Professional Documents
Culture Documents
Journal - Pone 2021
Uploaded by
cdsaludOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Journal - Pone 2021
Uploaded by
cdsaludCopyright:
Available Formats
PLOS ONE
RESEARCH ARTICLE
Influenza vaccine effectiveness against
influenza A in children based on the results of
various rapid influenza tests in the 2018/19
season
Masayoshi Shinjoh1, Norio Sugaya ID2*, Yoshio Yamaguchi3, Ichiro Ookawara4,
Yuji Nakata5, Atsushi Narabayashi6, Munehiro Furuichi1, Naoko Yoshida1,
Akinobu Kamei7, Yuu Kuramochi8, Akimichi Shibata9, Motoko Shimoyamada10,
Hisataka Nakazaki11, Naohiko Maejima12, Erika Yuasa13, Eriko Araki9, Naonori Maeda14,
Takuma Ohnishi15, Mitsuhiro Nishida16, Nobuhiko Taguchi2, Makoto Yoshida17,
a1111111111 Kenichiro Tsunematsu18, Meiwa Shibata19, Yasuhiro Hirano20, Shinichiro Sekiguchi1,
a1111111111 Chiharu Kawakami21, Keiko Mitamura22, Takao Takahashi1
a1111111111
a1111111111 1 Department of Pediatrics, Keio University School of Medicine, Tokyo, Japan, 2 Department of Pediatrics,
a1111111111 Keiyu Hospital, Kanagawa, Japan, 3 Institute of Clinical Research & Department of Infection and Allergy,
National Hospital Organization Tochigi Hospital, Tochigi, Japan, 4 Department of Pediatrics, Japanese Red
Cross Shizuoka Hospital, Shizuoka, Japan, 5 Department of Pediatrics, Nippon Koukan Hospital, Kanagawa,
Japan, 6 Department of Pediatrics, Kawasaki Municipal Hospital, Kanagawa, Japan, 7 Department
Pediatrics, Yokohama Municipal Citizen’s Hospital, Kanagawa, Japan, 8 Department of Pediatrics, Subaru
Health Insurance Society Ota Memorial Hospital, Gunma, Japan, 9 Department of Pediatrics, Japanese Red
OPEN ACCESS Cross Ashikaga Hospital, Tochigi, Japan, 10 Department of Pediatrics, Saitama City Hospital, Saitama,
Japan, 11 Department of Pediatrics, Tokyo Dental College Ichikawa General Hospital, Chiba, Japan,
Citation: Shinjoh M, Sugaya N, Yamaguchi Y, 12 Department of Pediatrics, Tokyo Metropolitan Ohtsuka Hospital, Tokyo, Japan, 13 Department of
Ookawara I, Nakata Y, Narabayashi A, et al. (2021) Pediatrics, Saiseikai Utsunomiya Hospital, Tochigi, Japan, 14 Department of Pediatrics, National Hospital
Influenza vaccine effectiveness against influenza A Organization Tokyo Medical Center, Tokyo, Japan, 15 Department of Pediatrics, National Hospital
in children based on the results of various rapid Organization Saitama Hospital, Saitama, Japan, 16 Department of Pediatrics, Shizuoka City Shimizu
influenza tests in the 2018/19 season. PLoS ONE Hospital, Shizuoka, Japan, 17 Department of Pediatrics, Sano Kosei General Hospital, Tochigi, Japan,
16(3): e0249005. https://doi.org/10.1371/journal. 18 Department of Pediatrics, Hino Municipal Hospital, Tokyo, Japan, 19 Department of Pediatrics,
pone.0249005 Yokohama Rosai Hospital, Kanagawa, Japan, 20 Department of Pediatrics, Hiratsuka City Hospital,
Kanagawa, Japan, 21 Yokohama City Institute of Public Health, Yokohama, Japan, 22 Department of
Editor: Ka Chun Chong, The Chinese University of Pediatrics, Eiju General Hospital, Tokyo, Japan
Hong Kong, HONG KONG
* sugaya-n@za2.so-net.ne.jp
Received: June 8, 2020
Accepted: March 9, 2021
Published: March 26, 2021 Abstract
Copyright: © 2021 Shinjoh et al. This is an open During influenza epidemics, Japanese clinicians routinely conduct rapid influenza diagnostic
access article distributed under the terms of the
Creative Commons Attribution License, which
tests (RIDTs) in patients with influenza-like illness, and patients with positive test results are
permits unrestricted use, distribution, and treated with anti-influenza drugs within 48 h after the onset of illness. We assessed the vac-
reproduction in any medium, provided the original cine effectiveness (VE) of inactivated influenza vaccine (IIV) in children (6 months–15 years
author and source are credited.
old, N = 4243), using a test-negative case-control design based on the results of RIDTs in
Data Availability Statement: Data cannot be the 2018/19 season. The VE against influenza A(H1N1)pdm and A(H3N2) was analyzed
shared publicly because the data set includes
separately using an RIDT kit specifically for detecting A(H1N1)pdm09. The adjusted VE
patients’ personal information. Data other than
confidential data are available from the Keio against combined influenza A (H1N1pdm and H3N2) and against A(H1N1)pdm09 was 39%
University Ethics Committee (https://www.ctr.med. (95% confidence interval [CI], 30%–46%) and 74% (95% CI, 39%–89%), respectively. By
keio.ac.jp/forms/form_a.html or FAX: 81-3-5379- contrast, the VE against non-A(H1N1)pdm09 influenza A (presumed to be H3N2) was very
1978) or Dr. Masayoshi Shinjoh (m-shinjo@z2.
low at 7%. The adjusted VE for preventing hospitalization was 56% (95% CI, 16%–77%)
keio.jp) for researchers who meet the criteria to
access the data. against influenza A. The VE against A(H1N1)pdm09 was consistently high in our studies.
PLOS ONE | https://doi.org/10.1371/journal.pone.0249005 March 26, 2021 1 / 12
PLOS ONE Influenza vaccine effectiveness in children, 2018/19
Funding: The authors received no specific funding By contrast, the VE against A(H3N2) was low not only in adults but also in children in the
for this work. 2018/19 season.
Competing interests: We have read the journal’s
policy and the authors of this manuscript have the
following competing interests: within 36 months,
Dr. Norio Sugaya has received speakers’ honoraria
from Chugai, Shionogi, Daiichi Sankyo, Astellas, Introduction
Merck, and Denka Seiken. Dr. Masayoshi Shinjoh In Japan, rapid influenza diagnostic tests (RIDTs) are considered core tools for determining
has received speakers’ honoraria from Shionogi,
whether or not to start treatment with anti-influenza drugs. During influenza epidemics, Japa-
Meiji Seika, Merck, Sumitomo Dainippon, Japan
Vaccine, Maruho, Astellas, Daiichi Sankyo, and nese clinicians routinely use RIDTs in the examination of patients with influenza-like illness,
grant support from Janssen. Dr. Keiko Mitamura and most patients with positive test results are treated with anti-influenza drugs within 48 h
has received speakers’ honoraria from Shionogi, after the onset of illness [1, 2]. We have reported the vaccine effectiveness (VE) in children
Meiji Seika, and manuscript fee from Astellas. Dr. using a test-negative case-control (TNCC) design based on the results of RIDT since the 2013/
Takao Takahashi has received speakers’ honoraria
14 season. Capitalizing on the advantage of the widespread use of RIDTs, we have been able to
from Daiichi Sankyo, GlaxoSmithKline, Japan
Vaccine, Pfizer, Merck, and grant support from
enroll over 3000 to 4000 children in our VE study every year [3–7]. Although the quality of
Daiichi Sankyo, Japan Vaccine, Pfizer, Merck, RIDT tests was reported to be insufficient [8], they are clearly on the agenda of public health
Takeda, and Astellas. Other authors have no authorities, clinicians, and health services managers in Japan, and the sensitivity and specifici-
competing interests regarding this study. This does ties of the tests that we used were satisfactory [9, 10].
not alter our adherence to PLOS ONE policies on The purpose of this study was to measure the VE in the 2018/19 season based on the results
sharing data and materials.
of RIDTs, including the VE for preventing hospitalization and by vaccine dose. In addition,
the VE against influenza A(H1N1)pdm09 was measured using an RIDT kit specifically for
detecting A(H1N1)pdm09.
Methods
To assess VE, we used a TNCC design based on RIDT results [3–7, 11]. Children who were 6
months to 15 years old who had a fever of �38˚C and were suspected of having influenza and
had received an RIDT at one of the outpatient clinics of 21 hospitals in Gunma, Tochigi, Sai-
tama, Tokyo, Chiba, Kanagawa, and Shizuoka Prefectures between November 1, 2018 and
March 31, 2019 were enrolled. All hospitals were located within a 70-mile radius of Tokyo. As
cough and other respiratory tract–related symptoms are less prominent, especially in younger
children, and as myalgias and malaise are not always seen in children [12], we did not include
symptoms other than fever. Consecutive sampling or whole sampling for each collaborator
was encouraged and performed, especially in hospitals with small sample size.
Quadrivalent influenza vaccine strains used in the 2018/19 season
The vaccine strains in the 2018/19 season were A/Singapore/GP1908/2015 (A(H1N1)pdm09)
(A/Michigan/45/2015-like), A/Singapore/INFIMH-16-0019/2016 (A(H3N2)), B/Phuket/3073/
2013 (Yamagata lineage), and B/Maryland/15/2016 (Victoria lineage).
The diagnosis of influenza
Nasopharyngeal swabs were obtained from patients. The swab for each test kit was inserted
deeply into the back of at least one nostril, left in place for several seconds, rotated to absorb
secretions, placed into the medium of each kit, and tested immediately. RIDT kits capable of
differentiating between influenza A and influenza B were used in all hospitals, including the
ImmunoAce FLU kit (TAUNS Laboratories, Inc., Shizuoka, Japan), Quick Chaser Flu A, B kit
(Mizuho Medy Co., Ltd., Saga, Japan), QuickNavi-Flu kit (Denka Seiken Co., Ltd., Tokyo,
Japan), Espline Influenza A&B-N kit (Fujirebio Inc., Tokyo, Japan), and Spotchem FLORA
FluAB (Arkray Factory, Inc., Shiga, Japan). All of these kits have high sensitivity
PLOS ONE | https://doi.org/10.1371/journal.pone.0249005 March 26, 2021 2 / 12
PLOS ONE Influenza vaccine effectiveness in children, 2018/19
(approximately 85%–95%) and specificity (up to 100%) compared to reverse transcription
polymerase chain reaction (RT-PCR) [6].
The ImunoAce Flu test is designed to not only detect influenza A or B, but also to detect A
(H1N1)pdm09 with the use of an additional test kit (Linjudge FluA/pdm, TAUNS Laborato-
ries, Inc., Shizuoka, Japan). Its sensitivity and specificity for A(H1N1)pdm09 were 97.6% (95%
confidence interval [CI]: 87.4%–99.9%) and 92.6% (95%CI: 82.1%–97.9%) in adults, respec-
tively [10]. Thus, by consecutively testing patients with the ImunoAce Flu test followed by the
Linjudge FluA/pdm test, we were able to diagnose whether a patient had A(H1N1)pdm09 or A
(H3N2) infection within a short time. In this study, we defined “A(H3N2)” as patients positive
for influenza A but negative for A(H1N1)pdm09 in hospitals where the test kit Linjudge FluA/
pdm had been used. However, it must be recognized that influenza A-positive with A(H1N1)
pdm09-negative does not always mean A(H3N2)-positive.
Case and control patient identification and VE
RIDT-positive patients were enrolled as cases and RIDT-negative patients were enrolled as
controls. The information shown in Table 1 was collected and recorded. The source of vacci-
nation information, including doses, was medical interviews and/or medical records from the
Maternal and Child Health Handbooks provided by local governments [13]. As the handbooks
are not digitalized, parents usually bring them to health visits. Patients who had already taken
anti-influenza viral drugs prior to the visit were excluded. VE was defined as “1- odds ratio
(OR),” and OR was calculated as follows:
(number of influenza-positives among vaccinated patients × number of influenza-negatives
among unvaccinated patients) / (number of influenza-negatives among vaccinated
patients × number of influenza-positives among unvaccinated patients).
Adjustments to the VE are explained below. The VE for preventing influenza A(H1N1)
pdm09 was also analyzed in three hospitals where the ImunoAce Flu and the Linjudge FluA/
pdm were used.
VE for preventing hospitalization
In the TNCC design, the cases were patients who were hospitalized because of influenza
(RIDT-positive hospitalized patients) after diagnosis at an outpatient clinic. Patients hospital-
ized because of influenza-like illness who were RIDT-negative served as the control group.
The VE for preventing influenza hospitalization was estimated based on the vaccine coverage
rate of both hospitalized patient groups.
VE by vaccine dose (6 months–12 years old)
In Japan, a single dose is recommended for children �13 years old, but a two-dose regimen is
recommended for all children aged 6 months to 12 years old [14]. Doses of 0.25 ml and 0.5 ml
are recommended for children 6 months to 2 years old and �3 years old, respectively. Approx-
imately 70% of vaccinated children 6 months to 12 years old receive two doses [15]. We
recorded the number of vaccine doses per patient (none, one, or two) and compared the VE
among them. The VE was calculated among all three groups (“none,” “one,” and “two”) using
three combinations (1. one vs. none, 2. two vs. none, and 3. two vs. one).
Statistical analyses and ethics
Statistical analyses were performed using the SPSS 25.0 software program (IBM, Chicago,
USA) and the Ekuseru-Toukei 2015 for Windows software program (Social Survey Research
PLOS ONE | https://doi.org/10.1371/journal.pone.0249005 March 26, 2021 3 / 12
PLOS ONE Influenza vaccine effectiveness in children, 2018/19
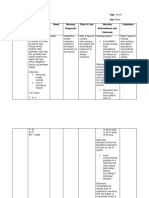
Table 1. Characteristics of children enrolled in 2018/19 season (n = 4243)� .
Characteristics Influenza A Positive (%) Influenza Negative (%) Difference between influenza A and influenza-
N = 2135 N = 2098 negative p-value��
Sex Female 971 (45) 915 (44) p = 0.211
Male 1162 (54) 1183 (56)
Not reported 2 (0) 0 (0)
Age 6–11 months 66 (3) 140 (7) p < 0.001
1–2 years 339 (16) 697 (33)
3–5 years 530 (25) 560 (27)
6–12 years 980 (46) 571 (27)
13–15 years 220 (10) 130 (6)
���
Comorbidity No 1811 (86) 1714 (83) p = 0.005
Yes 293 (14) 352 (17)
Month of onset November 11 (1) 142 (7) p < 0.001
December 235 (11) 454 (22)
January 1436 (67) 793 (38)
February 415 (19) 532 (25)
March 38 (2) 177 (8)
Clinic visit��� (hours after onset) <12 h 661 (33) 596 (33) p < 0.001
12–48 h 1259 (63) 1030 (57)
>48 h 67 (3) 178 (10)
Received vaccine during the season No 1368 (64) 1061 (51) p < 0.001
Yes 767 (36) 1037 (49)
Vaccine doses during the season��� None 1368 (64) 1061 (51) p < 0.001
One 222 (10) 251 (12)
Two 535 (25) 775 (37)
Treatment with antivirals��� No 61 (3) 1632 (97) p < 0.001
Any 1994 (97) 44 (3)
Hospitalized after diagnosis at outpatient Unvaccinated 48 59
clinics���
Vaccinated 26 71
Non-hospitalized after diagnosis at Unvaccinated 1320 964
outpatient clinics���
Vaccinated 740 896
�
: 10 children with influenza B were included in the 4243 enrolled patients.
��
: Chi-square test
���
: Some data were missing
https://doi.org/10.1371/journal.pone.0249005.t001
Information Co., Ltd., Tokyo, Japan). p < 0.05 was considered statistically significant for all
analyses.
To analyze the VE for both preventing influenza and preventing hospitalization, binary
logistic regression methods were chosen. Confounding factors, such as age (0–15 years old),
comorbidity (yes or no), colder or warmer area (northern, middle, or southern area of the
Kanto region), and month of onset, were entered in the analysis by the forced entry method.
For some analyses, the time tested after onset (<12, 12–48, and >48 h) was also entered. These
factors for adjustment have been the same since our 2013/14 study [3]. The chi-square test was
used to compare the test-positive and test-negative groups. To reduce the chance of type 1
errors, p-values were also Bonferroni corrected for the dose analysis (p-value <0.05/3 = 0.017
was also calculated in one table).
PLOS ONE | https://doi.org/10.1371/journal.pone.0249005 March 26, 2021 4 / 12
PLOS ONE Influenza vaccine effectiveness in children, 2018/19
This study was approved by the Keio University Ethics Committee (Approval Number
20130216, revised in 2018). Eligible patients and their guardians were informed about the
study objectives and methods verbally or via posters in outpatient clinics. We recorded the
necessary information using a standardized questionnaire sheet. The requirement for obtain-
ing written consent was waived by the Keio University Institutional Review Board because
testing patients with an RIDT is a standard practice, and all questions regarding this study are
essential in daily practice.
Results
The 2018/19 season in Japan
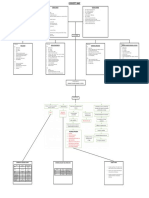
The change in the number of RIDT-positive or RIDT-negative patients is shown in Fig 1. The
influenza epidemic in the 2018/19 season was a mixed epidemic of influenza A subtypes. A
monophasic epidemic pattern of influenza A with a single peak in January (week 3 of 2020)
was observed. According to the World Health Organization (WHO)’s website [16], the influ-
enza viruses isolated/detected in the 2018/19 season consisted of A(H1N1)pdm09 (36%), A
(H3N2) (56%), and type B (8%). Based on the Japanese sentinel surveillance report, the esti-
mated number of influenza patients, including adults and children, who visited medical facili-
ties between week 36 of 2018 and week 17 of 2019 was approximately 12 million, meaning that
Fig 1. Number of patients tested by rapid influenza diagnostic tests by week in the column chart (n = 4243). Epidemic curves for A(H1N1)
pdm09 and A(H3N2) by the World Health Organization in the line graph [16].
https://doi.org/10.1371/journal.pone.0249005.g001
PLOS ONE | https://doi.org/10.1371/journal.pone.0249005 March 26, 2021 5 / 12
PLOS ONE Influenza vaccine effectiveness in children, 2018/19
Table 2. Adjusted vaccine effectiveness (VE) of quadrivalent inactivated influenza vaccine for preventing influenza in the 2018/19 season (n = 4243). VE for pre-
venting influenza A (N = 4243).
Age group VE% (95% CI) Cases (vaccinated, unvaccinated) Cases vaccinated, % Controls [vaccinated, unvaccinated] Controls vaccinated, %
a, b
6 months–15 years 39 (30–46) (767, 1368) 36 [1037, 1061] 49
38 (29–46) a, b, c
6–11 months 63 (15–84) a (9, 57) 14 [38, 102] 27
1–2 years 56 (42–67) a (128, 211) 38 [401, 296] 58
3–5 years 49 (35–61) a (201, 329) 38 [303, 257] 54
6–12 years 25 (6–39) a (365, 615) 37 [255, 316] 45
13–15 years -5 (-74–37) a (64, 156) 29 [40, 90] 31
a. Adjusted for comorbidity (yes or no), area (northern, middle, or southern area of the Kanto region), month of onset
b. Adjusted for age (0–15 years old)
c. Adjusted for time tested after onset (<12, 12–48, and >48 h)
https://doi.org/10.1371/journal.pone.0249005.t002
the scale of the epidemic was rather large this season [17]. All A(H1N1)pdm09 strains isolated
were classified as 6B.1A, belonging to the same subclade of the vaccine strain A/Singapore/
GP1908/2015 (A(H1N1)pdm09), and most of the A(H3N2) strains isolated were classified as
3C.2a, also belonging to the same subclade of the vaccine strain, A/Singapore/INFIMH-16-
0019/2016 (A(H3N2)) [17].
Characteristics of the enrollees in the 2018/19 season
A total of 4243 children 6 months to 15 years old were enrolled in the 2018/19 season
(Table 1). Children who were hospitalized and children who were not hospitalized after diag-
nosis at outpatient clinics were included in these analyses. Among the 4243 enrollees who were
eligible for inclusion in the analysis in this study, 2145 were RIDT-positive, including 2135
with influenza A and 10 with influenza B, and 2098 were RIDT-negative. As only 10 cases with
influenza B were reported, VE against influenza B was not analyzed in this study.
Of the children with influenza A, 97% (1920/1987) had received an RIDT within 48 h of
onset. Ninety-seven percent (1994/2055) of the children with influenza A were treated with
antivirals (neuraminidase inhibitors or baloxavir) (Table 1). The overall vaccine coverage rates
were 36% (767/2135), 30% (3/10), and 49% (1037/2098) for influenza A-positive, B-positive,
and control patients (RIDT-negative), respectively (Table 1).
VE for preventing influenza illness
The adjusted VE for preventing influenza A illness was 39% (95% CI, 30%–46%, N = 4233)
(Table 2). The adjusted VE was 63% at 6 to 11 months (95% CI, 15%–84%, N = 206) and 56%
at 1 to 2 years old (95% CI, 42%–67%, N = 1036) compared with 25% at 6 to 12 years old (95%
Table 3. Adjusted vaccine effectiveness (VE) of quadrivalent inactivated influenza vaccine for preventing influenza in the 2018/19 season (n = 4243). Adjusted vac-
cine effectiveness (VE) of quadrivalent inactivated influenza vaccine for preventing influenza A(H1N1)pdm09 and A(H3N2) in 3 hospitals that used rapid influenza diag-
nostic test kits for detecting A(H1N1)pdm09 (N = 238).
Type of influenza VE% (95% CI) a Cases (vaccinated, unvaccinated) Cases vaccinated, % Controls [vaccinated, unvaccinated] Controls vaccinated, %
Influenza A 37 (-11–64) (54, 53) 50 [84, 47] 64
A(H1N1)pdm09 74 (39–89) (10, 26) 28 [84, 47] 64
A(H3N2) 7 (-77–51) (44, 27) 62 [84, 47] 64
a. Adjusted for comorbidity (yes or no), area (northern, middle, or southern area of the Kanto region), month of onset, and age (0–15 y/o).
https://doi.org/10.1371/journal.pone.0249005.t003
PLOS ONE | https://doi.org/10.1371/journal.pone.0249005 March 26, 2021 6 / 12
PLOS ONE Influenza vaccine effectiveness in children, 2018/19
Table 4. Adjusted vaccine effectiveness (VE) of quadrivalent inactivated influenza vaccine for preventing influenza hospitalization in the 2018/19 season.
Type of influenza VE% (95% CI) a Cases (vaccinated, unvaccinated) Cases vaccinated, % Controls [vaccinated, unvaccinated] Controls vaccinated, %
Influenza A 56 (16–77) (26, 48) 35 [71, 59] 55
a. Adjusted for comorbidity (yes or no), area (northern, middle, or southern area of the Kanto region), month of onset, and age (0–15 y/o).
https://doi.org/10.1371/journal.pone.0249005.t004
CI, 6%–39%, N = 1551) and -5% at 13 to 15 years old (not significant; 95% CI, -74%–37%,
N = 350).
Of the 238 cases in 3 hospitals, 36 (10 vaccinated and 26 unvaccinated) cases were A(H1N1)
pdm09-positive, 71 (44 vaccinated and 27 unvaccinated) cases were A(H1N1)pdm09-negative
(defined as A(H3N2)), and 131 cases were influenza-negative. The adjusted VE for preventing
influenza A was 37% (95% CI, -11%–64%, N = 238) by ImmunoAce FLU, and the adjusted VE for
preventing influenza A(H1N1)pdm09 was 74% (95% CI, 39%–89%, N = 167) by Linjudge FluA/
pdm. The VE in preventing influenza A(H3N2) was 7% (95% CI, -77%–51%, N = 202) (Table 3).
VE for preventing hospitalization against influenza A
There were 205 hospitalized children (74, 1, and 130 in influenza A, B, and RIDT-negative,
respectively), and 3929 were not hospitalized (2060, 9, and 1860 in influenza A, B, and RIDT-
negative, respectively) after diagnosis at outpatient clinics (Table 1). The adjusted VE for pre-
venting hospitalization was 56% (95% CI, 16%–77%) (Table 4). Among 204 hospitalized cases
and controls, the vaccine coverage was 35% (26/74) and 55% (71/130), respectively (Table 4).
Among the 74 hospitalized children with influenza A, 8 (11%) and 10 (13%) had underlying
neurological diseases (such as epilepsy) and respiratory diseases (such as asthma), respectively,
and 33 (67%, 33/49) had seizures on admission.
VE by vaccine dose (6 months–12 years old)
The number of enrollees among influenza-positive and influenza-negative children by age
group is shown in Table 5. In general, both the one- and two-dose regimens significantly
reduced cases with influenza A (Table 6, “one vs. none,” “two vs. none”). Only the two-dose
regimen was effective for preventing influenza A in 6 to 11 month olds (adjusted VE, 62%
[95% CI, 9%–84%]) (p-value <0.05) and in 3 to 5 year olds (adjusted VE, 53% [95% CI, 38%–
64%]) (Bonferroni-corrected α p-value <0.05/3). There was no significant difference between
the one- and two-dose regimens.
Discussion
In the 2018/19 season, a relatively low VE against influenza A (i.e., 39%; 95% CI, 30%–46%,
N = 4233) was shown in this study, when the ratio of isolated strains for A(H1N1)pdm09 and
Table 5. Adjusted vaccine effectiveness (VE) of quadrivalent inactivated influenza vaccine by vaccine dose for preventing influenza illness among children in the
2018/19 season. Number of enrollees.
Influenza A Positive, n (%) Influenza Negative, n (%)
vaccine doses 0 1 2 Total 0 1 2 Total
6–11 months old 57 (86) 2 (3) 7 (11) 66 (100) 102 (73) 5 (4) 33 (24) 140 (100)
1–2 years old 211 (63) 18 (5) 108 (32) 337 (100) 296 (43) 81 (12) 313 (45) 690 (100)
3–5 years old 329 (63) 46 (9) 151 (29) 526 (100) 257 (46) 52 (9) 248 (45) 557 (100)
6–12 years old 615 (63) 98 (10) 263 (27) 976 (100) 316 (55) 76 (13) 178 (31) 570 (100)
total 1212 (64) 164 (9) 529 (28) 1905 (100) 971 (50) 214 (11) 772 (39) 19570)
https://doi.org/10.1371/journal.pone.0249005.t005
PLOS ONE | https://doi.org/10.1371/journal.pone.0249005 March 26, 2021 7 / 12
PLOS ONE Influenza vaccine effectiveness in children, 2018/19
Table 6. Adjusted vaccine effectiveness (VE) of quadrivalent inactivated influenza vaccine by vaccine dose for pre-
venting influenza illness among children in the 2018/19 season. Adjusted vaccine effectiveness (VE) against influ-
enza A by vaccine dose.
Age groupa Vaccine doses VE% (95% CI)
6–11 months one vs. none 65 (-210–96)
two vs. none 62 (9–84)�
two vs. one -24 (-1223–89)
1–2 years old one vs. none 68 (43–82)��
two vs. none 53 (37–65)��
two vs. one -57 (-179–12)
3–5 years old one vs. none 34 (-2–58)
two vs. none 53 (38–64)��
two vs. one 27 (-15–54)
6–12 years old one vs. none 32 (5–52)�
two vs. none 23 (2–39)�
two vs. one -13 (-63–21)
6 months–2 years old one vs. none 66 (42–80)��
(for 0.25 ml/dose) two vs. none 51 (37–63)��
two vs. one -51 (-164–14)
Total b one vs. none 41 (26–53)��
two vs. none 42 (32–50)��
two vs. one -9 (-40–15)
a. Adjusted for comorbidity (yes or no), area (northern, middle, or southern area of the Kanto region), month of
onset
b. Adjusted for comorbidity (yes or no), area (northern, middle, or southern area of the Kanto region), month of
onset, and age
�
p-value <0.05
��
p-value <0.05/3 = 0.017 (Bonferroni-corrected)
https://doi.org/10.1371/journal.pone.0249005.t006
A(H3N2) was approximately 40% vs. 60% in Japan [17]. Although the VE against influenza A
(H1N1)pdm09 was high (74%; 95% CI, 39%–89%, N = 167), the VE against influenza A
(H3N2) was very low (7%; 95% CI, -77%–51%, N = 202). Therefore, the low VE against influ-
enza A was probably due to a markedly reduced VE against influenza A(H3N2).
Although we previously reported low VEs against influenza A infection during influenza
epidemics mostly caused by the A(H3N2) subtype, such as 37% in 2014/15 (99% of influenza
A strains identified were A(H3N2)) [4] and 38% in 2016/17 (97% of influenza A strains identi-
fied were A(H3N2)) [6], the degree of reduction in the VE against influenza A was not as
extensive in children. Based on our experience, we concluded that the VE of IIV against A
(H3N2) was low but still effective in children. In contrast, the VE against A(H3N2) was very
low or not significant in adults in recent seasons [18, 19]. We recognized for the first time in
this study that the very low VE against A(H3N2) was a serious problem not only in adults but
also in children in the 2018/19 season.
In the 2018/19 season, the antigenicity of most A(H3N2) strains isolated in Japan was simi-
lar to the vaccine strain A/Singapore/INFIMH-16-0019/2016 (A(H3N2)) (genetic clade
3C.2a1) [17]. However, mutations in the egg-adapted vaccine strain of the A/Singapore/
INFIMH-16-0019/2016 (A(H3N2)) were suspected, which may lead to very low or no VE [17].
The VE against A(H1N1)pdm09 was consistently high in our studies. We previously
reported high VEs against A(H1N1)pdm09, such as 77% in the 2013/14 season, using RIDT
PLOS ONE | https://doi.org/10.1371/journal.pone.0249005 March 26, 2021 8 / 12
PLOS ONE Influenza vaccine effectiveness in children, 2018/19
kits specifically for detecting A(H1N1)pdm09, and the VE increased with age: from 67% in the
1- to 2-year-old group, to 84% in the 3- to 5-year-old group, and 90% in the 6- to 12-year-old
group [3]. A Clearline Influenza A/B/(H1N1)2009 kit (Alere Medical Co., Ltd., Tokyo, Japan)
or the combination of ImunoAce Flu and Linjudge FluA/pdm was used to detect A(H1N1)
pdm09 [3], but the former has since been withdrawn due to unstable results. According to the
antigenic analysis of A(H1N1)pdm09 strains, the antigenicity of most isolated strains was simi-
lar to that of the vaccine strain A/Singapore/GP1908/2015 (A(H1N1)pdm09) (A/Michigan/45/
2015-like) (genetic clade 6B.1) in the 2018/19 season [17].
Because we used RIDTs, digital immunoassays, or even rapid nucleic acid amplification
tests, we were unable to diagnose influenza A subtypes separately, except when RT-PCR was
performed. We believe that the combination of ImunoAce Flu and Linjudge FluA/pdm is
highly useful for distinguishing between influenza A subtypes compared with RT-PCR,
although the sensitivity and specificity of the combination of tests is lower than with RT-PCR
[10]. This combination of tests obtains results much more quickly than RT-PCR, and numer-
ous samples can be tested at the same time. The most important point is its cost, which, at
approximately USD$10 per test, is much cheaper than RT-PCR [10].
Using RT-PCR, high VE against A(H1N1)pdm09 in children was reported worldwide in
the 2018/19 season. In the US, where most of the isolated influenza type A strains were A
(H1N1)pdm09, the VE against A(H1N1)pdm09 in children 6 months to 17 years old was 62%
[20]. In Canada, the VE against A(H1N1)pdm09 in children 1 to 8 years old was as high as
91% [21]. In contrast, a low or non-significant VE against A(H3N2) in this season was also
reported among adults and children [18, 19].
In the present study, the VE for children 6 to 11 months old was shown to be the highest
among all age groups, although the VE in this age group has not been statistically significant in
our previous studies. It is generally thought that, in children 6 to 11 months old, the VE may
be lower than in older groups because the vaccine-induced antibody response is immature
[22]. However, it was reported that the VE of two doses of trivalent IIV in subjects 6 months to
<1 year old for the 2002/03 to 2007/08 seasons was the highest among all age groups [23].
More studies are needed to assess VE in infants 6 to 11 months old.
Although a meta-analysis showed no convincing evidence that the influenza vaccine
reduces mortality, hospitalization rates, or serious complications in children [24], we reported
that, in four of the five seasons from 2013 to 2018, the VEs for preventing hospitalization were
significantly effective [3–5], and the five-season VEs for preventing hospitalization for any
influenza, influenza A, and influenza B were 46% (95% CI, 33%–56%), 50% (95% CI, 36%–
60%), and 31% (95% CI, 4%–51%), respectively [7]. Furthermore, in the present study, the
adjusted VE for preventing hospitalization against influenza A was 56% (95% CI, 16%–77%,
N = 205), regardless of the relatively low VE for preventing illness against influenza A (39%).
Therefore, we presume that influenza vaccination is more important for preventing severe
influenza than for preventing influenza illness altogether.
Another observation was that only a two-dose regimen was effective against influenza A in
children 3 to 5 years old. In our combined analysis of five seasons (2013/14–2017/18), both
one- and two-dose regimens were effective against influenza A in all seasons [7]. The low effec-
tiveness of a single dose against influenza A in children 3 to 5 years old was likely caused by
the very low VE against influenza A(H3N2), which was only 7% in this recent season. We
believe that a two-dose regimen is appropriate in younger children, because the one-dose regi-
men has not always been found effective in our studies. This is consistent with previous find-
ings [22, 25, 26].
The major limitation of our past studies has been that our diagnostic tools are RIDTs, not
RT-PCR. The sensitivity of RIDTs was recently reported to be as low as 42.6% for influenza A
PLOS ONE | https://doi.org/10.1371/journal.pone.0249005 March 26, 2021 9 / 12
PLOS ONE Influenza vaccine effectiveness in children, 2018/19
and 33.2% for influenza B in adult patients, leading to a deep distrust of RIDTs in the world
medical community [8], although there was an issue in that report, with the timing of the sam-
ple collection for the RIDTs was not mentioned. This is relevant, as the sensitivity of RIDTs is
dependent on the viral load in the upper respiratory tract, and the viral titers of patients with
influenza virus infection in the upper respiratory tract peak during the first couple of days
after the onset of influenza infection before declining to undetectable levels within a week [27].
In contrast, in Japan, during the 2009 H1N1 pandemic, the sensitivity and specificity of the
RIDT (Prolast Flu AB, Mitsubishi Chemical Medience Corporation, Tokyo, Japan) was deter-
mined to be 80.0% and 97.1% in adults and children, compared with RT-PCR [9]. In 2020,
very high sensitivity, such as 97.1% of a widely used RIDT (ImunoAce Flu; TAUNS Laborato-
ries, Inc., Shizuoka, Japan) was reported in adults [10]. Moreover, the WHO Agenda for Public
Health noted that the reliability of rapid tests in Japan seems to be higher than that in other
countries, as most patients are tested within 48 h of the onset of illness [28]. Although the
imperfect specificity of RIDT contributes to bias in the test-negative design, VE studies using
RIDT have been reported [29, 30].
In conclusion, during the mixed influenza A subtype epidemic in the 2018/19 season, the
VE against influenza A was low (39%), but the VE against influenza A(H1N1)pdm09 was high
(74%). By contrast, the VE against influenza A(H3N2) was very low (7%). This very low VE
against A(H3N2) was a serious problem not only in adults but also in children and was attrib-
uted to mutations in the egg-adapted vaccine strain of A/Singapore/INFIMH-16-0019/2016 (A
(H3N2)) as observed or reported previously [18, 19, 31, 32]. Non-egg-based influenza vaccines
including cell-culture vaccines and those with nucleic acid technologies are promising [33].
Acknowledgments
This study would not have been possible without the excellent support from all the doctors of
members of the Keio Pediatric Influenza Research Group [3–7].
Author Contributions
Conceptualization: Norio Sugaya, Yoshio Yamaguchi, Shinichiro Sekiguchi, Chiharu Kawa-
kami, Keiko Mitamura, Takao Takahashi.
Data curation: Masayoshi Shinjoh, Yoshio Yamaguchi, Ichiro Ookawara, Yuji Nakata, Atsushi
Narabayashi, Munehiro Furuichi, Naoko Yoshida, Akinobu Kamei, Yuu Kuramochi, Aki-
michi Shibata, Motoko Shimoyamada, Hisataka Nakazaki, Naohiko Maejima, Erika Yuasa,
Eriko Araki, Naonori Maeda, Takuma Ohnishi, Mitsuhiro Nishida, Nobuhiko Taguchi,
Makoto Yoshida, Meiwa Shibata, Keiko Mitamura.
Formal analysis: Norio Sugaya, Nobuhiko Taguchi, Shinichiro Sekiguchi.
Investigation: Masayoshi Shinjoh, Norio Sugaya, Yoshio Yamaguchi, Atsushi Narabayashi,
Munehiro Furuichi, Naoko Yoshida, Akinobu Kamei, Yuu Kuramochi, Akimichi Shibata,
Motoko Shimoyamada, Naohiko Maejima, Erika Yuasa, Eriko Araki, Naonori Maeda,
Takuma Ohnishi, Mitsuhiro Nishida, Makoto Yoshida, Kenichiro Tsunematsu, Meiwa Shi-
bata, Yasuhiro Hirano.
Methodology: Masayoshi Shinjoh, Yoshio Yamaguchi, Atsushi Narabayashi, Hisataka Naka-
zaki, Naonori Maeda, Yasuhiro Hirano.
Project administration: Norio Sugaya, Ichiro Ookawara, Takao Takahashi.
Software: Yuji Nakata, Takuma Ohnishi.
PLOS ONE | https://doi.org/10.1371/journal.pone.0249005 March 26, 2021 10 / 12
PLOS ONE Influenza vaccine effectiveness in children, 2018/19
Supervision: Norio Sugaya, Yoshio Yamaguchi, Chiharu Kawakami, Keiko Mitamura, Takao
Takahashi.
Validation: Yoshio Yamaguchi, Mitsuhiro Nishida, Kenichiro Tsunematsu, Keiko Mitamura,
Takao Takahashi.
Writing – original draft: Masayoshi Shinjoh, Norio Sugaya.
Writing – review & editing: Masayoshi Shinjoh, Norio Sugaya.
References
1. Sugaya N. Widespread use of neuraminidase inhibitors in Japan. J Infect Chemother. 2011; 17(5):
595–601. https://doi.org/10.1007/s10156-011-0288-0 PMID: 21850418
2. Sugaya N, Shinjoh M, Mitamura K, Takahashi T. Very low pandemic influenza A (H1N1) 2009 mortality
associated with early neuraminidase inhibitor treatment in Japan: analysis of 1000 hospitalized children.
J Infect. 2011; 63(4): 288–294. https://doi.org/10.1016/j.jinf.2011.06.008 PMID: 21722665
3. Shinjoh M, Sugaya N, Yamaguchi Y, Tomidokoro Y, Sekiguchi S, Mitamura K, et al. Effectiveness of tri-
valent inactivated influenza vaccine in children estimated by a test-negative case-control design study
based on influenza rapid diagnostic test results. PLoS ONE. 2015; 10(8): e0136539. https://doi.org/10.
1371/journal.pone.0136539 PMID: 26317334
4. Sugaya N, Shinjoh M, Kawakami C, Yamaguchi Y, Yoshida M, Baba H, et al. Trivalent inactivated influ-
enza vaccine effective against influenza A(H3N2) variant viruses in children during the 2014/15 season,
Japan. Euro Surveill. 2016; 21(42): 30377. https://doi.org/10.2807/1560-7917.ES.2016.21.42.30377
PMID: 27784529
5. Sugaya N, Shinjoh M, Nakata Y, Tsunematsu K, Yamaguchi Y, Komiyama O, et al. Three-season effec-
tiveness of inactivated influenza vaccine in preventing influenza illness and hospitalization in children in
Japan, 2013–2016. Vaccine. 2018; 36(8): 1063–1071. https://doi.org/10.1016/j.vaccine.2018.01.024
PMID: 29361343
6. Shinjoh M, Sugaya N, Yamaguchi Y, Iibuchi N, Kamimaki I, Goto A, et al. Inactivated influenza vaccine
effectiveness and 435 an analysis of repeated vaccination for children during the 2016/17 season. Vac-
cine. 2018; 36(37): 5510–5518. https://doi.org/10.1016/j.vaccine.2018.07.065 PMID: 30093289
7. Shinjoh M, Sugaya N, Furuichi M, Araki E, Maeda N, Isshiki K, et al. Effectiveness of inactivated influ-
enza vaccine in children by vaccine dose, 2013–18. Vaccine. 2019; 37(30): 4047–4054. https://doi.org/
10.1016/j.vaccine.2019.05.090 PMID: 31186191
8. Merckx J, Wali R, Schiller I, Caya C, Gore GC, Chartrand C, et al. Diagnostic accuracy of novel and tra-
ditional rapid tests for influenza infection compared with reverse transcriptase polymerase chain reac-
tion: a systematic review and meta-analysis. Ann Intern Med. 2017; 167(6): 394–409. https://doi.org/10.
7326/M17-0848 PMID: 28869986
9. Harada D, Nishiuchi R, Iwasaki Y, Watanabe H, Tokorodani C, Kanazawa A, et al. Reliability of a rapid
test for the clinical diagnosis of influenza A/H1N1 2009. Scand J Infect Dis. 2012; 44(10):776–81.
https://doi.org/10.3109/00365548.2012.686670 PMID: 22803629
10. Seki Y, Oda Y, Sugaya N. Very high sensitivity of a rapid influenza diagnostic test in adults and elderly
individuals within 48 hours of the onset of illness. PLoS ONE 2020; 15(5): e0231217. https://doi.org/10.
1371/journal.pone.0231217 PMID: 32374728
11. Kimiya T, Shinjoh M, Anzo M, Takahashi H, Sekiguchi S, Sugaya N, et al. Effectiveness of inactivated
quadrivalent influenza vaccine in the 2015/2016 season as assessed in both a test-negative case-con-
trol study design and a traditional case-control study design. Europ J Ped. 2018; 177(7): 1009–1017.
https://doi.org/10.1007/s00431-018-3145-7 PMID: 29680993
12. McCullers JA. Influenza Viruses. In: James D. Cherry MD HG, Kaplan SL, Steinbach WJ Hotez PJ, edi-
tor. Feigin and Cherry’s textbook of pediatric infectious diseases. 8th ed. Philadelphia: Elsevier;
2019. pp. 1729–1745.
13. Nakamura Y. Maternal and child health handbook in Japan. JMAJ. 2010; 53(4): 259–265.
14. Ministry of Health Labour and Japan Welfare. Influenza Vaccination, Japan [Ministry of Health, Labour
and Welfare web site]. Available at: https://www.mhlw.go.jp/bunya/kenkou/kekkaku-kansenshou01/qa_
eng.html.
15. Pharmaceuticals and Medical Devices Agency (PMDA) Japan. Japanese interview form of inactivated
influenza vaccine (In Japanese). [PMDA web site]. Available at: https://www.info.pmda.go.jp/go/pack/
631340FA1047_1_31/.
PLOS ONE | https://doi.org/10.1371/journal.pone.0249005 March 26, 2021 11 / 12
PLOS ONE Influenza vaccine effectiveness in children, 2018/19
16. World Health Organization. Influenza Laboratory Surveillance Information. Data source: FluNet (www.
who.int/flunet), Global Influenza Surveillance and Response System (GISRS). Available at: http://apps.
who.int/flumart/Default?ReportNo=12.
17. The National Institute of Infectious Diseases. Influenza 2018/19 season, Japan. Available at: https://
www.niid.go.jp/niid/en/iasr/865-iasr/9288-477te.html.
18. Skowronski DM, Sabaiduc S, Leir S, Rose C, Zou M, Murti M, et al. Paradoxical clade- and age-specific
vaccine effectiveness during the 2018/19 influenza A(H3N2) epidemic in Canada: potential imprint-reg-
ulated effect of vaccine (I-REV). Euro Surveill. 2019; 24(46): 1900585. https://doi.org/10.2807/1560-
7917.ES.2019.24.46.1900585 PMID: 31771709
19. Kissling E, Pozo F, Buda S, Vilcu AM, Gherasim A, Brytting M, et al. Low 2018/19 vaccine effectiveness
against influenza A(H3N2) among 15-64-year-olds in Europe: exploration by birth cohort. Euro Surveill.
2019; 24(48): 1900604. https://doi.org/10.2807/1560-7917.ES.2019.24.48.1900604 PMID: 31796152
20. Doyle JD, Chung JR, Kim SS, Gaglani M, Raiyani C, Zimmerman RK, et al. Interim estimates of 2018–
19 seasonal influenza vaccine effectiveness—United States, February 2019. MMWR Morb Mortal Wkly
Rep. 2019; 68(6): 135–139. https://doi.org/10.15585/mmwr.mm6806a2 PMID: 30763298
21. Skowronski DM, Leir S, Sabaiduc S, Murti M, Dickinson JA, Olsha R, et al. Interim estimates of 2018/19
vaccine effectiveness against influenza A(H1N1)pdm09, Canada, January 2019. Euro Surveill. 2019;
24(4): 1900055. https://doi.org/10.2807/1560-7917.ES.2019.24.4.1900055 PMID: 30696523
22. Ito K, Mugitani A, Irie S, Ishibashi M, Takasaki Y, Shindo S, et al. Prior vaccinations improve immunoge-
nicity of inactivated influenza vaccine in young children aged 6 months to 3 years: A cohort study. Medi-
cine. 2018; 97(29): e11551. https://doi.org/10.1097/MD.0000000000011551 PMID: 30024549
23. Katayose M, Hosoya M, Haneda T, Yamaguchi H, Kawasaki Y, Sato M, et al. The effectiveness of triva-
lent inactivated influenza vaccine in children over six consecutive influenza seasons. Vaccine. 2011; 29
(9): 1844–1849. https://doi.org/10.1016/j.vaccine.2010.12.049 PMID: 21195802
24. Jefferson T, Rivetti A, Di Pietrantonj C, Demicheli V. Vaccines for preventing influenza in healthy chil-
dren. Cochrane Database Syst Rev. 2018;2(2): Cd004879. https://doi.org/10.1002/14651858.
CD004879.pub5 PMID: 29388195
25. Segaloff HE, Leventer-Roberts M, Riesel D, Malosh RE, Feldman BS, Shemer-Avni Y, et al. Influenza
vaccine effectiveness against hospitalization in fully and partially vaccinated children in Israel; 2015–16,
2016–17, and 2017–18. Clin Infect Dis 2019; 69(12): 2153–2161. https://doi.org/10.1093/cid/ciz125
PMID: 30753347
26. Thompson MG, Clippard J, Petrie JG, Jackson ML, McLean HQ, Gaglani M, et al. Influenza vaccine
effectiveness for fully and partially vaccinated children 6 months to 8 years old during 2011–2012 and
2012–2013: the importance of two priming doses. Pediatr Infect Dis J 2016; 35: 299–308. https://doi.
org/10.1097/INF.0000000000001006 PMID: 26658375
27. Ip DKM, Lau LLH, Chan KH, Fang VJ, Leung GM, Peiris MJS, et al. the dynamic relationship between
clinical symptomatology and viral shedding in naturally acquired seasonal and pandemic influenza virus
infections. Clin Infect Dis. 2016; 62(4): 431–437. https://doi.org/10.1093/cid/civ909 PMID: 26518469
28. World Health Organization. WHO public health research agenda for influenza: optimizing treatment of
patients, 2017 update. [WHO web site]. 2017. Available at: https://apps.who.int/iris/handle/10665/
259887.
29. Jackson ML, Rothman KJ. Effects of imperfect test sensitivity and specificity on observational studies of
influenza vaccine effectiveness. Vaccine 2015; 33: 1313–1316. https://doi.org/10.1016/j.vaccine.2015.
01.069 PMID: 25659280
30. Orenstein EW, De Serres G, Haber MJ, Shay DK, Bridges CB, Gargiullo P, et al. Methodologic issues
regarding the use of three observational study designs to assess influenza vaccine effectiveness. Int J
Epidemiol 2007; 36: 623–631. https://doi.org/10.1093/ije/dym021 PMID: 17403908
31. Kissling K. E, Rose A, Emborg H-D, Gherasim A, Pebody R, Pozo F, et al. Interim 2018/19 influenza
vaccine effectiveness: six European studies, October 2018 to January 2019. Euro Surveill 2019; 24:
1900121. https://doi.org/10.2807/1560-7917.ES.2019.24.1900121 PMID: 30808440
32. Flannery B, Kondor RJG, Chung JR, Gaglani M, Reis M, Zimmerman RK, et al. Spread of antigenically
drifted influenza A(H3N2) viruses and vaccine effectiveness in the United States during the 2018–2019
season. J Infect Dis 2019; 221: 8–15. https://doi.org/10.1093/infdis/jiz543 PMID: 31665373
33. Rockman S, Laurie KL, Parkes S, Wheatley A, Barr IG. New technologies for influenza vaccines. Micro-
organisms. 2020; 8: 1745. https://doi.org/10.3390/microorganisms8111745 PMID: 33172191
PLOS ONE | https://doi.org/10.1371/journal.pone.0249005 March 26, 2021 12 / 12
You might also like
- Living on the Frontline of COVID-19 in MCO And CMCO: Clinical Updates in COVID-19From EverandLiving on the Frontline of COVID-19 in MCO And CMCO: Clinical Updates in COVID-19No ratings yet
- 10 1016@j Vaccine 2019 05 090Document8 pages10 1016@j Vaccine 2019 05 090Muhammad Imam NoorNo ratings yet
- Honk R3Document29 pagesHonk R3fitri asymidaNo ratings yet
- Ohnishi 2021Document5 pagesOhnishi 2021As MaaNo ratings yet
- Intussusception Among Japanese Children: An Epidemiologic Study Using An Administrative DatabaseDocument6 pagesIntussusception Among Japanese Children: An Epidemiologic Study Using An Administrative DatabaseCasey CameronNo ratings yet
- Journal Pre-Proof: International Journal of Infectious DiseasesDocument44 pagesJournal Pre-Proof: International Journal of Infectious DiseasesIoana BiticaNo ratings yet
- 10 1016@j Jiac 2017 02 014Document12 pages10 1016@j Jiac 2017 02 014Achmad YunusNo ratings yet
- Title: Improvement in The Appropriate Antimicrobial Usage For Treating PediatricDocument23 pagesTitle: Improvement in The Appropriate Antimicrobial Usage For Treating PediatricSofia Marie GalendezNo ratings yet
- Acceptance of A COVID-19 VacciDocument12 pagesAcceptance of A COVID-19 VacciahmadNo ratings yet
- Effects of Pneumococcal Conjugate Vaccine On Genotypic Penicillin Resistance and Serotype Changes, Japan, 2010-2017Document11 pagesEffects of Pneumococcal Conjugate Vaccine On Genotypic Penicillin Resistance and Serotype Changes, Japan, 2010-2017Ana-Mihaela BalanuțaNo ratings yet
- The Association Between Motivation Prevention and Acceptance Vaccine Services For Prevention and Control of The COVID-19 On University Students in ThailandDocument5 pagesThe Association Between Motivation Prevention and Acceptance Vaccine Services For Prevention and Control of The COVID-19 On University Students in ThailandInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Epidemiology and InfectionDocument11 pagesEpidemiology and Infectionhasemana hasemanaNo ratings yet
- Fmed 08 691079Document6 pagesFmed 08 691079Andri Alhin putraNo ratings yet
- ARDSDocument9 pagesARDSrayalarasatitiNo ratings yet
- Changes in Childhood Vaccination During The Coronavirus Disease 2 - 2021 - VacciDocument7 pagesChanges in Childhood Vaccination During The Coronavirus Disease 2 - 2021 - VacciProfessor BiologiaNo ratings yet
- Spatial and Temporal Analysis of Dengue Infections in Queensland, Australia Recent Trend and PerspectivesDocument18 pagesSpatial and Temporal Analysis of Dengue Infections in Queensland, Australia Recent Trend and PerspectivesTenIs ForMeNo ratings yet
- The Rationality of Antibiotics Therapy Toward Children With Typhoid Fever at M.M. Dunda HospitalDocument4 pagesThe Rationality of Antibiotics Therapy Toward Children With Typhoid Fever at M.M. Dunda HospitalaisyahNo ratings yet
- Tugas PPD 1: Nama: Norwicha Rahmasari Putri NPM: 1102019156 Kelas: FK - B Dosen AkademikDocument13 pagesTugas PPD 1: Nama: Norwicha Rahmasari Putri NPM: 1102019156 Kelas: FK - B Dosen Akademikdhea1angela1putriNo ratings yet
- ExperimentalDocument6 pagesExperimentalDiego TorresNo ratings yet
- FavipiravirDocument9 pagesFavipiravirStephen JessicaNo ratings yet
- Acceptance of A COVID19 Vaccine in Southeast Asia A CrossSectional Study in IndonesiaDocument8 pagesAcceptance of A COVID19 Vaccine in Southeast Asia A CrossSectional Study in IndonesiaAntonio MoncayoNo ratings yet
- Ciy 866Document47 pagesCiy 866Ma. Bernadette PinedaNo ratings yet
- Eclinicalmedicine: Research PaperDocument8 pagesEclinicalmedicine: Research PaperHendris CitraNo ratings yet
- Epidemiology and Clinical Profile of PIMS-TS. Dhanalakshmi Ind Pediatr Aug 2020Document10 pagesEpidemiology and Clinical Profile of PIMS-TS. Dhanalakshmi Ind Pediatr Aug 2020Bala RamachandranNo ratings yet
- Low Anti Rubella Antibody Levels in Public FacilitDocument1 pageLow Anti Rubella Antibody Levels in Public FacilitSimbakutty VenkataramananNo ratings yet
- Dengue Pre Vaccination Screening and Positive PredDocument3 pagesDengue Pre Vaccination Screening and Positive PredSimbakutty VenkataramananNo ratings yet
- Etm 20 6 9260 PDFDocument7 pagesEtm 20 6 9260 PDFLina UkagoNo ratings yet
- Evidence-Based Clinical Practice Guideline For Adult Still's DiseaseDocument54 pagesEvidence-Based Clinical Practice Guideline For Adult Still's DiseaseNancy ManriqueNo ratings yet
- 21707-Article Text-40436-1-10-20181220Document5 pages21707-Article Text-40436-1-10-20181220apriliaviskaNo ratings yet
- Virus Influenza Guidlines PDFDocument47 pagesVirus Influenza Guidlines PDFМарија СерафимовскаNo ratings yet
- Efficacy and Safety of SildenafilDocument9 pagesEfficacy and Safety of SildenafilArif Nurhadi AtmokoNo ratings yet
- Ppe-2 ReviewDocument14 pagesPpe-2 ReviewSajin AlexanderNo ratings yet
- Ciy 866Document47 pagesCiy 866Skripsi ulmNo ratings yet
- Managemen OMADocument8 pagesManagemen OMAHefieNo ratings yet
- Pedsos 1Document7 pagesPedsos 1RizalMarubobSilalahiNo ratings yet
- Tranilast As An Adjunctive Therapy in Hospitalized Patients With Severe COVID - 19 - A Randomized Controlled TrialDocument10 pagesTranilast As An Adjunctive Therapy in Hospitalized Patients With Severe COVID - 19 - A Randomized Controlled TrialMax JaksicNo ratings yet
- Difyeri IndiaDocument5 pagesDifyeri IndiaDian Fajar FebrianiNo ratings yet
- Efficacy DSS - NCBI PDFDocument12 pagesEfficacy DSS - NCBI PDFKindy AgustinNo ratings yet
- A Comparative-Descriptive Analysis of Clinical Characteristics in 2019-Coronavirus-Infected Children and AdultsDocument28 pagesA Comparative-Descriptive Analysis of Clinical Characteristics in 2019-Coronavirus-Infected Children and AdultsPatrick NunsioNo ratings yet
- Profile of Antibiotic Use in Pediatric Patients With Pneumonia at Dr. M. Djamil Hospital Padang, West Sumatra, IndonesiaDocument4 pagesProfile of Antibiotic Use in Pediatric Patients With Pneumonia at Dr. M. Djamil Hospital Padang, West Sumatra, IndonesiaInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Prof. Erlina Burhan - CVDocument18 pagesProf. Erlina Burhan - CVgmsmsuNo ratings yet
- 1 BP Com Academic Write UpDocument8 pages1 BP Com Academic Write UpRenzelle MelisseNo ratings yet
- Journal Read ChiaDocument14 pagesJournal Read ChiaChris Tine ChiaNo ratings yet
- Pmed 1003208Document23 pagesPmed 1003208Nindie AulhieyaNo ratings yet
- JurnalDocument7 pagesJurnalRahmi SilviyaniNo ratings yet
- Epidemiology Characteristics of Streptococcus Pneumoniae From Children With Pneumonia in Shanghai: A Retrospective StudyDocument10 pagesEpidemiology Characteristics of Streptococcus Pneumoniae From Children With Pneumonia in Shanghai: A Retrospective StudyAna-Mihaela BalanuțaNo ratings yet
- Tugas Bahasa Inggris Jurnal Internasional: OlehDocument11 pagesTugas Bahasa Inggris Jurnal Internasional: Olehgekayu sartikaNo ratings yet
- Ventilator Associated Pneumonia: Incidence, Profile and Outcome in Pediatric Intensive Care Unit of Tertiary Care CentreDocument5 pagesVentilator Associated Pneumonia: Incidence, Profile and Outcome in Pediatric Intensive Care Unit of Tertiary Care CentreJoaquín SosaNo ratings yet
- 9f3d5d3d-0802-4661-98fe-6d2d6a6208a5Document11 pages9f3d5d3d-0802-4661-98fe-6d2d6a6208a5Yeol LoeyNo ratings yet
- Jurnal 2Document7 pagesJurnal 2zarazobellaNo ratings yet
- Rituximab TrialDocument9 pagesRituximab TrialsrildaNo ratings yet
- Mortality Study NepalDocument9 pagesMortality Study Nepalanindya_sNo ratings yet
- Pediatric Pulmonology - 2021 - Ullmann - Effects of The COVID 19 Pandemic and Lockdown On Symptom Control in PreschoolDocument5 pagesPediatric Pulmonology - 2021 - Ullmann - Effects of The COVID 19 Pandemic and Lockdown On Symptom Control in Preschoolyunike M KesNo ratings yet
- Ijcp 13891Document24 pagesIjcp 13891tugasdianok2No ratings yet
- Aniwada 1332015 BJMMR23249 DSNDocument11 pagesAniwada 1332015 BJMMR23249 DSNelias aniwadaNo ratings yet
- Evaluation of Drug Utilization Pattern of Antimicrobial Agents in Hyderabad Adult Patients of Otorhinolaryngology ENT, in A Tertiary Care Teaching Hospital TelanganaDocument5 pagesEvaluation of Drug Utilization Pattern of Antimicrobial Agents in Hyderabad Adult Patients of Otorhinolaryngology ENT, in A Tertiary Care Teaching Hospital TelanganaEditor IJTSRDNo ratings yet
- Clinico-Epidemiological Profile and Predictors of Outcome in Children With Diphtheria: A Study From Northern IndiaDocument6 pagesClinico-Epidemiological Profile and Predictors of Outcome in Children With Diphtheria: A Study From Northern IndiamariaprincesitaNo ratings yet
- Coronavirus Disease 2019 Related Clinical Studies: A Cross-Sectional AnalysisDocument8 pagesCoronavirus Disease 2019 Related Clinical Studies: A Cross-Sectional AnalysisMARY JANE BERMUDONo ratings yet
- Control Neonatal Coronavirus PDFDocument8 pagesControl Neonatal Coronavirus PDFAlways MusicNo ratings yet
- Review of Trial Therapies and Treatment For COVID-19: Lessons For IndonesiaDocument6 pagesReview of Trial Therapies and Treatment For COVID-19: Lessons For IndonesiaAri SudarsonoNo ratings yet
- European Journal of Epidemiology 2016Document5 pagesEuropean Journal of Epidemiology 2016cdsaludNo ratings yet
- Journal of Homosexuality 2012Document22 pagesJournal of Homosexuality 2012cdsaludNo ratings yet
- Plast Reconstr Surg Glob OpenDocument12 pagesPlast Reconstr Surg Glob OpencdsaludNo ratings yet
- J Skin Stem Cell. 2022 June 9 (2) E126321Document6 pagesJ Skin Stem Cell. 2022 June 9 (2) E126321cdsaludNo ratings yet
- Best Practive Clinical 2021Document17 pagesBest Practive Clinical 2021cdsaludNo ratings yet
- Clinical Pharmacy Therapeu - 2022 - Ding - Management of Biologics in Pregnant Lactating Patients With Inflammatory BowelDocument14 pagesClinical Pharmacy Therapeu - 2022 - Ding - Management of Biologics in Pregnant Lactating Patients With Inflammatory BowelcdsaludNo ratings yet
- Pediatr Clin North Am 2023 Tabla de ContenidoDocument4 pagesPediatr Clin North Am 2023 Tabla de ContenidocdsaludNo ratings yet
- Vaccines Ofr Adults 2021Document15 pagesVaccines Ofr Adults 2021cdsaludNo ratings yet
- Bris JR Hematol 2020Document18 pagesBris JR Hematol 2020cdsaludNo ratings yet
- E20201433 FullDocument15 pagesE20201433 FullcdsaludNo ratings yet
- Techical Reporte Adult VaccinationDocument55 pagesTechical Reporte Adult VaccinationcdsaludNo ratings yet
- GPC 475 Bronchiolitis AIAQS Compl enDocument125 pagesGPC 475 Bronchiolitis AIAQS Compl encdsaludNo ratings yet
- Clin Infect Dis 2009Document59 pagesClin Infect Dis 2009cdsaludNo ratings yet
- Mayo Clinic Proceedings 2021Document15 pagesMayo Clinic Proceedings 2021cdsaludNo ratings yet
- Ped Infect Disease Jr. 2023Document4 pagesPed Infect Disease Jr. 2023cdsaludNo ratings yet
- Syphilis World Health OrganizationDocument9 pagesSyphilis World Health OrganizationcdsaludNo ratings yet
- Aluminum and Vaccines Current State of KnowledgeDocument6 pagesAluminum and Vaccines Current State of KnowledgecdsaludNo ratings yet
- (19330715 - Journal of Neurosurgery 12Document7 pages(19330715 - Journal of Neurosurgery 12cdsaludNo ratings yet
- Interim Clinical Considerations For Use of COVID-19 Vaccines - Appendices, References, and Previous Updates - CDCDocument17 pagesInterim Clinical Considerations For Use of COVID-19 Vaccines - Appendices, References, and Previous Updates - CDCcdsaludNo ratings yet
- Drug Des Devel Ther 2009Document10 pagesDrug Des Devel Ther 2009cdsaludNo ratings yet
- Sindrome de ReyeDocument5 pagesSindrome de ReyecdsaludNo ratings yet
- MMWR Morb Mortal Wkly Rep 2023Document5 pagesMMWR Morb Mortal Wkly Rep 2023cdsaludNo ratings yet
- FFFFFFF: Health Declaration Form Health Declaration Form Health Declaration FormDocument1 pageFFFFFFF: Health Declaration Form Health Declaration Form Health Declaration FormLeny Goyo LaurenteNo ratings yet
- JKN Ketentuan RanapDocument8 pagesJKN Ketentuan RanapIkeNo ratings yet
- Laporan Obat Sesuai Foemularium Februari 2019Document24 pagesLaporan Obat Sesuai Foemularium Februari 2019Maria AmabiNo ratings yet
- Communicable Disease ActivitiesDocument11 pagesCommunicable Disease ActivitiesPlacida Mequiabas National High SchoolNo ratings yet
- 4 Thorax LungDocument1 page4 Thorax Lungconnie cNo ratings yet
- Register Meranti 2018Document178 pagesRegister Meranti 2018Rifat Bow AbdilahNo ratings yet
- Progressive Primary Pulmonary TB in A 15-Month Old ChildDocument1 pageProgressive Primary Pulmonary TB in A 15-Month Old ChildRenierose AgujetasNo ratings yet
- Cold vs. Flu vs. Allergies vs. COVID-19Document1 pageCold vs. Flu vs. Allergies vs. COVID-19prabuNo ratings yet
- Cough and Dyspnea Case StudyDocument4 pagesCough and Dyspnea Case StudyAbigail Balbuena100% (1)
- Patofisiologi Penyakit Infeksi Tuberkulosis: PendahuluanDocument5 pagesPatofisiologi Penyakit Infeksi Tuberkulosis: PendahuluanSalsabilla PutriNo ratings yet
- COVID-19 Dummy ReportDocument2 pagesCOVID-19 Dummy ReportVirat DaineNo ratings yet
- Bronchial Asthma and Acute AsthmaDocument23 pagesBronchial Asthma and Acute Asthmavivien kate perixNo ratings yet
- NCP PneumoniaDocument3 pagesNCP Pneumoniakaiserdominick100% (2)
- FeNO Interpretation Guide HighlightsDocument2 pagesFeNO Interpretation Guide HighlightsMarihell Juárez Corleone100% (1)
- Dialog Batuk 1Document5 pagesDialog Batuk 1Putri OctaviaNo ratings yet
- IM-CAP Concept MapDocument1 pageIM-CAP Concept MapTrisNo ratings yet
- When Well What Should I Do?: Call An Ambulance On 000Document2 pagesWhen Well What Should I Do?: Call An Ambulance On 000Sophia RoseNo ratings yet
- Americanas Neumo PDFDocument291 pagesAmericanas Neumo PDFUri MoraNo ratings yet
- Covid-19 Employee Self-Declaration FormDocument1 pageCovid-19 Employee Self-Declaration Formعبدالعزيز المالكيNo ratings yet
- CHEST PHYSIOTHERAPY IN NEONATES NotesDocument14 pagesCHEST PHYSIOTHERAPY IN NEONATES NotesAnu YadavNo ratings yet
- RTPCRDocument2 pagesRTPCRAaqib KhanNo ratings yet
- Acute Respiratory Infection: Darmawan B SetyantoDocument84 pagesAcute Respiratory Infection: Darmawan B SetyantonurhasanahNo ratings yet
- Speech Health: The New Normal After Pandemic Tittle: "Living Peace in The New Normal"Document2 pagesSpeech Health: The New Normal After Pandemic Tittle: "Living Peace in The New Normal"Nia GallaNo ratings yet
- NCPDocument4 pagesNCPJanella Kyle ParejaNo ratings yet
- COPD NotesDocument38 pagesCOPD NotesKudingLimMingYaoNo ratings yet
- Pulmonary-Tuberculosis - NCPDocument5 pagesPulmonary-Tuberculosis - NCPMae Therese B. MAGNONo ratings yet
- TracheitisDocument7 pagesTracheitisÁlvaro DezaNo ratings yet
- NCfIH Fast Facts Respiratory Syncytial VirusDocument6 pagesNCfIH Fast Facts Respiratory Syncytial VirusIndiana Family to FamilyNo ratings yet
- Chronic Interstitial (Restrictive Infiltrative) Lung DiseasesDocument44 pagesChronic Interstitial (Restrictive Infiltrative) Lung DiseasesAntony WaithakaNo ratings yet
- Rhinorrhea DefinitionDocument4 pagesRhinorrhea DefinitionNirmalaQuinnNo ratings yet
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (3)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (30)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 4 out of 5 stars4/5 (4)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (81)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (170)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (5)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisFrom EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisRating: 5 out of 5 stars5/5 (8)
- Empath: The Survival Guide For Highly Sensitive People: Protect Yourself From Narcissists & Toxic Relationships. Discover How to Stop Absorbing Other People's PainFrom EverandEmpath: The Survival Guide For Highly Sensitive People: Protect Yourself From Narcissists & Toxic Relationships. Discover How to Stop Absorbing Other People's PainRating: 4 out of 5 stars4/5 (95)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Summary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedRating: 4 out of 5 stars4/5 (61)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- The Marshmallow Test: Mastering Self-ControlFrom EverandThe Marshmallow Test: Mastering Self-ControlRating: 4.5 out of 5 stars4.5/5 (59)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesFrom EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesRating: 4.5 out of 5 stars4.5/5 (1412)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (45)