Professional Documents
Culture Documents
Clean Vs Sterile Dressing Techniques For.7
Clean Vs Sterile Dressing Techniques For.7
Uploaded by
Faozan FikriOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Clean Vs Sterile Dressing Techniques For.7
Clean Vs Sterile Dressing Techniques For.7
Uploaded by
Faozan FikriCopyright:
Available Formats
J Wound Ostomy Continence Nurs. 2012;39(2S):S30-S34.
Published by Lippincott Williams & Wilkins
Clean vs. Sterile Dressing
Techniques for Management
of Chronic Wounds
A Fact Sheet
Downloaded from http://journals.lww.com/jwocnonline by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3i3D0OdRyi7TvSFl4Cf3VC1y0abggQZXdtwnfKZBYtws= on 04/05/2022
Originated By: exist. Terms have been used interchangeably and all are
Wound, Ostomy and Continence Nurses Society (WOCN) subject to individual interpretation. The following defini-
Wound Committee and the Association for Professionals tions provide a point of reference for the terms used in
in Infection Control and Epidemiology, Inc. (APIC) 2000 this document.
Guidelines Committee Sterile technique. Sterile is generally defined as
Updated/Revised: WOCN Wound Committee, 2011 meaning free from microorganisms.3 Sterile technique in-
volves strategies used in patient care to reduce exposure to
Date Completed: microorganisms and maintain objects and areas as free
Original Publication Date: 2001 from microorganisms as possible. Sterile technique in-
Review/Update: 2005 volves meticulous hand washing, use of a sterile field, use
Revised: 2011 of sterile gloves for application of a sterile dressing, and
use of sterile instruments. “Sterile to sterile” rules involve
the use of only sterile instruments and materials in dress-
■ Purpose ing change procedures; and avoiding contact between
To present an update on the status of information about sterile instruments or materials and any non-sterile sur-
clean versus sterile dressing technique to manage chronic face or products. Sterile technique is considered most ap-
wounds. propriate in acute care hospital settings, for patients at
high risk for infection, and for certain procedures such as
sharp instrumental wound debridement.3-5
■ Background/History Clean technique. Clean means free of dirt, marks, or
This document originated in 2001 as a joint position state- stains.3 Clean technique involves strategies used in patient
ment from a collaborative effort of the Wound, Ostomy and care to reduce the overall number of microorganisms or to
Continence Nurses Society and the Association for prevent or reduce the risk of transmission of microorgan-
Professionals in Infection Control and Epidemiology, Inc.1,2 isms from one person to another or from one place to an-
Its purpose was to review the evidence about clean vs. ster- other. Clean technique involves meticulous handwashing,
ile technique and present approaches for chronic wound maintaining a clean environment by preparing a clean
care management. Then as now, areas of controversy exist field, using clean gloves and sterile instruments, and pre-
due to a lack of agreement on the definitions of “clean” and venting direct contamination of materials and supplies.
“sterile” technique, lack of consensus as to when each is No “sterile to sterile” rules apply. This technique may also
indicated in the management of chronic wounds, and lack be referred to as non-sterile. Clean technique is considered
of research to serve as a guide. Wound care practices are most appropriate for long-term care, home care, and some
extremely variable and are frequently based on rituals and clinic settings; for patients who are not at high risk for
traditions as opposed to a scientific foundation. infection; and for patients receiving routine dressings for
chronic wounds such as venous ulcers, or wounds healing
by secondary intention with granulation tissue.1-7
■ Discussion of Problems/Issue/Needs Aseptic technique. Asepsis or aseptic means free
Definition of terms from pathogenic microorganisms.3 Aseptic technique is
Clean versus sterile technique. Various definitions
and descriptions of dressing technique for wound care DOI: 10.1097/WON.0b013e3182478e06
S30 J WOCN ■ March/April 2012 Copyright © 2012 by the Wound, Ostomy and Continence Nurses Society
WON200342.indd S30 03/03/12 4:27 PM
J WOCN ■ Volume 39/Number 2S Clean vs. Sterile Dressing Techniques S31
the purposeful prevention of the transfer of organisms In patients who are immunosuppressed or have ischemic
from one person to another by keeping the microbe count wounds, signs of infection can be subtle. Signs of inflam-
to an irreducible minimum. Some authors have made a mation such as a faint halo of erythema and moderate
distinction between surgical asepsis or “sterile technique” amounts of drainage might be the only signs of an in-
used in surgery and medical asepsis or “clean technique” fected arterial wound.17 Studies have shown that in
that involves procedures to reduce the number and trans- chronic wounds, increasing pain, friable granulation tis-
mission of pathogens.4 sue, wound breakdown, and foul odor have high validity
No touch technique. No touch is a method of chang- for infection.17,18
ing surface dressings without directly touching the wound
or any surface that might come in contact with the wound. Definition of Wounds
Clean gloves are used along with sterile solution/supplies/ Wound. A wound is any break in the skin that can
dressings that are maintained as clean.8 vary from a superficial to a full thickness wound. A partial
Definition of infection. Infection has been defined thickness wound is confined to loss of the epidermis and
as a continuum from contamination, colonization, critical partial loss of the dermis; whereas a full thickness wound
colonization, biofilm, and infection.9 has a total loss of the epidermis and dermis and can in-
Contamination. Contamination is the presence of volve the deeper subcutaneous and muscle tissues and/or
non-replicating microorganisms on the surface of the bone.19,20
wound. All open wounds have some level of bacterial bur- Acute wound. Acute wounds occur suddenly and are
den that is ordinarily cleared by the host.9-11 commonly due to trauma or surgery, which triggers blood
Colonization. In colonization, microorganisms at- clotting and a wound repair process that leads to wound
tach to the wound surface and replicate but do not impair closure within 2-4 weeks.14,19
healing or cause signs and/or symptoms of infection. The Chronic wound. A chronic wound is a one that does
bacteria are not pathogenic and do not require treatment. not does not proceed through an orderly and timely repair
All chronic wounds are colonized to varying degrees.9 process requiring more than 4 weeks to heal such as vas-
Critical colonization. With critical colonization, cular wounds and pressure wounds.14,19
the organisms attach to the wound surface, replicate and Surgical wound. A surgical wound that heals in an
multiply to a level that affects skin cell proliferation and orderly and expected fashion may be considered an acute
tissue repair without provoking systemic signs of infec- wound. Surgical wounds heal by primary closure or are left
tion. There is no invasion of the healthy tissue at this open for delayed primary closure or healing by secondary
point.9 closure. Primary closure facilitates the fastest healing.
Biofilm. Approximately 70% of chronic wounds have However, infected wounds should not be primarily closed.21
biofilm.9 When organisms adhere to the wound surface,
they begin to develop biofilm, which is a complex system
of microorganisms embedded in an extracellular, polysac-
■ Gaps in Research Practice
charide matrix that protects from the invasion of other There is no definitive evidence that sterile technique is
organisms, phagocytosis, and many commonly used anti- superior to clean technique, improves outcomes, or is war-
biotics and antiseptics. Biofilms are difficult to treat and ranted when changing dressings on chronic wounds.8
eradicate.9 Recently it has been proposed that biofilm Insufficient evidence is available to determine if there are
might be present in all chronic wounds.12,13 significant differences in infection rates or healing when
Infection. Infection occurs when organisms on the wounds are treated using clean or sterile technique.14
wound surface invade the healthy tissue, reproduce, over- There is a lack of agreement in published expert opinion
whelm the host resistance, and create cellular injury lead- as to what constitutes sterile versus non-sterile technique
ing to local or systemic symptoms.9,14 Infection is often and when one or the other should be used.
described quantitatively as a bacterial count of greater
than 105 colony-forming units (CFU) per gram of tissue.9
However, some organisms such as beta-hemolytic strepto-
■ Overview of Research/Published
Expert Opinion
cocci impair wound healing at less than 105 CFU per gram
of tissue.15 According to Kravitz,16 infection should be de- Few national guidelines have addressed the topic of clean
fined as the presence of bacteria in any quantity that im- vs. sterile technique. Sterile technique and dressings have
pairs wound healing. been recommended for post-operative management of
Clinical signs of infection include lack of healing after wounds for 24-48 hours by the Centers for Disease Control
2 weeks of proper topical therapy, erythema, increase in and Prevention.22 No recommendations are provided be-
amount or change in character of exudate, odor, increased yond 48 hours for wounds with primary closure.22,23
local warmth, friable granulation tissue, edema or indura- In 1994, clinical practice guidelines for pressure ulcer
tion, pain or tenderness, fever, chills, elevated white blood treatment, published by the Agency for Health Care Policy
cell count, and elevated glucose in patients with diabetes.9 and Research, recommended use of clean gloves and clean
WON200342.indd S31 03/03/12 4:27 PM
S32 Clean vs. Sterile Dressing Techniques J WOCN ■ March/April 2012
dressings for pressure ulcers as long as the dressing proce- about the use of sterile vs. non-sterile gloves for wound
dures complied with the institution’s policies.24 Sterile care.31 The authors reported great variations in practice and
instruments were recommended for debridement. Recent that acute care nurses used sterile gloves for wound care
guidelines for pressure ulcers have not addressed specifics more commonly than home care nurses. In acute care, ster-
of clean or sterile technique other than to state that ile gloves were used more than non-sterile for packing
tap water or potable water can be used to clean pressure wounds, in cases of purulence or tunneling, or for open
ulcers and that sterile instruments are needed for sharp orthopedic wounds. Clean gloves were used for dressing
debridement.25 changes of intact surgical wounds and pressure ulcers. In
There is a paucity of research about clean vs. sterile home care, non-sterile gloves were commonly used except
technique for wound care and studies have varied greatly for open orthopedic wounds (i.e., exposed bone/tendon).
in their design and findings. Angeras, Brandberg, Falk, and Three factors that were identified as the most influential in
Seeman26 compared the use of sterile saline or tap water glove choice were type of wound, exposed bone, and im-
for cleaning acute traumatic soft tissue wounds and found munosuppression. Some of the other factors affecting glove
that the infection rate in the tap water group was 5.4% choice included type of dressing, type of drainage, time
compared to 10.3% in the group using sterile saline (p ⬍ .05) since surgery, licensure (i.e., registered nurse vs. licensed
with a 50% decrease in costs for the tap water group. vocational nurse), agency policy, physician preference, and
Two studies examined the strike through contamina- what they were taught in school.
tion in saturated sterile dressings. Alexander, Gannage, Lawson, Juliano, and Ratliff32 in a non-experimental,
Nichols, and Gaskins27 reported that when gauze sponges longitudinal study monitored infection rates and supply
were saturated directly in their wrapper, that contamina- costs of all patients with open surgical wounds healing by
tion occurred in 100% of sponges in uncoated wrappers. secondary intention before and 3 months after imple-
In the coated wrapped sponges, 80% exposed to menting non-sterile wound care. There was no statistically
Staphylococcus epidermidis and 20% exposed to significant difference in infection rates. Dressing costs and
Escherichia coli had strike through. In another study, cul- time to perform the wound care were reduced using non-
tures were taken from gauze sponges that were saturated sterile dressing techniques (i.e., staff did not use sterile
directly on their wrappers on hospital over-bed tables of gloves, scissors, or bowls).
postoperative surgical patients.28 The saturated gauze In 2006, Fellows and Crestodina reported that the op-
showed significant growth of microorganisms. The au- timal cleansing agent for wound cleaning should be ster-
thors reported there was no significant difference in strike- ile, noncytotoxic, and inexpensive.33 Because of the cost
through contamination in gauze saturated on coated or of sterile saline and reluctance of patients to discard un-
uncoated wrappers. Investigators in both these studies used solutions, Fellows and Crestodina conducted a small,
concluded that the practice of saturating gauze sponges on quasi-experimental study in a home health setting to
their wrappers was unacceptable. compare the bacterial content of home prepared saline
In 1993, Stotts and colleagues conducted a descriptive, made with distilled water and stored at room temperature
exploratory survey of members of WOCN to obtain infor- (2 gallons) to saline stored in a refrigerator (2 gallons).
mation regarding wound care practices in the United Based on cultures of the solutions immediately following
States.29 Two hundred and forty-two (242) members re- preparation and at weekly intervals for 4 weeks, the au-
sponded to the survey. Of the respondents, 51.4% reported thors concluded that saline solution prepared by patients
use of sterile technique and 43% reported use of non-ster- by adding table salt to distilled water (purchased from a
ile technique. Sterile technique was performed more fre- grocery store) remained bacteria free for a month if refrig-
quently in acute care than in other settings. It was also erated. The saline kept at room temperature had undesir-
reported that 90% of patients with open wounds being able levels of bacteria after 2 weeks. The authors
discharged from hospitals were taught to perform non- recommended further studies to confirm their findings.
sterile technique at home regardless of whether clean or An integrative literature review of seven published
sterile technique was used during hospitalization. studies of clean and sterile technique for dressings re-
In 1997, Stotts and colleagues compared the healing vealed that while there is a lack of consensus about the
rates and costs of sterile vs. clean technique in post-oper- benefit of clean versus sterile technique to improve heal-
ative patients (N ⫽ 30) who had wounds healing by sec- ing or infection rates, clean technique results in lower
ondary intentions following gastrointestinal surgery.30 costs.5
The authors reported there was no statistically significant
difference in the rate of wound healing between the two
groups (p ⬍ 0.55). The cost however was significantly
■ Conclusions
higher with sterile technique (p ⬍ .05) compared with There is not a consensus of expert opinion on the use of
clean technique. clean or sterile dressing technique in the management of
Also, in 1997, Wise, Hoffman, Grant, and Bostrom sur- chronic wounds. Research is limited and inconclusive
veyed staff nurses (N ⫽ 723) in five health care agencies about value of clean or sterile in healing outcomes. Limited
WON200342.indd S32 03/03/12 4:27 PM
J WOCN ■ Volume 39/Number 2S Clean vs. Sterile Dressing Techniques S33
evidence indicates clean technique reduces costs and c. Invasiveness of wound care procedure.
might require less time to perform. • How invasive is the procedure?
Wound care is provided in a variety of patient care set- • Is debridement to be performed?
tings including acute care, sub-acute care, long-term care, • Does the procedure involve changing a simple
outpatient clinics, and in the home. The question arises: transparent film or hydrocolloid dressing or
Should a different technique be utilized in the delivery of extensive packing of the wound?
wound care based on the health care setting? Decisions d. Health care setting.
made about the type of technique to be used may be more • Who will be doing the wound care?
reasonably based on what will be done to the wound, • What is the environment in which the care
rather than where or to whom the care is delivered.1,2 will be delivered?
Other factors that may influence the technique are the e. Selection/use of supplies/instruments.
status/acuity of the patient, the health care setting, and • Use and maintenance may be based on likeli-
type of caregiver.31 For instance, a frail, elderly patient who hood of exposure to organisms in the care setting.
is receiving immunosuppressant drugs who has a large, • What is clean, what is sterile, and what is con-
full thickness, sternal wound receiving daily dressing taminated?
changes might benefit from “sterile” technique. A middle- • Keep items apart by using no touch technique.
aged patient who was in an automobile accident and sub- f. Solutions for cleansing/treatment.
sequently developed a non-infected, Stage III pressure • Initially, solutions such as commercially prepared
ulcer treated with hydrocolloid dressings, changed every wound cleansers and normal saline are sterile.
3-4 days, might be adequately managed using “clean” • The shelf life of solutions once they are opened
technique. There is no scientific evidence or consensus is based on manufacturers’ recommendations
that any one of these conditions is more or less important and the policy of the health care institution
in selecting the appropriate method of care for the wound. providing the care. No definitive scientific evi-
It has been suggested that an assessment of patients risk dence exists to guide the policies of the health
for infection is an important factor in choosing the type care institution.
of technique.3,34 2. The Table addresses dressing technique for chronic
wounds.1,2,35
■ Recommendations
Recommendation for Education
Recommendations for Practice: Considerations for Health care facilities should develop policies and educa-
Clean Versus Sterile Technique tional programs for staff to enhance understanding and
1. The following factors should be considered when principles of asepsis, choosing and criteria for performing
planning and selecting dressing technique for clean or sterile technique.
chronic wound care.2,34
a. Patient factors, immune status, acute vs. chronic Recommendation for Research
wound. Research is needed to provide an evidence-basis to support
b. Type, location, and depth of the wound. either “clean” or “sterile” dressing technique to manage
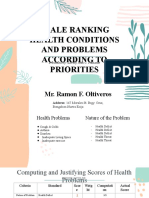
TABLE.
Suggested Dressing Technique for the Management of Chronic Wounds
Supplies (Includes Solutions
Intervention Hand Washing Gloves and Dressing Supplies) Instruments
Wound Cleansing Yes Clean Normal saline or commercially prepared Irrigate with sterile device;
wound cleanser maintain as clean per
Sterile, maintain as clean per policy* policy*
Routine Dressing Change without Yes Clean Sterile, maintain as clean per policy* Sterile; maintain as clean
Debridement per policy*
Dressing Change with Mechanical, Yes Clean Sterile, maintain as clean per policy* Sterile; maintain as clean
Chemical, or Enzymatic Debridement per policy*
Dressing Change with Sharp Yes Sterile Sterile Sterile
Conservative Bedside Debridement
*Maintain clean per policy means that each health care setting must establish policies that address the parameters for use/maintenance of supplies/solutions,
taking into consideration such factors as expiration dates, costs, and manufacturers’ recommendations.
WON200342.indd S33 03/03/12 4:27 PM
S34 Clean vs. Sterile Dressing Techniques J WOCN ■ March/April 2012
chronic wounds. Continued research is needed that exam- 18. Gardner SE, Frantz RA, Doebbling BN. The validity of the
ines patient outcomes in terms of healing, infection rates, clinical signs and symptoms used to identify localized chronic
wound infection. Wound Repair Regenerat. 2001;9:178-186.
and costs of clean vs. sterile techniques. Studies should
19. Doughty DB, Sparks-DeFriese B. Wound healing physiology. In:
clearly describe methods and supplies used for clean or Bryant RA, & Nix DP, eds. Acute and Chronic Wounds: Current
sterile technique. Large multi-site, randomized studies Management Concepts. 4th ed. St. Louis: Mosby-Elsevier; 2012:63-82.
across health care settings are needed to insure appropri- 20. Somerset M. ed. Wound Care Fundamentals. Wound Care Made
ate patient outcomes are achieved in a cost effective man- Incredibly Easy. 2nd ed. Philadelphia, PA: Lippincott Williams
& Wilkins; 2007:1-26.
ner that does not compromise patient safety.
21. Whitney JD. Surgical wounds and incision care. In: Bryant R,
& Nix D, eds. Acute & Chronic Wounds: Current Management
Concepts. 4th ed. St. Louis, MO: Elsevier Mosby; 2012:469-475.
■ References 22. Mangram AJ, Horan T, Pearson ML, Silver BS, Jarvis WR.
1. APIC & WOCN. Position Statement. Clean vs. Sterile: Guideline for Prevention of Surgical Site Infection. 1999;20:247-
Management of Chronic Wounds. APIC News. 2001. http:// 248. Centers for Disease Control and Prevention. http://www.
www.apic.org/AM/Template.cfm?Section⫽Topics1&CONTEN cdc.gov/ncidod/dhqp/pdf/guidelines/SSI.pdf. Accessed
TID⫽6376&TEMPLATE⫽/CM/ContentDisplay.cfm. Accessed March 16, 2011.
March 20, 2011. 23. Massachusetts Department of Public Health. Prevention of sur-
2. Wooten MK, Hawkins K. APIC 2000 Guidelines Committee. gical site infections. In: Prevention and control of healthcare-
Clean versus sterile: management of chronic wounds. J Wound, associated infections in Massachusetts, 2008. http://www.
Ostomy Contin Nurs. 2001;28:24A-26A. guidelines.gov/. Accessed January 29, 2011.
3. Rowley S, Clare S, Macqueen S, Molyneux R. ANTT v2: an up- 24. Bergstrom N, Bennett MA, Carlson C, et al. Treatment of Pressure
dated practice framework for aseptic technique. Br J Nurs. Ulcers. Clinical Practice Guideline No. 15:59-60. Rockville
2010;19:S5S11. (MD): Agency for Health Care Policy and Research, Public
4. Bates-Jensen BM, Ovington LG. Management of exudate and Health Service, US Department of Health and Human Services,
infection. In: Sussman C, & Bates-Jensen B, eds. Wound Care: A AHCPR Publication No. 95-0652.; 1994.
Collaborative Practice Manual for Physical Therapists and Nurses. 25. NPUAP-EPUAP (National Pressure Ulcer Advisory Panel-
3rd ed. Philadelphia, PA: Lippincott, Williams & Wilkins; European Pressure Ulcer Advisory Panel). Prevention and
2007:215-233. Treatment of Pressure Ulcers: Clinical Practice Guideline.
5. Ferreira AM, de Andrade D. Integrative review of the clean and Washington DC: National Pressure Advisory Panel; 2009.
sterile technique, agreement and disagreement in the execu- 26. Angeras MH, Brandberg A, Falk A, Seeman T. Comparison be-
tion of dressing. Acta Palulista de Enfermagem. 2008;21:117-121. tween sterile saline and tap water for the cleaning of acute
6. Aziz AM. Variations in aseptic technique and implications for traumatic soft tissue wounds. Eur J Surg. 1992;58:347-350.
infection control. Br J Nurs. 2009;18:26-31. 27. Alexander D, Gammage D, Nichols A, Gaskins D. Analysis of
7. Pegram A, Bloomfield J. Wound care: principles of aseptic tech- strike-through contamination in saturated sterile dressings.
nique. Ment Health Pract. 2010;14:14-18. Clin Nurs Res. 1992;1:28-34.
8. Rolstad BS, Bryant RA, Nix DP. Topical management. In: 28. Popovich DM, Alexander D, Rittman M, Mantorella C,
Bryant R, & Nix D, eds. Acute & Chronic Wounds: Current man- Jackson L. Strike-through contamination in saturated sterile
agement Concepts. 4th ed. St. Louis, MO: Elsevier Mosby; dressings: a clinical analysis. Clin Nurs Res. 1995;4:195-207.
2012:289-307. 29. Stotts NA, Barbour S, Slaughter R, Wipke-Tevis D. Wound care
9. Stotts NA. Wound Infection: Diagnosis and Management. In: practices in the United States. Ostomy Wound Manag.
Bryant R, & Nix D, eds. Acute & Chronic Wounds: Current 1993;39:59-62.
Management Concepts. 4th ed. St. Louis, MO: Elsevier Mosby; 30. Stotts NA, Barbour S, Slaughter R, et al. Sterile versus clean
2012:270-278. technique in postoperative wound care of patients with open
10. Sibbald RG, Woo KY, Ayello EA. Infection and inflammation. surgical wounds: a pilot study. J Wound, Ostomy Contin Nurs.
Ostomy Wound Manag. 2009;55(Suppl):15-18. 1997;24:10-8.
11. Landis SJ. Chronic wound infection and antimicrobial use. Adv 31. Wise LC, Hoffman J, Grant L, Bostrom J. Nursing wound care
Skin Wound Care. 2008;21:531-540. survey: sterile and nonsterile glove choice. J Wound, Ostomy
12. Cowan T. Biofilms and their management: implications for the Contin Nurs. 1997;24:144-150.
future of wound care. J Wound Care. 2010;19:117-120. 32. Lawson C, Juliano L, Ratliff C. Does sterile or nonsterile tech-
13. Wolcott RD, Cox SB, Dowd SE. Healing and healing rates of nique make a difference in wounds healing by secondary in-
chronic wounds in the age of molecular pathogen diagnostics. tention? Ostomy Wound Manag. 2003;49:56-8, 60.
J Wound Care. 2010;19:272-281. 33. Fellows J, Crestodina L. Home-prepared saline. J Wound,
14. Gray M, Doughty D. Clean versus sterile technique when Ostomy Contin Nurs. 2006;33:606-609.
changing wound dressings. J Wound, Ostomy Contin Nurs. 2001; 34. Flores A. Sterile versus non-sterile glove use and aseptic tech-
28:125-128. nique. Nurs Stand. 2008;23:35-39.
15. Bowler PG. The 105 bacterial growth guideline: reassessing its 35. Crow S, Thompson PJ. Infection control perspectives. In:
clinical relevance in wound healing. Ostomy Wound Manag. Krasner D, & Kane D, eds. Chronic Wound Care: A Course Book
2003;49:44-53. for Healthcare Professionals. 3rd ed. Wayne, PA: Health
16. Kravitz S. Infection: are we defining it accurately? Adv Skin Management Publications; 2001:357-367.
Wound Care. 2006;19:176.
17. Cutting KF, White RJ. Criteria for identifying wound infec- Date Approved by the WOCN Society Board of Directors:
tions–Revisited. Ostomy Wound Manag. 2005;51:28-34. September 27, 2011
WON200342.indd S34 03/03/12 4:27 PM
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5814)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- Group 3 Cardiovascular ProblemDocument52 pagesGroup 3 Cardiovascular ProblemWARREN WILLIAM PERAN100% (3)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Subjective Assessment FormDocument8 pagesSubjective Assessment FormTriana KarnadipaNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Concept Map in Head and Neck CancerDocument3 pagesConcept Map in Head and Neck CancerWendy EscalanteNo ratings yet
- Consolidated Annotated Frequency List: We Make NO CLAIMS As To The Accuracy or Efficacy of The Frequencies Posted Here!Document69 pagesConsolidated Annotated Frequency List: We Make NO CLAIMS As To The Accuracy or Efficacy of The Frequencies Posted Here!Matimba SimangoNo ratings yet
- The Healing Power of GarlicDocument306 pagesThe Healing Power of Garlicphilanthropistxmidget9110100% (4)
- 4.0 Thick-Fluids-Poster 2 2019Document1 page4.0 Thick-Fluids-Poster 2 2019Ada EzeNo ratings yet
- Sample Professional Portfolio NFDN 2005 Developmental GrowthDocument2 pagesSample Professional Portfolio NFDN 2005 Developmental GrowthAda EzeNo ratings yet
- 4.0 Eating Well For Your GallbladderDocument2 pages4.0 Eating Well For Your GallbladderAda EzeNo ratings yet
- 3.2 Guiding Principle For Subcutaneous TherapyDocument8 pages3.2 Guiding Principle For Subcutaneous TherapyAda EzeNo ratings yet
- SBAR Report To Physician About A Critical SituationDocument3 pagesSBAR Report To Physician About A Critical SituationAda EzeNo ratings yet
- Pet BrochureDocument20 pagesPet BrochureSheikh Hasnain AliNo ratings yet
- First Aid Kit ContentsDocument8 pagesFirst Aid Kit Contentsalexis mae lavitoriaNo ratings yet
- Pressure Injuries (Pressure Ulcers) and Wound Care - Practice Essentials, Background, AnatomyDocument13 pagesPressure Injuries (Pressure Ulcers) and Wound Care - Practice Essentials, Background, AnatomyKarilNo ratings yet
- 6 TypesDocument3 pages6 TypesSelena BejoNo ratings yet
- Anxiety Related To Hospitalization and Disease Condition As Manifested by Fiscal Expression and VerbalizationDocument2 pagesAnxiety Related To Hospitalization and Disease Condition As Manifested by Fiscal Expression and VerbalizationmonaNo ratings yet
- The Wills Eye Hospital Atlas of Clinical Ophthalmology: Second EditionDocument495 pagesThe Wills Eye Hospital Atlas of Clinical Ophthalmology: Second EditionPeer TutorNo ratings yet
- Website Tachycardia Algorithm DiagramDocument1 pageWebsite Tachycardia Algorithm Diagramcolette zgheibNo ratings yet
- Chronic Kidney DiseaseDocument18 pagesChronic Kidney DiseaseAde Cahyo IslamiNo ratings yet
- Fibromatosis of The Breast Mimicking Cancer: A Case Report: SciencedirectDocument5 pagesFibromatosis of The Breast Mimicking Cancer: A Case Report: SciencedirectNabilla Rahma PutriNo ratings yet
- Epididymitis and OrchitisDocument11 pagesEpididymitis and Orchitiscitra08No ratings yet
- Ophthalmonics 1st EditionDocument116 pagesOphthalmonics 1st Editiondhavalb2086% (7)
- Tuberculosis Spondylitis IIDocument40 pagesTuberculosis Spondylitis IICendraiin MinangkabauNo ratings yet
- Infectious Diseases and Their Treatment in Georgian Written SourcesDocument21 pagesInfectious Diseases and Their Treatment in Georgian Written SourcesIrina GogonaiaNo ratings yet
- Wound AssessmentDocument64 pagesWound AssessmentKeown MukhtarNo ratings yet
- Gan Cao Xie Xin TangDocument2 pagesGan Cao Xie Xin TangAshley Flores100% (1)
- Agents of Opportunistic MycosesDocument6 pagesAgents of Opportunistic MycosesReinDePabloNo ratings yet
- H1N1 Diagnosis, Management and TreatmentDocument56 pagesH1N1 Diagnosis, Management and TreatmentNishanth BabuNo ratings yet
- Algorithm Immunisation Status Jan2020Document1 pageAlgorithm Immunisation Status Jan2020Afsan BulbulNo ratings yet
- Practical 4 Cardivascular and Hepatobiliary SystemDocument9 pagesPractical 4 Cardivascular and Hepatobiliary SystemchinNo ratings yet
- Seroprevalence of Leptospirosis Among People in Shabramant Village, EgyptDocument9 pagesSeroprevalence of Leptospirosis Among People in Shabramant Village, EgyptHielmy Auliya HasyimNo ratings yet
- Susunan Acara Simposium Pertemuan Ilmiah Ilmu Penyakit Dalam (Pit Ipd) 2020Document4 pagesSusunan Acara Simposium Pertemuan Ilmiah Ilmu Penyakit Dalam (Pit Ipd) 2020Getty InasNo ratings yet
- Venous InsufficiencyDocument32 pagesVenous InsufficiencyRalucaNo ratings yet
- SCALE RANKING HEALTH CONDITIONS AND PROBLEMS ACCORDING TO PRIORITIES - Funtanar, Lovely Jean C.Document15 pagesSCALE RANKING HEALTH CONDITIONS AND PROBLEMS ACCORDING TO PRIORITIES - Funtanar, Lovely Jean C.Lovely FuntanarNo ratings yet
- Stds MCQDocument181 pagesStds MCQhesham100% (1)
- Shri Guru Ram Rai University: School of Agricultural ScienceDocument27 pagesShri Guru Ram Rai University: School of Agricultural Sciencesuyash joshiNo ratings yet