Professional Documents
Culture Documents
Management of Patient With Hypertension
Uploaded by
sosono7520 ratings0% found this document useful (0 votes)
5 views32 pagesOriginal Title
Management of patient with hypertension
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
5 views32 pagesManagement of Patient With Hypertension
Uploaded by
sosono752Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 32
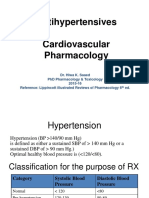
Assessment and Management
of Patients With Hypertension
Adult Health Nursing 1
Blood Pressure
• Blood Pressure = Cardiac Output x Peripheral Resistance
• Cardiac Output = Heart Rate x Stroke Volume
Hypertension
• High blood pressure
• Defined by the Seventh Report of the Joint National Commission on
the Prevention, Detection, Evaluation, and Treatment of High Blood
Pressure (JNC 7) as a systolic pressure greater than 140 mm Hg and a
diastolic pressure greater than 90 mm Hg. based on the average of
two or more accurate blood pressure measurements taken during
two or more contacts with a health care provider
Classification of Blood Pressure for Adults Age
18 and Older
Incidence of Hypertension—
“The Silent Killer”
• Primary hypertension.
• Secondary hypertension.
• 28–31% of the adult population of the U.S. has
hypertension.
• 90–95% of this population with hypertension has
primary hypertension.
• In Jordan the prevalence is 33.8% among men and
29.4% among women
Primary: Essential Hypertension
• Cause of essential hypertension is unknown; however, there are
several areas of investigation:
• a. Hyperactivity of sympathetic vasoconstricting nerves.
• b. Presence of vasoactive substance released from the arterial
endothelial cells, which acts on smooth muscle, sensitizing it to
vasoconstriction.
• c. Increased cardiac output, followed by arteriole constriction.
• d. Excessive dietary sodium intake, sodium retention, insulin
resistance, and hyperinsulinemia play roles
Secondary hypertension
• 1- Renal pathology:
• a. Chronic kidney disease, congenital ,pyelonephritis, renal artery
stenosis, acute and chronic glomerulonephritis
• b. Reduced blood flow to kidney causes release of renin. Renin reacts
with a serum protein to form angiotensin I, which is converted to
angiotenin II through the action of angiotensin-converting enzyme in
the lungs, leading to vasoconstriction and increased salt and water
retention.
• 2. Stenosis of aorta—The kidneys release renin when they sense
hypotension.
3. Endocrine disturbances:
a. tumor of the adrenal gland that causes release of
epinephrine and norepinephrine and a rise in BP (extremely
rare).
b. Adrenal cortex tumors lead to an increase in aldosterone
secretion (hyperaldosteronism) and an elevated BP (rare).
c. Cushing’s syndrome leads to an increase in adrenocortical
steroids (causing sodium and fluid retention) and
hypertension.
d. Hyperthyroidism causes increased cardiac output.
4. Obstructive sleep apnea causes nocturnal
hypertension, which leads to sustained daytime
hypertension.
5. Prescription medications such as estrogens and
steroids (cause fluid retention), sympathomimetics
(cause vasoconstriction
Factors Involved in the Control of Blood
Pressure
Factors that Influence the Development of
Hypertension
• Increased sympathetic nervous system activity
• Increased reabsorption of sodium chloride and water by the
kidneys
• Increased activity of the rennin-angiotensin system
• Decreased vasodilatation
• Insulin resistance:(insulin has role in vessel wall decrease
relaxation by effect on secretion of nitric oxide)
Manifestations of Hypertension
• Usually NO symptoms other than elevated blood pressure
• Symptoms seen related to organ damage are seen late and
are serious
• Retinal and other eye changes
• Renal damage
• Myocardial infarction
• Cardiac hypertrophy
• Stroke
Major Risk Factors of Hypertension
• Smoking
• Obesity
• Physical inactivity
• High blood lipid
• Diabetes mellitus
• Microalbuminuria or GFR < 60
• Older age
• Family history
Patient Assessment
• History and Physical assessment
• Laboratory tests
• Urinalysis
• Blood chemistry: BUN, lipid, electrolytes
• ECG
Treatment
• Usually initial medication treatment is a thiazide diuretic.
• Low doses are initiated and the medication dosage is
increased gradually if blood pressure does not reach target
goal.
• Additional medications are added if needed.
• Multiple medications may be needed to control blood
pressure.
• Lifestyle changes initiated to control BP must be maintained.
Medications
• Diuretic and related drugs
• Thiazide diuretics
• Loop diuretics
• Potassium sparing diuretics
• Aldosterone receptors blockers
• Central alpha2-agonists and other centrally acting
drugs(inhibit norepinephrine)
• Beta-blockers
• Alpha and beta blockers
Medications
• Vasodilators
• Angiotensin-converting enzyme (ACE) inhibitors
• Angiotenisin II antagonists
• Calcium channel blockers
Life style medication
• Weight loss
• Educed sodium intake
• Regular physical activity
• Diet: high in fruits, vegetables, and low-fat dairy
• DASH (dietary approach to stop hypertension) diet: is rich in
fruits, vegetables, whole grains, and low-fat dairy foods;
includes meat, fish, poultry, nuts and beans; and is limited in
sugar-sweetened foods and beverages, red meat, and added
fats
Complications of hypertension
Nursing History and Assessment
• History and risk factors
• Assess potential symptoms of target organ damage
• Angina, shortness of breath, altered speech, altered
vision, nosebleeds, headaches, dizziness, balance
problems, nocturia
• Cardiovascular assessment: apical and peripheral pulses
• Personal, social, and financial factors that will influence the
condition or its treatment
Nursing Diagnosis
• Knowledge deficit regarding the relation of the treatment
regimen and control of the disease process
• Noncompliance with therapeutic regimen related to side
effects of prescribed therapy
Nursing Planning
• Patient understanding of disease process
• Patient understanding of treatment regimen
• Patient participation in self-care
• Absence of complications
Nursing Intervenstions
• Patient teaching
• Support adherence to the treatment regimen
• Consultation/collaboration
• Follow-up care
• Emphasize control rather than cure
• Reinforce and support lifestyle changes
• A lifelong process
• Hypertensive emergency
• Blood pressure > 180/120 and must be lowered
immediately to prevent damage to target organs
Clinical manifestations
• Brain effects: a. Encephalopathy. b. Stroke. c. Progressive headache,
stupor, seizures.
• 2. Kidney effects: Decreased blood flow, vasoconstriction. Elevated
BUN. Increased plasma renin activity. Lowered urine-specific gravity.
Proteinuria. Renal failure.
• 3. Cardiac effects:
• a. Left-sided heart failure.
• b. Acute MI.
• c. Right-sided heart failure
Treatment
• Reduce BP 25% in first hour.
• Reduce to 160/100 over 6 hours.
• Then gradual reduction to normal over a period of days.
• Exceptions are ischemic stroke and aortic dissection.
• Medications
• IV vasodilators: sodium nitroprusside, nicardipine, fenodopam mesylate,
enalaprilat, nitrogylcerin
• Need very frequent monitoring of BP and cardiovascular status.
You might also like
- Hypertension HTNDocument42 pagesHypertension HTNpeter dymonNo ratings yet
- HypertensionDocument14 pagesHypertensiondrraziawardakNo ratings yet
- 2.1.1 HypertensionDocument14 pages2.1.1 HypertensionMUNEZERO EvaseNo ratings yet
- The Overview of Hypertension 2009Document50 pagesThe Overview of Hypertension 2009YeniNo ratings yet
- Hypertension LecturesDocument65 pagesHypertension LecturesAdebisiNo ratings yet
- Ch. 32 - Hypertension - EditedDocument43 pagesCh. 32 - Hypertension - Editedمحمد الحواجرةNo ratings yet
- Chemical Pathology of HypertensionDocument37 pagesChemical Pathology of Hypertensionp6hccq6jd7No ratings yet
- Hypertension PDFDocument85 pagesHypertension PDFDoogie ReynaldoNo ratings yet
- B HypertensionDocument15 pagesB Hypertensionabotawfeq abojalilNo ratings yet
- Scenario ThreeDocument25 pagesScenario Threeapi-3831474No ratings yet
- 6 Hypertension Nursing Care - Arif Setyo UpoyoDocument40 pages6 Hypertension Nursing Care - Arif Setyo UpoyoRizka Nur AgustinNo ratings yet
- Presented by Asmaa Abdelhameed AhmedDocument24 pagesPresented by Asmaa Abdelhameed AhmedSoma Al-mutairiNo ratings yet
- CH 33 Key PointsDocument4 pagesCH 33 Key PointsKara Dawn MasonNo ratings yet
- Measure Blood Pressure CorrectlyDocument56 pagesMeasure Blood Pressure CorrectlyAnna HaritonencoNo ratings yet
- Hypertension: Rojina Bhurtel Lecturer MmihsDocument36 pagesHypertension: Rojina Bhurtel Lecturer MmihsRojina Bhurtel100% (2)
- Hypertension For EMS ProvidersDocument35 pagesHypertension For EMS ProvidersPaulhotvw67100% (5)
- Nutrition and Hypertension Pa Tho GenesisDocument32 pagesNutrition and Hypertension Pa Tho GenesisLa Ode RinaldiNo ratings yet
- Team 1Document15 pagesTeam 1fauzi hardyNo ratings yet
- AAN 204 CARDIOVASCULAR NURSING COURSEWORKDocument118 pagesAAN 204 CARDIOVASCULAR NURSING COURSEWORKLucian CaelumNo ratings yet
- Hypertension: Hozan Jaza MSC Clinical Pharmacy College of Pharmacy 10/12/2020Document81 pagesHypertension: Hozan Jaza MSC Clinical Pharmacy College of Pharmacy 10/12/2020Alan K MhamadNo ratings yet
- Hypertension GuideDocument25 pagesHypertension GuideBulborea MihaelaNo ratings yet
- Hypertension: Prepared By: Dr. Shadab Kashif R.PH, M.SC (UK)Document18 pagesHypertension: Prepared By: Dr. Shadab Kashif R.PH, M.SC (UK)Ahmad Jamal HashmiNo ratings yet
- Hypertension OutlineDocument14 pagesHypertension OutlineMaria CayacoNo ratings yet
- Hypertension: by Krikor Jabourian Nakhleh Nehmeh Yara YounesDocument33 pagesHypertension: by Krikor Jabourian Nakhleh Nehmeh Yara YounesHamza DibNo ratings yet
- HypertensionDocument52 pagesHypertensionWahyunitadotokaNo ratings yet
- DocumentDocument10 pagesDocumentMulhma AlharbiNo ratings yet
- Hypertension: Margaret Xaira R. Mercado RNDocument36 pagesHypertension: Margaret Xaira R. Mercado RNMargaret Xaira Rubio MercadoNo ratings yet
- Young Hypertension FinalDocument27 pagesYoung Hypertension FinalMiyuru HasarangaNo ratings yet
- HT PDFDocument5 pagesHT PDFmist73No ratings yet
- Antihypertensive Drugs GuideDocument52 pagesAntihypertensive Drugs GuideAlan LealNo ratings yet
- Pharmacotherapy of HypertensionDocument52 pagesPharmacotherapy of HypertensionDrVinod Kumar Goud VemulaNo ratings yet
- Hypertension 1Document44 pagesHypertension 1intanNo ratings yet
- 3 HypertensionDocument26 pages3 Hypertensionsamar yousif mohamedNo ratings yet
- Hypertension and Dietary ManagementDocument81 pagesHypertension and Dietary ManagementSophie RoseNo ratings yet
- Gerontic Nursing: Elderly With Hypertension: Arranged Group 11: Suci Aulia (1714201042)Document15 pagesGerontic Nursing: Elderly With Hypertension: Arranged Group 11: Suci Aulia (1714201042)anisaNo ratings yet
- Clinical Research: Hypertension ManagementDocument4 pagesClinical Research: Hypertension ManagementJay Linus Rante SanchezNo ratings yet
- Pharmacotherapy - Hypertension - Dr. Mohammed KamalDocument85 pagesPharmacotherapy - Hypertension - Dr. Mohammed KamalMohammed KamalNo ratings yet
- Classification: HypertensionDocument13 pagesClassification: HypertensiontermskipopNo ratings yet
- Heart FailureDocument28 pagesHeart FailureaparnaNo ratings yet
- HypertensionDocument39 pagesHypertensionMa. Jewon LAGGUINo ratings yet
- Hipertensión Septiembre UMD 2023Document82 pagesHipertensión Septiembre UMD 2023Roberto TicasNo ratings yet
- HypertensionDocument39 pagesHypertensionapi-648595816No ratings yet
- Hypertension Treatment GuideDocument54 pagesHypertension Treatment GuidePatrick CommettantNo ratings yet
- Hypertension in Children GuideDocument25 pagesHypertension in Children GuidenonnyNo ratings yet
- Health Teaching PlanDocument10 pagesHealth Teaching PlanMariel Colminas100% (2)
- HypertensionDocument58 pagesHypertensionSHAHALOMGIR AHMEDNo ratings yet
- 1 - HTNDocument15 pages1 - HTNRawabi rawabi1997No ratings yet
- Hypertensive EmergencyDocument35 pagesHypertensive EmergencyABDIRAHIM ADAMNo ratings yet
- HypertensionDocument6 pagesHypertensionMatthew Michael100% (1)
- HypertensionDocument5 pagesHypertensionacissej_o3No ratings yet
- HypertensionDocument44 pagesHypertensionasadcabdi613No ratings yet
- BiologyDocument15 pagesBiologymeerabwarraich9112No ratings yet
- L12 HypertensionDocument9 pagesL12 HypertensionEslam Ibrahiem IbrahiemNo ratings yet
- Cardiovascular Drugs: Dr. April Dawn R. LuceroDocument122 pagesCardiovascular Drugs: Dr. April Dawn R. LuceroRjDNo ratings yet
- Diagnosis and Management of HypertensionDocument35 pagesDiagnosis and Management of HypertensionBasil Hussam100% (2)
- HypertensionDocument5 pagesHypertensionhamporkNo ratings yet
- HypertensionDocument141 pagesHypertensionAseelNo ratings yet
- Hypertension: Pathophysiology, Diagnostic Test, Medical Management, and Nursing Care PlanDocument12 pagesHypertension: Pathophysiology, Diagnostic Test, Medical Management, and Nursing Care PlanMaulidyaFadilahNo ratings yet
- HTN Presentation CHOs 2022Document34 pagesHTN Presentation CHOs 2022abdulrahmanbelewa96No ratings yet
- TUMOR MARKERS (Hand-Out) EDITDocument36 pagesTUMOR MARKERS (Hand-Out) EDITAliza Dewi FortuaNo ratings yet
- Pocket guide for antimicrobial use in horsesDocument4 pagesPocket guide for antimicrobial use in horsesMd NoumanNo ratings yet
- Jama Oka 2023 CG 230017 1701464130.47792Document2 pagesJama Oka 2023 CG 230017 1701464130.47792Aadityarajsinh GohilNo ratings yet
- Medicine & Pediatric SMLE Notes: Key Points for ExamsDocument23 pagesMedicine & Pediatric SMLE Notes: Key Points for Examsanmar alkhudhri100% (1)
- Post Natal AssessmentDocument8 pagesPost Natal Assessmentmohapatra devNo ratings yet
- Clinical Neurophysiology of The Vestibular System (001-057) PDFDocument57 pagesClinical Neurophysiology of The Vestibular System (001-057) PDFAriel CarterNo ratings yet
- Mayo Paediatricians Manual 4th EdDocument153 pagesMayo Paediatricians Manual 4th EdFalah NadeemNo ratings yet
- Drug MetoprololDocument1 pageDrug MetoprololSrkocher0% (1)
- Gastrointestinal Tract Disorders Upper Lower Organ: Stomatitis (Dietcd) Gastritis GerdDocument125 pagesGastrointestinal Tract Disorders Upper Lower Organ: Stomatitis (Dietcd) Gastritis GerdAnonymous rzPX6lUNo ratings yet
- DR Geeta Pangi HypertensionDocument6 pagesDR Geeta Pangi HypertensionSheera EiyraaNo ratings yet
- Clinical Case Report of Upper GI BleedDocument44 pagesClinical Case Report of Upper GI Bleedjoanna fitzmorrisNo ratings yet
- PSSS-1: Christian Rendy C Rendy Andhika Sulaeman Andrianto Susilo Theodorus SuwendiDocument30 pagesPSSS-1: Christian Rendy C Rendy Andhika Sulaeman Andrianto Susilo Theodorus SuwendiSulaeman Andrianto SusiloNo ratings yet
- CASE REPORT: IMMUNE THROMBOCYTOPENIC PURPURA (ITPDocument34 pagesCASE REPORT: IMMUNE THROMBOCYTOPENIC PURPURA (ITPFelinNo ratings yet
- Chronic gastritis and gastroduodenitis causes, symptoms, diagnosisDocument6 pagesChronic gastritis and gastroduodenitis causes, symptoms, diagnosisIvanNo ratings yet
- Derma OSCEDocument3 pagesDerma OSCEUsama El BazNo ratings yet
- NAlduaij Kuwait Snakes MENATOX2009Document19 pagesNAlduaij Kuwait Snakes MENATOX2009dave fowler0% (1)
- Tla1 Midterm BSC100Document3 pagesTla1 Midterm BSC100AXCEL V. ANTOQUENo ratings yet
- Adult Health III Final Study GuideDocument12 pagesAdult Health III Final Study GuideRyanne JNo ratings yet
- Aldosterone's Greatest Effect and RET Proto-Oncogene MutationsDocument35 pagesAldosterone's Greatest Effect and RET Proto-Oncogene Mutationsdoos150% (2)
- Alternating Horner Syndrome: Case Report and Review of The LiteratureDocument4 pagesAlternating Horner Syndrome: Case Report and Review of The LiteratureDanielle SangalangNo ratings yet
- Bee sting linked to Henoch-Schonlein purpura case reportDocument7 pagesBee sting linked to Henoch-Schonlein purpura case reportjoshkelNo ratings yet
- Practical Pain ManagementDocument13 pagesPractical Pain ManagementfrancistsyNo ratings yet
- Precision in MSDocument62 pagesPrecision in MSSnezana MihajlovicNo ratings yet
- A Systemic Review On Tuberculosis: SciencedirectDocument17 pagesA Systemic Review On Tuberculosis: Sciencedirectkarol lassoNo ratings yet
- Hepatic EncephalopathyDocument65 pagesHepatic Encephalopathyvishal padwaleNo ratings yet
- Managing Urolithiasis: Treatment and Nursing Care for Kidney StonesDocument34 pagesManaging Urolithiasis: Treatment and Nursing Care for Kidney StonesChandrashekar N.k.No ratings yet
- CNS case proforma for stroke evaluationDocument2 pagesCNS case proforma for stroke evaluationRiyaSingh100% (1)
- MATERNALDocument14 pagesMATERNALjhenwilliamsNo ratings yet
- All Conditions Data NCTDocument506 pagesAll Conditions Data NCTMuneer Ashraf0% (1)
- Preparing For The Long-Haul Autonomic Complications of COVID-19Document9 pagesPreparing For The Long-Haul Autonomic Complications of COVID-19Lenin SandovalNo ratings yet