Professional Documents
Culture Documents
JPD 11207
Uploaded by
mohamed aljapriOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
JPD 11207
Uploaded by
mohamed aljapriCopyright:
Available Formats
Open Access https://www.jparathyroid.
com
Journal of
Journal of Parathyroid Disease 2023,11, e11207
Commentary
DOI:10.34172/jpd.2023.11207
See the photo-clinic by Arabizadeh et al (doi: 10.34172/jpd.2023.11200)
Brown tumor in hyperparathyroidism; a new look at
an old problem
ID
Shiva Toumaj*
Implication for health policy/practice/research/medical education:
Brown tumors are uncommon in general (around 0.1%), however they tend to be more common in people with primary and secondary
hyperparathyroidism.
Keywords: Brown tumor, Primary hyperparathyroidism, Secondary hyperparathyroidism
Please cite this paper as: Toumaj S. Brown tumor in hyperparathyroidism; a new look at an old problem. J Parathyr Dis. 2023;11:e11207.
doi:10.34172/jpd.2023.11207.
Copyright © 2023 The Author(s); Published by Nickan Research Institute. This is an open-access article distributed under the terms of
the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the
original work is properly cited.
I
recently read the paper by Arabizadeh et al (1), facial bones contributing to just 4.5% of cases. The most
on “the pathology of brown tumor in a-36-year- typical site of primary hyperparathyroidism -associated
old man on maintenance hemodialysis” with great maxilla-facial brown tumors is the mandible. Differential
interest. Regarding this study, I would like to expand diagnoses of brown tumors include osteolytic metastasis,
the discussion with more recent data on this topic. The infectious diseases (bone abscess and osteomyelitis),
term “brown tumor” is a misnomer since it is not a real cancer, aneurysmal bone cyst, giant cell tumors, and
neoplasm. It was originally used to describe the tissue lesions from multiple myeloma (4). When Brown tumors
specimen’s typical dark reddish-brown color, which are located at unusual localization, the diagnosis might
occurs due to vascularity, hemorrhage, and deposits of be much more challenging. For the differential diagnosis
the pigment hemosiderin. In recent years, the brown of brown tumors in primary hyperparathyroidism, a
tumor diagnosis has become less prevalent (decreased multidisciplinary approach including clinical, laboratory,
from 80% in the past to 15% in the present), due to histologic, and imaging findings are needed. During the
improved techniques for screening and more frequent diagnosis process and the follow-up, imaging techniques
early detection of hyperparathyroidism. Brown tumors including X-rays, computerized tomography (CT)
are uncommon in general (around 0.1%), but they tend to scans, and magnetic resonance imaging (MRI) should
be more common in people with primary and secondary be conducted in combination. On X-ray, brown tumors
hyperparathyroidism. Regarding skeletal problems, exhibit a well-defined, translucent, lytic lesion with a thin
brown tumors are observed in 4.5% of patients with or weakened cortex, without specific signs. On either CT
primary hyperparathyroidism and 1.5–1.7% of patients or MRI, they could not reveal any characteristic changes.
with secondary hyperparathyroidism suffering from Only solid, mixed solid, and cystic, or cystic lesions may
chronic renal disease. In comparison to males, women are be detected. The diagnosis mainly relies on biopsy and
more likely to develop brown tumors (2). The incidence excessively increased parathyroid hormone (5).
increases with aging, with postmenopausal women Treatment for hyperphosphatemia with phosphate
reporting the majority of instances at ages higher than 50. binders, calcimimetics or active vitamin D, and
This may be related to hormonal imbalances, which may parathyroidectomy have all been found to be
be more common in females than males (3). helpful. Patients who fail to respond effectively to
Brown tumors can affect any skeletal component and parathyroidectomy and conservative therapy may need
can be solitary or multiple. The ribs, clavicle, tibia, femur, to have the tumoral masses surgically removed. This
pelvic girdle, and hands are the skeletal structures that is frequently required due to aesthetic concerns and
brown tumors most commonly affect, with the maxillo- functional issues related to swallowing and chewing (6).
Received: 5 May 2023, Accepted: 12 June 2023, ePublished: 27 June 2023
Independent Researcher, Miandoab, West Azerbaijan, Iran.
*Corresponding author: Shiva Toumaj, Email: tumajshiva@gmail.com
Toumaj S
References
Brown tumors can also result in neurological disorders 1. Arabizadeh N, Zakerzadeh D, Nakhaie R, Alinejad MA, Barati
and pathological fractures. Severe cases can result in P, Samiei A, et al. The pathology of brown tumor in a-36-
dysphagia and represent a serious medical condition if year-old man on maintenance hemodialysis. J Parathyr Dis.
not adequately treated. The conventional treatment for 2023;11:e11200.
2. Gosavi S, Kaur H, Gandhi P. Multifocal osteolytic lesions
small, solitary, localized lesions is the biopsy of suspected
of jaw as a road map to diagnosis of brown tumor of
lesions, followed by enucleation and curettage, including hyperparathyroidism: A rare case report with review of
the surrounding healthy bone. Marginal or segmental literature. J Oral Maxillofac Pathol. 2020;24:S59-S66. doi:
resections are performed on more extensive lesions, such 10.4103/jomfp.JOMFP_319_19.
3. Diacinti D, Cipriani C, Biamonte F, Pepe J, Colangelo L, Kripa
as multiple lesion areas and lesions with unclear margins.
E, et al. Imaging technologies in the differential diagnosis and
A minimally invasive surgical resection is the treatment of follow-up of brown tumor in primary hyperparathyroidism:
choice as there have been no occurrences of tumor mass Case report and review of the literature. Bone Rep.
recurrence subsequent resection of malignant changes. 2020;14:100745. doi: 10.1016/j.bonr.2020.100745.
Radical resection may still be required in some situations 4. Hu J, He S, Yang J, Ye C, Yang X, Xiao J. Management of
brown tumor of spine with primary hyperparathyroidism:
with large progressed lesions (7). A case report and literature review. Medicine (Baltimore).
However, the management of brown tumors still 2019;98:e15007. doi: 10.1097/MD.0000000000015007.
requires further investigations, hence, larger studies and 5. Majumdar S, Uppala D, Kotina S, Alekhya B. Brown tumor
more clinical trials are recommended on this subject. of hyperparathyroidism with multiple lesions. J Oral
Maxillofac Pathol. 2022;26:S111-S115. doi: 10.4103/jomfp.
jomfp_409_20.
Conflicts of interest 6. Xu W, Qu Y, Shi W, Ma B, Jiang H, Wang Y, et al. Multiple bone
The author declares no competing interests. brown tumor secondary to primary hyperparathyroidism: a
case report and literature review. Gland Surg. 2019;8:810-
Ethical issues 816. doi: 10.21037/gs.2019.11.14.
Ethical issues (including plagiarism, data fabrication, double 7. Shavlokhova V, Goeppert B, Gaida MM, Saravi B, Weichel
publication) have been completely observed by the author. F, Vollmer A, et al. Mandibular Brown Tumor as a Result of
Secondary Hyperparathyroidism: A Case Report with 5 Years
Funding/Support Follow-Up and Review of the Literature. Int J Environ Res
None. Public Health. 2021;18:7370. doi: 10.3390/ijerph18147370.
2 Journal of Parathyroid Disease, Volume 11, 2023
You might also like
- 1 s2.0 S2210261220309391 MainDocument4 pages1 s2.0 S2210261220309391 MainmbenitezNo ratings yet
- Brown TumorDocument4 pagesBrown TumorJeyachandran MariappanNo ratings yet
- Searching For The Culprit: Metastases From A Cancer of Unknown PrimaryDocument8 pagesSearching For The Culprit: Metastases From A Cancer of Unknown PrimarydafinfulvianarkanantaNo ratings yet
- Giant Cell Tumour of Bone: A Demographic Study From A Tumour Unit in South AfricaDocument6 pagesGiant Cell Tumour of Bone: A Demographic Study From A Tumour Unit in South AfricaRadenSiwi Bagus HadhiningratNo ratings yet
- F-FDG PET/CT in Metastatic Extramammary Paget 'S Disease: Nteresting MageDocument2 pagesF-FDG PET/CT in Metastatic Extramammary Paget 'S Disease: Nteresting MageLaura PredescuNo ratings yet
- Jurnal Patologi AnatomiDocument5 pagesJurnal Patologi Anatomiafiqzakieilhami11No ratings yet
- Jurnal Kedokteran Dan Kesehatan Indonesia: Indonesian Journal of Medicine and HealthDocument7 pagesJurnal Kedokteran Dan Kesehatan Indonesia: Indonesian Journal of Medicine and HealthNio DoodohNo ratings yet
- Multiple Bilateral Choroidal Metastasis From Anal MelanomaDocument2 pagesMultiple Bilateral Choroidal Metastasis From Anal MelanomaMoazzam FarooqiNo ratings yet
- Literature Review OsteosarcomaDocument8 pagesLiterature Review Osteosarcomaea813c29100% (1)
- Literature Review of OsteosarcomaDocument4 pagesLiterature Review of Osteosarcomachrvzyukg100% (1)
- 1.masas en CuelloDocument3 pages1.masas en CuelloIsaac TellezNo ratings yet
- Brown Tumors of The Oral Cavity: Presentation of 4 New Cases and A Systematic Literature ReviewDocument14 pagesBrown Tumors of The Oral Cavity: Presentation of 4 New Cases and A Systematic Literature Reviewisma wahyuniNo ratings yet
- Completion Thyroidectomy: Predicting Bilateral Disease: Originalresearcharticle Open AccessDocument7 pagesCompletion Thyroidectomy: Predicting Bilateral Disease: Originalresearcharticle Open AccessRadita Dwihaning PutriNo ratings yet
- Desmoid TumoursDocument234 pagesDesmoid TumoursJohn M. HemsworthNo ratings yet
- Chondrosarcoma of The Jaw: A Retrospective Series: ObjectivesDocument6 pagesChondrosarcoma of The Jaw: A Retrospective Series: ObjectivesOMFS FKG UnimusNo ratings yet
- Prediction of Malignancy and Adverse Outcome of Solid Pseudopapillary Tumor of The PancreasDocument11 pagesPrediction of Malignancy and Adverse Outcome of Solid Pseudopapillary Tumor of The PancreasPatricia BezneaNo ratings yet
- 2019 Article 757Document9 pages2019 Article 757ritvikNo ratings yet
- Soft Tissue Sarcoma in A Malignancy Prone Patient An UpdateDocument11 pagesSoft Tissue Sarcoma in A Malignancy Prone Patient An UpdateAthenaeum Scientific PublishersNo ratings yet
- Correlation of Level of Serum 25-Hydroxy Vitamin D and Gleason Score As A Measure of Aggressiveness of Prostate Cancer in Black AfricansDocument5 pagesCorrelation of Level of Serum 25-Hydroxy Vitamin D and Gleason Score As A Measure of Aggressiveness of Prostate Cancer in Black AfricansInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Prognostic Factors For Recurrence in Patients With Papillary Thyroid CarcinomaDocument8 pagesPrognostic Factors For Recurrence in Patients With Papillary Thyroid CarcinomaLeonardo LeónNo ratings yet
- Fibrothecoma: Clinical, Radiological and Immunohistochemical Data About An ObservationDocument4 pagesFibrothecoma: Clinical, Radiological and Immunohistochemical Data About An ObservationIJAR JOURNALNo ratings yet
- Unusually Rapid Growth of Brown Tumour in The Mandible After Parathyroidectomy Associated With The Presence of A Supernumerary Parathyroid GlandDocument5 pagesUnusually Rapid Growth of Brown Tumour in The Mandible After Parathyroidectomy Associated With The Presence of A Supernumerary Parathyroid Glandanang dwiNo ratings yet
- Research Paper On Bone CancerDocument5 pagesResearch Paper On Bone Cancerafeayaczb100% (1)
- Cancer Cytopathology - 2020 - Velleuer - Diagnostic Accuracy of Brush Biopsy Based Cytology For The Early Detection of OralDocument11 pagesCancer Cytopathology - 2020 - Velleuer - Diagnostic Accuracy of Brush Biopsy Based Cytology For The Early Detection of Oralopy dasNo ratings yet
- BPH and Prostate Cancer RiskDocument9 pagesBPH and Prostate Cancer RiskEvita LarasNo ratings yet
- EmerencyDocument3 pagesEmerencySehrish SiddiqueNo ratings yet
- NURS 530 Prostate CancerDocument7 pagesNURS 530 Prostate CancerVivian OcampoNo ratings yet
- Riginal Research: Journal of Advanced Medical and Dental Sciences ResearchDocument3 pagesRiginal Research: Journal of Advanced Medical and Dental Sciences Researchshivam sethiNo ratings yet
- Mohammadzadeh2015 Article PredictingTheProbabilityOfMoDocument8 pagesMohammadzadeh2015 Article PredictingTheProbabilityOfMosaba khosraviNo ratings yet
- Case Report: Gross Hematuria and Bladder Tumor in A Patient With Advanced Thyroid Papillary CarcinomaDocument4 pagesCase Report: Gross Hematuria and Bladder Tumor in A Patient With Advanced Thyroid Papillary CarcinomaLunaFiaNo ratings yet
- Cureus 0012 00000008418Document10 pagesCureus 0012 00000008418فرجني موغNo ratings yet
- PHD Thesis On Prostate CancerDocument5 pagesPHD Thesis On Prostate Cancermandyfroemmingfargo100% (2)
- Clinicopathological Characteristics and Prognosis of Ossifying Fibroma in The Jaws of Children: A Retrospective StudyDocument6 pagesClinicopathological Characteristics and Prognosis of Ossifying Fibroma in The Jaws of Children: A Retrospective Studyabeer alrofaeyNo ratings yet
- Endocrine Incidentalomas: Current Problems in SurgeryDocument28 pagesEndocrine Incidentalomas: Current Problems in SurgeryBolivar IseaNo ratings yet
- Wide Field of Cancerization Case Report: February 2017Document5 pagesWide Field of Cancerization Case Report: February 2017Mira AnggrianiNo ratings yet
- Dread Site of Relapse in Germ Cell Tumor of TestisDocument4 pagesDread Site of Relapse in Germ Cell Tumor of TestisIJAR JOURNALNo ratings yet
- Beird Hannah C Osteosarcoma 2022 12Document19 pagesBeird Hannah C Osteosarcoma 2022 12najibNo ratings yet
- Risk Factors For Bad Splits During Sagittal Split Ramus OsteotomyDocument5 pagesRisk Factors For Bad Splits During Sagittal Split Ramus OsteotomyAgustin LarezNo ratings yet
- ReviewDocument5 pagesReviewerickmattosNo ratings yet
- Dedifferentiated Chondrosarcoma: Radiological Features, Prognostic Factors and Survival Statistics in 23 PatientsDocument15 pagesDedifferentiated Chondrosarcoma: Radiological Features, Prognostic Factors and Survival Statistics in 23 PatientsHidayat ArifinNo ratings yet
- HN 04-2011 Sublingual Gland Tumors PDFDocument6 pagesHN 04-2011 Sublingual Gland Tumors PDFHafiz FatmarNo ratings yet
- Sex, Age, and Other Barriers For Prosthetic Referral Following Amputation and The Impact On SurvivalDocument9 pagesSex, Age, and Other Barriers For Prosthetic Referral Following Amputation and The Impact On SurvivallalaNo ratings yet
- Male Breast Cancer: An Institutional ExperienceDocument5 pagesMale Breast Cancer: An Institutional ExperienceIJAR JOURNALNo ratings yet
- Austin Head & Neck OncologyDocument2 pagesAustin Head & Neck OncologyAustin Publishing GroupNo ratings yet
- DP Endo v01n3p017021 enDocument5 pagesDP Endo v01n3p017021 enasdfasdNo ratings yet
- Step 1 5Document13 pagesStep 1 5Fitri Amelia RizkiNo ratings yet
- Approach To NTMNG Jcem 2011Document11 pagesApproach To NTMNG Jcem 2011IffatNaeemNo ratings yet
- jnm046045 1920.Document3 pagesjnm046045 1920.Rahul KashyapNo ratings yet
- Non Small-Cell Lung Cancer in A 15-Year-Old NonsmokerDocument2 pagesNon Small-Cell Lung Cancer in A 15-Year-Old Nonsmokertonirian99No ratings yet
- 2019 Tumores Odontogenicos PDFDocument16 pages2019 Tumores Odontogenicos PDFGissela AlvaradoNo ratings yet
- Wa0011Document4 pagesWa0011PatrickNicholsNo ratings yet
- Metastatic Vertebral Lesion Mimicking An Atypical Hemangioma WithDocument8 pagesMetastatic Vertebral Lesion Mimicking An Atypical Hemangioma Withsica_17_steaua6519No ratings yet
- ECD Vs Sup Parotidectomy ArticleDocument8 pagesECD Vs Sup Parotidectomy ArticleAmeena AzeemiNo ratings yet
- Hemangiopericytoma of Palate A Rare Case ReportDocument4 pagesHemangiopericytoma of Palate A Rare Case ReportIJAR JOURNALNo ratings yet
- Oral Cancer: The First Symptoms and Reasons For Delaying Correct Diagnosis and Appropriate TreatmentDocument9 pagesOral Cancer: The First Symptoms and Reasons For Delaying Correct Diagnosis and Appropriate TreatmentMarekNo ratings yet
- Single Institution Study On The Management of Childhood Bladder and Prostate RhabdomyosarcomaDocument5 pagesSingle Institution Study On The Management of Childhood Bladder and Prostate RhabdomyosarcomaIJAR JOURNALNo ratings yet
- Uterine Fibroma Associated With Stump (Smooth Muscle Tumour of Uncertain Malignant Potential) : Case ReportDocument3 pagesUterine Fibroma Associated With Stump (Smooth Muscle Tumour of Uncertain Malignant Potential) : Case ReportIJAR JOURNALNo ratings yet
- Clinical: Peripheral Ossifying Fibroma: A Case ReportDocument4 pagesClinical: Peripheral Ossifying Fibroma: A Case Reportsagarjangam123No ratings yet
- Example Research Paper On Prostate CancerDocument8 pagesExample Research Paper On Prostate Cancerzxnrvkrif100% (1)
- Halal Certification of Insect-Based Food A CritiqueDocument13 pagesHalal Certification of Insect-Based Food A CritiqueAhmadNo ratings yet
- Mayo Clinic Infectious Diseases Board Review Mayo Clinic Scientific PRDocument581 pagesMayo Clinic Infectious Diseases Board Review Mayo Clinic Scientific PRarahman16877% (13)
- Cutler Files Federal FilingDocument28 pagesCutler Files Federal FilingthisdogNo ratings yet
- AvidNEXIS ReadMe v2019.2 PDFDocument28 pagesAvidNEXIS ReadMe v2019.2 PDFAugusto Bravo FigueroaNo ratings yet
- ImagineFX 2018 156 JanuaryDocument116 pagesImagineFX 2018 156 JanuaryResimasc González100% (5)
- Q4-M5-Freedom of The Human PersonDocument27 pagesQ4-M5-Freedom of The Human PersonAngelo Ivan90% (20)
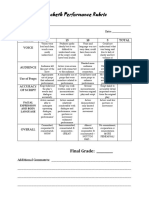
- Macbeth Performance Rubric: Final GradeDocument1 pageMacbeth Performance Rubric: Final GradeRodel BautistaNo ratings yet
- De Rama Vs Court of AppealsDocument2 pagesDe Rama Vs Court of AppealsPhilip VistalNo ratings yet
- 2021-2022 MIDTERM EXAM IN BENLATC (Nov. 03, 2021)Document9 pages2021-2022 MIDTERM EXAM IN BENLATC (Nov. 03, 2021)kimberlyNo ratings yet
- 11 Key Ring Nov 2021Document32 pages11 Key Ring Nov 2021bbbillyNo ratings yet
- Literal and Figurative Language Semi Detailed Lesson PlanDocument2 pagesLiteral and Figurative Language Semi Detailed Lesson PlanRichard FerolinoNo ratings yet
- Capillary Puncture (Materials and Procedure)Document36 pagesCapillary Puncture (Materials and Procedure)Angelica Camille B. AbaoNo ratings yet
- Technical Specificationas FlyoversDocument11 pagesTechnical Specificationas FlyoversRed Reloza100% (1)
- Research Paper On Hostel LifeDocument6 pagesResearch Paper On Hostel Lifezyjulejup0p3100% (1)
- Sources of International LawDocument7 pagesSources of International LawJonathan Valencia0% (1)
- Microbial Pathogenesis: SciencedirectDocument8 pagesMicrobial Pathogenesis: SciencedirectMaria Silvana AlvesNo ratings yet
- BatikDocument15 pagesBatikMuslimbinNasir100% (1)
- Malaysia Asean Math Olympiads: Rules and RegulationsDocument7 pagesMalaysia Asean Math Olympiads: Rules and RegulationsKarren Cacabelos SurNo ratings yet
- Samsung Case Study - Faiz Irfan Hajid - 1806153214Document9 pagesSamsung Case Study - Faiz Irfan Hajid - 1806153214Faiz Irfan HajidNo ratings yet
- Energy Conversion and Management: He Wang, Guofang Gong, Hongbin Zhou, Wei WangDocument10 pagesEnergy Conversion and Management: He Wang, Guofang Gong, Hongbin Zhou, Wei Wangbryan andres mora ramosNo ratings yet
- Department of Education: Training DesignDocument7 pagesDepartment of Education: Training DesignMarylen TrapalNo ratings yet
- Questionnaire of 16 PF English VersionDocument15 pagesQuestionnaire of 16 PF English VersionZaphiro deSade67% (3)
- Xtreme Trader GuideDocument50 pagesXtreme Trader GuideJagannath SamalNo ratings yet
- Parliament System of DemocracyDocument22 pagesParliament System of DemocracyRajnish DabasNo ratings yet
- Reviewer Rule 115 To 127Document21 pagesReviewer Rule 115 To 127Julio Ceazar SedanoNo ratings yet
- SA1 Time Table & Portions Grade VII PDFDocument2 pagesSA1 Time Table & Portions Grade VII PDFKrishnaNo ratings yet
- 2.2. Graham CookDocument9 pages2.2. Graham Cookamin138irNo ratings yet
- MSC Sahc SguerraDocument130 pagesMSC Sahc SguerraSoniaGPNo ratings yet
- Nurse Entrepreneur: Patricia Ann Bemis, RN CENDocument5 pagesNurse Entrepreneur: Patricia Ann Bemis, RN CENmariaNo ratings yet
- Hafnia AlveiDocument5 pagesHafnia AlveiluisNo ratings yet
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (5)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 4.5 out of 5 stars4.5/5 (84)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- The Twentysomething Treatment: A Revolutionary Remedy for an Uncertain AgeFrom EverandThe Twentysomething Treatment: A Revolutionary Remedy for an Uncertain AgeRating: 5 out of 5 stars5/5 (4)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (39)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (267)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 4 out of 5 stars4/5 (5)
- I Shouldn't Feel This Way: Name What’s Hard, Tame Your Guilt, and Transform Self-Sabotage into Brave ActionFrom EverandI Shouldn't Feel This Way: Name What’s Hard, Tame Your Guilt, and Transform Self-Sabotage into Brave ActionNo ratings yet
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (44)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (170)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (46)
- Summary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisFrom EverandSummary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisRating: 5 out of 5 stars5/5 (4)
- To Explain the World: The Discovery of Modern ScienceFrom EverandTo Explain the World: The Discovery of Modern ScienceRating: 3.5 out of 5 stars3.5/5 (51)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesFrom EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesRating: 4.5 out of 5 stars4.5/5 (1412)
- Self-Care for Autistic People: 100+ Ways to Recharge, De-Stress, and Unmask!From EverandSelf-Care for Autistic People: 100+ Ways to Recharge, De-Stress, and Unmask!Rating: 5 out of 5 stars5/5 (1)