Professional Documents
Culture Documents
Poster 1
Poster 1
Uploaded by
Fadel AhmadOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Poster 1
Poster 1
Uploaded by
Fadel AhmadCopyright:
Available Formats
ACINETOBACTER BAUMANNII RESISTEN
CARBAPENEM PADA VENTILATOR
ASSOCIATED PNEUMONIA
Fadel Ahmad Pratama, Irvan Medison, Dewi Wahyu Fitrina, Dessy Mizarti, Masrul Basyar, Sabrina Ermayanti
Department of Pulmonology and Respiratory Medicine, Faculty of Medicine Andalas University
BACKGROUND
Ventilator-associated pneumonia (VAP) is a Hospital Acquired Pneumonia (HAP) that occurs after 48 hours
of mechanical ventilation. VAP is one of the most common infections in the Intensive Care Unit (ICU) and
accounts 25% of ICU infections. Several studies have found that patients with HAP and VAP have a high
risk of infected by multidrug resistant bacteria associated with late onset VAP.
CASE ILLUSTRATION
• Female patient aged 32 years was consulted from the obstetrics department with post tracheostomy due
to indication of prolonged ventilator + P3A0H2 post vaginal partus + HELLP Syndrome + History of
decreased consciousness ec impending eclampsia antepartum + History of sepsis ec Intrauterine fetal
death (IUFD). Patients felt of increased shortness of breath since 2 days ago. Shortness of breath has been
felt since 20 days ago, tightness does decreases, increases with activity. The patient has been treated for 18
days. The patient was admitted to the ICU for 16 days with a 5-day ventilator attached and tracheostomy
was performed on day 6 of treatment in the ICU
• Examination of the patient's vital signs obtained, general condition of moderate pain, cooperative
composmentis awareness, blood pressure 130/79, HR 80x/min, RR: 22 x/min, T: 36.8 and SpO2: 98%
attached tracheostomy cannula with T-piece 5 lpm.
• Patients received ceftriaxone 2x2 grams and levofloxacin 1x750 mg for 2 days, then continued meropenem
3x1 grams and amikacin 1x1600 mg for 10 days. Patients received cefepime therapy 3x1 grams and
gentamicin 1x560 mg for 6 days.
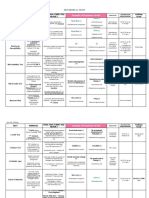
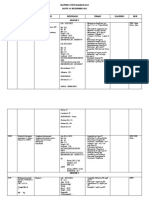
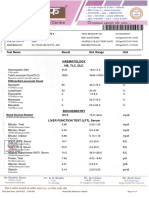
LABORATORY TEST RESULT RESULTS OF BLOOD GAS ANALYSIS
Haemoglobin 10,9 pH/ pCO2/ Effects of
10th
pO2/ 7,514/ 43,4/ 99/ metabolic
Hematocrti 35 August
HCO3/BE/ 35,3/ 11,5/ 96,5 alkalosis with
10th August 2022
Leukocyte 14.610 SpO2 mild ARDS
2022
Trombosit 189.000
GRAM STAINING RESULTS
Procalcitonin 11,4
Haemoglobin 11,7 Gram-positive coccus germ image,
25th July 2022
epithelium 0-1/LP, leukocytes > 25/LP
Hematocrti 33
15th August Leukocyte 8.510 4th August Gram-positive coccus germ image,
2022 2022 epithelium 0-1/LP, leukocytes > 25/LP.
Trombosit 302.000
Procalcitonin 0,52 10th August Gram-positive coccus germ image,
2022 epithelium 0-1/LP, leukocytes > 25/LP
Diffcount 0/0/0/62/25/9
CULTURE RESULTS AND SENSITIVITY OF BANAL SPUTUM GERMS
There are pathogenic bacteria Acinetobacter baumannii, isolated bacteria resistant to
carbapenems. Sensitivity results were obtained sensitive to Gentamicin and Trimethoprim /
25th July 2022 Sulfamethoxazole and Indeterminet to Tigecycline. Bacteria resistant to Ampicillin / Sulbactam,
Piperacillin / Tazobactam, Cefazolin, Ceftazidime, Ceftriaxone, Cefepime, Meropenem, Amikacin,
Ciprofloxacin.
There are pathogenic bacteria Acinetobacter baumannii, isolated bacteria resistant to
carbapenems. The sensitivity results were obtained sensitive to Tigecycline and resistant to
4th August 2022 Ampicillin / Sulbactam, Piperacillin / Tazobactam, Cefazolin, Ceftazidime, Ceftriaxone, Cefepime,
Meropenem, Amikacin, Gentamicin, Ciprofloxacin, Trimethoprim / Sulfamethoxazole.
10th August 2022 Same result on 4th August 2022
• Patients received ceftriaxone therapy 2x2 grams
and levofloxacin 1x750 mg for 2 days, then
continued meropenem 3x1 grams and amikacin
1x1600 mg for 10 days. Patients received cefepime
therapy 3x1 grams and gentamicin 1x560 mg for 6
days. When moved to the pulmonary treatment
room, patients received Tygecycline therapy
1x200 mg (i.v) the first day followed by 2x100 mg
H2 and so on, N acetylcysteine 2x200 mg (p.o)
and periodic suction. The patient is planned to
consul chest physiotherapy.
Figure 1. Thoracic photo dated 07/23/2022 (left), thoracic
DISCUSSION photo dated 08/03/2023 (right)
• Mechanical ventilation is an effective intervention
method to save the lives of critically ill patients CONCLUSION
and is often used in intensive care units.2
• VAP patients are at great risk of infection with
Increased duration of use of mechanical
multidrug-resistant bacteria.13 There are several
ventilation is associated with an increased
risk factors for antibiotic resistance in patients
incidence of VAP.7
such as treatment room factors, patient factors
REFERENCES
1. Perhimpunan Dokter Paru Indonesia (PDPI). Pneumonia Komuniti: Pedoman Diagnosis & Penatalaksanaan di and a history of previous pathogenic infections.
Indonesia. Perhimpun Dokter Paru Indonesia. 2019; 6: 1-52.
2. Wu D, Wu C, Zhang S, Zhong Y. Risk factors of ventilator-associated pneumonia in critically III patients. Front • Antibiotic therapy given based on the results of
Pharmacol. 2019;10: 1-7.
3. Li HY, Wang HS, Wang YL, Wang J, Huo XC, Zhao Q. Management of Ventilator-Associated Pneumonia: Quality
Asessment of Clinical Practice Guidelines and Variations in Recommendations on Drug Therapy for Prevention
the patient's sputum culture can provide good
and Treatment. Front Pharmacol. 2022; 13: 1-15.
4. Bougle A, Foucrier A, Dupont H, Montravers P, Ouattara A, Kalfon P, et al. Impact of the duration on antibiotics
outcomes.
on clinical events in patients with Pseudomonas aureginosa ventilator-associated pneumonia: study protocol
for a randomized controlled study. Trials BioMed Central. 2017; 18 (37): 1-8.
5. Xie X, Lyu J, Hussain T, Li M. Drug Prevention and Control of Ventilator-Associated Pneumonia. Front
Pharmacol. 2019;10: 1-9.
You might also like
- Hypnotic Self InductionDocument2 pagesHypnotic Self InductionDavid BradleuNo ratings yet
- Cognitive Therapy Scale Rating ManualDocument24 pagesCognitive Therapy Scale Rating Manualferreira.pipe3240No ratings yet
- How To Study Quickly and Effectively - 1. IntroductionDocument3 pagesHow To Study Quickly and Effectively - 1. IntroductionfuzzychanNo ratings yet
- Biochemical Tests in MicrobiologyDocument7 pagesBiochemical Tests in MicrobiologyKaoriMarieSembrano100% (1)
- The Death of James ForrestalDocument199 pagesThe Death of James ForrestalRich Wohltman100% (1)
- Psychiatric Case Clerking :)Document10 pagesPsychiatric Case Clerking :)Faiz Muhammad100% (4)
- nsg-436 Health Care Policy AnalysisDocument8 pagesnsg-436 Health Care Policy Analysisapi-491461037No ratings yet
- Report Geeti PaulDocument22 pagesReport Geeti PaulSAIKAT PAULNo ratings yet
- FIRST AID by Dr. Qasim AhmedDocument80 pagesFIRST AID by Dr. Qasim AhmedFaheem KhanNo ratings yet
- Clinical Trial ExecutionDocument5 pagesClinical Trial ExecutionSyeda Nishat Fathima TajNo ratings yet
- Nursing Laboratory and Diagnostic Tests Demystified, Second EditionFrom EverandNursing Laboratory and Diagnostic Tests Demystified, Second EditionNo ratings yet
- Conatct ListDocument58 pagesConatct ListBadal Bhattacharya50% (2)
- Poster 1Document1 pagePoster 1Fadel AhmadNo ratings yet
- Agua de Peptona Tamponada MerckDocument5 pagesAgua de Peptona Tamponada MerckLuz Katherine MartinezNo ratings yet
- Covid-19 RT PCR Test: Ms. Pranali Kakad Age/SexDocument1 pageCovid-19 RT PCR Test: Ms. Pranali Kakad Age/SexMOHINI ASWARNo ratings yet
- KARDIO 3 Desember 2022Document6 pagesKARDIO 3 Desember 2022IcutNo ratings yet
- EmbaDocument2 pagesEmbaIke Dian WahyuniNo ratings yet
- BacteriaDocument5 pagesBacteriaMohamed EssamNo ratings yet
- Dkab 328Document9 pagesDkab 328Bruno LopezNo ratings yet
- 10 1111@jcpt 13194Document5 pages10 1111@jcpt 13194Bladimir CentenoNo ratings yet
- SKANakhtarDocument2 pagesSKANakhtarSamreen KhanNo ratings yet
- Date 29/sep/2021 05:31PM 25/jul/21 09:13AM Unit Bio Ref IntervalDocument3 pagesDate 29/sep/2021 05:31PM 25/jul/21 09:13AM Unit Bio Ref IntervalUzma ZehraNo ratings yet
- Producing Kpc-Type Carbapenemases Mediated by Insertional Inactivation of The Phoq/Phop MGRB RegulatorDocument6 pagesProducing Kpc-Type Carbapenemases Mediated by Insertional Inactivation of The Phoq/Phop MGRB RegulatorABachiraya MongkhunNo ratings yet
- Coa Vitamin C R02Document1 pageCoa Vitamin C R02paulinaNo ratings yet
- 7.2 BacteriologyDocument12 pages7.2 BacteriologyClinical PharmersNo ratings yet
- Netz, 2002Document7 pagesNetz, 2002olindacabralNo ratings yet
- 418 515 AST-N327: Summary and Explanation Instructions For UseDocument3 pages418 515 AST-N327: Summary and Explanation Instructions For Usealesraa jawharatNo ratings yet
- Cefiderocol Resistance in Acinetobacter BaumanniiDocument4 pagesCefiderocol Resistance in Acinetobacter Baumanniiczikkely23No ratings yet
- Dia. Microbiology Lab 7Document4 pagesDia. Microbiology Lab 7alhaitham alqmeNo ratings yet
- Coa Vitamin ADocument1 pageCoa Vitamin ApaulinaNo ratings yet
- Cefadroxil Drug ProfileDocument17 pagesCefadroxil Drug ProfileChaudryNomiNo ratings yet
- Sanz Et Al 2024 KPC 2 Allelic Variants in Klebsiella Pneumoniae Isolates Resistant To Ceftazidime Avibactam FromDocument13 pagesSanz Et Al 2024 KPC 2 Allelic Variants in Klebsiella Pneumoniae Isolates Resistant To Ceftazidime Avibactam FromABMOHENo ratings yet
- 06 COA HYDROGEL MASK p01Document1 page06 COA HYDROGEL MASK p01paulinaNo ratings yet
- DAFTAR OBAT Troli Emergensi UNIT BEDAHDocument2 pagesDAFTAR OBAT Troli Emergensi UNIT BEDAHfarmasimoestopoNo ratings yet
- Assessment of in Vitro Antifungal Efficacy and in Vivo Toxicity of Amphotericin B-Loaded Plga and Plga-Peg Blend NanoparticlesDocument11 pagesAssessment of in Vitro Antifungal Efficacy and in Vivo Toxicity of Amphotericin B-Loaded Plga and Plga-Peg Blend NanoparticlesNurul syam annisaNo ratings yet
- COVID-19 Therapeutics Tracker: United Kingdom Japan China United States JapanDocument8 pagesCOVID-19 Therapeutics Tracker: United Kingdom Japan China United States JapantucchaNo ratings yet
- Cbcicompleteblood Count) : Patient NameDocument6 pagesCbcicompleteblood Count) : Patient NameGauravNo ratings yet
- Pet. SAM: 19020515 / 1585: 10 Months /: /: Dr. Kalleshwar: 18-02-2019 AT 07:54 PM: Anand Pet Clinic: 18-02-2019 AT 08:15 PMDocument1 pagePet. SAM: 19020515 / 1585: 10 Months /: /: Dr. Kalleshwar: 18-02-2019 AT 07:54 PM: Anand Pet Clinic: 18-02-2019 AT 08:15 PMShreya KrishnamurthyNo ratings yet
- Organism: Pseudomonas Species - Scanty GrowthDocument2 pagesOrganism: Pseudomonas Species - Scanty GrowthRitvik BasnotraNo ratings yet
- ReportDocument1 pageReportJeet SharmaNo ratings yet
- Principle General Information Experimental Procedure and EvaluationDocument2 pagesPrinciple General Information Experimental Procedure and Evaluationayuningtyas wahyuNo ratings yet
- Advances in Biomolecular Medicine - Molecular Detection of DHA-1 AmpC Beta-Lactamase Gene in Enterobacteriaceae Clinical Isolates in IndonesiaDocument5 pagesAdvances in Biomolecular Medicine - Molecular Detection of DHA-1 AmpC Beta-Lactamase Gene in Enterobacteriaceae Clinical Isolates in IndonesiabungaNo ratings yet
- 1981 - Ekramoddoullah, Kisil, Sehon - Isolation of Allergenically Active Cytochrome C From Kentucky Blue Grass PollenDocument10 pages1981 - Ekramoddoullah, Kisil, Sehon - Isolation of Allergenically Active Cytochrome C From Kentucky Blue Grass Pollenpond_1993No ratings yet
- Mapping GEH 1 9 22Document3 pagesMapping GEH 1 9 22naufalNo ratings yet
- Vectores y PlasmidosDocument7 pagesVectores y PlasmidosSarita UrbanoNo ratings yet
- Granucult™ VRB (Violet Red Bile Lactose) Agar Acc. Iso 4832 and Fda-BamDocument4 pagesGranucult™ VRB (Violet Red Bile Lactose) Agar Acc. Iso 4832 and Fda-BamnoeNo ratings yet
- BijuDocument1 pageBijusujith sureshNo ratings yet
- Mapping Aqshai (Iso) DPJP:DR - Evamusdalita, SP - PD Cow:Dr. Intandandr. Reza Senin, 20 November 2017Document10 pagesMapping Aqshai (Iso) DPJP:DR - Evamusdalita, SP - PD Cow:Dr. Intandandr. Reza Senin, 20 November 2017Luthfi LazuardiNo ratings yet
- 10.33073 - PJM 2022 023Document6 pages10.33073 - PJM 2022 023Andy SetiawanNo ratings yet
- PDF TextDocument3 pagesPDF TextABHISHEK SINGHNo ratings yet
- Membranas 2020 ModDocument23 pagesMembranas 2020 Modmordecai 21No ratings yet
- Merck Rebrand - 100908 - 1907Document5 pagesMerck Rebrand - 100908 - 1907Paula BautistaNo ratings yet
- Mede BlobDocument2 pagesMede BlobRahamTullaNo ratings yet
- Cloning and Expression of A Conjugated Bile Acid Hydrolase Gene From Lactobacillus Plantarum by Using A Direct Plate AssayDocument7 pagesCloning and Expression of A Conjugated Bile Acid Hydrolase Gene From Lactobacillus Plantarum by Using A Direct Plate AssayChris Letchford-JonesNo ratings yet
- Induction of Erythrocyte Shrinkage by OmeprazoleDocument5 pagesInduction of Erythrocyte Shrinkage by OmeprazoleANDREA ARIAS RIOSNo ratings yet
- Abhrak Bhasma (Biotite Mica Nanoparticles) Induces Cytotoxicity in Adenocarcinoma Human Alveolar Basal Epithelial Cells (A549)Document6 pagesAbhrak Bhasma (Biotite Mica Nanoparticles) Induces Cytotoxicity in Adenocarcinoma Human Alveolar Basal Epithelial Cells (A549)International Journal of Innovative Science and Research Technology100% (1)
- Webinar Difteri RSHSDocument11 pagesWebinar Difteri RSHSAndy JoeyNo ratings yet
- M17 Agar Terzaghi 115108 (BAL)Document1 pageM17 Agar Terzaghi 115108 (BAL)João PauloNo ratings yet
- Biwako NagahamaDocument24 pagesBiwako NagahamaAditya BasuNo ratings yet
- Cap. 7 Stoichiometry of Microbial Growth and Product Formation - M.Schuler F. Kargi - 2002Document12 pagesCap. 7 Stoichiometry of Microbial Growth and Product Formation - M.Schuler F. Kargi - 2002Kelvin JimenezNo ratings yet
- Leptospirosis Serodiagnosis by The Microscopic Agglutination Test. Current Protocols in MicrobiologyDocument18 pagesLeptospirosis Serodiagnosis by The Microscopic Agglutination Test. Current Protocols in Microbiologyscribd.glowing960No ratings yet
- Epidermidis Biofilms: Activity of Gallidermin On Staphylococcus Aureus and StaphylococcusDocument7 pagesEpidermidis Biofilms: Activity of Gallidermin On Staphylococcus Aureus and StaphylococcusnimertaNo ratings yet
- Glyconanoparticles For Targeted Tumor Therapy of Platinum Anticancer DrugDocument11 pagesGlyconanoparticles For Targeted Tumor Therapy of Platinum Anticancer DrugssNo ratings yet
- 6 Antibiotic AbbreviationsDocument2 pages6 Antibiotic AbbreviationsDeladem EmmanuelNo ratings yet
- Molecular Detection of Virulence Factors (Adhesion Genes) in Some Staphylococcus Epidermidis Locally Isolated From Different Clinical SourcesDocument5 pagesMolecular Detection of Virulence Factors (Adhesion Genes) in Some Staphylococcus Epidermidis Locally Isolated From Different Clinical SourcesKanhiya MahourNo ratings yet
- Eosin Methylene Blue Agar (EMB) : IndustryDocument2 pagesEosin Methylene Blue Agar (EMB) : Industrysigit the pembalapNo ratings yet
- You Can Offer Your Staff More Than 100 CE CreditsDocument2 pagesYou Can Offer Your Staff More Than 100 CE Creditsiq_dianaNo ratings yet
- Lapsus ArdiansyahDocument18 pagesLapsus ArdiansyahAFifah THamrinNo ratings yet
- Anti-Bacterial Effect of Extracts of Ocimum On Imipenem Resistant Gram Negative Bacteria Isolated From Burn Wound InfectionsDocument6 pagesAnti-Bacterial Effect of Extracts of Ocimum On Imipenem Resistant Gram Negative Bacteria Isolated From Burn Wound Infectionsvijaylatha rastogi100% (1)
- BibliographyDocument2 pagesBibliographyelvie21No ratings yet
- Genapril PDFDocument64 pagesGenapril PDFChoubey RanjeetNo ratings yet
- Demo Nail Care 7Document21 pagesDemo Nail Care 7Naddie SlaNo ratings yet
- 5 Management of URIs in Elective Surgery 2018Document8 pages5 Management of URIs in Elective Surgery 2018Yan Zhen YuanNo ratings yet
- EMS Pocket: Prehospital Reference GuideDocument10 pagesEMS Pocket: Prehospital Reference GuideStefanNo ratings yet
- CPR (Adult, Child, Infant)Document6 pagesCPR (Adult, Child, Infant)Ilyes FerenczNo ratings yet
- Importing General Medical DeviceDocument6 pagesImporting General Medical Devicebrbbk2No ratings yet
- VICH GL9 Good Clinical PraticeDocument30 pagesVICH GL9 Good Clinical Praticejulio_pastoreNo ratings yet
- 2016 Healthcare OutlookDocument38 pages2016 Healthcare OutlookeliforuNo ratings yet
- Jonathan Sudharta e - PrescriptionDocument53 pagesJonathan Sudharta e - PrescriptionAchmad FachryNo ratings yet
- Types of Cerebral PalsyDocument6 pagesTypes of Cerebral PalsySahil SahniNo ratings yet
- Syllabus: First B.H.M.S. Examination (Direct Course) II) Homoeopathic PharmacyDocument22 pagesSyllabus: First B.H.M.S. Examination (Direct Course) II) Homoeopathic Pharmacyms.anitha1980No ratings yet
- Diabetic MedicationsDocument2 pagesDiabetic Medicationsapi-288062111No ratings yet
- 12 Physical Education Hindi Medium Chapter 5Document23 pages12 Physical Education Hindi Medium Chapter 5KRISHAN KUMARNo ratings yet
- Laboratory Exercise No. 18 Urinary System I. Assessment Answer Each Item Guided by The Specific Instructions For Each Question Set. A. True/FalseDocument2 pagesLaboratory Exercise No. 18 Urinary System I. Assessment Answer Each Item Guided by The Specific Instructions For Each Question Set. A. True/FalseGalerose MalvarNo ratings yet
- JAK Neural PlasticityDocument15 pagesJAK Neural PlasticityOwais KhanNo ratings yet
- Haematology & CoagulationDocument1 pageHaematology & CoagulationRahilalab HydNo ratings yet
- Phytochemical and Pharmacological Review of Maja (Aegle Marmelos)Document24 pagesPhytochemical and Pharmacological Review of Maja (Aegle Marmelos)h_rivaiNo ratings yet
- Marketing Authorisation Application Maa Pre Submission Meeting Request Form Human - enDocument25 pagesMarketing Authorisation Application Maa Pre Submission Meeting Request Form Human - ensridevi100% (1)
- Common Medication Prefixes and Suffixes: Prefix/Suffix Class ExamplesDocument5 pagesCommon Medication Prefixes and Suffixes: Prefix/Suffix Class ExamplesZoe Brown-CrossNo ratings yet
- SH0518Document12 pagesSH0518Anonymous 9eadjPSJNgNo ratings yet