Professional Documents
Culture Documents
Intussusception in Children - A Clinical Review
Uploaded by
johanrubiano6Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Intussusception in Children - A Clinical Review
Uploaded by
johanrubiano6Copyright:
Available Formats
Acta Chirurgica Belgica
ISSN: 0001-5458 (Print) (Online) Journal homepage: http://www.tandfonline.com/loi/tacb20
Intussusception in Children: A Clinical Review
T. Charles, L. Penninga, J. C. Reurings & M. C. J. Berry
To cite this article: T. Charles, L. Penninga, J. C. Reurings & M. C. J. Berry (2015) Intussusception
in Children: A Clinical Review, Acta Chirurgica Belgica, 115:5, 327-333
To link to this article: http://dx.doi.org/10.1080/00015458.2015.11681124
Published online: 11 Mar 2016.
Submit your article to this journal
Article views: 1
View related articles
View Crossmark data
Full Terms & Conditions of access and use can be found at
http://www.tandfonline.com/action/journalInformation?journalCode=tacb20
Download by: [Universite Laval] Date: 02 May 2016, At: 06:54
Review paper
Acta Chir Belg, 2015, 115, 327-333
Intussusception in Children : A Clinical Review
T. Charles, L. Penninga, J. C. Reurings, M. C. J. Berry
Department of Orthopedic Surgery, University Hospital Erasme, Brussels Belgium ; Department of General Surgery,
Sint Elisabeth Hospital, Willemstad, Curaçao.
Abstract. Intussusception is the most common cause of small bowel obstruction in young infants. Therefore a high index
of suspicion and thorough knowledge of this condition is of major importance to be able to diagnose and treat this poten-
tially life threatening condition.
In this review we describe epdidemiology, etiology and clinical symptoms of intussuception. Furthermore, we describe
diagnostic modalties, especially ultrasonography as the primary choice for diagnosis. In addition, non-operative treat-
ment with different types of enema reduction techniques, and operative treatment by laparotomy and laparoscopy, and
Downloaded by [Universite Laval] at 06:54 02 May 2016
outcomes have been reviewed.
Introduction Pathogenesis
About 75 to 90% of cases intestinal intussusceptions are
Intussusception was first described in 1793 by the
idiopathic, although in these cases the presence of lym-
Scottish surgeon James Hunter, and is defined as a proxi-
phoid hyperplasia is frequently reported (1, 2, 4). This
mal bowel segment, or intussusceptum, that like a
hyperplasia of Peyer patches in the lymphoid-rich termi-
telescope moves into a distal bowel segment, or intus-
nal ileum could act as lead point for intussusception.
suscipiens. The associated mesentery is dragged within
In many cases of intussusception an influence of viral
the invaginated segment leading to venous congestion
factors has been suspected as almost 30% of the children
and edema. This results in ischemia, and eventually
experience a viral illness before the onset of intussuscep-
bowel necrosis, perforation and peritonitis if left untreat-
tions (5, 7, 8). An association with the adenovirus species
ed (1, 2).
C in more than one third of the cases has been reported in
There are different types of intussusception ; the ileo-
a prospective case-control study in Vietnam and
colic, ileo-ileo-colic, ileo-ileal, jejuno-jejunal and the
Australia (8). Recently an association with the respirato-
colo-colic type (3). The ileo-colic type, where the distal
ry syncytial virus has also been described (9).
ileum invaginates through the ileocaecal valve into the
The presence of a pathological lead point (PLP) occurs
caecum, is the most frequent type of intussusception and
in 1,5 to 12% of the cases of intussusceptions (1). The
accounts for 90% of the cases (1).
most common PLP in children is the Meckel’s
diverticulum, but other PLP as polyps, tumor, lympho-
ma, duplication cysts, parasites, hematoma, vascular
Epidemiology
malformation, inflamed appendix and inverted appendi-
ceal stump have also been described (1-3). Usually PLP
Intussusception is after appendicitis, the second most are found in children younger than 3 months of age and
common cause of an acute abdomen in children (1, 2), in children older than 5 years, with the incidence increas-
and the most common cause of small bowel obstruction ing with advancing age (1, 3).
in young infants (4). Systemic conditions such as Henoch-Schonlein
The worldwide incidence of intussusceptions ranges purpura, cystic fibrosis, Peutz-Jegher syndrome, familial
from 15 to 300 / 100 000 children per year (4). Intestinal polyposis and nephritic syndrome are described as
intussusception is usually seen in children between predisposing factors of intussusceptions (1-3). Indeed in-
3 months and 3 years of age, with a peak incidence tussusception caused by intestinal wall hematoma, thus
between 4 and 9 months of age (1-4). Boys are affected acting as a PLP, is the most common surgical complica-
approximately twice as often as girls (1, 3, 5, 6). tion of Henoch-Schonlein purpura (1).
5566-charles-.indd 327 29/10/15 12:00
328 T. Charles et al.
Intussusception has also been described in association
with abdominal trauma and during the postoperative
period (1).
Clinical manifestations
Abdominal pain occurs in 80 to 95% of cases (1). It is
characterized by the sudden onset of intermittent, crampy,
severe and progressive abdominal pain, usually with 15
to 20 minutes interval. In between episodes patients may
be completely asymptomatic. With prolonged intussus-
ception, the abdomen becomes more distended and signs
of peritonitis may occur when perforation occurs.
The presence of gross or occult blood in the stool is
reported in 50 to 70% of cases, and the mixture of blood
and mucus give a typical redcurrant jelly appearance (1). Figure 1. This figure represents a longitudinal view of an intus-
However the absence of blood in the stool does not susceptions as seen on the ultrasonography.
exclude intussusception. The palpation of an abdominal
Downloaded by [Universite Laval] at 06:54 02 May 2016
mass, typically a sausage-shaped mass in the upper right
quadrant of the abdomen has been described in up to 60%
of patients (1). This may be accompanied by emptiness the intussusceptum may suggest bowel ischemia and
due the absence of bowel in the right lower quadrant of predict potential irreducibility (2).
the abdomen. Due to the high sensitivity and specificity of abdomi-
The classic clinical triad of Ombredanne consists of nal ultrasonography and the radiation exposure associat-
intermittent abdominal pain, redcurrant jelly stool and a ed with a CT of the abdomen (3), an abdominal-CT
sausage-shaped abdominal mass. This triad is found in should only be used when other diagnostic modalities are
7.5 to 40% of cases (2, 3). unrevealing (1).
Other symptoms like emesis (60%), diarrhea (30%), Currently, there are no international guidelines for the
crying, lethargy, and altered consciousness, sepsis, shock diagnosis of intussusception. The Japanese Guidelines
and syncope have also been associated with the presence published in 2011 (3) divided clinical and radiological
of intussusceptions (1). These more aspecific findings findings associated with intussusception into 3 criteria ;
make the diagnosis of intussusception difficult (1, 10, criteria A (pain, bloody stool and palpable mass), criteria
11). B (vomitus, pallor, lethargy, shock and bowel gas pattern
on abdominal x-ray) and criteria C (all characteristic im-
Investigations ages of intussusception by contrast enema, ultrasonogra-
phy, CT or MRI). Definitive diagnosis of intussusception
Plain abdominal X-rays have a sensitivity between 29 is confirmed by the presence of 1 criteria C.
and 50%. In up to 25% of the cases plain abdominal X-
rays are completely normal (1). Therefore, they should Treatment
be reserved for cases when perforation is suspected (6).
Ultrasonography is the method of choice to diagnose in- Treatment of intussusception has to start as soon as pos-
tussusception. It has a sensitivity between 98 and 100% sible after suspicion of diagnosis with fluid resuscitation
and a specificity between 88 and 100% (1-3, 11). There- management. Early fluid resuscitation is important be-
fore, all children with clinical suspicion of intussuscep- cause most children with intussusception are dehydrated
tion should undergo abdominal ultrasonography (6). due to vomiting, decreased oral intake and third
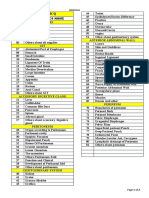
Two typical features are described (1, 2). The first sign is spacing (1-3).
the target/doughnut sign, seen on transverse views, and
represented by a central hyperechoic core, the intussus- Conservative treatment
ceptum and a hypoechoic outer rim of homogeneous tis- Non-operative management is indicated in hemodynami-
sue, the intussuscipiens. The second sign is the pseu- cally and clinically stable children, with high clinical
dokidney sign, seen on longitudinal views (Fig. 1). It is suspicion of intussusception or radiological evidence of
represented by a hyperechoic tubular centre covered by a intussusception, but without any evidence of bowel
hypoechoic rim producing a kidney-like appearance. perforation (1-3, 11-13).
Color Doppler can be used in addition to ultrasonogra- Non-operative management of intussusception uses
phy. A lack of color Doppler flow in the bowel wall of an enema reduction technique.
5566-charles-.indd 328 29/10/15 12:00
Intussusception in Children 329
The first report of reduction of intussusception by hy- of radiation exposure, better visualization of the intus-
drostatic pressure was published in 1876 by Hirschprung. susception and its reduction, and the possibility to detect
Ravitch and Morgan set the guidelines and popularized and recognize pathological lead points (2, 13). It was
the use of barium for enema reduction of intussusception speculated that detection of perforation during the proce-
in 1948 (1, 3). The barium enema technique is the dure could be less accurate with ultrasonography com-
therefore the most well-known reduction technique, and pared to fluoroscopy (13), but 2 retrospective studies
often referred as ‘the golden standard’. Until the past showed no problems in detection of perforation during
decade it remained also the most used method. Because ultrasonography guided procedures (20, 22).
of complications of chemical peritonitis, infection and Overall success rates of enema reduction techniques
adhesions when perforation occurs while using barium, for intussusception vary between 61 and 95% (1, 2, 5, 6,
other methods to perform enema reduction were devel- 10-13, 14, 17, 18, 20-22). Factors which decrease the
oped and applied (2). success rate for enema reduction techniques include
The use of water-soluble contrast has been described younger age (younger than one year of age), longer dura-
in few reports. These hypertonic solutions could induce tion of symptoms (usually more than 24 hours), early re-
rapid fluid shifts and electrolyte disturbances when per- currence, and other factors that suggest that the condition
foration occurs, and should therefore be diluted to iso- has progressed like ; the presence of bloody stool and
osmolar concentrations (13). radiographic signs of intestinal obstruction (12, 13, 23).
The use of normal saline for reduction of intussuscep- Differences in success rates might reflect the learning
Downloaded by [Universite Laval] at 06:54 02 May 2016
tion is not widely reported in the literature. Although, a curve of the radiologist with the used technique (6, 10,
few studies reported better reduction rates with saline en- 16), and the patient population encountered. Lower suc-
ema compared to barium enema reduction techniques. cess rates would be expected in regions of the world
Furthermore, this technique may cause less morbidity where a delay occurs in patients getting to the hospital in
when perforation occurs compared with other enema re- a timely manner (9, 23, 24).
duction techniques (3, 14). Bowel perforation with saline Medical interventions have been attempted to increase
techniques does not include the risk of chemical peritoni- reduction rates. Buscopan has been administrated, but
tis, the risk of fluid shift nor the risk of tension pneumo- no comparative studies exist to prove efficacy of busco-
peritoneum. pan (3). In addition, glucagon has been studied in three
Enema reduction using air has become the preferred randomised trials to increase reduction rates of intussus-
method of reduction of intussusception. Success rates ception, but no benefits of its use was found (3, 13, 25,
with air enema reduction appear to be higher compared 26).
to other enema techniques. Reduction is described as be- Sedation and general anesthesia have also been used
ing easier, presumably because air reduction allows the to improve reduction rates. It was observed that sedation
use of higher intra-colonic pressures. It might be safer, interferes with the Valsalva maneuver, and it is assumed
because during air reduction true intra-colonic pressures that this maneuver could protect against perforation (27).
can be monitored and controlled (1). Bowel visualization Sedation requires proper monitoring and, until now there
is more difficult with air enema reduction, especially is little evidence to support or refute the use of sedation.
when a large amount of gas in the small bowel is present A recent study by PURENNE et al. reported an increase in
near the intussusception (13, 15). reduction rates from 72 to 90% while using general anes-
When different techniques for enema reduction re- thesia compared to the use of sedation for enema reduc-
ported are compared, air enema reduction has the highest tion (28), while an older study showed no significant dif-
reduction rates (1, 2, 5, 17, 20, 21). A prospective study ference comparing sedation to general anesthesia to
reported reduction rates for air enema of 90%, for hydro- perform an enema reduction (29). Because of the promis-
static enema of 80% and for barium enema of 73% (5). In ing results of the recent study by PURENNE et al., it could
this german study, they calculated that the introduction of be useful to perform other studies to confirm or reject
air enema therapy as first-line treatment for intussuscep- their results.
tion might prevent 104 surgeries per year in Germany. A Perforation is the most feared complication of enema
recent meta-analysis showed that for every nine patients reduction, and perforation rates vary between < 1% to
treated with air enema reduction instead of hydrostatic 4% (1-3, 13). The variation in perforation rate might be
enema reduction, 1 failure would be avoided (NNT of related to the learning curve of the radiologist, a too ag-
9) (12). Another advantage for air enema reduction is gressive enema reduction approach, too high reduction
shorter fluoroscopic time and lower radiation exposure to pressures and patient selection, as in some centers pa-
the patient (19). tients considered to be at risk for perforation directly un-
Over time, fluoroscopy has been replaced by ultraso- dergo laparotomy or laparoscopy (13, 20). Risk factors
nography to monitor the reduction of the intussusception. for perforation include infants younger than 6 months of
Ultrasonography has many advantages such as absence age, presumably because of a thinner bowel wall (13,
5566-charles-.indd 329 29/10/15 12:00
330 T. Charles et al.
30). Delay between onset of symptoms and treatment is ca (4). As we noticed the need for surgical intervention is
also described as a risk factor, and the duration of symp- less common in developed areas, whereas in developing
toms in these cases is usually reported to be 36 to areas the percentages of surgical procedures to treat in-
48 hours, or longer (2, 9, 13, 23, 24, 30). tussusception remains high. This could be explained by a
Bramson and Blickman suggested in 1992 that bowel delay in seeking for medical attention (patient delay),
perforation already might be present prior to an attempt- less experience in radiological techniques, less access to
ed reduction, where the apposition of the two bowel seg- medical facilities and differences in healthcare infra-
ments could prevent the escape of intraluminal air into structures over the world (4, 6, 9, 24, 35).
the peritoneal cavity. When reduction is achieved, air A difference in surgical intervention rates could also
escapes and this gives the typical clinical and radiologi- be explained by a difference in decision making, as in
cal picture of free intraperitoneal air (31). some centers enema reduction is always stated as the
Perforation with air during air enema reduction might standard procedure before surgical intervention whereas
cause a tension pneumoperitoenum, in which intraperito- in other centers patients considered to be at risk for per-
neal air under pressure causes life-threatening ventilatory foration during enema reduction underwent directly a
and hemodynamic compromise. This is prevented by dis- surgical procedure (13, 20).
continuing the enema and releasing the air from the co- There is consensus that primary surgical intervention
lon (20). Needle decompression of the abdomen is found is indicated for patients with suspected intussusception
to be a safe and effective way to prevent tension (33). who are hemodynamically unstable, when there is evi-
Downloaded by [Universite Laval] at 06:54 02 May 2016
Though, conflicting with previous reports, all four chil- dence of bowel necrosis, bowel perforation or peritonitis,
dren in their review who complicated with perforation or when safe facilities to perform an enema reduction are
during air enema reduction needed a bowel resection. not available (1-3, 13, 36). Surgical treatment is also in-
In the past, when intussusception was found to be ir- dicated in cases of failure of the conservative therapy (1-
reducible after a first attempt of enema reduction, imme- 3, 13, 36). In addition, surgery is more often recommend-
diate surgery was standard practice. However, by the ed when a pathological lead point is the cause of
time laparotomy was performed some cases of intussus- intussusception (1-3, 13).
ception were found to be spontaneously reduced and When manual reduction of the intussusception is not
some other cases were really easy reduced manually dur- possible or when a pathological lead point or bowel ne-
ing surgery (3). Therefore, the concept of repeated de- crosis is present at the time of laparotomy or laparosco-
layed enema reduction has been introduced. A repeated py, bowel resection is indicated (3, 37). The need for
delayed attempt for enema reduction is indicated only bowel resection varies between 25 to 40% (6, 9, 11, 16,
when the patient is stable, without any evidence of nei- 18, 24, 28, 34, 35). Higher rates of bowel resection could
ther perforation nor peritonitis (3, 34). It is also required be explained by delayed presentation. A study from
that the first enema attempt was able to move the intus- Nigeria, reported that a delayed presentation of more
susception, thus achieving partial reduction (1, 3, 34). than 24 hours predisposed to bowel complications such
This because it is believed that a partial reduction and as increased irreducibility, and devitalized bowel at time
time interval between two attempts allow venous conges- of operation, and they suggested that this high incidence
tion and edema of the bowel to decrease, thus facilitating of bowel complications might favor primary surgical
reduction of the residual intussusceptions (3). The time intervention in most of these cases (24). Another retro-
delay between two attempts varies between 30 minutes spective study showed that the risk of bowel resection
and up to a few hours (2, 34). The optimal time interval during surgical reduction of the intussusception was 80%
has not been defined yet. Another discussion focuses on less when performed in a hospital employing full-time
the numbers of attempts that could be made before sur- pediatric surgeons after adjustment of the results (37).
gery is indicated. Despite absence of consensus on these They also noticed that ‘severe disease’ and concomitant
points, the ‘rule of threes’ is largely applied : no more gastro-intestinal pathology where also associated with a
than 3 attempts of 3 minutes (2, 3). But reports of more significantly increased risk of bowel resection during
frequent and longer successful attempts exist (34). surgery.
Surgical intervention in patients with intussusception
can be performed both as an open or laparoscopic proce-
Operative treatment
dure. Apelt and colleagues reviewed all laparoscopic re-
The need for surgical intervention for intussusception ductions of intussusception. They identified 10 retrospec-
varies in different regions of the world and between dif- tive studies with a total of 276 cases of laparoscopic
ferent hospitals. The incidence of surgery has been re- reduction of intussusceptions (38), and found a success
ported to vary from 13% in Asia, 20% in Europe, 28% in rate of 71%, with a subsequent conversion rate to lapa-
North America, 29% in Oceania and Eastern Mediterra- rotomy of 29%. Complications reported included : intra-
nean, 77% in Africa to 86% in Central and South Ameri- operative complications in 0,4% and postoperative com-
5566-charles-.indd 330 29/10/15 12:00
Intussusception in Children 331
plications in 2,9%. They concluded in their review that Outcomes
laparoscopy was an effective and safe way to reduce in-
tussusceptions in children. A French study described risk The success rates of enema reduction techniques vary
factors for conversion to laparotomy such as : more than between 61% and 95%, as described previously in our
1.5 days between onset of symptoms and diagnosis, pres- review (1, 2, 5, 6, 10-14, 17, 18, 20-22). Besides previous
ence of signs of peritonitis at primary clinical examina- described suggestions to explain this variation in rates,
tion and the presence of a pathological lead point (39). some authors also noted the presence of factors that
Laparoscopy is nowadays assumed to reduce hospital predisposed to lower reduction rates. Those risk factors
length of stay, postoperative complications especially include ; the younger age, the presence of rectal bleeding
wound infections, postoperative pain and improves cos- at clinical exam, the presence of radiographic signs of
metic results. But in this specific setting, we lack pro- bowel obstruction, a longer duration of symptoms (usu-
spective randomised trials comparing laparoscopy with ally more than 24 hours), early recurrence and an ileo-
laparotomy to confirm this. ileal or ileo-ileo-colic type of intussusceptions (9, 12, 13,
23, 24). These factors could be considered when decision
making towards the optimal treatment for a specific pa-
Recurrence
tient.
Besides the lack of adequate diagnostic criteria for in-
Recurrence tend to occur from 6 hours up to 4 years after tussusception, a recognized severity score for this condi-
Downloaded by [Universite Laval] at 06:54 02 May 2016
an initial episode of intussusception (40). The reported tion has also not yet been established. The Japanese
recurrence rates of intussusception after enema reduction Guidelines, published in 2011, proposed a severity as-
varies between 8 and 15%, independent of the used tech- sessment in order to optimize decision making regarding
nique (13, 40-42). One study found that recurrence rates preferred treatment for a patient suffering from intussus-
tended to increase with the number of recurrent epi- ceptions (3). Until now, this is the only report to propose
sode (41). After a first enema reduction, the recurrence a severity score for this condition. They distinguished
rate was found to be approximately 15,7%. After a sec- between severe, moderate and mild cases of intussuscep-
ond reduction it increased to 37,7%, after a third episode tion. The severe form is best described as being similar to
to 68,4% and after a fourth episode recurrence rate was the indications for primary surgery. A moderate intus-
nearly 100%. Recurrence rates after surgical reduction susception includes criteria such as factors known to de-
tend to be less high, between 1 to 3% after manual reduc- crease the success rates of enema reduction technique
tion during surgery (13, 40-42). No recurrence occurs and others criteria such as the location of the apex of the
when bowel resection is performed during surgery (13, intussusception beyond the splenic flexure, high leuco-
40-42). There are some controversies about whether or cytes, high C-reactive protein values, lack of blood flow
not an associated ileopexy decreases recurrence rates in assessed with Color Doppler, and the presence of a path-
the literature. ological lead point. Mild intussusceptions are therefore
Each recurrent episode of intussusception should be described as cases of intussusception presenting without
treated as if it was the first episode of intussusception (13, any of the above criteria of severe and moderate intus-
41, 42). This is recommended both when the reduction susception.
before the recurrence was a successful non-operative re- Exact numbers regarding morbidity associated with
duction and in case of a previous successful surgical re- intussusception are lacking. It seems that morbidity is
duction. For recurrences of intussusception, a surgical highly influenced by the time lapse between onset of
reduction should be considered in case of failure of non- symptoms and diagnosis (24). Most of the patients have
operative treatment, a suspected pathological lead point a favorable course if reduction is achieved within 24 hours
or in case of several recurrent episodes. Though, there from the onset of symptoms, while delayed presentation
are no specific recommendations about after how many decreases reduction rates and increases the need for surgi-
recurrent episodes surgical management is warranted. An cal intervention and associated surgical complica-
older study suggested that any patient who presented tions (23, 24). As mentioned, a case serie from Nigeria
with a third recurrent episode of intussusception within a reported that a delayed presentation predisposed to bowel
short period of time should be taken to surgery because complications with an increased irreducibility and pres-
of a high incidence of pathological lead point (23). An- ence of devitalized bowel at the time of diagnose (24).
other study referred to the increase of recurrence rates Mortality in association with intussusception is quite
with the number of episode, and suggested also that low (< 1%) in most parts of the world (4). Though, in
surgery should be considered after a third episode of Africa mortality up to 9,4% has been reported (4). This
intussusception (41). In the French study, as mentioned high mortality probably reflects the difference in health-
before, the authors described that recurrences can care infrastructure and the delay in seeking for medical
successfully be managed with laparoscopy (39). care (4, 24). Most African reports described a delay in
5566-charles-.indd 331 29/10/15 12:00
332 T. Charles et al.
seeking for medical attention of between 24 hours and 11. LEHNERT T., SORGE I., TILL H. et al. Intussusception in children –
clinical presentation, diagnosis and management. Int J Colorectal
4 days. Dis, 2009, 24 : 1187-1192.
12. BERES A. L., BAIRD R. An institutional analysis and systematic re-
Conclusions view with meta-analysis of pneumatic versus hydrostatic reduction
for pediatric intussusception. Surgery, 2013, 154 : 328-334.
13. DANEMAN A., NAVARRO O. Intussusception, Part 2 : An update on
Intussusception is the most common cause of small the evolution of management. Pediatr radiol, 2004, 34 : 97-108.
bowel obstruction in young infants. Therefore a high 14. DIGANT S. M., RUCHA S., EKTA D. Ultrasound guided reduction of
an ileocolic intussusception by a hydrostatic method by using
index of suspicion and thorough knowledge of this normal saline enema in paediatric patients : A sudy of 30 cases.
condition remain of major importance to be able to diag- J Clin Diagn Research, 2012, 6 : 1722-1725.
nose and treat this potentially life threatening condition. 15. HEDLUND G. L., JOHNSON J. F., STRIFE J. L. Ileocolic intussusception :
extensive reflux of air preceding pneumatic reduction. Radiology,
Abdominal ultrasonography is the primary diagnostic 1990, 174 : 187-189.
tool in the work op of intussusception, because of its high 16. SHEKHERDIMIAN S., LEE S. L. Management of pediatric intussuscep-
specificity and sensitivity, and the absence of radiation tion in general hospitals : diagnosis, treatment, and differences
based on age. World J Pediatr, 2011, 7 : 70-73.
exposure. 17. WANG G., LUI X. G., ZITSMAN J. L. Nonfluoroscopic reduction of
Air enema reduction techniques monitored by ultra- intussusception by air enema. World J Surg, 1995, 19 : 435-438.
sonography is the preferred first line treatment in many 18. ALEHOSSEIN M., BABAHEIDARIAN P., SALAMATI P. Comparison of
different modalities for reducing childhood intussusception. Iran J
institutions with good results and few complications. Radiol, 2011, 8 : 83-87.
Surgery should be performed when bowel necrosis or 19. SHIELS W. E., MAVES C. K., HEDLUND G. L. et al. Air enema for
Downloaded by [Universite Laval] at 06:54 02 May 2016
perforation is suspected. Furthermore, surgical reduction diagnosis and reduction of intussusception : clinical experience
and pressure correlates. Radiology, 1991, 181 : 169-172.
is indicated when non-operative treatment with enema 20. YOON C. H., KIM H. J., GOO H. W. Intussusception in children :
reduction fails, and a laparoscopic approach should be US-guided Pneumatic reduction – Initial experience. Radiology,
considered. 2001, 218 : 85-88.
21. HADIDI A. T., SHAL N. E. Childhood intussusception : a comparative
International diagnostic criteria guidelines and sever- study of non surgical management. J Pediatr Surg, 1999, 34 : 304-
ity scores are needed to guide towards adequate and 307.
optimal treatment for this condition. Furthermore, pro- 22. WANG G. D., LUI S. J. Enema reduction of intussusception by
hydrostatic pressure under ultrasound guidance : a report of 377
spective, preferable randomized studies are warranted to cases. J Pediatr Surg, 1988, 23 : 814-818.
establish firm evidence regarding treatment guidelines 23. MCDERMOTT V. G., TAYLOR T., MACKENZIE S. et al. Pneumatic
for this condition. reduction of intussusceptions : clinical experience and factors
affecting outcomes. Clin Radiol, 1994, 49 : 30-34.
24. EKENZE S. O., MGBOR S. O. Childhood intussusception : the
implications of delayed presentation. Afr J Pediatr Surg, 2011, 8 :
15-18.
References 25. FRANKEN E. A. Jr., SMITH W. L., CHEMISH S. M. et al. The use of
glucagon in hydrostatic reduction of intussusception : a double-
1. WASSEEM M., ROSENBERG H. K. Intussusception. Pediatr Emerg blind study of 30 patients. Radiology, 1983, 146 : 687-689.
Care, 2008, 24 : 793-800. 26. MORTENSSON W., EKLÖF O., LAURIN S. Hydrostatic reduction of
2. APPLEGATE K. E. Intussusception in children : evidence-based childhood intussusception. The role of adjuvant glucagon
diagnosis and treatment. Pediatr Radiol, 2009, 39 Suppl 2 : S140- medication. Acta Radiol Diagn, 1984, 25 : 261-264.
143. 27. SHIELS W. E. II, KIRKS D. R., KELLER G. L. et al. Colonic perforation
3. ITO Y., KUSAKAWA I., MURATA Y. et al. Japanese guidelines for the by air and liquid enemas : comparison study in young pigs. AJR,
management of intussusception in children, 2011. Pediatr Int, 1993, 160 : 931-935.
2012, 54 : 948-958. 28. PURENNE E., FRANCHI-ABELLA S., BRANCHEREAU S. et al. General
4. JIANG J., JIANG B., PARASHAR U. et al. Childhood intussusception : a anesthesia for intussusception reduction by enema. Pediatr
literature review. PLoS One, 2013, 8 : e68482. Anaesth, 2012, 22 : 1211-1215.
5. JENKE A. C., KLAASSEN-MIELKE R., ZILBAUER M. et al. 29. SUZUKI M., HAYAKAWA K., NISHIMURA K. et al. Intussusception : the
Intussusception : incidence and treatment insights from the role of general anesthesia during hydrostatic barium reduction.
nationwide German surveillance. J Pediatr Gastroenterol Nutr, Radiat Med, 1999, 17 : 121-124.
2011, 52 : 446-451. 30. DANEMAN A., ALTON D. J., EIN S. et al. Perforation during attempted
6. SAMAD L., MARVEN S., BASHIR H. E. et al. Prospective surveillance intussusception reduction in children – a comparison of perforation
study of the management of intussusception in the UK and Irish with barium and air. Pediatr Radiol, 1995, 25 : 81-88.
infants. Br J Surg, 2012, 99 : 411-415. 31. BRAMSON T., BLICKMAN J. G. Perforation during hydrostatic
7. NYLUND C. M., DENSON L. A., NOEL J. M. Bacterial enteritis as risk reduction of intussusception : Proposed mechanism and review of
factor for childhood intussusception : A retrospective cohort study. the literature. J Pediatr Surg, 1992, 27 : 589-591.
J Pediatr, 2010, 156 : 791-795. 32. HERNANZ-SCHULMAN M., FOSTER C., MAXA R. et al. Experimental
8. BINES J. E., NGUYEN L. T., JUSTICE F. A. et al. Risk factors for study of mortality and morbidity of contrast media and standardized
intussusception in infants in Vietnam and Australia : Adenovirus fecal dose in the peritoneal cavity. Pediatr Radiol, 2000, 30 : 369-
implicated, but not Rotavirus. J Pediatr, 2006, 149 : 452-460. 378.
9. SAEZ-LLORENS X., VELÀZQUEZ F. R., LOPEZ P. et al. A multi-country 33. FALLON S. C., KIM E. S., NAIK-MATHURIA B. J. et al. Needle
study of intussusceptions in children under 2 years of age in Latin decompression to avoid tension pneumoperitoneum and
America : Analysis of prospective surveillance data. BMC hemodynamic compromise after pneumatic reduction of pediatric
gastroenterology, 2013, 13 : 95. intussusception. Pediatr Radiol, 2013, 43 : 662-667.
10. TAREEN F., RYAN S., AVANZINI S. et al. Does the length of history 34. PAZO A., HILL J., LOSEK J. D. Delayed repeat enema in the
influence the outcomes of pneumatic reduction of intussusception management of intussusception. Pediatr Emerg Care, 2010, 26 :
in children ? Pediatr Surg Int, 2011, 27 : 587-589. 640-645.
5566-charles-.indd 332 29/10/15 12:00
Intussusception in Children 333
35. SONMEZ K., TURKYILMAZ Z., DEMIROGULLARI B. et al. Intussusception 40. JUSTICE F. A., NGUYEN L. T., TRAN S. N. et al. Recurrent
in children : Experience with 105 patients in a department of intussusception in infants. J Ped Child health, 2011, 47 : 802-805.
paedriatric surgery, Turkey. SAJS, 2012, 50 : 37-39. 41. HSU W. L., LEE H. C., YEUNG C. Y. et al. Recurrent intussusception :
36. CHEUNG S. T., LEE K. H., YUENG T. H. et al. Minimally invasive when should surgical intervention be performed ? Pediatr
approach in the management of childhood intussusceptions. ANZ J Neonatol, 2012, 53 : 300-303.
Surg, 2007, 77 : 778-781. 42. NIRAMIS R., WATANATITTAN S., KRUATRACHUE A. et al. Management
37. MCATEER J. P., KWON S., LARIVIERE C. A. et al. Pediatric specialist of recurrent intussuception : nonoperative or operative reduction ?
care is associated with a lower risk of bowel resection in children J Pediatr Surg, 2010, 45 : 2175-2180.
with intussusception : a population-based analysis. J Am Coll Surg,
2013, 217 : 226-232.
38. APELT N., FEATHERSTONE N., GIULIANI S. Laparoscopic treatment of
intussusception in children : a systematic review. J Pediatr Surg, T. Charles, M.D.
2013, 48 : 1789-1793.
Department of Orthopedic surgery
39. BONNARD A., DEMARCHE M., DIMITRIU C. et al. Indications for
laparoscopy in the management of intussusception : A multicenter University Hospital Erasme
retrospective study conducted by the French Study Group for Lenniksebaan 808
Pediatric Laparoscopy. J Pediatr Surg, 2008, 43 : 1249-1253. 1070 Brussels, Belgium
Downloaded by [Universite Laval] at 06:54 02 May 2016
5566-charles-.indd 333 29/10/15 12:00
You might also like
- The Perioperative Nurse's Duties and Responsibilities: Surgical Nursing DefinedDocument9 pagesThe Perioperative Nurse's Duties and Responsibilities: Surgical Nursing DefinedSiena Lou CeniaNo ratings yet
- TapiDocument2 pagesTapiSaurav SultaniaNo ratings yet
- Atresia EsofagusDocument7 pagesAtresia EsofagusTommysNo ratings yet
- XX Uroflowmetric Evaluation of Patients With Hypospadias Treated in Our Clinic (#409281) - 523261Document4 pagesXX Uroflowmetric Evaluation of Patients With Hypospadias Treated in Our Clinic (#409281) - 523261Ashwin KumarNo ratings yet
- Current Diagnosis and Image-Guided Reduction For Intussusception in ChildrenDocument10 pagesCurrent Diagnosis and Image-Guided Reduction For Intussusception in ChildrenMostafa MosbehNo ratings yet
- Intussusception: Afua A.J. Hesse Francis A. Abantanga Kokila LakhooDocument8 pagesIntussusception: Afua A.J. Hesse Francis A. Abantanga Kokila LakhooFATIN NAJIHAHNo ratings yet
- Intussusception - Practice Essentials, Background, Etiology and PathophysiologyDocument10 pagesIntussusception - Practice Essentials, Background, Etiology and PathophysiologyfkNo ratings yet
- The Surgical Management of Necrotizing Enterocolitis - July 2018Document4 pagesThe Surgical Management of Necrotizing Enterocolitis - July 2018Hengky TanNo ratings yet
- Journal Reading TOA - TamiDocument14 pagesJournal Reading TOA - Tamicharyadita putriNo ratings yet
- Fistula in AnoDocument5 pagesFistula in AnoIoannis ValioulisNo ratings yet
- International Journal of Surgery Case ReportsDocument3 pagesInternational Journal of Surgery Case ReportsDr David NekouNo ratings yet
- Adult Intussusception: An Institutional Experience and Review of LiteratureDocument6 pagesAdult Intussusception: An Institutional Experience and Review of LiteraturenurfitriaNo ratings yet
- Intussusception TransDocument4 pagesIntussusception TransJames Maravillas100% (1)
- Jurnal THT NiaDocument5 pagesJurnal THT NianiajaplaniNo ratings yet
- Peritonsillar Abscess: Complication of Acute Tonsillitis or Weber's Glands Infection?Document9 pagesPeritonsillar Abscess: Complication of Acute Tonsillitis or Weber's Glands Infection?holly theressaNo ratings yet
- IntussuceptionDocument8 pagesIntussuceptionInomy ClaudiaNo ratings yet
- Hirschsprung Disease PDFDocument8 pagesHirschsprung Disease PDFAlchemistalazkaNo ratings yet
- Whiteford2007 Abses PerianalDocument8 pagesWhiteford2007 Abses PerianalPudyo KriswhardaniNo ratings yet
- Saboo 2017Document6 pagesSaboo 2017jjeongjjangNo ratings yet
- Peutz-Jeghers Syndrome in A Woman Presenting As Intussusception Case ReportDocument5 pagesPeutz-Jeghers Syndrome in A Woman Presenting As Intussusception Case ReportDillaNo ratings yet
- Money Tips Ebook Vol 1 V3Document25 pagesMoney Tips Ebook Vol 1 V3Chauthiran Agamudaiyar100% (1)
- International Journal of Recent Scientific ResearchDocument5 pagesInternational Journal of Recent Scientific ResearchifahInayahNo ratings yet
- Rectovaginal Fistulae: Bidhan Das, MD Michael Snyder, MDDocument7 pagesRectovaginal Fistulae: Bidhan Das, MD Michael Snyder, MDNovaNo ratings yet
- Kim 2015Document4 pagesKim 2015ruthameliapNo ratings yet
- Seminars in Fetal & Neonatal Medicine: Steven M. Donn, Sunil K. SinhaDocument6 pagesSeminars in Fetal & Neonatal Medicine: Steven M. Donn, Sunil K. SinhadeniNo ratings yet
- Actinomicose Cervico-Facial. 2020Document7 pagesActinomicose Cervico-Facial. 2020Vinícius FlorentinoNo ratings yet
- Aydin 2016Document5 pagesAydin 2016nurfitriaNo ratings yet
- Nihms 1657970Document20 pagesNihms 1657970mchojnacki81No ratings yet
- Mini Review: Current Concepts in The Management of Anterior Urethral StricturesDocument8 pagesMini Review: Current Concepts in The Management of Anterior Urethral StricturesDwi WiraNo ratings yet
- 1 s2.0 S0140673623009662 MainDocument14 pages1 s2.0 S0140673623009662 MainKesia MaldonadoNo ratings yet
- Journal EmpyemaDocument6 pagesJournal EmpyemaElisaNo ratings yet
- Intussusception 161007042729 PDFDocument44 pagesIntussusception 161007042729 PDFDina MarselinaNo ratings yet
- Human Taeniasis: Current Insights Into Prevention and Management Strategies in Endemic CountriesDocument10 pagesHuman Taeniasis: Current Insights Into Prevention and Management Strategies in Endemic CountriesIndra KusumaNo ratings yet
- Perianal Abscess - Abstract - Europe PMCDocument6 pagesPerianal Abscess - Abstract - Europe PMCRidha Aswina DalimuntheNo ratings yet
- Defining Urinary Tract InfectionDocument5 pagesDefining Urinary Tract InfectionTamara LopezNo ratings yet
- Ding 2020Document6 pagesDing 2020Ridha Aswina DalimuntheNo ratings yet
- Hydatid Disease of The Liver: ReviewDocument8 pagesHydatid Disease of The Liver: ReviewRafki HidayatNo ratings yet
- Die 1Document18 pagesDie 1juan carlos pradaNo ratings yet
- The Management of Asherman Syndrome: A Review of LiteratureDocument11 pagesThe Management of Asherman Syndrome: A Review of LiteratureEuphra Adellheid100% (1)
- Intestinal Atresia: A Case ReportDocument3 pagesIntestinal Atresia: A Case ReportOvamelia JulioNo ratings yet
- Fistula Ani Japanese GuidelineDocument7 pagesFistula Ani Japanese GuidelinevivianmtNo ratings yet
- Case Scenario: Anesthesia For Maternal-Fetal Surgery: The Ex Utero Intrapartum Therapy (EXIT) ProcedureDocument7 pagesCase Scenario: Anesthesia For Maternal-Fetal Surgery: The Ex Utero Intrapartum Therapy (EXIT) ProcedureHilton EmilNo ratings yet
- 2010 TEPTSemin Pediatr Surg 2010 May 19296106Document12 pages2010 TEPTSemin Pediatr Surg 2010 May 19296106Riyan DarundryoNo ratings yet
- Uia30 Anaesthesia For Paediatric Ear Nose and Throat SurgeryDocument6 pagesUia30 Anaesthesia For Paediatric Ear Nose and Throat SurgeryAshokNo ratings yet
- 03-Ajpcr 46713 20230510 V1Document4 pages03-Ajpcr 46713 20230510 V1DipteshPatilNo ratings yet
- Intussusception - A Case ReportDocument3 pagesIntussusception - A Case ReportAgustinus HuangNo ratings yet
- p1319 PDFDocument4 pagesp1319 PDFSyairodhiNo ratings yet
- Focseneanu2015 PDFDocument3 pagesFocseneanu2015 PDFAniydaNo ratings yet
- Abcese FistuleDocument8 pagesAbcese FistuleDenis StoicaNo ratings yet
- Implantación Endometrial - GenéticaDocument9 pagesImplantación Endometrial - GenéticaMaríaJoséPinedaNo ratings yet
- Ileus in Adults: MedicineDocument11 pagesIleus in Adults: MedicineAmanda PutriNo ratings yet
- The Research Progress of Acute Small Bowel PerforaDocument5 pagesThe Research Progress of Acute Small Bowel PerforaIlham PrayogoNo ratings yet
- A Case of Adult Intussusception: A Case ReportDocument4 pagesA Case of Adult Intussusception: A Case ReportIJAR JOURNALNo ratings yet
- Current Care and Investigational Therapies in AchondroplasiaDocument8 pagesCurrent Care and Investigational Therapies in Achondroplasiachristian roblesNo ratings yet
- Gastroschisis Omphalocele PDFDocument5 pagesGastroschisis Omphalocele PDFFariz Eka SetiawanNo ratings yet
- EsofagusDocument7 pagesEsofagusWillie VanegasNo ratings yet
- Appendicitis ManuscriptDocument4 pagesAppendicitis Manuscriptkint manlangitNo ratings yet
- Congenital ChylothoraxDocument11 pagesCongenital ChylothoraxFabsscribNo ratings yet
- Side-to-Side Refluxing Nondismembered Ureterocystotomy A Novel Strategy To Address Obstructed Megaureters in Children. 2017. ESTUDIO CLINICODocument9 pagesSide-to-Side Refluxing Nondismembered Ureterocystotomy A Novel Strategy To Address Obstructed Megaureters in Children. 2017. ESTUDIO CLINICOPaz MoncayoNo ratings yet
- A Compilation of Cellular and Tissue Xenotransplantation Studies (1838-2022): A Promising Approach for the Treatment of DiseasesFrom EverandA Compilation of Cellular and Tissue Xenotransplantation Studies (1838-2022): A Promising Approach for the Treatment of DiseasesNo ratings yet
- JD Fs Papilla Preservation FlapDocument7 pagesJD Fs Papilla Preservation FlapReshmaa RajendranNo ratings yet
- 2023 Periprosthetic Joint InfectionDocument12 pages2023 Periprosthetic Joint InfectionAnaNo ratings yet
- The Pelvis IiDocument25 pagesThe Pelvis IiFaith ChepoghishoNo ratings yet
- Answer KeyDocument24 pagesAnswer KeyLyka Mae Imbat - PacnisNo ratings yet
- Comparison of Enamel Microabrasion With A Combined Approach To The Esthetic Management of Fluorosed TeethDocument10 pagesComparison of Enamel Microabrasion With A Combined Approach To The Esthetic Management of Fluorosed TeethVera CaninaNo ratings yet
- 06 Perineum GenitaliaDocument24 pages06 Perineum GenitaliaRoger ViloNo ratings yet
- Pi Is 0733862722000797Document12 pagesPi Is 0733862722000797Hames SeguraNo ratings yet
- Guyton Hall PHYSIOLOGY Chapter 9 PDFDocument8 pagesGuyton Hall PHYSIOLOGY Chapter 9 PDFOsman NazirNo ratings yet
- 2 Dilemma of Inferior TurbinateDocument17 pages2 Dilemma of Inferior TurbinateputrivbpNo ratings yet
- PulmDocument11 pagesPulmNia IarajuliNo ratings yet
- ERMP 2019-Part I (Document20 pagesERMP 2019-Part I (Nesreden Jemal KedirNo ratings yet
- Anatomia de Puntos Craneometricos PDFDocument35 pagesAnatomia de Puntos Craneometricos PDFAlberto SalazarNo ratings yet
- PIIS0889540612002740Document13 pagesPIIS0889540612002740Aly OsmanNo ratings yet
- Introductiontoclinicalyears 120903072338 Phpapp01Document58 pagesIntroductiontoclinicalyears 120903072338 Phpapp01Atik Badshah SHAIKHNo ratings yet
- Ex Fix Safe Zone For LE by Fahad AJDocument1 pageEx Fix Safe Zone For LE by Fahad AJAlHasaNo ratings yet
- Histology of Heart and Vessels - ANAT3888 - 2023Document41 pagesHistology of Heart and Vessels - ANAT3888 - 2023RachaelNo ratings yet
- Lateral Tendon Disorders Peroneal Tendinopathy Differential DiagnosisDocument5 pagesLateral Tendon Disorders Peroneal Tendinopathy Differential Diagnosischu_chiang_3No ratings yet
- MedetomidineDocument4 pagesMedetomidineHanifa Agus SetyawanNo ratings yet
- Romsons-All-Product CATALOG PDFDocument53 pagesRomsons-All-Product CATALOG PDFrendysamanosuke71% (7)
- Post Partum Hemorrhage (PPH) : Nasheel Kaur Gill Supervisor: DR KosillaDocument40 pagesPost Partum Hemorrhage (PPH) : Nasheel Kaur Gill Supervisor: DR KosillaHaziq MarsNo ratings yet
- Coronary Artery Stent Thrombosis - Incidence and Risk Factors - UpToDateDocument21 pagesCoronary Artery Stent Thrombosis - Incidence and Risk Factors - UpToDateCarlos Rubio LópezNo ratings yet
- A MCQ: Si - No Sub Topics NameDocument2 pagesA MCQ: Si - No Sub Topics NameInzamamul Haque ShihabNo ratings yet
- 11 Maxillofacial SBADocument50 pages11 Maxillofacial SBAArjun KumarNo ratings yet
- Traumatic Injury of The Eye (Blunt (A)Document33 pagesTraumatic Injury of The Eye (Blunt (A)Xavier Irey BakasaNo ratings yet
- Tonsillotomy - Partial - and Complete Tonsillectomy Surgical TechniqueDocument18 pagesTonsillotomy - Partial - and Complete Tonsillectomy Surgical Techniquearsalan adilNo ratings yet
- Arthroscopic Bankart RepairDocument14 pagesArthroscopic Bankart RepairDavid Paul RajNo ratings yet
- Approved Hospitals Attendants PDFDocument59 pagesApproved Hospitals Attendants PDFsthnmNo ratings yet
- Chapter 1.differential Diagnosis and Treatment of Epigastric Dyspepsia SyndromeDocument86 pagesChapter 1.differential Diagnosis and Treatment of Epigastric Dyspepsia SyndromeShravan SharmaNo ratings yet
- Test 1 - General & Oral Anatomy & Physiology (Student Copy)Document5 pagesTest 1 - General & Oral Anatomy & Physiology (Student Copy)dr.jah9No ratings yet