n (%) 20/21 (49/51) 14/13 (52/48) 0.806
Age, years 67.0 (57.0–72.0) 69.0 (66.0–74.0) 0.198
Duration of disease, years 2.2 (1.0–3.5) 2.0 (1.0–3.0) 0.840
UPDRS part 3 score 28.0 (22.0–32.0) 26.0 (19.5–33.0) 0.459
HY stage 1/2/3, n (%) 6/32/3 (14.6/78.0/7.3) 3/16/8 (11.1/59.3/29.6) 0.061
PD, Parkinson’s disease; MSA-P, multiple system atrophy with predominant parkinsonism; UPDRS, unified
Parkinson’s disease rating scale; HY, Hohen and Yahr.
https://doi.org/10.1371/journal.pone.0180744.t001
PLOS ONE | https://doi.org/10.1371/journal.pone.0180744 July 6, 2017 4 / 10
COMPASS 31 for differentiation of MSA and PD
Table 2. Results of the evaluation of autonomic function between PD and MSA-P patients using the COMPASS 31 and objective autonomic func-
tion test.
PD (n = 41) MSA-P (n = 27) p-value
COMPASS 31
total score 12.8 (4.8–27.0) 32.1 (17.5–43.3) <0.001a
orthostatic intolerance 8.0 (0–16.0) 20.0 (4.0–32.0) 0.003a
vasomotor 0 (0–0) 0 (0–0) 0.678
secretomotor 0 (0–3.2) 2.1 (0.0–4.3) 0.175
gastrointestinal 3.6 (0.4–6.3) 6.3 (3.6–8.9) 0.004a
bladder 1.1 (0–1.7) 3.3 (1.1–6.7) <0.001a
pupillomotor 0.3 (0–1.0) 0 (0–1.3) 0.839
Objective autonomic function test
E:I ratio 1.1 (1.0–1.2) 1.1 (1.1–1.1) 0.020a
Valsalva ratio 1.4 (1.2–1.6) 1.3 (1.2–1.4) 0.032
pressure recovery time, s 1.0 (1.0–3.0) 10.0 (3.0–24.0) <0.001a
orthostatic hypotension, n (%) 0 (0) 15 (77.8) <0.001a
abnormality in SSR, n (%) 5 (12.2) 7 (29.6) 0.106
PD, Parkinson’s disease; MSA-P, multiple system atrophy with predominant parkinsonism; COMPASS 31, composite autonomic symptom scale 31
questionnaire; E:I ratio, expiration:inspiration ratio; OH, orthostatic hypotension; SSR, sympathetic skin reflex.
a
p-value < 0.05
https://doi.org/10.1371/journal.pone.0180744.t002
of 90.2% (76.9–97.3 for 95% CI), moderate sensitivity of 66.7% (46.0–83.5 for 95% CI), and an
AUC of 0.789 (0.669–0.909 for 95% CI) with a cut-off score of 3.
Discussion
This is the first study to investigate the COMPASS 31 for differential diagnosis between
MSA-P and PD. Because parkinsonism and autonomic dysfunction are common to both
MSA-P and PD, it is difficult to differentiate one from the other. Therefore, precise evaluation
of autonomic dysfunction is important and helpful. In this study, COMPASS 31 scores were
well-correlated with objective AFT results in patients with parkinsonism. Furthermore, there
was a significant difference in COMPASS 31 score between MSA-P and PD patients, and
COMPASS 31 total score showed high sensitivity for the diagnosis of MSA-P. Based on these
results, the COMPASS 31 could be a convenient and useful tool for screening MSA-P in
patients with parkinsonism even from an early stage.
Classically, the objective AFT was regarded as the main tool for diagnosing autonomic dys-
function, but an expensive immovable device and a trained operator are required for this eval-
uation. Moreover, there is still controversy on the efficacy of using the objective AFT to
differentiate between MSA and PD [4–8]. However, autonomic function can be easily assessed
in practice with a self-rated questionnaire. The COMPASS-31 has already been reported in
previous studies as a useful diagnostic tool for various neurologic diseases [10–12]. In this
study, we demonstrated that COMPASS 31 scores were well-correlated with objective AFT
results in patients with parkinsonism. Especially, total COMPASS 31 score and the sub-scores
for orthostatic intolerance, and gastrointestinal function were significantly correlated with E:I
ratio, Valsalva ratio, PRT, OH, and SSR, which had significantly more involvement in MSA-P
patients compared with PD patients, except SSR. Therefore, we suggest that the COMPASS 31
could be a useful tool to evaluate autonomic dysfunction in patients with parkinsonism.
PLOS ONE | https://doi.org/10.1371/journal.pone.0180744 July 6, 2017 5 / 10
COMPASS 31 for differentiation of MSA and PD
Fig 1. Comparison of COMPASS 31 scores among the patients with PD and MSA-P. The MSA-P patient group had
higher total COMPASS 31 scores and higher sub-scores in the orthostatic intolerance, gastrointestinal, and bladder
domains compared with PD patients. The error bars represent the standard error of mean. COMPASS 31, composite
autonomic symptom scale 31 questionnaire; PD, Parkinson’s disease; MSA-P, multiple system atrophy with predominant
parkinsonism. *p-value < 0.05.
https://doi.org/10.1371/journal.pone.0180744.g001
When we compared autonomic dysfunction between MSA-P and PD patients using the
COMPASS 31, MSA-P patients showed a higher total COMPASS 31 score than patients with
PD. Similarly, previous studies also revealed more severe autonomic involvements in MSA-P
compared to PD patients [5, 7, 8]. Particularly, MSA-P patients demonstrated higher scores
for orthostatic intolerance, gastrointestinal and bladder function than PD patients. In terms of
the objective AFT, more severe abnormalities in E:I ratio, Valsalva ratio, PRT, and OH were
seen in MSA-P compared with PD patients. In particular, PRT was much longer in MSA-P
patients compared with PD patients, and more than 3/4 of subjects with MSA-P showed OH
in response to HUT, while no PD patients showed OH. Based on these results, both the COM-
PASS 31 and objective AFT showed noticeable cardiovascular involvement in MSA-P
PLOS ONE | https://doi.org/10.1371/journal.pone.0180744 July 6, 2017 6 / 10
COMPASS 31 for differentiation of MSA and PD
Fig 2. ROC curve for COMPASS 31 total score diagnostic performance. With 13.25 as the cut-off score
for differential diagnosis of MSA-P from PD, the total COMPASS 31 score demonstrated high sensitivity
(92.6%) and moderate specificity (51.2%) with an area under the curve of 0.765. ROC, receiver operating
characteristic; COMPASS 31, composite autonomic symptom scale 31 questionnaire; MSA-P, multiple
system atrophy with predominant parkinsonism; PD, Parkinson’s disease.
https://doi.org/10.1371/journal.pone.0180744.g002
compared with PD patients. Although a previous study reported cardiovascular autonomic
dysfunction in the early stages of PD [2], MSA-P patients have been shown to have more car-
diovascular dysfunction than PD patients, which is similar to our results [4]. In addition, sub-
jects with MSA-P showed more gastrointestinal and bladder symptoms based on COMPASS
31 scores compared to patients with PD. Considering that the objective AFT is not a proper
tool for evaluating gastrointestinal and bladder function [20], the COMPASS 31 could cover
an even wider-spectrum of autonomic dysfunction, and thus could be more helpful for precise
evaluation of dysautonomia in patients with parkinsonism.
When we examined the sensitivity and specificity of the COMPASS 31 for the differentia-
tion of MSA-P from PD, COMPASS 31 total score showed high sensitivity but moderate
specificity. A previous study using a scoring system based on the objective AFT reported a sen-
sitivity of 89% and specificity of 70% [5], and another study using a battery of cardiovascular
autonomic tests showed a sensitivity of 91% and specificity of 94% [4]. Therefore, compared
with previous studies [4, 5], we suggest that the total COMPASS 31 score can be used as
PLOS ONE | https://doi.org/10.1371/journal.pone.0180744 July 6, 2017 7 / 10
COMPASS 31 for differentiation of MSA and PD
screening tool for MSA-P in patients with parkinsonism based on the high sensitivity shown
in our results.
Despite high sensitivity, the COMPASS 31 demonstrated moderate specificity. Relatively
low specificity could result from the recruitment of early, drug-naïve patients in this study, ir
from the limitation of COMPASS 31. Considering it is difficult to distinguish PD from
MSA-P, especially in early stage, we aimed to investigate the clinical implications of COM-
PASS 31 for differentiation in patients with early stage. Additionally, to overcome the possible
limitation of COMPASS 31, we need instruments/biomarkers with high specificity. In previous
studies, the objective AFT showed relatively high specificity compared with our results [4, 5],
and the objective AFT could compensate the limitation of COMPASS 31. Moreover, the blad-
der domain sub-score had high specificity (90.2%) in our study (S2 Table), thus the sub-score
of this domain could be also used to overcome the low specificity of COMPASS 31, when
using total COMPASS 31 score.
MSA is usually divided into two subtypes based on the predominant symptoms: parkinson-
ism (MSA-P) and cerebellar ataxia (MSA-C). Unlike previous studies [6, 7], we only enrolled
patients with PD and MSA-P and did not enroll patients with MSA-C because it is difficult to
differentiate MSA-P, but not MSA-C, from PD in the early stages. Additionally, when compar-
ing autonomic dysfunction between MSA and PD patients, it is important to minimize possi-
ble confounding factors. Considering that the autonomic nervous system is usually more
involved in disease progression, we enrolled MSA-P and PD patients with similar disease
severity. However, because the main symptom of MSA-C is ataxia, not parkinsonism, it is diffi-
cult to match the disease severity of MSA-C and PD. Furthermore, we recruited drug-naïve
MSA-P and PD patients in our study to minimize other possible confounding factors due to
dopaminergic medications.
This study has some limitations. First, our sample size was relatively small. However, even
with a small sample size, we found that the COMPASS 31 was a useful tool for evaluating auto-
nomic function in patients with parkinsonism and could be used as a screening tool for
MSA-P. Additionally, we enrolled drug-naïve, early stage subjects with MSA-P and PD. Con-
sidering clinical diagnosis could be changed with follow up, there is a possibility for changed
diagnosis. However, all the PD patients in our study showed excellent response to dopaminer-
gic medication and were also confirmed with dopamine transporter PET. Another limitation
is that our study was cross-sectional. Since autonomic involvement could be more prominent
with disease progression, it is important to investigate further with longitudinal follow-up
studies. In this study, we focused on the utility of the COMPASS 31 in patients with parkinson-
ism since the differential diagnosis between MSA-P and PD is usually difficult in the early
stages of these diseases. Moreover, we recruited drug-naïve MSA-P and PD patients so we
could eliminate possible confounds due to medications or disease severity. Lastly, we did not
enroll normal controls. In this study, our primary objective was to determine the efficacy of
the COMPASS 31 in patients with parkinsonism, thus we enrolled patients with MSA-P and
PD, two of the most common and dominant diseases in parkinsonism.
In conclusion, the COMPASS 31 was a convenient and effective tool for the evaluation of auto-
nomic function in patients with parkinsonism along with the objective AFT. Furthermore, consid-
ering that the total COMPASS 31 score showed high sensitivity for differentiating between MSA-P
and PD, this questionnaire could be a helpful tool for screening MSA-P from parkinsonism.
Supporting information
S1 Fig. Correlations between the total COMPASS 31 score and objective autonomic func-
tion test results in all enrolled subjects. Spearman correlation analysis was performed to
PLOS ONE | https://doi.org/10.1371/journal.pone.0180744 July 6, 2017 8 / 10
COMPASS 31 for differentiation of MSA and PD
determine the relationship between the total COMPASS 31 score (y-axis) and E:I ratio, Val-
salva ratio, and pressure recovery time (x-axis). The total COMPASS 31 score showed negative
correlations with the E:I ratio (A) and Valsalva ratio (B). A significant positive correlation was
observed between the total COMPASS 31 score and pressure recovery time (C).
(TIF)
S1 Table. Correlation analysis between COMPASS 31 scores and objective autonomic
function test results. E:I ratio, expiration:inspiration ratio; PRT, pressure recovery time; OH,
orthostatic hypotension; SSR, sympathetic skin reflex. p-values below 0.029 are considered sig-
nificant and marked with an asterisk based on Bonferroni corrections.
(DOCX)
S2 Table. Discriminant analysis results using the COMPASS 31 score for differential diag-
nosis of MSA-P from PD. COMPASS 31, composite autonomic symptom scale 31 question-
naire; MSA-P, multiple system atrophy with predominant parkinsonism; PD, Parkinson’s
disease; CI, confidence interval; AUC, area under the curve.
(DOCX)
Author Contributions
Conceptualization: Younsoo Kim, Jin Myoung Seok, Kun-Hyun Kim, Jin Whan Cho, Suyeon
Park, Byoung Joon Kim, Jinyoung Youn.
Data curation: Jongkyu Park, Kun-Hyun Kim, Hyun-jin Kim, Byoung Joon Kim, Jinyoung
Youn.
Formal analysis: Younsoo Kim, Jin Myoung Seok, Ju-Hong Min, Suyeon Park, Byoung Joon
Kim, Jinyoung Youn.
Investigation: Jongkyu Park, Kun-Hyun Kim, Ju-Hong Min, Hyun-jin Kim, Byoung Joon
Kim, Jinyoung Youn.
Methodology: Younsoo Kim, Jin Myoung Seok, Ju-Hong Min, Jin Whan Cho, Hyun-jin Kim,
Jinyoung Youn.
Project administration: Byoung Joon Kim, Jinyoung Youn.
Resources: Younsoo Kim, Jinyoung Youn.
Supervision: Jin Myoung Seok, Jin Whan Cho, Byoung Joon Kim, Jinyoung Youn.
Validation: Suyeon Park, Byoung Joon Kim, Jinyoung Youn.
Visualization: Suyeon Park, Jinyoung Youn.
Writing – original draft: Younsoo Kim, Suyeon Park, Jinyoung Youn.
Writing – review & editing: Jin Myoung Seok, Jongkyu Park, Suyeon Park, Byoung Joon
Kim, Jinyoung Youn.
References
1. Gilman S, Wenning GK, Low PA, Brooks DJ, Mathias CJ, Trojanowski JQ, et al. Second consensus
statement on the diagnosis of multiple system atrophy. Neurology. 2008; 71(9):670–6. Epub 2008/08/
30. https://doi.org/10.1212/01.wnl.0000324625.00404.15 PMID: 18725592; PubMed Central PMCID:
PMCPmc2676993.
2. Kim JS, Lee SH, Oh YS, Park JW, An JY, Park SK, et al. Cardiovascular Autonomic Dysfunction in Mild
and Advanced Parkinson’s Disease. Journal of movement disorders. 2016; 9(2):97–103. https://doi.
org/10.14802/jmd.16001 PMID: 27020456; PubMed Central PMCID: PMC4886202.
PLOS ONE | https://doi.org/10.1371/journal.pone.0180744 July 6, 2017 9 / 10
COMPASS 31 for differentiation of MSA and PD
3. Kim JB, Kim BJ, Koh SB, Park KW. Autonomic dysfunction according to disease progression in Parkin-
son’s disease. Parkinsonism & related disorders. 2014; 20(3):303–7. https://doi.org/10.1016/j.
parkreldis.2013.12.001 PMID: 24382402.
4. Baschieri F, Calandra-Buonaura G, Doria A, Mastrolilli F, Palareti A, Barletta G, et al. Cardiovascular
autonomic testing performed with a new integrated instrumental approach is useful in differentiating
MSA-P from PD at an early stage. Parkinsonism & related disorders. 2015; 21(5):477–82. https://doi.
org/10.1016/j.parkreldis.2015.02.011 PMID: 25749354.
5. Kimpinski K, Iodice V, Burton DD, Camilleri M, Mullan BP, Lipp A, et al. The role of autonomic testing in
the differentiation of Parkinson’s disease from multiple system atrophy. Journal of the neurological sci-
ences. 2012; 317(1–2):92–6. https://doi.org/10.1016/j.jns.2012.02.023 PMID: 22421352; PubMed Cen-
tral PMCID: PMC3340456.
6. Riley DE, Chelimsky TC. Autonomic nervous system testing may not distinguish multiple system atro-
phy from Parkinson’s disease. Journal of neurology, neurosurgery, and psychiatry. 2003; 74(1):56–60.
PMID: 12486267; PubMed Central PMCID: PMC1738185. https://doi.org/10.1136/jnnp.74.1.56
7. Lipp A, Sandroni P, Ahlskog E, Fealey RD, Kimpinski K, Iodice V, et al. Prospective Differentiation of
Multiple System Atrophy From Parkinson Disease, With and Without Autonomic Failure. Arch Neurol.
2009; 66(6):742–50. https://doi.org/10.1001/archneurol.2009.71 PMID: 19506134
8. Reimann M, Schmidt C, Herting B, Prieur S, Junghanns S, Schweitzer K, et al. Comprehensive auto-
nomic assessment does not differentiate between Parkinson’s disease, multiple system atrophy and
progressive supranuclear palsy. Journal of neural transmission. 2010; 117(1):69–76. https://doi.org/10.
1007/s00702-009-0313-y PMID: 19763772.
9. Sletten DM, Suarez GA, Low PA, Mandrekar J, Singer W. COMPASS 31: a refined and abbreviated
Composite Autonomic Symptom Score. Mayo Clinic proceedings. 2012; 87(12):1196–201. https://doi.
org/10.1016/j.mayocp.2012.10.013 PMID: 23218087; PubMed Central PMCID: PMC3541923.
10. Cortez MM, Nagi Reddy SK, Goodman B, Carter JL, Wingerchuk DM. Autonomic symptom burden is
associated with MS-related fatigue and quality of life. Multiple sclerosis and related disorders. 2015; 4
(3):258–63. https://doi.org/10.1016/j.msard.2015.03.007 PMID: 26008943.
11. Treister R, O’Neil K, Downs HM, Oaklander AL. Validation of the composite autonomic symptom scale
31 (COMPASS-31) in patients with and without small fiber polyneuropathy. European journal of neurol-
ogy. 2015; 22(7):1124–30. https://doi.org/10.1111/ene.12717 PMID: 25907824; PubMed Central
PMCID: PMC4464987.
12. Kang JH, Kim JK, Hong SH, Lee CH, Choi BY. Heart Rate Variability for Quantification of Autonomic
Dysfunction in Fibromyalgia. Annals of rehabilitation medicine. 2016; 40(2):301–9. https://doi.org/10.
5535/arm.2016.40.2.301 PMID: 27152281; PubMed Central PMCID: PMC4855125.
13. Chaudhuri KR, Schapira AH. Non-motor symptoms of Parkinson’s disease: dopaminergic pathophysiol-
ogy and treatment. Lancet Neurol. 2009; 8(5):464–74. https://doi.org/10.1016/S1474-4422(09)70068-7
PMID: 19375664.
14. Hughes AJ, Daniel SE, Kilford L, Lees AJ. Accuracy of clinical diagnosis of idiopathic Parkinson’s dis-
ease: a clinico-pathological study of 100 cases. Journal of neurology, neurosurgery, and psychiatry.
1992; 55(3):181–4. Epub 1992/03/01. PMID: 1564476; PubMed Central PMCID: PMCPmc1014720.
15. Hoehn MM, Yahr MD. Parkinsonism: onset, progression, and mortality. 1967. Neurology. 1998; 50
(2):318 and 16 pages following. PMID: 9484345.
16. Vogel ER, Sandroni P, Low PA. Blood pressure recovery from Valsalva maneuver in patients with auto-
nomic failure. Neurology. 2005; 65(10):1533–7. https://doi.org/10.1212/01.wnl.0000184504.13173.ef
PMID: 16301478.
17. Novak P. Quantitative autonomic testing. Journal of visualized experiments: JoVE. 2011;(53). https://
doi.org/10.3791/2502 PMID: 21788940; PubMed Central PMCID: PMC3196175.
18. Chung EJ, Lee WY, Yoon WT, Kim BJ, Lee GH. MIBG scintigraphy for differentiating Parkinson’s dis-
ease with autonomic dysfunction from Parkinsonism-predominant multiple system atrophy. Mov Disord.
2009; 24(11):1650–5. https://doi.org/10.1002/mds.22649 PMID: 19514077.
19. Yokota T, Matsunaga T, Okiyama R, Hirose K, Tanabe H, Furukawa T, et al. Sympathetic skin response
in patients with multiple sclerosis compared with patients with spinal cord transection and normal con-
trols. Brain. 1991; 114 (Pt 3):1381–94. PMID: 2065256.
20. Low PA. Composite Autonomic Scoring Scale for Laboratory Quantification of Generalized Autonomic
Failure. Mayo Clinic proceedings. 1993; 68:748–52. PMID: 8392653
PLOS ONE | https://doi.org/10.1371/journal.pone.0180744 July 6, 2017 10 / 10
You might also like
- Unani Medicine in India WebDocument122 pagesUnani Medicine in India WebHiramandalam Patanjali100% (2)
- Non Invasive VentilationDocument442 pagesNon Invasive Ventilationagnese valentiniNo ratings yet
- Week 7 - Nail Disorder and DiseasesDocument46 pagesWeek 7 - Nail Disorder and DiseasesGinalynRapirapHuitNo ratings yet
- COCOLIFE Heathcare Reimbursement FormDocument2 pagesCOCOLIFE Heathcare Reimbursement FormMJVP0% (1)
- The Association of Blood Pressure and Primary Open-Angle Glaucoma: A Meta-AnalysisDocument23 pagesThe Association of Blood Pressure and Primary Open-Angle Glaucoma: A Meta-AnalysisSarah Martinauli HarahapNo ratings yet
- Korean COMPASS-31Document11 pagesKorean COMPASS-31Margareth HildariaNo ratings yet
- Korean SCOPA AUTDocument6 pagesKorean SCOPA AUTMargareth HildariaNo ratings yet
- CSF ParkinsonDocument4 pagesCSF ParkinsonYunita Christiani BiyangNo ratings yet
- Pharmacotherapy For Diabetic Peripheral Neuropathy Pain and Quality of LifeDocument11 pagesPharmacotherapy For Diabetic Peripheral Neuropathy Pain and Quality of LifeAF KoasNo ratings yet
- Panda 2021Document9 pagesPanda 2021rayan1996.officialNo ratings yet
- 60 - Minocycline Combination Therapy Withfluvoxaminein Moderate-To-Severe Obsessive-Compulsive Disorder, A Placebo-Controlled, Double-Blind, Randomized TrialDocument10 pages60 - Minocycline Combination Therapy Withfluvoxaminein Moderate-To-Severe Obsessive-Compulsive Disorder, A Placebo-Controlled, Double-Blind, Randomized TrialPaula CantalapiedraNo ratings yet
- Efficacy and Acceptability of Pharmacological Treat-Ments For Depressive Disorders in Primary Care: Systematic Review and Network Meta-AnalysisDocument11 pagesEfficacy and Acceptability of Pharmacological Treat-Ments For Depressive Disorders in Primary Care: Systematic Review and Network Meta-AnalysisPutri YingNo ratings yet
- Greek SCOPA-AUTDocument6 pagesGreek SCOPA-AUTMargareth HildariaNo ratings yet
- Autonomic Function and Motor Subtypes in Parkinson's DiseaseDocument11 pagesAutonomic Function and Motor Subtypes in Parkinson's DiseaseCarla AlmeidaNo ratings yet
- Equilibrio y Movilidad en Pacientes Con Enfermedad de Parkinson Recién Diagnosticada Seguimiento de Cinco Años de Una Cohorte en El Norte de SueciaDocument10 pagesEquilibrio y Movilidad en Pacientes Con Enfermedad de Parkinson Recién Diagnosticada Seguimiento de Cinco Años de Una Cohorte en El Norte de SueciacamilaNo ratings yet
- RamachandranDocument9 pagesRamachandranjojobaggins100% (1)
- Second Generation Antipsychotic-Induced Obsessive-Compulsive Symptoms in Schizophrenia: A Review of The Experimental LiteratureDocument17 pagesSecond Generation Antipsychotic-Induced Obsessive-Compulsive Symptoms in Schizophrenia: A Review of The Experimental LiteratureDerek TantaleánNo ratings yet
- UA ParkinsonDocument6 pagesUA ParkinsonNgọc LamNo ratings yet
- Journal Pone 0276012Document15 pagesJournal Pone 0276012hardi adiyatmaNo ratings yet
- Autonomic Dysregulation Cognition and Fatigue in People With Depression and in Active and Healthy Controls Observational Cohort StudyDocument11 pagesAutonomic Dysregulation Cognition and Fatigue in People With Depression and in Active and Healthy Controls Observational Cohort StudyValentina De La PazNo ratings yet
- tmp1329 TMPDocument11 pagestmp1329 TMPFrontiersNo ratings yet
- Pone 0159966Document16 pagesPone 0159966JESICA PAOLA RODRIGUEZ PEREZNo ratings yet
- Slide Jurnal Efusi PleuraDocument8 pagesSlide Jurnal Efusi PleuraolakasturiNo ratings yet
- Effects of Risperidone and Olanzapine Dose Reduction On Cognitive Function in Stable Patients With SchizophreniaDocument6 pagesEffects of Risperidone and Olanzapine Dose Reduction On Cognitive Function in Stable Patients With Schizophreniawen zhangNo ratings yet
- Panss 78Document24 pagesPanss 78ijmalNo ratings yet
- Neu 2015 4192Document14 pagesNeu 2015 4192Dea RitungNo ratings yet
- Possible Effect of Acupuncture in Autism Spectrum DisorderDocument3 pagesPossible Effect of Acupuncture in Autism Spectrum DisorderPaul NguyenNo ratings yet
- Age at Onset and Parkinson Disease PhenotypeDocument9 pagesAge at Onset and Parkinson Disease Phenotypemariel gonzalezNo ratings yet
- Z Al-Roubaie - 2020Document12 pagesZ Al-Roubaie - 2020Kossay ZaouiNo ratings yet
- Atrofia Multiples Sitemas 2009Document7 pagesAtrofia Multiples Sitemas 2009Miztli CervantesNo ratings yet
- Tratamiento en APP 2013Document34 pagesTratamiento en APP 2013Mauricio EtchegarayNo ratings yet
- Journal Pone 0070571Document8 pagesJournal Pone 0070571Basil AlsaadiNo ratings yet
- A Systematic Review and Network Meta-Analysis To AssessDocument13 pagesA Systematic Review and Network Meta-Analysis To AssessastrogliaNo ratings yet
- Sepede G, 2016Document21 pagesSepede G, 2016Bianca PerezNo ratings yet
- Mortality in Pediatric Acute Respiratory Distress Syndrome: A Systematic Review and Meta-AnalysisDocument9 pagesMortality in Pediatric Acute Respiratory Distress Syndrome: A Systematic Review and Meta-Analysisesya putrri oktareginaNo ratings yet
- Heterogenitate BPDocument8 pagesHeterogenitate BPCarmen CiursaşNo ratings yet
- Lurasidone For Adolescent SchizophreniaDocument11 pagesLurasidone For Adolescent Schizophreniaromany hosnyNo ratings yet
- (1479683X - European Journal of Endocrinology) THERAPY OF ENDOCRINE DISEASE - A systematic review and meta-analysis of α-lipoic acid in the treatment of diabetic peripheral neuropathyDocument7 pages(1479683X - European Journal of Endocrinology) THERAPY OF ENDOCRINE DISEASE - A systematic review and meta-analysis of α-lipoic acid in the treatment of diabetic peripheral neuropathyHendri YantoNo ratings yet
- 2014 KimDocument6 pages2014 Kimnermal93No ratings yet
- Barrionuevo 2018Document7 pagesBarrionuevo 2018hlwNo ratings yet
- Leukotriene Antagonists in Nasal Polyposis: A Meta-Analysis and Systematic ReviewDocument8 pagesLeukotriene Antagonists in Nasal Polyposis: A Meta-Analysis and Systematic ReviewRezaNo ratings yet
- Cognitive Impairment in Patients With Parkinsons Disease A 30month Followup StudyDocument11 pagesCognitive Impairment in Patients With Parkinsons Disease A 30month Followup StudyAisyahImasSetiawatiNo ratings yet
- PTJ 1620Document18 pagesPTJ 1620Martina SimangunsongNo ratings yet
- Dysautonomia Is Associated With Structural and Functional Alterations in Parkinson DiseaseDocument13 pagesDysautonomia Is Associated With Structural and Functional Alterations in Parkinson DiseaseolgaguerreroNo ratings yet
- Lian 2021Document11 pagesLian 2021RickyconsuegraNo ratings yet
- Acta Psychiatr Scand - 2013 - Bourne - Neuropsychological Testing of Cognitive Impairment in Euthymic Bipolar Disorder AnDocument14 pagesActa Psychiatr Scand - 2013 - Bourne - Neuropsychological Testing of Cognitive Impairment in Euthymic Bipolar Disorder AnJeriesnal GamingNo ratings yet
- Duailibi 2017Document7 pagesDuailibi 2017Iván Tonatiuh Jiménez MolinaNo ratings yet
- Factors Associated With Patellofemoral Pain Syndrome: A Systematic ReviewDocument17 pagesFactors Associated With Patellofemoral Pain Syndrome: A Systematic Reviewנתנאל מושקוביץNo ratings yet
- Dexlansoprazole Vs Esomeprazole ERGEDocument12 pagesDexlansoprazole Vs Esomeprazole ERGELuis Felipe Gomez AndradeNo ratings yet
- Parkinson Subtypes Progress Differently PDFDocument8 pagesParkinson Subtypes Progress Differently PDFParisNo ratings yet
- RMD Open-2016-KalyoncuDocument9 pagesRMD Open-2016-KalyoncuneoslaveNo ratings yet
- Evaluation and Comparison of Three Assays For Molecular Detection of Spinal Muscular AtrophyDocument11 pagesEvaluation and Comparison of Three Assays For Molecular Detection of Spinal Muscular AtrophyRainie PhamNo ratings yet
- Meta-Analysis of Randomized Controlled Trials On TDocument18 pagesMeta-Analysis of Randomized Controlled Trials On TIbrahim SabraNo ratings yet
- A Systematic Review of Neuropsychiatric and Cognitive AssessmentsDocument12 pagesA Systematic Review of Neuropsychiatric and Cognitive Assessmentskarenina10No ratings yet
- Fnins 13 00472Document18 pagesFnins 13 00472Infinity PsychiatryNo ratings yet
- Texte 9Document12 pagesTexte 9Clara ScemamaNo ratings yet
- Congantive Metobolic Symdrome Case StudyDocument6 pagesCongantive Metobolic Symdrome Case StudyPrachiti ChavanNo ratings yet
- Development and Validation of The FSIQ-RMS A New PDocument14 pagesDevelopment and Validation of The FSIQ-RMS A New Psda asfNo ratings yet
- Skripsi Full Teks Tanpa Bab Pembahasan PDFDocument68 pagesSkripsi Full Teks Tanpa Bab Pembahasan PDFahmad faisalNo ratings yet
- Skripsi Full Teks Tanpa Bab Pembahasan PDFDocument68 pagesSkripsi Full Teks Tanpa Bab Pembahasan PDFahmad faisalNo ratings yet
- BJP 2011 Thase 501 7Document8 pagesBJP 2011 Thase 501 7Joanne Suguitan- GarciaNo ratings yet
- BD 3Document14 pagesBD 3aboharaNo ratings yet
- Review Dysphagia Tto PoststrokeDocument7 pagesReview Dysphagia Tto PoststrokeTrinidad OdaeNo ratings yet
- C4T Pulmonary Stenosis - WebDocument2 pagesC4T Pulmonary Stenosis - WebraosudhNo ratings yet
- The Top 15 Best Selling Cancer Drugs in 2022Document16 pagesThe Top 15 Best Selling Cancer Drugs in 2022Soma YasaswiNo ratings yet
- Unit 4 Reading (Lisnawatie)Document2 pagesUnit 4 Reading (Lisnawatie)Lisna WatieNo ratings yet
- ProjDocument37 pagesProjM LubisNo ratings yet
- Nurs362 Professional Development PlanDocument4 pagesNurs362 Professional Development Planapi-272566401No ratings yet
- Feline Anaplasmosis 2020Document14 pagesFeline Anaplasmosis 2020Birdella GwenNo ratings yet
- Agenda Zoonotic Influenza Webinar - 8-9 May 2023Document2 pagesAgenda Zoonotic Influenza Webinar - 8-9 May 2023haniefahmadNo ratings yet
- DR René KABERA :this Situation Was AlarmingDocument2 pagesDR René KABERA :this Situation Was AlarmingKABERA RENENo ratings yet
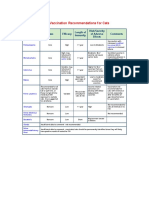
- AVMA Vaccination Recommendations F or CatsDocument2 pagesAVMA Vaccination Recommendations F or CatsHazim Azmi Al-QadryNo ratings yet
- Medical Problems in The 19th CenturyDocument9 pagesMedical Problems in The 19th CenturyWill TeeceNo ratings yet
- BOPTDocument7 pagesBOPThelmuth0207No ratings yet
- Bronchopneumonia TreatmentDocument2 pagesBronchopneumonia TreatmentJam RapaconNo ratings yet
- Breast ScreeningDocument76 pagesBreast ScreeningBenny KurniawanNo ratings yet
- Us ObDocument16 pagesUs ObWahyu RianiNo ratings yet
- Malaria ProtocolDocument8 pagesMalaria ProtocolPERFECT CLASSESNo ratings yet
- 3rd Year-Community Medicine Study GuideDocument78 pages3rd Year-Community Medicine Study GuideNasir HussainNo ratings yet
- School Health Examination Form EDITEDDocument2 pagesSchool Health Examination Form EDITEDjustine mae villaruelNo ratings yet
- 1 Running Head: Cauti Bundle EffectivenessDocument9 pages1 Running Head: Cauti Bundle Effectivenessapi-544117547No ratings yet
- CSS Perio ObieDocument11 pagesCSS Perio ObieRobbyRamadhonieNo ratings yet
- Safety ProgramDocument24 pagesSafety ProgramJuan CruzNo ratings yet
- Informed Consent For Nursing ProceduresDocument2 pagesInformed Consent For Nursing ProceduresZNo ratings yet
- Report of Medical Examination and Vaccination RecordDocument14 pagesReport of Medical Examination and Vaccination RecordHrishi WaghNo ratings yet
- Issues Paper Kim Werschler and Becky WerschlerDocument12 pagesIssues Paper Kim Werschler and Becky WerschlerKimberly WerschlerNo ratings yet
- Role of Statistics in HealthcareDocument4 pagesRole of Statistics in HealthcareSumita ChatterjeeNo ratings yet
- Reviewing Harm Reduction For People Who Inject Drugs in Asia - The Necessity For GrowthDocument5 pagesReviewing Harm Reduction For People Who Inject Drugs in Asia - The Necessity For GrowthAura NirwanaNo ratings yet
- PulpotecDocument2 pagesPulpotecFeras Al-ZbounNo ratings yet