Professional Documents
Culture Documents
Faith-Based Delivery of Science-Based Care
Uploaded by
lepanto3535Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Faith-Based Delivery of Science-Based Care
Uploaded by
lepanto3535Copyright:
Available Formats
Comment
Faith-based delivery of science-based care
Faith is too often perceived as a force that divides. In Criticism of the influence of dogma on practice can Published Online
July 7, 2015
The Lancet, a new Series1–3 examines the potential of faith- arise from an incomplete appreciation of the doctrinal http://dx.doi.org/10.1016/
based health care to unite and heal. The Series is led by basis that frames different approaches to health. In the S0140-6736(15)61104-7
Ed Mills, from Global Evaluative Sciences in Vancouver, second Series paper, Andrew Tomkins and coauthors,2 See Comment pages e22
and e24
Canada, and supported financially by a grant from Capital who come from several religious traditions, examine the
See Series pages 1765, 1776,
for Good, which connects donors with organisations basis for controversies in faith and health, and separate and 1786
working in health and other development areas. This myths from messages. They provide faith-based For Capital for Good see
http://www.capitalforgood.org
Lancet Series on faith-based health care draws together explanations for different practices that are valuable to
the insights and experiences of authors from several any clinician in a multifaith environment. Appreciation
countries and denominations, academic institutions, and of spiritual, social, and cultural dimensions of health are
non-governmental organisations (NGOs). Faith-based crucial to care.6 Better understanding of the reasons for
organisations deliver a substantial volume of health care, different practices provides opportunities to reframe
and their common visions of stewardship, inclusiveness, faith as part of the solution, rather than the problem, in
dignity, and justice make many such organisations complex consultations.
ideally suited as key partners for delivering the post-2015 Jean Duff and Warren Buckingham III3 conclude
Sustainable Development Goals. the Series with five recommendations to facilitate
Religions are about more than good deeds; yet they collaboration between governments and NGOs with
also inspire behaviours and actions as an expression of faith-based entities, which build on existing strengths to
faith, which can benefit others. For instance, respect for improve health outcomes. Among these is the need for
the diversity of the natural world and preservation of improved measurement of the benefits that faith-based
its resources and habitats. Service—particularly care for organisations bring to health-care delivery and outcomes.
the sick—is another characteristic. In that care, faith is Faith-based organisations translate beliefs into
regularly present, even though it may be silent. Faith is action through funding, commissioning, researching,
interwoven with local culture and overlaid by personal or providing care. By studying the presence and unique
beliefs and organised religions that can make the attributes of faith-based care through the lens of health,
disentanglement of individual components a challenge. this Series provides a platform for broader engagement
The purpose of this Series is to examine how faith-based between faith-based groups, medical practitioners,
behaviours influence the delivery of health care at an and policy makers. Such engagement, and better
organisational level. A vivid example is the response to recognition and utilisation of faith-inspired behaviours,
the Ebola outbreak, as described in a Comment for this
Series by Katherine Marshall and Sally Smith.4
In the first Series paper, Jill Olivier and colleagues1
analyse the characteristics of faith-based care in Africa. A
particular strength of faith-inspired organisations is the
care they give to populations marginalised by poverty or
stigma. Such faith-based care complements government
facilities and extends the reach of services beyond
traditional populations. Indeed, faith-based organisations
account for about 20% of the total number of agencies
working to combat HIV/AIDS in Africa.5 To maximise the
contributions of faith-based care, it is essential that such
Philippe Lissac/Godong/Corbis
providers are as professional in their organisation and
management of human resources, and as evidence-based
in practice, as any other health-care provider. The faith
moniker does not excuse shortcomings.
www.thelancet.com Vol 386 October 31, 2015 1709
Comment
has the potential to accelerate and improve health and 3 Duff JF, Buckingham WW III. Strengthening of partnerships between the
public sector and faith-based groups. Lancet 2015; published online July 7.
social outcomes. http://dx.doi.org/10.1016/S0140-6736(15)60250-1.
4 Marshall K, Smith S. Religion and Ebola: learning from experience.
Lancet 2015; published online July 7. http://dx.doi.org/10.1016/
William Summerskill, Richard Horton S0140-6736(15)61082-0.
The Lancet, London EC2Y 5AS, UK 5 WHO. The world health report 2004: changing history, community
participation in public health. Geneva: World Health Organization, 2004.
1 Olivier J, Tsimpo C, Gemignani R, et al. Understanding the roles of faith-
based health-care providers in Africa: review of the evidence with a focus 6 General Medical Council. Good clinical practice. Manchester: General
on magnitude, reach, cost, and satisfaction. Lancet 2015; published online Medical Council, 2014. http://www.gmc-uk.org/static/documents/
July 7. http://dx.doi.org/10.1016/S0140-6736(15)60251-3. content/Good_medical_practice_-_English_0914.pdf (accessed June 13,
2015).
2 Tomkins A, Duff J, Fitzgibbon A, et al. Controversies in faith and health
care. Lancet 2015; published online July 7. http://dx.doi.org/10.1016/
S0140-6736(15)60252-5.
Long working hours: an avoidable cause of stroke?
Published Online William Osler, in an article about atherosclerosis comprising more than 5 million person-years of follow-
August 20, 2015
http://dx.doi.org/10.1016/
published 100 years ago, wrote that the main cause up, including not only myocardial infarction but also
S0140-6736(15)61000-5 of myocardial infarction was “wear and tear of life”.1 stroke as endpoints. So far, Kivimäki and colleagues’
See Articles page 1739 Although we now have more detailed theories regarding results provide the strongest indication of a causal
the causal mechanisms, there is still some kinship association between long working hours and an aspect
between modern studies of work-related determinants of cardiovascular disease—namely, stroke. On the other
of cardiovascular diseases and Osler’s broad approach to hand, the authors report a less convincing association
the cause of disease.2 between long working hours and coronary heart
One important aspect of work environment is working disease (RR 1·13, 95% CI 1·02–1·26). Because coronary
time. Long working hours correlate with increased heart disease is more prevalent than stroke in people
incidence of cardiovascular diseases and their risk of working age,8 this finding is an interesting one
factors.3,4 However, contradictory results show that that has probably been missed because of the smaller
long working hours are not associated with increased populations studied previously.
risk of metabolic syndrome.5 In a working paper from In the present study, the investigators were able to
2003, White and Beswick reviewed 66 studies from adjust for various confounding factors (ie, age, sex,
1920 to 2002 with a guarded conclusion that there are socioeconomic status, smoking, body-mass index,
“…potentially negative effects of working long hours physical activity, and alcohol consumption). But, as in
on physical health. The strongest evidence probably many epidemiological studies, outcome is measured
concerns the links with cardiovascular disorder…”.6 with better accuracy than exposure—working time
In The Lancet, Miki Kivimäki and colleagues7 present is self-assessed and measured just once. And, as in
findings from a meta-analysis of long working all observational studies, there could be selection
hours and risk of cardiovascular disease, based on effects (eg, work involvement—the degree to which an
both published and unpublished data, for up to employee is engaged in and enthusiastic about doing
603 838 men and women from 24 cohorts in Europe, his or her work) and confounding factors (eg, workload
the USA, and Australia. The investigators conclude or sleeping hours) that are not controlled for.
that, compared with standard working hours of Prevention of cardiovascular diseases almost
35–40 h per week, long working hours (defined as exclusively focuses on medical and individual preventive
working ≥55 h per week) are a risk factor mainly for measures.9 Findings from other studies have shown
stroke (relative risk [RR] 1·33, 95% CI 1·11–1·61), with that this approach is not always simple and tends to
estimates showing a dose–response association (RR increase inequities in health, because individuals with
1·10 [95% CI 0·94–1·28] for 41–48 h, 1·27 [1·03–1·56] the most favourable socioeconomic situation are often
for 49–54 h, and 1·33 [1·11–1·61] for ≥55 h per week). the most successful in implementing these preventive
The study is a pioneering one because of its large scale, activities.10
1710 www.thelancet.com Vol 386 October 31, 2015
You might also like
- The en Cultured Body-BookDocument174 pagesThe en Cultured Body-BooksidorelaNo ratings yet
- Peer Support Within A Health Care Context - A Concept AnalysisDocument12 pagesPeer Support Within A Health Care Context - A Concept AnalysisretnoNo ratings yet
- Ecg Essentials 2 PDFDocument45 pagesEcg Essentials 2 PDFjaikishan marathe 69No ratings yet
- Acute Heart FailureDocument71 pagesAcute Heart FailureVivek Anandan100% (1)
- Flourishing: Health, Disease, and Bioethics in Theological PerspectiveFrom EverandFlourishing: Health, Disease, and Bioethics in Theological PerspectiveNo ratings yet
- Solution Manual For Statistics For Nursing Research A Workbook For Evidence Based Practice 3rd Edition Susan Grove Daisha Cipher Full DownloadDocument3 pagesSolution Manual For Statistics For Nursing Research A Workbook For Evidence Based Practice 3rd Edition Susan Grove Daisha Cipher Full Downloadandreasmithpitornwgbc100% (39)
- Crawford HEALTHISM AND THE MEDICALIZATION OF EVERYDAY LIFEDocument25 pagesCrawford HEALTHISM AND THE MEDICALIZATION OF EVERYDAY LIFElilit sol100% (1)
- Priority in Public Health PDFDocument351 pagesPriority in Public Health PDFKheir Mussa100% (2)
- CHF (Dr. Devi, SP - JP)Document17 pagesCHF (Dr. Devi, SP - JP)sriworoNo ratings yet
- Interactive Code Blue Evaluation FormDocument2 pagesInteractive Code Blue Evaluation FormAyman Ali100% (1)
- On Emergency DrugsDocument25 pagesOn Emergency DrugsBikram Chhetry100% (1)
- Caring, Curing, Coping: Nurse, Physician, and Patient RelationshipsFrom EverandCaring, Curing, Coping: Nurse, Physician, and Patient RelationshipsNo ratings yet
- Distributing Health Care: Principles, Practices and PoliticsFrom EverandDistributing Health Care: Principles, Practices and PoliticsNo ratings yet
- Population HealthDocument444 pagesPopulation HealthC R D100% (3)
- Handbook of Qualitative Health Research For Evidence-Based PracticeDocument569 pagesHandbook of Qualitative Health Research For Evidence-Based PracticeMariana LepinskyNo ratings yet
- PIIS0140673616325703Document3 pagesPIIS0140673616325703Jose Angel BarreraNo ratings yet
- Wellness Beliefs Scale PostPrintDocument32 pagesWellness Beliefs Scale PostPrintSophia YangNo ratings yet
- B MJ Defining HealthDocument4 pagesB MJ Defining HealthWathsala ShyamaliNo ratings yet
- Health Social Care Comm - 2011 - Lucock - Self Care in Mental Health Services A Narrative ReviewDocument15 pagesHealth Social Care Comm - 2011 - Lucock - Self Care in Mental Health Services A Narrative ReviewDina NabilaNo ratings yet
- September/October 2010 Leaders' LinkDocument5 pagesSeptember/October 2010 Leaders' LinkiqsolutionsNo ratings yet
- September/October 2011 Leaders' LinkDocument4 pagesSeptember/October 2011 Leaders' LinkiqsolutionsNo ratings yet
- How Should We Define Health?: BMJ (Online) July 2011Document4 pagesHow Should We Define Health?: BMJ (Online) July 2011DigiferNo ratings yet
- 2002 Bringing The Best of Medical Librarianship To TheDocument10 pages2002 Bringing The Best of Medical Librarianship To TheXavier JorgeNo ratings yet
- How Should We Define Health?: BMJ Clinical Research July 2011Document4 pagesHow Should We Define Health?: BMJ Clinical Research July 2011John Joseph SalvaleonNo ratings yet
- How Should We Define Health?: BMJ Clinical Research July 2011Document4 pagesHow Should We Define Health?: BMJ Clinical Research July 2011AbysekaNo ratings yet
- How Should We Define Health?: BMJ Clinical Research July 2011Document4 pagesHow Should We Define Health?: BMJ Clinical Research July 2011Rej HaanNo ratings yet
- Environmental, Social, and Governance: A Framework for the Future of HealthcareFrom EverandEnvironmental, Social, and Governance: A Framework for the Future of HealthcareNo ratings yet
- DiabetesDocument6 pagesDiabetesAyin FajarNo ratings yet
- How Should We Define Health?: BMJ (Online) July 2011Document4 pagesHow Should We Define Health?: BMJ (Online) July 2011Frances Iehsia VillaNo ratings yet
- I Thought I Was Not For Medical Field, Until I WasDocument5 pagesI Thought I Was Not For Medical Field, Until I WasDanica EasabelleNo ratings yet
- CHN2 JournalDocument4 pagesCHN2 JournalTAYABAN, KENNETH JAKE, Q.No ratings yet
- Harrington God Health PDFDocument28 pagesHarrington God Health PDFjulfukarNo ratings yet
- Yates-Doerr. Contando Cuerpos...Document18 pagesYates-Doerr. Contando Cuerpos...María BergeroNo ratings yet
- Why Not User Charges? The Real Issues: Greg Stoddart Morris Barer Robert Evans Vandna BhatiaDocument34 pagesWhy Not User Charges? The Real Issues: Greg Stoddart Morris Barer Robert Evans Vandna BhatiaUmair JumaniNo ratings yet
- July/August 2010 Leaders' LinkDocument3 pagesJuly/August 2010 Leaders' LinkiqsolutionsNo ratings yet
- Public Health Research PapersDocument7 pagesPublic Health Research Papersp1zajywigyd2100% (1)
- BMJdefininghealthDocument4 pagesBMJdefininghealthjab0010No ratings yet
- Evaluating Marketing Strategies in Organ DonationDocument8 pagesEvaluating Marketing Strategies in Organ DonationSharuni GanesonNo ratings yet
- Exploring Experiences of and Attitudes Towards Mental Illness and Disclosure Amongst Health Care Professionals A Qualitative StudyDocument8 pagesExploring Experiences of and Attitudes Towards Mental Illness and Disclosure Amongst Health Care Professionals A Qualitative StudyleticiaNo ratings yet
- Greymatter January2017Document8 pagesGreymatter January2017sNo ratings yet
- @does Gender and Cultural Diversity Matter For SustainabilityDocument18 pages@does Gender and Cultural Diversity Matter For SustainabilityKlislaine LimaNo ratings yet
- An International Comparison of Factors Affecting Quality of Life Among Patients With Congestive Heart Failure: A Cross-Sectional StudyDocument15 pagesAn International Comparison of Factors Affecting Quality of Life Among Patients With Congestive Heart Failure: A Cross-Sectional Studyشبلي غرايبهNo ratings yet
- Guia Laboratorio. ReglamentoDocument4 pagesGuia Laboratorio. ReglamentoNathalia MojicaNo ratings yet
- Iastate DissertationDocument8 pagesIastate DissertationWriteMyCollegePaperForMeSingapore100% (1)
- BMJdefininghealthDocument4 pagesBMJdefininghealthTibiNo ratings yet
- Annotated BibliographyDocument8 pagesAnnotated BibliographySuchitaNo ratings yet
- LC 2Document11 pagesLC 2kvargasNo ratings yet
- How Should We Define Health?: BMJ (Online) July 2011Document4 pagesHow Should We Define Health?: BMJ (Online) July 2011hmzphs kolamuruNo ratings yet
- 2 - Huber Et Al (2011) - How Shold We Define HealthDocument4 pages2 - Huber Et Al (2011) - How Shold We Define HealthCorrado BisottoNo ratings yet
- Public Health EthicsDocument17 pagesPublic Health EthicsNongre ArphonNo ratings yet
- NSG 106Document12 pagesNSG 106Anipah AmintaoNo ratings yet
- Family-Centered Health PromotionDocument4 pagesFamily-Centered Health PromotionDasha KudelskayaNo ratings yet
- Healthcare: Spirituality in Renal Supportive Care: A Thematic ReviewDocument20 pagesHealthcare: Spirituality in Renal Supportive Care: A Thematic ReviewAmna ShahNo ratings yet
- Nurturing Hope, A Human Centric Approach To Kidney Transplant Awareness and Organ Donation EducationDocument4 pagesNurturing Hope, A Human Centric Approach To Kidney Transplant Awareness and Organ Donation EducationInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- How To Write A Public Health Research PaperDocument8 pagesHow To Write A Public Health Research Paperwqbdxbvkg100% (1)
- BMC Public HealthDocument28 pagesBMC Public Healthzeeleung99No ratings yet
- COVID 19 Anxiety, Peteet, J. RDocument2 pagesCOVID 19 Anxiety, Peteet, J. RJackyDanielsNo ratings yet
- The Nhs in 2030 PDFDocument48 pagesThe Nhs in 2030 PDFIsaac StanleyNo ratings yet
- Ni Hms 898083Document18 pagesNi Hms 898083Thusith WijayawardenaNo ratings yet
- Ni Hms 898083Document18 pagesNi Hms 898083Thusith WijayawardenaNo ratings yet
- Organizing Healthcare For Changing Markets: The Case of Ascension HealthDocument14 pagesOrganizing Healthcare For Changing Markets: The Case of Ascension Healtheman mamdohNo ratings yet
- Sociology of Medicine PDFDocument13 pagesSociology of Medicine PDFaditya_2k100% (1)
- Faith Healing Research PaperDocument8 pagesFaith Healing Research Paperfveec9sx100% (1)
- Gille, Felix, Sarah Smith, and Nicholas MaysDocument4 pagesGille, Felix, Sarah Smith, and Nicholas MaysMuhammad NasherNo ratings yet
- Paul Willis - Trans AdultsDocument11 pagesPaul Willis - Trans Adultsมา ยาNo ratings yet
- Acute Chest PainDocument103 pagesAcute Chest PainYajjat GargNo ratings yet
- Family Medicine I - All Questions For Final and MidtermDocument64 pagesFamily Medicine I - All Questions For Final and Midtermzdfdgsdgsh sggaesgsNo ratings yet
- Pathophysiology of Cardiogenic Pulmonary Edema - UpToDateDocument14 pagesPathophysiology of Cardiogenic Pulmonary Edema - UpToDateStefani AtlleNo ratings yet
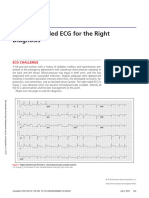
- 2018.the Right-Sided ECG For The Right DiagnosisDocument3 pages2018.the Right-Sided ECG For The Right DiagnosisWeila dos Santos VieiraNo ratings yet
- Adult, Child, and Infant Written Exam CPR Pro For The Professional RescuerDocument7 pagesAdult, Child, and Infant Written Exam CPR Pro For The Professional RescuerNguyen NamNo ratings yet
- Cardiac Function TestsDocument40 pagesCardiac Function TestsAkua Konama AttakoraNo ratings yet
- Table of Contents YjcafDocument3 pagesTable of Contents Yjcafntsn3100No ratings yet
- Practice ECGStripsDocument300 pagesPractice ECGStripsrobby zayendraNo ratings yet
- Use of Vasopressors and Inotropes - UpToDateDocument25 pagesUse of Vasopressors and Inotropes - UpToDateVictor Mendoza - MendezNo ratings yet
- ABCD2 ScoreDocument1 pageABCD2 ScoreMayo EnterprisesNo ratings yet
- Central Venous Monitoring 2022Document17 pagesCentral Venous Monitoring 2022AngieNo ratings yet
- RAAS WorksheetDocument2 pagesRAAS WorksheetParis ParisNo ratings yet
- Oefc 00 Ae Medicine 1 SB Un1Document8 pagesOefc 00 Ae Medicine 1 SB Un1Angela MercadoNo ratings yet
- CHAPTER 2 CT in CardiologyDocument9 pagesCHAPTER 2 CT in CardiologyAshvanee sharmaNo ratings yet
- Vascular Dementia: By: Omar Nuhic 4th Year Student Subject: PsychiatryDocument10 pagesVascular Dementia: By: Omar Nuhic 4th Year Student Subject: PsychiatryOmar NuhicNo ratings yet
- Test Bank For Therapeutic Exercise Foundations and Techniques 6th Edition KisnerDocument5 pagesTest Bank For Therapeutic Exercise Foundations and Techniques 6th Edition KisnerXavierKimydfj100% (29)
- Case Điện tâm đồDocument287 pagesCase Điện tâm đồSelina BerniceNo ratings yet
- Jurnal Reaading - Egi Dwi Satria Versi PDFDocument21 pagesJurnal Reaading - Egi Dwi Satria Versi PDFEgi Dwi SatriaNo ratings yet
- Heart Failure: Applied Medicine BY: Dr. Kinza IftikharDocument17 pagesHeart Failure: Applied Medicine BY: Dr. Kinza IftikharsabaamjadNo ratings yet
- Outspoken Raina Ash Full ChapterDocument77 pagesOutspoken Raina Ash Full Chapternancy.wesley488100% (3)
- Swimming Exercise: Impact of Aquatic Exercise On Cardiovascular HealthDocument11 pagesSwimming Exercise: Impact of Aquatic Exercise On Cardiovascular HealthMihail RonnyNo ratings yet
- Hypertrophic Cardiomyopathy: Joisy Aloor Leonard Shaju Smit Bhaisare Shawn RyneDocument36 pagesHypertrophic Cardiomyopathy: Joisy Aloor Leonard Shaju Smit Bhaisare Shawn RyneJoisy Aloor100% (1)
- 2 Book Clinical - Applications - and - Interaction - Between - HRV - and - Heart - RateDocument168 pages2 Book Clinical - Applications - and - Interaction - Between - HRV - and - Heart - RateJulio OliveiraNo ratings yet
- Microcirculation Monitoring - LOCAL GhalebDocument46 pagesMicrocirculation Monitoring - LOCAL GhalebGHALEB A. AlmekhlafiNo ratings yet