Professional Documents
Culture Documents
Comforting Strategies and Perceived Barriers To Pe
Comforting Strategies and Perceived Barriers To Pe
Uploaded by
MiaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Comforting Strategies and Perceived Barriers To Pe
Comforting Strategies and Perceived Barriers To Pe
Uploaded by
MiaCopyright:
Available Formats
Katende and Mugabi BMC Pediatrics (2015) 15:122
DOI 10.1186/s12887-015-0438-0
RESEARCH ARTICLE Open Access
Comforting strategies and perceived barriers
to pediatric pain management during IV line
insertion procedure in Uganda’s national referral
hospital: A descriptive study
Godfrey Katende1* and Benedicto Mugabi2
Abstract
Background: Venipuncture and intravenous (IV) cannula insertions are the two common sources of pain in hospitalized
children and health care today. The WHO asserts that, pain relief is a basic fundamental right and requires a
multidisciplinary approach. Nonpharmacological comforting strategies when implemented are important to relive pain
related distress in children during peripheral IV line insertion. However, evidence to date that suggests implementation
of such strategies and their barriers in Uganda remains very limited. This study aimed at establishing the current practices
in regard to the use of comforting strategies and the perceived barriers faced by health care providers to implement
pediatric pain management during IV line insertion procedure in Uganda’s national referral hospital, Mulago.
Method: A cross sectional and descriptive study was conducted between December 1, 2012 and February 28, 2013
involving doctors, nurses and interns in six pediatric wards of Mulago Hospital in Uganda. A pre-tested self- administered
and semi- structured questionnaire was used to collect the data. Data was entered into SPSS and descriptive statistics run
on all the variables.
Results: Of the 120 questionnaires distributed, 105 (RR = 87.5 %) were returned and completed. The evidence based
comforting strategies used for pain management during IV line insertion by the majority of health care professionals
were; skin to skin (51 %) and appropriate upright positioning of the child on mother’s lap (69 %). The least
used comforting strategies were; allowing the child to suck his thumb or hand (70 %), use of distraction (69 %) and
directing the child to suck one of his fingers into his mouth (90 %). The identified barriers to implementing comforting
strategies were; lack of time (42 %), having emergency situations (18 %), and not knowing the right method to use
(11 %). Of 105, 100 (95 %) reported that there is need for continuous professional development on comforting strategies.
Conclusions: Findings demonstrated that fewer health care providers used some evidence based comforting strategies
of pain relief during pediatric peripheral IV line insertion. Distraction and other evidence based strategies for pain and
distress relieve are less often used by the majority of the health care providers. Incorporating pediatric pain management
content in all health professionals training curricula could improve the current practices for better health outcomes.
Keywords: Comforting strategies, Health care provider, Pain management, Pediatric
* Correspondence: katendeg@yahoo.com
1
Sultan Qaboos University, College of Nursing, 123 Muscat, Oman
Full list of author information is available at the end of the article
© 2015 Katende and Mugabi. Open Access This article is distributed under the terms of the Creative Commons Attribution
4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and
reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to
the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver
(http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
Content courtesy of Springer Nature, terms of use apply. Rights reserved.
Katende and Mugabi BMC Pediatrics (2015) 15:122 Page 2 of 8
Background access. These include; attitudes of society as regards to
Venipuncture and intravenous (IV) cannula insertions pain perception [15], misconception about pain in children
are the two most common procedures and sources of [15], inadequate knowledge [1], underuse of pain assess-
pain in hospitalized children in health care today [1, 2]. ment tools [16], and lack of recognized standards and
Managing pain proactively during IV cannula insertions guidelines for pain relief [1, 17]. Additionally, lack of
or venous access is desirable [2]. Although reports show family-centered care where family member is not always
that elimination or relief of pain is an important respon- encouraged as well as not teaching parents what to do to
sibility of physicians and nurses caring for children [3], help the child is some of the reported barriers to imple-
studies show that parent participation through their menting pain management strategies for pediatric venous
presence and positioning significantly reduce distress access [1, 17].
when starting an IV in young children [4]. The WHO To our knowledge and based on the needs assessment
asserts that, pain relief is a basic human fundamental right conducted in Uganda in 2011 [18], none of the current
[5, 6] and requires a multidisciplinary approach [1, 6]. Like health care providers’ training curricula used, prepares
the adult patients, unmanaged or poorly managed pain in health care professionals to manage pediatric pain.
children can result in a variety of negative long-term con- Additionally, there is little no existing guidelines available
sequences [5, 7]. to direct procedural comfort management by health care
Currently, the general scientific community supports the providers on the pediatric wards in Mulago National
understanding of infant perception of pain and other Referral Hospital. Furthermore, there is no documented
noxious stimuli [7]. There is considerable evidence that report available on health care providers’ use of any evi-
shows a significant proportion of children undergoing dence based interventions for pediatric pain management
venipuncture experience moderate to severe pain as well as during peripheral IV line insertion procedures putting
elevated levels of pre-procedural and procedural dis- children at risk for suboptimal procedural comfort
tress [6, 7]. Evidence based non-pharmacological pain management [17, 19]. This study aimed at establish-
management strategies such as distraction strategies ing the current practices regarding the use of com-
are feasible and implemented by all health care pro- forting strategies for pediatric pain management by
viders [3]. Non- pharmacological interventions for pain Ugandan health care providers during peripheral IV
relief in infants are those that focus on creating a favor- line insertion procedure. In addition, to determine the
able environment, offering pleasant stimuli and cen- barriers impeding the implementation of evidence
tered on maternal care [8]. based comforting strategies to pain management dur-
Health care professionals performing any kind of ing IV line insertion identified.
venipuncture or intravenous cannula insertion procedure
should optimize the use available clinical practice guide-
lines. The used guidelines should advocate for comforting Methods
strategies to ameliorate pain and distress related to venous Study design and setting
access procedures in children [1, 9–11]. Maintaing a This was a cross sectional and descriptive study involv-
friendly environment when performing painful procedures ing a convenient sample nurses, doctors and interns
is imperative [8, 9]. Although there is a growing body of (N = 105) working in six (6) pediatric wards with the
knowledge about nonpharmacological interventions use help of a semi- structured self-administered question-
to increase comfort of children during painful procedures naire designed by the authors. The study was con-
[8, 9, 12], their implementation to date in low resource ducted between December 1, 2012 and February 28,
settings such as Uganda remains very limited [13]. Non- 2013 at Mulago Hospital. Mulago hospital is a lar-
pharmacological strategies are documented as cost effect- gest Uganda’s national referral and teaching hospital
ive and easy to administer without formal regulation [8]. with a bed capacity of 1500. The hospital is organized into
Currently, Challenges faced by Uganda include low specialization units/departments and among these is
human resources for health, a growing population, double pediatric department where the study was conducted. The
disease burden of infectious and non-communicable dis- pediatric and child health care department has more than
eases as well as limited access to free published practice 6 large units organized into wards: infectious (Jellife), non-
guidelines [14]. Nonpharmacological comforting interven- infectious (Stanfield), pediatric surgery (2C), pediatric
tions performed by health care providers are the best choice intensive care unit (SCU), acute care unit, nutrition and
for their additional benefits for better outcomes [8] espe- rehabilitation (Mwanamujimu), Pediatric cancer (LTC),
cially in childhood routine immunizations in primary health well as the young child clinic (YCC). Each of the pediatric
care arena. ward has a bed capacity of 50–100 beds depending on the
Numerous reports have documented barriers to imple- size of the building. The study participants were from 6
menting pain management strategies for pediatric venous pediatric wards.
Content courtesy of Springer Nature, terms of use apply. Rights reserved.
Katende and Mugabi BMC Pediatrics (2015) 15:122 Page 3 of 8
Participants and recruitment comforting strategies for pediatric IV line insertion
In order to obtain the required sample (N = 105), the (50 % - estimated as no study available in Uganda on
eligibility criteria for inclusion in the study were set; the subject), e = desired level of precision of 5 %, z =
having worked in a pediatric unit for at least no less 95 % CI (1.96). Sample size required would be 384
than 3 months and having performed peripheral IV participants. Since the number of doctors and nurses
cannula insertion. The study received approval from working in Mulago pediatric wards is small, all of
the Makerere University Research Ethics Committee were individually approached to participate in the
(REC: REF 2012–055), as well as obtaining permission from study to achieve a total sample of 105 participants.
the Department of Pediatrics and Child health, Mulago
Hospital. Doctors, nurses and interns are health care pro- Analysis
viders who participated in the study after consent obtained. Data collected was entered and analyzed using Statistical
Package for Social Sciences (SPSS version 12). Descriptive
Data collection statistics was run on all the variables including demo-
Health care providers who consented and met the eligibil- graphics to identify and exclude missing data. Frequencies
ity criteria received a self-administered semi-structured and percentages were obtained to guide in the interpret-
questionnaire given by three of the trained research ation of the results.
assistants (RAs). The research assistants collected the
completed questionnaires from the participants. The Results
developed questionnaire with the use of literature review Demographic characteristics
identified health workers’ comforting strategies used dur- Of 120 questionnaires distributed, 105 (RR = 87.5 %) were
ing peripheral intravenous line insertion. The question- returned and completed. All the participants (N = 105)
naire consisted of seven (7) demographic characteristics who participated in the study worked in mainly the 6 (Six)
questions: education background (professional cadre), sex, pediatric units or wards, with a mean age of 31 years
age, tribe, work experience, and employment status. (ranging from 23 to 60 years) and a mean working
Another set of 18 questions related to their experience experience of 10 years (ranging from 2 to 30 years).
using comforting strategies during the IV line insertion Majorities (74 %) of the participants were female health
procedure were given. This section elicited “yes” and “no” care workers and almost an equal number (50 %) had per-
responses where a yes meant that the participant had used manent employment at the hospital (Table 1).
that comforting strategy and no, meant having not used
that particular strategy or intervention. Three (3) ques- Comforting strategies used by health care workers during
tions asked participants about the need for continuous peripheral IV line insertion
professional development in IV line insertion and use of Comforting strategies for pain management mostly used
comforting strategies as well as a self-rating question on by health workers during peripheral IV line insertion
their skills in IV line insertion. The last section on per- were; greeting the child (72 %) and greeting the parent
ceived barriers was a multiple responses question that or care taker (90 %). More than half (51 %) of the Health
solicited the participants’ opinions on why they did not care providers encouraged skin-to skin contact with the
use any of the comforting strategies during pediatric IV mother, encouraged the mother to breast feed (58 %),
line insertion. Participants were asked to indicate impedi- positioned the child appropriately on mothers lap in up-
ment factors using the options provided and if any other right position (85 %) but also in addition, ensured that
to fill in the space provided. the chosen position was comfortable (69 %) and obtained
Before actual data collection, two pediatric IV line consent from mother or child (57 %) (Table 2).
insertion experts reviewed the questionnaire and their On the other hand, the least used comforting strat-
input incorporated in the final version. A pilot study egies by the majority of health care providers in pediatric
was conducted and consisted of 10 health care pro- pain management were; allowing the child to suck his
viders (5 doctors and 5 nurses) from another nearby thumb or hand (70 %), directing one of the child’s fin-
hospital pediatric unit and based on their responses gers into its mouth for sucking (90 %), allowing the child
and feedback, the questionnaire was finalized for use. to have freedom to select the chosen position (72 %) and
Thirty (30) questions were retained on the final ver- use of distraction techniques (69 %). A good number
sion and the average estimated time to complete the (82 %) of health care providers did not provide a play
questionnaire was 45 min. preparation like a doll nor consulted the child or mother
on previous successes and failures of IV insertion (63 %)
Sample size estimation (Table 2).
Using Kish Leslie (1965) formula: n = z2pq/e2, where Furthermore, less than half of health care providers
p = proportion of health care professionals using (47 %) responded that there was no preparation in their
Content courtesy of Springer Nature, terms of use apply. Rights reserved.
Katende and Mugabi BMC Pediatrics (2015) 15:122 Page 4 of 8
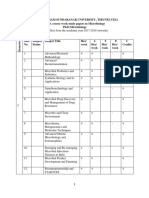
Table 1 Socio-demographic characteristics of the study Perceived barriers to implementing comforting strategies
participants for pain management during IV line insertion procedure
Variable Frequency (N = 105) Percentage (%) A number of barriers that impeded implementation of
comforting strategies for pain management during IV
Sex line insertion procedures in children were identified.
Female 78 74 The majority of the participating health care providers
Male 27 26 responded lack of time for implementation the strategies
Religion
(42 %), having an emergency situation and encounter
(18 %), and irritability of children (13 %). Additionally,
Catholic 34 32
health care providers identified not knowing the right
Moslem 7 7 method to use (11 %) as an implementation barrier
Protestant 39 37 (Fig. 1). Other barriers identified were; age related,
a
Others 25 24 work overload, not expecting children to get much
Age pain, lack of distractive materials as well as not think-
≤30 years 44 42
ing that it was important to control pain in this vul-
nerable group (Fig. 1).
>30 years 61 58
Tribe
Ganda 48 46 Discussion
Nkore 12 11 Generally, pediatric pain management remains a huge
Others 45 43 challenge to all health care providers in primary, acute
Professional Cadre
and other settings in Uganda. It is even more challen-
ging for low resource settings such as Mulago hospital
Medical Officer 17 16
where pain management is not a fundamental right for
Senior Housing Officer 22 21 all patients regardless of the available resources. For this
(SHO)
reason, the WHO continues to emphasize pain manage-
BSN 22 21
ment as a fundamental right regardless of age, culture,
Diploma nurse 30 29 race, ethnicity and socio economic status [5, 6].
MSN 1 1 Although there is increased awareness of pain manage-
Certificate nurse 3 3 ment in adult patients [20, 21], pain management in
Othersb 10 10 pediatric patients should be given a high priority by all
health care professionals through advocating for optimal
Years of Working experience
use of comforting strategies that reduce pain distress dur-
>3 m < 1 year 24 23
ing painful procedures [3, 21]. However, our study demon-
1–3 years 12 11 strated the use of some evidence based comforting
4–6 years 18 17 strategies for pediatric pain management during IV line
7–10 years 17 16 insertion by the participating health care professionals at
More than 10 years 34 32 the Mulago national referral and teaching hospital.
Considerably not evidence based comforting strategy
Employment status
for pediatric pain relief; health care professionals reported
Intern (doctors and nurses) 31 30
greeting a child and relative or care taker as a comforting
SHO 21 20 strategy of pain management during venous access pro-
Permanent employee 53 50 cedure. In this study, greeting is an important facet for
Other 0 0 enhancing rapport and creating a friendly environment
MSN Masters of Science in Nursing Degree, BSN Bachelors of Science in that begins with a warm greeting. The finding is supported
Nursing Degree, SHO Senior House Officer by findings of two different studies that recommended cre-
Othersa = Pentecostal, Seventh Day Adventist, Atheist and Jehovah witness
Othersb = Nursing Aids, senior student nurses
ating a friendly environment for painful procedures [8, 9].
Conversely, study findings demonstrated that, health care
respective health programs in regard to IV line insertion. professionals are not aware of the evidence based com-
Half of the health care providers (50 %) rated themselves forting interventions for pediatric pain management.
“good” at IV line insertion skill. The majority (95 %) This could be simply because they have limited access
reported that continuous professional development on to evidence based guidelines that describe these strat-
comforting strategies for pediatric pain management was egies. Limited access to evidence based guidelines is a
necessary (Table 3). major cause of practice variability as found in one study
Content courtesy of Springer Nature, terms of use apply. Rights reserved.
Katende and Mugabi BMC Pediatrics (2015) 15:122 Page 5 of 8
Table 2 Comforting strategies used by health care providers Table 2 Comforting strategies used by health care providers
during IV line insertion during IV line insertion (Continued)
Comforting strategy Frequency Percentage No 99 94
(%) N = 105
Established distraction techniques
Greeted the child
Yes 33 31
Yes 75 72
No 72 69
No 30 29
Positioned the child appropriately
Greeted the parent/care taker
Yes 89 85
Yes 94 90
No 16 15
No 11 10
Allowed the child freedom to select its chosen
Allowed child to suckle preferred thumb and position
or hand
Yes 29 28
Yes 31 30
No 76 72
No 74 70
Ensured that the chosen position was
Directed one of the child’s fingers into its comfortable
mouth for sucking
Yes 72 69
Yes 10 10
No 33 31
No 95 90
Provided play preparation like a doll
Avoided the hand the child favored to use
Yes 19 18
Yes 47 45
No 86 82
No 58 55
Consulted the child and mother on previous
Encouraged skin-to-skin contact with mother successes and failures
Yes 54 51 Yes 39 37
No 51 49 No 66 63
Encouraged the mother to breast feed her
child
Yes 61 58
conducted at the same hospital about hypertension
No 44 42
management guidelines [14].
Explained procedure to the child and gave
opportunity to ask questions
Using current evidence practice guidelines has benefits
of improving patient care and outcomes [8]. Moreover,
Yes 44 42
making clinical guidelines accessible and available for
No 61 58 use enhances current practice for improved patient out-
Directed the mother to tuck her child comes but also, plays a vital role in advocating for their
Yes 40 38 use [13, 14]. Complex organizations such as Mulago hos-
No 65 62 pital have a duty to source or develop guidelines in order
Directed the mother to hand-swaddle
to regulate or inform practitioners of the current practices.
her child The WHO regularly publishes free online practice guide-
Yes 41 39 lines adaptable in low resource settings [14]. Undeniably,
procedural pain management guidelines for use in children
No 64 61
are necessary for improve procedural outcomes [2]. Not-
Obtained verbal consent from child
and mother
withstanding, unmanaged pediatric pain is a cause of life
threatening mental illnesses such as post-traumatic stress
Yes 60 57
disorders [22]. In addition,,many studies report the poten-
No 45 43 tial benefits of managing pain and distress in children;
Consulted and offered the child the reducing subsequent morbidity and preventing delayed
preferred choice of pain relief
healing [23]. Unfortunately, evaluation of our study against
Yes 6 6 other studies other studies in Africa and Uganda is a
challenge due to paucity of studies to compare good
practices in pediatric pain management. Studies con-
ducted in Uganda, mostly on the skin-to-skin or kanga-
roo method provide evidence of the kangaroo method
Content courtesy of Springer Nature, terms of use apply. Rights reserved.
Katende and Mugabi BMC Pediatrics (2015) 15:122 Page 6 of 8
Table 3 Self-rating on use of comforting strategies and IV line swaddling methods for pain relief. Studies support tucking
insertion skills and swaddling efficacious in reducing pain related
Variable Frequency Percentage distress [12, 25].
(%) N = 105 Despite the lack of available evidence based guidelines
Health program prepared me in IV line on pediatric pain management during IV line insertion
insertion
procedure, health care providers’ implemented some
Yes 56 53 comforting strategies available to them. The lack of evi-
No 49 47 dence based guidelines for use by the health care profes-
Self –rating on IV line insertion skills sional partly explains why fewer health care providers
1. Excellent 11 10 used less of the evidence based comforting strategies. In
fact, half of the health care providers confessed that health
2. Very good 40 38
training programs had not prepared them for the skill of
3. Good 53 50
pediatric IV line insertion and therefore, majority
4. poor 1 1 identified the dare need for continuous professional
Continuous professional develop needs on development about comforting strategies for pediatric
comforting strategies during IV line insertion pain management.
Yes 100 95 Other evidence based comforting interventions underu-
No 5 5 tilized by health care providers were; use of destructions
techniques and asking a mother or child about previous
as one that promotes growth and development as well success or failure of IV line insertion. This finding could
as bonding in preterm babies [24]. Still, in Uganda, be interpreted that health care providers simply do not
little or nothing is documented about kangaroo involve patients in planning their management [26]. It
method as a comforting strategy for pain relief during should be noted that parental involvement including;
IV line insertion. But, this study with support from a positioning, being present and use of distraction tech-
systematic review, provides evidence for the kangaroo niques are efficient methods in reducing pain distress
method as efficacious in improving pain reactivity in children [12, 26, 27]. Health care professional un-
when the caregiver places the infant on the bare chest derstanding that different comforting strategies are
before, during and after a painful procedure [12]. No efficient for different ages with appropriately use
wonder, slightly higher than half of the health profes- when needed is paramount [12, 27].
sionals used skin-to-skin method in the context of In our study, the barriers to using evidence based
kangaroo but underscored the use of tucking and comforting strategies are identified. Specifically and
Fig. 1 Barriers to implementing comforting strategies for pain management during IV line insertion procedure
Content courtesy of Springer Nature, terms of use apply. Rights reserved.
Katende and Mugabi BMC Pediatrics (2015) 15:122 Page 7 of 8
interestingly, participating health care providers reported officers, nurses, residents and other health care profes-
that they did not have time to implement these strat- sionals is essential.
egies. Health care providers reported that having an
emergency situations, children being irritable, and not Conclusions
knowing the right methods to use are impeding factors In conclusion, findings showed that fewer health care pro-
to implement comforting strategies. These are similar to viders used some evidence based comforting strategies of
those identified in a study by Zempsky [1]. It is worth pain relief during pediatric peripheral IV line insertion.
noting that the identified barriers significantly affect the Distraction and other evidence based comforting strat-
provision of quality health care in low resource settings egies for pain and distress relieve are less often used by
such as Mulago hospital and should be addressed. Add- the majority of health care providers. Seemingly, lack of
itionally, the barriers add to existing challenges of low time, and work overload were major barriers identified to
human resources for health [14]. implementing comforting strategies of pain management
As a limitation, we acknowledge that our study was during pediatric IV line insertion. Incorporating pediatric
limited by the sampling technique and the small number pain management content in all health professionals train-
of participating health care professionals. Therefore, re- ing curricula could improve the current practices for
sults cannot be generalizable. The study also faced the better health outcomes.
challenge of scarcity of literature from Africa and Uganda
and therefore, inference with low-income settings was a Abbreviations
challenge. Lastly, the authors depended on self-report SPSS: Statistical Package for Social Sciences; IV: Intravenous; N: Total number
of participants; REC: Research Ethics Committee; REF: Reference Number.
information obtained through questionnaire.
Competing interests
Implications for practice The authors declare that they have no competing interests.
Evidence based nonpharmacological interventions for pain
management during IV line insertion are feasible and cost Authors’ contributions
effective for all health care professions to administer [3, 8]. Author BM was involved in conception of this paper, data analysis designing
the data collection tools, analyzing the data and reviewing the manuscript.
Nurses are the first persons to have encounters with the Author GK was involved in the drafting of the paper for intellectual content,
patients including children in all health care settings. Again, designing data collection tool, data analysis, writing the manuscript, and
nurses also perform the majority of the patient procedures review of the manuscript till final submission. All authors read and approved
final manuscript.
including treatment, immunizations and IV line insertions.
Being aware of comforting strategies for pain management
Acknowledgments
is an important part in nurses’ job. However, the lack of We thank Dr. Sara Groves who helped in interpreting the data.
guidelines may compromise their functionality in the health
Author details
care team especially when it comes to pain management in 1
Sultan Qaboos University, College of Nursing, 123 Muscat, Oman.
children. For Uganda’s case, developing clinical guidelines 2
Department of Nursing, Makerere University,College of Health Sciences, 256
and disseminating them widely is diserable to address the Kampala, Uganda.
existing practice gaps among health care providers. Adapt-
Received: 23 December 2014 Accepted: 28 August 2015
ing existing guidelines for use by health care professionals
is a starting point. Additionally, there is need to enhance
collaborative teamwork with a focus on family centered References
care approach to pain management. Further research to de- 1. Zempsky WT. Optimizing the management of peripheral venous access
pain in children: evidence, impact, and implication. Pediatrics. 2008;122
termine the acceptance level of health care professionals in Suppl 3:121.
the use of guidelines for pain management that focus on 2. Kennedy RM, Luhmann J, Zempsky WT. Clinical implications of unmanaged
venous access procedures warrants investigation. needle-insertion pain and distress in children. Pediatrics. 2008;122 Suppl
3:130.
3. American Academy of Pediatrics. Committee on psychosocial aspects of
Implication for health professional education child and family health american pain society task force on pain in infants,
Health professional education that focuses on pain children, and adolescents: The assessment and management of acute pain
in infants, children, and adolescents. Pediatrics. 2001;108(3):793–7.
management in children is desirable. Integrating this 4. Sparks LA, Setlik J, Luhman J. Parental Holding and positioning to decrease
important subject area in the existing health profes- IV distress in young children: A randomized controlled trial. J Pediatr Nur.
sions curricula is imperative for practice change. There 2007;22(6):440–7.
5. Green CR, Todd KH, Lebovitis A, Francis M. Disparities in pain: ethical issues.
is need for continuous profession development for all Pain Med. 2006;7(6):530–3.
staff rotating in pediatric units about pain management 6. Brennan F, Carr D, Cousins M. Pain management: A fundamental human
strategies for pediatric patients. Implementing such right. Anesth Analg. 2007;105(1):205–21.
7. Slater R, Cornelissen L, Fabrizil L, Patten D, Yaxen J, Warley A, et al. Oral
educational program as part of the orientation program Sucrose as an anelegisic drug for procedural pain in newborn infants: a
during pediatric rotation for interns, senior house randomized controlled trial. Lancet. 2010;376:1225–32.
Content courtesy of Springer Nature, terms of use apply. Rights reserved.
Katende and Mugabi BMC Pediatrics (2015) 15:122 Page 8 of 8
8. Fernandes A, Campbell-Yeo M, Johnston CC. Procedural pain management
for neonates using nonpharmacological strategies: part 1: sensorial
interventions. Adv Neonatal Care. 2011;11(4):235–41.
9. Finley GA, Franck LS, Grunau RE, Baeyer CL. Why children’s pain matters.
Pain Clin Updates XIII. 2005;4:1–6.
10. Infusion Nurses Society. Infusion nursing standards of practice: local
anesthesia. J Infus Nurs. 2006;29(1 suppl):S1–92.
11. Zempsky WT, Cravero JP. American academy of pediatrics, committee on
pediatric emergency medicine and section on anesthesiology and pain
medicine: relief of pain and anxiety in pediatric patients in emergency
medical systems. Pediatrics. 2004;114(5):1348–56.
12. Pillai Riddell RR, Racine NM, Turcotte K, Uman LS, Horton RE, Din Osmun L,
et al. Non-pharmacological management of infant and young child
procedure pain. Cochrane Database Syst Rev. 2011;10:CD006275.
13. Bhargava R, Young KD. Procedural pain management patterns in academic
pediatric emergency departments. Acad Emerg Med. 2007;14(5):479–82.
14. Katende G, Groves S, Becker K. Hypertension education intervention with
Ugandan nurses working in hospital outpatient clinic: a pilot study. Nursing
Res Practice. 2014;2014:1–6. 710702.
15. Epstein B. The american society of Anesthesiologist’s efforts in developing
guidelines for sedation and analgesia for non-anesthesiologists: The 40th
rovenstine lecture. Anesthesiology. 2003;98(5):1261–8.
16. Czarnecki ML, Simons K, Thompson J, Armus C, Hanson T, Berg T, et al.
Barriers to pediatric pain management: A nursing perspective. Pain Manag
Nurs. 2011;12(3):154–62.
17. Walker PC, Wanger DS. Treatment of pain in pediatric patient. J Pharm
Pract. 2003;16:261–75.
18. Kiguli S, Baingana R, Paina L, Mafigiri D, Groves S, Katende G, et al.
Situational analysis of teaching and learning of medicine and nursing
students at Makerere University college of health sciences. BMC Int Health
Hum Rights. 2011;11(Suppliment1):S3.
19. MacLean S, Obispo J, Young KD. The gap between pediatric emergency
department procedural pain management treatments available and actual
practice. Pediatr Emerg Care. 2007;23(2):87–93.
20. Weiner DK, Kim YS, Bonino P, Wang J. Low back pain in older adults: are we
utilizing health resources wisely. Pain Med. 2006;7(2):143–50.
21. Johnston CC, Fernande AM, Campbell-Yeo M. Pain in neonates is different.
Pain. 2011;152:S65–73.
22. Woodin KA, Rodewald LE, Humiston SG, Carges MS, Schaffer SJ, Szilagyi PG.
Physician and parent opinions: are children becoming pincushions from
immunizations? Arch Pediatr Adolesc Med. 2005;149(8):845–9.
23. Kharasch S, Saxe G, Zuckerman B. Pain treatment: Opportunities and
challenges. ArchPediatr Adolesc Med. 2003;157(11):1054–6.
24. Waiswa P, Nyanzi S, Namusoke-Kalungi S, Peterson S, Tomson G, Pariyo GW.
“I never thought that this baby would survive”; I thought that it would die
any time: Perceptions and care for preterm babies in eastern Uganda. Trop
Med Int Health. 2010;15(10):1140–7.
25. Cong X, Ludington-Hoe SM, McCain G, Pingfu F. Kangaroo care modifies
preterm infant heart rate variability in response to heel stick pain: Pilot
study. Early Hum Dev. 2009;85:561–7.
26. Cohen LL. Behavioral approaches to anxiety and pain management for
pediatric venous access. Pediatrics. 2008;122(3 supplement):S134–9.
27. Cignacco E, Hamers JPH, Stoffel L, Van Lingen RA, Gessler P, McDougall J,
et al. The efficacy of non-pharmacologic interventions in the management
of procedural pain in preterm and term neonates: A systematic literature
review. Eur J Pain. 2007;11(2):139–52.
Submit your next manuscript to BioMed Central
and take full advantage of:
• Convenient online submission
• Thorough peer review
• No space constraints or color figure charges
• Immediate publication on acceptance
• Inclusion in PubMed, CAS, Scopus and Google Scholar
• Research which is freely available for redistribution
Submit your manuscript at
www.biomedcentral.com/submit
Content courtesy of Springer Nature, terms of use apply. Rights reserved.
Terms and Conditions
Springer Nature journal content, brought to you courtesy of Springer Nature Customer Service Center GmbH (“Springer Nature”).
Springer Nature supports a reasonable amount of sharing of research papers by authors, subscribers and authorised users (“Users”), for small-
scale personal, non-commercial use provided that all copyright, trade and service marks and other proprietary notices are maintained. By
accessing, sharing, receiving or otherwise using the Springer Nature journal content you agree to these terms of use (“Terms”). For these
purposes, Springer Nature considers academic use (by researchers and students) to be non-commercial.
These Terms are supplementary and will apply in addition to any applicable website terms and conditions, a relevant site licence or a personal
subscription. These Terms will prevail over any conflict or ambiguity with regards to the relevant terms, a site licence or a personal subscription
(to the extent of the conflict or ambiguity only). For Creative Commons-licensed articles, the terms of the Creative Commons license used will
apply.
We collect and use personal data to provide access to the Springer Nature journal content. We may also use these personal data internally within
ResearchGate and Springer Nature and as agreed share it, in an anonymised way, for purposes of tracking, analysis and reporting. We will not
otherwise disclose your personal data outside the ResearchGate or the Springer Nature group of companies unless we have your permission as
detailed in the Privacy Policy.
While Users may use the Springer Nature journal content for small scale, personal non-commercial use, it is important to note that Users may
not:
1. use such content for the purpose of providing other users with access on a regular or large scale basis or as a means to circumvent access
control;
2. use such content where to do so would be considered a criminal or statutory offence in any jurisdiction, or gives rise to civil liability, or is
otherwise unlawful;
3. falsely or misleadingly imply or suggest endorsement, approval , sponsorship, or association unless explicitly agreed to by Springer Nature in
writing;
4. use bots or other automated methods to access the content or redirect messages
5. override any security feature or exclusionary protocol; or
6. share the content in order to create substitute for Springer Nature products or services or a systematic database of Springer Nature journal
content.
In line with the restriction against commercial use, Springer Nature does not permit the creation of a product or service that creates revenue,
royalties, rent or income from our content or its inclusion as part of a paid for service or for other commercial gain. Springer Nature journal
content cannot be used for inter-library loans and librarians may not upload Springer Nature journal content on a large scale into their, or any
other, institutional repository.
These terms of use are reviewed regularly and may be amended at any time. Springer Nature is not obligated to publish any information or
content on this website and may remove it or features or functionality at our sole discretion, at any time with or without notice. Springer Nature
may revoke this licence to you at any time and remove access to any copies of the Springer Nature journal content which have been saved.
To the fullest extent permitted by law, Springer Nature makes no warranties, representations or guarantees to Users, either express or implied
with respect to the Springer nature journal content and all parties disclaim and waive any implied warranties or warranties imposed by law,
including merchantability or fitness for any particular purpose.
Please note that these rights do not automatically extend to content, data or other material published by Springer Nature that may be licensed
from third parties.
If you would like to use or distribute our Springer Nature journal content to a wider audience or on a regular basis or in any other manner not
expressly permitted by these Terms, please contact Springer Nature at
onlineservice@springernature.com
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (843)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5807)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (346)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Summary Chapter I To V (Io Psych Aamodt)Document10 pagesSummary Chapter I To V (Io Psych Aamodt)Joseanne Marielle75% (4)
- ED802 - CtitiquePaper - Teaching and Learning SupervisionDocument6 pagesED802 - CtitiquePaper - Teaching and Learning Supervisiongmarico5176No ratings yet
- Psa 530: Audit Sampling and Other Selective TestingDocument49 pagesPsa 530: Audit Sampling and Other Selective TestingJeric IsraelNo ratings yet
- WEBSTER - Measurement, Instrumentation, and Sensors Handbook, John G. Webster, Halit Eren-Halaman-121-135Document15 pagesWEBSTER - Measurement, Instrumentation, and Sensors Handbook, John G. Webster, Halit Eren-Halaman-121-135rizka rianiNo ratings yet
- Course Work Syllabus PDFDocument318 pagesCourse Work Syllabus PDFshivacrazzeNo ratings yet
- Co4 - Sampling and Sampling Distributions (Difference Between Means and Proportion)Document28 pagesCo4 - Sampling and Sampling Distributions (Difference Between Means and Proportion)RFSNo ratings yet
- Quantitative Ethnobotany Analysis With eDocument17 pagesQuantitative Ethnobotany Analysis With eBladimir Vera MarinNo ratings yet
- BON 410 (2023, Assignment 1 Question Paper)Document3 pagesBON 410 (2023, Assignment 1 Question Paper)GretheNo ratings yet
- DMDW SyllabusDocument2 pagesDMDW Syllabushellrider22No ratings yet
- Density BasedDocument52 pagesDensity BasedNermine LimemeNo ratings yet
- 3-ADALINE (Adaptive Linear Neuron) (Widrow & Hoff, 1960) : W X T EDocument8 pages3-ADALINE (Adaptive Linear Neuron) (Widrow & Hoff, 1960) : W X T Emuhanad alkhalisyNo ratings yet
- Programa Ciencia de Datos y Machine Learning Con Python - Feb23Document13 pagesPrograma Ciencia de Datos y Machine Learning Con Python - Feb23Carlos cardoza correaNo ratings yet
- 1 s2.0 S875572231400074X MainDocument10 pages1 s2.0 S875572231400074X MainAngelina PondeteNo ratings yet
- Exp 3Document4 pagesExp 3jayNo ratings yet
- De La Salle University - Dasmariñas: Demand Estimation For Macao Imperial Milk Tea in Cavite: A Case of Generation Z/IgenDocument27 pagesDe La Salle University - Dasmariñas: Demand Estimation For Macao Imperial Milk Tea in Cavite: A Case of Generation Z/IgenHazel Joy UgatesNo ratings yet
- Board Diversity and Its Effects On Bank Performance - An International Analysis PDFDocument13 pagesBoard Diversity and Its Effects On Bank Performance - An International Analysis PDFDavid Adeabah OsafoNo ratings yet
- Are Female Mallards Attracted To The Color Green?Document5 pagesAre Female Mallards Attracted To The Color Green?Daniel BrownNo ratings yet
- Download pdf Applied Probability And Stochastic Processes Second Edition Beichelt 2 ebook full chapterDocument53 pagesDownload pdf Applied Probability And Stochastic Processes Second Edition Beichelt 2 ebook full chapterclaudia.woltz265100% (2)
- The Comparison of Pre-Competition Anxiety and State Anger Between Female and Male Volleyball PlayersDocument6 pagesThe Comparison of Pre-Competition Anxiety and State Anger Between Female and Male Volleyball PlayersZiel SlamberNo ratings yet
- MINITAB STATISTICAL SOFTWARE For All AgesDocument7 pagesMINITAB STATISTICAL SOFTWARE For All AgesEko NurprasetyoNo ratings yet
- Metropolitan University, Sylhet: (Answer All The Questions)Document2 pagesMetropolitan University, Sylhet: (Answer All The Questions)Rifatur RahmanNo ratings yet
- Errors Related To Clinical Research TratDocument11 pagesErrors Related To Clinical Research Tratapi-661456802No ratings yet
- Asif Hanif: Analysis With Chi-SquareDocument14 pagesAsif Hanif: Analysis With Chi-SquareAsad ChaudharyNo ratings yet
- ThesesDocument30 pagesThesesPrecilla C. StephenNo ratings yet
- TUTORIAL 7: Multiple Linear Regression I. Multiple RegressionDocument6 pagesTUTORIAL 7: Multiple Linear Regression I. Multiple RegressionSumit KumarNo ratings yet
- SyllabusDocument11 pagesSyllabusJerry HeNo ratings yet
- Tuljaram Chaturchand College of Arts, Science and Commerce, BaramatiDocument20 pagesTuljaram Chaturchand College of Arts, Science and Commerce, BaramatiLiban Ali MohamudNo ratings yet
- Choosing The Correct Statistical Test in SAS, Stata and SPSSDocument3 pagesChoosing The Correct Statistical Test in SAS, Stata and SPSSunu doiNo ratings yet
- MBA Syllabus From 2019-20 190819 PDFDocument99 pagesMBA Syllabus From 2019-20 190819 PDFNilesh YNo ratings yet
- BSN 3 4 Group 7 Final ManuscriptDocument64 pagesBSN 3 4 Group 7 Final ManuscriptGave gonzalesNo ratings yet