Professional Documents
Culture Documents
2022 - Management of Periodontal Intrabony Defect Using Sticky Bone and GTR Membrane: A Case Report
Uploaded by
Jontavius GilbertCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2022 - Management of Periodontal Intrabony Defect Using Sticky Bone and GTR Membrane: A Case Report
Uploaded by
Jontavius GilbertCopyright:
Available Formats
International Journal of Science and Research (IJSR)
ISSN: 2319-7064
SJIF (2022): 7.942
Management of Periodontal Intrabony Defect Using
Sticky Bone and GTR Membrane: A Case Report
Dr. Prince Soni1, Dr. Madhu S. Ratre2, Dr. Shaleen Khetarpal3, Dr. Sakshi Chokhandre4
1
M.D.S. Student, Govt. College of Dentistry, Indore, Madhya Pradesh, India (452001)
Corresponding author Email: drpsoni24[at]gmail.com
2
Professor and HOD, Govt. College of Dentistry, Indore, Madhya Pradesh, India (452001)
smadhu16feb[at]yahoo.co.in
3
Reader, Govt. College of Dentistry, Indore, Madhya Pradesh, India (452001)
drshaleenk[at]gmail.com
4
M.D.S. Student, Govt. College of Dentistry, Indore, Madhya Pradesh, India (452001)
sakshichokhandre[at]gmail.com
Abstract: Background: Periodontal regeneration in particular represents regain of lost periodontal tissues either by regenerative
techniques to be used alone or in combination with an adjunct. Platelet-rich Fibrin (PRF) is an autologous product that is derived from
whole blood by applying the process of gradient density centrifugation. Use of platelet concentrates is promising due to its autologous
nature, release of multiple growth factors, low cost, ease of procurement and comfortable handling. Injectable PRF (i-PRF) can be
combined with bone grafts to form sticky bone with superior handling and healing properties. Hereby, we report a case with intra bony
defects treated with sticky bone and barrier membrane with a 1-year follow-up. Methodology: 10 ml of the patient’s venous blood was
collected and i-PRF was obtained by low centrifugation protocol. Sticky bone was prepared by mixing i-PRF with alloplast and was
placed in intrabony defect. A bioresorbable collagen membrane was placed over the sticky bone followed by periodontal flap closure.
Results: A reduction in the Probing pocket depth (PPD) from 7mm (Pre-operative) to 3mm, Clinical attachment loss (CAL) from 8mm to
4mm. Conclusion: Significant improvement in clinical parameters such as PPD, CAL and radiographic bone fill indicates success of
regenerative therapy using i-PRF with bone grafts.
Keywords: Bone loss, Intrabony defects, Periodontitis, Periodontal regeneration, PRF, Bone grafts
1. Introduction chief complaint of food impaction in the lower right back
tooth region since1year. The patient was systemically
Periodontitis is an inflammatory disease with varied levels healthy. Periodontal examination revealed periodontal
of periodontal attachment loss and bone destruction.1 pockets in relation to #43 and #44.There was no mobility
Periodontal regeneration has been defined as “the noted. Probing pocket depth (PPD) was recorded with a
reproduction or reconstitution of a lost or injured part to UNC-15 probe (Hu-Friedy, USA). #43 on the distal surface
restore the architecture and function of the periodontium.”2 had a PPD of 7mm [Fig.1]. The Clinical attachment loss
Predictable regeneration of periodontium is a challenge (CAL) was 8mm on distal surface of #43. Intra-oral
faced worldwide because this process requires an organized periapical radiograph (IOPA)revealed vertical bone loss in
succession of complicated biological events.3The biological relation to #43 and #44 upto apical third of root[Fig.2].
mechanisms which provide a rationale for bone grafting are Vitality test using electric pulp tester revealed #43 as vital.
osteogenesis, osteoinduction and osteoconduction.4 Platelets Routine hematological investigations revealed a normal
contain various growth factors in abundance entrapped in the blood picture. The treatment plan consisted of scaling and
alpha granules. These growth factors promote the root planning followed by regenerative therapy for intrabony
regeneration irrespective of being utilized alone or in defects. The patient was advised 0.2% chlorhexidine mouth
combination with other materials.5-7 Platelet-rich fibrin rinse twice daily.
(PRF) was first described by Choukroun et al. in 2001 in
France as a second-generation platelet concentrate because The patient was recalled 6 weeks after phase-I therapy and
the natural concentrate is produced without any the clinical parameters were re-evaluated. Thereby, surgical
anticoagulants or gelifying agents.8In the past decade, so intervention was necessary. Periodontal regenerative therapy
called injectable-PRF (i-PRF) has been developed using using sticky bone and barrier membrane was planned in
lower centrifugation protocols. i-PRF remains liquid for relation to #43 and #44. The procedure, advantages and
approximately 15 mins.9 The Bone graft is mixed with i-PRF associated risks were explained to the patient.
to form bone graft matrix called “Sticky bone” which makes
it a manipulative mass.10 Surgical Phase
After obtaining patient’s consent, local anaesthesia was
2. Case Report administered. Sulcular and interdental incision were placed
followed
A 58-year-old male patient reported to the Department of
Periodontology, Govt. College of Dentistry, Indore, with a
Volume 11 Issue 6, June 2022
www.ijsr.net
Licensed Under Creative Commons Attribution CC BY
Paper ID: SR22617114645 DOI: 10.21275/SR22617114645 1105
International Journal of Science and Research (IJSR)
ISSN: 2319-7064
SJIF (2022): 7.942
Figure 1: Pre-operative pocket probing depth
Figure 1: Bone defect exposed
i-PRF was prepared as follows: 10 ml of patient’s venous
blood was collected from the median cephalic vein
(antecubital fossa) into a plastic test tube without anti-
coagulants. [Fig.4a]. The collected blood was subjected to
centrifugation (Remi R-8C, Remi Electotechnik LTD, India)
at 700 rpm for 3 mins. The obtained i-PRF was collected
with a syringe (Fig.4b) and mixed with an alloplast
Figure 2: Pre-operative intraoral periapical view radiograph
(SYBOGRAF-T, Eucare Pharmaceuticals, Chennai, India).
A cohesive mass termed sticky bone was formed which can
by elevation of full-thickness flap in relation to #42, #43 and
be manipulated according to defect morphology (Fig.4c).
#44 [Fig.3]. The area was debrided to remove subgingival
calculus and granulation tissue. The width and depth of the
Pre-suturing was done using 5-0 polypropylene sutures
intra bony defect was measured using UNC-15 periodontal
(Prolene Ethicon, Puerto Rico, USA). Sticky bone was
probe.
placed at the defect area [Fig. 5a] followed by the placement
of a GTR membrane (Periocol, Eucare pharmaceuticals,
Chennai, India) cut into a dumbbell-shape [Fig. 5b]. The
facial and lingual flaps were approximated using a
horizontal mattress suture [Fig. 5c]. Non eugenol
periodontal dressing (COEpak, GC, USA) was placed for 14
days. Patient was advised to restrain from mechanical
cleaning aids at the operated area for 1 month.
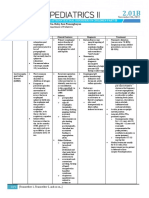
Figure 2: a) Aspiration of blood from greater cephalic vein, b) Prepared i-PRF collected in sterile syringe,
c) Sticky bone made by mixing bone graft with i-PRF
Volume 11 Issue 6, June 2022
www.ijsr.net
Licensed Under Creative Commons Attribution CC BY
Paper ID: SR22617114645 DOI: 10.21275/SR22617114645 1106
International Journal of Science and Research (IJSR)
ISSN: 2319-7064
SJIF (2022): 7.942
Figure 3: a) Placement of sticky bone in defect, b) Placement of GTR membrane, c) Sutures placed
Amoxicillin + clavulanic acid (500 mg + 125mg) 1 tds, Dental research industry has been progressively concerned
Analgesic –Ibuprofen (400mg) 1 tds and Chlorhexidine over the past two decades with placement biologically inert,
0.2% rinse thrice a day, were prescribed. synthetic and autologous materials into periodontal
intrabony defect.
Following surgery, patient was re-evaluated at regular
intervals of 3months for 1year. Necessary de-plaquing was In our case report, intrabony defects of the patient in relation
done and patient was reinforced for plaque control at recall to #43 and #44 was treated with i-PRF in combination with
visits. There was a reduction in the PPD and CAL from alloplastas sticky bone and GTR membrane to attempt
7mm and 8mm (pre-operative) to 3mm and 4mm (1-year periodontal regeneration.
post-operative) respectively. There was no mobility noted at
any of the follow-up visits. Radiographically, a partial defect PRF contains numerous growth factors like platelet-derived
fill was achieved [Fig.6]. growth factor (PDGF), transforming growth factor (TGF),
vascular endothelial growth factor (VEGF) etc. that has the
potential to modulate and up-regulate tissue healing.12
Injectable PRF (i-PRF) is formed at low centrifugation
settings of 700rpm for 3 minutes. It can be injected in liquid
form or mixed with bone graft to give a well agglutinated
growth factors-enriched bone graft “steak” for bone grafting
i.e., sticky bone.
After application, i-PRF immediately coagulates into a clot
rich with growth factors, which has been reported to be
constantly released over a period of 10–14 days. Presence of
higher number of leukocytes in i-PRF has advantage as it
Figure 4: 1-year follow-up intraoral periapical view
favours more growth factor release and local antimicrobial
radiograph
action and thus promotes tissue wound healing. Sticky bone
aids in better handling and stabilization of bone graft mass
3. Discussion which helps in acceleration of tissue healing, providing bulk
and also minimizing bone loss during healing phase.10Sohn
The ideal goal for regerative periodontal therapy is the et al. demonstrated that i-PRF has excellent
reconstitution of connective tissue attachment and alveolar biocompatibility, induces a significant number of cell
bone which has been destroyed by the periodontal migration and proliferation and when compared to PRP,
disease.11Complete periodontal regeneration after various better osteogenic differentiation has been documented.13
treatment modalities is difficult to achieve because of
differential healing abilities of periodontal tissues. The Bone grafts in combination with a barrier membrane have
events range from cell migration to differentiation and been shown in literature to enhance the regenerative
incorporation of numerous cytokines and growth factors for outcomes. Filling the defect with sticky bone and covering it
regulation.[3] with a barrier membrane have shown to accelerate the bone
formation and wound healing with superior periodontal
The most favourable outcome for regenerative periodontal regeneration. i-PRF with bone graft (sticky bone) can be
therapy is the regain of lost supporting tissues. Some of the easily moulded into the desired and required shape, aiding in
regenerative therapies advocated include, open flap its easy handling and also in preventing dispersion.14 Studies
debridement; open flap debridement with bone grafts/bone have shown that following 10 days, an additional release of
substitutes, and guided tissue regeneration (GTR). growth factors could be expected from i-PRF.15 Hence, in
Volume 11 Issue 6, June 2022
www.ijsr.net
Licensed Under Creative Commons Attribution CC BY
Paper ID: SR22617114645 DOI: 10.21275/SR22617114645 1107
International Journal of Science and Research (IJSR)
ISSN: 2319-7064
SJIF (2022): 7.942
this study i-PRF with bone graft and sterile barrier [7] Chatterjee A, Debnath K. Comparative evaluation of
membrane was decided to be used for regeneration. growth factors from platelet concentrates: An in vitro
study. J Indian Soc Periodontol2019; 23:322-8.
As described by Sculean et al.16 in the systematic review, [8] Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan
that most studies have demonstrated superior histologic AJ, Mouhyi J, et al. Platelet-rich fibrin (PRF): A
healing following the combination of barrier membranes and second-generation platelet concentrate. Part II:
grafting materials than following open flap debridement, Platelet-relate biologic features. Oral Surg Oral Med
hence in this case with the use of sticky bone, GTR Oral Pathol Oral RadiolEndod 2006; 101:e45-50.
membrane was also placed for better outcome. Other bone [9] Ghanaati S, Booms P, Orlowska A, Kubesch A,
graft materials like bovine bone, allografts, etc have also Lorenz J, Rutkowski J, Landes C, Sader R, Kirkpatrick
been studied extensively for placement in intraosseous bone CJ, et.al. Advanced platelet-rich fibrin: a new concept
defects. Some authors evaluated the effect of PRF and for cell-based tissue engineering by means of
bioactive glass and found significant results in terms of inflammatory cells. Journal of Oral Implantology.
clinical and radiographic outcomes at 1 year follow-up.17 2014 Dec; 40 (6):679-89.
[10] Wang X, Zhang Y, Choukroun J, Ghanaati S, Miron
Preoperatively, a PPD and CAL value in our patient was RJ. Effects of an injectable platelet-rich fibrin on
recorded as 7mm and 8mm respectively. At 1 year post- osteoblast behavior and bone tissue formation in
operatively, the values reduced to 3mm and 4 mm comparison to platelet-rich plasma. Platelets. 2018 Jan
respectively. The results of this report shows that with the 2; 29 (1):48-55. Zander HA, Polson AM, Heijl LC.
use of i-PRF and bone graft material (sticky bone) along Goals of periodontal therapy. J Periodontol1976;
with a barrier membrane, it was possible to regenerate wide 47:261-6.
intrabony defect. [11] Zander HA, Polson AM, Heijl LC. Goals of
periodontal therapy. Journal of periodontology. 1976
4. Conclusion May; 47 (5):261-6.
[12] Blumenthal NM, Alves ME, Al-Huwais S, HoĠauer
According to the results obtained in this case report, it could AM, Koperski RD. Defect Determined regenerative
be concluded that the positive clinical impact of additional options for treating periodontal intrabony defects in
application of PRF with alloplastic graft material in Baboons. J Periodontol2003; 74:10-24.
treatment of periodontal intrabony defect is based on [13] Sohn DS, Huang B, Kim J, Park WE, Park CC.
reduction in probing pocket depth, gain in clinical Utilization of autologous concentrated growth factors
attachment level, significant radiographic defect bone fill, (CGF) enriched bone graft matrix (sticky bone) and
improved patient comfort and early wound healing. CGF-enriched fibrin membrane in implant dentistry. J
Implant Adv Clin Dent. 2015 Dec; 7 (10):11-8.
However, long-term, multicentre randomized, controlled [14] Soni R, Priya A, Yadav H, Mishra N, Kumar L. Bone
clinical trial will be required to substantiate the observations augmentation with sticky bone and platelet-rich fibrin
of the present case report. by ridge-split technique and nasal floor engagement for
immediate loading of dental implant after extracting
References impacted canine. National journal of maxillofacial
surgery. 2019 Jan; 10 (1):98.
[1] Giannobile WV. The potential role of growth and [15] Miron RJ, Fujioka-Kobayashi M, Hernandez M,
differentiation factors in periodontal regeneration J Kandalam U, Zhang Y, Ghanaati S, et.al. Injectable
Periodontol 1996; 67:545–553. platelet rich fibrin (i-PRF): opportunities in
[2] Bajaj P, Rao NS, Agarwal E, Pradeep AR. Treatment regenerative dentistry?. Clinical oral investigations.
of intrabony defect with platelet rich fi brin: A case 2017 Nov; 21 (8):2619-27.
report. Arch Oral Sci Res 2011; 1:90-4. [16] Sculean A, Nikolidakis D, Schwarz F. Regeneration of
[3] McCulloch CA. Basic considerations in periodontal periodontal tissues: combinations of barrier
wound healing to achieve regeneration. Periodontol membranes and grafting materials–biological
2000 1993; 1:16-25 foundation and preclinical evidence: a systematic
[4] Klokkevold, PR, Jovanovic, SA: Advanced Implant review. Journal of clinical periodontology. 2008 Sep;
Surgery and Bone Grafting Techniques. In Newman, 35:106-16.
Takei, Carranza, editors: Carranza's Clinical [17] Ratre MS, Nasir S, Khetarpal S, Verma M. Effective
Periodontology, 9th Edition. Philadelphia: Management of Periodontal Intraosseous Defects using
W.B.Saunders Co. 2002. Pg. 907-8. combination of Bioactive Glass+ Platelet-rich Fibrin:
[5] Nevins M, Kao RT, McGuire MK, McClain PK, A Clinical and Radiographic Evaluation. International
Hinrichs JE, McAllister BS, et al. Platelet-derived Journal of Preventive and Clinical Dental Research,
growth factor promotes periodontal regeneration in April-June 2018; 5 (2):98-101
localized osseous defects: 36-month extension results
from a randomized, controlled, double-masked clinical
trial. J Periodontol2013; 84:456-64.
[6] Zhang L, Leeman E, Carnes DC, Graves DT. Human
osteoblasts synthesize and respond to platelet-derived
growth factor. Am J Physiol 1991; 261:C348-54.
Volume 11 Issue 6, June 2022
www.ijsr.net
Licensed Under Creative Commons Attribution CC BY
Paper ID: SR22617114645 DOI: 10.21275/SR22617114645 1108
You might also like
- Artículo Khoury2018Document10 pagesArtículo Khoury2018Basma Derdabi100% (1)
- Tunnel Access For Guided Bone Regeneration in The Maxillary AnteriorDocument6 pagesTunnel Access For Guided Bone Regeneration in The Maxillary Anteriormax100% (1)
- A1 Medical OphCatDocument265 pagesA1 Medical OphCatRikyo LunaNo ratings yet
- MCQs & EMQ For DOHNSDocument162 pagesMCQs & EMQ For DOHNSyasino0% (1)
- Cosmetic Dermatology Products and Procedures Download Online (PDF, EpubDocument5 pagesCosmetic Dermatology Products and Procedures Download Online (PDF, EpubandrewNo ratings yet
- A Nursing PortfolioDocument7 pagesA Nursing Portfolioabhi100% (3)
- Art Perfil de Emergencia Implantes PDFDocument7 pagesArt Perfil de Emergencia Implantes PDFdiego alenadro trujilloNo ratings yet
- Assessment of Alveolar Bone Augmentation in Intrabony Defects Employing Platelet-Rich Fibrin (PRF) Membrane and Sticky Bone (Injectable-PRF & Demineralized Freeze-Dried Bone Graft) - A Case ReportDocument4 pagesAssessment of Alveolar Bone Augmentation in Intrabony Defects Employing Platelet-Rich Fibrin (PRF) Membrane and Sticky Bone (Injectable-PRF & Demineralized Freeze-Dried Bone Graft) - A Case ReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Rde 39 51Document5 pagesRde 39 51Sashwat SathishNo ratings yet
- 20 DR Arvind UDDocument7 pages20 DR Arvind UDJohn SmithNo ratings yet
- Surgical Management of A Large Periapical Lesion With PRF and Xenograft - A Case ReportDocument3 pagesSurgical Management of A Large Periapical Lesion With PRF and Xenograft - A Case ReportJohn SmithNo ratings yet
- Ab 2019Document7 pagesAb 2019Dome CárdenasNo ratings yet
- 2022 - Platelet-Rich Fibrin - A Wonder Material For Periodontal Regeneration - A Clinical Case SeriesDocument4 pages2022 - Platelet-Rich Fibrin - A Wonder Material For Periodontal Regeneration - A Clinical Case SeriesJontavius GilbertNo ratings yet
- Ramus Onlay Bone Graft For Maxillary Alveolar Ridge Augmentation-A Case ReportDocument9 pagesRamus Onlay Bone Graft For Maxillary Alveolar Ridge Augmentation-A Case ReportIJAR JOURNALNo ratings yet
- PRF Extraction SocketDocument5 pagesPRF Extraction Socketmandeep sharmaNo ratings yet
- Periodontal Management of Non Healing Endodontic Lesion - A Case ReportDocument5 pagesPeriodontal Management of Non Healing Endodontic Lesion - A Case ReportbubuvulpeaNo ratings yet
- Root Canat Tratment With RPFDocument6 pagesRoot Canat Tratment With RPFAna-Maria HriscuNo ratings yet
- Egg Shell and Nano Technology A Veritable Combination To Promote Regeneration of Bone in Intrabony Defect: A Case ReportDocument6 pagesEgg Shell and Nano Technology A Veritable Combination To Promote Regeneration of Bone in Intrabony Defect: A Case ReportAngga SaputraNo ratings yet
- Yoon 2014Document7 pagesYoon 2014aleegaleanoNo ratings yet
- Regeneration of Periapical Bone in Surgical Endodontics: A Case ReportDocument7 pagesRegeneration of Periapical Bone in Surgical Endodontics: A Case ReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- 371-Article Text-1509-3-10-20210710Document6 pages371-Article Text-1509-3-10-20210710Fransiski HoNo ratings yet
- Guided Bone Regeneration Simultaneous With Implant Placement Using Bovine-DerivedDocument13 pagesGuided Bone Regeneration Simultaneous With Implant Placement Using Bovine-DerivedCamilo Andrés Sabogal ArguelloNo ratings yet
- HaseebaK EtalDocument5 pagesHaseebaK EtalIndah VitasariNo ratings yet
- Immediate Implant Placement FollowingDocument3 pagesImmediate Implant Placement FollowingHarsh ChansoriaNo ratings yet
- Immediate Dentoalveolar Restoration in Compromised Sockets: Technique and Bone BiologyDocument14 pagesImmediate Dentoalveolar Restoration in Compromised Sockets: Technique and Bone BiologyMichal PerkowskiNo ratings yet
- 2023 - Clinical observation of Porcine Collagen Membrane + artificial Bovine Bone Granules Guided tissue regeneration combined with Autologous CGF in the treatment of severe periodontitis bone defect - RCTDocument5 pages2023 - Clinical observation of Porcine Collagen Membrane + artificial Bovine Bone Granules Guided tissue regeneration combined with Autologous CGF in the treatment of severe periodontitis bone defect - RCTJontavius GilbertNo ratings yet
- Ejd 9 288Document6 pagesEjd 9 288rahmat riduanNo ratings yet
- 06.Long-Term Follow-Up On Soft and Hard TissueDocument8 pages06.Long-Term Follow-Up On Soft and Hard Tissue친절No ratings yet
- Endodontic and Surgical Treatment of Chronic Apical Periodontitis A Randomized Clinical StudyDocument9 pagesEndodontic and Surgical Treatment of Chronic Apical Periodontitis A Randomized Clinical StudyexpertodentalboliviaNo ratings yet
- Witek 2019Document7 pagesWitek 2019Alejandro FereñoNo ratings yet
- Preserving of A Tooth Related With Central Giant Cell Granuloma With Noninvasive Curettage Years Followedup Case ReportDocument4 pagesPreserving of A Tooth Related With Central Giant Cell Granuloma With Noninvasive Curettage Years Followedup Case ReportMaya GusmanNo ratings yet
- Apiko 3Document4 pagesApiko 3Asri DamayantiNo ratings yet
- Single Visit Apexification Procedure of A Traumatically Injured Tooth With A Novel Bioinductive Material (Biodentine)Document5 pagesSingle Visit Apexification Procedure of A Traumatically Injured Tooth With A Novel Bioinductive Material (Biodentine)fatimahNo ratings yet
- GTRJan 2021Document5 pagesGTRJan 2021Astha TimothyNo ratings yet
- Comparative Evaluation of Initial Crestal Bone Loss Around Dental Implants Using Flapless or Flap Method: An in Vivo StudyDocument9 pagesComparative Evaluation of Initial Crestal Bone Loss Around Dental Implants Using Flapless or Flap Method: An in Vivo StudyIJAR JOURNALNo ratings yet
- A Multiple Tooth Tale: A Unique Case Report of 33 OdontomesDocument5 pagesA Multiple Tooth Tale: A Unique Case Report of 33 OdontomesIJAR JOURNALNo ratings yet
- 737 Ijar-23255Document7 pages737 Ijar-23255Louis HutahaeanNo ratings yet
- The Management of Periodontitis With HypercementosDocument4 pagesThe Management of Periodontitis With HypercementosPretty HiaNo ratings yet
- The Influence of Cortical Bone Perforation On Guided Bone Regeneration in HumansDocument6 pagesThe Influence of Cortical Bone Perforation On Guided Bone Regeneration in Humanspin.to.teethNo ratings yet
- The Applications of Regenerative Medicine in Sinus Lift Procedures A Systematic ReviewDocument14 pagesThe Applications of Regenerative Medicine in Sinus Lift Procedures A Systematic ReviewBagis Emre GulNo ratings yet
- Interdisciplinary Management of A Severely Compromised Periodontal Patient - Case ReportDocument10 pagesInterdisciplinary Management of A Severely Compromised Periodontal Patient - Case ReportAPinhaoFerreiraNo ratings yet
- Assessment of Bone Regeneration After Placement of Immediate Implants Using Sticky Bone and CGF MembraneDocument8 pagesAssessment of Bone Regeneration After Placement of Immediate Implants Using Sticky Bone and CGF MembraneIJAR JOURNALNo ratings yet
- 10 1111@cid 12748Document8 pages10 1111@cid 12748Behnam TaghaviNo ratings yet
- PDF Docs 1Document8 pagesPDF Docs 1vivek kNo ratings yet
- DR Bhaumik Nanavati Proof ApprovedDocument6 pagesDR Bhaumik Nanavati Proof ApprovedFahmi FirmansyahNo ratings yet
- Anterior Ridge Extension Using Modified Kazanjian Technique in Mandible-A Clinical StudyDocument5 pagesAnterior Ridge Extension Using Modified Kazanjian Technique in Mandible-A Clinical StudyHélder MouraNo ratings yet
- Cone Beam Computed Tomography As A Tool For The Analysis of Bone Fill in Intrabony Defects With Use of Nanogentm Bone GraftDocument10 pagesCone Beam Computed Tomography As A Tool For The Analysis of Bone Fill in Intrabony Defects With Use of Nanogentm Bone GraftIJAR JOURNALNo ratings yet
- Caso Clínico de Sausage TechniqueDocument12 pagesCaso Clínico de Sausage Techniquealessandra camposNo ratings yet
- IJPRDDEC2013EYEPROSTHESISDocument6 pagesIJPRDDEC2013EYEPROSTHESISSahana RangarajanNo ratings yet
- Retrospective Study: Lateral Ridge Augmentation Using Autogenous Dentin: Tooth-Shell Technique vs. Bone-Shell TechniqueDocument12 pagesRetrospective Study: Lateral Ridge Augmentation Using Autogenous Dentin: Tooth-Shell Technique vs. Bone-Shell TechniqueNarissaporn ChaiprakitNo ratings yet
- Surgical Management of Periapical Lesion Inmaxillary Incisorswith Combined Bone Graft and Platelet - Rich Fibrin: A Case ReportDocument5 pagesSurgical Management of Periapical Lesion Inmaxillary Incisorswith Combined Bone Graft and Platelet - Rich Fibrin: A Case ReportTMDCH JournalNo ratings yet
- A Study of Functional Outcome of Distal Tibial Extra-Articular Fracture Fixed With Locking Compression Plate Using MIPPO TechniqueDocument6 pagesA Study of Functional Outcome of Distal Tibial Extra-Articular Fracture Fixed With Locking Compression Plate Using MIPPO TechniqueShivalingaiah GirishNo ratings yet
- Strategic Use of Telescopic Retainers and Semi-Rigid Precision Attachments in A Geriatric Patient: A Case ReportDocument6 pagesStrategic Use of Telescopic Retainers and Semi-Rigid Precision Attachments in A Geriatric Patient: A Case ReportAlina AlexandraNo ratings yet
- The Efficiency of Using Advanced PRF-xenograft Mixture Around Immediate Implants in The Esthetic Zone: A Randomized Controlled Clinical TrialDocument6 pagesThe Efficiency of Using Advanced PRF-xenograft Mixture Around Immediate Implants in The Esthetic Zone: A Randomized Controlled Clinical TrialAnukriti SrivastaavaNo ratings yet
- Regenerative Pulp Therapy For Immature Non-Vital Tooth: A Case ReportDocument4 pagesRegenerative Pulp Therapy For Immature Non-Vital Tooth: A Case ReportHansen WalaNo ratings yet
- CCD 4 509Document3 pagesCCD 4 509gbaez.88No ratings yet
- BIODENTINEDocument5 pagesBIODENTINERiyoandaNo ratings yet
- Platelet Rich Fibrin in Implant Dentistry in Combination With New Bone Regenerative Techique in Elderly PatientsDocument12 pagesPlatelet Rich Fibrin in Implant Dentistry in Combination With New Bone Regenerative Techique in Elderly PatientsgeraldineNo ratings yet
- PeriimplantitisDocument4 pagesPeriimplantitisFantino UreñaNo ratings yet
- Hegde 2014Document4 pagesHegde 2014Harshitha RajannaNo ratings yet
- Periosteum-Derived Micro-Grafts For Tissue RegenerDocument6 pagesPeriosteum-Derived Micro-Grafts For Tissue RegenerAndrea AriasNo ratings yet
- Roll Man 2013Document6 pagesRoll Man 2013SergioNo ratings yet
- 1 Ijdrdjun20181Document4 pages1 Ijdrdjun20181TJPRC PublicationsNo ratings yet
- Peri-Implant Complications: A Clinical Guide to Diagnosis and TreatmentFrom EverandPeri-Implant Complications: A Clinical Guide to Diagnosis and TreatmentNo ratings yet
- Research Article: Periodontal ScienceDocument10 pagesResearch Article: Periodontal ScienceJontavius GilbertNo ratings yet
- 2023 - Quirynen - Do Autologous Platelet Concentrates APCs Have A Role in Intra Oral Bone - ReviewDocument16 pages2023 - Quirynen - Do Autologous Platelet Concentrates APCs Have A Role in Intra Oral Bone - ReviewJontavius GilbertNo ratings yet
- Long-Term Clinical Outcomes of Periodontal Regeneration With Enamel Matrix Derivative: A Retrospective Cohort Study With A Mean Follow-Up of 10 YearsDocument12 pagesLong-Term Clinical Outcomes of Periodontal Regeneration With Enamel Matrix Derivative: A Retrospective Cohort Study With A Mean Follow-Up of 10 YearsJontavius GilbertNo ratings yet
- 2013 - Holtzclaw - Amnion Chorion Allograft Barrier Used For Guided Tissue Regeneration TreatmentDocument7 pages2013 - Holtzclaw - Amnion Chorion Allograft Barrier Used For Guided Tissue Regeneration TreatmentJontavius GilbertNo ratings yet
- Preoperative PhysiotherapyDocument15 pagesPreoperative PhysiotherapysstavrosNo ratings yet
- Block I - Subspec EndorsementsDocument4 pagesBlock I - Subspec EndorsementsCarlos NiñoNo ratings yet
- postMBBSallotmentROUNDone PDFDocument163 pagespostMBBSallotmentROUNDone PDFrosyuaNo ratings yet
- Comparison of Hyperbaric Levobupivacaine/ Bupivacaine For Ceserean SectionDocument6 pagesComparison of Hyperbaric Levobupivacaine/ Bupivacaine For Ceserean SectionIJAR JOURNALNo ratings yet
- CJDocument6 pagesCJjanella tatingNo ratings yet
- Efficacy and Safety of Forced Air Warming System Versus Passive Warming Measures in Major Surgeries A Systematic ReviewDocument8 pagesEfficacy and Safety of Forced Air Warming System Versus Passive Warming Measures in Major Surgeries A Systematic ReviewHerald Scholarly Open AccessNo ratings yet
- Buffalo Catalogue 2018Document40 pagesBuffalo Catalogue 2018زكريا دبوانNo ratings yet
- UntitledDocument4 pagesUntitledCarl GarciaNo ratings yet
- Royal Medical Services Professional Training Division Logbook For Surgery ResidentsDocument58 pagesRoyal Medical Services Professional Training Division Logbook For Surgery ResidentsMohammed SameerNo ratings yet
- Cognitair BrochureDocument12 pagesCognitair BrochureNikhil VallamkonduNo ratings yet
- Biliary AtresiaDocument13 pagesBiliary AtresiaGündüz AğayevNo ratings yet
- Medical Terminology A Short Course 7Th Edition Chabner Test Bank Full Chapter PDFDocument33 pagesMedical Terminology A Short Course 7Th Edition Chabner Test Bank Full Chapter PDFdonaldbau62h100% (12)
- Lymphedema Classification, Diagnosis, TherapyDocument12 pagesLymphedema Classification, Diagnosis, Therapymaevy dwiNo ratings yet
- Final Nursing Care PlanDocument12 pagesFinal Nursing Care PlanBerina SelimovicNo ratings yet
- Endoscopic Release of The Piriformis TendonDocument6 pagesEndoscopic Release of The Piriformis TendonKinjal SharmaNo ratings yet
- Anesthetic Nursing L5Document79 pagesAnesthetic Nursing L5MaxNo ratings yet
- Thoracic - Outlet - Syndrome TOS NEWDocument26 pagesThoracic - Outlet - Syndrome TOS NEWHanine HassanNo ratings yet
- The New Dimension: User Guide G and CDocument96 pagesThe New Dimension: User Guide G and CForkasfkgunpadNo ratings yet
- ISAPS 2017 International Study Cosmetic Procedures NEWDocument73 pagesISAPS 2017 International Study Cosmetic Procedures NEWEva Marie NejarNo ratings yet
- Optimal Structure of Cardiac Surgery UnitDocument9 pagesOptimal Structure of Cardiac Surgery Unitshoriwe68No ratings yet
- Ehra White Book 2015 Web Final 1Document592 pagesEhra White Book 2015 Web Final 1Earth BorneNo ratings yet
- Tamang Sagot: 1. What Are The Goals of The Z Benefits?Document7 pagesTamang Sagot: 1. What Are The Goals of The Z Benefits?Ramil LaysonNo ratings yet
- Vanguard ROCC BrochureDocument2 pagesVanguard ROCC BrochureBobNo ratings yet
- Ethico - Moral Responsibility of Nurses in Surgery: Ethical PrinciplesDocument9 pagesEthico - Moral Responsibility of Nurses in Surgery: Ethical PrinciplesClaire BatiaoNo ratings yet
- Children Part I Continuation TABLEDocument5 pagesChildren Part I Continuation TABLEMaikka IlaganNo ratings yet
- Grafts and Grafting Techniques in Implants - A ReviewDocument25 pagesGrafts and Grafting Techniques in Implants - A ReviewIJAR JOURNALNo ratings yet