Professional Documents
Culture Documents
Ofaa439 1535
Uploaded by
Noel Saúl Argüello Sánchez0 ratings0% found this document useful (0 votes)
2 views2 pagesOriginal Title
ofaa439.1535
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
2 views2 pagesOfaa439 1535
Uploaded by
Noel Saúl Argüello SánchezCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 2
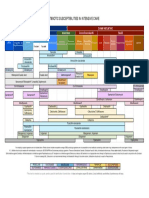
Figure 1- Age distribution of children who received azithromycin prescriptions Figure 1: Choosing Wisely pediatric urinary tract infection
ection diagnostic algorithm
during the study period
Downloaded from https://academic.oup.com/ofid/article/7/Supplement_1/S687/6057672 by guest on 27 October 2023
Figure 2: Patients included/excluded with exclusion criteria
Figure 2- Distribution of diagnoses associated with azithromycin prescriptions
Conclusion: Acute otitis media and pharyngitis accounted for almost half of
the diagnoses associated with azithromycin prescriptions. Treatment guidelines for
both conditions recommend PCN-based therapy as first-line treatment unless there
is a history of PCN allergy. Only a quarter of the patients had allergy documented to
PCN or amoxicillin and, therefore, azithromycin would be considered a suboptimal
antimicrobial choice. These results provide us with a stewardship opportunity to
nudge providers to select appropriate antimicrobial based on diagnosis and history
of allergy.
Disclosures. All Authors: No reported disclosures
1353. Pediatric Urinary Tract Infections: A Choosing Wisely Initiative to
Advance Antimicrobial Stewardship and Diagnostic Accuracy in the Emergency
Department
Michael Prodanuk, MD1; Yen Foong, MD1; Valene Singh, MD1; Laura Morrissey,
MD1; Michelle Science, MD, MSc, FRCPC2; Olivia Ostrow, MD3; 1Department of
Paediatrics, University of Toronto, Toronto, Ontario, Canada; 2The Hospital for Sick
Children, Toronto, ON, Canada; 3Division of Pediatric Emergency Medicine, The
Hospital for Sick Children, University of Toronto, Toronto, Ontario, Canada
Session: P-60. Pediatric Antimicrobial Stewardship (inpatient/outpatient pediatric
focused)
Background. Urinary tract infection (UTI) is a common diagnosis in the pedi-
atric emergency department (ED) that often results in empiric antibiotic treatment
prior to culture results. A 2016 cohort study from our centre found that 47% of
children diagnosed with a UTI and prescribed antibiotics had a negative urine cul-
ture. None of these patients were notified of the misdiagnosis or told to discontinue
antibiotics.
Poster Abstracts • OFID 2020:7 (Suppl 1) • S687
Methods. Institutional approval was obtained for a quality improvement project Background. Vancomycin is frequently used empirically in suspected sepsis
in our quaternary pediatric ED. For uncomplicated pediatric UTIs, the aim was to in neonatal intensive care unit (NICU). However, inappropriate or unnecessary
reduce misdiagnosis by 50% and promote antimicrobial stewardship over a 24-month use can lead to additional morbidities and emergence of drug resistant pathogens.
period. Using the Model for Improvement, two interventions were implemented Standardization of vancomycin use is imperative for safer and more efficient patient
using PDSA cycles: (1) a UTI diagnostic algorithm embedded in the electronic med- care.
ical record, (2) a urine culture callback system. Outcome measures included the Methods. This study was part of a QI initiative to optimize vancomycin use by
percentage of patients with UTI misdiagnosis (urine culture negative) and antibiot- revising a standardized late onset sepsis (LOS) guideline with defined indications and
ic-days saved. Process measures included adherence to the UTI algorithm and call- criteria for empiric vancomycin. The implementation was started in 9/19 after comple-
back system as well as antibiotic duration standardization. As a balancing measure, tion of providers’ education. To reduce seasonal variations, 1/19-3/19 (pre-guideline)
patients developing positive urine cultures without UTI diagnosis were reviewed for and 12/19-2/20 (post-implementation) data was retrospectively compared, includ-
potential harm. ing demographics, antibiotic indications, days of therapy/1000 patient days (AUR),
Figure 3: Run chart of urinary tract infection misdiagnosis rate positive cultures, isolated pathogens and resistance profiles. Clinical outcomes and
adherence to the guideline were evaluated. Wilcoxon rank sum test was applied for
continuous variables and Pearson chi-square test was applied for categorical variables.
p< 0.05 was considered significant.
Results. There were 53 LOS antibiotic courses in 35 patients pre-guideline and
113 in 64 patients post-implementation. We found an overall increase in vancomycin
AUR in the post-implementation period (66.92 vs. 70.72, respectively, p=0.79), how-
ever, largely due to appropriate use of vancomycin for documented infections with
Downloaded from https://academic.oup.com/ofid/article/7/Supplement_1/S687/6057672 by guest on 27 October 2023
gram-positive pathogens (including CONS and MRSE). Mortality was not statistic-
ally significant between two periods (Table 1 and 2). Vancomycin was ordered signifi-
cantly less empirically, as per guideline, in the post implementation period (71.43% vs
46.15%, p=0.02). Adherence to the LOS antibiotics guideline was 69%.
Table 1: Demographic characteristics of infants pre and post-guideline
Figure 4: Callback system - Percent patients contacted and antibiotics-
days saved
Table 2: Therapy indication, medication exposure and clinical outcomes 30 days
after LOS treatment pre and post-guideline
Results. From June 2017-April 2020, 2,183 children (0.97% of all visits) were
diagnosed with a UTI in the ED. 1,381 (63.3%) met inclusion criteria for analysis.
Following UTI algorithm launch, median UTI misdiagnosis decreased by 20% (52.5%
vs. 32.5%), median correct antibiotic duration increased by 30% (45.2% vs. 75.1%),
and algorithm adherence was 78.9%. With implementation of the callback system,
1,678 antibiotic-days were saved as mean patients contacted to discontinue antibiotics
increased from 0% to 76.8%. Of 106 patients with positive urine cultures with missed
UTI diagnosis over a 29-month period, 8 patients returned to the ED within 72 hours
and 2 patients required admission for intravenous antibiotics.
Conclusion. Implementation of a UTI diagnostic algorithm and urine culture
callback system for uncomplicated pediatric UTIs reduced UTI misdiagnosis and pro-
moted antimicrobial and resource stewardship in the ED. Future directions include
improving UTI algorithm adherence through targeted clinician audit and feedback,
plus sustainability planning.
Disclosures. Olivia Ostrow, MD, Choosing Wisely Canada (Advisor or Review
Panel member)
1354. Reducing vancomycin utilization rate in a level 4 NICU
Millie R. Chang, MD1; Kanokporn Mongkolrattanothai, MD2; Steven Chin, MD3;
Yijie Li, PhD3; Regina Orbach, PharmD2; Leslie Stach, PharmD2; Srikumar Nair,
MD3; Vladana Milisavljevic, MD3; 1LAC-USC Medical Center/Children’s Hospital
Los Angeles, Pasadena, California; 2Children Hospital Los Angeles, los angeles, CA;
3
Children’s Hospital Los Angeles, Los Angeles, California
Session: P-60. Pediatric Antimicrobial Stewardship (inpatient/outpatient pediatric
focused)
S688 • OFID 2020:7 (Suppl 1) • Poster Abstracts
You might also like
- Antibiotics 11 00022Document16 pagesAntibiotics 11 00022Putri RamadhaniNo ratings yet
- Antimicrobialstewardship Approachesinthe Intensivecareunit: Sarah B. Doernberg,, Henry F. ChambersDocument22 pagesAntimicrobialstewardship Approachesinthe Intensivecareunit: Sarah B. Doernberg,, Henry F. ChambersecaicedoNo ratings yet
- Prior Antibiotics and Risk of Antibiotic-Resistant Community-Acquired Urinary Tract Infection: A Case - Control StudyDocument8 pagesPrior Antibiotics and Risk of Antibiotic-Resistant Community-Acquired Urinary Tract Infection: A Case - Control StudySyed AmanNo ratings yet
- P009 Assessing The Status Quo Ulcerative Colitis.10Document2 pagesP009 Assessing The Status Quo Ulcerative Colitis.10Santiago ZamudioNo ratings yet
- Fmed 08 584813Document12 pagesFmed 08 584813Annisa SetyantiNo ratings yet
- Using Antibiograms To Improve Antibiotic PrescribingDocument7 pagesUsing Antibiograms To Improve Antibiotic PrescribingfaradillasuciNo ratings yet
- 655 1767 1 PBDocument9 pages655 1767 1 PBFARMASI PRIMA HUSADA SUKOREJONo ratings yet
- Antimicrobial Susceptibility Testing - A Primer For Clinicians 2009 - ReadDocument18 pagesAntimicrobial Susceptibility Testing - A Primer For Clinicians 2009 - ReadJayelle2No ratings yet
- Antibiotic in PicuDocument4 pagesAntibiotic in PicuVickha Dian HapsariNo ratings yet
- آنتی بیوتیک و آپاندیسDocument4 pagesآنتی بیوتیک و آپاندیسmohammad attarzadehNo ratings yet
- s13054 023 04626 ZDocument8 pagess13054 023 04626 ZDipendra PoudelNo ratings yet
- Ultra-Short Course Antibiotics For Pneumonia With Preserved OxygenationDocument2 pagesUltra-Short Course Antibiotics For Pneumonia With Preserved Oxygenationapi-648891519No ratings yet
- Audit&FeedbackDocument8 pagesAudit&FeedbackfatiisaadatNo ratings yet
- Steinberg 2009Document7 pagesSteinberg 2009majedNo ratings yet
- Pharmacokinetics of Vancomycin in Critically Ill Children: A Systematic ReviewDocument18 pagesPharmacokinetics of Vancomycin in Critically Ill Children: A Systematic ReviewDeski MadeNo ratings yet
- Karsies Et Al 2014Document7 pagesKarsies Et Al 2014Quỳnh Nguyễn Thị NhưNo ratings yet
- Influence of Antibiotic Susceptibility Test Results On The Change of Ciprofloxacin and Ofloxacin-Based TreatmentsDocument7 pagesInfluence of Antibiotic Susceptibility Test Results On The Change of Ciprofloxacin and Ofloxacin-Based TreatmentsEstiPramestiningtyasNo ratings yet
- Point Prevalence Study of Antibiotics Use in Paediatric Wards of A Tertiary Health Facility in Kaduna NigeriaDocument8 pagesPoint Prevalence Study of Antibiotics Use in Paediatric Wards of A Tertiary Health Facility in Kaduna NigeriaInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Effect of Procalcitonin-Guided AntibioticDocument11 pagesEffect of Procalcitonin-Guided AntibioticRaul ContrerasNo ratings yet
- Vacuna de Rabia en Humanos PDFDocument7 pagesVacuna de Rabia en Humanos PDFMelina ayalaNo ratings yet
- Antibiotic Strategies in Severe Nosocomial Sepsis: Why Do We Not De-Escalate More Often?Document7 pagesAntibiotic Strategies in Severe Nosocomial Sepsis: Why Do We Not De-Escalate More Often?Anonymous 2kPiJhIlFNo ratings yet
- PROA 4 Texto Explicativo SpanishDocument7 pagesPROA 4 Texto Explicativo SpanishLili VargasNo ratings yet
- Jac-Antimicrobial ResistanceDocument7 pagesJac-Antimicrobial ResistanceKarla HernandezNo ratings yet
- MDocument6 pagesMMathilda UllyNo ratings yet
- 44 2 159Document19 pages44 2 159Nicole MariaNo ratings yet
- Antibiotic Stewardship in The Intensive Care Unit: ReviewDocument12 pagesAntibiotic Stewardship in The Intensive Care Unit: ReviewLesly Peinado TorresNo ratings yet
- Profil Kualitas Dan Kuantitas Penggunaan Antibiotik Profilaksis Pada Pre, On, Dan Post Bedah Di Rumah Sakit Provinsi (RSP) NTBDocument10 pagesProfil Kualitas Dan Kuantitas Penggunaan Antibiotik Profilaksis Pada Pre, On, Dan Post Bedah Di Rumah Sakit Provinsi (RSP) NTBHeryanti PusparisaNo ratings yet
- Randomized Placebo-Controlled Trial of Topical Mupirocin To Reduce Staphylococcus Aureus Colonization in Infants in The Neonatal Intensive Care UnitDocument8 pagesRandomized Placebo-Controlled Trial of Topical Mupirocin To Reduce Staphylococcus Aureus Colonization in Infants in The Neonatal Intensive Care UnitJovie Anne CabangalNo ratings yet
- A Randomized Controlled Trial of Probiotics For Clostridium Dif Cile Infection in AdultsDocument4 pagesA Randomized Controlled Trial of Probiotics For Clostridium Dif Cile Infection in Adults林新中No ratings yet
- Hamdi Cohort Critical AppraisalDocument37 pagesHamdi Cohort Critical AppraisalHamdi MichaelCCNo ratings yet
- 15684-Article Text-51937-1-10-20220301Document12 pages15684-Article Text-51937-1-10-20220301omniyaNo ratings yet
- tmpA70B TMPDocument3 pagestmpA70B TMPFrontiersNo ratings yet
- Procalcitonin and AB DecisionsDocument10 pagesProcalcitonin and AB DecisionsDennysson CorreiaNo ratings yet
- Surgical Site Infection and Cellulitis After Breast And/or Axillary SurgeryDocument7 pagesSurgical Site Infection and Cellulitis After Breast And/or Axillary SurgeryDr-Rabia AlmamalookNo ratings yet
- New and Developing Diagnostic Technologies For Urinary Tract Infections - PMCDocument25 pagesNew and Developing Diagnostic Technologies For Urinary Tract Infections - PMCPuran pataNo ratings yet
- Evaluation of Prescribing Patterns of Antibiotics in General Medicine Ward in A Tertiary Care HospitalDocument6 pagesEvaluation of Prescribing Patterns of Antibiotics in General Medicine Ward in A Tertiary Care HospitalEditor IJTSRDNo ratings yet
- Topical Antibiotics To Prevent Surgical Site Infection After Minor Surgery in Primary CareDocument5 pagesTopical Antibiotics To Prevent Surgical Site Infection After Minor Surgery in Primary CarePitchya WangmeesriNo ratings yet
- Antibiotico YPronosticoDocument6 pagesAntibiotico YPronosticoagonzale52No ratings yet
- Jiaa 221Document13 pagesJiaa 221AndradaLavricNo ratings yet
- Effectiveness of Investments in Leadership and Management Capacity in Thecontext of National Epi ProgramsDocument2 pagesEffectiveness of Investments in Leadership and Management Capacity in Thecontext of National Epi ProgramsZheefNo ratings yet
- To Assess The Criteria of Choice of Antimicrobials Prescribed in Various Clinical Departments of Govt Doon Hospital Rashmi SinglaDocument6 pagesTo Assess The Criteria of Choice of Antimicrobials Prescribed in Various Clinical Departments of Govt Doon Hospital Rashmi SinglaTriple ANo ratings yet
- Jac-Antimicrobial ResistanceDocument7 pagesJac-Antimicrobial ResistanceJuan Manuel Jiménez LeónNo ratings yet
- Antibiotecoterapia en SepsisDocument13 pagesAntibiotecoterapia en SepsisJuan Pablo Arteaga VargasNo ratings yet
- Patient Perception Toward The Use of Fecal Microbial Therapy in The Treatment of Antibiotic-Associated Diarrhea in Selected Hospital of Delhi NCRDocument4 pagesPatient Perception Toward The Use of Fecal Microbial Therapy in The Treatment of Antibiotic-Associated Diarrhea in Selected Hospital of Delhi NCRInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- IDSA Meningitis GuidelinesDocument18 pagesIDSA Meningitis GuidelinesSahid López GarcíaNo ratings yet
- Timing of Antimicrobial Prophylaxis and Infectious Complications in Pediatric Patients Undergoing AppendicectomyDocument3 pagesTiming of Antimicrobial Prophylaxis and Infectious Complications in Pediatric Patients Undergoing AppendicectomyJuan J. Acosta VelásquezNo ratings yet
- Antibiotic Usage in Common and Uncommon Infection in Primary Care Setting - Daerah RompinDocument91 pagesAntibiotic Usage in Common and Uncommon Infection in Primary Care Setting - Daerah RompinMonysyha AtriNo ratings yet
- Research Article: Risk Factors and Prevention Strategies of Nosocomial Infection in Geriatric PatientsDocument6 pagesResearch Article: Risk Factors and Prevention Strategies of Nosocomial Infection in Geriatric Patientschristian demasabuNo ratings yet
- JM 002169Document4 pagesJM 002169edisonballaNo ratings yet
- Jurnal AnestesiDocument24 pagesJurnal AnestesiSeruni Allisa AslimNo ratings yet
- Song 2018Document7 pagesSong 2018Jonathan RyanNo ratings yet
- Antibiotics 11 00308Document17 pagesAntibiotics 11 00308Beatrice BănicăNo ratings yet
- Clin Infect Dis.-2007-Dellit-159-77Document19 pagesClin Infect Dis.-2007-Dellit-159-77Melo PerezNo ratings yet
- LSHTM Research Online: Usage GuidlinesDocument11 pagesLSHTM Research Online: Usage GuidlinesnomdeplumNo ratings yet
- Efficacy and Safety of A Decision Rule For Using Antibiotics in Children With Pneumonia and Vaccinated Against Pneumococcus. A Randomized Controlled TrialDocument7 pagesEfficacy and Safety of A Decision Rule For Using Antibiotics in Children With Pneumonia and Vaccinated Against Pneumococcus. A Randomized Controlled TrialMuhammad FachrurozieNo ratings yet
- Timing of Administration of Prophylactic Antibiotics For Caesarean Section: A Systematic Review and Meta-AnalysisDocument9 pagesTiming of Administration of Prophylactic Antibiotics For Caesarean Section: A Systematic Review and Meta-AnalysissriNo ratings yet
- WSC Abstracts - 2011Document667 pagesWSC Abstracts - 2011cyber_zac52No ratings yet
- Volume Probiotic Adjuvant Therapy Chronic Urticaria 4842allasp1Document8 pagesVolume Probiotic Adjuvant Therapy Chronic Urticaria 4842allasp1fatima amaliaNo ratings yet
- COVID-19 Vaccination of Patients With Chronic Immune-Mediated Inflammatory DiseaseDocument6 pagesCOVID-19 Vaccination of Patients With Chronic Immune-Mediated Inflammatory DiseaseSangeetha VijianNo ratings yet
- Functionalized Nanomaterials for the Management of Microbial Infection: A Strategy to Address Microbial Drug ResistanceFrom EverandFunctionalized Nanomaterials for the Management of Microbial Infection: A Strategy to Address Microbial Drug ResistanceRabah BoukherroubNo ratings yet
- A Critical Care Echocardiography-Driven Approach To Undifferentiated ShockDocument7 pagesA Critical Care Echocardiography-Driven Approach To Undifferentiated ShockNoel Saúl Argüello SánchezNo ratings yet
- Cannabis Induced Cardiac Arrhythmias: A Case SeriesDocument9 pagesCannabis Induced Cardiac Arrhythmias: A Case SeriesNoel Saúl Argüello SánchezNo ratings yet
- Gastroesophageal Reflux Disease (GERD) : Patient Population: Objective: Key PointsDocument12 pagesGastroesophageal Reflux Disease (GERD) : Patient Population: Objective: Key PointsRavindraNo ratings yet
- Nejm PahDocument16 pagesNejm PahAlexander XavierNo ratings yet
- MOOC PP en 3.5Document7 pagesMOOC PP en 3.5Noel Saúl Argüello SánchezNo ratings yet
- TBC Print PDFDocument15 pagesTBC Print PDFIntan FitayantiNo ratings yet
- CRISPR-Cas9 in Vivo Gene Editing For Transthyretin AmyloidosisDocument10 pagesCRISPR-Cas9 in Vivo Gene Editing For Transthyretin AmyloidosisNoel Saúl Argüello SánchezNo ratings yet
- TBC Print PDFDocument15 pagesTBC Print PDFIntan FitayantiNo ratings yet
- Monoclonal Gammopathy of Renal Significance: Review ArticleDocument11 pagesMonoclonal Gammopathy of Renal Significance: Review ArticleNoel Saúl Argüello SánchezNo ratings yet
- Neuroprosthesis For Decoding Speech in A Paralyzed Person With AnarthriaDocument11 pagesNeuroprosthesis For Decoding Speech in A Paralyzed Person With AnarthriaNoel Saúl Argüello SánchezNo ratings yet
- Antibiotic Susceptibilities in Intensive Care: Gram Positive Gram NegativeDocument1 pageAntibiotic Susceptibilities in Intensive Care: Gram Positive Gram NegativeFaisal Reza AdiebNo ratings yet
- Cannabis Induced Cardiac Arrhythmias: A Case SeriesDocument9 pagesCannabis Induced Cardiac Arrhythmias: A Case SeriesNoel Saúl Argüello SánchezNo ratings yet
- Neonatal Genetic SyndromesDocument11 pagesNeonatal Genetic SyndromesNoel Saúl Argüello SánchezNo ratings yet
- Neuroprosthesis For Decoding Speech in A Paralyzed Person With AnarthriaDocument11 pagesNeuroprosthesis For Decoding Speech in A Paralyzed Person With AnarthriaNoel Saúl Argüello SánchezNo ratings yet
- EAU Pocket Guidelines On Urological Infections 2021Document25 pagesEAU Pocket Guidelines On Urological Infections 2021Noel Saúl Argüello SánchezNo ratings yet
- Personal View: Mark Abie Horowitz, David TaylorDocument9 pagesPersonal View: Mark Abie Horowitz, David TaylorNoel Saúl Argüello SánchezNo ratings yet
- Fallone 2019Document10 pagesFallone 2019Noel Saúl Argüello SánchezNo ratings yet
- String Theory For DummiesDocument1 pageString Theory For DummiesNoel Saúl Argüello SánchezNo ratings yet
- EAU Pocket Guidelines On Urological Infections 2021Document25 pagesEAU Pocket Guidelines On Urological Infections 2021Noel Saúl Argüello SánchezNo ratings yet
- Review of Bilirubin Neurotoxicity II: Preventing and Treating Acute Bilirubin Encephalopathy and Kernicterus Spectrum DisordersDocument6 pagesReview of Bilirubin Neurotoxicity II: Preventing and Treating Acute Bilirubin Encephalopathy and Kernicterus Spectrum DisordersNoel Saúl Argüello SánchezNo ratings yet
- Chapmarinum 2017 ASMDocument18 pagesChapmarinum 2017 ASMNoel Saúl Argüello SánchezNo ratings yet
- Relationship Between Cannabis Use and Erectile Dysfunction: A Systematic Review and Meta-AnalysisDocument7 pagesRelationship Between Cannabis Use and Erectile Dysfunction: A Systematic Review and Meta-AnalysisNoel Saúl Argüello SánchezNo ratings yet
- dkh130 PDFDocument7 pagesdkh130 PDFNoel Saúl Argüello SánchezNo ratings yet
- Intermittent Fasting 2018Document14 pagesIntermittent Fasting 2018joao manoelNo ratings yet
- Clinical Research: Heart Failure/cardiomyopathyDocument8 pagesClinical Research: Heart Failure/cardiomyopathyNoel Saúl Argüello SánchezNo ratings yet
- Antimicrobial Agents and Chemotherapy-1998-Den Hollander-749.full PDFDocument6 pagesAntimicrobial Agents and Chemotherapy-1998-Den Hollander-749.full PDFNoel Saúl Argüello SánchezNo ratings yet
- Mechanisms of The Post-Antibiotic Effects Induced by Rifampicin and Gentamicin in Escherichia ColiDocument5 pagesMechanisms of The Post-Antibiotic Effects Induced by Rifampicin and Gentamicin in Escherichia ColiNoel Saúl Argüello SánchezNo ratings yet
- Comparative Study of Bactericidal Activities, Postantibiotic Effects, and Effects On Bacterial Virulence of Penicillin G and Six Macrolides Against Streptococcus PneumoniaeDocument4 pagesComparative Study of Bactericidal Activities, Postantibiotic Effects, and Effects On Bacterial Virulence of Penicillin G and Six Macrolides Against Streptococcus PneumoniaeNoel Saúl Argüello SánchezNo ratings yet
- dkh130 PDFDocument7 pagesdkh130 PDFNoel Saúl Argüello SánchezNo ratings yet
- Primer: Multiple SclerosisDocument27 pagesPrimer: Multiple SclerosisNoel Saúl Argüello SánchezNo ratings yet
- Cardiac FibromaDocument12 pagesCardiac FibromaBhupendraNo ratings yet
- Clinical Collection 2017 2018Document1,602 pagesClinical Collection 2017 2018Laura GranadosNo ratings yet
- African Trypanosomiasis: Practice Essentials, Background, Pathophysiology and EtiologyDocument5 pagesAfrican Trypanosomiasis: Practice Essentials, Background, Pathophysiology and EtiologyFika Anugrah ZulfathonNo ratings yet
- 49 Neural Regulation in Animals-2018 PDFDocument61 pages49 Neural Regulation in Animals-2018 PDFlaw0516No ratings yet
- Drug Dosage Mechanism of Action Indication Contraindications Adverse Effects Nursing ResponsibilitiesDocument1 pageDrug Dosage Mechanism of Action Indication Contraindications Adverse Effects Nursing ResponsibilitiesJeyser T. GamutiaNo ratings yet
- Advances in Coeliac Disease: ReviewDocument9 pagesAdvances in Coeliac Disease: ReviewCamilo ReyesNo ratings yet
- Nutrients: Obesity and Dyslipidemia in South AsiansDocument26 pagesNutrients: Obesity and Dyslipidemia in South AsiansFitriNo ratings yet
- 8 Thyroid PatternsDocument6 pages8 Thyroid Patternsmyscribkanji100% (1)
- Anatomical Zodiacal Degrees PDFDocument6 pagesAnatomical Zodiacal Degrees PDFMaria Marissa100% (2)
- Anatomi Hidung Dan Sinus Paranasal 2Document54 pagesAnatomi Hidung Dan Sinus Paranasal 2anditri weningtyas0% (1)
- Health Checkup: How To Live 100 YearsDocument8 pagesHealth Checkup: How To Live 100 YearsMutante TrioNo ratings yet
- Budwig Cancer GuideDocument118 pagesBudwig Cancer Guidejosip_982156232100% (4)
- Clinical Applications of Neuroimaging in PsychiatryDocument10 pagesClinical Applications of Neuroimaging in PsychiatryJujuNo ratings yet
- MCN-OB Questions and RationalesDocument23 pagesMCN-OB Questions and RationalesRI NA100% (3)
- Triptico El PulpoDocument2 pagesTriptico El PulpoJunStefNo ratings yet
- Endocrine Answer KeyDocument10 pagesEndocrine Answer KeyJoyce LimNo ratings yet
- Atkins DietDocument10 pagesAtkins Dietfenny100% (1)
- Magic Wave July 2011 PDF 69Document19 pagesMagic Wave July 2011 PDF 69Budi TurmokoNo ratings yet
- Drug Interaction Report PDFDocument111 pagesDrug Interaction Report PDFbaerbaNo ratings yet
- Acute Flaccid Paralysis ApproachDocument20 pagesAcute Flaccid Paralysis ApproachKAMLESH RATHODNo ratings yet
- The Yellow Wallpaper by Charlotte Perkins Gilman RianDocument2 pagesThe Yellow Wallpaper by Charlotte Perkins Gilman RianRian Indra FadillahNo ratings yet
- OSCE Master List - CardiologyDocument10 pagesOSCE Master List - CardiologyRebecca WongNo ratings yet
- Cor PulmonaleDocument13 pagesCor PulmonaleHayaNo ratings yet
- Sarcoma de Kaposi PDFDocument4 pagesSarcoma de Kaposi PDFXavier AltamiranoNo ratings yet
- Emedicine Hypersemesis GravidarumDocument26 pagesEmedicine Hypersemesis GravidarumAnonymous 3OoumAUytNo ratings yet
- Rehabilitation of Spinal Cord InjuriesDocument10 pagesRehabilitation of Spinal Cord InjuriesShl Kapre100% (1)
- Lista Decese Reactii Adverse Vaccin C0vld 04JUNE2021Document171 pagesLista Decese Reactii Adverse Vaccin C0vld 04JUNE2021abalansNo ratings yet
- CRIM ExemptingDocument88 pagesCRIM ExemptingKara LorejoNo ratings yet
- AKP Jan. 2022Document30 pagesAKP Jan. 2022jcNo ratings yet
- Case Study,,,,,,pneumoniaDocument52 pagesCase Study,,,,,,pneumoniaJaillah Reigne Cura0% (1)