Professional Documents
Culture Documents
Care of Clients With Gastrointestinal Disorders
Care of Clients With Gastrointestinal Disorders
Uploaded by
Marie Antionette MondragonOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Care of Clients With Gastrointestinal Disorders
Care of Clients With Gastrointestinal Disorders
Uploaded by
Marie Antionette MondragonCopyright:
Available Formats
Care of Clients with
Gastrointestinal Disorders
Abdominal Pain Nausea and Vomiting
O Onset: “When did the pain begin?” Nausea is a vague, uncomfortable sensation of
sickness that may or may not be followed by
Location: “Please point where exactly you vomiting
L fee the pain.” Vomiting is a physiologic protective response
Duration: “How long does the pain last?” that limits the effects of noxious agents by
D emptying the stomach contents and secretions
Characteristic: “Please describe the pain of small intestine
C you feel in your abdomen.” Triggers: odors, activity, medications, food
intake
A Aggravating: “What triggers the pain?”
R Relieving: “What relieves the pain?”
Change in Bowel Habits
Diarrhea: an abnormal increase in frequency
T Timing: “When does the pain occur?” and liquidity of stool or in daily stool weight or
volume
S Severity: “Please rate your pain from 1-10” Commonly occurs when the contents move
so rapidly through the intestine and colon that
there is inadequate time for the GI secretions
Dyspepsia and oral contents to be absorbed.
Constipation: a decrease in frequency of
stool, or stools that are hard, dry, and of
Upper abdominal discomfort associated with smaller volume than typical
eating
Most common symptom of patients with GI
dysfunction
Typically caused by fatty foods, salads,
Change in Stool
coarse vegetables, and highly seasoned foods Characteristics
Normal stool
Intestinal Gas light to dark brown
Accumulation of gas in GI tract Melena
Belching: expulsion of gas from stomach Black tarry stool indicative of upper GI
through the mouth bleeding
Flatulence: expulsion of gas from the rectum
May indicate food intolerance or gallbladder Hematochezia
disease Bright red blood in stool
Steatorrhea
Fatty stool
Latent phase
Alcoholic stool
light- gray or clay- colored stool resulting
from decreased or absent conjugated bilirubin
Diagnostic Tests for GI UGI Tract Study (Barium Swallow)
Visualizes esophagus, stomach, duodenum, and
Disorders jejunum
Contrast medium: Barium sulfate – white,
chalky substance
Fecal Occult Blood Test (FOBT)/ Guaiac Test X-rays are taken on standing and lying position
Stool for occult blood Nursing interventions:
Done to detect GI bleeding Pre-procedure:
Preparation: • NPO 6-8 hours
• High fiber diet for 48-72 hours Post-procedure:
• Avoid red meat, poultry, turnips, horse radish, • Laxatives, as ordered
cauliflower, and melon – false positive result • Increase OFI
• Avoid vitamin C – false negative result • Inform client that stool may become white
• Hold 48hrs prior: steroids, iron, indomethacin, for 24-72 hours
colchicine LGI Tract Study (Barium Enema)
3 stool specimens will be collected for three Visualization of colon through x- rays after
consecutive days rectal installation of barium
Stool for Ova, Parasites, and E. histolytica (OPEH) Barium enema is C/I for patients with active
Clean technique inflammatory diseases, fistula, or suspected
Send fresh, warm specimen (within 30 mins) perforation of colon.
• Diatrizoic acid is used instead (watersoluble
Stool for Culture and Sensitivity iodinated contrast medium)
Nursing interventions:
Identifies microorganism and determines • Low- residue diet 1 to 2 days before
appropriate antibiotic therapy • Clear liquid diet and laxative the evening
Sterile technique before
Use sterile collection tube and sterile cotton- • NPO post-midnight
tipped applicator to collect specimen • Cleansing enema until clear in AM of
Abdominal Ultrasound (UTZ) procedure
• Schedule before any upper GI studies
Ultrasonography is a noninvasive diagnostic
technique in which high- frequency sound Computed Tomography (CT) Scan
waves are passed into the internal body Provides cross- sectional images of abdominal
structures, and the ultrasonic echoes are organs and structures.
recorded on an oscilloscope as they strike Used to detect and localize many inflammatory
tissues of different densities. conditions in the colon (appendicitis,
Used to detect: diverticulitis, regional enteritis, and ulcerative
• Enlargement of gallbladder, pancreas, colitis)
presence of gallstones, ectopic pregnancy, Painless procedure, but uses radiation
appendicitis Nursing interventions:
Sound waves cannot travel through bones, gas, • Clear liquid diet in AM
or fluid • If using contrast medium:
Nursing interventions: • NPO 2-4 hours
• NPO 8 to 12 hours prior to UTZ • Check for allergies to seafood and iodine
• If for gallbladder studies, fat-free meal the • Assess for claustrophobia
evening before • Instruct client to remain still during entire
• Schedule barium studies after ultrasonography procedure
since barium interferes with sound wave
transmission
Magnetic Resonance Imaging (MRI) Nursing Interventions (Post op):
Noninvasive technique that uses magnetic fields • Position to supine for a few minutes
and radiowaves to produce images of area • Assess for signs of perforation – bleeding,
being studied pain, fever
Used to evaluate abdominal soft tissues as well • Hot Sitz bath to relieve discomfort in
as blood vessels, abscesses, fistulas, anorectal area
neoplasms, and other sources of bleeding
Nursing Interventions:
• Pre- procedure:
Common Nursing Procedures
• NPO 6-8 hours
• Remove all jewelries and other metals
• Inform patient and family that procedure
for Clients with GI Disorders
lasts for 60 to 90 minutes, inform that the MRI Gastrointestinal Decompression
machine will make a knocking sound during the
procedure Enteral Feeding (NGT, PEG/PEJ)
• Assess for claustrophobia
Contraindications:
• Pacemakers Parenteral Nutrition
• Aneurysm clips Gastric and Intestinal Decompression
• Orthopedic screws
The removal of gas or fluid to prevent
Upper GI Endoscopy gastric and intestinal distention
Direct visualization of esophagus, stomach, and Achieved through the use of nasogastric
duodenum tubes (NGT) or nasoenteric tubes
Nursing interventions (Pre op): Nasoenteric Tubes
• Obtain written consent
• NPO 6-8 hours Nursing interventions:
• Administer Atropine sulfate, as ordered After insertion of nasoenteric tubes, turn
• Administer sedatives/narcotics/tranquilizers, patient to the RIGHT side. This facilitates
as ordered passage of tube to the duodenum.
• Remove dentures or bridges Shortening of length of tube from the outside
• Lidocaine spray is applied to the posterior indicates passage of tube to duodenum
pharynx to depress gag reflex.
• Instruct not to swallow saliva Enteral Feeding
Nursing Interventions (Post op): Nasogastric Tube Feeding
• Position to side- lying position Also called gastric gavage
• NPO until gag reflex returns Feeding formula should be at ROOM
• NSS gargle TEMPERATURE. Cold formula causes cramps.
• Monitor VS Position: semi- fowler’s to high- fowler’s
• Assess: bleeding, crepitus, fever, neck/throat Check NGT placement:
pain, dyspnea, dysphagia, back/shoulder pain • BEST- x-ray
Lower GI Endoscopy • Check pH of Gastric secretions (Should
be acidic with pH of 1-3)
Proctosigmoidoscopy • Note color of aspirate (greenish or
yellowish)
Direct visualization of sigmoid and rectum • Introduce 10 mL of air into NGT and
Colonoscopy auscultate epigastric area for gurgling sounds
After each feeding, instill 30 to 60 mL of
Direct visualization of the colon water
Nursing Interventions (Pre op) Have the client remain in semi- to high-
• Obtain written consent fowler’s position for 30 to 60 minutes after
• Clear liquid diet 24 hours before procedure feeding
• Administer laxative/cathartic, as ordered
• Cleansing enema until clear
• Position to knee-chest/lateral position during
procedure
• Assess for vasovagal stimulation
Gastrostomy/Jejunostomy Feeding Total Parenteral Nutrition (TPN)
Primary purpose: to administer glucose
Gastrostomy Indications:
stoma is in the stomach • Clients who need extensive nutritional support
A procedure in which an opening is created over an extended period of time
into the stomach either for the purpose of • Site of catheter insertion: SUBCLAVIAN vein
administering nutrition, fluids, and medications • Type of solution: hypertonic (25% to 35%
via a feeding tube, or for gastric dextrose)
decompression. Nursing interventions:
Preferred way of enteral feeding for • Administer TPN at ROOM TEMPERATURE •
nutritional support of greater than 4 weeks Consume TPN within 24 hours
• Change IV tubing every 24 hours
Jejunostomy • Use an infusion pump to maintain a steady
stoma is in the jejunum infusion rate
A surgically placed opening in the jejunum for • If infusion is delayed, DO NOT catch up.
the purpose of administering nutrition, fluids, Notify physician.
and medications • Monitor urine and blood glucose levels.
Indicated when gastric route is not accessible, • Provide skin care on the catheter insertion
or to decrease aspiration risk when stomach site
is not functioning adequately to process and
empty food or fluids The removal of gas or fluid to prevent
gastric and intestinal distention
Achieved through the use of nasogastric
tubes (NGT) or nasoenteric tubes
Nasoenteric Tubes
Nursing interventions:
After insertion of nasoenteric tubes, turn
patient to the RIGHT side. This facilitates
passage of tube to the duodenum.
Shortening of length of tube from the outside
indicates passage of tube to duodenum
Enteral Feeding
Nasogastric Tube Feeding
Also called gastric gavage
Feeding formula should be at ROOM
Gastrostomy Jejunostomy TEMPERATURE. Cold formula causes cramps.
Gastrostomy/Jejunostomy Feeding Position: semi- fowler’s to high- fowler’s
Check NGT placement:
Feeding should be at ROOM temperature • BEST- x-ray
Position: semi- to high- fowler’s position • Check pH of Gastric secretions (Should
Check patency: be acidic with pH of 1-3)
• Instill 15 to 30 ml of water • Note color of aspirate (greenish or
Have the client remain in semi- to high fowler's yellowish)
position for 30 to 60 mins after feeding • Introduce 10 mL of air into NGT and
auscultate epigastric area for gurgling sounds
Parenteral Nutrition After each feeding, instill 30 to 60 mL of
A method of providing nutrients to the body water
by an IV route Have the client remain in semi- to high-
Goals: fowler’s position for 30 to 60 minutes after
• To improve nutritional status feeding
• Establish a positive nitrogen balance
• Maintain muscle mass
• Promote weight maintenance or gain
• Enhance healing process
Positive Nitrogen Balance
Positive nitrogen balance is necessary to
create an anabolic environment, allowing the
body to build new muscle
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5807)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (346)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- NotesDocument4 pagesNotesMarie Antionette MondragonNo ratings yet
- Green and Brown UI Frame Style Types of Bullying PosterDocument3 pagesGreen and Brown UI Frame Style Types of Bullying PosterMarie Antionette MondragonNo ratings yet
- Diagnostic Testing For Urinary System DisordersDocument3 pagesDiagnostic Testing For Urinary System DisordersMarie Antionette MondragonNo ratings yet
- Brown Abstract Things To Do List and PlannerDocument3 pagesBrown Abstract Things To Do List and PlannerMarie Antionette MondragonNo ratings yet
- 13 Principles of Aseptic TechniqueDocument1 page13 Principles of Aseptic TechniqueMarie Antionette MondragonNo ratings yet
- D. NCM 234-Medical ConditionsDocument77 pagesD. NCM 234-Medical ConditionsMarie Antionette MondragonNo ratings yet
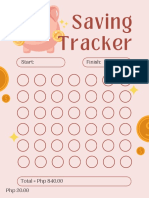
- Saving Tracker: Start: FinishDocument6 pagesSaving Tracker: Start: FinishMarie Antionette MondragonNo ratings yet
- Preop NotesDocument10 pagesPreop NotesMarie Antionette MondragonNo ratings yet
- Record of Newborn CareDocument1 pageRecord of Newborn CareMarie Antionette MondragonNo ratings yet
- Importance of LipidsDocument1 pageImportance of LipidsMarie Antionette MondragonNo ratings yet
- A. NCM 234 - REPRODUCTIVE FUNCTION DISORDERS (Week 3)Document57 pagesA. NCM 234 - REPRODUCTIVE FUNCTION DISORDERS (Week 3)Marie Antionette MondragonNo ratings yet
- Digital Scrapbook - Espina - n1Document15 pagesDigital Scrapbook - Espina - n1Marie Antionette MondragonNo ratings yet
- SIRITUAL NEEDS QUESTIONNAIRE (SPQN)Document3 pagesSIRITUAL NEEDS QUESTIONNAIRE (SPQN)Marie Antionette MondragonNo ratings yet
- B. NCM 234 - SEXUALLY TRANSMITTED DISEASES (Week 3)Document134 pagesB. NCM 234 - SEXUALLY TRANSMITTED DISEASES (Week 3)Marie Antionette MondragonNo ratings yet
- Classification of FatsDocument2 pagesClassification of FatsMarie Antionette MondragonNo ratings yet
- 7 - Asian RegionalismDocument33 pages7 - Asian RegionalismMarie Antionette MondragonNo ratings yet
- Line Dance ModuleDocument34 pagesLine Dance ModuleMarie Antionette MondragonNo ratings yet
- Global Governance - 5Document44 pagesGlobal Governance - 5Marie Antionette MondragonNo ratings yet
- The Globalization of Religions - 6Document24 pagesThe Globalization of Religions - 6Marie Antionette MondragonNo ratings yet
- 6 - The World of RegionsDocument38 pages6 - The World of RegionsMarie Antionette MondragonNo ratings yet
- Why Dragonpay?: Compared With Other Platforms, Fao Can Confirm and Verify Payments Faster Via DragonpayDocument10 pagesWhy Dragonpay?: Compared With Other Platforms, Fao Can Confirm and Verify Payments Faster Via DragonpayMarie Antionette MondragonNo ratings yet
- TimelineDocument12 pagesTimelineMarie Antionette MondragonNo ratings yet