Professional Documents
Culture Documents
How Do Patients With Urinary Incontinence Perceive Care Given by Their General Practitioner? A Cross-Sectional Study
Uploaded by
drilaydacayOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
How Do Patients With Urinary Incontinence Perceive Care Given by Their General Practitioner? A Cross-Sectional Study
Uploaded by
drilaydacayCopyright:
Available Formats
doi: 10.1111/j.1742-1241.2007.01693.
ORIGINAL PAPER
How do patients with urinary incontinence perceive care
given by their general practitioner? A cross-sectional
study
P. Albers-Heitner,1 B. Berghmans,2 F. Nieman,3 T. Lagro-Janssen,4 R. Winkens5
1
Integrated Care Unit, SUMMARY
University Hospital Maastricht, What’s known
Maastricht, the Netherlands Background: Urinary incontinence (UI) is a widespread problem, affecting quality • Urinary incontinence (UI) is a widespread problem
2
Pelvic care Center Maastricht of life and leading to high costs, mainly caused by incontinence pads. It seems with great impact on quality of life and with high
(PcCM), University Hospital annual costs for patients, health insurance
that, despite guidelines, many UI patients get pads from their general practitioner
Maastricht, Maastricht, the
companies and society in general.
Netherlands (GP) without adequate diagnostics or treatment. Objectives: To assess what fur-
3 • Worldwide evidence-based clinical practice
Department of Clinical ther treatment UI patients receive from their GP next to pads and to measure
guidelines recommend lifestyle advices, bladder
Epidemiology and Medical patient satisfaction with care. Methods: A postal survey among UI patients who
Technology Assessment, training and pelvic floor muscle training as the
started pad use in the past 12 months. Main outcome: Satisfaction with UI care. first step in initial management of stress, urgency
University Hospital Maastricht,
Maastricht, the Netherlands Results: We analysed 208 questionnaires. 29.3% of pad users had no direct con- and mixed UI.
4
Women’s Studies Medicine, tact with their GP for a pad prescription. Of 147 UI patients who visited their GP • Many healthcare experts in this field express their
Department of General Practice 50.3% only got pads. 25% of patients was not satisfied with the information on serious doubts about the quality of care for UI.
UMC, St. Radboud University
UI received from their GP, especially younger patients, women, less healthy
Hospital Nijmegen, Nijmegen,
patients and patients with urgency UI. Conclusions: Dutch UI patients using pads What’s new
the Netherlands
5 • Dutch UI patients using pads (care) on
Department of General experience suboptimal GP care and management. Factors identified through patient
prescription* experience suboptimal GP
Practice, Maastricht University feedback should be used to improve quality of care for UI in primary care.
and Integrated Care Unit, management (cure and care).
University Hospital Maastricht, • UI patients want more information and education
Maastricht, the Netherlands about their UI than currently provided.
• This article provides necessary patient feedback
Correspondence to: for improvement of GP management.
Pytha Albers-Heitner,
Integrated Care Unit, University
Hospital Maastricht, PO Box
5800, 6202 AZ Maastricht,
and large all these guideline patterns in primary or
the Netherlands
Introduction
Tel.: + 31 43 3875391 in specialised care contain the same messages and
Fax: + 31 43 3874438
Urinary incontinence (UI) is a widespread medical initial management steps. When UI patients are seek-
Email:
c.albers@caphri.unimaas.nl problem with a great impact on quality of life and ing professional help, in many European countries,
with high annual costs, mainly caused by the use of such as the United Kingdom and the Netherlands,
Disclosures
incontinence pads. However, the prevalence of UI is they will first present to the general practitioner
None.
under-reported and under-diagnosed, a fact which is (GP) (3,4). Over 1 million people in the Netherlands
The departments 1, 2 and 5 often not recognised by healthcare providers. Gener- suffer from UI. Earlier studies have revealed that one
are involved in the School for
ally, prevalence of ‘any UI’ in young adult women of four people with UI (250,000) do not seek medi-
Public Health and Primary Care
(Caphri) of Maastricht amounts to 20–30%, increasing up to 30–40% in cal help. From the remaining 750,000 UI patients
University, the Netherlands. middle-aged females and up to 30–50% in the elderly who do seek medical help, 79% (590,000) get incon-
patients. UI prevalence in men, although not investi- tinence pads on prescription to a total amount in
In the Netherlands, a first-time
prescription by a physician is gated to the same extent as for females, appears costs of roughly 160 million euros each year (€270
needed to get pads paid by the much lower but increases with age (1–3). There are per patient per year). In the Netherlands a first time
insurance company.
worldwide evidence-based clinical practice guidelines prescription by a physician is needed to get pads
for initial management, assessment and treatment for paid by the insurance company. By their sheer
UI with lifestyle advices, bladder training (BT) and amounts pads are the most expensive of all health-
pelvic floor muscle training (PFMT) for all health care aids. Due to ageing of the population a further
professionals dealing with UI. In addition to this, increase of both prevalence and costs of UI in the
medical therapy and other physical therapy adjuncts near future is to be expected (1). It is often hypoth-
and devices belong to initial management (1–3). By esised that pads are necessary and are prescribed next
ª 2008 The Authors
508 Journal compilation ª 2008 Blackwell Publishing Ltd Int J Clin Pract, March 2008, 62, 3, 508–515
Perceptions of urinary incontinence patients 509
to the recommended ⁄ necessary treatment. However, literature was found to answer our specific questions
given the magnitude of this health problem and the on the satisfaction with care received for UI. There-
high costs for incontinence pads, the impression rises fore, we developed a pilot questionnaire loosely
that many UI patients get incontinence pads from based on the ‘European Project on Patient Evalua-
their GP without adequate diagnostics and treatment tion of General Practice Care’ (EUROPEP), a stan-
(5,6). This would imply a very great number of dardised and validated instrument to evaluate
patients with suboptimal care and unnecessary high specific aspects of GP care (12).
costs of incontinence pads. Consequently many Perceptions of UI care are measured by questions
healthcare experts in this field express their serious on actual experiences of clinical care (indicators
doubts about the quality of care for UI (1–3). based on Guideline on Urinary Incontinence of the
To improve efficacy and acceptability of care it is Dutch College of General Practitioners) (GLUI) (13).
important to listen carefully to the patient’s opinion Frequency, amount, impact, severity and type of UI
(7). Patient feedback surveys are increasingly seen as and perceived cause of symptoms of UI are measured
a key component in monitoring and improving qual- using the International Consultation on Incontinence
ity of care (8). However, there is a limited number Questionnaire-Short Form (ICIQ-UI SF). The ICIQ-
of studies evaluating improvement in care in this UI SF has been tested and is recommended for use
specific population, hence, availability of data is in both clinical and epidemiological studies (14).
sparse (9,10). Therefore, we conducted a cross-sec- Additionally, patient characteristics were assessed
tional sample survey in the Netherlands among adult [age, gender and perceived general health with five
UI patients, who recently received incontinence pads. response options from (very) well to (very) bad
First, we assessed what kind of initial management (15)]. After a pilot with 15 respondents a revised
pad users have got from their GP during the past questionnaire was used in this study. For measuring
12 months. Furthermore, we assessed satisfaction of ‘patient satisfaction’ statements are used with
patients with GP care. The main research questions response measured by a 5-point Likert scale with
are: ‘What kind of initial management do UI patients items having answering categories ranging from
get from their GP and is this management related to ‘complete disagreement’ (score 1) to ‘complete agree-
patient characteristics? Are pad users satisfied with ment’ (score 5). Severity of UI is measured using
GP care and is satisfaction related to patient charac- weighted scores on three questions from the ICIQ-
teristics and type of care received?’ UI SF (self-reported UI frequency, perceived UI
quantity and UI interference with everyday life in the
past 4 weeks) with an overall score theoretically
Methods
ranging from 0 to 21. Scores from three items of the
Our primary outcome measure is patient satisfaction self-diagnostic instrument are combined to classify
with care for UI received from their GP. To avoid the perceived type of UI as stress (SUI), urgency
recall bias we focused on measuring satisfaction dur- (UUI) or mixed UI (MUI): ‘leaks before you can get
ing the 12 months preceding the survey. We assumed to the toilet’, ‘leaks when you cough or sneeze’ and
that a number of 150–200 UI patients using pads ‘leaks when you are physically active ⁄ exercising’. Def-
was necessary to accurately and representatively mea- initions of UI are conform International Continence
sure the degree of satisfaction with care received. A Society (ICS) standards (16).
non-response of 75% was considered possible, so we
contacted approximately 800 pad users to participate
Statistics
in the study. The study was held in two Dutch
regions. In one region (A, low urbanisation rate) Mean and standard deviation values are reported for
patients were detected from pharmacists data and a univariate distributions of variates, frequencies and
private company providing pads. In the other region percentages for categorical data. Kolmogorov–
(B, high urbanisation rate) names and addresses Smirnov tests were used to investigate normality of
from a regional health insurance company were used. distributions. Bivariate analysis was performed in
Patients had to be adult and capable to fill in forms. cross-tabulations either with vL2 statistics or by corre-
Only patients who had pads prescribed within lations (r, Pearson correlation or q, Spearman rank
12 months were included. Questionnaires were dis- correlation coefficient). Independent groups Student’s
tributed either immediately at delivery of the pads or t-tests were performed on normally distributed vari-
by post. Representativeness of the sample of UI ates and Mann–Whitney (M–W) tests on non-nor-
patients was cross-checked with data from the mally distributed variables. Multivariate distributions
European Prospective Urinary Incontinence Research of categorical data or items belonging to a domain
(PURE) study (11). No questionnaire in the were analysed by higher-order cross-tabulations to
ª 2008 The Authors
Journal compilation ª 2008 Blackwell Publishing Ltd Int J Clin Pract, March 2008, 62, 3, 508–515
510 Perceptions of urinary incontinence patients
find patterns in response. Logistic regression analysis Fifteen per cent of the patients could not be classi-
was performed to analyse which patient characteris- fied because of lacking responses. More than half of
tics were associated with care received. Multivariate respondents said they had a moderate-to-(very) poor
analysis of (sets of) items supposed to belong to com- general health. There is a significant relationship
mon domains was performed by principal component between a poor general health and a higher UI sever-
analysis using list-wise deletion of missing cases. ity sum score (Pearson r = 0.256; p = 0.001).
Oblique rotation of factors was used and factor load- Of the 208 patients, 70.7% remembered to have
ings had to be minimally 0.60 or –0.60. Cronbach’s visited their GP during the past 12 months.
alpha was used to measure the internal consistency of
intended scale(s) found as factors. Final scales were Initial management by the GP
formed by summing the scores of the 5-point Likert Half of the patients who consulted their GP reported
items belonging to each factor divided by the number that they only got pads prescribed (Table 2). Only
of validly scored items. This way the resulting scale 16% said they got information, explanation or
scores would also lie within the 1 (fully agree) to 5 instructions on making a bladder diary, BT or
(fully disagree) range. Missing data in the numerator PFMT. 25% reported to be referred to the physio-
of the scale construction were set on zero and therapist and ⁄ or to the medical specialist. Referral is
patients had to have four of six valid (non-zero) much higher in patients with a high severity sum
scores on the items belonging to the scale in the score [log-likelihood v2: 7.05 (p = 0.008),
denominator to obtain a valid total scale score. An OR = 1.169, 95%CI 1.036–1.318]. Of all patients
explorative multivariate (dummy) regression analysis 11% (n = 16) (SUI, 6; UUI, 4; MUI, 5; other UI, 1)
was performed for each of satisfaction scales to ana- got a prescription for medication of whom 6%
lyse if (clinical) patient characteristics, such as gender, (n = 9) as a single treatment.
age, type of UI and severity of UI, did have a statisti-
cally significant relationship with them. Type of care Patient satisfaction
given by the GP as reported by patients was also used In principal component analysis on items measuring
as a potential predictor in both satisfaction scale satisfaction with the amount and quality of GP care
models. For this purpose, the reported type of care is two factors were found (Table 3). The first can be
categorised into four classes: ‘only pads’, ‘advice next named ‘personal attention received with regard to
to pads’, ‘referral next to pads and ⁄ or advice’ and UI’, the second can be called ‘information and advice
‘medication ⁄ pessary next to pads and ⁄ or advice’. received with regard to UI’. Reliability of both
A p-value of < 0.05 was considered as statistically intended scales was sufficient (Cronbach’s a = 0.96
significant. All data were analysed with spss-pc, and a = 0.97 respectively), and no items had to be
version 12 and 15 (SPSS Inc., Chicago, IL, USA). removed to enhance reliability even further. Overall
scale mean for the evaluation of ‘personal attention’
is 4.31 (SD 1.03), so, the percentage of patients
Results
agreeing with these positively stated items is approxi-
Between January 2005 and February 2006 question- mately 100% · 4.31 ⁄ 5.00 = 86%. Overall scale mean
naires were handed to 869 UI patients using pads on for the evaluation of ‘advice and information’
prescription. In region A, 444 (51%) patients were appears to be somewhat lower (3.69), so, the per-
recruited and 425 (49%) patients in region B. In centage of patients agreeing with these positively sta-
total 285 (33%) questionnaires were returned, 77 ted items is approximately 100% · 3.69 ⁄ 5.00 = 74%.
(9%) were blank, thus 208 (24%) could be further Using the scale ‘evaluation of the attention the GP
analysed. Major reasons for non-response were has given to the UI problem’ as a dependent variable
‘no ⁄ too little UI (n = 37) or not interested ⁄ no time’ the final (dummy) regression model includes four
(n = 14). statistically significant predictors: age, general health
perception, type of UI and the type of care received
Patient characteristics (Table 4). Younger people, the self-assessed less
Respondents were mainly women and they were sig- healthy people and patients with UUI are less satis-
nificantly younger than men (p = 0.047) (Table 1). fied with the attention they received from the GP
Most (86%) respondents reported having UI at least (p = 0.016, p = 0.041 and p = 0.007 respectively).
daily and more than half reported to have moderate- Patients who have been referred are more satisfied
to-large amounts of UI. The mean ICIQ-UI SF sever- with the attention from the GP (p = 0.013). Predic-
ity score was 12.6 (SD 3.9). Of the 208 patients, 40% tors tend to strengthen each other within the regres-
reported that they presumably suffer from SUI, 14% sion model, e.g. having UUI compared with SUI is
from UUI, while the scores from 30% suggest MUI. significantly correlated with higher age (r = 0.32,
ª 2008 The Authors
Journal compilation ª 2008 Blackwell Publishing Ltd Int J Clin Pract, March 2008, 62, 3, 508–515
Perceptions of urinary incontinence patients 511
Table 1 Demographic and clinical characteristics of the patients in the survey
Patient characteristics Overall Females Males
Gender, n (%) 208 (100) 183 (90.1) 20 (9.9)
missing = 5 (2)
Age, mean ± SD 63.6 (13.1) 62.9 (13.0) 68.8 (13.7)*
missing = 16 (7.7) missing = 19 (9.1)
UI frequency, n (%)
£ 1x ⁄ week 12 (5.8) 10 (4.9) 2 (1.0)
2 ⁄ 3 ⁄ week 18 (8.7) 15 (7.4) 3 (1.5)
‡ 7 ⁄ week 178 (85.6) 158 (77.8) 15 (7.4)
missing = 5 (2.4)
UI amount, n (%)
Small 86 (42.0) 77 (38.3) 8 (4)
Moderate 97 (47.3) 87 (43.3) 7 (3.5)
Large 22 (10.7) 17 (8.5) 5 (2.5)
missing = 3 (1.4) missing = 7 (3.4)
UI impact on daily life mean ± SD (scale 0–10) 5.6 (2.7) 5.5 (2.7) 6.6 (2.9)
missing = 28 (13.5) missing = 31 (14.9)
ICIQ-UI SF severity sumscore mean ± SD (score 0–21) 12.6 (3.9) 12.5 (3.8) 13.8 (4.9)
missing = 30 (14.4) missing = 33 (15.9)
UI type , n (%)
SUI 84 (40.4) 75 (36.9) 5 (2.5)
UUI 29 (13.9) 25 (12.3) 4 (2)
MUI 63 (30.3) 63 (31) 0
Other ⁄ unknown 32 (15.4) 20 (9.9) 11 (5.4)
missing = 5 (2.4)
General health, n (%)
(very) good 81 (39.5) 72 (36) 7 (3.5)
Moderate 89 (43.4) 79 (39.5) 8 (4)
(very) bad 35 (17.1) 29 (14.5) 5 (2.5)
missing = 3 (1.4) missing = 8 (3.8)
Visited the GP in the past 12 months, n (%) 147 (70.7) 130 (90.3) 14 (9.7)
missing = 3 (2)
UI, urinary incontinence; ICIQ-UI SF, International Consultation on Incontinence Questionnaire-Short Form; SUI, stress urinary inconti-
nence; UUI, urgency urinary incontinence; MUI, mixed urinary incontinence; GP, general practitioner.
Because of rounding off, the (valid) % differs from 100%.
*Student’s t-test, p = 0.047.
Conform ICIQ-UI Short Form (14).
Table 2 Received type of care from GP as reported by UI pad users who visited their GP at least once during the past
year
Received type of care reported by UI patients Freq 147 % 100
Only pads 74 50.3
Pads plus advice on BT or PFMT from GP (verbally, during vaginal examination only and ⁄ or by means 23 15.6
of a bladder diary)
Pads plus referral to physical therapist (some combined with advice ⁄ information from GP) 16 10.9
Pads plus referral to medical specialist (some combined with advice ⁄ information from GP) 13 8.8
Pads plus referral both to PT and to medical specialist (some combined with advice ⁄ information from GP) 7 4.8
Pads plus only medication (9) and pessary (1) 10 6.8
Pads plus other (unknown) 4 2.7
BT, bladder training; PFMT, pelvic floor muscle training; GP, general practitioner; PT, physical therapist.
Because of rounding off, the (valid) % differs from 100%.
ª 2008 The Authors
Journal compilation ª 2008 Blackwell Publishing Ltd Int J Clin Pract, March 2008, 62, 3, 508–515
512 Perceptions of urinary incontinence patients
Table 3 Satisfaction of patients with ‘personal attention’ and ‘information and advice’ on UI given by the GP during consultation on found
correlations (n = 147)
Scale mean (SD) Factor loadings
1 = do not in Obliquely
agree at all rotated Principal
Response 5 = completely Component
Personal attention: ‘Regarding UI: n (%) agree Analysis
...GP offered help quickly’ 110 (75) 4.27 (1.6) 0.980 0.163
...GP offered good help’ 98 (67) 4.26 (1.2) 0.915 0.027
...GP was interested in my case’ 114 (78) 4.33 (1.1) 0.896 0.064
...GP listened well’ 114 (78) 4.35 (1.1) 0.862 0.070
...GP had enough time for me’ 126 (86) 4.21 (1.2) 0.796 0.178
...GP advised me so I felt well enough to do my regular daily activities’ 98 (67) 4.11 (1.3) 0.770 0.155
Overall scale attention [missing 32 (21.7)] 115 (78.2) 4.31 (1.03) Cronbach’s a = 0.96
Advice and information: ‘Regarding UI:
...GP explained the purpose of tests and treatment’ 94 (64) 3.41 (1.5) 0.145 1.029
...GP helped me to see the importance of following his ⁄ her advice’ 94 (64) 3.66 (1.4) 0.014 0.948
...GP prepared me for what to expect from treatment or referral’ 63 (43) 3.51 (1.4) 0.013 0.965
...GP told me what I wanted to know on UI 97 (66) 3.79 (1.4) 0.072 0.871
...GP did involve me in decisions about medical care’ 96 (65) 3.89 (1.4) 0.208 0.709
...GP offered suggestions for prevention (e.g. advice on BT, PFMT and lifestyle)’ 96 (65) 3.75 (1.4) 0.272 0.631
Overall scale information [missing 55 (37.4)] 92 (62.6) 3.69 (1.27) Cronbach’s a = 0.97
UI, urinary incontinence; GP, general practitioner; BT, bladder training; PFMT, pelvic floor muscle training.
Table 4 Final model (dummy) regression analysis results using the patient’s ‘evaluation of the personal attention’ as a
‘dependent’ variable. Variance explained 0.220; list-wise deletion of missing cases (n = 87)
Unstandardised Standardised
coefficients coefficients
Final model Predictors B Std. Error Beta t p-value
Constant 3.402 0.652 5.220 < 0.001
Age (years) 0.023 0.009 0.261 2.454 0.016
General health (1–3) )0.335 0.162 )0.213 )2.076 0.041
Type UI dummies UUI vs. SUI )0.974 0.349 )0.313 )2.792 0.007
MUI vs. SUI )0.331 0.237 )0.145 )1.394 0.167
GP care dummies Advice GP vs. pads 0.246 0.299 0.088 0.824 0.413
Therapy GP vs. pads 0.155 0.440 0.038 0.354 0.725
Referral vs. pads 0.630 0.248 0.279 2.546 0.013
UI, urinary incontinence; SUI, stress urinary incontinence; UUI, urgency urinary incontinence; MUI, mixed urinary incontinence; GP, gen-
eral practitioner; PT, physical therapist. Scale values of ‘personal attention’ lie between 1 = low evaluation and 5 = high evaluation.
The three ‘GP care’ dummy variables (having 0–1 scores) contrast GP advice, -therapy ánd referral to other caregivers (PT, specialist)
with only pads (zero-score control group); the two ‘type of UI’ dummy variables (0–1) contrast ‘UUI’ and ‘MUI’ with ‘SUI’ (zero-score
control group). General health evaluation is a trichotomy with categories 1 = (very) good, 2 = moderate, 3 = (very) bad. A positive
coefficient indicates a higher evaluation of the ‘personal attention’, a negative a lower one.
p < 0.001), and UUI patients seem referred more patient gender and age, general health perception,
often than SUI patients (r = 0.16, p = 0.040). type of UI and the type of care received (Table 5).
Using the scale ‘evaluation of the information and Women, younger people and the less healthy people
advice the GP has given concerning the UI problem’ are less satisfied with the advice and information
as a dependent variable the final (dummy) regression they received (respectively p = 0.023, p = 0.006 and
model includes five statistically significant predictors: p = 0.049). Patients who have been referred and
ª 2008 The Authors
Journal compilation ª 2008 Blackwell Publishing Ltd Int J Clin Pract, March 2008, 62, 3, 508–515
Perceptions of urinary incontinence patients 513
Table 5 Final model (dummy) regression analysis results using the patient’s evaluation of the ‘information and advice’
as a ‘dependent’ variable. Variance explained 0.376; list-wise deletion of missing cases (n = 70)
Unstandardised Standardised
coefficients coefficients
Final model Predictors B Std. Error Beta t p-value
Constant 2.017 0.799 2.525 0.014
Age (years) 0.032 0.011 0.314 2.865 0.006
Gender(# vs. $) 1.297 0.554 0.261 2.341 0.023
General health (1–3) )0.407 0.202 )0.212 )2.012 0.049
GP care Advice GP vs. pads 0.671 0.359 0.203 1.867 0.067
Therapy GP vs. pads 0.365 0.675 0.058 0.541 0.591
Referral vs. pads 1.145 0.330 0.397 3.473 0.001
Type UI UUI vs. SUI )1.473 0.479 )0.384 )3.075 0.003
MUI vs. SUI )0.102 0.301 )0.037 )0.340 0.735
Legends and for dummies description, see Table 4.
Scale values of ‘information and advice’ lie between 1 = low evaluation and 5 = high evaluation. Gender is categorised as # = 2 and
$ = 1. A positive coefficient indicates a higher evaluation of the ‘information and advice’, a negative a lower one.
patients with SUI are more satisfied about advice or the medical specialist. This level of ‘any conser-
and information from the GP (p = 0.001 and 0.003 vative treatment besides pads’ is higher than that
respectively). found in the PURE study within Germany, Spain
or UK ⁄ Ireland (respectively 32%, 20% and 45%)
(17). Our referral rate (25%) and the prescription
Discussion
of medications for UI (11%) is higher than Dutch
Main results data of new patients with UI in primary care of
To our knowledge, this is the first study, where UI 12% and 9.8% respectively [Unpublished data from
patients, who recently got their first prescription for the Second Dutch National Survey 28 ⁄ 08 ⁄ 2007].
pads, have reported in detail on their experiences This might be explained by the fact that we only
with GP care. First, our study reveals that one of selected pad users who might have more severe
three UI patients had admittedly no direct contact and complex UI. Prescription of medication is very
with their GP for their pad prescription. This obvi- low compared with data of the PURE study from
ously indicates that pads are prescribed through a Germany, Spain and UK ⁄ Ireland (41%, 25% and
practice nurse ⁄ GP assistant as a delegated task. It 39%). Medication, in addition to lifestyle advices,
also surmises that, once pads are prescribed, effects BT and PFMT, especially in patients with UUI and
of advices on treatments like BT and ⁄ or PFMT and MUI for the UUI component, can be used to opti-
pad use are not monitored by the GP over time as mise treatment effect. Nevertheless, Dutch GPs
advised in guidelines (13). appear to be reluctant in the prescription of medi-
Second, over half of the UI patients who visited cation, which is in agreement with guidelines.
their GP said they only got pads. It seems obvious Third and finally, we found that one of four UI
that these patients either received no adequate patients is not satisfied with the information and
diagnostics and treatment aimed on cure or pre- advice on UI received from their GP, particularly in
vention as recommended as initial management in younger patients, women, self-proclaimed less
guidelines or they could not remember any healthy patients and patients with UUI. The satisfac-
attempts of this from their GP (1–3). These find- tion rate on information and advice is low compared
ings confirm the self-reported results on GP man- with primary care studies where in general 80–90%
agement in the same parts of the Netherlands at of patients is satisfied with issues on information
the same period in a separate study (6). Our study received during consultation (18). One explanation
also supports the impression that the compliance might be that half of the respondents only got pads
of GPs with the diagnostic advices might be from their GP and in general being given more
doubtful. The other half of UI patients either got information tends to correlate with higher satisfac-
‘treatment’ by their GP or were referred to the PT tion levels.
ª 2008 The Authors
Journal compilation ª 2008 Blackwell Publishing Ltd Int J Clin Pract, March 2008, 62, 3, 508–515
514 Perceptions of urinary incontinence patients
Strengths and limitations of the study prescribed. This way the possibility that results from
Before drawing any conclusions on the basis of our respondents differ in a meaningful way from non-
findings the following needs to be considered. The respondents, thus biasing results, seems not plausible
183 women in our sample appear to be similar on (19).
age and urbanisation with the 778 Dutch women in
the PURE study (11). Practical consequences
Although our data on distribution for type of UI Our findings confirm the impression that too many
may be somewhat biased, as we only could classify UI patients only receive pads without adequate
163 women because of missing scores on items diagnostics and treatment by their GP as recom-
needed to classify patients, distribution is rather mended in clinical practice guidelines on UI (13).
consistent with those from epidemiological literature A large number of UI patients may receive subopti-
(2,3). Patients in our study reported more frequent mal care and because of life-long use of pads this
and more severe UI than the population in the will lead to often unnecessary high costs of inconti-
PURE study. This seems logical as the PURE study nence pads as no cure or improvement is aimed
included all UI patients in primary care and not for. Our findings confirm results of reviews on the
only pad users (11). We were especially interested use of UI guidelines in several European countries.
in patients who were still using pads or were pre- There is a potential need for local initiatives that
scribed pads and generally this would indicate a take into account patient perceptions to implement
group that is still incontinent and likely did not guidelines and to improve quality of care for UI
receive adequate therapy. This is an inherent bias of patients (6,8,20,21). In line with other chronic dis-
the study design. eases, adequate UI management by the GP requires
Increase of prevalence of UI in men over 80 might more time than GPs have available for patient care
explain the few male respondents in our study (1). overall. This is especially true in case of more com-
Most studies have a large fraction of other ⁄ unclassi- plex problems, such as severe SUI, UUI and MUI,
fied types UI in men (2). or concurrent co-morbidities. Therefore, further
One of the potential limitations of this study is research should focus on solutions how to support
that it relies on self-reported retrospective data GPs to meet recommended standards for quality of
instead of medical records. Consequently, there is a care for UI. One of the solutions might be multi-
chance of recall bias where patients report inaccurate disciplinary guidelines as developed by a team of
or incomplete information on care provided by the Dutch GPs and physiotherapists, e.g. ‘National Mul-
GP during the past 12 months prior to this study. tidisciplinary Agreement’ (LESA) (22). Next to this,
Next to this, we did not ask patients for reasons why educating the physicians, with the inclusion of
they did or did not get their therapies in this study. guidelines in the medical syllabus, at an early stage
It is possible that patients refused any prospect of a in their training, may help raise awareness of valu-
referral or a prescription for medication and only able tools and could also make a worthwhile impact
wanted a pad. In two Dutch studies, GPs mention (21). Another solution might be alternative methods
that patient motivation played a role in working of service delivery, such as a substitution of tasks
according to guidelines on UI (5,6). on treatment of UI patients in primary care by con-
Moreover, the data might be biased by missing tinence nurses, specially trained in line with the
respondents, whose reasons not to participate are success of other specialised nurses. First experiments
mostly various (8). As the study is cross-sectional, with this kind of intervention for UI patients seem
we cannot test for causal relationships, but we can to be promising, but more research is needed (23).
only examine statistical associations. Earlier studies have revealed that one of four people
Finally, we analysed 208 questionnaires which with UI do not seek medical help (13). Availability
means a crude response rate of 24%. This seems low and accessibility of an intervention by specialised
compared with response rates for patients’ surveys continence nurses might also lower the threshold
with a mean response rate of 60% (standard devia- for patients to seek help.
tion 21%) (19). One explanation might be that Moreover, many countries are setting up integrated
besides an explanatory letter with standard informa- continence care services to improve the process of
tion which accompanied the questionnaire, no referral between primary and secondary care and to
reminders or any incentives were used. Nonetheless, offer opportunities to stay up to date with important
the respondents showed to be representative (age, new developments in the management of bladder
gender, urbanisation, type and severity of UI) for problems for all allied healthcare professionals
Dutch patients in primary care who got pads (20,21,24).
ª 2008 The Authors
Journal compilation ª 2008 Blackwell Publishing Ltd Int J Clin Pract, March 2008, 62, 3, 508–515
Perceptions of urinary incontinence patients 515
Conclusion family doctors. A cross-sectional study. J Eval Clin Pract 2007; ‘in
press’.
Dutch UI patients using pads on prescription experi- 7 Hu T-W, Wagner TH. Health-related consequences of overactive
bladder: an economic perspective. BJU Int 2005; 96: 43–5.
ence suboptimal GP care and management. Consid-
8 Coulter A. Can patients assess the quality of health care? BMJ
ering that adequate GP UI management is time 2006; 333: 1–2.
consuming, especially in case of more complex prob- 9 Monz B, Pons M, Hampel C et al. Patient-reported impact of uri-
lems, such as severe SUI, UUI and MUI, or concur- nary incontinence – Results from treatment seeking women in 14
European countries. Maturitas 2005; 30 (Suppl. 2): 24–34.
rent co-morbidities, further research should focus on 10 Teunissen TAM, Weel van C, Lagro-Janssen ALM. Urinary incon-
effective primary care interventions to support GPs tinence in older people living in the community examining help-
and on solutions to tackle major barriers and to seeking behaviour. Br J Gen Pract 2005; 55: 776–82.
introduce facilitators. Factors identified through 11 Sykes D, Castro R, Pons ME et al.. Characteristics of female outpa-
tients with urinary incontinence participating in a 6-month obser-
patient feedback should be used to improve quality vational study in 14 European countries. Maturitas 2005; 52
of care for UI in primary care. (Suppl. 2):13–23.
12 Wensing M, Mainz J, Grol R. Standardised instrument for patient
evaluations of general practice care in Europe. Eur J Gen Pract
Acknowledgements 2000; 6: 82–7.
13 Lagro-Janssen ALM, Teunissen D, Breedveldt-Boer HP et al..
This work was supported in part by an unrestricted NHG-Standaard Incontinentie voor Urine M46 Eerste herziening
Grant of Pfizer. (Dutch College Guideline on Urinary Incontinence. First revision).
Nederlands Tijdschrift voor Urologie 2006; 49: 501–10.
The authors thank pharmacists, MediReva V.O.F.
14 Avery K, Donovan J, Peters T et al. ICI-Q: a brief and robust mea-
Maastricht and Azivo, The Hague for support and sure for evaluating the symptoms and impact of urinary inconti-
distributing the questionnaires. We thank Wendy nence. Neurourol Urodyn 2004; 23: 322–30.
Engering and Huub Verheyden for data entry and 15 Burstrom B, Fredlund P. Self rated health: Is it as good a pre-
dictor of subsequent mortality among adults in lower as well as
patients for participating in the survey.
in higher social classes? J Epidemiol Community Health 2001; 55:
836–40.
16 Abrams P, Cardozo L, Fall M et al. The standardisation of termi-
Author contributions nology of lower urinary tract function: Report from the Standardi-
sation Sub-committee of the International Continence Society.
P.A.H., B.B., T.L.J., R.W. participated in the con- Neurourol Urodyn 2002; 21: 167–78.
cept ⁄ design of the survey. F.N. was especially helpful 17 Papanicolaou S, Pons ME, Hampel C et al. Medical resource utilisa-
in statistical analysis ⁄ interpretation of the study. All tion and cost of care for women seeking treatment for urinary
authors have made substantial contributions to: (1) incontinence in an outpatient setting. Examples from three countries
participating in the PURE study. Maturitas 2005; 52 (Suppl. 2):
analysis and interpretation of data, (2) drafting the S35–47.
article or revising it critically for important intellec- 18 Grol R, Wensing M, Mainz J et al. Patients in Europe evaluate
tual content and (3) have approved the final version general practice care: an international comparison. Br J Gen Pract
2000; 50: 882–7.
of the manuscript.
19 Asch D, Jedrziewski M, Christakis N. Response rates to mail sur-
veys published in medical journals. J Clin Epidemiol 1997; 50:
1129–36.
References 20 Kirby M. Managing stress urinary incontinence – a primary care
1 Teunissen TA, van den Bosch WJH, van den Hoogen HJ, issue. Int J Clin Pract 2006; 60: 184–9.
Lagro-Janssen AL. Prevalence of urinary, fecal and double inconti- 21 Kirby M, Artibani W, Cardozo L et al. Overactive bladder: the
nence in the elderly living at home. Int Urogynecol J 2004; 15: 10–3. importance of new guidance. Int J Clin Pract 2006; 60: 1263–71.
2 Abrams P, Cardozo L, Khoury S, Wein A. Incontinence. 3rd Inter- 22 Faber E, Custers JWH, Berghmans LCM et al. Landelijke Eerstelijns
national Consultation. Monaco: Health Publication Ltd, 2005. Samenwerkings Afspraak Incontinentie voor Urine (National First
3 Norton P, Brubaker L. Urinary incontinence in women. Lancet Line Multidisciplinary Agreement) ‘LESA’. Huisarts Wet 2007; 50:
2006; 367: 57–67. S9–12.
4 O’Donnell M, Viktrup L, Hunskaar S. The role of general practi- 23 Du Moulin MFMT, Hamers JPH, Paulus A et al.. The role of the
tioners in the initial management of women with urinary inconti- nurse in community continence care: a systematic review. Int
nence in France, Germany, Spain and the UK. Eur J Gen Pract J Nurs Stud 2005; 42: 479–92.
2007; 13: 20–6. 24 Monz B, Hampel C, Porkess S et al. A description of health care
5 Teunissen D, van den Bosch W, van Weel C, Lagro-Janssen T. Uri- provision and access to treatment for women with urinary inconti-
nary incontinence in the elderly: attitudes and experiences of gen- nence in Europe: a five-country comparison. Maturitas 2005; 52
eral practitioners. A focus group study. Scand J Prim Health Care (Suppl. 2): S3–12.
2006; 24: 56–61.
6 Albers-Heitner P, Berghmans B, Nieman F et al. Adherence to
professional guidelines for patients with urinary incontinence by Paper received October 2007, accepted December 2007
ª 2008 The Authors
Journal compilation ª 2008 Blackwell Publishing Ltd Int J Clin Pract, March 2008, 62, 3, 508–515
You might also like
- Medical Billing TerminologyDocument49 pagesMedical Billing TerminologyBhuvana Bala100% (4)
- Chronic Pain Management ChartsDocument2 pagesChronic Pain Management Chartslrpokhrel100% (3)
- Scaffolding-Cop-2021 Code of PracticeDocument77 pagesScaffolding-Cop-2021 Code of PracticeArdamitNo ratings yet
- Ambulatory CareDocument26 pagesAmbulatory CareRain Collins0% (1)
- Ambulatory CareDocument24 pagesAmbulatory CareAru VermaNo ratings yet
- 2019 Monitoreo Hemodinamico PDFDocument476 pages2019 Monitoreo Hemodinamico PDFCurro MirallesNo ratings yet
- Calculation of DosesDocument12 pagesCalculation of DosesFranklin Jayoma ManaoNo ratings yet
- 3.levels of Health CareDocument43 pages3.levels of Health CareNamrah AfzalNo ratings yet
- BDLS 3 2 IntroduDocument18 pagesBDLS 3 2 IntroduAhmad Althof Malihul Adi100% (2)
- Introduction of Community MedicineDocument111 pagesIntroduction of Community MedicineSanjeet SahNo ratings yet
- Knowledge and Practice Towards Care and MaintenancDocument7 pagesKnowledge and Practice Towards Care and MaintenancyunishaNo ratings yet
- Adime Note GDMDocument2 pagesAdime Note GDMapi-242547654100% (1)
- Trends and Issues in MSNDocument26 pagesTrends and Issues in MSNAmmineni Syam Prasad100% (7)
- BMC Health Services ResearchDocument7 pagesBMC Health Services ResearchmartingomezrNo ratings yet
- Chinese Perspective of The Role of Primary Care in Cancer Control PDFDocument2 pagesChinese Perspective of The Role of Primary Care in Cancer Control PDFANGIE MARIANA AGUDELO GILNo ratings yet
- Penny - CNS Lecture - 13 Sept 2017Document69 pagesPenny - CNS Lecture - 13 Sept 2017hkdawnwongNo ratings yet
- 7 PubmedDocument12 pages7 PubmedNydia Isabel Ruiz AntonioNo ratings yet
- Nonurgent Patients in The Emergency Department? A French Formula To Prevent MisuseDocument6 pagesNonurgent Patients in The Emergency Department? A French Formula To Prevent MisuseLizbeth HernandezNo ratings yet
- EWMA - HomeCare - WoundCare - May2014 PDFDocument44 pagesEWMA - HomeCare - WoundCare - May2014 PDFMuhYaminNo ratings yet
- Ambulatory CareDocument24 pagesAmbulatory CareAru Verma100% (1)
- 3 Telemedicine For PatientsDocument18 pages3 Telemedicine For PatientsRonald Rey MenorNo ratings yet
- 3 Telemedicine For PatientsDocument18 pages3 Telemedicine For PatientsRonald Rey MenorNo ratings yet
- Chronic Disease Management and Remote Patient Monitoring: Research - Debate - Policy - NewsDocument52 pagesChronic Disease Management and Remote Patient Monitoring: Research - Debate - Policy - NewsAlejandro CardonaNo ratings yet
- IT-supported Integrated Care Pathways For Diabetes: A Compilation and Review of Good PracticesDocument15 pagesIT-supported Integrated Care Pathways For Diabetes: A Compilation and Review of Good PracticesKenny BellodasNo ratings yet
- s13224 020 01346 0Document4 pagess13224 020 01346 0priyanka mishraNo ratings yet
- Using ICT in SchoolDocument5 pagesUsing ICT in Schoolsiti syuhada binti zainalNo ratings yet
- Surving Sepsis Campaign ResultDocument8 pagesSurving Sepsis Campaign Resultmaria arenas de itaNo ratings yet
- Personalized Specialty Care: Value-Based Healthcare Frontrunners from the NetherlandsFrom EverandPersonalized Specialty Care: Value-Based Healthcare Frontrunners from the NetherlandsNico van WeertNo ratings yet
- End of Life Care DissertationDocument8 pagesEnd of Life Care DissertationCustomCollegePapersMadison100% (1)
- 1307 ArticleText 4207 2 10 20200904 PDFDocument5 pages1307 ArticleText 4207 2 10 20200904 PDFahmedbilalakhtar20No ratings yet
- Patient Satisfaction and Associated Factors Among Ad - 2021 - International JourDocument6 pagesPatient Satisfaction and Associated Factors Among Ad - 2021 - International JourRonald QuezadaNo ratings yet
- Toward An Ultrasound Curriculum For Critical Care Medicine PDFDocument15 pagesToward An Ultrasound Curriculum For Critical Care Medicine PDFBasilia CahuichNo ratings yet
- Primary Care ClinicDocument4 pagesPrimary Care ClinicKyla VillamorNo ratings yet
- Pressure UlcerDocument5 pagesPressure Ulcerifi medanNo ratings yet
- Special Issue 1 3Document129 pagesSpecial Issue 1 3Amit PasiNo ratings yet
- Raynak 2020Document17 pagesRaynak 2020javier rosales ortegaNo ratings yet
- The Perception and Knowledge About Episiotomy: A Cross-Sectional Survey Involving Healthcare Workers in A Low-And Middle-Income CountryDocument6 pagesThe Perception and Knowledge About Episiotomy: A Cross-Sectional Survey Involving Healthcare Workers in A Low-And Middle-Income Countrydior00No ratings yet
- Strategies Adapted For Patient-Oriented Care and Satisfaction During TheDocument7 pagesStrategies Adapted For Patient-Oriented Care and Satisfaction During TheRagni MishraNo ratings yet
- Compiled Chapters 1 41Document92 pagesCompiled Chapters 1 41K4 Printing ServicesNo ratings yet
- Endometriosis Care in Wales1Document81 pagesEndometriosis Care in Wales1Mary De la HozNo ratings yet
- International Archives of Nursing and Health Care Ianhc 1 007Document6 pagesInternational Archives of Nursing and Health Care Ianhc 1 007hawaniniNo ratings yet
- Now or Never - Patient LeafletDocument6 pagesNow or Never - Patient LeafletSandeep_Bellap_5543No ratings yet
- Journal HyponatremiaDocument39 pagesJournal HyponatremiadharmaNo ratings yet
- Continuity Care....... : Wahyudi Istiono Departemen Kedokteran Keluarga Dan Komunitas FK UGMDocument127 pagesContinuity Care....... : Wahyudi Istiono Departemen Kedokteran Keluarga Dan Komunitas FK UGMJony SaputraNo ratings yet
- Introduction:-: Ambulatory Healthcare Organizations IntroducedDocument7 pagesIntroduction:-: Ambulatory Healthcare Organizations Introducedanimesh pandaNo ratings yet
- The Importance of A Geriatric Approach in MedicineDocument5 pagesThe Importance of A Geriatric Approach in MedicineSiena KaleiNo ratings yet
- 1 s2.0 S0197457220300550 MainDocument5 pages1 s2.0 S0197457220300550 Mainruby susmawatiNo ratings yet
- Fenice StudyDocument9 pagesFenice StudyIrvan TanpomasNo ratings yet
- Comprehensive Geriatric Assessment For Older AdultsDocument3 pagesComprehensive Geriatric Assessment For Older Adultsdasty brownNo ratings yet
- 1999 Landi Italy Impact of Integrated Home Care Services On Hospital UseDocument5 pages1999 Landi Italy Impact of Integrated Home Care Services On Hospital UseJackson TakahashiNo ratings yet
- Comisión LancetDocument66 pagesComisión LancetKaya CromoNo ratings yet
- Trends & Issue MSNDocument47 pagesTrends & Issue MSNgemergencycareNo ratings yet
- Investigating The Preferences of Older People For Telehealth As A New Model of Health Care Service Delivery: A Discrete Choice ExperimentDocument13 pagesInvestigating The Preferences of Older People For Telehealth As A New Model of Health Care Service Delivery: A Discrete Choice Experimenttherese BNo ratings yet
- Training and Professional Development For Nurses and Healthcare Support Workers: Supporting Foundation For Quality and Good Practice For Care of The Acutely III Older PersonDocument7 pagesTraining and Professional Development For Nurses and Healthcare Support Workers: Supporting Foundation For Quality and Good Practice For Care of The Acutely III Older PersonAdnan QamarNo ratings yet
- Maurer Et Al., CURICT1 Usage, Qual. Relevance UCARE, WAOJ 2020Document14 pagesMaurer Et Al., CURICT1 Usage, Qual. Relevance UCARE, WAOJ 2020frecamaguNo ratings yet
- 5-Telemedicine Guidance On Navigating Ethical and Legal ImplicationsDocument13 pages5-Telemedicine Guidance On Navigating Ethical and Legal ImplicationsRonald Rey MenorNo ratings yet
- Current Trends in Community NursingDocument9 pagesCurrent Trends in Community Nursingnavasree nimmiNo ratings yet
- Effects of Home-Based Chronic Wound Care TrainingDocument19 pagesEffects of Home-Based Chronic Wound Care TrainingNathaniel PulidoNo ratings yet
- Nurses Knowledge, Attitudes and Practices Towards Prevention of Pressure Ulcers at Kilimanjaro Christian Medical CenterDocument8 pagesNurses Knowledge, Attitudes and Practices Towards Prevention of Pressure Ulcers at Kilimanjaro Christian Medical CenterInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Needle Stick and Sharp Injuries and Associated Factors Among Nurses Workingin Jimma University Specialized Hospital South West Ethiopia 2167 1168 1000291Document8 pagesNeedle Stick and Sharp Injuries and Associated Factors Among Nurses Workingin Jimma University Specialized Hospital South West Ethiopia 2167 1168 1000291MrLarry DolorNo ratings yet
- APPG Patient Empowerment ReportDocument36 pagesAPPG Patient Empowerment ReportkiranNo ratings yet
- 388-Article Text-1059-1-10-20200112Document3 pages388-Article Text-1059-1-10-20200112Nurhaliza AnjliNo ratings yet
- Group - Four - Project-ProposalDocument37 pagesGroup - Four - Project-ProposalTahir m. AbdelaNo ratings yet
- European Journal of Oncology Nursing: A B C D A B e F G A B H FDocument10 pagesEuropean Journal of Oncology Nursing: A B C D A B e F G A B H FBety RindaNo ratings yet
- Lit ReviewDocument8 pagesLit Reviewapi-314668605No ratings yet
- Are We Making The Most of SupplementsDocument3 pagesAre We Making The Most of SupplementsEmmanuel SánchezNo ratings yet
- CHN 104Document1 pageCHN 104May MayNo ratings yet
- Principles of Nutrition - UADocument3 pagesPrinciples of Nutrition - UABiggiePiggie12345No ratings yet
- Clinical Veterinary Advisor Dogs and Cats by Etienne Cote DVMDACVIMCardiology and Small Animal Internal Medicine - 5 Star ReviewDocument2 pagesClinical Veterinary Advisor Dogs and Cats by Etienne Cote DVMDACVIMCardiology and Small Animal Internal Medicine - 5 Star ReviewMirsad Gilic0% (1)
- Study Finished NewDocument63 pagesStudy Finished NewMilanNo ratings yet
- Interpreting For ChildrenDocument16 pagesInterpreting For ChildrenIușan MihaelaNo ratings yet
- Autism Spectrum Disorders: A Booklet For Parents and CarersDocument40 pagesAutism Spectrum Disorders: A Booklet For Parents and CarersAndreea SanduNo ratings yet
- Topics For Skills Laboratory N - 104 Community Health Nursing 1Document2 pagesTopics For Skills Laboratory N - 104 Community Health Nursing 1Bem PladeroNo ratings yet
- Group1 Week8298Document54 pagesGroup1 Week8298ABEGAIL BALLORANNo ratings yet
- People As Resource Class 9 NotesDocument6 pagesPeople As Resource Class 9 Notessidd230100% (2)
- CAP ADHD Form PDFDocument1 pageCAP ADHD Form PDFrohailNo ratings yet
- Medical Insurance PolicyDocument47 pagesMedical Insurance PolicyTaimoorNo ratings yet
- Nejmoa 1804092Document11 pagesNejmoa 1804092Daniel GuérinNo ratings yet
- 2021 All JCs Prelim Paper 1Document4 pages2021 All JCs Prelim Paper 1qiyunNo ratings yet
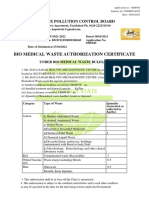
- Bio Medical Waste Authorization Certificate: Haryana State Pollution Control BoardDocument3 pagesBio Medical Waste Authorization Certificate: Haryana State Pollution Control BoardManishNo ratings yet
- Katherine E. Stickels: ObjectivesDocument4 pagesKatherine E. Stickels: Objectivesapi-358969355No ratings yet
- 2011 Wingspread Forum ReportDocument74 pages2011 Wingspread Forum ReportCenterForCitizenDiplomacyNo ratings yet
- Peritonsillar AbscessDocument2 pagesPeritonsillar AbscessKevin Leo Lucero AragonesNo ratings yet
- DLP 4demo 1st QR Respiratory System Grade 9Document6 pagesDLP 4demo 1st QR Respiratory System Grade 9Janiko Jethro Abang IbrahimNo ratings yet
- Alcohol ResearcDocument85 pagesAlcohol ResearcEmmanuel de LeonNo ratings yet
- English For Academic and Professional Purposes: Quarter 2 - Module 8Document35 pagesEnglish For Academic and Professional Purposes: Quarter 2 - Module 8Unick Soriano NastorNo ratings yet
- Carmarthen in SpotlightDocument1 pageCarmarthen in SpotlightDigital MediaNo ratings yet
- 2011 Anglu K VBE PagrDocument16 pages2011 Anglu K VBE PagrTomas GuNo ratings yet