Professional Documents
Culture Documents
Blood Transfusion
Blood Transfusion
Uploaded by
Marshin Thea CelociaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Blood Transfusion
Blood Transfusion
Uploaded by
Marshin Thea CelociaCopyright:
Available Formats
→ Is the introduction of whole blood or blood components into → Donor blood is converted into various products, including:
venous circulation. • Packed red blood cells (RBCs)
• Whole blood
---------------------------HISTORY------------------------------ • Platelets
• Fresh frozen plasma
• Albumin
→ Where blood transfused in humans started. • Cryoprecipitates
→ Physician William Harvey fully described circulation and → Also known as an erythrocyte, this cell contains hemoglobin,
properties of blood. which binds to oxygen in the lungs, and carries the oxygen
throughout the body by way of the circulatory system.
→ The first successful blood transfusion was done by physician
Richard Lower in England on a dog. → A type of blood product that are used to replace erythrocytes
lost as a result of trauma or surgical intervention or in clients
with bone marrow suppression.
→ The first human blood transfusion was performed by Dr. → Used to increase the oxygen-carrying of blood in anemias,
Philip Syng Physick. surgery, and disorders with slow bleeding.
→ 1 unit of PRBCs has the same amount of oxygen-carrying
RBCs as a unit of whole blood.
→ The first transfusion of human blood for the treatment of → 1 unit raises hematocrit by approximately 2% to 3%.
hemorrhage was performed by Dr. James Blundell in
London.
→ Blood unaltered, as it is taken from the donor.
→ Composed of RBCs, plasma, and plasma proteins.
→ Landsteiner described ABO groups. → It is administered primarily to treat hypovolemic shock
resulting from hemorrhage.
→ Not commonly used except for extreme cases of acute
→ The Kimpton-Brown transfusion apparatus was commonly hemorrhage.
used before citration. → Replaces blood volume and all blood products: RBCs,
plasma, plasma proteins, fresh platelets, and other clotting
factors.
→ First use of blood storage.
→ A type of blood cell that is involved in the clotting process.
→ Levine described the Rh factor. → Platelets are administered to clients with low platelet counts
as a means of preventing hemorrhage and to
-----------------------------BLOOD------------------------------ thrombocytopenic clients who are actively bleeding or
scheduled for invasive procedures.
→ Replaces platelets in clients with bleeding disorders or
→ Is a familiar red fluid in the body that contain white blood platelet deficiency.
cells, red blood cells, platelet, proteins, and other elements.
→ Fresh platelets are most effective.
→ Each part of the blood has special function and can be
→ Each unit should increase the average adult client’s platelet
separated from each other.
count by about 5,000 platelets/microliter.
→ A type of blood component administered to augment clotting
factors in clients who are deficient in such factors.
→ Provides clotting factors.
→ Does not need to be typed and crossmatched (contains no
RBCs).
→ A type of blood component administered to augment clotting
factors in clients who are deficient in such factors.
→ A type of plasma protein that is used to treat hypovolemic
shock or hypoalbuminemia.
→ Albumin and plasma protein fraction are used as blood
volume expander and provides plasma proteins.
→ Various blood components used to remedy deficiencies of
clotting factors in conditions such as hemophilia or von
Willebrand disease.
→ Used for clients with clotting factor deficiencies.
→ Each provides different factor involved in the clotting compared with the name on the client's identification band
pathway; cryoprecipitate also contains fibrinogen. or bracelet.
→ The recipient’s ABO and Rh types are identified.
→ An antibody screen is performed to determine whether
antibodies other than anti-A and anti-B are present.
ABO
- A type of antigen system. Crossmatching
- The ABO type of the - Is performed:
donor should be compatible with the recipient's. ✓ Donor red blood cells (RBCs) are combined with the
recipient’s serum and Coombs’ serum.
Human blood is commonly classified into four ✓ The crossmatch is compatible if no RBC
main groups: A, B, AB, and O. agglutination occurs = no antibodies are present.
→ The universal RBC donor is O-negative; the universal
recipient is AB-positive.
→ The surface membrane of the red blood cell (RBC) is
characterized by glycoproteins known as antigens.
→ More than 400 different antigens have been identified on the
RBC membrane.
→ Yet, A, B, and Rh antigens are the most important in
determining blood group or type.
→ These are proteins produced by B lymphocytes; they consist
of two light and two heavy chains that form a Y shape.
→ These antibodies are often called agglutinins.
• Rh positive (Rh+) blood that contains the Rh factor. → Transfusion of ABO- or Rh- incompatible blood can result
• Rh negative (Rh-) blood that does not contains the Rh in a hemolytic transfusion reaction, which causes
factor. destruction of the transfused RBCs and subsequent risk of
kidney damage or failure.
→ Unlike the ABO system, Rh blood does not naturally contain
Rh antibodies.
Exposure to blood containing Rh factor (e.g., an Rh-mother
carrying a fetus with Rh + blood, or transfusion of Rh+
blood into a client who is Rh-)
Rh ANTIBODIES DEVELOP
→ Client blood samples are drawn and labeled at the bedside;
the client is asked to state his or her name, which is
→ A type of autologous donation in which blood is suctioned
from a client’s body cavities, joint spaces, and other closed
body sites during a procedure.
→ Blood obtained through blood salvage may need to undergo
“washing”, a process that removes tissue debris, before
being infused.
→ A compatible donor who has been selected by the recipient
or, in a procedure also known as directed donation,
volunteers to donate on behalf of the client.
→ Infusion of blood taken from a designated donor does not
reduce the risk of bloodborne infection, but recipients often
feel more comfortable about taking blood from a donor they
know and approve of.
• Never store blood in a refrigerator other than those used in
blood banks (blood bank refrigerators are equipped with
controlled temperatures designed for blood storage).
• Make sure that the blood is left at room temperature for no
more than 30 minutes before starting the transfusion.
Blood must be returned to the blood bank if it has not been
started.
• A transfusion should be completed within 4 hours of
initiation. The maximum time for use of a blood filter is 4
hours (Phillips & Gorski, 2014).
• No fluid other than normal saline solution should be added
to blood components, nor should medications be added to
a blood transfusion.
• The recommended rate of infusion varies with the blood
component being transfused and the client's condition, but
generally blood is infused as quickly as the client's
condition will allow.
• Blood products containing few RBCs, such as platelets,
may be infused rapidly (over 15 to 30 minutes), but care
should be taken to avoid circulatory overload.
• Vital signs and lung sounds should be assessed before the
transfusion, again after the first 15 minutes of transfusion,
and every hour until 1 hour has passed since the
transfusion was completed.
→ Donation of the client's own blood before a scheduled
procedure or in anticipation of some other future need.
→ With another nurse (most agencies require an RN), verify
→ Reduces the risk of disease transmission and potential
the following before initiating the transfusion (Phillips &
transfusion complications but is not an option for a client
Gorski, 2014, p. 731):
with leukemia or bacteremia.
✓ Order: Check the blood or component against the
primary care provider’s written order.
✓ Transfusion consent form: Ensure the form is
completed per facility policy.
✓ Client identification: The name and identification
number on the client’s identification band must be
identical to the name and number attached to the unit
of blood.
✓ Unit identification: The unit identification number on
the blood container, the transfusion form, and the tag
attached to the unit must agree.
✓ Blood type: The ABO group and Rh type on the
primary label of the donor unit must agree with those
recorded on the transfusion form.
✓ Expiration: The expiration date and time of the donor
unit should be verified as acceptable.
✓ Compatibility: The interpretation of compatibility
testing must be recorded on the transfusion form and
on the tag attached to the unit.
✓ Appearance: There should be no discoloration,
foaming, bubbles, cloudiness, clots or clumps, or loss
of integrity of the container.
• To restore blood volume after severe hemorrhage.
• To restore the oxygen-carrying capacity of the blood.
• To provide plasma factors, such as antihemophilic factor
(AHF) or factor VIII, or platelet concentrates, which
prevent or treat bleeding
• Vital signs.
• Physical examination including fluid balance and heart
and lung sounds as manifestations of hypo- or
hypervolemia.
• Status of infusion site.
• Blood test results such as hemoglobin value or platelet
count.
• Any unusual symptoms.
• Prior to performing the procedure, introduce self and
verify the client’s identity using agency protocol. Explain
to the client what you are going to do, why it is necessary,
and how he or she can participate.
• Instruct the client to report promptly any sudden chills,
nausea, itching, rash, dyspnea, back pain, or other unusual
symptoms.
• Provide for client privacy and prepare the client.
• Perform hand hygiene and observe other appropriate
infection prevention procedures.
• Prepare the infusion equipment.
• Prime the tubing.
• Start the saline solution.
• Obtain the correct blood component for the client.
• Prepare the blood bag. Invert the blood bag gently several
times to mix the cells with the plasma.
• Establish the blood transfusion.
✓ Close the upper clamp below the IV saline solution
container.
✓ Open the upper clamp below the blood bag.
• Observe the client closely for the first 15 minutes.
✓ Phillips and Gorski (2014) report that the AABB
recommends that “transfusions of RBCs be started
at 1–2 mL/min for the first 15 minutes of the
transfusion” (p. 732).
• Document relevant data.
✓ Record starting the blood, including vital signs, type
of blood, blood unit number, sequence number (e.g.,
#1 of three ordered units), site of the venipuncture,
size of the catheter, and drip rate.
• Monitor the client.
✓ Fifteen minutes after initiating the transfusion (or
according to agency policy), check the vital signs.
✓ If there are no signs of a reaction, establish the
required flow rate.
• Follow agency protocol for appropriate disposition of the
used supplies.
• Document relevant data.
✓ Record completion of the transfusion, the amount of
blood absorbed, the blood unit number, and the vital
signs.
✓ If the primary IV infusion was continued, record
connecting it.
✓ Also record the transfusion on the IV flow sheet and
intake and output record.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5814)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Chapter 27 CVD QuizletDocument29 pagesChapter 27 CVD QuizletMarshin Thea Celocia0% (1)
- Agents For Treating Heart FailureDocument6 pagesAgents For Treating Heart FailureMarshin Thea CelociaNo ratings yet
- Hematologic FunctionDocument12 pagesHematologic FunctionMarshin Thea CelociaNo ratings yet
- Chapter 26 Dysrhythmias Quizlet 3Document12 pagesChapter 26 Dysrhythmias Quizlet 3Marshin Thea CelociaNo ratings yet
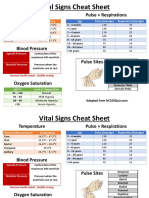
- Temperature Pulse + RespirationsDocument2 pagesTemperature Pulse + RespirationsMarshin Thea Celocia100% (1)
- Case Study Not FinalDocument45 pagesCase Study Not FinalMarshin Thea CelociaNo ratings yet
- Typology of Nursing Process (Format)Document10 pagesTypology of Nursing Process (Format)Marshin Thea CelociaNo ratings yet
- Ortho DSDocument3 pagesOrtho DSMarshin Thea CelociaNo ratings yet
- NcpsDocument5 pagesNcpsMarshin Thea CelociaNo ratings yet
- NcpsDocument5 pagesNcpsMarshin Thea CelociaNo ratings yet
- Ortho NCPDocument3 pagesOrtho NCPMarshin Thea CelociaNo ratings yet