Professional Documents
Culture Documents
Endocarditis - Symptoms and Causes - Mayo Clinic
Uploaded by
Briandon CanlasCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Endocarditis - Symptoms and Causes - Mayo Clinic
Uploaded by
Briandon CanlasCopyright:
Available Formats
COVID-19: Advice, updates and
vaccine options
English
MENU SEARCH
Request an Appointment
Patient Care & Health Information Diseases & Conditions
Endocarditis
SECTIONS
Overview
Endocarditis is a life-threatening
inflammation of the inner lining of
your heart's chambers and valves
(endocardium).
Endocarditis is usually caused by
an infection. Bacteria, fungi or
other germs from another part of
your body, such as your mouth, Endocarditis
spread through your bloodstream
and attach to damaged areas in
your heart. If it's not treated
quickly, endocarditis can damage or destroy your heart
valves. Treatments for endocarditis include
medications and, sometimes, surgery.
Advertisement
Mayo Clinic does not endorse companies or products.
Advertising revenue supports our not-for-profit mission.
Advertising & Sponsorship
Policy Opportunities Ad Choices
People at greatest risk of endocarditis usually have
damaged heart valves, artificial heart valves or other
heart defects.
Symptoms
Endocarditis may develop slowly or suddenly,
depending on what germs are causing the infection
and whether you have any underlying heart problems.
Signs and symptoms of endocarditis can vary from
person to person.
Common signs and symptoms of endocarditis include:
Aching joints and muscles
Chest pain when you breathe
Fatigue
Flu-like symptoms, such as fever and chills
Night sweats
Shortness of breath
Swelling in your feet, legs or abdomen
A new or changed heart murmur, which is the
heart sound made by blood rushing through your
heart
Less common signs and symptoms of endocarditis can
include:
Unexplained weight loss
Blood in your urine, which you might be able to
see or that your doctor might see when he or she
views your urine under a microscope
Tenderness in your spleen, which is an infection-
fighting organ located just below your left rib cage
Red spots on the soles of your feet or the palms
of your hands (Janeway lesions)
Red, tender spots under the skin of your fingers
or toes (Osler's nodes)
Tiny purple or red spots, called petechiae (puh-
TEE-kee-ee), on the skin, in the whites of your
eyes or inside your mouth
When to see a doctor
If you have signs or symptoms of endocarditis, see
your doctor as soon as possible — especially if you
have risk factors for this serious infection, such as a
heart defect or history of endocarditis. Although less
serious conditions can cause similar signs and
symptoms, you won't know for sure until you're
evaluated by your doctor.
If you've been diagnosed with endocarditis, tell your
doctor about any signs or symptoms that may mean
your infection is getting worse, such as:
Chills
Fever
Headaches
Joint pain
Shortness of breath
If you're being treated with antibiotics for endocarditis,
tell your doctor if you develop diarrhea, a rash, itching
or joint pain. These signs and symptoms may mean
you're having a reaction to your prescribed antibiotic.
Request an Appointment at Mayo Clinic
Causes
Endocarditis occurs when germs, usually bacteria,
enter your bloodstream, travel to your heart, and
attach to abnormal heart valves or damaged heart
tissue. Fungi or other germs also may cause
endocarditis.
Usually, your immune system destroys any harmful
bacteria that enter your bloodstream. However,
bacteria that live in your mouth, throat or other parts of
your body, such as your skin or your gut, can
sometimes cause endocarditis under the right
circumstances.
Bacteria, fungi and other germs that cause
endocarditis might enter your bloodstream through:
Improper dental care. Proper toothbrushing and
flossing helps prevent gum disease. If you don't
take good care of your teeth and gums, brushing
could cause unhealthy gums to bleed, giving
bacteria a chance to enter your bloodstream.
Some dental procedures that can cut your gums
also may allow bacteria to enter your
bloodstream.
Catheters. Bacteria can enter your body through
a thin tube that doctors sometimes use to inject or
remove fluid from the body (catheter). This is
more likely to occur if the catheter is in place for a
long period of time. For example, you may have a
catheter if you need long-term dialysis.
Illegal IV drug use. Contaminated needles and
syringes are a special concern for people who
use illegal IV drugs, such as heroin or cocaine.
Often, individuals who use these types of drugs
don't have access to clean, unused needles or
syringes.
Risk factors
You're more likely to develop
endocarditis if you have faulty,
diseased or damaged heart
valves. However, endocarditis
does occasionally occur in
previously healthy people.
You have an increased risk of
endocarditis if you have:
Chambers and
Older age. Endocarditis valves of the
occurs most often in older heart
adults over age 60.
Artificial heart valves. Germs are more likely to
attach to an artificial (prosthetic) heart valve than
to a normal heart valve.
Damaged heart valves. Certain medical
conditions, such as rheumatic fever or infection,
can damage or scar one or more of your heart
valves, increasing the risk of infection.
Congenital heart defects. If you were born with
certain types of heart defects, such as an
irregular heart or abnormal heart valves, your
heart may be more susceptible to infection.
Implanted heart device. Bacteria can attach to
an implanted device, such as a pacemaker,
causing an infection of the heart's lining.
A history of endocarditis. Endocarditis can
damage heart tissue and valves, increasing the
risk of a future heart infection.
A history of illegal IV drug use. People who use
illegal drugs by injecting them are at a greater risk
of endocarditis. The needles used to inject drugs
can be contaminated with the bacteria that can
cause endocarditis.
Poor dental health. A healthy mouth and healthy
gums are essential for good health. If you don't
brush and floss regularly, bacteria can grow
inside your mouth and may enter your
bloodstream through a cut on your gums.
Long-term catheter use. Having a catheter in
place for a long period of time (indwelling
catheter) increases your risk of endocarditis.
If you're at risk of endocarditis, let all of your doctors
know. You may want to request an endocarditis wallet
card from the American Heart Association. Check with
your local chapter or print the card from the
association's website.
Complications
In endocarditis, clumps made of germs and cell pieces
form an abnormal mass in your heart. These clumps,
called vegetations, can break loose and travel to your
brain, lungs, abdominal organs, kidneys, or arms and
legs.
As a result, endocarditis can cause several
complications, including:
Heart problems, such as heart murmur, heart
valve damage and heart failure
Stroke
Pockets of collected pus (abscesses) that
develop in the heart, brain, lungs and other
organs
Blood clot in a lung artery (pulmonary embolism)
Kidney damage
Enlarged spleen
Prevention
You can take the following steps to help prevent
endocarditis:
Know the signs and symptoms of
endocarditis. See your doctor immediately if you
develop any signs or symptoms, especially a
fever that won't go away, unexplained fatigue, any
type of skin infection, or open cuts or sores that
don't heal properly.
Take care of your teeth and gums. Brush and
floss your teeth and gums often, and have regular
dental checkups. Good dental hygiene is an
important part of maintaining your overall health.
Don't use illegal IV drugs. Dirty needles can
send bacteria into your bloodstream, increasing
your risk of endocarditis.
Preventive antibiotics
Certain dental and medical procedures may allow
bacteria to enter your bloodstream.
If you're at high risk of endocarditis, the American
Heart Association recommends taking antibiotics an
hour before having any dental work done.
You're at high risk of endocarditis and need antibiotics
before dental work if you have:
A history of endocarditis
A man-made (prosthetic mechanical) heart valve
A heart transplant, in some cases
Certain types of congenital heart disease
Congenital heart disease surgery in the last six
months
If you have endocarditis or any type of congenital heart
disease, talk to your doctor and dentist about your
risks and whether you need preventive antibiotics.
By Mayo Clinic Staff
Request an Appointment at Mayo Clinic
Diagnosis & treatment
Nov. 14, 2020
Advertisement
Mayo Clinic does not endorse companies or products.
Advertising revenue supports our not-for-profit mission.
Advertising & Sponsorship
Policy Opportunities Ad Choices
Share on: Facebook Twitter
Show references
Related
Endocarditis
Associated Procedures
Chest X-rays
CT scan
Electrocardiogram (ECG or EKG)
Show more associated procedures
Endocarditis
Symptoms & causes
Diagnosis & treatment
Doctors & departments
Advertisement
Mayo Clinic Press
Check out these best-sellers and special offers on books
and newsletters from Mayo Clinic.
Try Mayo Clinic Health Letter - get FREE book
NEW - Back and Neck Health
Mayo Clinic on Digestive Health
NEW - Live Younger Longer
Simple, effective Home Remedies
CON-20303974
Patient Care & Health Information
Diseases & Conditions
Endocarditis
Request Appointment
Contact Us
About Mayo Clinic
Employees
Find a Job
Site Map
About This Site
Twitter
Facebook
PinterestYouTube
Mayo Clinic is a not-for-profit organization. Make a donation.
Any use of this site constitutes your agreement to the Terms and
Conditions and Privacy Policy linked below.
Terms and Conditions
Privacy Policy
Notice of Privacy Practices
Notice of Nondiscrimination
A single copy of these materials may be reprinted for
noncommercial personal use only. "Mayo," "Mayo Clinic,"
"MayoClinic.org," "Mayo Clinic Healthy Living," and the triple-shield
Mayo Clinic logo are trademarks of Mayo Foundation for Medical
Education and Research.
This site complies with the
HONcode standard for trustworthy health
information:
verify here.
© 1998-2021 Mayo Foundation for Medical Education and
Research (MFMER). All rights reserved.
You might also like
- Xavier University Nursing Case Analysis on Infective EndocarditisDocument6 pagesXavier University Nursing Case Analysis on Infective EndocarditisDudil GoatNo ratings yet
- Endocarditis, Pericarditic, Myocarditis: TopicDocument104 pagesEndocarditis, Pericarditic, Myocarditis: TopicOM VERMANo ratings yet
- NASA - Guidelines For Management of Circadian DesynchronyDocument47 pagesNASA - Guidelines For Management of Circadian DesynchronyJab100% (1)
- Wolfe - Understanding and Treating Anxiety Disorders An Integrative Approach To Healing The Wounded Self (2005)Document300 pagesWolfe - Understanding and Treating Anxiety Disorders An Integrative Approach To Healing The Wounded Self (2005)Ruxandra Pop100% (5)
- Uncontrolled Blood Sugar NCPDocument4 pagesUncontrolled Blood Sugar NCPRawan KhateebNo ratings yet
- Infective Endocarditis GuideDocument7 pagesInfective Endocarditis GuideAkarsh RamNo ratings yet
- Report Pathopysiology (Endocarditis) 12Document7 pagesReport Pathopysiology (Endocarditis) 12Ade Yulina Mursyidah Sa'adNo ratings yet
- Endocarditis: Causes, Symptoms, Diagnosis and TreatmentDocument4 pagesEndocarditis: Causes, Symptoms, Diagnosis and TreatmentRedho Sara PratiwiNo ratings yet
- Infectious EndocarditisDocument4 pagesInfectious EndocarditisKhalid Mahmud Arifin100% (1)
- What Is Infective Endocarditis?Document5 pagesWhat Is Infective Endocarditis?prasenjit_gayenNo ratings yet
- Understanding Rheumatic FeverDocument7 pagesUnderstanding Rheumatic FevergitozsbyNo ratings yet
- Risk Factors Include Having: Congenital Heart DefectsDocument3 pagesRisk Factors Include Having: Congenital Heart Defectspragna novaNo ratings yet
- New Patients EndocarditisDocument1 pageNew Patients EndocarditisnayanastarNo ratings yet
- Endocarditis, MyocarditisDocument37 pagesEndocarditis, MyocarditisJuma AwarNo ratings yet
- Arteriovenous Fistula: Twitter Facebook Pinterest YoutubeDocument8 pagesArteriovenous Fistula: Twitter Facebook Pinterest YoutubeJG RNNo ratings yet
- Congenital Heart DiseaseDocument5 pagesCongenital Heart DiseaseZAY EMNo ratings yet
- Acterial Endocarditis: Email UsDocument4 pagesActerial Endocarditis: Email UsCatherine LoyolaNo ratings yet
- Myocarditis Symptoms and CausesDocument1 pageMyocarditis Symptoms and Causesdmwcgghg22No ratings yet
- Cardio InfectionDocument6 pagesCardio InfectionCindy Mae de la TorreNo ratings yet
- Proper Way To Maintain A Healthy Circulatory and Respiratory SystemDocument4 pagesProper Way To Maintain A Healthy Circulatory and Respiratory SystemJakob IsraelNo ratings yet
- Case Study Worksheet EndocarditisDocument6 pagesCase Study Worksheet EndocarditisSharlee StoneNo ratings yet
- Causes of MyocarditisDocument3 pagesCauses of MyocarditisTeresa CardinozaNo ratings yet
- Recog Manag Diff Type Carditis Endo Myo PericardiditDocument7 pagesRecog Manag Diff Type Carditis Endo Myo PericardiditArdi WidiatmikaNo ratings yet
- Pubmed Health: Ventricular Septal DefectDocument3 pagesPubmed Health: Ventricular Septal DefectfildzahNo ratings yet
- Cardiovascular System ExplainedDocument18 pagesCardiovascular System ExplainedJkiathlene JauganNo ratings yet
- Splinter Hemorrhages - Symptoms, Causes, and Treatments PDFDocument10 pagesSplinter Hemorrhages - Symptoms, Causes, and Treatments PDFNeymar RonaldoNo ratings yet
- By Mayo Clinic StaffDocument7 pagesBy Mayo Clinic StaffKeith PerryNo ratings yet
- Infective EndocarditisDocument66 pagesInfective Endocarditissanjivdas100% (4)
- Heart ConditionsDocument6 pagesHeart ConditionsAlanNo ratings yet
- Causes and Treatment of Myocarditis in ChildrenDocument9 pagesCauses and Treatment of Myocarditis in ChildrenMILENA SIERRANo ratings yet
- Rheumatic Heart DiseaseDocument10 pagesRheumatic Heart DiseaseSuhas IngaleNo ratings yet
- Week 1Document7 pagesWeek 1Balkess NajemNo ratings yet
- 9 Nail Problems You Shouldn't Ignore: Spot Issues EarlyDocument10 pages9 Nail Problems You Shouldn't Ignore: Spot Issues EarlySvarogNo ratings yet
- Adults Community Acquired PneumoniaDocument7 pagesAdults Community Acquired PneumoniaDEth JU NafenNo ratings yet
- Rheumatic Heart Disease Causes, Symptoms, and TreatmentDocument4 pagesRheumatic Heart Disease Causes, Symptoms, and TreatmentJhen Jhen100% (1)
- Rheumatic Heart DiseaseDocument14 pagesRheumatic Heart Diseaseudaybujji100% (1)
- Research Paper Heart AttackDocument4 pagesResearch Paper Heart Attackmtxziixgf100% (1)
- Non Communicable MaterialDocument15 pagesNon Communicable Materialjennybrightz940No ratings yet
- VSD: Symptoms, Causes, Treatment of Ventricular Septal DefectDocument6 pagesVSD: Symptoms, Causes, Treatment of Ventricular Septal DefectFauzan Luthfi A MNo ratings yet
- Congenital Heart DiseaseDocument2 pagesCongenital Heart DiseaseZAY EMNo ratings yet
- Cardiac Infections: (Outside To Inside)Document7 pagesCardiac Infections: (Outside To Inside)Ashley MalsonNo ratings yet
- Rheumatic Heart Disease and Fever ExplainedDocument2 pagesRheumatic Heart Disease and Fever ExplainedDiaz RahmadiNo ratings yet
- Pericardial Effusio2Document7 pagesPericardial Effusio2bhelskieNo ratings yet
- Activity On Diseases of The Circulatory SystemDocument11 pagesActivity On Diseases of The Circulatory SystemMarisol Taloza RenonNo ratings yet
- Infective Endocarditis: Hariprasad KDocument28 pagesInfective Endocarditis: Hariprasad KHari Prasad K100% (1)
- Peripheral Arterial DseDocument2 pagesPeripheral Arterial Dsemiss RNNo ratings yet
- Non Communicable DiseasesDocument45 pagesNon Communicable DiseasesCess BuanNo ratings yet
- Carotid Artery Disease FlyerDocument2 pagesCarotid Artery Disease Flyerdinh son myNo ratings yet
- Is Any Type of Smoking Safe?Document9 pagesIs Any Type of Smoking Safe?Ore Perez CañeteNo ratings yet
- Causes Symptoms Diagnosis Treatment EndocarditisDocument12 pagesCauses Symptoms Diagnosis Treatment EndocarditisPriyanjali SainiNo ratings yet
- Toate Bolile CardiovasculareDocument6 pagesToate Bolile CardiovasculareAnca CopreanNo ratings yet
- Stroke ManagementDocument11 pagesStroke ManagementFercho MedNo ratings yet
- Peripheral Vascular Disease DiagnosisDocument2 pagesPeripheral Vascular Disease DiagnosisRchophell NamkhangNo ratings yet
- Health Module 6Document20 pagesHealth Module 6Kjwein Aia RivadeneiraNo ratings yet
- CHD Updated March 20Document69 pagesCHD Updated March 20Jibran Jones GarciaNo ratings yet
- 6 Surprising Signs of An Unhealthy HeartDocument3 pages6 Surprising Signs of An Unhealthy HeartDefault User100% (1)
- Bacterial EndocarditisDocument18 pagesBacterial Endocarditistherese100% (2)
- Heart DiseaseDocument40 pagesHeart DiseaseAhmer TahirNo ratings yet
- 1 What Is BleedingDocument4 pages1 What Is Bleedingbeba macasinagNo ratings yet
- Disorders Related To Respiration & CirculationDocument19 pagesDisorders Related To Respiration & Circulationsamria 2005No ratings yet
- How Does A Dog Get Endocarditis?Document4 pagesHow Does A Dog Get Endocarditis?YanNo ratings yet
- Abruptio PlacentaDocument36 pagesAbruptio PlacentaBriandon CanlasNo ratings yet
- ABRUPTIO PLACENTA Final 3.0Document51 pagesABRUPTIO PLACENTA Final 3.0Briandon CanlasNo ratings yet
- NanotechnologyDocument7 pagesNanotechnologyBriandon CanlasNo ratings yet
- City of TarlacDocument2 pagesCity of TarlacBriandon CanlasNo ratings yet
- Sickle Cell Sickle Cell Crisis 17Document2 pagesSickle Cell Sickle Cell Crisis 17Briandon CanlasNo ratings yet
- Tarlac Dike With The Biography of Kerima Polotan TuveraDocument2 pagesTarlac Dike With The Biography of Kerima Polotan TuveraBriandon Canlas86% (14)
- The Countries of The WorldDocument2 pagesThe Countries of The WorldBriandon CanlasNo ratings yet
- Introduction To Arduino: By: Brian Don CanlasDocument5 pagesIntroduction To Arduino: By: Brian Don CanlasBriandon CanlasNo ratings yet
- LaarniDocument4 pagesLaarniBriandon CanlasNo ratings yet
- LaarniDocument4 pagesLaarniBriandon CanlasNo ratings yet
- Bijender Sindhu, DR - Manoj Sharma, DR - Raj K Biraynia. Comparison of Clinic and Home Based Exercise Programs After Total Knee Arthroplasty A Pilot StudyDocument12 pagesBijender Sindhu, DR - Manoj Sharma, DR - Raj K Biraynia. Comparison of Clinic and Home Based Exercise Programs After Total Knee Arthroplasty A Pilot StudyDr. Krishna N. SharmaNo ratings yet
- TIMI Score Explained: Risk Assessment for NSTEMI, STEMI and Unstable AnginaDocument8 pagesTIMI Score Explained: Risk Assessment for NSTEMI, STEMI and Unstable AnginaBenny TrisaktyariNo ratings yet
- 12. Refer to12. Consult with cardiologist forcardiologist for further evaluationfurther evaluation and management.and managementDocument4 pages12. Refer to12. Consult with cardiologist forcardiologist for further evaluationfurther evaluation and management.and managementGiselle RomeroNo ratings yet
- World Health Organization Dimensions of Adherence.9Document7 pagesWorld Health Organization Dimensions of Adherence.9Lucky Radja PonoNo ratings yet
- Naturopathy Revised2014-15 01102015 PDFDocument103 pagesNaturopathy Revised2014-15 01102015 PDFRajesh KumarNo ratings yet
- Drug Dose Determination Using Pharmacokinetic PrinciplesDocument36 pagesDrug Dose Determination Using Pharmacokinetic PrinciplesSreya Sanil100% (1)
- Brintellix: What Is in This LeafletDocument5 pagesBrintellix: What Is in This LeafletFsNo ratings yet
- Methylene Blue Therapy of Viral DiseaseDocument15 pagesMethylene Blue Therapy of Viral DiseaseEstevam Dimas100% (1)
- Gary Earle ResumeDocument2 pagesGary Earle Resumeapi-310096159No ratings yet
- Impact Factor 2007Document81 pagesImpact Factor 2007PhilFrenchNo ratings yet
- MCFARLANE - 2016 - ARD - EULAR-recommendations - FibromyalgiaDocument11 pagesMCFARLANE - 2016 - ARD - EULAR-recommendations - FibromyalgiaTata2666No ratings yet
- Randomized Controlled TrialsDocument22 pagesRandomized Controlled TrialsJerome G ThampiNo ratings yet
- Children's Hospital of Eastern Ontario Pain Scale (CHEOPS)Document3 pagesChildren's Hospital of Eastern Ontario Pain Scale (CHEOPS)Nick O NeillNo ratings yet
- DV - Laringoskopi IndirekDocument4 pagesDV - Laringoskopi Indirekdies_vadisNo ratings yet
- AHM 250 4 Provider CompensationDocument16 pagesAHM 250 4 Provider Compensationdeepakraj610No ratings yet
- Interstitial Pulmonary PatternsDocument12 pagesInterstitial Pulmonary PatternsjohnNo ratings yet
- Otiflox New Ear DropsDocument9 pagesOtiflox New Ear DropsShreyas ModiNo ratings yet
- Wrist Fractures Recovery GuideDocument5 pagesWrist Fractures Recovery Guideat tNo ratings yet
- Prelim Round 2 IMDocument6 pagesPrelim Round 2 IMmld ozilNo ratings yet
- Cytodrug PrecationsDocument26 pagesCytodrug Precationsksumanpharma8801No ratings yet
- ALSANGEDY BULLETS FOR PACES Conversion DisorderDocument2 pagesALSANGEDY BULLETS FOR PACES Conversion DisordersohailsuNo ratings yet
- Chapter IIDocument31 pagesChapter IIyssa_03No ratings yet
- Famotidine (Pepcid)Document1 pageFamotidine (Pepcid)Adrianne BazoNo ratings yet
- Efficacy of Attachment-Based Family Therapy Compared To Treatment As Usual For Suicidal Ideation in Adolescents With MDDDocument11 pagesEfficacy of Attachment-Based Family Therapy Compared To Treatment As Usual For Suicidal Ideation in Adolescents With MDDGabriela MoralesNo ratings yet
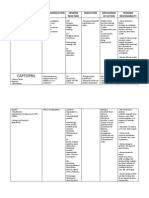
- Amlodipine Captopril MetronidazoleDocument5 pagesAmlodipine Captopril Metronidazolekhrysty1506No ratings yet
- Eating Disorders and The Internet: The Therapeutic PossibilitiesDocument7 pagesEating Disorders and The Internet: The Therapeutic PossibilitiesPaula SalidoNo ratings yet
- Etg MeningitisDocument1 pageEtg MeningitisAtika Indah SariNo ratings yet