Professional Documents
Culture Documents
Toxicología Veterinaria
Toxicología Veterinaria
Uploaded by
Catalina Petrel0 ratings0% found this document useful (0 votes)
4 views5 pagesOriginal Title
Toxicología veterinaria
Copyright
© © All Rights Reserved
Available Formats
PDF or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
0 ratings0% found this document useful (0 votes)
4 views5 pagesToxicología Veterinaria
Toxicología Veterinaria
Uploaded by
Catalina PetrelCopyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
You are on page 1of 5
Bs @, ALOOHOLS AND GLYG:
resulting in lactic acidosis. Almost all propylene glycol is
‘metabolized within 24h of ingestion,
Diagnosis and treatment
(Clinical signs depend on the quantity ingested and may
include depression, ataxia, muscle fasciculations, hypo-
tension, osmotic diuresis, respiratory arrest, and circula
tory collapse, Clinical signs in ruminants are similar to
those seen in other species and include ataxia, depres
sion, and recumbency (Pintchuck eal, 1993). Laboratory
findings include metabolic acidosis, increased anion gap,
and hyperosmolality of the plasma and the presence of
Heinz bodies in cats and horses. Diagnosis is usually
based on history of exposure and can be confirmed by
measuring propylene glycol concentrations in urine and
serum by gas chromatography. Treatment forall species
is supportive and includes correction of hydration and
acid-base abnormalities,
Butylene glycol toxicosis,
Butylene glycol (12, 13, and 14-butanediol) has the
structural formula C\H,O; and a molecular weight of
90 Da, Butylene glycol is used as antifreeze, as an ind
trial cleaner, and in cosmetics. It is also a component of
polyurethane and is used to make Spandex. Although no
published reports of butylene glycol toxicosis in domestic
Animals were found in the literature, there are numerous
reports of human intoxications from butylene glycol or the
metabolite gamma-hydroxybutyrate (Dyer, 1991; Mack,
1983). Butylene glycol and the metabolite gamma-hydroxy-
butyrate ate used as “recreational” drugs and were once
‘marketed by health food stores asa food additive for body-
builders anc to treat depression and insomnia,
1,3-Butanediol has been used as an antidote for exper:
mental EG toxicosis in dogs because itis a competitive
substrate for ADH (Taal eal, 1982; Murphy et al, 1984
Cox etal, 1992) Although it was found to be a more effec
tive antidote than ethanol, in that more unmetabolized
FG was excreted in the urine in patients treated with
1 a-butanediol, CNS depression was as severe of more
severe than that induced by ethanol therapy, and plasma
hyperosmolality and metabolic acidosis were more severe
than with ethanol therapy (Thrall ¢ al, 1982)
Toxicokinetics
Butylene glyco! is metabolized by ADH to acetoacetate and
-gamma-hydroxybutyrate, the so-called “date rape” drug,
Mechanism of action
Butylene glycol is @ CNS depressant much like ethanol,
due to the effect of the gamma-hydroxybutyrate on the
NS, and in large quantities can result in seizures and.
respiratory arrest
Treatment
‘Therapy for butylene glycol toxicosis in humans is sup.
portive, similar to therapy for ethanol toxicosis.
yylene glycol toxicosis
EG has the structural formula C,H,0; and a molecular
weight of 62 Da. EG is used primarily as an antifreeze
and windshield devicing agent. Its small molecular
weight makes it very effective in lowering the freezing
point of water. EG is also used as a cryoprotectant for
embryo preservation; in the manufacture of polyester
compounds; a8 a solvent in the paint and plastic indus
tries; and as an ingredient in photographie developing.
solutions, hydraulic brake fluid and motor oil, and inks
and wood stains (Davis et al, 1997). The most readily
available source of EG in the home is antifreeze solu
tions, which consist of approximately 95% EC.
Texicokineties
Unlike the other alcohols (with the exception of metha-
nol in primates) and glycols, the metabolites of EG are
very toxic. EG is initially oxidized to glycoaldehyde by
ADH, and glycoaldenyde is then oxidized to glycolic
acid and then to glyoxylie acid. Glyoxylie acid is prima
rily converted to oxalie acid but may follow several met-
abolic pathways; end produets may also include glycine,
formic acid, hippuric acid, oxalomalie acid, and benzoic
acid. Calcium is bound t© oxalic acid, resulting in cal-
cium oxalate crystal formation, Calcium oxalate crystal
deposition is widespread but is most severe in the kid-
ney, and crystalluria is a consistent finding in animals
producing urine (Grauer eal, 1984; Thrall et al, 1984)
Mechanism of action
EG per se has no major effects other than GI irrita-
tion and increased serum. osmolality. Glycoaldehyde,
the first metabolite, is thought to be primarily respon-
sible for CNS dysfunction; respiration, glucose, and
serotonin metabolism are depressed; and CNS amine
concentrations are altered (Parry and Wallach, 1974;
Gordon and Hunter, 1982). Hypocaleemia secondary
to caleium oxalate deposition may contribute to CNS
signs, although the concurrent metabolic acidosis shifts
calcism to the ionized active state, reducing the chances
of hypocaleemia-associated clinical signs. Acidosis
is also thought to lead to altered levels of conscious
ness and cerebral damage. Most of the metabolites are
very eytotoxie to renal tubular epithelium, and some
‘GLYCOL TOMIOOSES| 739
renal epithelial and interstitial damage may be associ
ated with caleium oxalate crystal formation within the
renal tubules (de Water eal, 1999). Renal epithelial cell,
death appears to be due primarily to destruction of cyto-
plasmic organelles, especially mitochondria (Bachman
and Goldberg, 1971). Metabolic acidosis is often severe
and has a deleterious effect on multiple organ systems
Glycolic acid accumulation is the primary cause of
the metabolic acidosis associated with EG intoxication
acobsen ef al, 1984), although other acid metabolites
also contribute. Glycolic acid accumulates because the
lactic dehydrogenase enzyme that metabolizes glycolic
to glyoxylic acid becomes saturated
Toxicity
Before it is metabolized, EG is no more toxic than etha-
nol, although FG is a more potent CNS depressant
than ethanol (Berger and Ayyar, 1981). However, EG is
biotransformed to highly toxic metabolites that result in
severe metabolic acidosis and acute renal failure, hall
marks of EG poisoning (Thrall etal, 1984b; Dial etal,
1994a,b; Davis ef al, 1997). The minimum lethal dose
of undiluted EG is 6 mL/kg in the dog (Kersting and
Nielson, 1956) and 1.51aL./kg in the cat (Milles, 1946)
Clinical signs
Clinical signs ate dose dependent and can be divided into
those caused by unmetabolized EG and those caused by
its toxic metabolites, The onset of clinical signe is almost
always acute. Early clinical signs are usually observed
30min after ingestion and often last until approximately
Dh after ingestion; they are primarily associated with
EG-induced gastric irritation and high EG blood con-
centrations. These signs commonly include nausea and
vomiting, CNS depression, ataxia and knuckling, muscle
fasciculations, decteased withdrawal reflexes and righting.
ability, Aypothermia, and osmotic diuresis with resultant
polyuria and polydipsia (Grauer etal, 1984; Thrall etal,
198db; Connally etal, 1996). As CNS depression increases
in severity, dogs drink less but osmotic diuresis persists,
resulting in dehydration. In dogs, CNS signs abate after
approximately 12h, and patients may briefly appear to
have recovered, Cats usually remain markedly depressed
and do not exhibit polydipsia, Animals may be severely
hypothermic, particularly if housed outside during the
winter months. Clinical signs associated with the toxic
metabolites are primarily related to oliguric renal failure,
Which is evident by 35-72h following ingestion in dogs
and by 12-26h following ingestion in cats. Clinical signe
may include severe lethargy or coma, seizures, anorexia,
vomiting, oral uleers and salivation, and oliguria with iso
sthenuria, Anuria often develops 72-96h after ingestion
The kidneys are often swollen and painful, particularly
incats
Early laboratory abnormalities
Abnormal laboratory findings can also be divided into
those associated with early EG intoxication, which may
bbe related to the presence of EG per se oF to its toxic
metabolites, and those associated with late EG intox!-
cation, most of which are related to renal failure. Early
abnormalities are primarily due to the presence of acid
metabolites of EG in the serum that result in metabolic
acidosis and inchide decreased plasma bicarbonate
concentration and increased anion gap. In addition,
hyperphosphatemia may occur due to ingestion of a.
phosphate rust inhibitor present in some commercial
antifreeze products (Grauer «tal, 1984; Connally et al,
1996). The decreased plasma bicarbonate (HCO) con
centration can be seen as early as 1h following EG inges-
tion. Metabolites of EG significantly increase the pool of
tunmeasured anions and cause an increased anion gap.
The anion gap is increased by Sh after ingestion, peaks
at 6h after EG concentration, which peaks 1-6h follow
ing ingestion, and EG is usually no longer detectable in
the serum or urine 48-72h after ingestion (Thrall etal,
1982; Grauer ef al, 1984; Dial ef al, 1994a,b). Kits (eg.
Ethylene Glycol Test Kit, PRN Pharmacol, Pensacola,
FL) are available that accurately estimate blood EG.
concentrations with a minimum detection limit of
50mg/dl, and the results correlate well with other
established methods of measuring EG concentrations
such as gat chromatography (Dasgupta eal, 1995),
although the presence of propylene glycol or glycerol
in the blood may cause a false-positive test reaction,
Ethanol and methanol do not result in a false-positive
test result. Cats may be intoxicated with a lethal dose of
EG that is below the 50mg/dL. detectable level of the EG
test kt. Therefore, if the test kit is negative and historical
findings as well as clinical signs are compatible with EG.
ingestion, the recommendation isto initiate appropriate
therapy for EG intoxication as well as submit a serum,
sample to a reference laboratory capable of determining.
a quantitative concentration
Determination of serum osmolality is also useful for
diagnosing early EG toxicosis, although other osmoti-
cally active, low-molecular-weight alcohols and glycols
also increase serum osmolality (Ammar and Heckerling,
1996), Seram osmolality is increased by 1h alter inges-
tion of EG, increasing in parallel with serum E
centrations (Dial et al, 1994a,b). When measured serum.
osmolality (by osmometzy) is compared to calculated.
serum osmolality, the difference is referred to as the
fosmole or osmolal gap. If calculated osmolality is not
provided on the biochemical profile printout, osmolal
ity in mOsm/kg may be calculated using the following,
formula
1.85 (Na” +K°) + glucose /18 + BUN/28 ~
740 @, ALOOHOLS AND GLYG:
Normal serum osmolality is 280-S10mOsm/kg, and the
normal osmole gap is less than 10mOsm/kg, Serum osmo
Inlity as high as 450mOsm/kg. and an esmole gap as high
a5 150mOsm kg may be seen 3h aftr ingestion, depen!
ing on the quantity of antifreeze ingested (Jacobsen # al,
1982b; Grauer eal, 198). Both the gap and the measured
osmolality may remain signiicanly high for approx
mately 18h after ingestion. Multiplication of the osmole
zap by 5 yields an approximate serum FC concentration in
sg/Al. (@urkhart and Kulig, 19%), Fach 100mg/l incre
rent increase in EG concentration contributes approx:
rately 16mOsm/kg 1,0 to the serum osmolality (Eder
ctl, 1988), Simultaneous or sequental increases in esmole
and anion gaps are very suggestive of BG intoxication
AAs EG is metabolized, its contribution to the osmole gap
diminishes because the accumulating negatively charged
retabolites do not contribute to the osmole gap (Eder
tal, 1998) Two types of instruments are used to measure
cosmolalty ~ feering point cemometers and vapor pres
sure osmometers. Because BG ie nonvolatile (boing point,
197°), tis detected by either the freezing point or vapor
pressure methods. However, methanol, ethanal, and other
‘Volatile compounds although conteibuting to serum osmo
Inlity may go undetected if assayed by the vapor pressure
method. Most clinical laboratories use the freezing point
method (Kruse and Cadnapaphorncha, 199). Osmolality
can be measured using serum or plain; if the latter is
‘used, heparin isthe preferred anticoagulant. Other antico
agulants, such as EDTA, can markedly increase osmolal-
sty and can result im spurious increases in the osmole gp
(Krse and Cadnapaphornchai, 1991),
Dogs are issthenuri (urine specific gravity of 1.008
1.012) by 3 following ingestion of EG due to osmotic
diuresis and serum hyperosmolality-induced polydipsio
(Grauer al, 1984; Dale al, 1994). The urine specific
gravity in cats is also decreased by 3h after ingestion but
‘may be above the isosthenutic range (Dial e al, 19946;
Fogazz, 1996). Calcium oxalate crystalluria is 3 com
‘mon finding and may be observed as early as 3 and
6h after ingestion inthe eat and dog, respectively, 35 2
result of oxalic acid combining with calcium (Dial al,
19943,5) Calcium oxalate monohydrate erystals ae vari
ably sized, clea, sb-sided prisms (Figure 601) (Seully
fa, 1979; Godolphin eal, 1980; Teeinsky etal, 1981;
Jacobsen ef al, 19828; Kramer etal, 1984; Foi eal, 1985;
Thrall al, 1985; Steinhart, 1990). In animals and people
poisoned with EG, the monohydrate form is observed
rote frequently than the dihydrate form, which appears
a5 an envelope or Maltese cross (Connally eta, 1996;
dere al, 1998). Dumbbell or sheafshaped crystals are
cbserved infrequently. The detection of calcium oxalate
cryatalluria, particularly the monohydrate form, pro:
vides strong Supporting evidence for the diagnosis of
EG poisoning (Fogszzi, 1995). Urinary pH consistently
decreases following EG ingestion,
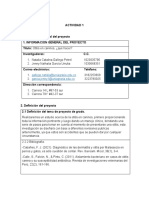
FIGURE 60.1 Calcium oxste monchye
ined light) fom 3 dog with EG toxiosie
te cystals (pola
Another diagnostic procedure that may be helpful in
detecting early EG intoxication is examination ofthe oral
cavity, face, paws, vomitus, and urine with a Wood's
lamp to determine whether they appear fluorescent
Many antifreeze solutions manufactured today contain
sodium fluorescein, a fluorescent dye that aids in the
detection of leaks in vehicle coolant systems. The dye is
excreted in the urine for up to 6h following ingestion of
the antifreeze (Winter ef al, 1990). A negative test does
not eliminate the possibility of EG ingestion because not
all antifreeze solutions contain the dye
Late laboratory abnormalities
With the onset of renal damage and subsequent
decreased glomerular filtration, serum creatinine and
blood urea nitrogen (BUN) concentrations increase. In
the dog, these increases begin to occur between 24 and
48h following EG ingestion. In the cat, BUN and creati-
nine begin to increase approximately 12h after ingestion;
however, because cats do not develop polydipsia, this
may be in part due to dehydration, Serum phosphorus
concentrations increase at this time due to decreased
glomerular filtration. Hyperkalemia develops with the
onset of oliguria and anuria. Serum calcium concen-
tration is decreased in approximately half of patients
(Thrall etal, 1984b; Connally et al, 1996) and is due to
formation of insoluble calcium oxalate. Clinical signs
fof hypocalcemia are infrequently observed because
acidosis results in a shift to the ionized, physiologi-
cally active form of caleium, Serum glucose concentra
tion is increased in approximately 50% of dogs and cats
(Thrall ef al, 1984; Connally ef al, 1996) and is attrib
uted to inhibition of glucose metabolism by aldehydes,
increased epinephrine and endogenous corticosteroids,
and uremia, Animals presenting with late EG poison-
ing are likely to have little or no osmole gap inerease but
will have an increased osmolality (whether calculated or
‘GLYOOL TOXIGOSES v4
measured) because of the azotemia and hyperglycemia,
Animals remain isosthenuric in the later stages of toxico-
sis due to renal dysfunction and impaired ability to con-
centrate urine, Calcium oxalate crystalluria persists for
as long as animals are producing urine. Urine abnormali-
ties associated with renal damage may include hematu-
ria, proteinuria, and glucosuria. Granular and cellular
casts, white blood cells, red blood cells, and renal epi-
thelial cells may be observed in the sediment of some
patients (Thrall etal, 1984b; Connally etal, 1996),
Treatment
‘Therapy for EG poisoning is aimed at preventing
absorption, increasing excretion, and preventing metab-
olism of EG. Supportive care to correct fluid, acid-base,
and electrolyte imbalances is also helpful, Although ther:
apeutic recommendations have traditionally included
Induetion of vomiting, gastric lavage, and administra-
tion of activated charcoal (Thrall eta, 1995, 1998), i is
likely that these procedures are not beneficial because
of the rapidity with which EG is absorbed (Davis etal,
1997), The most critical aspect of therapy is based
fon prevention of EG oxidation by ADI, the enzyme
responsible for the initial reaction in the EG metabolic
pathway (Parry and Wallach, 1974), Typically, dogs must
be treated within 8h following ingestion and cats must
be treated within 3h for teatment to be successful (Dial
al, 1994a,6). However, this is somewhat dependent on.
the amount of EG ingested. Historically, teating EG toxi-
cosis has been directed toward inhibiting BC: metabolism
with ethanol, 2 competitive substrate that has a higher
affinity for ADH than EG (Penumarthy and Oehme,
1975; Bostrom and Li, 1980), Ethanol has numerous dis
advantages because it enhances many of the metabolic
effects of EG, Both ethanol and EG are CNS depressants,
and its the compounded CNS depression that most lim-
its the usefulness of ethanol as an antidote. Additional
disadvantages of ethanol treatment include its metabo-
lism to acetaldehyde, which impairs glucose metabo-
lism and is a cerebral iritant. Ethanol also contributes to
‘metabolic acidosis by enhancing the formation of lactic
acid from pyruvate and may potentiate hypocalcemia
(Money et al, 1989). Moreover, ethanol compounds the
effects of EG induced osmotic diuresis and serum hyper
osmolality (Kruse and Cadnapaphornchai, 1994),
“{Methylpyrazole (fomepizole) has become the pre:
ferred antidote in dogs (Grauet etal, 1987; Dial eta, 1989;
Connally e a, 1996) and cats (Thrall etal, 2008; Connally
«tal, 2010). Fomepizole is an ADH inhibitor, not a competi-
tive substrate, and it does not induce CNS depression (in
dogs), diuresis, or hyperosmolality at the recommended
dosage. The recommended dose of fomepizole for dogs is
20mg/kg body weight ix initially, followed by 15mg/kg,
iv. at 12 and 24h and Smg/kg iv. at 36h (Grover eal,
1987; Connally e al, 1996; Tal etal, 2006), Cats must be
given a much higher dose of fomepizole than dogs because
feline ADH is less effectively inhibited by fomepizole than,
is canine ADH (Connally etal, 2000, 2010). Cats are ini-
tially treated with 125mg/kg fomepizole iv. fllowed by
31.25mq/kg ix: fomepizole at 12, 24, and 36h. The only
adverse clinical sign that the authors have observed is
CNS depression that appears to be fomepizole related
(Connally etal, 2010). If ingestion of a large dose of EG
is suspected, repeating serum quantification tests can be
performed to determine whether contiauation of therapy
beyond 36h is necessary: Alternatively, additional doses of
fomepizole can be administered empirically. Fomepizole
is commercially available as Antizol-Vet (Orphan Medical,
Minnetonka, MN), which can be conveniently reconsti-
tuted. Appropriate therapy also consist of iv lids to cor-
rect dehyération, increase tissue perfusion, and promote
diuresis. ‘The fluid volume administered should be based
‘on the maintenance, deficit, and continuing loss needs of
the patent. Frequent measurement of urine production,
serum urea nitrogen and creatinine, and blood pH, bisarbo-
nate, ionized calcium, and electrolytes daily oF twice daily,
will help guide fd and electrolyte therapy (Graver, 1958)
Bicarbonate should be given slowly ix: to core the meta~
bolic acidosis. Hypothermia can be controlled with blan-
kets or the use ofa pad with circulating warm water.
Im animals that are azotemic and in oligutie renal fail-
ure on presentation, almost all of the EG has been metab-
‘lized, and treatment to inhibit ADIT is likely to be of
little benefit. However, ADH inhibitors should be given
up to 36h following ingestion to prevent the metabolism.
of any residual EG. Fluid, electrolyte, and acid-base dis-
orders should be corrected and diuresis established, if
possible, Diuretics, particularly mannitol, may be help
ful. The tubular damage caused by EG may be revers-
ible, but tubular repair can take weeks to months
‘Animals may take up to 1 year following EG toxicosis to
regain concentrating ability, and some remain isosthenu-
ric. Supportive care to maintain the patient during the
Bev f renal bul regeneton nen, nd
neal dialysis may be useful (Shahar and Holmberg,
1985; Fox etal, 1987, Crisp eta, 1989). Hemodialysis
has been attempted in dogs with EG induced renal fil-
lure (DiBartola ea, 1985) and has been shown to have a
relatively good success rate in cats with acute renal fil-
ture (Langston eta, 1997). Renal transplantation has also,
‘been used with variable success in cats with renal failure
(Gregory et al, 1992; Mathews and Gregory, 1997) and
thas been described in dogs (Nemeth etal, 1997).
Prognosis
EG has 2 very high potential for a lethal outcome, but
‘vith early recognition of the syndrome and timely insti-
tution of therapy, animals ean be saved. The quantity of
a (@. ALCOHOLS AND GLYCOLS
IEG ingested, rate of absorption, and time interval prior
to institution of therapy are variables that affect the
prognosis. The prognosis is excellent in dogs treated
‘with fomepizole within 5h of ingesting EG. In a retro-
spective study of dogs with confirmed EG poisoning,
all of the dogs that were azotemic when initially treated
died. OF the dogs that did not have azotemia when ini-
tially treated, approximately 90% survived (Connally
tal, 1996). The prognosis for cats is reasonably good
if treatment is instituted within 3h following ingestion
(Dial etal, 19845) In contrast, the prognosis in humans
who survive the initial syndrome of severe acidosis is,
very good. Terminal renal fuilure in humans is raze, and
‘most human patients regain renal function by 2 months
following EG poisoning (Davis «f al, 1997) likely due
to the effectiveness of hemodialysis therapy in humans
(Cheristiansson etal, 1993),
CONCLUSIONS
Ethanol, methanol, isopropanel, propylene glycol, buty-
Tene glycol, and marijuana toxicosis can produce ataxia
and other CNS signs similar to those seen in acute EG
poisoning but are much less common than EG texico-
sis (Godbold ea, 1979; Hurd-Kuenzi, 1983; Theall etal,
19849; Suter, 1992). These disorders can be differenti-
ated by the diagnostic laboratory tests discussed previ-
ously, Other causes of an increased anion gap include
diabetic ketoacidosis and lactic acidosis; these disorders
can also be differentiated by appropriate laboratory tests.
Other causes of increased osmolality include ethanol,
isopropanol, methanol, and propylene glycol toxicosis.
Ethanol, like EG, can also produce hypocalcemia (Money.
al, 1989), Other differentials for acute renal failure
include leptospitosis, ibuprofen and other nonsteroidal
antiinflammatory drug toxicosis, aminoglycoside anti-
biotics, hemolyticuremic syndrome, cholecalciferol toxi-
cosis, grape and raisin toxicosis in dogs, and ingestion of
coxalate-containing plants such as philodendron and lily
toxicosis in eats (Brown eta, 1985, 1996; Spyridakis eal,
1985; Gunther ef al, 1988; Peterson etal, 1991; Holloway
ft al, 1993; Rivers et al, 1996; Vaden et ah, 19973;
Poortinga and Hungerford, 1998; Forrester and Troy, 1999;
Adin and Cowgill, 2000; Hovda, 2000; Rumbeiha et al,
2000; Singleton, 2001; Langston, 2002; Tefft, 2001). The
majority of dogs with grape and raisin toxicosis are hyper-
calcemic, a5 are animals with cholecaliferol toxicosis
(ooshee and Forrester, 190; Gwaltney-Brant etal, 2001);
hypercalcemia is not associated with EG toxicosis (Thrall
al, 1984b; Connally tal, 1996). Acute renal failure must
be differentiated from acutely decompensated chronic
renal failure, Carbamylated hemoglobin concentration
has been shown to be useful in making this differentia:
tion (Vaden et al, 1997b; Helene et al, 2001) In addition,
animals with ehronic renal failure may be anemic and in
poor body condition, history of the duration of clinical
signs is also helpful. Continuing to increase the awareness
ofthe toxicity of EG, as well as other alcohols and glycols,
will aid in preventing exposure and result in earlier pres-
entation of animals.
REFERENCES
‘Adin CA, Cowgill LD 2000) Treatment and outcome of dogs with
Teptosprsis: 36 cases (990-1998) | Aw Vet Mol Assoc 216
sna,
‘Ammar KA, Heckerlng PS (1986) Ethylene glyeol poisoning with
2 normal ation gap eaused by concurrent ethanol ingestion:
Importance ofthe csmolal gap. Am] Kihey Dis 27: 130-18,
Anonjmot {1930) Poste death from drinking ethylene glycol
(Prestone”) queries and minor notes. | A Mat Asso 8 1940,
Bachman B, Colaberg 1 (1971) Reappraisal of the toxicology of
llene glycol lt Mitochondrial elects. Pood Cosmet Toil 8
Bs
Sareloux DG, Hond GR, Krenzeok EP, Cooper H, Yale [A 2002)
“American Academy of Clinisl Toxicology practice guidlines
fon the treatment of methanol poisoning, in Toss 0415-446
aston |, Osha F (1981) The sncidence and characterises ofan
‘mal poisonings seen at Kanane State Univesity from 1975 to
1980 Ve ar Tal 28: 101-102,
Bauer MC, Weiss Dj, Ferman V (19823) Hematologic alterations in
dul cis fd 6 or 12% propylene gycal. mj Vet Res $69.72
Baer MC, Weiss DJ, Perman V (1928) Hematological alterations
in kittens induced by 6 and 12% etary propylene glyco. Vet
Ham Tene 94 127-134
Berger ]R, Ayyar DR (1981) Neurological complications of ethylene
Eco intonation: report ofa case Arch Newel 8724-728,
Bishol K (2069) Methanol. In Small Animal Texcolpy, Peterson M,
“Talat P (ed) Saunders St Lovis, MO, pp 80-384,
Biscotl K @008b) Propylene glyeol Soll Animal Toxic,
Peterson M, Talett P (ede). Saunders, St Lou's, MO,
pp. 996-10
Bosttom WE, Li T (1980) Alcohol dehydrogenase enzyme, In
"gre Base of Detoition, jakoby W fe). Academic Press,
New York pp. 281-248
Brown CA, Reberts AW, Miler MA, Davis DA, Brown SA,
Bolin CA, JateciBlack J, Greene CE, Mile Lich) D (1996)
Lao ntergins erat gigas nec i doe
Browa 5A, Basal JA, Crowell WA (1985) Gentamicinassociated
‘ee renal faire nthe dog | An Vt Ma Arse 186: 66-690
Burkhart KK, Kuli KW (199) The other alcohol. Erg Med Cli
[North Am 8 913928
CChazspion HR, Baker SP, Benner C (1975) Alcohol inonistion and
Serum osmolality Lancet 11402-1404
CChresanaton LK, Kaepersion KE, Kuling PE, Ovrebo $ (1995)
“Treatment of severe ethylene giyel intoxication with contin
‘ue arteriovenous hemofiltration eisiyie Tool Cli Tosi!
3267-290,
CChistopher MIM, Perman V, Eaton JW (188%) Contibuion of pro
‘yleneglyebinduced Hin body formation to anemia in et.
VA Ve ed Asoc 19: 1045-1056,
You might also like
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5813)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- EcotoxicologiaDocument1 pageEcotoxicologiaCatalina PetrelNo ratings yet
- Planos Topográficos en AnimalesDocument1 pagePlanos Topográficos en AnimalesCatalina PetrelNo ratings yet
- Act TopcicologiaDocument1 pageAct TopcicologiaCatalina PetrelNo ratings yet
- 6.etilenglicol (Gupta 2010)Document5 pages6.etilenglicol (Gupta 2010)Catalina PetrelNo ratings yet
- Copia de AdopciónDocument3 pagesCopia de AdopciónCatalina PetrelNo ratings yet
- Copia de Taller Teledetección Combinación de Imágenes2021-2 VDocument3 pagesCopia de Taller Teledetección Combinación de Imágenes2021-2 VCatalina PetrelNo ratings yet
- Copia de Trabajo Actividad 6Document9 pagesCopia de Trabajo Actividad 6Catalina PetrelNo ratings yet
- ACTIVIDAD 1-Proyecto de GradoDocument2 pagesACTIVIDAD 1-Proyecto de GradoCatalina PetrelNo ratings yet
- Copia de Indicaciones Mapa Conceptual NormativaDocument2 pagesCopia de Indicaciones Mapa Conceptual NormativaCatalina PetrelNo ratings yet
- INFORME TRANSFERENCIA CarotenoidesDocument6 pagesINFORME TRANSFERENCIA CarotenoidesCatalina PetrelNo ratings yet