Professional Documents
Culture Documents
Statisticsmrcpch 220704164612 Dc2ff6ad
Statisticsmrcpch 220704164612 Dc2ff6ad
Uploaded by
anitn20200 ratings0% found this document useful (0 votes)
9 views30 pagesOriginal Title
statisticsmrcpch-220704164612-dc2ff6ad
Copyright
© © All Rights Reserved
Available Formats
PDF or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
0 ratings0% found this document useful (0 votes)
9 views30 pagesStatisticsmrcpch 220704164612 Dc2ff6ad
Statisticsmrcpch 220704164612 Dc2ff6ad
Uploaded by
anitn2020Copyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
You are on page 1of 30
Statistics for the MRCPCH
irst Edition
2015
Statistics as
Important definitions
Incidence
© Incidence — the number of new cases within a defined population at a specified time
Incidence rate the numberof new cases per population at risk in a given time period
© Incidence rate = is a ratio of the number of individuals in the population who develop an illness in a given
time period (commonly 1 year) divided by the total numberof individuals at risk for the illness during that
time period (e.g. the number of IV drug abusers newly diagnosed with AIDS in 2013 divided by the number of
IV drug abusers in the population during 2013)
© Incidence proportion (cumulative incidence) + ‘he number of new
divided by the size of the popukation initially
diseased persons and 28 develop a condition over 2 years of observation, the incidence proportion is 28 cases
per 1,000 persons — 2.8%
ses within a specified time period
risk, For example, if'a population initially contains 1,000 non-
Number of new eases within a defined population ata specified time
Incidence rate = “FT population at isk daring the same period of me
Prevalence
Prevalence — the total number of cases within a defined population at a specified time
Prevalence rate— the total number of cases per population at risk in a given time period
© Prevalence rate— is a ratio of the number of individuals in the population who have an illness (e.g. AEDS)
divided by the total number of individuals at risk ‘or the illness
© Point prevalence — is a ratio of the number of individuals who have an illness at a specific point in time (e.g
the number of people who have AIDS on August 31, 2013) divided by the total population who could have the
illness on that date
© Period prevalence is a ratio of the number of individuals who have an illness during a specific time period
(e.g, the number of people who have AIDS in 2013) divided by the total population who could have the illness
during that specific time period
© Lifetime prevalence (LTP)— the proportion of a population that at some point in their life (up to the time of
assessment) have experienced the condition
‘© Prevalence rates are affected by the incidence of tie disease and the duration of illness
‘Total number of cases within adefined population ata specified time
Pisienrs al Toial population at risk daring the same period of time
%* Prevalence answers "How many people have this disease right now" and incidence answers "How many people
per year newly acquire this disease?”
+ Prevalence mate of an illness is decreased either when putients recover or die
Attack rate
+ Itis the cumulative incidence of infection over a period of time. This is typically used during an epidemic (e.g
during the influenza outbreak, the attack rate was 12%)
Itis the biostatistical measure of frequency of morbidity, or speed of spread, in an at risk population
Iris calculated by taking the number of new cases in the population at risk and dividing by the number of
persons at risk inthe population. Its usually expressed as a percentage
+ Forexample — if,aftera picnic, 20 out of 40 people who ate fried chicken and 10 out of 50 people who ate
fried fish become ill - the attack rate is 50% for chicken and 20% for fish
Number af new eases in the pepulation at risk
‘Attack rate = —"\imber of persons at isk inthe population
Statistics asa
Mortality rates
© Mortality rate is the number of deaths within a defined po pulation at a specified time
‘+ Mortality rate is typically expressed in units of deaths per 1000 individuals per year
The standardized mortality ratio is the observed mortality rate divided by the expected mortality rate
© Proportionate mortality rate (PMR) is used to determine the relative importanee of a specific cause of death in
relation to all causes of death in a population (e.g. the leading cause of death in USA in 1980 was heart disease
with a PMR of 38.2%)
© Stilbirth rate + number of stillbirths (i.e. babies bom with no signs of life after 24 weeks’
1000 total births
restation) per
© Perinatal mortality rate — number of stillbirths and deaths within the first week of life per 1000 total births
© Neonatal mortality mate > number of deaths of live bom babies aged upto | month per 1000 live births
© Infant mortality rate — number of deaths ofall infants aged under | year per 1000 live births
‘Number of deaths during one year
Montality rate = x 1000
“Total population at mid-year
Seat ‘Number of deaths due tw a diseases ina speeitied period of time
Case fatality te = Taper of cases of the disasein tiesame perodofume "100
Number of deaths froma,
3 siven cause ina specified period of time
Ee TToia] number of deaths inthe same period of me
x 100
Number of til births in a period of time
x 1000
‘Total number of births (ive & sill in the same period of time
Still birth rate =
‘Number of still births and early neonatal deaths (<7 days old) ina period of time
Beninatel matali iyate Total number of birth (live & sill) in the same period of time IDO)
Msn my «a acto
i oye = a cE
“Toul number of five births in the same period of time
© Stillbirth + fetal death and expulsion from the uterus after 24 weeks" gestation
°% Miscarriage/abortion — fetal death and expulsion fromthe uierus before 24 weeks" gestation
Study design
Research questions
* Aresearch study should always be designed to answera particular research question. The question usually
relates to a specific population, For example:
* Does taking folie acid early in pregnancy prevent neural tube defects?
+ Isa new inhaled steroial better than current treatment for improving lung function among eystic fibrosis,
patients?
© Is low birth weight associated with hypertension in later life?
A .well-built clinical foreground question should have 4 components. The PICO model is @ helpful tool that
assists you in organizing and focusing your foreground question into a searchable query
+ P= Patient, Problem, Population
+ How would you describe a group of patients similar to you?
* What are the most important characteristics 0” the patient?
‘+ 1 =Intervention, Prognostic Factor, Exposure
+ What main intervention are you considering?
+ What do you want to do with this patient?
* What is the main altemative being considered?
‘omparison (can be none or placebo)
* What isthe main altemative to com pare withthe intervention”
+ Are you trying to decide between 2 drugs, a drug and no medication or placebo, or? diagnostic tests?
+ 0=Outcome
What are you trying to accomplish, measure, prove oraffect?
* Outcomes may be disease-oriented or patientoriented
+ For exsple
+ P= pregnant women; I = folic acid:
+ P=CF patients;
+ P=newborm;
= no folic acid; O = neural tube defect ~ yes/no
new inhaled steroid: C = current treatment, O = improvement in lung function
low birthweight; C = normal birthweight; © = hypertension
‘© To answer the specified research question, random samples of the relevant populations are taken (e.g. pregnant
women, cystic fibrosis patients, LBW individuals, and normal birthweight individuals)
‘© Based on the differences found between the different groups of samples, inferences are made about the
populations from which they were randomly sampled. For example:
"Ifthe women in the sample taking folic acid have fewer neural tube defects, it may be inferred that taking
folic acid during pregnancy will reduce the incidence of neural tube defects in the population
If among our sample of CF patients, those taking steroids have better lung function on average than those
‘on current treatment, the inference might be that steroids improve lung function among CF patients in
‘general, Note that some of the patients in the sample who were on current treatment may have had better
Jung function than some of those using steroids, but itis the average difference that is considered
"If there is a difference in hypertensive rates between samples of individuals who were and were not of
LB
it may be inferred that birth weight is associated with later hypertension in the population in general
Confounding
* Confounding may be an important source of error
+ Acconfounding factor isa background variable (ie. something not of dinect interest) which:
* Is different between the groups being compared, and
+ Affects the outcome being studied
Ina study to compare the effect of folic acid supp.ementation in early pregnancy on neural tube defect
will be a confounding factor if:
* Either the folic acid group or placebo group tends to consist of older-women, and.
* Older womenare more, or less, likely to havea child with a neural tube defect,
Statisties asa
‘+ When studying the effects of a new inhled steroid against standard therapy for eystic fibrosis patients, disease
severity will be a confounder if:
* One of the groups (new steroid or standard therapy) consists of more severely affected patients, and
= Disease severity affects the outcome measure (lung function)
‘© In the comparison of hypertension rates between LBW and not LBW, social class will be a confounder if:
+ The LBW tubies are more likely to have lower social class, and
"Social class is associated with the risk of hypertension
+ Ia difference is found between the groups (folic acid//placebo, new steroid/standard therapy, and Low/nosmal
birth weight) we will not know whether the differences are, respectively, the results of folic acid or age, of the
potency of the new steroid or the severity of disease in the patient, or of birth weight or social class
© Confounding may be avoided by matching indivicuals in the
© For example;
© We could age-maich folic acid and placebo pairs
groups according to potential confounders
* We could recruit individuals of low and normal birth weight from similar social classes,
= We could find pairs of cystic fibrosis patients of similar disease severity, and randomly allocate one of
each puirto receive the new steroid while the other receives standard therapy
Different types of studies EBM Levels of Evidence
A, Descriptive studies Pyramid
LL Case reports
2 Case-series Actin noc te ies
3. Surveys studies
4 Qualitative studies
B
2. Cross-sectional study
3. Cohort study
4, Evological study
C. Experimental studies
1. Randomized control trials
a) Double blind study:
b) Single blind study
SEs
©) Unblinded study
2. Crossover study
Case series and case reports
+ They consist either of collections of reports on the treatment of inclividual patients with the same condition, or
of reports on a single patient
* Theyare used to illustrate an aspect of a condition, the treatment or the adverse reaction to treatment
* Theyhave no control group (one to compare outcomes), so they have no statistical validity
+ The benefits of case series/reports are that they are easy to understand and can be written up ina very short
period of time
t=
f ——=
Journal article
+ — 6
Patient Chart notes
4
Statistics as
Observational studies
©The researchers don't change anything, They only observe and document what occurs in one or more groups
of individuals (e.g. those who do and do not take folic acid early in pregnancy)
© When am observational study compares 2 groups, it may be categorized as being either:
1, Case control study — consider differences be-ween the groups in the past
2 Cross-sectional study — consider differences between the groups at the present time
3. Cohort study + consider differences between the groups in the future
© Case control study
+ Itis a retrospective study. This means that you begin at the end (with the disease), and then work
backwards, to hunt for possible causes
* Itusually compare diseased and healthy groups, and look back in time to see what they have done
differently in the past that may have led to disease
‘These studies are concemed with aetiology rather than treatment. They are more suitable for rare diseases
* ‘These studies can’t calculate incidence, prevalence, or relative risk. Results are expressed as odds ratios
* Case control studies are less reliable than either randomized controlled trials or eohortstudies
For example —* a study in which colon cance patients are asked what kinds of food they have eaten in the
past and the answers are compared with a selected healthy control group
$F HH | Take histories,
tet
Pasienis with condiion fe cancer)
[+ Draw conclusions
Comparison group (non-patiens)
ttt
© o & | Paeninores
© Crosssectionat study (transversal study, prevalence study)
+ A study that examines the relationship between diseases (or other health-related characteristics) and other
variables of intetest as they exist in a defined population at a specified time (Le, exposure and outcomes
are both measured atthe same time)
+ Iti usually used for quantifying:
* The prevalence of a disease or risk factor
+ Theaccuracy ofa diagnostic test
+ These stuties allow determination of prevalence and relative risk; but not the incidence
+ Itean’t evaluate hypotheses about causation, as it doesn’t take into account how the timing of exposure
to a risk factor relates to the development of disease
* For example + what is the current prevalence of cystic fibrosis in a population of adolescents ?
+ Another example— Is there an association between diabetes and overweight ?
© Cohort study (longitudinal study)
* ‘Two or more groups of subpeets are selected on the basis of their exposure or lack of exposure to a
particular risk factor or agent (e.g. drinking alcohol ornot, smoking or not, eating a high-fat diet or not),
and follow the groups forward in time to see how many in each group develop a particular disease
Cohort studies are used to establish causation of a disease or to evaluate the outcome/impact of treatment,
‘when randomized controlled clinical trials ae not possible ( more suitable for common diseases)
* Cohort studies my be either:
a) Prospective — exposure factors are identified at the beginning of a study ancl a defined population is,
followed into the future
b) Retrospective — past medical record for the defined population are used to identify exposure Factors
Prospective cohort studies are more reliable chan retrospective cohort studies
Statistics aca
* Cohort studies allow determination of incidence and relative risk: but not the prevalence
* Disadvantages include the large numbers required for rare outcomes. problems of drop-out bias, ancl
changes in practice during long follow-up periods
Cohort studies are used for determining the outcome of infants bom prematurely
© 6% & | Follow overtime eeee
aoe a ee
Group of lnerest (ex. smokers)
Compare outcomes
Comparison Group (e.g. non-smokers
eeee bees
4 & & | Followoertine ce %
© Ecological study
Here the unit of analysis is a population rathe- than an individual, and association across different
populations is investigated
«For example— an ecological study may look at the association between prematurity and childhood cancer
rates in different countries, to see whether those countries with higher prematurity rates also have higher
levels of childhood cancers
(Case-control studies Cohortstudies
Suitable for rare diseases Suitable for common diseases
‘Short study Gime and cheaper to perioam Prolonged study time with potential for mereasing
drop-out rates, and therefore more cost!
‘Smaller number of subpem required Lange number of subpets usually required
Bias may occur inthe selection of cares Tess selection bias oceurs
controls, and in ascertaining exposure
Because data collected reivospectively, some data | Prospective dala collection may be mow accunie
ay not be available or of poorer quality
No volunieersubjpets needed Subpew mally vouMeer
‘Can'tdetermine incidence, prevalence or whative | Can determine incidence, relative risk & airibuable
risk, Results are expressed as odds ratios risk; but can’t calculate prevalence
Estimate of ime [rom exposure io development | Estimate of time from exposure to developmeat of
of disease is not possible disease is possible
+e Case-control studies can’t calculate incidence, prevalerce, or relative risk, Results are expressedas odds ratios
“Cross-sectional allow determination of prevalence and relative risk; but not the inciclence
Se Cohort studies allow determination of incidence and reative risk; but not the prevalence
+e Case-control studies are highly prone to selection and recall bias
Randomized controlled trial (rando!
ized clinical trial, RCT)
+ Itis the mainstay of experimental medical studies, normally used in testi
«In randomized controlled studies:
* There are two groups, one treatment group and one control group. The treatmen
ew drugs and treatments
soup receives the
treatment under investigation, and the control group receives either no treatment (placebo) or standard
treatment. The control group does not necessarily consist of normal healthy individ wals
+ Patients are randomly assigned to ll groups
‘+ Placebo isa pharmacologically inert dummy, identical in appearance to the treatment(s), should normally be
used for the control group, when there is no conventional treatment available
Having a control group allows for a comparison of treatments (e.g. treatment A produced favorable results
‘56% of the time versus treatment B in which only25% of patients had favorable results)
+ Randomization means that each patient has the sume chance of being assigned to either of the groups,
regardless of their personal
waracteristies. Note that random does not mean haphazard or systematic
6
Statistics aon
Randomization helps to avoid the selection bias ia the assignment process. It also increases the probability
that differences between groups can be attributed to the treatment(s) under study
Allocation concealment means that the allocation (to treatment or control) is unknown before the individ ual
is entered into the study
RCT may be either:
a) Double-blind — neither the patient nor the medical staff/physician knows which treatment the patient has
been randomized to receive
b). Single-blind — either the patient or the medical staff/physician does not know (usually the patient)
©) Unblinded (or open) + both the patient and the medical staff/physician know
Itis preferable that studies are blincled, because knowl
a bias in the results
‘There are certain types of questions on which RCT can’t be done for ethical reasons, for instance, if patients
were asked to undertake harmful experiences (e.g smoking) or denied any treatment beyond a placebo when
there are known effective treatments
of treatment may affect the outcome and introduce
For example — studies of treatments that consist essentially of taking pills are very easy to do double blind:
the patient takes one of two pills of identical size, shape, and color, and neither the patient nor the physician
needs to know which is which
“The "random" in RCT refers to the equal chance in allocation of individuals to either experimental or control group,
not to the way the sample is drawn
Treatment Grow Follow
tt tt
| —Lt + tt Pr,
Compare reais
t
t
t
t
t
Control Gro Followup
Patiens / tt t?
Rano signet tt tt
Stages of drug developmentin clinical triak
Phase ‘Main aims
Preclinical | In vitro studies — pharmacology and wsicology in laboraiory animals
Phase || Checking for safety —» safety, tolerabiliy, pharmacokinetics, pharmacodynamics ba healthy
individuals andior patients
Phise2 | Checking for effieacy and dosing —> inal weamneut studies to determine the eliicacy and dosing
of the drug in asmall number of patients
Phase 3 | Confirm the results —» large RCTs comparng the new drug with the curont gold samdard drug
Phase + | Post-marketing surveillance —» long-tem salety and rare events in all patients prescribed the dn
Crossover studies
Ina crossover (or withim-patient) study, each patient receives treatment and placebo in a rand om order
Crossover studies are only suitable for chronic disorders that are not cured, but for which treatment may give
temporary relief
‘There should be no carryover effect of the treatment from one treatment period to the next
Sometimes, it is necessary to leave a gap between the end of the first treatment and the startof the next to
ensure that there is no overlap. This gap period is known as a washout period
‘The outcome may ormay not be normally distributed
Statistics as
Systematic review
adda
© Itisa comprehensive survey of a topic that takes great care to find all relevant studies of the highest level of
evidence (both published & unpublished) — assess each study — synthesize the findings from individual
studies in an unbiased, explicit and reproducible way and present a balanced and impartial summary of the
findings with due consideration of any flaws in the evidence
‘= Inthis way itcan be wed forthe evaluation of either existing or new technologies and practices
‘© Assystematic review is more rigorous than a traditional literature review & attempts to reduce influence of bias
© The difference benween a systematic neview ancl a meta-analysis is that a systematic review looks at the whole
picture (qualitative view), while a meta-analysis looks forthe specific statistical picture ( quantitative view)
Includes both published and unpublished studies
sTuby STUDY sTUuDY STUDY
1 2 3 4
Rigorous analysis and appraisal of|
‘individual studies
Systematic
Review
© Meta-analysis isa systematic, objective way to combine data from many studies, usually from RCTs, and
amive ata pooled estimate of treatment effectivenzss and statistical significance
‘Meta-analysis can also combine data from case-control and cohort stuclies
‘The results of a meta-analysis are usually expressed as odds ratio or relative risks
© The advantage to merging these data is that it ine
otherwise be possible
© Two problems with meta-analysis:
rases sample size and allows foranalyses that would not
a) Publication bias — studies showing no effector little effect are often not publisited and just
b). The quality of the design of the studies from which data is pulled
© This can lead to misleading results when all the data on the subject from “published” literature are summarized
Sina Sata State Satie!
‘The results of a before and after study should always be viewed with great caution
‘The results of both case-control studies and meta-anal
‘The mainaim of randomization is to remove selection bias and confounding
Consentto ranclomization should be obtained as a part of the overall consent to the study
Crossover trials are less prone to confounding and are more efficient than parallel trials (different patients on each
are usually expressed as odds ratio
treatment), and should be preferred where the nature and eutcome for the treatments allows them
x
n to determine whethera certain factoris causally implicated in the onset of a rare disease is
‘The best study des
case-control study
8
Statistics as
c
paring study designs
There may be many ways to address a particular rsearch question (e.g. if we wish to determine whether
smoking is causally associated with Lung ‘would potentially ad dress this question:
+ Case-control studies — would select a group of lung cancer patients and a group of healthy controls to
see how they differed in previous behaviors (ie. smoking)
* Cross-sectional studies — would show that those with lung cancer are more likely to be curent smokers
* Cohort studies + would select groups of currently healthy smokers and non.smokers, and follow these
forward in time to see whether one group was more likely to develop lung cancer
+ Ecological studies — might show a relationship between levels of smoking and lung cancer rates in
different countries/regions
+ Randomized controlled trial (RCT) — would randomly allocate healthy individuals to smoke or not,
and then see who developed lung cancer (une:hical)
* Inall of the study types, there is potential for confoundi
incer, eny of the follow’
‘eg if the smokers are more likely to drinkalcohol)
Matching the strongest research designs to clinical questions
‘Question Design
(Causationand risk factor | Case contol stuies, Cohom studies
Prevalence and diagnosis | Cross-sectional studies
Tneidence and prognosis | Color studies
Treatment Randomized consoled trails (RCT)
Intention-to-treat analysis
© NRT, the outcomes for the two allocation groups (those allocated to active treatment and those allocated to
control) should be compared irrespective of whether patients actually received or completed allocated
treatment(s) or had missing data or poor compliance
© This avoids introdueing bias into the assessment of treatment
Interim analysis
© Analyses that are cartied out before the end of the clinical trial in onter to assess whether the accumulating
data are beginning to demonstrate a beneficial effect of one treatment over the other with sufficient certainty
‘© This can avoid further patients being randomized ‘o the inferior treatment
Criteria for assessing causation
1. Specificity + ifa variable is associated with a single outcome, and the outcome is associated with only a
single possible cause, then the zelationship is more likely to be causal
‘Strength — strong associations are more likely than weak ones
Consistercy — multiple studies find ing the same thing are more likely to be causal
‘Temporality + causes must precede effects. This is absolutely necessary to suggest causation
Biological gradient + if an increased exposure isassociated with an increased rate or severity of disease, then
causality is more likely
6. Plausibility—+ hypotheses should sound reasonable, However, new epidemiolog’
knowledge
7. Coherence ~ cawsal association is strengthened if epidemiological data fits in with pathology
8. Experiment if the cause is removed and disease frequency declines, the likelihood of a causal link is
strengthened
findings may expand
9. Analogy ifa similar association has been shown to be causal, then the association under investigation is
more likely to be causal
%¥ Case-control studies are useful forstudying disease types with a long latent period
Se Observational studies cannot be randomized
9
Statistics a0
Bias, reliability and validity
Sampling bias + volunteer subjects in a study may not be representative of the population being studied:
asa consequence, the results of the study may not be generalizable to the entire population
election bias occurs when. there is a systematic difference in the way study groups are chosen. One
‘method of decreasing this bias is randomization
Recall bias — patients who experience an adverse outcome have a different likelihood of recalling an
expos ure than do patients who do not have an adverse outcome, independent of the true extent of the exposure
Expectancy bias — occurs when a physician knows which patients are in treatment versus placebo group,
causing the physician to draw conclusions supporing the expected outcome. One method of decreasing this
bias is a double-blind design
Late- look bias + results from information being gathered too late to draw conclusions about the disease or
expos ure of interest from the entire study: population. For instance, more severe cases may have already died
Measurement bi
Hawthorne effect describes how people act differently when being watched
Proficiency bias — this is an issue when compariag the effects of different treatments administered at multiple
sites. Physicians at one site may have more skill, thereby providing better treatment
Publication bias (Pasitive-outcome bias)
+ Ibis where researchers publish only favorable results
* Itis the tendency to publish research with a positive outcome more frequently than research witha
negative outcome
+ Negative outcome refers to finding nothing of statistical significance or causal consequence, not to finding
that something affects us negatively
Media bias — refers to the tendency of the media to publish medical study stories with positive outcomes
much more frequently than such stories with negative outcomes
— describes how information gathered affects information collected. For example, the
Reducing bias in clinical treatment trials
Blind studies, placebos, crossover studies, and randomized studies are used to reduce bias
Blind studies
* The expectations of subjects can influence the effectiveness of treatment
* Blind studies attompt to reduce this influence
* Ima single-blind study — the subject does not know what treatment he orshe is receiving
* Ina double-blind study — neither the subject nor the clinician-evaluator knows what treatment the
subject is receiving
Placebo responses
* Ima blind drug study, a subject may receive a placebo (an inactive substance) rather than the active drug
+ People receiving the placebo are the control group
+ People receiving the active drug are the experimental group
* A number of subjects in research studies respond to the treatment with placebos alone (the placebo effect)
Crossover stuies
* Ina crossover study, subjects are randomly assigned to one ofthe two groups
* Subjects in Group 1 frst receive the drug, ancsubjeets in Group 2 firstreceive the placebo
+ Laterin the crossover study, the groups switch + those in Group I receive the placebo, and those in
Group 2 receive the drug
* Because all of the subjects receive both drug and placebo, each subject acts as his or her own control
Randomization
+ Tnonler to ensure that the proportion of sicke-and healthier people is the same in the treatment and
contol (placebo) groups, subjects are randomly assigned to the groups
* The numberof sub jects in each group does net have to be eq ual
10
Statistics asm
Reliability
* Reliability refers to the reproducibility or dependability of results
* Interraterreliability — is a measure of whether the results of the test are similar when the test is administered
by adi fferent rater orexaminer
© Test-tetest reliability + is a measure of whether the results of the testare similar when the person is tested a
second or third time
Validity
+ Iisa measure of the appropriateness ofa test, that is, whether the test assesses what it was designed to assess
(c.g, Does a new IQ test really measure IQ or does it instead measure educational leve!?)
© Sensi
ty and specificity are components of validity
%* To be useful, testing instruments must be bias-free, reliable, and valid
+e Coverage is the proportion of children in a population who have been screened over a period of time
% Acceptable screening tests should give a yield of at least 1 in 10,000 positive diagnoses of a treatable condition
Statisties as
Quantifying risk
Absolute risk, relative risk, attributable risk, and the odds (orodds risk) ratio are measures used to quantify
risk in population studies
# The ods matiois calculated forcase-control studies and! meta-analyses
© Absolute, relative, and attributable risks are calculated for cohort studies
© Risk
* tis the probability that an event will happen
* As one boy is born for every two births — the risk (probability) of giving birth to a boy is 12 or 0.50
+ fone in every 100 patients suffers a side effect from a treatment — the risk is 1/100 or 0.01
© Absolute risk
+ It is the probability that a person will have a medical event
+ Its the ratio of the number of people who: have a medical event divided by all of the people who could
have the event because of their medical condition
* Absolute risk is expressed as a percentage
* Absolute risk is equal to the incidence rate
* For example — research studies have found that among 10,000 people age 7S and over who take
dug like ibuprofen for osteoarthritis pain, 15 of them will die from stomach bleeding. The absolute
riskof dying from stomach bleeding is 15 outof 10,000, or 0, 154 of people taking ibuprofen
© Alolute risk reduction (ARR)
= This the difference in absolute risks
+ tis away of measuring the size of a difference between two treatments
+ Forexample — if the incidence rate of lung canceramong the people in Newark and in Trenton, New
Jersey, in 2013 is 20/1,000 and 15/1000 respectively + the absolute risk is 20/1,000 or 20% in Newark
and 1.5% in Trenton — the ARR is 20% ~ 15% =0.5¢%
* Another example — ima clinical trial of a drug to prevent migraines, 2 of 100 people taking the drug
experience a migraine (2%), compared with 4 of 100 people taking a placebo (4%) —> The absolute risk
% = 2%, That is, there were 2% fewer migraines in people taking the drug
reduction is 4%
+ Relative risk (RR)
+ Itcompames the incidence rate of a disorder among indi viduals exposed toa risk Factor(e.g. ung cancer
among smokers} withthe incidence rate of the same disorder among individuals mot exposed to risk factor
* RR is the incidence rate of the exposed (or treated) group (ie. experimental event rate = EER) divided by
the incidence rate of the unexposed (or untreated) group (ie. control event rate = CER)
+ RR=EER+CER
+ Forexample — incidence mate of lung canceramong smokers ina city in New Jeney is 20/1,000 (0.02)
while the incidence rate of lung cancer among non-smokers in this city is 2/1,000 (0,002), Therefore, the
fold increase in risk of lung cancer (the relative risk) for smokers vs. nonsmokers in this New Jensey
population is 0.02 + 0.002 = 10
* A relative risk of 10 means that in this city, ifan individual smokes, his or herrlsk of getting lung cancer
is 10 times that of a non-smoker
+ Relative risk reduction (RRR)
* It is the proportion or percentage by which an intervention reduces the event rate
+ RRR = (CER ~ EER) +CER
+ Forexample — in a clinical trial of a drug-to >revent migraines, 2 of 100 people taking the drug
experience a migraine (2%), compared with 4 of 100 people taking a placebo (47)
+ RRR=(0.04-0.02) + 0.04= 0.5 = 50%
© Attributable risk
* Attributable risk is useful for determining what would happen in a study population if the risk factor were
removed (e.g, determining how common lung cancer would be in a study if people did not smoke)
+ Attributable risk is the incidence rate of the unexposed group subtracted from the incidence rate of the
exposed group
12
Statistics Asm
* Attributable risk = EER - CER
* For example + incidence rate of lu
while the incidence rate of lung cancer among non-smokers in this city is 2/1,000 (0,002), therefore, the
riskof lung cancer attributable to smoking (the attributable risk) in this New Jersey city's population is
0,02 ~ 002 = 0.018 (181,000)
© Oukte
‘ancer among smokers ina city in New Jersey is 20/1, 000 (0.023,
‘They are calculated by dividing number of times an event happens by number of times it does not happen
* For every two births, one boy is born and one boy is not bom — the odds of givi
I= 1.015050
* [fone in every 100 patients suffers a side effect from a treatment —+ odds are 1/99; while risk is 1/100
© Odds ratios (OR)
"An odds ratio is a measure of associ:
birth to a boy are
ion between an exposure and an outcome
+ An odds ratio is a relative measure of effect, which allows the comparison of the intervention group of a
study relative to the comparison or placebo g1oup
Since incidence data are not available in a case-control study, the odds ratio (ie. odds risk ratio) can be
used as an estimate of relative risk in such studies
* They are calculated by dividing ods of having been exposed to a risk factor by odds in a control group
* An odds ratio of I — the likelihood of exposure to the risk factor is identical for both cases and controls
+ Anodds ratio of > | + the likelihood of exposure to the risk factor is greater for cases than for controls
+ An ds ratio of < | + the likelihood of exposure to the risk factor is lower for eases than for controls
* Odds ratios should always be presented with their (95%) confidence intervals
© [fClineludes 1 — the relationship between risk exposure and disease occurrence is not statistically
significant
‘+ IfCI does not include | + the relationshia between risk exposure & disease occurrence is statistically
significant
* ‘The width of the interval estimates the precision of the odds ratio
+ Assmall Cl — indicates a higher level of precision of the odds ratio
‘¢ A large CI — indicates a lower level of precision of the odds ratio
Relative rk | Confidence interval Interpretation
177 (U.22- 2.45y Statistically significant (inerwased risk)
163 (85-246) NOT statistically significant (risk i the Same)
O78 (0560.94) Statistically significant (decreased risk)
TTERR > 10, then subiract 1,0 and read as percent increase, So 1,77 means one group has 77% more eases than the othe,
=I RR < 10, then subiract from 1,0 and read as reduction n risk, So 0.78 means ane gio up has a 22% reduction in risk.
Example 251 Caleulating the Odds Ratio
(f 200 patients in the hospital, 50 have lung cancer. Of these 50 patients, 45 are smokers. Of
the remaining 150 hospitalized patients who do not have lung cancer, 60 are smokers. Use
tis information to calculate the odds rato for smoking and lung cancer in this hospitalized
patient population,
Pocple wih ing cancer
Pecple wirut ung at
(aD) =(45)(90)
(BC) = (51060)
=13.5 = Odds ratio
‘An odds ratio of13.5 means that in this population, a person with lung cancer was 13.5 times
‘more likely to have smoked than a person without lung eancer.
13
Statisties asm
© Number needed to treat (NNT)
+ NNTis the number of persons who need to take a treatment for one person to benefit from the treatment
* It is the reciprocal of ARR, and is more meanngful than the RRR for assessing the efficacy of a treatment
* RRRis constant regantless of risk, whereas NNT is likely to be higher in low risk groups
+ NNT is I divided by the ARR [NNT =1+ ARR]
© Number needed to harm (NNH)
* NNH is the number of persons who nead to be exposed to a risk factor or one person to be harmed who
‘would otherwise not be harmed
+ NH is I divided by the attributable risk [NNH
ttributable risk]
Example 25.2 Number Nee
Aresearch study is done to determine if new drug (Drug S) will prevent stroke in men aged
55-65 with hypertension.
Four thousand hypertensive men in this age group are randomly assigned to a group
taking Drug (n= 2,000) or a placebo (n= 2,000).
Over 10 years there were 1,200 strokes in the placebo group and 200 strokes im the Drug
S group,
Based on these data, how many men would have to be treated with Drug S to prevent one
case of stroke?
‘The absolute rsk of stroke in the placebo group is 1,200/2,000 = 60%.
‘The absolute risk of stroke in the Drug group is 200/2,000 = 10%.
‘The absolute risk reduction is therefore 60% - 10% =50%.
Since 50% of the hypertensive men were saved from stroke by the drug, the NNT is 1/0.5=2.0,
‘Therefore, two men would have to be irexted with the Drug to prevent one case of stroke.
to Treat
Absolute risk
Absolute risk reduction = the difference in absolute risks
Relative risk = BER = CER
‘Attributable risk = EER -CER
Relative risk reduction = (CER - EER) + CER
NNT= 1 + absolute risk reduction
NNH = | = attributable risk
Odds ratio= (A x D) = (Bx ©)
(Odds and risk give similar values for rare events, but may be very different for common events,
(Odds ratio are best described as the odds of an event in one group divided by the odds of the event in another
‘The test thresholds the value below which treatment is not required
‘The treatment threshold is the value at which a test is not warranted as the diagnosis is clinically very likely
incidence rate
Ad ddd dead
Statistics asm
Clinical probability
Clinical probability is the number of times an event actually occurs divided by the number of times the event
Example 25.4 Clinical Probability
“After 3 years of elinical trials of a new medication to treat migraine headache, it is deter-
‘mined that 20% of patients taking the new medication develop hypertension. Iftwo patients
(patients A and B) take the drug, calculate the following probabilities.
41. The probability that both patient A and patient 8 will davelop hypertensi
‘Thisis calculated by multiptyingthe prob ability of developing hypertension by theprob-
ability of B developing hypertension (the multiplication rule far independent events).
‘The probability of A developing hypertension =0.20 =20%,
The probability of B developing hypertensi =20%.
‘The probability of both A and B developing hypertension =0.200.20=0.04 = 4%.
‘2 The probability that at least one ofthe two patients (either A or B or both A and B)
will develop hypertension:
‘This is caleulated by adding the probability of A developing hypertension to the prob-
ability of B developing hypertension anc then subtracting the probability of both A and
B developing hypertension (the addition rule).
020 +0.20-0.04=0.36=36%,
‘3. The probability that neither patient A nor patient B will develop hypertensi
This is calculated by multiplying the probability of patient A being normotensive by the
probability of patient B being normotensive: Probability of both being normotensive =
(1. = probability of A being hypertensive) x (1 = probability of B being hypertensive) =
0.80 ~0.80=0.54= 64%,
15,
Sita tisties as
Screening tests
«Screening tests are often used to identify individuals atriskof disease. Individuals who are positive on
screening may be investigated further to determine whether they actually have the disease
* Some of those whore scrwen-positive will not have the disease ({e. falve-positive sereen test)
+ Some of those whoaze sereen-negative will have che disease (1c. Fake-negative screen test)
# This gives a 4-fold situation as shown in the box below (a,b, cand d are the numbers of individuals who fall
into each ofthe 4 categories)
Sea test aa tit src Totals
+ There are severalsummary measures that are often used to quantity how good a screening testis:
* Sensitivity — is the proportion of true positives correctly ident
positive screening test in diseased individuals [a +(a+c)] x 100
+ Specificity is the proportion of true negatives correctly identified by the test—> proportion of true
negative sereening test in healthy individuals + [d = (b+ d] x 100
+ Positive predictive value — describes the chance of a patient having the disease if the test is positive +
proportion of true positive screening test inall positive individuals — [a =¢a +b)]x 100
* Negative predictive value — describes the cxance of a patient being disease fiee if the testis negative —
proportion of true negative screening test in al negative individuals — [d =(e +d)] x 100
+ Prevalence (pretest probability) — (a +c) +(a+b+e+d)
* Aceuracy — proportion of true +ve and true~ve toall individuals + (a +d)=(a+b+e+d)
+ Systematic error = (a+b) = (a+)
+ Forall of these measures, larger values are associated with betler screening tests
ied by the test — proportion of tue
* A high sensitivity implies few false negatives, which is important for very rare or lethal diseases
+ A high specificity implies few false positives, which is important For common diseases (e.g. diabetes)
+ Predictive value is the test's ability to identify those individuals who truly have the disease (true positive)
gst all those individuals whose screening tests are positive (true positive + false positive)
‘+ The sensitivity, specificity, and likelihoad ratios do mot depend on the prevalence of the disease
‘The PPV and NPV depend on the prevallence of the disease, and may vary from population to population
* If the prevalence is increased — PPV increases, NPV decreases & the proportion of fake positives decreases,
© Lowering the screening cut-off level:
* Increases the sensitivity, fake-positive results, and negative predictive value (NPV)
* Decreases the specificity, false-negative results, and positive predictive value (PPV)
+ No change in the incidence or prevalence of tre disease
od ratios
‘© These compare the probability of the test result given that the individual has the disease to the probability of
the result occurring if they are disease free
© They are calculated from the sensitivity and spect‘city, and are not dependent on disease prevalence
+ Positive likelihood ratio (LR4+) — sensitivity + (100~speciticity)
© Negative likelihood ratio (LR-) — (100 sensitivity) + specificity
© LR> 1 indicates that the test result is associated with the presence of the disease
© LR <0.1 indicates that the test result is associated with the absence of disease
‘Pre-test odds — the odds of having the disease before you «lo the test — [pretest probability ~ (1 - pretest
probability)]
© Post-test odds — the odds of having the disease efter you did the test + pre-test odds x LR+
ES
16
Statisties as
Pre.test probability (~ prevalence) — is the pro2ortion of people in the population at risk who have the
disease at a specific time or time interval (ie. the point prevalence or the period. prevalence of the disease)
Post-test probability — is the proportion of patients testing positive who truly have the disease — [post-test
odds +(1 + posttest odds)]
‘The mule of thumb is that a high sensitivity helps to rule out disease (SnOut) anda high specificity helps to rule in
(Spin) disease
Example
A screening testis applied to 300 patients with and without disease X. Of 100 who have the disease, 60 test
positive: andl of 200 without the disease, only 20 test postive
‘The following table can be constructed:
Screening test result Dias X | Disasefree [Towle
Positive (indicating possible disease) 60 20 80
Negative 0 Tso 2207
Touls 100. 200) 300
a+ (atc) =60 + (60 + 40) = 0.6 or 50%E
Specificity = d +(b +d) = 180 +(20 + 180)= 0.9 or 90%
Positive predictive walus (a+b) = 60 +(60 + 20) =0.75 or 75%
Sensitivity
# Negative predictive value =d +(c +d) =180 + (40+ 180) =0.8 or 80%
* Prevalence (pre-test probability) = (a +c) +(a+b + c+ d) = 100 +300 =
© Accumicy = (a +d) +(a+ b+ e+) = (60 + 180) +300 = 08 or 80%
Systematic error =(a + b) =(a+e) =
= Positive likelihood ratio (LR) 100-90)
‘+ Negative likelihood ratio (LR-) = [(100— sensitivity) + specificity] = (100 ~60) +90 =0.44
* Pre-test odds = [pretest probability = (I - pretest probability)] = 0.33 + (1 ~0.33) =0.49
# Post-test odds = pre-test odds x LR+ = 0.49x 6 = 294
‘= Post-test probability = [post-test odds + (1 + post-test oids)] = 2.94 (I + 2.94) = 0.75
Example
* Ina study of the utility of serum procalcitonin level for early diagnosis of bacteraemia, £00 consecutive febrile
patients admitted to hospital were tested for serum procalcitonin and culture of bacteria It was reported that
serum procalcitonin level above 0,5 microgram/L had a speciticity of 90% in detecting bacteraemia
+ A specificity of 90%% means that 90Fé of individuals without the disease ( bacteraemia) will test negative
(serum procaleitonin levels less than 0.5 jig/L.)
+ Therefore, 10% of individuals without the disease (bacteraemia) would be expected to falsely test positive
(serum procaleitonin levels more than 0.5 jig/L)
Example
Ina study of the utility of serum procalcitonin level for early diagnosis of bacteraemia, 100 consecutive febrile
patients admitted to hospital were tested for serum procalcitonin and culture of bacteria. It was reported that
citonin level below 0.5 microgram/L had a negative predictive value of 95% in detecting
NPV of 95% means that 95% of patients who hav2 serum procalcitonin level below 0.5 microgram/L (tested
negative) do not have bacteraemia
‘Therefore, 5% of patients who have serum procalcitonin level below 0.5 micr
‘would be expected to have bacteraemia
sram/L (Fabely tested negative)
Statistics ASM
Types of data
Distributions
Data may be either qualitutive (categoric) or quantita five (numes
4) Qualitative data + can be nominal or ondinal
b) Quantitative data— can be discrete or continuous,
Qualitative (categorie) datae
* Deals with descriptions
"Data can be observed but not measured. For example:
+ Colour of eyes blue, green, brown, etc
+ Socio-economic status + low, middle, orhigh
"Qualitative dats are classified as either:
‘* Nominal — if there is no natural onder between the categories (e.g, eye colour)
* Ordinal + if there is a natural order between the categories (e.g. exam results, socio-economic status)
+ Ifthere are only two categories, then the variable is binary
Quan titative (numeric) dite:
* Deals with numbers
* Data can be measured (e.g length, height, area, volume, weight, speed, time, temperature, humidity)
+ Quintitative data are classitied as either:
* Discrete — if the measurements are integers (Le. a whole number such as 3 or 4, but not 3.5) (e.g
‘number of people in a household, number of cigarettes smoked per day, number of antibiotic courses)
+ Contimious — if the measurements can take on any value, usually within some range (BW, HR, BP)
* Quantities such as sex and weight are called variables, because the value of these quantities vary from
one observation to another
= Numb
calculated to describe important featurse of the data are called statistics
Ranking data
Ranking the data involves putting the values in numerical order, and then assigning new values to denote
‘where in the ordered set they fall
We give the smallest value the rank 1, the next largest walue the number 2, the next largest number 3 ete
‘The numbers 1.2.3... that are assigned to the various values are called the ranks
‘The highest value will have a rank equal to the total number in the sample (i.e. if there are a values in the
sample, the largest value will have rank: 2)
Equal data values should be given equal ranks, Ta achieve this, the corresponding ranks will be averaged
between the data values
Non-parametric tests use the ranks rather than the original data values in the subsequent analysis,
‘The median (ie. middle ranked value) is used as a measure of centre
Non-parametric tests make comparisons of medians between groups as opposed to parametric tests which
compare means
‘The ranks yield a lot less information than the original values and are not very sensitive to changes in the data
For example — rank the following sample of 14 values (2, 34, 8, 7, 25,2. 34, 34, 67.
+ Sorting the values into the order of magnitude gives + -7, -5. 2. 0,2,2, 7, 23,25,
* Ranks are assigned
Watues [7 [3 [2 [0 ]2 [2 [7 [23 [25 [28 [38 [se a
Ranks [1 2 Ps lal? tetets 19 Lol? 1? 1? bs
+ There are 14 numbers + the smallest value has a rank of 1, while the largest number has a rank of 14
"The ranks 5 and 6 need to be assigned to the two "2's — hence assign rank (546)/2 = 54 to each value 2
"The ranks 11,12 and 13 need to be assigned to the three "M's — hence assign rank (11412413)/3 = 12 to
each value 34
Statistics aM
* ‘Thus, the ranks for the sample will be:
Vatees [TTS [2] 0. > [2 [7 [23 125 es Ps [LT
Ranks [1 [2 Ps |e] sels4[7)s [9 fof [a2 faa fis
Measures of central tendency
i
2
Mean (= average)
+ The sumof the values of the observations div-ded by the numbers of observations
* Use the mean to describe the middle of a set of data that does not have an outlier
Median (= middle)
‘The central value of data series when the values are lined up in order of magnitude (50 percentile value)
* Use the med ian to describe the mieldle of a set of data that does have an outlier
+ To get the median — you first put your numbers in an ascending or descending order
+ If you have an odd number of numbers — the median is the center number (e.g
3.4.9)
* If you have an even number of numbers —» the median is the average of the two innermost numbers (& g
2.5 is the median for the numbers f, 2, 3,7)
Mode (= must frequent)
© ‘The most frequently occurring value in a set of observations
3 is the median forthe
numbers 1,
Its not always representative of the true cena value
* Use the mode when the data is non-numeric or when asked to choose the most popular item
+ tis possible to have more than one mode, and itis possible to have no mode
* fthere is no mode + write “no mode’, and do not write zero (0)
For example — find the mean, median and mode for the following data: 5, 15, 10, 15,5, 10, 10, 20, 25, 15
+ Firstly. you will need to organize the data in an ascending onder — 5,5, 10, 10, 10, 15, 15, 15, 20, 25
"Mean =(5 +5 +104 10+ 10-415 419 +15 +20-+25) +10 = 130+ 10=13
+ Median — 5,5, 10, 10, HO)15, 15, 15, 20, 25
‘© Listing the data in onler (from smallest to largest) is the easiest way to find the median
+ ‘The numbers 10 and 15 both fallin the middle
‘+ Average these two numbers to get the median — (10-+15)+2= 12.5
* Mode — Two numbers appear most often (10 and 15), There are three 10's and three 15's, In this
example there are two answers for the mode
‘What will happen to the measures of central tendency if we add the same amount to all data values, or
multiply each data value by the same amount?
Data ‘Mean | Median [Mode
‘Original Data Set 6.78.10 2.141415.16.20 [22 | | 4
"Add 3 19 each dat value 910,11, 18 15,1717, 18.19.57 [152 | le | 17
Muliply 2 times each data value | 12, 14.16, 20, 24, 28. 28. 3032.0 | 244 [26 | 28
When added — since all values are shifted the sme amount, the measures of central tentleney all shifted by
the same amount. If you add 3 to each data value you will add 3 to the mean, mode and median
‘When multiplied + since all values are affected by the same multiplicative values, the measures of central
tendency will feel the same affect. Ifyou multiply each data value by 2, you will multiply the mean, mode
and median by 2
al Esty of Scones the lowes score repced with cae
19
Statistics acm
* The two sets of scores above are identical except forthe first score, The set on the left shows the actual
scores. The set on the right shows what would happen ifone of the scores was WAY out of range in regard to
the otherscores, Such a termis called an outlier
© With the outlier the mean changed, but the meslian did not change
Shapes of distribution
A. Normal distribu tion (Gaussian or Bell-shaped distribution
+ The normal distribution is symmetrical and bell-shaped, with one side the mirrorimage of the other
* Ifdistribution is normal:
* The mean and standard deviation are preferable as a summary of the data
* The mean, median, and mode are equal
* About 68% of the observations fall within one standard deviation of the mean
About 98% of the observations fall within 2 standard deviations of the mean
+ About 99.7% of the observations fall within 3 standard deviations of the mean
B. Skewed dstibuton
@ Adutebutieo tot i axyemnet (eset)
© [fdistiibution is skewed — the median & interquartile range (IQR) are preferable as a summary of data
‘+ The skew is named acconding to the direction in which the tail points
+. ‘Acstowed Gitdintbeviie lopgartull ammogtbe: evorvsioe is sontilindel oc ogee
1° Acs cst th Tonge tale the dighervelies i sewed Wright oe poniedysinred
© In general, if the curve is skewed:
x Tip tran i cinays ona ne bag
Fhesmnd natvaynon bes bop ofbe crs
* The median is somewhere between the two
en eee
i Whee te aan see privy stowed Pea 5 nitions ate
Kiepiteonsk:—_iligtionhy aii
se
=
a r
i x
—————
as
> Logarithmic conversion may transforma skewed distri>ution toa normal distribution
eA positive skew has the tail to the right, and the mean greater than the median
oe A negative skew has the tail to the left, and the median greater than the mean
+e For skewed distributions, the median is a better representation of central tendency than is the mean
Statistics ASM
Measures of variability
+ Measures of variability tell you how “spread out” or how much variability is present in a set of numbers
«Measures of variability should be reported along with measures of central tendency because they: provide very
different but complementary and important information
+ Aneasy way to get the idea of variability isto look at two sets of data, one that is highly variable and one that
is mot very variable
+ For example, which of these two sels of numbers appears to be the most spread out, Set A or Set BP
Set A 93, 96, 98. 99, 99, 99, 100
* Set B— 10,29, 52, 69, 87,92, 100
# Ifyou said Set B is more spread out, then you are right! The numbers in set B are more spreat! out
they are more variability
‘© Measures of variability include the range, the variance, and the standard deviation
* Range
+ It is the difference between the largest and smallest value
* For example the range in Set shown above i 7, and the range in Set B shown above is,
ince (c
+ It is the average of the squared differences between each value and the mean
* Thmeasures how fara set of numbers is spread out
* Ittells you (exactly) the average deviation from the mean, in "squared units’
+ Assmall variance indicates thatthe data points tend to be very close to the mean and hence to each other,
while a high variance indicates that the Gata points are very spread out from the mean and from each other
* A variance of zero indicates that all the values are identical (e.g. forthe data 3, 3.3,3, 3, 3, the variance
and standand deviation will equal z2r0)
* For example, how to calculate the variance forthe following data 3, 4, 4, 5.6.8
+ Firstly, calculate the mean (3 4444454648) =6=5
‘© Then foreach number: subtract the mean and square the result — [(3-5)' +(4-5)"+ (4-5)'+ (5+
(6-5)*+ (8-51 =4+1+1404149= 16
+ Finally, calculate the average of those squared differences + 16 +6=2.7
© Standard deviation (o)
* It is the square root of the variance
+ ‘The standard deviation tells you (approximately) how farthe mumbers tend to vary from the mean.
* SD should only be used when the data has a normal distribution
* Iis important to distinguish between the standard deviation of a population and the standard deviation of
sample. They have different notation, and they are computed differently
* The standard deviation of a population is denoted by 6, and the standard deviation ofa sample, by s
that is,
se Percentile or centile — the value below whicha certain percentage of values fall. The value at the 50" percentile
means that half the data is above and half below that value,
de Interquartile range — usually describes the data which fall between the 25" and 75" percentile
se Lead time — the interval between identification ofa condition by screening and the development of symptoms,
© Lag time — the interval between an intervention being assessed as clinically useful and an intervention actually
entering everyday practice
21
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5810)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- PICU SGH Survival Guide May 2019Document23 pagesPICU SGH Survival Guide May 2019anitn2020No ratings yet
- 2020 Medical GuidelinesDocument406 pages2020 Medical Guidelinesanitn2020No ratings yet
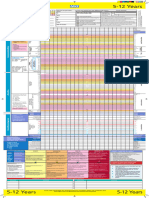
- Pews Observation and Escalation Chart 5 12 Years UpdatedDocument1 pagePews Observation and Escalation Chart 5 12 Years Updatedanitn2020No ratings yet
- National GuidelineDocument110 pagesNational Guidelineanitn2020No ratings yet