Professional Documents
Culture Documents
Emergency Nursing Midterms
Uploaded by
Mutya XD0 ratings0% found this document useful (0 votes)
4 views3 pagesOriginal Title
EMERGENCY NURSING MIDTERMS
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
4 views3 pagesEmergency Nursing Midterms
Uploaded by
Mutya XDCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 3
EMERGENCY NURSING: WEEK 1
BASIC LIFE SUPPORT (BLS)
- Trains participants to promptly recognize several CARDIO PULMONARY RESUSCITATION (CPR)
life-threatening emergencies, give high-quality
- Is an emergency life-saving procedure performed
chest compressions, deliver appropriate
when the heart stops beating.
ventilations and provide early use of an AED
- Is an emergency procedure that combines chest
- Is the foundation of saving lives after cardiac
compressions often with artificial ventilation in an
arrest.
effort to manually preserve intact brain function
- A level of medical care which is used for victims of
until further measures are taken to restore
life threatening illnesses or injuries until they can
spontaneous blood circulation and breathing in a
be given full medical care at the hospital. It can be
person who is in cardiac arrest.
provided by trained medical personnel, including
emergency medical technicians, paramedics, and • PURPOSE
by qualified bystanders. - To support life by means of hemodynamics,
- Includes psychomotor skills to perform high quality through chain of activities.
CPR, using automated external defibrillator (AED) - To reverse the initialing pathophysiological event.
and relieving an obstructed airway. - To prevent irreversible damage from anoxia
- Foundation of saving lives after cardiac arrest (absence of oxygen)
- “Cardiac arrest happens in our home”
• MAIN COMPONENTS
CHAIN OF SURVIVAL
1. Chest compression
- Actions in the chain of survival differ according to 2. Airway
settings (in-hospital vs. out-of-hospital) and age 3. Breathing
group
CARDIAC ARREST
• ADULT OUT-OF-HOSPITAL CHAIN OF SURVIVAL
- Sudden cessation of mechanical activity of heart
1. Activation of Emergency response with some or no electrical activity.
2. High-quality CPR - Cessation of normal circulation of blood due to
3. Defibrillation failure of heart to contract effectively.
4. Advanced resuscitation - Maybe reversible by rapid intervention but will
5. Post Cardiac Arrest Care lead to death in tis absences.
6. Recovery
• CAUSES
• ADULT IN-HOSPITAL CHAIN OF SURVIVAL
- Acute Myocardial Infarction
1. Early Recognition and Prevention - Cardiomyopathy
2. Activation of Emergency Response - Rhythm disturbances
3. High-Quality CPR - Congestive Heart Failure
4. Defibrillation - Cardiac Tamponade
5. Post Cardiac Arrest Care - Hypoxia
6. Recovery - Pulmonary Embolism
• PEDIATRIC OUT-OF-HOSPITAL CHAIN OF SURVIVAL - Tension Pneumothorax
- Respiratory Failuret
1. Prevention
- Airway obstruction
2. Activation of Emergency Response
- Sepsis
3. High-Quality CPR
- Electrolyte Imbalance
4. Advanced Resuscitation
- Hypoglycemia
5. Post Cardiac Arrest Care
- Anaphylaxis
6. Recovery
- Hypovolemia
• PEDIATRIC IN-HOSPITAL CHAIN OF SURVIVAL
CARDIO-PULMONARY RESUSCITATION
1. Early Recognition and Prevention
- 30:2
2. Activation of Emergency Response
- To support life by means of hemodynamic through
3. High-Quality CPR
chain of activities
4. Advanced Resuscitation
5. Post Cardiac Arrest Care • MAIN COMPONENTS (CAB)
6. Recovery Compression
Airway
Breathing
- Allow complete chest recoil
- Minimize interruption in compression
• WHEN TO GIVE CPR?
- Change compressor every 2 minutes or sooner if
BLS is needed when the individual: fatigued
- Is unconscious - If no advanced airway, 15:2 compression
- Is not breathing ventilation ratio
- Has an abnormal pulse rate - If advanced airway provide continuous
compressions and give a breath every 2-3 seconds
• WHEN NOT TO GIVE CPR?
AIRWAY ASSESSMENT AND BREATHING
- Neither scene nor the victim and the rescuer is
safe To open airway:
- Patient has developed rigor mortis (stiff body) 1. Head-Tilt Chin Lift
- Has normal pulse and breathing 2. Jaw Thrust
• WHY C-A-B? RESCUE BREATH
- To emphasize the simplest but the most important • MOUTH-TO-MOUTH
step
- Open airway. Pinch the nose. Seal mouth-to-
- To increase survival rate in sudden cardiac arrest
mouth contact. Blow.
- Patient’s blood stays oxygenated for 4-6 minutes
after last breath but circulation should be • MOUTH-TO-NOSE
restarted at the earliest
- Lockjaw. Seal mouth to nose contact. Blow with
- Rescue breathing almost always delays chest
more force.
compression
- Tidal volume: 500-600ml
• COMPONENTS - Each breath over 1 seconds with enough volume
to rise victim’s chest
1. Ensure scene safety
2. Check for response and assessment • MOUTH-TO-BARRIER DEVICE BREATHING
3. Call for help
- Head tilt chin lift. Seal from nasal bridge to chin in
4. Activate EMS
a ‘C’ pattern. Blow.
5. Chest Compression
- Protects rescuer from contact with a victim’s
• OUTCOME OF ASSESSMENT blood, vomitus and saliva, and from breathing the
air that the victim exhales.
Normal breathing (+) Pulse Monitor
felt • BAG-VALVE-MASK RESUSCITATIONS
No normal breathing (+) pulse Rescue breaths
No normal breathing (-) pulse Start CPR immediately - Open airway. First rescuer seals the mask in ‘E-C’
CHEST COMPRESSION pattern. Second rescuer provide ventilation.
- 2020 AHA guidelines for CPR has re-emphasized EARLY DEFIBRILLATION
early initiation of CPR (compression) by rescuers. AUTOMATED EXTERNAL DEFIBRILLATOR (AED)
- Is the foundation of CPR. - AED is an integral component of BLS protocol
- Push hard, push fast. - AED deliver defibrillations to specific two
- Hands-only CPR. shockable dysrhythmias (VFib and VTach)
HIGH-QUALITY CPR • AED SAFETY
• ADULT - Make sure the patient is as dry as possible.
Rescuers should not be in contact with water
- Push hard (at least 2 inches [5 cm]) and fast (100-
- Avoid getting AED or AED pads wet if possible
120/min)
- Make sure pads are not touching metal surface
- Allow complete chest recoil
- Position the pads at least an inch away from metal
- Minimize interruptions in compressions
piercings, 3cm away from pacemakers.
- Avoid excessive ventilation
- Be cautious with medication patches. Remove the
- Change compressor every 2 minutes, or sooner if
patch beforehand.
fatigued
- Excessive chest hair can affect pad-to-skin contact
- If no advanced airway, 30:2 compression
- When advised ‘CLEAR’, make sure no one is in
ventilation ration
contact
• PEDIATRIC - Do not use alcohol to wipe
- Do not use defibrillator around inflammable
- Push hard (2 ½ of antero-posterior diameter of
materials.
chest) and fast (100-120/min)
You might also like
- Cardiac Arrest PDFDocument4 pagesCardiac Arrest PDFYogi drNo ratings yet
- CPRDocument27 pagesCPRZaman ZaimNo ratings yet
- Cardioplumonary RDocument40 pagesCardioplumonary RABREHAM BUKULONo ratings yet
- Cardiorespiratory Arrest (FS)Document55 pagesCardiorespiratory Arrest (FS)Ahmad AzharNo ratings yet
- Konsep Code BlueDocument89 pagesKonsep Code BlueChris Van BlouseNo ratings yet
- CPR BrochureDocument2 pagesCPR Brochureapi-527938320No ratings yet
- AHA-PALS 2010: Pediatric Chain of SurvivalDocument10 pagesAHA-PALS 2010: Pediatric Chain of SurvivalIsabel CastilloNo ratings yet
- Basic Life SupportDocument4 pagesBasic Life SupportBernize ManzanoNo ratings yet
- Post Resuscitation CareDocument3 pagesPost Resuscitation CareprashsubbuNo ratings yet
- Jam IsolaDocument11 pagesJam IsolaCAMOMILLE ROSE JAMISOLANo ratings yet
- Abc - IcuDocument55 pagesAbc - Icuhoney requermeNo ratings yet
- BLS For The Nurses WeekDocument63 pagesBLS For The Nurses WeekPrince Rener Velasco PeraNo ratings yet
- Cardiopulmonary RESUSCITATION (CPR) & Critical in Medicine: Dr. Sameer Shaikh M.D. Medicine Asist. Prof. Dept of MedicineDocument84 pagesCardiopulmonary RESUSCITATION (CPR) & Critical in Medicine: Dr. Sameer Shaikh M.D. Medicine Asist. Prof. Dept of MedicineMedicine DepartmentNo ratings yet
- Cardiopulmonery ArrestDocument8 pagesCardiopulmonery Arrestt9d2014No ratings yet
- Emergency Drugs (LEAD)Document8 pagesEmergency Drugs (LEAD)RayePrudenteNo ratings yet
- Basic Life Support (BLS) : ObjectivesDocument9 pagesBasic Life Support (BLS) : Objectivespdfs.olpNo ratings yet
- Curs Prim Ajutor 2023 - MG An V - RCR - EnglishDocument21 pagesCurs Prim Ajutor 2023 - MG An V - RCR - Englishhulia jokoNo ratings yet
- CPCRDocument51 pagesCPCRAnushaNo ratings yet
- Basic Life Support 2017Document40 pagesBasic Life Support 2017Vega E Rahma WNo ratings yet
- CPCRDocument36 pagesCPCRapi-19916399100% (1)
- Lesson 2 Cardiopulmonary Resuscitation: Electric ShockDocument1 pageLesson 2 Cardiopulmonary Resuscitation: Electric ShockMoxie MacadoNo ratings yet
- Lesson 2 Cardiopulmonary Resuscitation: Electric ShockDocument1 pageLesson 2 Cardiopulmonary Resuscitation: Electric ShockMoxie MacadoNo ratings yet
- Cardiorespiratory Arrest (FS)Document88 pagesCardiorespiratory Arrest (FS)haerul ikhsanNo ratings yet
- Presenting Problems in Cardiovascular Disease - 457: Abnormal Heart SoundsDocument19 pagesPresenting Problems in Cardiovascular Disease - 457: Abnormal Heart SoundsDarawan MirzaNo ratings yet
- Cardiopulmonary Resuscitation (CPR) : Zeeshan Ali Pihs IslamabadDocument84 pagesCardiopulmonary Resuscitation (CPR) : Zeeshan Ali Pihs IslamabadHaseeb ur RehmanNo ratings yet
- Introduction - CPR PerspectiveDocument62 pagesIntroduction - CPR PerspectiveImtiaz AhmadNo ratings yet
- Nelec2 Week 17Document13 pagesNelec2 Week 17Michelle MallareNo ratings yet
- Basic Life SupportDocument24 pagesBasic Life SupporthelmismutNo ratings yet
- Basic Life Support 2006Document55 pagesBasic Life Support 2006sadabahmadNo ratings yet
- Cardiac ArrestDocument4 pagesCardiac Arrestapi-648401824No ratings yet
- Cardiopulmonary ResuscitationDocument20 pagesCardiopulmonary ResuscitationDrmirfat AlkashifNo ratings yet
- Dr. Putu, SP - An-Ti First Response in Emergency - SOPI 2023Document29 pagesDr. Putu, SP - An-Ti First Response in Emergency - SOPI 2023AlLen Rohi RiwuNo ratings yet
- Learning Material 1 Adult CPRDocument10 pagesLearning Material 1 Adult CPR3B ABAN, Daryl Lloyd G.No ratings yet
- Tongwen Sun Emergency Department, The First Teaching Hospitalof Zhengzhou UniversityDocument59 pagesTongwen Sun Emergency Department, The First Teaching Hospitalof Zhengzhou Universityapi-19916399No ratings yet
- CPRDocument19 pagesCPRNidhi KaushalNo ratings yet
- 1.assignment On CPRDocument7 pages1.assignment On CPRsantosh kumarNo ratings yet
- Basic Life SuportDocument70 pagesBasic Life SuportOana Alexandra PavaleanuNo ratings yet
- Finals Act 2Document1 pageFinals Act 2zoro100 88No ratings yet
- BLS MBBSDocument102 pagesBLS MBBSsurgeonvileNo ratings yet
- Acls 30-10-23Document63 pagesAcls 30-10-23lakshmiNo ratings yet
- Study Notes Emergency MedicineDocument12 pagesStudy Notes Emergency MedicineMedShare57% (7)
- 2019 BLS 1 - Revisi Akhir - PPT - Final DR - APRILDocument34 pages2019 BLS 1 - Revisi Akhir - PPT - Final DR - APRILarga setyo adjiNo ratings yet
- Cardiopulmonar Y ResuscitationDocument34 pagesCardiopulmonar Y ResuscitationRatuSitiKhadijahSarahNo ratings yet
- 14 CPR PDFDocument75 pages14 CPR PDFBlessy Susan100% (1)
- Poly-Trauma: by Dr. Elias Ahmed October 2003Document14 pagesPoly-Trauma: by Dr. Elias Ahmed October 2003Sisay FentaNo ratings yet
- Cardiac Arrest of MedicinesDocument38 pagesCardiac Arrest of MedicinesAtirah AaNo ratings yet
- Assessment of Critically Ill PatientsDocument4 pagesAssessment of Critically Ill PatientsAa AaNo ratings yet
- CPR 2014 SeminarDocument43 pagesCPR 2014 SeminarMinale MenberuNo ratings yet
- Approach To Acutely Ill PatientDocument22 pagesApproach To Acutely Ill PatientSarah RamliNo ratings yet
- Multiple TraumaDocument5 pagesMultiple TraumaChristabel EdithNo ratings yet
- DEFIB PPT at PrakaraDocument52 pagesDEFIB PPT at Prakarakvl kandulaNo ratings yet
- Seminar ON Cardiopulmonary Resuscitation: Submitted To Submitted byDocument18 pagesSeminar ON Cardiopulmonary Resuscitation: Submitted To Submitted bymerin sunilNo ratings yet
- Cardiac EmergenciesDocument29 pagesCardiac EmergenciesAhmad MohamadNo ratings yet
- 2.1. Pharmacological Therapeutics. 2.2. Basic Cardiac Life Support (BCLS) and Advanced Cardiac Life Support (ACLS) in Neonates and ChildDocument3 pages2.1. Pharmacological Therapeutics. 2.2. Basic Cardiac Life Support (BCLS) and Advanced Cardiac Life Support (ACLS) in Neonates and Childclint xavier odangoNo ratings yet
- 2009 UCSD Medical Center Advanced Resuscitation Training ManualDocument19 pages2009 UCSD Medical Center Advanced Resuscitation Training Manualernest_lohNo ratings yet
- 8-Adult Advanced Life Support Algorithm 2021Document1 page8-Adult Advanced Life Support Algorithm 2021khaledNo ratings yet
- Acls Mega Code 1Document31 pagesAcls Mega Code 1mj8bfgxbyjNo ratings yet
- 44 CPR PDFDocument14 pages44 CPR PDFBramantyo NugrosNo ratings yet
- Immediate Life Support for healthcare Practitioners: A Step-By-Step GuideFrom EverandImmediate Life Support for healthcare Practitioners: A Step-By-Step GuideNo ratings yet
- Drug Study - PiptazDocument1 pageDrug Study - PiptazMutya XDNo ratings yet
- Anti-Parkinson AgentsDocument35 pagesAnti-Parkinson AgentsMutya XDNo ratings yet
- Family AssessmentDocument71 pagesFamily AssessmentMutya XDNo ratings yet
- Funda MidtermsDocument13 pagesFunda MidtermsMutya XDNo ratings yet
- Neurobiochemical Basis of Psychiatric DisorderDocument2 pagesNeurobiochemical Basis of Psychiatric DisorderMutya XDNo ratings yet
- About Monkey PoxDocument3 pagesAbout Monkey PoxObakoma Josiah100% (1)
- Collagen FoodsDocument11 pagesCollagen FoodsPaul SavvyNo ratings yet
- Disney PrincessesDocument18 pagesDisney Princessesapi-214858613No ratings yet
- NurseLabs QnA#4Document36 pagesNurseLabs QnA#4Jill Noelle100% (1)
- Bracha - 2004 - Freeze Flight FrightDocument7 pagesBracha - 2004 - Freeze Flight FrightCK MawerNo ratings yet
- Review Article Yoda THD DM (Manuskrip)Document4 pagesReview Article Yoda THD DM (Manuskrip)shafiyyah putri maulanaNo ratings yet
- Pasteur Eng MiddleDocument4 pagesPasteur Eng MiddleRoykoNo ratings yet
- Cau Hoi Trac Nghiem Anh LTDH Cau Hoi Trac NghiemDocument18 pagesCau Hoi Trac Nghiem Anh LTDH Cau Hoi Trac NghiemLai NguyênNo ratings yet
- Apothio Hemp LawsuitDocument58 pagesApothio Hemp LawsuitLaw&CrimeNo ratings yet
- DR Antonious CV N & AEDocument27 pagesDR Antonious CV N & AEdoctorantoniNo ratings yet
- 2nd Quarter Exam Science 10Document11 pages2nd Quarter Exam Science 10Brille Anthony BunielNo ratings yet
- Ncma: Health AssessmentDocument25 pagesNcma: Health AssessmentBb PrintsNo ratings yet
- Identification of High Risk PregnanciesDocument15 pagesIdentification of High Risk PregnanciesVidya Ganesh100% (12)
- Key Points: Information About Your Procedure From The British Association of Urological Surgeons (BAUS)Document6 pagesKey Points: Information About Your Procedure From The British Association of Urological Surgeons (BAUS)diva aurelliaNo ratings yet
- The Ayurvedic Pharmacopoeia of India: Part - Ii (Formulations) Volume - I First Edition Monographs Ebook V.1.0Document187 pagesThe Ayurvedic Pharmacopoeia of India: Part - Ii (Formulations) Volume - I First Edition Monographs Ebook V.1.0VinitSharmaNo ratings yet
- Food and Toxicity-Natural ToxinsDocument47 pagesFood and Toxicity-Natural Toxinsflorina.andreea100% (1)
- BangkasDocument5 pagesBangkasJulianne BangkasNo ratings yet
- Allergic RhinitisDocument8 pagesAllergic RhinitisJuanNo ratings yet
- Kumpulan Soal Bahasa Inggris 2004Document8 pagesKumpulan Soal Bahasa Inggris 2004Achmady Kusuma WijayaNo ratings yet
- Scheduling: IndiaDocument5 pagesScheduling: IndiaCristinaNo ratings yet
- NCP For PTSDDocument3 pagesNCP For PTSDjhaze09100% (4)
- NCP OsteosarcomaDocument6 pagesNCP OsteosarcomaNiksNo ratings yet
- Activ One Policy WordingDocument55 pagesActiv One Policy WordingAditya SinghNo ratings yet
- Biocontrol Potential of Trichoderma Spp. Against Fusarium Oxysporum in Solanum Lycopersicum LDocument6 pagesBiocontrol Potential of Trichoderma Spp. Against Fusarium Oxysporum in Solanum Lycopersicum LMartinius TinNo ratings yet
- Symptoms of ColitisDocument5 pagesSymptoms of ColitisChatrina TandiloloNo ratings yet
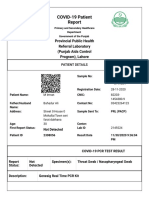
- Https Covid-19.Pshealthpunjab - Gov.pk PublicSampleResults PatientPublicSampleResultDocument2 pagesHttps Covid-19.Pshealthpunjab - Gov.pk PublicSampleResults PatientPublicSampleResultmuhammad imranNo ratings yet
- Ob WARDDocument7 pagesOb WARDNursingNooBNo ratings yet
- RLE Module 2M - Chest Physiotherapy, Postural Drainage, Nebulization, Chest Tube Drainage Systems, Blood TransfusionDocument57 pagesRLE Module 2M - Chest Physiotherapy, Postural Drainage, Nebulization, Chest Tube Drainage Systems, Blood TransfusionAlexa GoteraNo ratings yet
- Package Insert - 048437-01 - en - 422243Document22 pagesPackage Insert - 048437-01 - en - 422243HadiNo ratings yet
- Does The Behaviour of Using Electronic Cigarette Correlates With Respiratory Disease Symptoms?Document6 pagesDoes The Behaviour of Using Electronic Cigarette Correlates With Respiratory Disease Symptoms?Ninuk KurniawatiNo ratings yet