Professional Documents
Culture Documents
Paper 1 de Discusión Semana 2
Uploaded by
Jairo GuachamínOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Paper 1 de Discusión Semana 2
Uploaded by
Jairo GuachamínCopyright:
Available Formats
633
REVIEWS
HPV Infection in Women: Psychosexual Impact of Genital Warts
and Intraepithelial Lesions
Alessandra Graziottin, MD,* and Audrey Serafini, MD†
*H. San Raffaele Resnati Center of Gynecology and Medical Sexology, Milan, Italy; †IRCCS San Raffaele Department of
Obstetrics and Gynecology, Milan, Italy
DOI: 10.1111/j.1743-6109.2008.01151.x
ABSTRACT
Introduction. Genital Human Papillomavirus (HPV) infection is the most commonly occurring sexually transmitted
viral infection in humans. HPV is a wide family of DNA viruses, which may cause benign skin and mucosal tumors
(genital, anal, or oral warts), intraepithelial neoplasias, and/or malignant cancers in different organs. Women are
more susceptible to the oncogenic effect of HPVs, mostly at the genital site on the uterine cervix.
Aims. This review analyzes the impact of: (i) genital warts (GWs) and their treatment; (ii) HPV-related genital, oral,
and anal precancerous lesions on women’s sexual function.
Methods. A Medline search was carried out. Search terms were HPV, GWs, intraepithelial neoplasia, cervical cancer,
anal cancer, oral cancer, epidemiology, HPV risk factors, sexual dysfunctions, desire disorders, arousal disorders,
dyspareunia, vulvar vestibulitis, vulvodynia, orgasmic difficulties, sexual repertoire, couple sexual problems, depres-
sion, anxiety, pap smear, screening program, therapy, and vaccines.
Main Outcome Measures. Sexual consequences of HPV infection in women, specifically GWs and intraepithelial
HPV-related neoplasia.
Results. Psychosexual vulnerability increases with number of recurrences of HPV infections. Depression, anxiety,
and anger are the emotions most frequently reported. However, to date, there is no conclusive evidence of a specific
correlation between HPV infection and a specific female sexual disorder. The relationship between HPV and vulvar
vestibulitis/vulvodynia-related dyspareunia seems not to be direct. Counseling problems, the role of anti-HPV
vaccine, and the concept of the high-risk partner are discussed. The reader is offered a practical approach with
clinically relevant recommendations that may prove useful in his/her daily practice when dealing with HPV-infected
women and couples.
Conclusion. The evidence of psychosexual consequences of HPV-related GWs and intraepithelial lesions is limited.
Specific research on the sexual impact of GWs and intraepithelial HPV-related lesion in women is urgently needed.
Graziottin A, and Serafini A. HPV infection in women: Psychosexual impact of genital warts and intraepi-
thelial lesions. J Sex Med 2009;6:633–645.
Key Words. HPV; Genital Warts; Intraepithelial Neoplasia; Cervical Cancer; Anal HPV Infection; Oral HPV
Infection; Female Sexual Dysfunctions; Dyspareunia; Psychosexual Issues; HPV Vaccine; High-Risk Partners;
Anxiety; Depression
Introduction or oral warts), or malignant cancers in different
organs. Women are more susceptible to the onco-
G enital Human Papillomavirus (HPV) infec-
tion is the most commonly occurring sexu-
ally transmitted viral infection in humans [1]. HPV
genic effect of HPVs, mostly at the genital site and
on the uterine cervix [2].
The literature on HPVs is substantial and
is a wide family of DNA viruses that may cause increasing. The main areas of research include the
benign skin and mucosal tumors (genital, anal, virological characteristics of HPVs, epidemiology,
© 2009 International Society for Sexual Medicine J Sex Med 2009;6:633–645
634 Graziottin and Serafini
medical and oncological impact of the infection with the clinical experience of the authors (implied
and related diseases, prevention strategies through when no data are referenced). Key articles and
appropriate barrier contraception, pap smear reviews are summarized in primis to give the reader
screening, and the potential role of vaccines [3,4]. a full, although concise understanding of the main
However, research investigating the relation- characteristics of HPVs, mechanisms of action,
ship between HPV infections and sexual dysfunc- mode of infection, prevention, principles of diag-
tions in women is limited. It is only in recent years nosis, and treatment, and after that, the literature
that research in this area has increased. This has review was focused on HPV infection’s conse-
occurred in parallel with the growing rate of infec- quences on women’s psychosexual health. The
tions and consequent psychosocial burden. search was conducted in Pub Med. Explicit search
HPV-related diseases may have a significant terms that enable the search to be replicated were
impact on women’s sexuality because: used. They include: HPV, GWs, intraepithelial
neoplasia, cervical cancer, anal cancer, oral cancer,
1. It is a sexually transmitted disease (STD)
epidemiology, HPV risk factors, sexual dysfunc-
particularly affecting the vulva and the
tions, desire disorders, arousal disorders, dyspareu-
uterine cervix. For biological, emotional, and
nia, vulvar vestibulitis, vulvodynia, orgasmic
symbolic reasons, they are the key organs for
difficulties, sexual repertoire, couple sexual prob-
women’s eroticism. HPV-related disorders may:
lems, medical comorbidities, psychosexual issues,
(i) threaten personal and genital health; (ii)
anxiety, depression, pap-smear, screening program,
convey the sense of something degrading,
therapy, and vaccines. There was no restriction
and/or a connotation of stigma, which may
on geographic setting. The search was limited to
induce the woman to feel ashamed, “dirty”, and
English literature.
inadequate [5–14]; and (iii) question the health
A total of 123 studies was collected. Abstracts
of the partner and his loyalty and commitment
and articles were reviewed independently by the
to the couple, thus potentially affecting sexual
authors. A final list of articles was then deter-
function and raising critical issues for the rela-
mined. Only 17 articles investigated HPV infec-
tionship [8].
tion’s psychosexual consequences as their primary
2. It may contribute to vulvodynia and sexual pain
aim. However, only one was a controlled study [9].
disorders, namely dyspareunia, associated with
Given the paucity of the controlled studies, all 17
and/or consequent to vulvar laser treatment
studies were considered, and the level of evidence
[15].
was defined as follows: 1a—systematic review of
3. It is a potentially oncogenic disease, which may
randomized controlled trials; 1b—individual ran-
convey a more serious threat for the woman’s
domized controlled trial; 2a—systematic review
genital and general health, specifically increas-
of cohort study; 2b—individual cohort study;
ing fear and anxiety [5–10,12–14]. Worry asso-
3a—systematic review of case-control studies;
ciated with repeated exams and consultations,
3b—individual case-control study; 4—case series;
and invasive and painful treatments, which
5—expert opinion. Editorials and articles with no
increase in case of recurrences, adds further
abstract were excluded.
vulnerability to the woman’s emotional and
sexual well-being [8].
The article will analyze the impact of HPVs
Epidemiology
infections on women’s psychosexual health.
Medical consequences such as urogenital and It is estimated that in the United States alone, 20
proctological comorbidity will be included when million individuals are infected with HPV. Age-
they interfere with the sexuality of the woman and standardized HPV prevalence worldwide has been
the couple. shown to vary, nearly 20 times between popula-
tions, from 1.4% in Spain to 25.6% in Nigeria
[16]. Epidemiological studies suggest that about
Method
80% of women will have acquired genital HPV by
Given the complexity of the topic, this article will age 50, which makes HPV infection the norm
focus on the impact on women’s sexuality of genital rather than the exception [17–19].
warts (GWs) and intraepithelial precancerous Epidemiology of HPV-related lesions is
lesions. The analysis of HPV psychosexual impact further usually differentiated between benign and
relies mainly on levels of evidence 2 and 3, along precancerous/cancerous lesions:
J Sex Med 2009;6:633–645
Psychosexual Impact of HPV Infection in Women 635
GWs many years to develop, with a peak in risk at about
Dinh et al. collected data on GW diagnosis 35–55 years of age [27,28].
history, and on socio-demographic and sexual Cervical cancer is an important cause of lost
behavior variables, from 8,849 sexually active men years of life in relatively young women. World-
and women aged 18 to 59, to determine the per- wide, the ratio of mortality to incidence is 55%,
centage of subjects who reported having been with higher survival rates and with quite good
diagnosed with GWs in the United States from prognosis in low-risk regions but with lower sur-
1999 to 2004. Overall, 5.6% of 18- to 59-year-old vival in developing countries, where many cases
subjects reported having ever been diagnosed with are present at relatively advanced stages [26].
GWs. The percentage resulted higher in women
(7.2%) than in men (4%). GW diagnosis peaked
among 25- to 34-year-old women (10.4%) and 35- Main Characteristics and Mechanism of Action
to 44-year-old men (6.0%) [20]. of HPV
Focusing on women, the incidence of GWs
varies in different countries. Robust epidemiologi- Characteristics
cal data for GWs in Europe comes from the HPVs are a group of small DNA viruses. The
United Kingdom, where GWs are a notifiable double-stranded, circular DNA genomes of all
disease. Epidemiological data for GWs are limited HPVs are approximately 8 kb in size.
for other countries in Europe. In France, a recent To date, over 100 different viral types have been
prospective observational study estimated an identified, and about one-third of these infect epi-
overall incidence of 228.9 ¥ 100,000 in women thelial cells in the genital tract. The viral types that
15–65 years [21]. infect the genital tract fall into two categories:
A population-based cross-sectional study in high risk and low risk. The high-risk types are
69,147 women (18–45 years of age) randomly associated with the development of anogenital
chosen from the general population in Denmark, cancers, while infections by the low-risk HPVs
Iceland, Norway, and Sweden reported that 1 in 10 mainly induce benign GWs [30].
women in the Nordic countries experienced GWs The taxonomic status of HPV types, subtypes,
before the age of 45, with an increasing occurrence and variants is based on the sequence of their L1
in younger birth cohorts [22]. In southern Europe, genes, which differ from each other by at least
a Spanish study found that 16.9% of women aged 10%, 2–10%, and 2%, respectively [31]. L1 genes
16–20 visiting STD clinics were affected by GW determine variations in the protein of the viral
[23]. In Greece, a cross-sectional study performed capsid, i.e., the container of the DNA virus. Vac-
in STD clinics showed that 47% of the sample cines contain the different proteins identifying
of 829 women had GW [24]. A recent Italian genotypes no. 6, 11, 16 and 18, thus inducing
publication estimated the incidence of GWs at antibodies able to selectively protect against the
4.3 ¥ 1,000 women in the general female popula- viruses specifically identified by the protein-
tion attending gynecological visits [25]. number-plate [31] (Box 1).
The virus infects keratinocytes in the basal
Intraepithelial Neoplasia and Cervical Cancer layers of stratified squamous epithelium of critical
HPV types that infect the genital area are classified sexual areas such as mouth, vagina, and anus. Cells
as either oncogenic low-risk (e.g., 6, 11, 42, 43, 44) in the basal layer consist of stem cells and transit-
or oncogenic high-risk types (e.g., 16, 18, 31, 33, amplifying cells that are continuously dividing and
45, 52), according to their associated lesions. provide a reservoir of cells for the suprabasal
High-risk HPV causes almost all cases of regions. HPV infection of these cells leads to the
intraepithelial and invasive cervical cancer (ICC). activation of a cascade of a viral gene expression
This cancer is the second most common cancer that, perturbing the epithelial cell differentiation,
among women worldwide, with an estimated results, at the end of this cell cycle , in the produc-
493,000 new cases and 274,000 deaths in 2002 tion of HPV virions [32].
[26], with 80% of new cases occurring in develop- In fact, normally, when basal cells undergo cell
ing countries [27,28]. Overall, 70% of ICC cases division, the daughter cell that migrates into the
were associated with either HPV16 (55%) or 18 suprabasal compartment withdraws from the cell
(15%). The six next most common types, namely cycle and initiates a program of terminal differen-
HPV31, 33, 35, 45, 52, and 58, accounted for an tiation. However, in HPV-positive human kerati-
additional 18% of cases [29]. These cancers take nocytes and cervical epithelial cells, the suprabasal
J Sex Med 2009;6:633–645
636 Graziottin and Serafini
BOX 1 The New HPV Vaccines: A Hope for the Future
New prophylactic HPV vaccines promise to dramatically reduce the incidence of clinical consequences
of HPV infection, mainly precancerous cervical lesion cervical cancer, and also other precancerous
genital lesions, genital warts, and cytological abnormalities. The quadrivalent vaccine currently
approved by FDA and EMEA utilizes four different “virus-like particles”, thus enabling the immune
system to protect against HPV viruses corresponding to genotypes 6, 11, 16, and 18. This will have a
prophylactic impact on about 90% of condylomata and more than 70% of invasive cervical cancers (the
remaining being caused by others genotypes) [25].
Among children 9–15 years old and young women aged 15–26 years not previously infected with
vaccine-type HPV strains, prophylactic HPV vaccination appears to be highly efficacious [26].
Vaccination is not a substitute for routine cervical screening. Since no vaccine is 100% effective and
not provide protection against non-vaccine HPV types, or against existing HPV infections, routine
cervical screening remains critically important and should follow local recommendations.
The HPV vaccines do not protect against other sexually transmitted diseases, therefore appropriate
precautions against sexually transmitted diseases should continue to be used.
cells continue DNA synthesis and express markers have been recognized as causative agents of cervi-
for cell proliferation [32]. cal, anal, vulvar, and laryngeal cancers. These
Within this suprabasal compartment, cells sexually transmitted viruses are associated with
support the amplification of the viral genome, the more than 70% of cervical cancer cases [34,35].
expression of capsid genes and the assembly of
progeny virus, and the final encapsidation of HPV Clinical Consequences
DNA to generate a new virus occurs within the Clinical sequelae in cases of low-risk HPV infec-
terminally differentiated cell compartment [32]. tion consist of GWs, which can cause significant
Most HPV infections are “cleared” by the physical and psychosocial distress.
immune system and do not result in clinical dis- Respiratory tract papillomatosis are associated
eases [33]. The majority of sexually active adults with HPV types 6 and 11; these HPV types are also
will be infected with HPV at least once in their commonly associated with GWs. The incidence of
lives. However, sexually active women less than 25 respiratory tract papillomatosis in young adults is
years of age consistently have the highest rates of increasing [36–38]. It has been postulated that oro-
infection [32]. The anatomical characteristics of genital contact is the means of transmission in this
the female genital tract, mainly in the genital age group. In view of the high infectivity of GWs,
mucosal histology, may in part explain female vul- it is interesting to note the low prevalence of
nerability for clinical sequelae. oro-pharyngeal warts in adults indulging in oro-
Precise mechanisms determining the final genital contact. Clinical manifestations of high-risk
outcomes are currently unknown. When immu- HPV cervical infection include a wide range of
nocompetence is weakened and/or the virus cytological/hystological abnormalities, like abnor-
belongs to one of the more aggressive oncogenic mal pap test results, low-grade squamous intra-
subtypes, cancer may finally occur [34]. In epithelial lesions (LSIL), high-grade squamous
the case of high-risk HPV infection that cause intraepithelial lesions (HSIL), and cervical cancer.
cervical cancer development, the viral life cycle is Other genital sites, such as vulvar and vaginal, could
perturbed in two ways: the loss of terminal be the target for high-risk (HR) HPV carcinogen-
differentiation on cell cycle that leads to a cellular esis with comparison of precancerous (high-grade
state that cannot support the full viral life vulvar intraepithelial neoplasia [VIN] or vaginal
cycle, and the circular viral DNA genome, which intraepithelial neoplasia [VaIN]) or invasive cancer.
normally resides as a nuclear plasmid, often Oral HPV is strongly associated with oral squa-
becomes integrated into the host genome and mous cell carcinoma, suggesting that HPV-16 and
thereby becomes disrupted and its replication -18 are risk factors for oral cancer [37,38]. A sig-
defective. nificant association with tobacco and alcohol has
Types of HPVs, such as HPV-16, HPV-18, been confirmed. In addition, a family history of
which are designated “high-risk” or “oncogenic,” cancer is associated with OSCC [36–38].
J Sex Med 2009;6:633–645
Psychosexual Impact of HPV Infection in Women 637
Anal HPV infections in women are usually distress, psychological comorbidities, and negative
underestimated because women do not think or sexual outcomes).
report they had unprotected anal sex, and physi-
cians usually do not ask about this sexual practice.
Diagnosis
The health risks of unprotected anal sex appear to
be severely underestimated by a substantial pro- The diagnosis of HPV infection and the clinical
portion of sexually active women and men. Among consequences can be made following an abnormal
heterosexuals, reported rates of condom use are smear test or HPV testing.
almost universally lower for anal than for vaginal Cervical HPV-related lesions are typically
intercourse [39]. A U.S. survey and other data asymptomatic, but in the case of invasive diseases,
suggest that, in terms of absolute numbers, some symptoms like atypical vaginal blood losses,
approximately seven times more women than smelly vaginal discharge, urinary or anorectal
homosexual men engage in unprotected receptive symptoms, and weight loss could arise as conse-
anal intercourse [39]. quences of malignant proliferation and cancer.
Anal intraepithelial neoplasia (AIN) is a con- For GWs, visual inspection is normally suffi-
sequence of chronic HPV infection in the anal cient for diagnosis.
canal and appears to be driven by high viral loads
of HPV. AIN natural history resembles that
Therapy
of cervical intraepithelial neoplasia. Low-grade
lesions frequently resolve, but high-grade lesions Treatments of precancerous HPV-related lesions
are much more stable. HIV-positive men and include a wide range of interventions, according to
women who practice receptive anal intercourse the type and site of lesions, extension, and severity.
are at the highest risk of AIN [40]. The incidence For GWs, both medical and surgical treatments
of AIN has increased significantly in the last are available.
decades [41]. Early and late recurrences of the infection and
Also, the progression of the disease has an related pathologies are frequent. They may have a
impact on sexual health. The sense of a health very different impact from the psychosexual point
threat can be very different depending on the of view, according to the severity of lesions,
grade of the lesions: LSIL vs. HSIL or cancer in aggressiveness of related treatments and their side
situ, as they require a different aggressiveness of effects, frequency of recurrences and their severity,
treatment and follow up. and quality of psychosexual support from relatives
One of the main biases in the studies surveyed is and health care providers.
that they cluster together lesions of all degrees.
Currently, there are neither effective means of pre-
Psychosexual Impact of HPV Infections
venting HPV transmission nor cures for clinical
manifestations: infection can only be totally pre- Despite HPV infection being among the most
vented via complete sexual abstinence. Good but common STDs seen in clinical practice, attention
not total protection is achieved when there is con- has only begun to focus on the psychological or
sistent condom use during every type of intimacy psychosexual impact of this diagnosis on the indi-
(oral, vaginal, anal), and the condom is applied prior vidual. The few studies that exist suggest adverse
to any contact. Prophylactic VLP L1 vaccines are psychological and psychosexual sequelae may be
now available. They protect women against clinical common [43,44].
consequences of some types of HPV. Bivalent and Regarding the evaluation of the specific psycho-
quadrivalent formulations protect from HPV sexual impact for different forms of clinical HPV
16,18-related cervical cancer and high-grade cervi- sequelae, while much research has been published
cal intraepithelial neoplasia. Quadrivalent formu- on the mode of transmission of HPV-related oral
lations also protect from HPV 6,11,16,18-related lesions, epidemiology, and other oral disease-
vulvar and vaginal precancerous lesion and GWs. related issues, to the author’s knowledge, no
Treatment for clinical sequelae such as GWs and studies have been published on the psychosexual
precancerous cervical lesion consists of removing consequences of oral HPV infections. The same
the problematic cells, decreasing HPV viral load, consideration could be made of HPV-related anal
and watching for recurrence. This method con- lesion; in fact, no specific published literature
sumes significant health care resources and is costly exists on psychosexual consequences of anal HPV
[42]. Some costs are difficult to estimate (personal infections. So the available studies are focused
J Sex Med 2009;6:633–645
638 Graziottin and Serafini
on genital—i.e., vulvar/vaginal/cervical—lesions. was sent to 428 women aged 20–64 to measure
However, oral and anal infections are increasing psychosocial and psychosexual consequences of
and should be investigated from the point of view HPV infection. Anxiety, distress, and feelings
of their potential psychosexual impact as well. about current, past, and future sexual relationships
In the clinical setting, women with flourishing, were also investigated. Women with normal cytol-
massive, disfiguring GWs may express specific ogy who tested positive for HPV were significantly
“cosmetic” concerns, at the risk of persistent more anxious and distressed than HPV-negative
modification of the genitals and fears of being women using both a state anxiety measure
rejected by partners. However, no mention of this F(1,267) = 29, P < 0.0001] and a screening specific
specific issue can be found in the clinical literature measure of psychological distress F(1,267) = 69,
published thus far. Given the increasing focus P < 0.0001]. Women with an abnormal or unsatis-
women have of the cosmetic appearance of their factory smear result who tested HPV positive were
genitals and its impact on their self-image and significantly more distressed than HPV-negative
self-esteem, the cosmetic impact of flourishing women with the same smear result F(1,267) = 8.8,
GWs deserves to be specifically evaluated [45]. P 1/4 0.002], but there was no significant differ-
The evidence emerging from the literature and ence in the state of anxiety. The HPV-positive
from our clinical experience suggests the existence women felt significantly worse about their sexual
of several peaks of vulnerability because of HPV relationships. Approximately one-third of women
infection. Different stages in the diagnosis and who tested positive reported feeling worse about
treatment of HPV infection may have a different past and future sexual relationships compared with
impact on women and couples. The “timing” less than 2% of HPV-negative women.
effect can overlap with a number of variables, Even in this investigation, the findings suggest
causing psychosexual impairment or leading to that testing positive for HPV may have an adverse
overt sexual dysfunctions. psychosocial impact, with increased anxiety, dis-
tress, and concern about sexual relationships [6].
Psychosexual Impact of the Diagnosis To assess the psychosocial impact of HPV
HPV testing may offer a number of advantages to testing as an adjunct to cytology in routine primary
conventional cervical screening, such as increased cervical screening, a controlled study was carried
sensitivity to high-grade precancerous disease, the out. The trial provides a randomized setting of
potential to increase screening intervals for HPV revealed HPV results vs. concealed results permit-
negative women and the reduction of unnecessary ting valid comparisons for assessing true psycho-
colposcopies among women with borderline social impact. The intervention was a revealed
smears. However, HPV testing has been criticized high-risk HPV test result in addition to cervical
for its lack of specificity and the potential for large cytology. The main outcome was measured using
numbers of women to test positive in the absence the General Health Questionnaire (GHQ-28),
of clinically significant cytological abnormality Spielberger State–Trait Anxiety Inventory and
[46,47]. Sexual Rating Scale (SRS). Among women with
Conaglen et al., in their individual case control mildly abnormal or normal cytology, receiving an
study on 101 consecutive clients attending an STD HPV (+ve) result did not impact significantly on
clinic, evaluated with four validated question- GHQ caseness and mean scores or on Spielberger
naires, found that those diagnosed with a first State and Trait scores when compared with women
episode of HPV had considerable psychological in whom the HPV (+ve) test result was concealed.
difficulties (25% of the HPV-positive group com- Among women with normal cytology, receiving an
plained suffering social dysfunction vs. 7.9% of HPV (+ve) result was associated with a reduction in
the HPV-negative group; 17.9% reported severe the sexual rating scale compared with similar
depression vs. 10.5%); 29% of men and 10% of women whose HPV (+ve) result was concealed. We
women with a first episode of GWs could be clas- can conclude that HPV testing does not add sig-
sified as having sexual concerns at their first visit. nificant psychological distress when combined with
However, the diagnosis of HPV was not associated cytology in routine primary cervical screening [9].
with a greater psychological or psychosexual im- Maggino et al. [7] evaluated the impact of
pact than that reported for other sexually trans- the communication of an HPV diagnosis on the
mitted infections [5]. cognitive–behavioral aspect, emotional experi-
Similar results were reported in a study by ences, psychic–physical well-being, and psycho-
McCaffery et al. [6] A postal questionnaire survey sexual sphere in young women between the ages of
J Sex Med 2009;6:633–645
Psychosexual Impact of HPV Infection in Women 639
20 and 45. Three self-evaluating questionnaires ment. The pattern of initial anxiety is modulated
(the Cognitive Behavioral Assessment-20, the by the attitude of the physician: reassuring vs.
SAT-P, and the BISF-W) were administered to 36 neglecting to clarify the most critical questions
women who had been diagnosed with an HPV and/or referring the woman to the net.
infection and 36 women who had never been diag-
nosed with HPV. A total of 36% of the experimen- The only thing that I do go back on is like what is it? If
I keep carrying on, how long will I have it? What will
tal group reacted to the diagnosis with fear, 29% they do for it? What will the long term effects be for
reacted with anxiety, while only 3% of women did me? They’re the questions that go over a lot. The other
things are just fleeting thoughts like now I sit and think
react with anger. Significant differences emerged about it. Could it be that? Could it be this? Every now
and again I’ll think about it for whatever the reason and
in two samples regarding state of anxiety and they’re my thoughts that I always have [8].
obsessive and compulsive aspects, while there were
no significant differences between the two groups Not surprisingly, emotional responses following
regarding the subjective satisfaction with life the second HPV test varied greatly by whether or
quality and sexual function. A significant positive not that test was positive. Negative feelings
correlation was found between the sum of anxiety included fear and anxiety about cancer and becom-
and fear expressed at the time of the diagnosis and ing ill, concerns about fertility, feelings of being
the trait anxiety reported in the CBA-2.0. The unclean because of the sexually transmitted nature
results indicate that the prevalent emotions felt at of HPV, concerns about transmission and sexual
the time of the diagnosis are fear and anxiety. The relationships, a negative impact on feelings about
persons who were diagnosed with an HPV in- sex, and relationship issues including blaming a
fection resulted as having higher levels of trait partner for the infection. Overall, women appeared
anxiety, obsessions, compulsions, and behaviors to be more distressed by a second HPV-positive
and worries related to hygiene [7]. result than a single one, and expressed a clear pre-
To evaluate the psychosocial impact of taking ference for immediate colposcopy over continued
part in repeated testing for HPV, Waller used surveillance [8].
in-depth interviews that were carried out with 30
women who were HPV positive with normal
cytology at trial baseline, and attended for a repeat Psychosexual Impact of the Therapy
HPV test 12 months later [8]. HPV genital lesions’ treatment (physical–chemical
This excellent qualitative study indicates that therapy, diathermocoagulation, and laser therapy
feelings of shock, confusion, and distress about or pharmacological therapy with imiquimod) is
testing HPV positive were common. These feel- usually long and painful and can cause sexual
ings are frequently related to the sexually trans- impairments [43,48]. The higher the number of
mitted nature of HPV and concerns. They were the interventions, the more painful the technique
articulated about: (i) where the virus had come and the severity of the scarring, the more severe is
from; and (ii) anxiety about the health implications the potential psychosexual impact [43,48]. Unfor-
of HPV. Anxiety was triggered by lack of knowl- tunately, while the etiology of the psychosexual
edge about HPV and followed by seeking further impact has been discussed in different articles, con-
information about HPV from the Internet. Once trolled studies on the impact of different therapies
some of the confusion had been resolved, women are lacking. Filiberti assessed the psychological and
seemed able to put the result to the back of their psychodynamic aspects of patients with widespread
mind until the next test. Particularly reassuring genital HPV infection entering into a clinical trial
was the knowledge that the virus could lie dormant in which they were randomly assigned to three
for a long time, so exposure was not necessarily treatment groups: CO2 laser ablation, intramuscu-
recent and its presence did not mean that a partner lar interferon-alpha, and CO2 laser ablation plus
had been unfaithful [8]. intramuscolar interferon-alpha. Results indicated
that 57% of the patients experienced sexual impair-
I mean if he’d had an affair with somebody then I would ments after therapy. The main reasons for sexuality
have been angry and upset. As it is . . . it’s something change were: the disease itself, fear of infecting the
that I think he’s had before our relationship, I trust him
a hundred per cent. partner, pain during the intercourse, and forced
use of condom. Sixteen percent of the patients
Women were also reassured by the fact that reported a worsening of the relationship with the
HPV does not cause symptoms, is highly preva- partner. No difference was found between the dif-
lent, and can clear spontaneously without treat- ferent treatment groups [48].
J Sex Med 2009;6:633–645
640 Graziottin and Serafini
HPV Infection, Vulvodynia, and Dyspareunia Morin [15] found that there was an association
between treatment for vulvar HPV infection and
It seems that a link between GWs and vulvodynia vulvodynia. This can occur when either pharma-
is not due to the clinical HPV-related disease itself cologic (Imiquimod) or physical treatment (either
but as consequences of the treatment of the genital laser or diathermo-coagulation [DTC]) cause per-
lesions. “Vulvodynia is a prevalent and highly dis- sistent introital/vulvar pain as a persistent side
tressing disorder, with major consequences for effect of treatment. This negative outcome is
interpersonal and psychological well-being [49]. common when physical treatment is:
Vulvodynia is a diverse, multifactorial phenom-
enon that impairs the psychological, physical, 1. Extensive, because of the magnitude/extension
and reproductive health of approximately 10% of of the vulvar GWs.
women at some point in their lives [49–53]. The 2. Repeated, because of warts’ recurrence or
management of these patients requires a sensitive re-infection.
provider who can coordinate a multidisciplinary 3. Overzealous (with deep lesions and neuropathic
approach to their care. Despite the lack of large- pain).
scale, placebo-controlled trials, several new treat- 4. Associated with a defensive contraction of the
ment options exist [52,54]. elevator ani, because of the iatrogenic pain.
Two studies, in fact, do not support the associa- This, in turn, can contribute to introital dys-
tion between vulvar HPV infection and vulvodynia pareunia, reflex inhibition of lubrication, vaginal
or vulvar vestibulitis. Smith found that a history dryness and micro-abrasion of the introital
of genital infections is associated with an increased mucosa (during intercourse subsequent to
risk of vulvar vestibulitis syndrome (VVS): bacterial treatment) and chronic introital inflammation
vaginosis (odds ratio, OR = 9.4), Candida albicans leading to vulvar vestibulitis and vulvodynia.
(OR = 5.7), pelvic inflammatory disease (PID)
(OR = 11.2), trichomoniasis (OR = 20.6), and
The Silent Carrier or the High-Risk Man:
vulvar dysplasia (OR = l5.7), but no risk associated
The He-Partner
with HPV, atypical squamous cells of undeter-
mined significance, cervical dysplasia, GWs, A specific issue to be dealt with when counseling
chlamydia, genital herpes, or gonorrhea [55]. women which HPV infections relates to “who
Gaunt et al. investigated the prevalence of HPV infected whom” [8]. This question becomes more
in patients with VVS by using a polymerase chain painful when oncogenic HPV strains are etiologi-
reaction (PCR) primer set that detects known cally related to precancerous lesions that can
HPV types. They retrospectively identified 38 progress to cervical or vulvar cancer [7,8]. Studies
patients with VVS who underwent therapeutic assessing the carrier or infected status of partners
surgical excision of the vestibule. Eleven controls of HPV-infected women indicate that subclinical
without vestibulitis who underwent vestibular lesions are far more common than diagnosed by
excision for conditions unrelated to HPV infection simple visual genital examination [57,58].
were identified prospectively. Surgical specimens Penile lesions were seen in 68% of the male
were examined for the presence of HPV DNA by sexual partners of women with intraepithelial cer-
PCR amplification. DNA sequencing was used to vical neoplasia, when examined by visual inspec-
determine HPV type. They found that the preva- tion, or when available, with the colposcopic
lence of HPV among patients with VVS was 21 instrument. More than one lesion type was diag-
vs. 36% among controls. Group B HPV types nosed in 15% of cases. Flat lesions, papular lesions,
accounted for 4 of the 10 (40%) HPV types found and condylomata acuminata were seen in 83%,
in patients with VVS. Overall, in both patient and 29%, and 4% of cases, respectively. HPV was
control samples, a spectrum of HPV types were detected in 59% of the penile scrapings, containing
identified, encompassing many branches of the mainly oncogenic HPV types. When penile lesions
HPV phylogenetic tree. No etiologic association were present, 67% of penile scrapings were positive
was apparent. The low rate of observed infection for HPV, whereas 37% were HPV-positive when
in women with and without VVS and the diversity no lesions were visible. Penile lesions are frequently
of HPV types identified suggest incidental virus found in sexual partners of women with cervical
carriage rather than direct cause and effect. The intraepithelial neoplasia, when appropriately exam-
underlying cause of this debilitating condition ined. Most of these lesions are subclinical (i.e., only
remains unknown [56]. visible after acetowhite staining and/or with HPV
J Sex Med 2009;6:633–645
Psychosexual Impact of HPV Infection in Women 641
DNA test of the partner). They are often associated Many search for information on the Internet and
with the presence of high-risk HPV, indicating that report being even more scared. Partners may
male sexual partners of women with cervical present with a wide range of negative affects that
intraepithelial neoplasia might constitute a reser- should be addressed in parallel [12]. Ensuring that
voir for high-risk HPV [57,58]. women are aware that HPV is a common condi-
tion and limiting potential negative consequences
by appropriate follow up and medical interven-
Discussion
tions (when needed) may reduce the negative feel-
Women have a gender-specific vulnerability to the ings and anxiety experienced by women with HPV
health and sexual consequences of HPV infections. [13].
They have almost twice the percentage of GWs in Clinical experience indicates that women with a
comparison with men [20]. Women have a higher satisfying sexuality before the HPV diagnosis are
vulnerability to oncogenic HPV, mostly at cervical those less vulnerable to the long-term negative
and vulvar site. (The age-standardized incidence consequences of GWs and their treatments.
of vulvar cancer averages between 1 and 2 per However, controlled studies are needed to support
100,000 women in Western countries. Epidemio- this claim. Vulnerability increases in women expe-
logical studies have identified sexual factors, par- riencing dysfunctional sexuality prior to diagnosis,
ticularly HPV infection, as increasing risk) [59]. in single women, in women with troubled relation-
The health and sexual risks linked to HPV ships, or when the infection strongly suggests the
infections are currently underestimated by women partner has had unprotected sex outside of the
themselves. relationship [8]. Clinical correlates include loss of
Research on the specific impact of GWs and sexual desire, more difficult mental and genital
intraepithelial neoplasias on sexual function and arousal, dyspareunia, less frequent intercourse,
relationship in women is limited. Research focuses and a qualitative and quantitative reduction of the
more on general psychological outcomes, such as repertoire of sexual behaviors. After HPV genital
depression, anxiety, guilt, anger, rage, or sexuality infection, many women refuse further passive oral
as a general issue rather than focusing on specific sex for fear of infecting their partner.
dimensions of women’s sexuality [5–14]. To the Overall, preliminary data indicate that sexual
author’s knowledge, no studies using validated morbidity is more correlated to frequency of
sexual questionnaires, such as the Female Sexual recurrences than to different treatments per se
Function Index or Profile of Female Sexual Func- [48]. Prevention and early diagnosis of recurrences
tion, have been published. The only disorder may reduce the long-term sexual consequences of
investigated to explore if it could be related to HPV infection in women. Active counseling on
HPV infection is dyspareunia via the link with potential female sexual dysfunctions worsened or
vulvodynia/vulvar vestibulitis. However, the rela- precipitated by HPV infection should be part of
tionship between HPV and vulvar vestibulitis- the routine medical approach.
related dyspareunia appears to be eventually a Physicians should also actively investigate pre-
sequelae of the HPV-related diseases treatment vious unprotected anal sex in women with genital
rather than the HPV infection itself [15,55,56]. HPV infection, to avoid the collusion of silence
In previous studies, couple-related psychosexual and the risk of undiagnosed highly aggressive AIN
issues have only been explored as part of a broader [39–41]. After the diagnosis of perianal or anal
analysis, with no follow-up studies specifically HPV-related diseases, many refuse any further
examining couple outcomes after treatment for anal intimacy. In the clinical setting, the most fre-
GWs or intraepithelial neoplasia. quently reported feeling is a sense of guilt, anal sex
More data have been produced on the impact of still being considered in many countries as inap-
HPV diagnosis on the emotional and psychosexual propriate or even transgressive.
well-being. Health care providers should actively inform
Communicating the diagnosis, through correct women against the risk of unprotected anal sex.
and exhaustive information on HPV infection and Women are frequently very disturbed to dis-
its psychosexual meaning, should be consistently cover that a partner they loved may have infected
offered by the clinician to HPV-positive women them. “What is the role of men who are sexual
and their partners (if the couple is willing to be partners of women with genital HPV infection
consulted together). Many women are surprised and/or cancer?” This is a sensitive question
and upset upon learning about HPV [5–7,10]. increasingly raised in clinical consultation by
J Sex Med 2009;6:633–645
642 Graziottin and Serafini
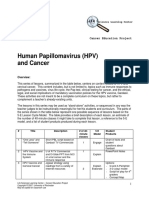
Table 1 HPV infection risk factors and gender vulnerability in women
Youth Moscicki Ab, 2007 [63].
Saleh MM, Seoud AA, Zaklama MS, 2007 [64].
Winer Rl, Feng Q, Hughes JP et al., 2008 [65].
Gender (female) Steben M, Duarte-Franco E, 2007 [66].
Hariri S, Dunne EF, Sternberg M, et al., 1991 [74].
Dinh TH, Sternberg M, Dunne EF, 2008 [20].
High number of sexual partners Moscicki Ab, 2007 [63].
Saleh MM, Seoud AA, Zaklama MS, 2007 [64].
Winer Rl, Feng Q, Hughes JP et al., 2008 [65].
Non-consistently protected sex Epstein RJ, 2005 [67].
Co-infection with chlamydia trachomatis Anttila T, Saikku P, Koskela P, et al. 2001 [68].
Bosch FX, de Sanjosè S., 2007 [69].
Ault KA, 2006 [32].
Co-infection with herpes simplex virus Smith JS, Herrero R, Bosetti C, et al., 2002 [70].
Bosch FX, de Sanjosè S., 2007 [69].
Smoking Castellsaguè X, Munoz N. 2003 [71].
Bosch FX, de Sanjosè S., 2007 [69].
Immunosuppression (HIV, immunosuppressive therapy) Strickler HD, Burk RD, Fazzari M, et al. 2005 [72].
Cameron JE, 2007 [73].
Pregnancy Strickler HD, Burk RD, Fazzari M, et al. 2005 [72].
both affected women and their partners [8]. HPV Conclusions
testing of the partner, or penis examination, Women are at an increasing risk of HPV infections
should be considered part of the diagnostic and related lesions, with a specific and underesti-
assessment of partners of HPV-infected women mated vulnerability to the risk of anal infections
[57,58]. The sexual impact of being an inducer or (Table 1). Psychosexual vulnerability increases with
a carrier or HPV infections should be investi- the number of recurrences of HPV infections. Fear,
gated. Psychosexual and informative counseling anxiety, anger, and depression are the emotions
to both partners is critical to prevent further most frequently reported [5–14]. However, to date,
negative psychosexual outcomes during diagnosis there is no conclusive evidence of a correlation
and treatment of HPV-related lesions. Husbands between HPV infection and a specific female sexual
and couples express their relief and gratitude disorder. The relationship between HPV and
when these issues and potential difficulties and/or vulvodynia/vulvar vestibulitis-related dyspareunia
misunderstandings are openly and spontaneously seems indirect [15,55,56]. Anti-HPV vaccine may
raised by the physician during the consultation reduce the incidence of HPV infection and the
and when practical suggestions are given to over- related psychosexual consequences [62]. However,
come physical and emotional problems. Guilty no data have been produced so far on this issue. The
feelings may be pervasive, rooted in the past per- potential of a “high-risk partner” should be consid-
sonal sex life. On the other hand, aggressive feel- ered and diagnosed while counseling HPV-infected
ings against the partner considered responsible women. Specific research on the sexual impact of
for the infection (of having “caught” it) and the GWs and intraepithelial HPV-related lesion in
subsequent precancerous or cancerous lesions women is urgently needed.
may dominate the clinical picture in a minority of
cases [7,60–62]. Individual and couple counseling Corresponding Author: Alessandra Graziottin,
is critical to addressing these feelings that may MD, Via Enrico Panzacchi 6, 20123 Milano, Italy. Tel:
affect the motivational–affective roots of desire ++39-02-72002177; Fax: ++39-02-876758; E-mail:
and couple commitment. a.graziottin@studiograziottin.it.
Overall, the published data indicate that many Conflict of Interest: None declared.
more questions remain unaddressed than answered
in this emerging field of STDs. More research is
needed on all the aspects that remain neglected in Statement of Authorship
the evaluation of psychosexual outcomes of GWs Category 1
and intraepithelial neoplasias. The evidence is (a) Conception and Design
more consistent regarding the outcomes of treat- Alessandra Graziottin; Audrey Serafini
ments after cervical, genital, and anal cancers. This (b) Acquisition of Data
will be reviewed in a separate article. Alessandra Graziottin; Audrey Serafini
J Sex Med 2009;6:633–645
Psychosexual Impact of HPV Infection in Women 643
(c) Analysis and Interpretation of Data 10 Clarke P, Ebel C, Catotti DN, Stewart S. The psy-
Alessandra Graziottin; Audrey Serafini chosocial impact of human papillomavirus infection:
Implications for health care providers. Int J STD
AIDS 1996;7:197–200.
Category 2 11 Scrivener LD, Green J, Hetherton J, Brook G. Dis-
(a) Drafting the Article closure of anogenital warts to sexual partners. Sex
Alessandra Graziottin; Audrey Serafini Transm Infect 2008;84:179–82.
(b) Revising It for Intellectual Content 12 Harper DM. Why am I scared of HPV? CA Cancer
Alessandra Graziottin; Audrey Serafini J Clin 2004;54:245–7.
13 Waller J, Marlow LA, Wardle J. The association
Category 3 between knowledge of HPV and feelings of stigma,
shame and anxiety. Sex Transm Infect 2007;83:
(a) Final Approval of the Completed Article
155–9.
Alessandra Graziottin; Audrey Serafini
14 Anhang R, Goodman A, Goldie SJ. HPV com-
munication: Review of existing research and recom-
mendations for patient education. CA Cancer J Clin
References
2004;54:248–59.
1 Capra G, Giovannelli L, Bellavia C, Migliore MC, 15 Morin C, Bouchard C, Brisson J, Fortier M,
Caleca MP, Perino A, Ammatuna P. HPV genotype Blanchette C, Meisels A. Human papillomaviruses
prevalence in cytologically abnormal cervical and vulvar vestibulitis. Obstet Gynecol 2000;95:
samples from women living in south Italy. Virus Res 683–7.
2008;133:195–200. 16 Clifford GM, Gallus S, Herrero R, Muñoz N,
2 Paavonen J. Human papillomavirus infection and Snijders PJ, Vaccarella S, Anh PT, Ferreccio C,
the development of cervical cancer and related Hieu NT, Matos E, Molano M, Rajkumar R, Ronco
genital neoplasias. Int J Infect Dis 2007;11 G, de Sanjosé S, Shin HR, Sukvirach S, Thomas JO,
(2 suppl):S3–9. Tunsakul S, Meijer CJ, Franceschi S, IARC HPV
3 Moscicki AB. Conservative management of adoles- Surveys Prevalence Study Group. Worldwide distri-
cents with abnormal cytology and histology. J Natl bution of human papillomavirus types in cytologi-
Compr Canc Netw 2008;6:101–6. cally normal women in the International Agency for
4 Barr E, Gause CK, Bautista OM, Railkar RA, Lupi- Research on Cancer HPV prevalence surveys: A
nacci LC, Insinga RP, Sings HL, Haupt RM. pooled analysis. Lancet 2005;366:991–8.
Impact of a prophylactic quadrivalent human papil- 17 Koutsky LA, Galloway DA, Holmes KK. Epidemi-
lomavirus (types 6, 11, 16, 18) L1 virus-like particle ology of genital human papillomavirus infection.
vaccine in a sexually active population of North Epidemiol Rev 1988;10:122–63.
American women. Am J Obstet Gynecol 2008;198: 18 Myers ER, McCrory DC, Nanda K, Bastian L,
261.e1–11. Matchar DB. Mathematical model for the natural
5 Conaglen HM, Hughes R, Conaglen JV, Morgan J. history of human papillomavirus infection and cer-
A prospective study of the psychological impact on vical carcinogenesis. Am J Epidemiol 2000;151:
patients of first diagnosis of human papillomavirus. 1158–71.
Int J STD AIDS 2001;12:651–8. 19 Gravitt PE, Jamshidi R. Diagnosis and manage-
6 McCaffery K, Waller J, Forrest S, Cadman L, ment of oncogenic cervical human papillomavirus
Szarewski A, Wardle J. Testing positive for human infection. Infect Dis Clin North Am 2005;19:439–
papillomavirus in routine cervical screening: Exami- 58.
nation of psychosocial impact. BJOG 2004;111: 20 Dinh TH, Sternberg M, Dunne EF, Markowitz LE.
1437–43. Genital warts among 18- to 59-year-olds in the
7 Maggino T, Casadei D, Panontin E, Fadda E, United States, national health and nutrition exami-
Zampieri MC, Donà MA, Soldà M, Altoè G. Impact nation survey, 1999–2004. Sex Transm Dis 2008;35:
of an HPV diagnosis on the quality of life in young 357–60.
women. Gynecol Oncol 2007;107(1 suppl 1): 21 Monsonégo J, Breugelmans JG, Bouée S, Lafuma A,
S175–9. Bénard S, Rémy V. Anogenital warts incidence,
8 Waller J, McCaffery K, Kitchner H, Nazroo J, medical management and costs in women consult-
Wardle J. Women’s experiences of repeated HPV ing gynecologists in France. Gynecol Obstet Fertil
testing in the context of cervical cancer screening: A 2007;35:107–13.
qualitative study. Psychol Oncol 2007;16:196–204. 22 Kjaer SK, Tran TN, Sparen P, Tryggvadottir L,
9 Kitchener HC, Fletcher I, Roberts C, Wheeler P, Munk C, Dasbach E, Liaw KL, Nygård J, Nygård
Almonte M, Maguire P. The psychosocial impact of M. The burden of genital warts: A study of nearly
human papillomavirus testing in primary cervical 70,000 women from the general female population
screening-a study within a randomized trial. Int J in the 4 Nordic countries. J Infect Dis 2007;196:
Gynecol Cancer 2008;18:743–8. 1447–54.
J Sex Med 2009;6:633–645
644 Graziottin and Serafini
23 Orduña Domingo A, Chu JJ, Eiros Bouza JM, controversial role in oral oncogenesis, premalignant
Bratos Pérez MA, Gutiérrez Rodríguez MP, and malignant lesions (review). Int J Oncol
Almaraz Gómez A, Useros Fernández JL, 2007;30:813–23.
Rodríguez Torres A. Age and sex distribution of 38 Anaya-Saavedra G, Ramírez-Amador V, Irigoyen-
sexually transmitted diseases in Valladolid. A study Camacho ME, García-Cuellar CM, Guido-Jiménez
of 5076 cases. Rev Sanid Hig Publica (Madr) M, Méndez-Martínez R, García-Carrancá A. High
1991;65:247–58. association of human papillomavirus infection with
24 Kyriakis KP, Hadjivassiliou M, Paparizos VA, Riga oral cancer: A case-control study. Arch Med Res
P, Katsambas A. Determinants of GW cases detec- 2008;39:189–97.
tion rates among STD clinics in Athens, Greece. Int 39 Halperin DT. Heterosexual anal intercourse: Preva-
J Dermatol 2005;44:650–3. lence, cultural factors, and HIV infection and other
25 Vittori G, Mateelli A, Boselli F, Naldi L, Emberti health risks, Part I. AIDS Patient Care STDS
Gialloreti L. Anew approach to estimate Genital 1999;13:717–30.
Warts incidence and prevalence in the Italian 40 Fox PA. Human papillomavirus and anal intraepi-
general female population. It J Gynaecol Obstet thelial neoplasia. Curr Opin Infect Dis 2006;19:
2008;20:33–42. 62–6.
26 Parkin DM, Bray F. Chapter 2: The burden of 41 Parés D, Mullerat J, Pera M. Anal intraepithelial
HPV-related cancers. Vaccine 2006;24S3:S3/11–S3/ neoplasia. Med Clin (Barc) 2006;127:749–55.
25. 42 Fleurence RL, Dixon JM, Milanova TF, Beusterien
27 Schiffman M, Castle PE, Jeronimo J, Rodriguez AC, KM. Review of the economic and quality of life
Wacholder S. Human papillomavirus and cervical burden of cervical Human papillomavirus disease.
cancer. Lancet 2007;370:890–907. AJOG 2007;196:206–12.
28 Parkin DM, Bray F, Ferlay J, Pisani P. Global 43 Linnehan MJ, Groce NE. Counseling and educa-
cancer statistics, 2002. CA Cancer J Clin tional interventions for women with genital human
2005;55:74–108. papillomavirus infection. AIDS Patient Care STDS
29 Smith J, Lindsay L, Hoots B, Keys J, Franceschi S, 2000;14:439–45.
Winer R, Clifford GM. Human papillomavirus type 44 Voog E, Löwhagen GB. Follow-up of men with
distribution in invasive cervical cancer and high- genital papillomavirus infection: Psychosexual
grade cervical lesions: A meta-analysis update. Int J aspects. Acta Derm Venereol 1992;72:185–6.
Cancer 2007;121:621–32. 45 Goodman MP, Bachmann G, Johnson C, Fourcroy
30 Longworth MS, Laimins LA. Pathogenesis of JL, Goldstein A, Goldstein G, Sklar S. Is elective
Human Papillomaviruses in Differentiating Epithe- vulvar plastic surgery ever warranted, and what
lia. Microbiol Mol Biol Rev 2004;June:362–72. screening should be conducted preoperatively? J Sex
31 de Villiers EM, Fauquet C, Broker TR, Bernard Med 2007;4:269–76.
HU, zur Hausen H. Classification of papillomavi- 46 Woodman CB, Collins S, Winter H, Bailey A, Ellis
ruses. Virology 2004;324:17–27. J, Prior P, Yates M, Rollason TP, Young LS. The
32 Ault KA. Epidemiology and natural history of natural history of cervical human papillomavirus
human papillomavirus infections in the female infection in young women: A longitudinal cohort
genital tract. Infect Dis Obstet Gynecol 2006;(2006 study. Lancet 2001;357:1831–6.
suppl):40470. 47 Miller AB. Natural history of cervical human papil-
33 Sellors JW, Karwalajtys TL, Kaczorowski J, lomavirus infections. Lancet 2001;357:1816.
Mahony JB, Lytwyn A, Chong S, Sparrow J, Lorincz 48 Filiberti A, Tamburini M, Stefanon B, Merola M,
A, Survey of HPV in Ontario Women Group. Inci- Bandieramonte G, Ventafridda V, De Palo G. Psy-
dence, clearance and predictors of human papillo- chological aspects of genital human papillomavirus
mavirus infection in women. CMAJ 2003;168: infection: A preliminary report. J Psychosom Obstet
421–5. Gynaecol 1993;14:145–52.
34 Munger K, Howley PM. Human papillomavirus 49 Bachmann G, Rosen R, Pinn V, Utian W, Ayers C,
immortalization and transformation functions. Basson R, Binik Y, Brown C, Foster D, Gibbons J,
Virus Res 2002;89:213–28. Goldstein I, Graziottin A, Haefner H, Harlow B,
35 Zheng ZM, Baker CC. Papillomavirus genome Kellogg Spadt S, Leiblum S, Masheb R, Reed B,
structure, expression, and post-transcriptional regu- Sobel J, Veasley C, Wesselmann U, Witkin S. Vul-
lation. Front Biosci 2006;11:2286–302. vodynia: A state-of-the-art consensus on definitions,
36 Clarke J, Terry RM, Lacey CJ. A study to estimate diagnosis and management. J Reprod Med 2006;51:
the prevalence of upper respiratory tract papilloma- 447–56.
tosis in patients with genital warts. Int J STD AIDS 50 Graziottin A, Brotto LA. Vulvar vestibulitis syn-
1991;2:114–5. drome: A clinical approach. J Sex Marital Ther
37 Campisi G, Panzarella V, Giuliani M, Lajolo C, Di 2004;30:125–39.
Fede O, Falaschini S, Di Liberto C, Scully C, Lo 51 Zolnoun D, Hartmann K, Lamvu G, As-Sanie S,
Muzio L. Human papillomavirus: Its identity and Maixner W, Steege J. A conceptual model for the
J Sex Med 2009;6:633–645
Psychosexual Impact of HPV Infection in Women 645
pathophysiology of vulvar vestibulitis syndrome. adolescents referred with abnormal cervical smears.
Obstet Gynecol Surv 2006;61:395–401. J Obstet Gynaecol 2007;27:824–7.
52 Goldstein AT, Burrows L. Vulvodynia. J Sex Med 65 Winer RL, Feng Q, Hughes JP, O’Reilly S, Kiviat
2008;5:5–14. NB, Koutsky LA. Risk of female human papilloma-
53 Greenstein A, Ben-Aroya Z, Fass O, Militscher I, virus acquisition associated with first male sex
Roslik Y, Chen J, Abramov L. Vulvar vestibulitis partner. J Infect Dis 2008;197:279–82.
syndrome and estrogen dose of oral contraceptive 66 Steben M, Duarte-Franco E. Human papillomavi-
pills. J Sex Med 2007;4:1679–83. rus infection: Epidemiology and pathophysiology.
54 Pukall C, Kandyba K, Amsel R, Khalifé S, Binik Y. Gynecol Oncol 2007;2(107 suppl):S2–5.
Effectiveness of hypnosis for the treatment of vulvar 67 Epstein RJ. Primary prevention of human
vestibulitis syndrome: A preliminary investigation. papillomavirus-dependent neoplasia: No condom,
J Sex Med 2007;4:417–25. no sex. Eur J Cancer 2005;41:2595–600.
55 Smith EM, Ritchie JM, Galask R, Pugh EE, Jia J, 68 Anttila T, Saikku P, Koskela P, Bloigu A, Dillner J,
Ricks-McGillan J. Case-control study of vulvar ves- Ikäheimo I, Jellum E, Lehtinen M, Lenner P,
tibulitis risk associated with genital infections. Infect Hakulinen T, Närvänen A, Pukkala E, Thoresen S,
Dis Obstet Gynecol 2002;10:193–202. Youngman L, Paavonen J. Serotypes of Chlamydia
56 Gaunt G, Good AE, McGovern RM, Stanhope trachomatis and risk for development of cervical
CR, Gostout BS. Human papillomavirus in vulvar squamous cell carcinoma. JAMA 2001;285:47–51.
vestibulitis syndrome. J Reprod Med 2007;52:485– 69 Bosch FX, de Sanjosé S. The epidemiology of
9. human papillomavirus infection and cervical cancer.
57 Bleeker MC, Hogewoning CJ, Van Den Brule AJ, Dis Markers 2007;23:213–27.
Voorhorst FJ, Van Andel RE, Risse EK, Starink 70 Smith JS, Herrero R, Bosetti C, Muñoz N, Bosch
TM, Meijer CJ. Penile lesions and human papillo- FX, Eluf-Neto J, Castellsagué X, Meijer CJ, Van
mavirus in male sexual partners of women with cer- den Brule AJ, Franceschi S, Ashley R, International
vical intraepithelial neoplasia. J Am Acad Dermatol Agency for Research on Cancer (IARC) Multicen-
2002;47:351–7. tric Cervical Cancer Study Group. Herpes simplex
58 Bleeker MC, Snijders PF, Voorhorst FJ, Meijer CJ. virus-2 as a human papillomavirus cofactor in the
Flat penile lesions: The infectious “invisible” link in etiology of invasive cervical cancer. J Natl Cancer
the transmission of human papillomavirus. Int J Inst 2002;94:1604–13.
Cancer 2006;119:2505–12.62. 71 Castellsaguè X, Munoz N. Chapter 3: Cofactors
59 Giles GG, Kneale BL. Vulvar cancer: The Cinder- in human papillomavirus carcinogenesis: Role of
ella of gynaecological oncology. Aust N Z J Obstet parity, oral contraceptives, and tobacco smoking.
Gynaecol 1995;35:71–5. J Natl Cancer Inst Monogr 2003;31:20–8.
60 Grassi L, Indelli M, Marzola M, Maestri A, Santini 72 Strickler HD, Burk RD, Fazzari M, Anastos K,
A, Piva E, Boccalon M. Depressive symptoms and Minkoff H, Massad LS, Hall C, Bacon M, Levine
quality of life in home care assisted cancer patients. AM, Watts DH, Silverberg MJ, Xue X, Schlecht
J Pain & Sympt Mgmt 1996;12:300–7. NF, Melnick S, Palefsky JM. Natural history and
61 Seibel M, Freeman M, Graves WL. Carcinoma of possible reactivation of human papillomavirus in
the cervix and sexual function. Obstet Gynecol human immunodeficiency virus-positive women.
1980;55:484–7. J Natl Cancer Inst 2005;97:577–86.
62 Rambout L, Hopkins L, Hutton B, Fergusson D. 73 Cameron JE, Hagensee ME. Human papillomavirus
Prophylactic vaccination against human papilloma- infection and disease in the HIV+ individual. Cancer
virus infection and disease in women: A systematic Treat Res 2007;133:185–213.
review of randomized controlled trials. CMAJ 74 Hariri S, Dunne EF, Sternberg M, Unger ER,
2007;177:469–79. Meadows KS, Karem KL, Markowitz LE. Seroepi-
63 Moscicki AB. HPV infections in adolescents. Dis demiology of human papillomavirus type 11 in the
Markers 2007;23:229–34. United States: Results from the third national health
64 Saleh MM, Seoud AA, Zaklama MS. Study of and nutrition examination survey, 1991–1994. Sex
the demographic criteria and management of Transm Dis 2008;35:298–303.
J Sex Med 2009;6:633–645
You might also like
- The Complete Guide to HPV: Symptoms, Risks, Diagnosis & TreatmentsFrom EverandThe Complete Guide to HPV: Symptoms, Risks, Diagnosis & TreatmentsNo ratings yet
- Prevalence of HPV Infection Among MenDocument14 pagesPrevalence of HPV Infection Among MenpolianaspricigoNo ratings yet
- VPH en HombresDocument11 pagesVPH en HombreshielitousNo ratings yet
- Patterns of Incident Genital Human Papillomavirus Infection in Women: A Literature Review and Meta-AnalysisDocument11 pagesPatterns of Incident Genital Human Papillomavirus Infection in Women: A Literature Review and Meta-Analysiswmn94No ratings yet
- Doct. ETSITS 3Document13 pagesDoct. ETSITS 3Vanessa CaballeroNo ratings yet
- Nejmcp 2108502Document9 pagesNejmcp 2108502Manuel GilNo ratings yet
- Aspectos Biológicos, Terapeuticos en Mujeres Con VIH Comparado A Hombres AIDS ReviewDocument8 pagesAspectos Biológicos, Terapeuticos en Mujeres Con VIH Comparado A Hombres AIDS ReviewIsmaelJoséGonzálezGuzmánNo ratings yet
- Genital Herpes: Clinical PracticeDocument9 pagesGenital Herpes: Clinical PracticeIsabellaRuthNo ratings yet
- RH Fs Risk FactorsDocument2 pagesRH Fs Risk FactorsfentroispNo ratings yet
- Anyone Can Have An STDDocument12 pagesAnyone Can Have An STDjordyeeNo ratings yet
- ThesisDocument23 pagesThesisAnushika AgarwalNo ratings yet
- Nej MCP 2108502Document9 pagesNej MCP 2108502Marialejandra GuevaraNo ratings yet
- Prevalence and Incidence of Genital Warts and Cervical Human Papillomavirus Infections in Nigerian WomenDocument10 pagesPrevalence and Incidence of Genital Warts and Cervical Human Papillomavirus Infections in Nigerian WomenRiszki_03No ratings yet
- WS Nihms448407Document11 pagesWS Nihms448407ayubahriNo ratings yet
- HPV Vaccine Against Anal HPV Infection and Anal Intraepithelial NeoplasiaDocument10 pagesHPV Vaccine Against Anal HPV Infection and Anal Intraepithelial NeoplasiaszarysimbaNo ratings yet
- UKPMC Funders Group: Author ManuscriptDocument9 pagesUKPMC Funders Group: Author ManuscriptNikita BowmanNo ratings yet
- High Risk HPVDocument6 pagesHigh Risk HPVjawaralopangNo ratings yet
- Journal - Pone.0146603 S Ebrahim Final PublicationDocument10 pagesJournal - Pone.0146603 S Ebrahim Final PublicationSumayyah EbrahimNo ratings yet
- Gonorrhea Infection in Women: Prevalence, Effects, Screening, and ManagementDocument14 pagesGonorrhea Infection in Women: Prevalence, Effects, Screening, and ManagementMaulana MalikibrahimNo ratings yet
- HIV Infectivity Per Coital ActDocument8 pagesHIV Infectivity Per Coital Actkedirali921No ratings yet
- Jkon 11 171Document8 pagesJkon 11 171pangaribuansantaNo ratings yet
- Ching 13Document2 pagesChing 13rochelleNo ratings yet
- Screenshot 2022-08-12 at 6.19.42 PMDocument1 pageScreenshot 2022-08-12 at 6.19.42 PMKayla AdamsNo ratings yet
- Ni Hms 411988Document14 pagesNi Hms 411988woouuw0903No ratings yet
- Úlceras Genitales AFP 2020Document7 pagesÚlceras Genitales AFP 2020Juanita MesaNo ratings yet
- Literature Review On Human PapillomavirusDocument8 pagesLiterature Review On Human Papillomavirusf0typiwydeb3100% (1)
- Virology of Human Papillomavirus Infections and The Link To CancerDocument10 pagesVirology of Human Papillomavirus Infections and The Link To Canceralejandro fernandezNo ratings yet
- Knowledge Attitudes and Testing Preferences For Herpes Simplex Virus Infections Among Undergraduate Students at A Large University in Los Angeles CDocument7 pagesKnowledge Attitudes and Testing Preferences For Herpes Simplex Virus Infections Among Undergraduate Students at A Large University in Los Angeles CMr SoehartoNo ratings yet
- According To CDC: Biologic PlausibilityDocument7 pagesAccording To CDC: Biologic PlausibilityJpt YapNo ratings yet
- Marrazzo Et Al 2010 VaginoseDocument11 pagesMarrazzo Et Al 2010 Vaginoseirvinaldi9No ratings yet
- Syphilis Epidemic Among Men Who Have Sex With Men: A Global Systematic Review and Meta-Analysis of Prevalence, Incidence, and Associated FactorsDocument11 pagesSyphilis Epidemic Among Men Who Have Sex With Men: A Global Systematic Review and Meta-Analysis of Prevalence, Incidence, and Associated FactorsEldie RahimNo ratings yet
- Chlamydia Trachomatis Infection in Female Partners of Circumcised and Uncircumcised Adult MenDocument10 pagesChlamydia Trachomatis Infection in Female Partners of Circumcised and Uncircumcised Adult MenJuan Andre' MarquinezNo ratings yet
- An Update On Oral Human Papillomavirus Infection: Review ArticleDocument7 pagesAn Update On Oral Human Papillomavirus Infection: Review ArticlebungagladysNo ratings yet
- Lectura ClaseDocument6 pagesLectura ClasemjjuliannamartinezNo ratings yet
- Schiff Man 1993Document7 pagesSchiff Man 1993ema 274No ratings yet
- Human Papillomavirus Infection in Shenyang City, People's Republic of China: A Population-Based StudyDocument5 pagesHuman Papillomavirus Infection in Shenyang City, People's Republic of China: A Population-Based StudyyoggihermawanNo ratings yet
- Prevalence, Associated Factors and Health Impact of Intimate Partner Violence Against Women in Different Life StagesDocument12 pagesPrevalence, Associated Factors and Health Impact of Intimate Partner Violence Against Women in Different Life StagesAlma AcevedoNo ratings yet
- Knowledge Attitudes and Testing Preferences For Herpes Simplex Virus Infections Among Undergraduate Students at A Large University in Los AngelesDocument7 pagesKnowledge Attitudes and Testing Preferences For Herpes Simplex Virus Infections Among Undergraduate Students at A Large University in Los AngelessesiaNo ratings yet
- International Journal of Women's DermatologyDocument9 pagesInternational Journal of Women's DermatologykaltrinaramaNo ratings yet
- Nihms 1614989Document18 pagesNihms 1614989JENNIFER STEFANiA ROJAS VEGANo ratings yet
- Sexually Transmitted Diseases Autosaved - Docx 22222Document5 pagesSexually Transmitted Diseases Autosaved - Docx 22222Badang Casio JoeyNo ratings yet
- Jama Tuddenham 2022 RV 210018 1641310196.58344Document12 pagesJama Tuddenham 2022 RV 210018 1641310196.58344Drax The destroyerNo ratings yet
- A Link Between Human Papilloma Virus Vaccination and Primary Ovarian Insufficiency: Current AnalysisDocument6 pagesA Link Between Human Papilloma Virus Vaccination and Primary Ovarian Insufficiency: Current AnalysisAnca CucuNo ratings yet
- 75 Bosch1995 PDFDocument7 pages75 Bosch1995 PDFRonaLd Jackson SinagaNo ratings yet
- Teachers' Topics The Pharmacotherapy of The Modern Day Epidemic Infection With Human Immunodeficiency Virus (HIV)Document9 pagesTeachers' Topics The Pharmacotherapy of The Modern Day Epidemic Infection With Human Immunodeficiency Virus (HIV)amin2002No ratings yet
- Sexuality, Sexual Health, and Sexually Transmitted Infections in Adolescents and Young AdultsDocument4 pagesSexuality, Sexual Health, and Sexually Transmitted Infections in Adolescents and Young AdultsyehkzprxisluvsstrvNo ratings yet
- Jir 342Document4 pagesJir 342Hanifa AdaniNo ratings yet
- Prevalence of Bacterial Vaginosis: 2001-2004 National Health and Nutrition Examination Survey DataDocument7 pagesPrevalence of Bacterial Vaginosis: 2001-2004 National Health and Nutrition Examination Survey DataYossy VesriNo ratings yet
- Howe 1999Document9 pagesHowe 1999CQNo ratings yet
- JPMH 2018 03 E194Document6 pagesJPMH 2018 03 E194Annisa dwi UtariNo ratings yet
- Jurnal Condyloma AcuminataDocument11 pagesJurnal Condyloma Acuminataperussi pranadiptaNo ratings yet
- The Complete Guide to Genital Herpes: Symptoms, Risks, Diagnosis & TreatmentsFrom EverandThe Complete Guide to Genital Herpes: Symptoms, Risks, Diagnosis & TreatmentsNo ratings yet
- Global Perspectives on the Transmission of Zoonotic RNA Viruses from Wild Animal Species to Humans: Zoonotic, Epizootic, and Anthropogenic Viral PathogensFrom EverandGlobal Perspectives on the Transmission of Zoonotic RNA Viruses from Wild Animal Species to Humans: Zoonotic, Epizootic, and Anthropogenic Viral PathogensNo ratings yet
- Sexuality by Mejri JabeurDocument88 pagesSexuality by Mejri JabeurStvgal Gamal100% (1)
- Ge 111: Understanding The SelfDocument33 pagesGe 111: Understanding The SelfJonnah QuindoNo ratings yet
- Shaws Text Book of GynecologyDocument438 pagesShaws Text Book of GynecologySumeera Nirmal Samarakkody100% (2)
- Why Should We Have SexDocument4 pagesWhy Should We Have SexFoshissle Yuki JahpNo ratings yet
- Human Papilloma Virus HPV PSPD PDFDocument11 pagesHuman Papilloma Virus HPV PSPD PDFHenok Nugrahawanto100% (1)
- Merck Form 10-kDocument208 pagesMerck Form 10-kKerine ChunNo ratings yet
- Intraepithelial Neoplasia of The Lower Genital TractDocument54 pagesIntraepithelial Neoplasia of The Lower Genital TractDee SarajanNo ratings yet
- Abnormal Cervical CytologyDocument21 pagesAbnormal Cervical CytologyNatalia HaikaliNo ratings yet
- Infertility Concern With Gardasil HPV Vaccine Auto Saved)Document8 pagesInfertility Concern With Gardasil HPV Vaccine Auto Saved)TomGambillNo ratings yet
- Functional Preservation and Quality of Life in Head & Neck Radiotherapy PDFDocument320 pagesFunctional Preservation and Quality of Life in Head & Neck Radiotherapy PDFRakesh JadhavNo ratings yet
- Penile CancerDocument46 pagesPenile CancerRifky Budi TriyatnoNo ratings yet
- Benefits Summary Updated (Contractors) FinalDocument25 pagesBenefits Summary Updated (Contractors) FinalSithu HeinNo ratings yet
- Distribuţia Genotipurilor Virusului Papiloma Uman La Paciente Din Zona MoldoveiDocument5 pagesDistribuţia Genotipurilor Virusului Papiloma Uman La Paciente Din Zona MoldoveiZama VitalieNo ratings yet
- Article On Human Papilloma VirusDocument5 pagesArticle On Human Papilloma VirusHafiz SabghatullahNo ratings yet
- HPV VaccineDocument1 pageHPV VaccineBrix ValdrizNo ratings yet
- Bikes & Beauties Magazine. November 2010Document48 pagesBikes & Beauties Magazine. November 2010Carlos CharrutiNo ratings yet
- CPT Top 500 Codes OB/GYN - Women's HealthDocument2 pagesCPT Top 500 Codes OB/GYN - Women's HealthMeredith Barb40% (10)
- Answers - Mock MEQ Exam 2020Document21 pagesAnswers - Mock MEQ Exam 2020JunYuuuNo ratings yet
- 2012 UpmcccanualreportDocument70 pages2012 Upmcccanualreportapi-290001443No ratings yet
- A Review On Cervical Cancer VaccinationDocument3 pagesA Review On Cervical Cancer VaccinationKIU PUBLICATION AND EXTENSIONNo ratings yet
- Literature Review of Cervix CancerDocument6 pagesLiterature Review of Cervix Cancerzyfepyfej0p2100% (1)
- Gynaecologic CytologyDocument194 pagesGynaecologic CytologyArun Kumar100% (2)
- Human Papillomavirus (HPV) : Treatment, Symptoms, and CausesDocument9 pagesHuman Papillomavirus (HPV) : Treatment, Symptoms, and CausesPaul LauNo ratings yet
- HPV and Cancer PDFDocument44 pagesHPV and Cancer PDFAzikah RohimahhNo ratings yet
- Sign99 - Management of Cervical CancerDocument77 pagesSign99 - Management of Cervical CancerPoljarLijanNo ratings yet
- PAPSMEARASMDocument10 pagesPAPSMEARASMericNo ratings yet
- Brosur KIT HPV DNADocument2 pagesBrosur KIT HPV DNARonna EfriyanaNo ratings yet
- Vaksinasi Dewasa Sby 14Document51 pagesVaksinasi Dewasa Sby 14Ku Ha KuNo ratings yet
- 5-Aminolevulinic Acid Photodynamic Therapy For Condyloma Acuminatum of Urethral MeatusDocument19 pages5-Aminolevulinic Acid Photodynamic Therapy For Condyloma Acuminatum of Urethral MeatusRiefka Ananda ZulfaNo ratings yet
- A.18 Hypochlorous-AcidDocument57 pagesA.18 Hypochlorous-AcidHervian LanangNo ratings yet