Professional Documents
Culture Documents
Obs Paper
Uploaded by
Nelson NgulubeOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Obs Paper
Uploaded by
Nelson NgulubeCopyright:
Available Formats
FACULTY OF MEDICINE
DEPARTMENT OF OBSTETRICS AND GYNAECOLOGY
UNIVERSITY EXAMINATIONS JULY 2018
OBGY 310
OBSTETRICS AND GYNAECOLOGY PAPER 1 - OBSTETRICS
12th JULY 2018
TIME: Three Hours TOTAL MARKS: 100
Examiners: Dr C. Mkandawire
INSTRUCTIONS FOR THE WHOLE PAPER
1. Write your computer number on this question paper………………………
2. Time allocated is 3 hours
3. Section 1 contains five (5) short note questions. Answer all five (5).
4. Answer the short notes in the booklet. Begin each answer on a new page.
5. Section 2 contains 50 MCQs each with five (5) stems. Answer all.
6. Answer MCQs on the answer sheet provided. One mark for a correct answer,
zero for a blank and minus half for a wrong answer.
7. Both Section 1 and Section 2 contribute equal marks.
8. This whole question paper should be handed in at the end of the exam
LAMU_MB ChB OBGY310_Finals_Paper 1_Obstetrics. July 2018 Page 1
SECTION 1: SHORT NOTES QUESTIONS:
Write short answers on each of the following:
1. A patient is seen in antenatal clinic at 34 weeks gestation and has a
haemoglobin of 8g/dL
i. What could be the causes of the anaemia in such a pregnant woman?
(1.5marks)
ii. What investigations would you do? (2.5 marks)
iii. What are the suitable ways to increase the haemoglobin in this patient? (3
marks)
iv. How can you minimize blood loss at delivery? (3 marks)
2. A woman at 36 weeks is admitted to hospital. The relatives say she had
convulsed at home and is semi-conscious.
i. What other history should be sought from the relatives? (3 marks)
ii. What examination would help with the differential diagnosis? (3 marks)
iii. What investigations would help with the differential diagnosis? (2 marks)
iv. Briefly describe how the patient should be managed if it is believed to be
eclampsia? (2 marks)
3. A patient is seen in antenatal clinic at 36 weeks gestation and has a height
of fundus of 26 cm.
i. What important questions would you ask on history to help in this case? (2.5
marks)
ii. What important examination findings will assist? (2.5 marks)
iii. What investigations would you do? (2.5 marks)
iv. If it is intrauterine growth restriction, outline briefly the management
antenatally and in labour (2.5 marks)
LAMU_MB ChB OBGY310_Finals_Paper 1_Obstetrics. July 2018 Page 2
4. A 20-year-old primigravida is referred from a clinic because of raised blood
pressure of 180/120mmHg and 3+ proteinuria at 30 weeks gestation.
i. What is the mean arterial blood pressure? (1 mark)
ii. How can you bring the blood pressure down in this emergency? (2.5
marks)
iii. Briefly outline key points in history and examination you would elicit? (4.5
marks)
iv. Briefly outline how she should be managed? (2 marks)
5. Postpartum haemorrhage (PPH)
i. Define postpartum haemorrhage. (1 mark)
ii. What risk factors can you identify that may lead to PPH? (3 marks)
iii. Briefly outline what can be done in anticipation (2 marks)
iv. Briefly describe how you would manage a woman who has just delivered and
has postpartum haemorrhage. (4 marks)
LAMU_MB ChB OBGY310_Finals_Paper 1_Obstetrics. July 2018 Page 3
SECTION 2: MULTIPLE CHOICE QUESTIONS
There are 50 MCQs each with five statements
Answer true (T) or False (F) for each on the answer sheet provided
Negative marking applies as per instructions on front.
1. A pregnant uterus that is larger than the period of amenorrhea could be due to:
A. Generalized edema F
B. Obesity F
C. Wrong dates T
D. Placenta praevia F
E. Polyhydramnios T
2. Maternal cardiovascular and haematological changes in pregnancy
A. the red cell mass decreases F
B. the haemoglobin and white cell count decreases F
C. the erythrocyte sedimentation rate increases T
D. the stroke volume increases T
E. the peripheral resistance and mean arterial pressure decrease T
3. Warning symptoms given to a pregnant woman to look out for include:
A. Bleeding per vagina. T
B. Sudden loss of fluid T
C. Abdominal pain T
D. Excessive salivation (ptyalism) F
E. Body swelling F
4. Regarding iron deficiency anaemia in pregnancy:
A. Iron demand in pregnancy increases in the last 4 weeks of pregnancy F
B. Higher levels of serum ferritin confirm the diagnosis F
C. It is more common in multiple pregnancy T
D. It is usually treated with oral iron T
E. Blood transfusion should be avoided unless it is below 8g/dL T
5. With regards to twin pregnancy
A. Monozygotic twins have similar incidence worldwide F
B. Maternal mortality is significantly increased T
C. Corticosteroids are recommended from 30 weeks gestation T
D. Tocolysis is contraindicated T
E. The second twin should be delivered by caesarean section if it is in a breech
presentation F
LAMU_MB ChB OBGY310_Finals_Paper 1_Obstetrics. July 2018 Page 4
6. The following are signs of premature labor:
A. Increased vaginal discharge. T
B. Regular sustained uterine contractions. T
C. Low back pain. T
D. Cervical dilation to 4 cm. T
E. Worsening pelvic pressure T
7. The risk of premature preterm rupture of the fetal membranes includes:
A. Preeclampsia. F
B. Maternal septicaemia. T
C. Antepartum haemorrhage F
D. Previous premature labour T
E. Cervical cerclage F
8. The following are included in the biophysical profile for the risk assessment of a post-
term fetus:
A. Fetal breathing T
B. Amniotic fluid volume. T
C. Fetal tone. T
D. Contraction stress test (CST) F
E. Fetal size F
9. The following statements regarding eclampsia and its management are correct:
A. It rarely occurs in multiparous patients. F
B. It causes hyper-reflexia. T
C. May occur in absence of hypertension and proteinuria F
D. The maintenance dose of MgSO4 should be increased if urine output is > 100ml/h. F
E. Antidote for MgSO4 is calcium sulfate F
10. The following conditions may predispose to a breech presentation:
A. Hydrocephalus T
B. Contracted pelvis. F
C. Placenta previa T
D. Prematurity T
E. Septate uterus T
LAMU_MB ChB OBGY310_Finals_Paper 1_Obstetrics. July 2018 Page 5
11. Intrauterine death of the fetus is associated with
A. diabetes mellitus F
B. pre-eclampsia T
C. hydrops fetalis T
D. syphilis F
E. chorioamnionitis T
12. Suggestive criteria of intrauterine fetal death include the following:
A. Milk secretion from the breast F
B. Dark brown vaginal discharge T
C. Pregnancy test becomes negative within 24 hours F
D. Spalding's sign on plain X-ray T
E. Hypofibrinogenemia F
13. Placenta praevia
A. is associated with caesarean section T
B. is associated with abnormal lie T
C. may become symptomatic for the first time in labour F
D. is always treated by caesarean section T
E. can predispose to postpartum haemorrhage T
14. Induction of labour can be associated with:
A. Maternal hypernatraemia F?
B. Placental abruption F
C. Uterine rupture T
D. Fetal distress T
E. Postpartum haemorrhage T
15. Chorioamnionitis
A. Is a recognized cause of preterm labour T
B. Does not occur in the absence of maternal pyrexia T
C. Can be prevented using prophylactic antibiotics in preterm premature rupture of
membranes T
D. It is associated with early amniotomy in labour T
E. fetal tachycardia is the first sign F
16. The following conditions are characteristically associated with oligohydramnios:
A. Talipes equinovarus T
B. Fetal imperforate anus F
C. Fetal congenital adrenal hyperplasia F
D. Anencephaly F
E. Fetal renal agenesis T
LAMU_MB ChB OBGY310_Finals_Paper 1_Obstetrics. July 2018 Page 6
17. Polyhydramnios is associated with the following:
A. Chorioangioma of the placenta T
B. Maternal diabetes mellitus T
C. Hydatidiform mole F
D. Hydrops fetalis T
E. Multiple pregnancy T
18. The following statements regarding true labor pains are correct:
A. They are regular T
B. They are relieved by sedation or enema F
C. They are accompanied by cervical dilatation T
D. They may be associated with rupture of membranes T
E. They increase in intensity by time T
19. In relation to the mechanism of labour:
A. Engagement is said to have occurred when the widest part of the presenting part has
passed through the false pelvis. F
B. Restitution occurs after external rotation. F
C. Extension occurs after internal rotation. T
D. Extension occurs at ‘crowning’. T
E. Descent of the fetal head is needed before flexion, internal rotation and extension
can occur. T
20. Regarding face presentation:
A. The presenting diameter is the submento-bregmatic, which is 9.5 cm T
B. It is commonly due to fetal thyroid tumours T
C. The dominator is the chin T
D. The engaging diameter equals the suboccipito bregmatic diameter in length F
E. Mentor posterior easily delivers vaginally F
21. The following regarding cord presentation are correct:
A. Is more common with malpresentations. T
B. May be associated with abnormal shape of the pelvis. F
C. Carries the risk of cord prolapse. T
D. Can be diagnosed by vaginally. T
E. Is associated with rupture of membranes. F
LAMU_MB ChB OBGY310_Finals_Paper 1_Obstetrics. July 2018 Page 7
22. The occipito-posterior position
A. usually turns to deliver as occipito-anterior position T
B. may proceed to deep transverse arrest
C. is associated with a prolonged first stage F
D. is associated with a prolonged second stage T
E. The sub-mental bregmatic diameter presents
23. Vaginal bleeding in the first stage of labour may be due to:
A. Placental abruption. T
B. Cervical fibroids. F
C. Ruptured uterus. F
D. Vaginal trauma. F
E. Vasa praevia. T
24. Management of intrapartum acute fetal distress includes the following:
A. Oxygen administration T
B. Change of maternal position F
C. Fetal heart monitoring every 5 minutes F
D. Correction of maternal hypotension T
E. Instrumental delivery T
25. Predisposing factors for uterine atony include the following:
A. Low parity F
B. Preeclampsia F
C. Precipitous labor T
D. Oligohydramnios F
E. Multiple pregnancy T
26. Active management of the third stage of labour
A. involves the Mathews-Duncan method F
B. requires intravenous syntocinon T
C. increases the risk that a manual removal of placenta will be needed F
D. increases the likelihood of postpartum haemorrhage F
E. begins with delivery of the fetal trunk F
27. Management of shoulder dystocia may include the following procedures:
A. Vigorous fundal pressure. F
B. Corkscrew rotation of the shoulders. T
C. Generous episiotomy T
D. Shoulder girdle rotation into one of the oblique diameters of the pelvis. T
E. McRobert’s manoeuvre T
LAMU_MB ChB OBGY310_Finals_Paper 1_Obstetrics. July 2018 Page 8
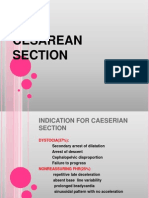
28. Advantages of lower segment caesarean section over upper segment caesarean
section include the following:
A. Less bleeding unless extended T
B. Less paralytic ileus. T
C. Used if there are pelvic adhesions. F
D. Less incidence of subsequent uterine rupture. T
E. Less infection F
29. The following are prerequisites for instrumental delivery:
A. Head must be engaged. T
B. Fetus must present either by the vertex or by the face with the chin posterior. F
C. Cervix must be completely dilated. T
D. Membranes must be ruptured. T
E. Bladder must be empty T
30. The following complications are more likely after caesarean section than after vaginal
delivery:
A. Pulmonary embolism. T
B. Secondary postpartum haemorrhage. T
C. Postnatal depression. T
D. Amniotic fluid embolism. T
E. Infection. T
31. Puerperal pyrexia
A. usually appears 48 - 60 hours after delivery F
B. is usually due to breast engorgement F
C. is a notifiable disease F
D. is a significant cause of maternal mortality F
E. is usually due to Chlamydia F
32. Postpartum haemorrhage
A. It is less likely if oxytocics are administered routinely in the third stage of labour T
B. Is primarily if it occurs within in the first 12 hours F
C. Is common after both placenta previa and abruption placentae T
D. May require manual removal of placenta T
E. Bleeding disorders are a common cause T
LAMU_MB ChB OBGY310_Finals_Paper 1_Obstetrics. July 2018 Page 9
33. A pregnant patient 36 weeks gestation comes in with painless vaginal bleeding,
moderate in amount, and her vitals are stable. The following should be done
A. Immediate caesarean section F
B. Fluid replacement and send serum for blood cross-match F
C. Perform ultrasound if available T
D. Put the patient under observation T
E. Start blood transfusion immediately F
34. During lactation
A. progesterone promotes growth of ducts rather than alveoli
B. oestrogens inhibit the lactogenic effect of prolactin
C prolactin secretion increases in the early puerperium T
D. prolactin causes milk ejection F
E. oxytocin causes milk ejection T
35. The following applies to antenatal visits
A. Focused antenatal care requires at least 6 antenatal visits. F
B. It is not necessary to test the blood pressure at every antenatal visit. F
C. A pelvic examination is essential in antenatal clinics to confirm early pregnancy. F
D. All pregnant women should have an HIV test. T
E. Prophylactic antimalarials and haematinics should be provided in antenatal clinic. T
36. Regarding pre-eclampsia or pregnancy induced hypertension
A. It only occurs in the primigravida. F
B. The presence of a fetus is not essential to the development of the disease. F
C. Platelet counts are reduced T
D. Pregnancy should not be terminated before 40 weeks of pregnancy. F
E. Acute renal failure is a well-known complication. T
37. Drugs used in pregnancy hypertension.
A. A bolus of intravenous hydralazine every 15 minutes is used in acute hypertension in
pregnancy. T
B. Labetalol is the preferred choice of antihypertensive in pregnancy. T
C. Magnesium sulfate can be used to control hypertension in eclampsia. F
D. Magnesium sulfate only prevents recurrent convulsions in eclampsia within 24
hours. F
E. Calcium carbonate can be used to reverse magnesium sulfate toxicity. F
LAMU_MB ChB OBGY310_Finals_Paper 1_Obstetrics. July 2018 Page 10
38. Preterm premature rupture of membranes (PPROM)
A. Can recur if there is a history of PPROM T
B. Delivery should be expedited F
C. Maternal antibiotics prolongs onset of labour F
D. Is commoner in multiple pregnancies T
E. A speculum examination should be done T
39. Regarding Dizygotic twining;
A. Twin to twin transfusion phenomenon is a common complication F
B. The incidence is constant worldwide. F
C. Twin one is always bigger than twin two. F
D. Twins may appear identical F
E. May arise from one fertilized ovum F
40. HIV and pregnancy
A. An HIV test is compulsory during the antenatal period T
B. Combined antiretroviral therapy (cART) is only commenced after 28 weeks F
C. For an unbooked woman in labour, if found HIV positive cART is commenced after
delivery F
D. A woman may wish to discontinue cART after delivery and breastfeeding F
E. An infant should be on nevirapine as long as it is breastfed T
41. Fibroids in pregnancy
A. Fibroids can cause infertility T
B. Red degeneration of a fibroid in pregnancy is an indication for early delivery. F
C. Fibroids found at caesarean section should not be removed. T
D. A history of myomectomy is an automatic indication for caesarean section. T
E. Postpartum haemorrhage is commonly associated with a fibroid uterus. T
42. Regarding a small for dates baby
A. An error in gestational age may be the cause. T
B. A chromosomal abnormality is an association. T
C. Uteroplacental insufficiency is a common cause. T
D. Can occur in a small woman. T
E. In a growth restricted baby, caesarean section is the preferred mode of delivery. F
LAMU_MB ChB OBGY310_Finals_Paper 1_Obstetrics. July 2018 Page 11
43. Regarding vaginal breech delivery:
A. Arrest of the after coming head occurs can occur in preterm T
B. Artificial rupture of the membranes is recommended in the early stages of labour. F
C. Respiratory distress is commoner in babies born by caesarean section. F
D. preterm breech should always be delivered by Caesarean section. F
E. Ultrasound is the best diagnostic tool in deciding which breech presentations may be
permitted to deliver vaginally. T
44. In antepartum haemorrhage
A. an aetiological factor for placenta praevia is uterine fibroid F
B. the most accurate method of diagnosing placenta praevia is by digital examination F
C. the length of the umbilical cord has a bearing on the aetiology of abruption placentae T
D. there is no place for conservative management in abruptio placentae T
E. vasa praevia can never be diagnosed before delivery F
45. Vaginal delivery is contraindicated in the presence of:
A. transverse lie of the second twin. F
B. central placenta praevia with a dead fetus at 28 weeks. T
C. previous caesarean section for cephalopelvic disproportion. F
D. cord prolapse in the second stage of labour. T
E. gastroschisis. F
46. When delivering a second twin vaginally
A. Oxytocin is contraindicated T
B. Malpresentation is common T
C. If transverse lie internal podalic version is an option T
D. The membranes must be allowed to rupture spontaneously F
E. If cephalic presentation, a forceps or ventouse can be used T
47. In antepartum haemorrhage
A. an aetiological factor for placenta praevia is uterine fibroid F
B. the most accurate method of diagnosing placenta praevia is by digital examination F
C. the length of the umbilical cord has no bearing on the aetiology of abruption
placentae F
D. there is no place for conservative management in abruptio placentae T
E. vasa praevia can never be diagnosed before delivery F
LAMU_MB ChB OBGY310_Finals_Paper 1_Obstetrics. July 2018 Page 12
48. Malaria in pregnancy
A. Placenta is the preferred site of sequestration and development of malaria parasite T
B. Anaemia due to malaria is more common and severe between 16-29 weeks.
C. Regarding anaemia, it is better to transfuse whole blood than packed cells. T
D. Acute pulmonary oedema is a less common complication of malaria in pregnancy
compared to the non-pregnant population F
E. Intermittent presumptive treatment can equally use quinine. T
49. Regarding post term pregnancies
A. The standard of definition of post term pregnancy is 40 weeks or more T
B. Post term pregnancies are commoner in first pregnancies F
C. The risk of post term pregnancy is substantially increased if the first birth was post
term T
D. Meconium aspiration is a known complication op post term neonates T
E. Pregnancies must be induced by 42 completed weeks gestation F
50. Side-effects of oxytocin include:
A. fetal distress. T
B. hypernatraemia.
C. amniotic fluid embolism.
D. uterine rupture.
E. hyperprolactinaemia.
End of Examination
LAMU_MB ChB OBGY310_Finals_Paper 1_Obstetrics. July 2018 Page 13
You might also like
- NCLEX: Pharmacology for Nurses: 100 Practice Questions with Rationales to help you Pass the NCLEX!From EverandNCLEX: Pharmacology for Nurses: 100 Practice Questions with Rationales to help you Pass the NCLEX!Rating: 5 out of 5 stars5/5 (4)
- Management of Labor and DeliveryFrom EverandManagement of Labor and DeliveryGeorge A. MaconesNo ratings yet
- Assisted Reproductive Techniques For Class 12 Investigatory ProjectDocument9 pagesAssisted Reproductive Techniques For Class 12 Investigatory Projectjerusha50% (6)
- Case Study On Breech BirthDocument65 pagesCase Study On Breech BirthSujan Shrestha94% (32)
- CP102B FinalsDocument6 pagesCP102B FinalsAldrin Riel BoyanoNo ratings yet
- Obstetrics and Gynecology Review QuestionsDocument11 pagesObstetrics and Gynecology Review QuestionsnoblefxNo ratings yet
- Polyhydramnios and Oligohydramnios - Background, Pathophysiology, EtiologyDocument4 pagesPolyhydramnios and Oligohydramnios - Background, Pathophysiology, EtiologyAhmad FahroziNo ratings yet
- Ob &gyDocument6 pagesOb &gyThumz ThuminNo ratings yet
- Obstetrics Evidence-Based Algorithms, 2016Document351 pagesObstetrics Evidence-Based Algorithms, 2016stase anak80% (5)
- Test Drill OBDocument8 pagesTest Drill OBViviane Ńíáshéè Basod100% (1)
- Assisted Reproductive TechnologyDocument14 pagesAssisted Reproductive Technologyarchana jainNo ratings yet
- Postpartum QuestionsDocument100 pagesPostpartum QuestionswickwaxNo ratings yet
- ComplicationsDocument22 pagesComplicationsLyra LoonNo ratings yet
- Obstructed LabourDocument15 pagesObstructed LaboursunilNo ratings yet
- ObstetricsDocument46 pagesObstetricsanaskabaha100% (3)
- Obstetrics and Gynecology Mock ReviewDocument14 pagesObstetrics and Gynecology Mock ReviewokurimkuriNo ratings yet
- Maternal ExamsDocument37 pagesMaternal ExamsMarianne Baquilala100% (2)
- BreechDocument38 pagesBreechsanthiyasandy100% (2)
- Ob QuestionsDocument7 pagesOb Questionslbordonada100% (1)
- Maternity NursingDocument24 pagesMaternity NursingJen Arcillas Tuble - Iledan100% (1)
- Medical School Companion Obstetrics and Gynecology Practice Question BookFrom EverandMedical School Companion Obstetrics and Gynecology Practice Question BookNo ratings yet
- Multiple Choice Questions in Paediatric SurgeryFrom EverandMultiple Choice Questions in Paediatric SurgeryRating: 1 out of 5 stars1/5 (1)
- Types of AbortionDocument2 pagesTypes of AbortionMaako MonteverdeNo ratings yet
- PNLE Sample Test QuestionsDocument12 pagesPNLE Sample Test QuestionsHam-Ham LootNo ratings yet
- Maternal and Child Health Nursing Practice Questions With RationaleDocument76 pagesMaternal and Child Health Nursing Practice Questions With RationaleLrak Eed93% (30)
- Maternal Multiple Choice QuestionsDocument3 pagesMaternal Multiple Choice QuestionsDani Michaela100% (1)
- 11 16Document27 pages11 16Iful SaifullahNo ratings yet
- Cesarean SectionDocument42 pagesCesarean SectionP Kasikrishnaraja100% (1)
- Obgy QN BNKDocument21 pagesObgy QN BNKZemen addiss100% (1)
- Maternal and Child Health Pracice Test 1-2-3Document84 pagesMaternal and Child Health Pracice Test 1-2-3chuppepay100% (1)
- Review Questions On MCHNDocument42 pagesReview Questions On MCHNprokuno100% (30)
- MCNDocument23 pagesMCNJASTINE NICOLE SABORNIDONo ratings yet
- Maternal and Child HealthDocument28 pagesMaternal and Child Health지창욱No ratings yet
- Dental Management of the Pregnant PatientFrom EverandDental Management of the Pregnant PatientChristos A. SkouterisNo ratings yet
- Ob 1Document13 pagesOb 1iandame100% (1)
- Ob RN 1Document47 pagesOb RN 1zenaNo ratings yet
- Soal MCQ UNSRI 2009Document18 pagesSoal MCQ UNSRI 2009SuzetteNo ratings yet
- MCN 1Document9 pagesMCN 1Margarita RemolloNo ratings yet
- Midwive COC EXAMDocument21 pagesMidwive COC EXAManteneh100% (1)
- Question 3Document19 pagesQuestion 3Anonymous LF9aizGhaNo ratings yet
- MCN Test BankDocument10 pagesMCN Test BankMho Pimentel Vanguardia100% (1)
- Maternal and Child Nursing QuestionsDocument87 pagesMaternal and Child Nursing QuestionsAnn Michelle Tarrobago50% (2)
- p1 Exam FinalDocument21 pagesp1 Exam FinalLeevine DelimaNo ratings yet
- مهم اسئلةDocument19 pagesمهم اسئلةnada elfarraNo ratings yet
- Care of Mother and Child (Well-Client)Document67 pagesCare of Mother and Child (Well-Client)Jake Padua100% (2)
- NMC Exams Past Questions 24 of 24Document105 pagesNMC Exams Past Questions 24 of 24Petrina AmoahNo ratings yet
- P2 Gyn 4Document13 pagesP2 Gyn 4Nelson NgulubeNo ratings yet
- Exit Exam WolaytaDocument18 pagesExit Exam WolaytaMilkii Du Nikus100% (1)
- For PMCDocument14 pagesFor PMCRawanNo ratings yet
- B. ThelarcheDocument12 pagesB. ThelarchecjrurNo ratings yet
- Ob Pathological 2 - Multiple ChoiceDocument9 pagesOb Pathological 2 - Multiple ChoiceFerdinand Sherwin MorataNo ratings yet
- Apex Paper 1 Obstetrics Final ExamDocument15 pagesApex Paper 1 Obstetrics Final ExamNelson NgulubeNo ratings yet
- Crash Course FinalDocument6 pagesCrash Course FinalAbdikadir AhmedNo ratings yet
- Maternal and Child Health Practice Test Part 1Document12 pagesMaternal and Child Health Practice Test Part 1Spislgal PhilipNo ratings yet
- شامل متيرنتي 2012Document10 pagesشامل متيرنتي 2012Ayah NaemNo ratings yet
- All Reviewers For Maternal 2Document96 pagesAll Reviewers For Maternal 2Divo SkyeNo ratings yet
- Gyna B 1517305798 PDFDocument12 pagesGyna B 1517305798 PDFMohammed AhmedNo ratings yet
- ERPM RevisionDocument7 pagesERPM RevisionNalin Abeysinghe100% (1)
- Maternal QuestionsDocument7 pagesMaternal Questionsjhae_darilayNo ratings yet
- Medicine Colloquium Exam - 2019 ADocument39 pagesMedicine Colloquium Exam - 2019 ArachaNo ratings yet
- PENTING!!!!!Document18 pagesPENTING!!!!!Kevin NoyaNo ratings yet
- ReviewerDocument9 pagesReviewerAndRenNo ratings yet
- Duty Ob ExamDocument3 pagesDuty Ob ExamKATHERINE GRACE JOSENo ratings yet
- Comprehensive Jima-2Document21 pagesComprehensive Jima-2Milkii Du NikusNo ratings yet
- Soal-Soal PretesDocument8 pagesSoal-Soal Pretespoker011007No ratings yet
- MCN Drill 1Document23 pagesMCN Drill 1Cai Velasco DecenaNo ratings yet
- Gyna Exams DR - Moh.ramadanDocument93 pagesGyna Exams DR - Moh.ramadanMahmoud AbouelsoudNo ratings yet
- AbortionDocument8 pagesAbortionJenny Rose GriñoNo ratings yet
- Diagnostic Features of Disease: Based on French's Index of Differential DiagnosisFrom EverandDiagnostic Features of Disease: Based on French's Index of Differential DiagnosisRating: 1 out of 5 stars1/5 (1)
- RNSG 2504 TPAL ExamplesDocument1 pageRNSG 2504 TPAL ExamplesJohn Christopher JosolNo ratings yet
- Preterm Labor and Postterm PregnancyDocument33 pagesPreterm Labor and Postterm PregnancySteven IrvingNo ratings yet
- Nle QuestionsDocument2 pagesNle Questionsrandz c thinksNo ratings yet
- Inj July 2010Document37 pagesInj July 2010TamilNurse.comNo ratings yet
- Assignment Front PageDocument6 pagesAssignment Front PageAjay DNo ratings yet
- Postnatal - Care On Admission To The Ward PDFDocument3 pagesPostnatal - Care On Admission To The Ward PDFHellenKyakuwaireNo ratings yet
- Antepartum HemorrhageDocument52 pagesAntepartum HemorrhageKomalah ChenasammyNo ratings yet
- Daftar Pustaka 3Document8 pagesDaftar Pustaka 3Marsela Renasari PrestyNo ratings yet
- 2008 Gomez Ut Artery PIDocument5 pages2008 Gomez Ut Artery PIRibeiro SáNo ratings yet
- Trifan Bianca Maria 802745329Document2 pagesTrifan Bianca Maria 802745329trifanbianca20.11.2003No ratings yet
- 1 Products of Conception - Libre PathologyDocument8 pages1 Products of Conception - Libre PathologyfadoNo ratings yet
- 2-Post TermDocument13 pages2-Post TermAbc DefNo ratings yet
- Labor Curve and PartographDocument50 pagesLabor Curve and PartographJhervy VillanuevaNo ratings yet
- Group Health Presentation: Trademor Marketing (PVT) LimitedDocument32 pagesGroup Health Presentation: Trademor Marketing (PVT) Limitedkhinsha mujahidNo ratings yet
- New Vision University Syllabus: 1. General InformationDocument11 pagesNew Vision University Syllabus: 1. General InformationkharaNo ratings yet
- Health Education For Record BookDocument24 pagesHealth Education For Record BookRoselineTiggaNo ratings yet
- Infertility PDFDocument3 pagesInfertility PDFdharshiniNo ratings yet
- Polyhydramnios CASE STUDY: Download NowDocument14 pagesPolyhydramnios CASE STUDY: Download NowJv LalparaNo ratings yet
- PartographDocument4 pagesPartographElonah Gien DimalaluanNo ratings yet
- 2017.104 - The - Leopold - Maneuver - PosterDocument1 page2017.104 - The - Leopold - Maneuver - PosterRey CelNo ratings yet