Professional Documents
Culture Documents
Copd 11 535
Uploaded by
Rasangi Sumudu Clare SuraweeraOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Copd 11 535
Uploaded by
Rasangi Sumudu Clare SuraweeraCopyright:
Available Formats
International Journal of COPD Dovepress
open access to scientific and medical research
Open Access Full Text Article Review
The optimum timing to wean invasive ventilation
for patients with AECOPD or COPD with
pulmonary infection
This article was published in the following Dove Press journal:
International Journal of COPD
14 March 2016
Number of times this article has been viewed
Yuanlin Song, 1 Rongchang Abstract: COPD is characterized by a progressive decline in lung function and mental and
Chen, 2 Qingyuan Zhan, 3 physical comorbidities. It is a significant burden worldwide due to its growing prevalence,
Shujing Chen, 1 Zujin Luo, 4 comorbidities, and mortality. Complication by bronchial-pulmonary infection causes 50%–90%
Jiaxian Ou, 1 Chen Wang 3 of acute exacerbations of COPD (AECOPD), which may lead to the aggregation of COPD
symptoms and the development of acute respiratory failure. Non-invasive or invasive ventila-
1
Department of Pulmonary Medicine,
Zhongshan Hospital, Fudan University, tion (IV) is usually implemented to treat acute respiratory failure. However, ventilatory support
Shanghai, 2Guangzhou Institute of (mainly IV) should be discarded as soon as possible to prevent the onset of time-dependent
Respiratory Disease, Guangzhou, complications. To withdraw IV, an optimum timing has to be selected based on weaning assess-
3
Department of Respiratory and
Critical Care Medicine, Beijing ment and spontaneous breathing trial or replacement of IV by non-IV at pulmonary infection
China-Japan Friendship Hospital, control window. The former method is more suitable for patients with AECOPD without
4
Department of Pulmonary Medicine,
significant bronchial-pulmonary infection while the latter method is more suitable for patients
Chaoyang Hospital, Beijing, People’s
Republic of China with AECOPD with acute significant bronchial-pulmonary infection.
Keywords: mechanical ventilation, weaning, spontaneous breathing trial, pulmonary control
window, chronic obstructive pulmonary disease
Video abstract Introduction
COPD is characterized by a progressive decline in lung function and mental and physi-
cal comorbidities (eg, depression, dystrophy, and heart failure).1 An exacerbation of
COPD is an acute event caused by several factors. To those patients who need ventilator
support because of lung infection, weaning mechanical ventilation may be particularly
difficult. The clinician’s concern is the optimum timing regarding the condition of
the patient to wean mechanical ventilation. Unfortunately, there is no consensus or
guideline that can give us a distinct conclusion. The aim of this paper is to summarize
the evidence-based optimum timing to wean invasive ventilation (IV) in patients with
acute exacerbations of COPD (AECOPD) or COPD with pulmonary infection.
Point your SmartPhone at the code above. If you have a
QR code reader the video abstract will appear. Or use: COPD and its AECOPD and lung infection in COPD
http://youtu.be/KNFo236SFqA COPD is currently a significant burden in the People’s Republic of China because
of greater risk exposure and uneven medical resource allocation between urban and
remote areas. A population-based, cross-sectional survey conducted between 2002 and
Correspondence: Chen Wang 2004 suggested a COPD prevalence of 8.2% among Chinese population over 40 years
Department of Respiratory and
Critical Care Medicine, Beijing
old.2 Other studies reported varied prevalence ranging from 5% to 13%.3–6 According
China-Japan Friendship Hospital, to the 2004 Global Burden of Disease study, an annual sum of 3 million people die of
2 East Yinghua Road, Beijing, 100029,
People’s Republic of China
COPD worldwide. In the People’s Republic of China alone, COPD-related mortality
Email cyh-birm@263.net was 27.3 in males and 21.3 in females per 100,000 heads according to a national,
submit your manuscript | www.dovepress.com International Journal of COPD 2016:11 535–542 535
Dovepress © 2016 Song et al. This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php
http://dx.doi.org/10.2147/COPD.S96541
and incorporate the Creative Commons Attribution – Non Commercial (unported, v3.0) License (http://creativecommons.org/licenses/by-nc/3.0/). By accessing the work you
hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission
for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms (https://www.dovepress.com/terms.php).
Song et al Dovepress
prospective cohort study conducted between 1990 and 2000. disease are susceptible to lung infection. As stated earlier,
Acute chronic respiratory failure, heart failure, pulmonary lung infection usually accounts for 50%–70% of AECOPD.
infection, pulmonary embolism, cardiac arrhythmia, and Not all lung infections in COPD need intensive care. Only
lung cancer are the major causes of death in patients with the patients who meet the criteria for hospital admission or
COPD according to a cross-sectional study involving ten ICU admission need to be treated in a timely manner.
European centers.7
AECOPD are a common cause of comorbidities and COPD- Treatment for AECOPD/COPD with lung
related mortality.8–11 They are characterized by an increase in the infection patients
symptoms of dyspnea, sputum volume, and sputum purulence Hospital admission is warranted in an increasing number
with or without symptoms of upper respiratory infection.12 of patients with AECOPD to prevent ARF onset.24 An
They may also involve worsening of existing symptoms, which “ABC approach” involving antibiotics, bronchodilators,
require alterations in treatment ranging from antibiotic admin- and corticosteroids is generally extended to maximize
istration, short courses of oral corticosteroids, and increased lung function and to reverse the predisposing causes of
bronchodilator usage.13–14 Reported AECOPD incidence varied exacerbations.25 Mechanical ventilation is also suggested
between 2.5 and 3 episodes per patient and year.15 Being its in 26%–74% of patients with COPD so that the respiratory
major cause, infection accounted for 50%–70% AECOPD muscle load may be alleviated to reduce dyspnea and
occurrences worldwide and 80%–90% AECOPD occurrences respiratory rate and improve arterial oxygenation, partial
in the People’s Republic of China alone.16,17 Other predisposing pressure of carbon dioxide in arterial blood (PaCO2), and
factors include environmental pollution, low temperatures, and pH.26–28 The criteria to start ventilatory support vary but
concomitant heart failure.18,19 Subsequent onset of acute respi- commonly involve the following: 1) moderate to severe dys-
ratory failure (ARF) may result if AECOPD are accompanied pnea where accessory muscles are recruited and abdominal
by bronchial infections, bronchospasm, left ventricular failure, breathing prevails; 2) hypercapnic acidosis (pH ,7.35);
pneumonia, pneumothorax, or thromboembolism. Once ARF 3) tachypnea (.25 rpm).29
occurs, in-patient mortality (4%–30%) substantially rise up to Non-invasive ventilation (NIV) is validated in patients
50% among elderly patients and 11%–26% among intensive with early AECOPD because their tolerable coughing ability
care unit (ICU) patients.10,20–23 suggests a stronger need for respiratory muscle fatigue relief
Lung infection other than acute exacerbation is quite rather than airway clearance. It is thus initially provided for
common in patients with COPD. The most prevalent form patients with severe AECOPD with respiratory acidosis to
is community-acquired pneumonia. Bronchoscopic studies reduce intubation rate, shorten ICU stay, and decrease patient
have shown that at least 50% of patients have bacteria exis- mortality. Nonetheless, IV is indicated if NIV measures fail
tence in their lower airway during exacerbations of COPD.1 to improve clinical manifestation and blood gas parameters
Viruses are also the common etiology of COPD exacerba- 1 hour after implementation.29 Any patient with ineffective
tion next to bacteria. Many patients with COPD who have airway clearance (eg, post-surgical patients or patients with
comorbidities such as hypertension, diabetes, cardiovascular COPD with hypercapnic ARF and pneumonia) needs IV
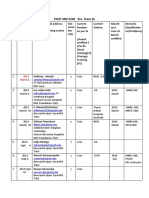
Table 1 Indications for non-invasive ventilation (NIV) and invasive ventilation (IV)
NIV indications IV indications
Clinical manifestations Cardiac/respiratory arrest
Moderate to severe dyspnea Non-respiratory organ failure
Respiratory rate over 25 breaths/min Severe upper gastrointestinal bleeding
Obvious use of accessory muscles Hemodynamic instability
Paradoxical breathing Unstable cardiac arrhythmia
Gas-exchange abnormalities Facial surgery
PaCO2 exceeding 45 mmHg Facial trauma or deformity
pH below 7.35 Upper airway obstruction
PaO2/FiO2 below 250 mmHg Inability to cooperate
Airway protection
Clear of secretions and saliva
A high risk of aspiration
Abbreviations: FiO2, fraction of inspired oxygen; PaO2, partial pressure of oxygen in arterial blood; PaCO2, partial pressure of carbon dioxide in arterial blood.
536 submit your manuscript | www.dovepress.com International Journal of COPD 2016:11
Dovepress
Dovepress AECOPD or COPD patients with pulmonary infection
support to improve sputum discharge and ventilation. Table 1 optimal time when NIV should replace IV. According to the
summarizes the indications for both ventilation types.30 Chinese Guideline for Mechanical Ventilation in Patients
In spite of its importance, IV should be discarded when- with Acute Exacerbation of Chronic Obstructive Pulmonary
ever appropriate to avoid time-dependent complications Disease 2007, weaning with T-tube is advised in COPD
associated with intubation, tracheotomy, or ventilation patients without obvious bronchial-pulmonary infection
(Table 2).31–33 To derive optimum advantages from mechani- while replacement by NIV at pulmonary infection control
cal ventilation, one should identify the optimum timing for (PIC) window is advised in COPD patients with obvious
withdrawal so that complications may be prevented while bronchial-pulmonary infection.
respiratory function is restored. NIV has been suggested
to serve the purpose because it was identically capable in Weaning in COPD patients without
unloading respiratory muscles.34 Its application after IV also obvious bronchial-pulmonary infection
significantly reduced weaning time, alleviated ventilator- Tobin summarized six stages in mechanical ventilatory
associated complications, and improved survival. 35–37 support: 1) treatment of ARF; 2) suspicion that weaning
However, no consensus has yet been reached regarding the may be possible; 3) assessment of readiness to wean;
4) spontaneous breathing trial (SBT); 5) extubation; and
Table 2 Complications associated with intubation, tracheotomy, 6) reintubation when required. One is only liberated from
or ventilation IV when he successfully passes the first five steps and
Common complications of intubation and tracheotomy avoids the last.
Airway complications Weaning accounts for almost half of the time in
Laryngeal edema
mechanical ventilation and allows resumption of spontaneous
Tracheal mucosal trauma
Contamination of the lower respiratory tract breathing after gradual reduction of mechanical support.38–42
Loss of humidifying function of the upper airway Randomized and non-randomized historical cohort studies
Common complications of mechanical ventilation verified a more significant reduction in the duration of
Mechanical complications mechanical ventilation when a weaning protocol, involving
Accidental disconnection
Leaks in the ventilator circuit
weaning parameter evaluation and subsequent breathing
Loss of electrical power trials, was used instead of mere clinical judgment.43–46 In view
Loss of gas pressure of general delays in weaning and the associated increase in
Pulmonary complications
mortality,41,47,48 assessment should be performed every day
Ventilator-induced lung injury
Barotrauma to allow prompt initiation of weaning.
Oxygen toxicity Variations exist between protocols but weaning param-
Atelectasis eters essentially stem from observations in respiratory
Nosocomial pneumonia
mechanics, gas exchange, and breathing patterns. Table 3 is
Inflammation
Auto-PEEP a list of parameters to be considered before weaning.47 Daily
Asynchrony screen of weaning parameters was found to have predicted a
Acid–base complications successful extubation with 82% accuracy, nearly 90% sensi-
Respiratory acidosis
Respiratory alkalosis
tivity and positive predictive values. Significance of passing
Cardiovascular complications the screen could also be extended to hospital survival predic-
Reduced venous return tion during the 1st week and a half of mechanical ventilation.
Reduced cardiac output
Its prognostic significance seemed to be limited though, since
Hypotension
Gastrointestinal and nutritional complications up to 29% of the patients failed the screen but withstood
Gastrointestinal bleeding extubation.49 Thus, a successful weaning attempt does not
Malnutrition necessarily require fulfillment of all the mentioned criteria.
Renal complications
SBT is usually granted to a patient who has passed the
Reduced urine output
Increase in antidiuretic hormone (ADH) and decrease weaning assessment. SBT failure is defined by 1) objec-
in atrial natriuretic peptide (ANP) tive indices such as tachypnea, tachycardia, hypertension,
Neuromuscular complications hypotension, hypoxemia or acidosis, and arrhythmia; 2) sub-
Sleep deprivation
Increased intracranial pressure
jective indices such as agitation or distress, depressed mental
Critical illness weakness status, diaphoresis, and evidence of increasing effort.47 Subse-
Abbreviation: PEEP, positive end-expiratory pressure. quently, weaning failure refers to SBT failure or the need for
International Journal of COPD 2016:11 submit your manuscript | www.dovepress.com
537
Dovepress
Song et al Dovepress
Table 3 Assessment of weaning parameters
Clinical assessment 1. Adequate cough
2. Absence of excessive tracheobronchial secretion
3. Resolution of disease acute phase for which the patient was intubated
Objective measurement 4. Clinical stability
Stable cardiovascular status (ie, fc #140 beats/min), systolic BP 90–160 mmHg,
no or minimal vasopressors
Stable metabolic status
5. Adequate oxygenation
SaO2 .90% on FiO2 0.4 (or PaO2/FiO2 $150 mmHg)
PEEP #8 cm H2O
6. Adequate pulmonary function
fR #35 breaths/min
MIP #-20 to -25 cm H2O
VT .5 mL/kg
fR/VT ,105 breaths/min/L
No significant respiratory acidosis
7. Adequate mentation
8. No sedation or adequate mentation on sedation (or stable neurologic patient)
Abbreviations: BP, blood pressure; fc, frequency of cardiotach; FiO2, fraction of inspired oxygen; fR, frequency of respiration; MIP, maximal inspiratory pressure; PaO2, partial
pressure of oxygen in arterial blood; PEEP, positive end-expiratory pressure; SaO2, arterial oxygen saturation; VT, tidal volume.
reintubation within 48 hours of extubation.50,51 According to pressure support might have surpassed T-tube because it
the number of attempts or days prior to successful weaning, compensated for the extra breathing workload caused by an
patients may be classified into three groups:47 1) simple wean- endotracheal tube.57–61 In addition, Cabello et al observed
ing (patients who proceeded from initiation of weaning to more successful pressure support trials in difficult-to-wean
extubation on the first attempt without difficulty); 2) difficult patients when positive end-expiratory pressure (PEEP; 5 cm
weaning (patients failing the first attempt who took up to three H2O) was incorporated to PSV.62 This could be explained by
attempts or as long as 7 days from the first SBT to achieve the abilities of PEEP to 1) reduce respiratory muscle energy
successful weaning); and 3) prolonged weaning (patients who expenditure;63 2) attenuate intrinsic PEEP so that the work
failed at least three weaning attempts or required .7 days of of breathing required to trigger the ventilator reduces;64,65
weaning after the first SBT). Independent factors suggestive and 3) decrease pulmonary artery occlusion pressure.62 For
of prolonged weaning include COPD occurrence,47 higher the past few years, computer-driven automated weaning
PaCO2 and heart rate during the first SBT.52 Sellares et al was introduced to perform SBT automatically in intubated
also found a higher PaCO2 and heart rate among prolonged patients but its value remained questionable from results of
weaning patients before their first SBT, implying their worse different studies.66 Generally, the technology failed to facili-
condition when subjected to the initial trial.52 tate weaning in surgical patients but prevailed in difficult-
SBT is commonly delivered via pressure support ven- to-wean patients,67 such as those with COPD, ischemic heart
tilation (PSV) at 7 cm H2O, continuous positive airway disease, and immunosuppresion.68,69
pressure, or T-piece. A conventional protocol-directed SBT NIV has been proposed as an alternative weaning tool
takes 120 minutes but a 30 minutes trial performed via either in COPD patients who failed SBT. According to a number
T-tubes or PSV was found to be equally effective in iden- of randomized controlled studies and meta-analysis, such
tifying successful extubations.44,53 Comparing the delivery application was associated with reduced mechanical ventila-
frequency, once-daily and multiple-daily T-piece trials were tion, shortened ICU and hospital stay, decreased incidence
found to be equally effective.50 Consensus has also been of septic shock, and pneumonia and improved survival.35,37,70
established over the identical validity of pressure support Theoretically speaking, extubated patients administered with
and T-tube in SBT.54 A similar conclusion was valid among NIV should not be declared as weaning success unless they
infants and children when pressure support was 10 cm H2O.55 ultimately get rid of the ventilatory support. Increased use of
Further to these findings, pressure support was found to over- NIV as a weaning tool thus leads to a new weaning category
run T-tube in difficult-to-wean patients since success of the called “weaning in progress” wherein extubated patients con-
former and failure of the latter regardlessly indicated suc- tinue to be supported by NIV. In spite of its benefits among
cessful extubation with unchanged reintubation rate.56 Indeed, COPD patients, NIV should not be indicated in all patients
538 submit your manuscript | www.dovepress.com International Journal of COPD 2016:11
Dovepress
Dovepress AECOPD or COPD patients with pulmonary infection
Table 4 Standard of the PIC window
Indexes Evaluation
Imaging change Significantly decreased radiographic infiltrations
Ventilator settings 10–12 beats/min for SIMV
10–12 cm H2O for PSV
Body temperature #38°C
Leukocyte count ,10,000/mm3 or 2,000/mm3 less than before
Sputum quantity Significantly reduced
Lightening of sputum color Changed to white
Decreased density of sputum ,II (second level)
Abbreviations: PIC, pulmonary infection control; PSV, pressure support ventilation; SIMV, synchronized intermittent mandatory ventilation.
failing SBT because they may be exposed to extubation from IV in exchange for NIV at PIC window while the
failure due to substantial comorbidities.47 control groups proceeded with IV throughout. By the end
To summarize, the amount of time needed for IV libera- of the trials, the study groups were found to possess lower
tion depends on a sequence of events including suspicion for ventilator-associated pneumonia risks and mortality rate
weaning possibility, performance of weaning assessment, while requiring shorter durations of IV, ventilatory support,
and weaning itself. In order to promptly discard ventilatory and ICU stay.17,74 Another study with nine patients yielded
support, weaning assessment is daily performed in ventilated similar results except in two patients who presented with
patients. When SBT fails in selected COPD patients, NIV unstable hemodynamic condition and consciousness distur-
may be recruited to shorten the duration of IV. bance correspondingly.75
While the significance of PIC window has been verified,
Replacement of invasive ventilation by one should be reminded of how proper training, skills, and
non-invasive ventilation at PIC window observation ascertain the identification of such a stage. Zhang
In the People’s Republic of China, 80%–90% AECOPD failed to recognize PIC window in several clinical cases thus
cases occur as a result of bronchial-pulmonary infection. A led to delay in response and subsequently compromised prog-
significant proportion of them further develop into hyper- nosis and increased medical costs.75 An increased intubation
capnic respiratory failure which requires invasive ventilatory rate has also been associated previously with inexperienced
support. In order to restore respiratory function and avoid labor among hypercapnic ARF patients.76,77 Such results
time-dependent complications, studies are being conducted suggested how proper caring and observation hold the key
to search for an optimum timing to discard IV. to the betterment of all ventilated patients above other clini-
PIC window has been defined as a prompt stage of con- cal advancements.
trolled pulmonary infection following artificial airway estab-
lishment, sputum drainage, and antibiotic administration. Conclusion
It was marked by thinning and decrease of sputum; clear- Ventilatory support is essential among AECOPD patients to
ing of sputum cloudiness; decreases in body temperature, prevent and treat ARF. While NIV is increasingly suggested
radiographic infiltrations, and leukocytes (Table 4).17 At this as a primary option, IV may not be avoided under certain
stage, COPD patients with severe hypercapnic respiratory conditions. In such cases, strategies should be implemented
failure tend to be more stable and respiratory muscle fatigue to discard IV as soon as possible so that time-dependent
becomes relatively more significant in the development of complications may not arise as a result of prolonged IV.
respiratory failure.17 Wang et al17 proposed this stage as an In AECOPD patients, weaning by SBT (assisted with NIV)
optimum timing to replace IV with NIV so that ventilatory is suggested under insignificant bronchial-pulmonary infec-
insufficiency and respiratory muscle fatigue may be resolved tion while replacement by NIV at PIC window is encouraged
while lower airway infection and ventilator-associated under significant bronchial-pulmonary infection.
pneumonia can be avoided. Such a hypothesis was veri-
fied through a prospective cohort study and a prospective, Acknowledgments
multi-centered, randomized controlled trial among COPD The work was supported by the National Key Technology
patients with severe hypercapnic respiratory failure. 71–73 R&D Program of the 12th National Five-year Development
In both research plans, the study groups were liberated Plan (2012BAI05B01 and 2012BAI05B02), the National
International Journal of COPD 2016:11 submit your manuscript | www.dovepress.com
539
Dovepress
Song et al Dovepress
Nature Science Foundation of China (81170056, 81400018, 17. Wang C, Shang M, Huang K, et al. Sequential non-invasive mechani-
cal ventilation following short-term invasive mechanical ventilation
and 81400002), the Shanghai Committee of Science and in COPD induced hypercapnic respiratory failure. Chin Med J (Engl).
Technology (11411951102 and 12JC1402300), and the 2003;116:39–43.
Academic Special Science and Research Foundation for PhD 18. Miravitlles M, Murio C, Guerrero T. Factors associated with relapse
after ambulatory treatment of acute exacerbations of chronic bronchitis,
Education (20130071110044). DAFNE Study Group. Eur Respir J. 2001;17:928–933.
19. Viegi G, Maio S, Pistelli F, Baldacci S, Carrozzi L. Epidemiology of
chronic obstructive pulmonary disease: health effects of air pollution.
Disclosure Respirology. 2006;11:523–532.
The authors report no conflicts of interest in this work. 20. American Thoracic Society Statement. Standards for the diagnosis
and care of patients with chronic obstructive pulmonary disease. Am J
Respir Crit Care Med. 1995;152:S77–S120.
References 21. Seneff MG, Wagner DP, Wagner RP, Zimmerman JE, Knaus WA.
1. Rabe KF, Hurd S, Anzueto A, et al. Global initiative for Chronic Hospital and 1-year survival of patients admitted to intensive care
Obstructive Lung Disease. Global strategy for the diagnosis, manage- units with acute exacerbation of chronic obstructive pulmonary disease.
ment, and prevention of chronic obstructive pulmonary disease: GOLD JAMA. 1995;274:1852–1857.
executive summary. Am J Respir Crit Care Med. 2007;176:532–555. 22. Bach PB, Brown C, Gelfand SE, McCrory DC; American College of
2. Zhong N, Wang C, Yao W, et al. Prevalence of chronic obstructive Physicians-American Society of Internal Medicine; American College
pulmonary disease in China: a large, population-based survey. Am J of Chest Physicians. Management of acute exacerbations of chronic
Respir Crit Care Med. 2007;176:753–760. obstructive pulmonary disease: a summary and appraisal of published
3. Tang G, Yuan F, Pang Y, et al. Survey on prevalence and risk factors evidence. Ann Intern Med. 2001;134:600–620.
of COPD in rural areas in Anhui province. Chin J Tuberc Respir Dis. 23. Patil SP, Krishnan JA, Lechtzin N, Diette GB. In-hospital mortality
2001;24:245. Chinese. following acute exacerbations of chronic obstructive pulmonary disease.
4. Xu F, Yin XY, Zhang M, Shen H, Lu L, Xu Y. Prevalence of physician- Arch Intern Med. 2003;163:1180–1186.
diagnosed COPD and its association with smoking among urban 24. Tabak YP, Sun X, Johannes RS, Gupta V, Shorr AF. Mortality and need
and rural residents in regional mainland China. Chest. 2005;128: for mechanical ventilation in acute exacerbations of chronic obstructive
2818–2823. pulmonary disease: development and validation of a simple risk score.
5. Liu SM, Wang XP, Wang DL, et al. Epidemiologic analysis of Arch Intern Med. 2009;169(17):1595–1602.
COPD in Guangdong province. Zhonghua Yi Xue Za Zhi. 2005;85: 25. Ambrosino N, Vagheggini G. Non-invasive ventilation in exacerbations
747–752. Chinese. of COPD. Int J Chron Obstruct Pulmon Dis. 2007;2(4):471–476.
6. Shan S, Chen B. Epidemiology investigation of chronic obstructive 26. Farah R, Makhoul N. Optimal time needed for withdrawal of mechani-
pulmonary disease in city and country of Tianjin. Med J Tianjin Univ. cal ventilation in patients with chronic obstructive pulmonary disease.
2007;35:488–490. Chinese. Isr Med Assoc J. 2011;13(10):609–612.
7. Zielinski J, MacNee W, Wedzicha J, et al. Causes of death in patients 27. Rodrìguez-Roisin R. COPD exacerbations-5: management. Thorax.
with COPD and chronic respiratory failure. Monaldi Arch Chest Dis. 2006;61:535–444.
1997;52:43–47. 28. Brochard L, Isabey D, Piquet J, et al. Reversal of acute exacerbations
8. Peters DK, Kochanek DK, Murphy SL. Deaths: final data for 1996. of chronic obstructive lung disease by inspiratory assistance with a face
Natl Vital Stat Rep. 1998;47–100. mask. N Engl J Med. 1990;323:1523–1530.
9. Higgins MW, Thom T. Incidence, prevalence and mortality: intra- and 29. García Vicente E, Sandoval Almengor JC, Díaz Caballero LA, Salgado
inter-country difference. In: Hensley MJ, Saunders NA, editors. Clinical Campo JC. Invasive mechanical ventilation in COPD and asthma. Med
Epidemiology of Chronic Obstructive Pulmonary Disease. New York: Intensiva. 2011;35:288–298.
Marcel Dekker, 1990;23–43. 30. Pelosi P, Jaber S. Noninvasive respiratory support in the perioperative
10. Connors AF Jr, Dawson NV, Thomas C, et al. Outcomes following period. Curr Opin Anaesthesiol. 2010;23:233–238.
acute exacerbation of severe chronic obstructive lung disease. The 31. Fagon JY, Chastre J, Domart Y, et al. Nosocomial pneumonia in patients
SUPPORT investigators (Study to Understand Prognoses and Prefer- receiving continuous mechanical ventilation. Prospective analysis of
ences for Outcomes and Risks of Treatment). Am J Respir Crit Care 52 episodes with use of a protected specimen brush and quantitative
Med. 1996;154:959–967. culture techniques. Am Rev Respir Dis. 1989;139:877–884.
11. Fuso L, Incalzi RA, Pistelli R, et al. Predicting mortality of patients 32. Pingleton SK. Complications of acute respiratory failure. Am Rev Respir
hospitalized for acutely exacerbated chronic obstructive pulmonary Dis. 1988;137:1463–1493.
disease. Am J Med. 1995;98:272–277. 33. Hess DR, MacIntyre NR. Mechanical ventilation. In: Hess DR,
12. Anthonisen NR, Manfreda J, Warren CP, Hershfield ES, Harding GK, MacIntyre N, Mishoe S, et al. editors. Respiratory Care: Principles and
Nelson NA. Antibiotic therapy in exacerbations of chronic obstructive Practice. Massachusetts: Jones and Bartlett Publishers. 2011;462–500.
pulmonary disease. Ann Intern Med. 1987;106:196–204. 34. Vitacca M, Ambrosino N, Clini E, et al. Physiological response to
13. Paggiaro PL, Dahle R, Bakran I, Frith L, Hollingworth K, Efthimiou J. pressure support ventilation delivered before and after extubation in
Multicentre randomised placebo-controlled trial of inhaled fluticasone COPD patients not capable of totally spontaneous autonomous breath-
proprionate in patients with chronic obstructive pulmonary disease. ing. Am J Respir Crit Care Med. 2001;164:638–641.
Lancet. 1998;351:73–80. 35. Nava S, Ambrosino N, Clini E, et al. Noninvasive mechanical ventilation
14. Burge PS, Calverley PM, Jones PW, Spencer S, Anderson JA, Maslen TK. in the weaning of patients with respiratory failure due to chronic obstruc-
Randomised, double blind, placebo controlled study of fluticasone propi- tive pulmonary disease. Ann Intern Med. 1998;128:721–728.
onate in patients with moderate to severe chronic obstructive pulmonary 36. Girault C, Daudenthun I, Chevron V, Tamion F, Leroy J, Bonmarchand G.
disease: the ISOLDE trial. BMJ. 2000;320:1297–1303. Noninvasive ventilation as a systematic extubation and weaning tech-
15. Wedzicha JA, Donaldson GC. Exacerbations of chronic obstructive nique in acute-on-chronic respiratory failure. Am J Respir Crit Care
pulmonary disease. Respir Care. 2003;48:1204–1213. Med. 1999;160:86–92.
16. Borrell E, Rodríguez M, Torán P, et al. Incidence and risk factors of 37. Budweiser S, Baur T, Jörres RA, Kollert F, Pfeifer M, Heinemann F.
exacerbations among COPD patients in primary health care: APMPOC Noninvasive ventilation during persisting weaning failure. Am J Respir
study. BMC Public Health. 2009;9:8. Crit Care Med. 2003;168:70–76.
540 submit your manuscript | www.dovepress.com International Journal of COPD 2016:11
Dovepress
Dovepress AECOPD or COPD patients with pulmonary infection
38. Esteban A, Alía I, Ibañez J, Benito S, Tobin MJ. Modes of mechani- 60. Kuhlen R, Max M, Dembinski R, Terbeck S, Jürgens E, Rossaint R.
cal ventilation and weaning. A national survey of Spanish hospitals. Breathing pattern and workload during automatic tube compen-
The Spanish Lung Failure Collaborative Group. Chest. 1994;106: sation, pressure support and T-piece trials in weaning patients.
1188–1193. Eur J Anaesthesiol. 2003;20:10–16.
39. Esteban A, Ferguson ND, Meade MO, et al. Evolution of mechanical 61. Conti G, De Blasi RA, Lappa A, et al. Evaluation of respiratory system
ventilation in response to clinical research. Am J Respir Crit Care Med. resistance in mechanically ventilated patients: the role of the endotra-
2008;177:170–177. cheal tube. Intensive Care Med. 1994;20:421–424.
40. Ely EW, Baker AM, Dunagan DP, et al. Effect on the duration of 62. Cabello B, Thille AW, Roche-Campo F, Brochard L, Gómez FJ,
mechanical ventilation of identifying patients capable of breathing Mancebo J. Physiological comparison of three spontaneous breath-
spontaneously. N Engl J Med. 1996;335:1864–1869. ing trials in difficult-to-wean patients. Intensive Care Med. 2010;36:
41. Esteban A, Anzueto A, Frutos F, et al. Characteristics and outcomes in 1171–1179.
adult patients receiving mechanical ventilation: a 28-day international 63. Sassoon CS, Light RW, Lodia R, Sieck GC, Mahutte CK. Pressure-time
study. JAMA. 2002;287(3):345–355. product during continuous positive airway pressure, pressure support
42. Lemaire F, Teboul JL, Cinotti L, et al. Acute left ventricular dys- ventilation, and T-piece during weaning from mechanical ventilation.
function during unsuccessful weaning from mechanical ventilation. Am Rev Respir Dis. 1991;143:469–475.
Anesthesiology. 1988;69:171–179. 64. Mancebo J, Albaladejo P, Touchard D, et al. Airway occlusion pres-
43. Epstein SK, Ciubotaru RL, Wong JB. Effect of failed extubation on the sure to titrate positive end-expiratory pressure in patients with dynamic
outcome of mechanical ventilation. Chest. 1997;112:186–192. hyperinflation. Anesthesiology. 2000;93:81–90.
44. Esteban A, Alía I, Tobin MJ, et al. Effect of spontaneous breathing trial 65. Smith TC, Marini JJ. Impact of PEEP on lung mechanics and
duration on outcome of attempts to discontinue mechanical ventilation. work of breathing in severe airflow obstruction. J Appl Physiol.
Spanish Lung Failure Collaborative Group. Am J Respir Crit Care Med. 1988;65(4):1488–1499.
1999;159:512–518. 66. Dojat M, Harf A, Touchard D, Lemaire F, Brochard L. Clinical evalua-
45. Zilberberg MD, de Wit M, Pirone JR, Shorr AF. Growth in adult tion of a computer-controlled pressure support mode. Am J Respir Crit
prolonged acute mechanical ventilation: implications for healthcare Care Med. 2000;161:1161–1166.
delivery. Crit Care Med. 2008;36:1451–1455. 67. Rose L, Presneill JJ, Johnston L, Cade JF. A randomised, controlled
46. Epstein SK, Ciubotaru RL. Independent effects of etiology of failure trial of conventional versus automated weaning from mechanical
and time to reintubation on outcome for patients failing extubation. ventilation using SmartCareTM/PS. Intensive Care Med. 2008;34:
Am J Respir Crit Care Med. 1998;158:489–493. 1788–1795.
47. Boles JM, Bion J, Connors A, et al. Weaning from mechanical ventila- 68. Lellouche F, Mancebo J, Jolliet P, et al. A multicenter randomized trial
tion. Eur Respir J. 2007;29:1033–1056. of computer-driven protocolized weaning from mechanical ventilation.
48. Coplin WM, Pierson DJ, Cooley KD, Newell DW, Rubenfeld GD. Impli- Am J Respir Crit Care Med. 2006;174:894–900.
cations of extubation delay in brain-injured patients meeting standard 69. Liu L, Xu XT, Yang Y, Huang YZ, Liu SQ, Qiu HB. Computer-driven
weaning criteria. Am J Respir Crit Care Med. 2000;161:1530–1536. automated weaning reduces weaning duration in difficult-to-wean
49. Ely EW, Baker AM, Evans GW, Haponik EF. The prognostic signifi- patients. Chin Med J. 2013;126:1814–1818.
cance of passing a daily screen of weaning parameters. Intensive Care 70. Burns KE, Adhikari NK, Meade MO. A meta-analysis of noninvasive
Med. 1999;25:581–587. weaning to facilitate liberation from mechanical ventilation. Can J
50. Esteban A, Frutos F, Tobin MJ, et al. A comparison of four methods Anaesth. 2006;53:305–315.
of weaning patients from mechanical ventilation. Spanish Lung Failure 71. Kollef MH. Avoidance of tracheal intubation as a strategy to prevent
Collaborative Group. N Engl J Med. 1995;332:345–350. ventilator-associated pneumonia. Intensive Care Med. 1999;25:
51. Vallverdú I, Calaf N, Subirana M, Net A, Benito S, Mancebo J. Clini- 553–555.
cal characteristics, respiratory functional parameters, and outcome of a 72. Nourdine K, Combes P, Carton MJ, Beuret P, Cannamela A, Ducreux JC.
two-hour T-piece trial in patients weaning from mechanical ventilation. Does noninvasive ventilation reduce the ICU nosocomial infection
Am J Respir Crit Care Med. 1998;158:1855–1862. risk? A prospective clinical survey. Intensive Care Med. 1999;25:
52. Sellares J, Ferrer M, Cano E, Loureiro H, Valencia M, Torres A. Pre- 567–573.
dictors of prolonged weaning and survival during ventilator weaning 73. Plant PK, Eliott MW. Non-invasive ventilation in acute exacerbations
in a respiratory ICU. Intensive Care Med. 2011;37:775–784. of COPD. Q J Med. 1998;91:657–660.
53. Perren A, Domenighetti G, Mauri S, Genini F, Vizzardi N. Protocol- 74. Collaborating Research Group for Noninvasive Mechanical Ventilation
directed weaning from mechanical ventilation: clinical outcome in of Chinese Respiratory Society. Pulmonary infection control window in
patients randomized for a 30-min or 120-min trial with pressure support treatment of severe respiratory failure of chronic obstructive pulmonary
ventilation. Intensive Care Med. 2002;28:1058–1063. diseases: a prospective, randomized controlled, multi-centred study.
54. Richard C, Beydon L, Cantagrel S, et al. Weaning from mechanical venti- Chin Med J (Engl). 2005;118(19):1589–1594.
lation. Consensus recommendations. Reanimation. 2001;10:697–698. 75. Zhang X. Pulmonary infection control window as a switching point for
55. Farias JA, Retta A, Alía I, et al. A comparison of two methods to perform consequential ventilation: an encouraging finding in treatment of acute
a breathing trial before extubation in pediatric intensive care patients. respiratory failure of chronic obstructive pulmonary disease. Chin Med
Intensive Care Med. 2001;27:1649–1654. J (Engl). 2005;118(19):1587–1588.
56. Ezingeard E, Diconne E, Guyomarch S, et al. Weaning from mechanical 76. Carlucci A, Delmastro M, Rubini F, Fracchia C, Nava S. Changes in
ventilation with pressure support in patients failing a T-tube trial of the practice of non-invasive ventilation in treating COPD patients over
spontaneous breathing. Intensive Care Med. 2006;32:165–169. 8 years. Intensive Care Med. 2003;29:419–425.
57. Fiastro JF, Habib MP, Quan SF. Pressure support compensation for 77. Nouira S, Marghli S, Belghith M, Besbes L, Elatrous S, Abroug F.
inspiratory work due to endotracheal tubes and demand continuous Once daily oral ofloxacin in chronic obstructive pulmonary disease
positive airway pressure. Chest. 1988;93:499–505. exacerbation requiring mechanical ventilation: a randomized placebo-
58. Straus C, Louis B, Isabey D, Lemaire F, Harf A, Brochard L. controlled trial. Lancet. 2001;358:2020–2025.
Contribution of the endotracheal tube and the upper airway to breathing
workload. Am J Respir Crit Care Med. 1998;157:23–30.
59. Brochard L, Rua F, Lorino H, Lemaire F, Harf A. Inspiratory pressure
support compensates for the additional work of breathing caused by
the endotracheal tube. Anesthesiology. 1991;75:739–745.
International Journal of COPD 2016:11 submit your manuscript | www.dovepress.com
541
Dovepress
Song et al Dovepress
International Journal of COPD Dovepress
Publish your work in this journal
The International Journal of COPD is an international, peer-reviewed This journal is indexed on PubMed Central, MedLine and CAS. The
journal of therapeutics and pharmacology focusing on concise rapid manuscript management system is completely online and includes a
reporting of clinical studies and reviews in COPD. Special focus is given very quick and fair peer-review system, which is all easy to use. Visit
to the pathophysiological processes underlying the disease, intervention http://www.dovepress.com/testimonials.php to read real quotes from
programs, patient focused education, and self management protocols. published authors.
Submit your manuscript here: http://www.dovepress.com/international-journal-of-chronic-obstructive-pulmonary-disease-journal
542 submit your manuscript | www.dovepress.com International Journal of COPD 2016:11
Dovepress
You might also like
- Diagnosis and Treatment of Chronic CoughFrom EverandDiagnosis and Treatment of Chronic CoughSang Heon ChoNo ratings yet
- Copd 2019Document18 pagesCopd 2019Ella EllaNo ratings yet
- Farmacología ArtículoDocument7 pagesFarmacología ArtículoLuz Villegas RomeroNo ratings yet
- COPDex Stroke 2017Document8 pagesCOPDex Stroke 2017Angelica ChavesNo ratings yet
- Phenotypes Copd 2018Document10 pagesPhenotypes Copd 2018Angelica ChavesNo ratings yet
- Hub TBC DG CopdDocument7 pagesHub TBC DG CopdAmalNo ratings yet
- Comparison of Flutter DeviceDocument6 pagesComparison of Flutter DeviceAditiya RahmanNo ratings yet
- Proteome Profiling of Lung Tissues in ChronicDocument8 pagesProteome Profiling of Lung Tissues in ChronicAndreea MoalesNo ratings yet
- Acute Exacerbation of COPD Is It The Stroke of The LungsDocument9 pagesAcute Exacerbation of COPD Is It The Stroke of The LungsBruna AlencarNo ratings yet
- Clinical, Physiological, and Radiological Features of Asthma-Chronic Obstructive Pulmonary Disease Overlap SyndromeDocument7 pagesClinical, Physiological, and Radiological Features of Asthma-Chronic Obstructive Pulmonary Disease Overlap SyndromeAghniaNo ratings yet
- Inoue Et Al. - 2017 - Prevalence and Characteristics of Asthma-COPD OverDocument8 pagesInoue Et Al. - 2017 - Prevalence and Characteristics of Asthma-COPD OverĐức Tài NguyễnNo ratings yet
- Copd 9 027Document13 pagesCopd 9 027Yussuf MuhammadNo ratings yet
- Sumber Abstrak PPOKDocument12 pagesSumber Abstrak PPOKKiociNo ratings yet
- COPD 365771 New Perspectives On Chronic Obstructive Pulmonary DiseaseDocument10 pagesCOPD 365771 New Perspectives On Chronic Obstructive Pulmonary DiseaseDi LaNo ratings yet
- Pauwels 2004Document8 pagesPauwels 2004srichakadharsri911No ratings yet
- Atypical Pathogen Distribution in Chinese Hospitalized AECOPD Patients, A Multicenter Cross-Sectional Study 2021Document10 pagesAtypical Pathogen Distribution in Chinese Hospitalized AECOPD Patients, A Multicenter Cross-Sectional Study 2021amyNo ratings yet
- Clinical Issues of Mucus Accumulation in COPDDocument12 pagesClinical Issues of Mucus Accumulation in COPDastriedamaliaamanatNo ratings yet
- Blouet 2018 SDocument10 pagesBlouet 2018 SnarykNo ratings yet
- Jurnal Pendukung 3Document11 pagesJurnal Pendukung 3Sonia Ayu AndiniNo ratings yet
- A Belgian Survey On The Diagnosis of Asthma - COPD Overlap SyndromeDocument13 pagesA Belgian Survey On The Diagnosis of Asthma - COPD Overlap SyndromesyahrulNo ratings yet
- 5 ArticddcleDocument6 pages5 ArticddcleRosi MauliniNo ratings yet
- 2019 - Chronic Obstructive Pulmonary Disease andDocument6 pages2019 - Chronic Obstructive Pulmonary Disease andAndreea MoalesNo ratings yet
- 2020 - Association Between Systemic and PulmonaryDocument11 pages2020 - Association Between Systemic and PulmonaryAndreea MoalesNo ratings yet
- 5 ArticleDocument6 pages5 ArticleVidini Kusuma AjiNo ratings yet
- Jurnal SOPTDocument10 pagesJurnal SOPTAnonymous Skzf3D2HNo ratings yet
- Li 38 533Document7 pagesLi 38 533techiemedicNo ratings yet
- Burden and Characteristics of Severe ChronicDocument10 pagesBurden and Characteristics of Severe ChronicAndreea MoalesNo ratings yet
- Lung Blast InjuryDocument10 pagesLung Blast InjuryHany ElbarougyNo ratings yet
- Ventilatory Strategies in Obstructive Lung. Parrilla2014Document10 pagesVentilatory Strategies in Obstructive Lung. Parrilla2014EzeBorjesNo ratings yet
- Dysfunctional Lung AnatomyDocument7 pagesDysfunctional Lung AnatomyMoira SetiawanNo ratings yet
- Update On The Pathogenesis of Chronic Obstructive Pulmonary DiseaseDocument9 pagesUpdate On The Pathogenesis of Chronic Obstructive Pulmonary DiseaseHum BlumNo ratings yet
- Medical EnglishDocument4 pagesMedical EnglishDiana MinzatNo ratings yet
- Point of Care Procalcitonin Test To Reduce Antibiotic Exposure in Patients Hospitalized With Acute Exacerbation of COPDDocument10 pagesPoint of Care Procalcitonin Test To Reduce Antibiotic Exposure in Patients Hospitalized With Acute Exacerbation of COPDjiglly23No ratings yet
- Air Pollution As An Early Determinant of COPD: Zhuyi Lu, Patrice Coll, Bernard Maitre, Ralph Epaud and Sophie LanoneDocument13 pagesAir Pollution As An Early Determinant of COPD: Zhuyi Lu, Patrice Coll, Bernard Maitre, Ralph Epaud and Sophie LanoneywtmyxpezickztrkcfNo ratings yet
- Obstructive Sleep Apnea Increases The Prevalence of Hypertension in Patients With Chronic Obstructive DiseaseDocument11 pagesObstructive Sleep Apnea Increases The Prevalence of Hypertension in Patients With Chronic Obstructive Diseasem9966822No ratings yet
- Copd 224735 Impact of Peak Oxygen Pulse On Patients With Chronic ObstrucDocument9 pagesCopd 224735 Impact of Peak Oxygen Pulse On Patients With Chronic ObstrucaninnaNo ratings yet
- Ija 59 574Document10 pagesIja 59 574Vasu DevanNo ratings yet
- Obstructive Sleep Apnea in Chronic Obstructive PulmonaryDocument5 pagesObstructive Sleep Apnea in Chronic Obstructive PulmonaryGeorge Cătălin AlexandruNo ratings yet
- EurasianJPulmonol21121-2072943 054529Document8 pagesEurasianJPulmonol21121-2072943 054529Fathanah Yanti MphNo ratings yet
- Exhaled Breath Analysis in The Differentiation of Pneumonia From Acute Pulmonary OedemaDocument7 pagesExhaled Breath Analysis in The Differentiation of Pneumonia From Acute Pulmonary OedemaAkka RakaNo ratings yet
- Chronic Obstructive Pulmonary DiseaseDocument33 pagesChronic Obstructive Pulmonary DiseaseEspers BluesNo ratings yet
- Chronic Bronchitis and COPDDocument11 pagesChronic Bronchitis and COPDRodli AkbarNo ratings yet
- Exacerbations of CopdDocument10 pagesExacerbations of CopdMelissa PeñataNo ratings yet
- Bronchite Chhronique 2022Document12 pagesBronchite Chhronique 2022Ella EllaNo ratings yet
- Understanding Copd-Overlap SyndromesDocument63 pagesUnderstanding Copd-Overlap SyndromesGeorge Cătălin AlexandruNo ratings yet
- FullDocument10 pagesFullMuhammad SajidannorNo ratings yet
- Li Et Al 2020 Smoking Status Affects Clinical Characteristics and Disease Course of Acute Exacerbation of ChronicDocument10 pagesLi Et Al 2020 Smoking Status Affects Clinical Characteristics and Disease Course of Acute Exacerbation of ChronicNur Syah Fitriyana RamadhaniNo ratings yet
- Ohar 2016Document13 pagesOhar 2016lasinah272No ratings yet
- Assessment of Cardiovascular Changes Among Chronic Obstructive Pulmonary Disease Patients at Rural Tertiary Care Center of Northern IndiaDocument5 pagesAssessment of Cardiovascular Changes Among Chronic Obstructive Pulmonary Disease Patients at Rural Tertiary Care Center of Northern IndiaKarthik SNo ratings yet
- Chronic Obstructive Pulmonary Disease: Linking Outcomes and Pathobiology of Disease ModificationDocument5 pagesChronic Obstructive Pulmonary Disease: Linking Outcomes and Pathobiology of Disease ModificationAnonymous jbWresQ0lNo ratings yet
- Article AMPc Relajación Del M LisoDocument11 pagesArticle AMPc Relajación Del M LisoJonatan LZNo ratings yet
- Copd 10 1703Document7 pagesCopd 10 1703Maria Camila SanabriaNo ratings yet
- Management of Acute Exacerbation of Copd: Dr. Fanny WS KoDocument3 pagesManagement of Acute Exacerbation of Copd: Dr. Fanny WS KoCalca NeusNo ratings yet
- Epid COPDDocument9 pagesEpid COPDAgung WistaraNo ratings yet
- ENG JCOPDF-2019-0128-StringerDocument11 pagesENG JCOPDF-2019-0128-Stringerulfiandi rizkiNo ratings yet
- Copd: Defining and Magnitude of ProblemDocument37 pagesCopd: Defining and Magnitude of ProblemSiti AmandaNo ratings yet
- Lood Eosinophil Percentage As A Predictor of Response Toinhaled Corticosteroid in BronchiectasisDocument8 pagesLood Eosinophil Percentage As A Predictor of Response Toinhaled Corticosteroid in BronchiectasiskarlosNo ratings yet
- Jurnal INTER BANTUL DG RIZADocument12 pagesJurnal INTER BANTUL DG RIZAMuhammad Amin KutbiNo ratings yet
- Epidemiology of Chronic Obstructive Pulmonary Disease: A Literature ReviewDocument39 pagesEpidemiology of Chronic Obstructive Pulmonary Disease: A Literature ReviewgalihNo ratings yet
- Sarkar Et Al-2017-The Clinical Respiratory JournalDocument11 pagesSarkar Et Al-2017-The Clinical Respiratory JournalAntoninus HengkyNo ratings yet
- Anaphylaxis Assessment and Referral After Emergency Treatment PDF 35109510368965Document15 pagesAnaphylaxis Assessment and Referral After Emergency Treatment PDF 35109510368965Rasangi Sumudu Clare SuraweeraNo ratings yet
- CCM1Document5 pagesCCM1Rasangi Sumudu Clare SuraweeraNo ratings yet
- Ccr16 BookDocument228 pagesCcr16 BookRasangi Sumudu Clare SuraweeraNo ratings yet
- Schools With Soul Case Studies and Frameworks 3Document39 pagesSchools With Soul Case Studies and Frameworks 3Rasangi Sumudu Clare SuraweeraNo ratings yet
- Gastroparesis in Adults Oral Erythromycin PDF 54116458939430341Document29 pagesGastroparesis in Adults Oral Erythromycin PDF 54116458939430341Rasangi Sumudu Clare SuraweeraNo ratings yet
- Peripheral Vasopressor Guide FinalDocument16 pagesPeripheral Vasopressor Guide FinalRasangi Sumudu Clare SuraweeraNo ratings yet
- AnaphylaxisDocument13 pagesAnaphylaxisRasangi Sumudu Clare SuraweeraNo ratings yet
- RT Consult Form Side #2Document1 pageRT Consult Form Side #2Rick Frea100% (1)
- Navodaya Vidayalaya SamitiDocument100 pagesNavodaya Vidayalaya SamitiAnoopNo ratings yet
- Final Result Stray Vacancy Round PG 2021Document45 pagesFinal Result Stray Vacancy Round PG 2021suryadev s24No ratings yet
- Evita V300 enDocument4 pagesEvita V300 enIgor VinoraNo ratings yet
- Guide To Oxygen Delivery SystemDocument3 pagesGuide To Oxygen Delivery SystemDarwin Villestas0% (1)
- Supplementary Questions Concerning Asthma Bronchitis or Other Pulmonary SymptomsDocument1 pageSupplementary Questions Concerning Asthma Bronchitis or Other Pulmonary SymptomsJackophiliNo ratings yet
- Personalized Mechanical VentilationDocument371 pagesPersonalized Mechanical VentilationAngy SaenzNo ratings yet
- Critical Care Therapy and Respiratory Care Section: 1.0 DescriptionDocument7 pagesCritical Care Therapy and Respiratory Care Section: 1.0 DescriptionLenny Ronalyn QuitorianoNo ratings yet
- Chapter 01Document7 pagesChapter 01Robert Kerwick100% (5)
- Trauma ThoraksDocument35 pagesTrauma ThoraksmayaNo ratings yet
- 3100A Quick Reference Card FinalDocument2 pages3100A Quick Reference Card FinalSwami MeeraNo ratings yet
- Pulmonary FibrosisDocument4 pagesPulmonary FibrosisDimpal Choudhary100% (2)
- Asthma Cough SymptomsDocument5 pagesAsthma Cough SymptomsAiman TahirNo ratings yet
- 08 10 Main3Document41 pages08 10 Main3Lindsey RobbinsNo ratings yet
- Can The Plateau Be Higher Than The Peak PressureDocument6 pagesCan The Plateau Be Higher Than The Peak Pressurealejandro montesNo ratings yet
- Lung Sounds Auscultation - 1Document3 pagesLung Sounds Auscultation - 1George BarajazNo ratings yet
- Terapi Oksigen PDFDocument50 pagesTerapi Oksigen PDFelianamuis100% (1)
- Pulmonary Pathophysiology The Essentials-2013-CD PDFDocument196 pagesPulmonary Pathophysiology The Essentials-2013-CD PDFMena HashemNo ratings yet
- Chest Trauma3Document120 pagesChest Trauma3Rojelle LezamaNo ratings yet
- COPD SimDocument10 pagesCOPD Simbarbara60% (5)
- Lung - HRCT Basic Interpretatio NDocument19 pagesLung - HRCT Basic Interpretatio NHarsha VijaykumarNo ratings yet
- Diagnosis of Asthma, COPD and asthma-COPD Overlap Syndrome (ACOS)Document20 pagesDiagnosis of Asthma, COPD and asthma-COPD Overlap Syndrome (ACOS)ThaRie MoCcaztNo ratings yet
- Esophageal and Transpulmonary Pressure in The Clinical Setting - Meaning, Usefulness and PerspectivesDocument14 pagesEsophageal and Transpulmonary Pressure in The Clinical Setting - Meaning, Usefulness and PerspectivesSüleyman YıldırımNo ratings yet
- GINA Severe Asthma Guide 2023 PDFDocument51 pagesGINA Severe Asthma Guide 2023 PDFalfonsinaNo ratings yet
- BronchiectasisDocument36 pagesBronchiectasisMujeeb AfzalNo ratings yet
- Mechanical Ventilation Made Easy - 2009Document484 pagesMechanical Ventilation Made Easy - 2009Dan Bobeica75% (4)
- RMVS001 Rapidly Manufactured Ventilator Specification PDFDocument9 pagesRMVS001 Rapidly Manufactured Ventilator Specification PDFjalmeida88No ratings yet
- Nursing Care PlanDocument3 pagesNursing Care PlanMarielle SorianoNo ratings yet
- High Flow Nasal Cannula Versus Continuous Positive Airway PressureDocument13 pagesHigh Flow Nasal Cannula Versus Continuous Positive Airway PressurefitriNo ratings yet
- Ventilater CareDocument6 pagesVentilater CarehelenfreedaeqdNo ratings yet