Professional Documents
Culture Documents
DD Past PPR 5 (Solved)
DD Past PPR 5 (Solved)
Uploaded by
Eliza Butt0 ratings0% found this document useful (0 votes)
4 views29 pagesOriginal Title
DD past ppr 5 (solved)
Copyright
© © All Rights Reserved
Available Formats
PDF or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
0 ratings0% found this document useful (0 votes)
4 views29 pagesDD Past PPR 5 (Solved)
DD Past PPR 5 (Solved)
Uploaded by
Eliza ButtCopyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
You are on page 1of 29
Write a detailed note on Comparison of Systemic
Versus Musculoskeletal Pain?
Pain is an unpleasant sensation experienced by
individuals in response to actual or potential
tissue damage.
It is a complex and multifaceted phenomenon
that can be classified into different types based
on its location, duration, intensity, and underlying
cause.
Two broad categories of pain are systemic and
musculoskeletal pain, which differ in their
underlying mechanisms, location, and clinical
alles
Systemic Pain:
Systemic pain refers to pain that originates from
deep tissues and organs, such as the viscera, that
are innervated by autonomic nerves. It is often
described as a diffuse, dull, and aching sensation
that is difficult to localize.
Systemic pain can arise from various conditions,
including inflammation, infection, ischemia, or
cancer, and it is often accompanied by other
SV7an) 2) Kola teo0 (Ne M-1U- 1PM RAT lc] XM E- Ue UL CMmLaLe}
loss of appetite.
Systemic pain can also be referred to other areas
of the body and can be exacerbated by emotional
stress or physical activity. Examples of conditions
that can cause systemic pain include
fibromyalgia, chronic fatigue syndrome, lupus,
and irritable bowel syndrome.
Musculoskeletal Pain:
Musculoskeletal pain, on the other hand, refers to
pain that originates from the musculoskeletal
system, which includes the bones, joints,
muscles, tendons, and ligaments. It is often
described as a sharp, stabbing, or throbbing
sensation that is well-localized to a specific area
of the body.
Musculoskeletal pain can be caused by various
conditions such as sprains, strains, fractures,
osteoarthritis, rheumatoid arthritis, tendonitis,
and bursitis. Musculoskeletal pain can be
exacerbated by physical activity, cold weather, or
prolonged sitting or standing.
Differences between Systemic and
Musculoskeletal Pain:
Location:
The primary difference between systemic and
musculoskeletal pain is their location. Systemic
pain is often diffuse and difficult to localize, while
musculoskeletal pain is well-localized to a
specific area of the body.
Nature:
Systemic pain is often described as a dull, aching
sensation, while musculoskeletal pain is
described as a sharp, stabbing, or throbbing
sensation.
Causes:
Systemic pain can be caused by a wide range of
conditions, including inflammation, infection,
ischemia, or cancer, while musculoskeletal pain is
mainly caused by disorders of the
musculoskeletal system, such as sprains, strains,
and osteoarthritis.
Associated Symptoms:
Systemic pain is often accompanied by other
symptoms, such as fever, malaise, fatigue, and
loss of appetite, while musculoskeletal pain is
typically not associated with these symptoms.
Referred Pain:
Systemic pain can be referred to other areas of
the body, while musculoskeletal pain is usually
not referred.
Write a note on nail bed assessment
SU cMarel Mem RU ecel MUM Ulg egg crea Un METI
plate, and it is responsible for nail growth and
protection. Nail bed assessment is an important
part of a physical examination, especially for
Pe-V t= a1 MAUL Arla) (Ole (xoe) mm wT Me Xt oooe
The assessment of the nail bed involves
examining the nail plate, surrounding skin, and
the nail bed itself. The assessment may include
the following steps:
Inspection:
The clinician inspects the nail plate, looking for
any discoloration, ridges, deformities, or signs of
trauma or infection. They also examine the
surrounding skin for signs of inflammation,
redness, or tenderness.
Lazlleyc1t(0 a
The clinician gently presses on the nail plate to
check for tenderness or pain. They may also
press on the surrounding tissue to assess for any
signs of infection.
Sensory examination:
The clinician tests the patient's sensation in the
nail bed by touching it with a cotton swab or
other soft object.
Capillary refill test:
The clinician presses on the nail bed and releases
fe coool Sta eae om ORCA
to its normal color. Delayed capillary refill can
indicate poor blood flow to the nail bed.
Range of motion:
The clinician checks the range of motion of the
finger or toe to assess for any joint or tendon
injuries that may affect the nail bed.
Overall, nail bed assessment is an important part
of the physical examination, and it can provide
valuable information about the patient's overall
health, as well as any underlying nail conditions
or injuries that require further investigation or
treatment.
Write a note on lymph node palpation
Lymph node palpation is a physical examination
technique used by healthcare professionals to
assess the size, consistency, mobility, and
tenderness of lymph nodes.
Lymph nodes are small, bean-shaped structures
found throughout the body, but they are most
commonly palpable in the neck, armpit, and groin
regions.
During lymph node palpation, the healthcare
professional will use their fingers to feel for any
enlarged or tender lymph nodes. They may use
one or both hands to gently press down on the
skin over the lymph nodes to feel their size and
consistency. They may also use a rolling motion
to assess their mobility.
Lymph node palpation is typically performed as
part of a routine physical examination, or when a
patient presents with symptoms such as swelling,
tenderness, or redness in an area of the body
where lymph nodes are located. Enlarged or
tender lymph nodes can be a sign of an infection,
inflammation, or cancer, and further diagnostic
testing may be necessary.
It's important to note that lymph node palpation
should be performed by a trained healthcare
professional, as inexperienced or incorrect
techniques can lead to inaccurate results or even
harm to the patient. If you have concerns about
your lymph nodes or any symptoms you are
experiencing, you should speak to your
healthcare provider.
Write a detailed note on Mechanisms of Referred
Visceral Pain?
Visceral pain refers to pain that arises from the
organs or tissues in the body's cavities, such as
the abdomen, thorax, or pelvis. Referred visceral
pain occurs when pain is perceived in an area of
the body that is innervated by the same spinal
segments as the affected organ but is not the
location of the organ itself.
The mechanisms underlying referred visceral
pain are complex and not entirely understood.
This note will outline some of the proposed
mechanisms of referred visceral pain.
Convergence-Projection Theory:
The convergence-projection theory is the most
widely accepted theory to explain referred
visceral pain. According to this theory, the
nociceptive (pain-sensing) fibers from an organ
and somatic (body surface) tissues converge on
the same second-order neurons in the dorsal
horn of the spinal cord.
These neurons then project to the same areas of
the brain, causing confusion in the pain
perception. This results in the perception of pain
in the somatic tissue even though the actual
source of the pain is the visceral organ.
Segmental Autonomic Dysreflexia:
Segmental autonomic dysreflexia (SAD) is a
proposed mechanism for referred visceral pain in
patients with spinal cord injury. SAD occurs when
SU e-e RAM ALC) DUO AM Ca MNO lenacl Mie lato Roll
the autonomic nervous system, which can result
in the spread of pain signals to nearby somatic
tissue. This can result in the perception of pain in
areas that are not directly innervated by the
affected organ.
Shared Pathways:
The sensory fibers from the viscera and somatic
SUSI Saree X Ny OR MNES
where they converge before transmitting to the
cortex. This shared pathway allows for cross-talk
between the two types of fibers, leading to the
perception of pain in the somatic tissue.
Sensitization:
Sensitization refers to the increased sensitivity of
the neurons in the dorsal horn of the spinal cord
to pain signals. This can occur as a result of
inflammation, injury, or chronic pain. When
sensitization occurs, a stimulus that would not
normally cause pain can trigger a pain response.
This can lead to the perception of pain in somatic
tissue that is not directly innervated by the
affected organ.
(eo ler-leSTousiiir4-1 (et B
OTnie ES ela melee eM VaR Real Ue}
nervous system becomes sensitized to pain
signals. This can occur as a result of chronic
pain, injury, or inflammation. When central
sensitization occurs, the threshold for pain
perception is lowered, leading to the perception
(olor EXOLRAL1 Com CSU CM UAL nCoL me] [Kore
innervated by the affected organ.
In conclusion, the mechanisms underlying
referred visceral pain are complex and not
entirely understood. Proposed mechanisms
include convergence-projection theory,
segmental autonomic dysreflexia, shared
pathways, sensitization, and central sensitization.
Further research is needed to fully understand
the mechanisms of referred visceral pain and
develop effective treatments for this condition.
Write a note on Signs and symptoms of
Gastrointestinal Disorder?
Gastrointestinal (Gl) disorders refer to a group of
medical conditions that affect the digestive
system, which includes the mouth, esophagus,
stomach, intestines, liver, pancreas, and
gallbladder.
Signs and symptoms of GI disorders can vary
depending on the type and severity of the
Cofe ate lean
However, some common signs and symptoms
include:
Abdominal pain or discomfort:
This is acommon symptom of many GI
disorders, including ulcers, gastritis, irritable
bowel syndrome, and inflammatory bowel
(elk
Bloating:
A feeling of fullness or swelling in the abdomen,
which can be caused by excessive gas or fluid in
the digestive tract.
Constipation:
Difficulty passing stool or infrequent bowel
movements, which can be caused by a variety of
factors such as low fiber diet, dehydration, or
medication side effects.
Pye TetntaeH
Loose or watery stools, which can be caused by
infections, food intolerance, or inflammatory
bowel disease.
Nausea and vomiting:
These symptoms can be caused by a variety of GI
disorders, including viral gastroenteritis, food
poisoning, or motion sickness.
Heartburn or acid reflux:
A burning sensation in the chest or throat caused
by stomach acid backing up into the esophagus,
which can be caused by gastroesophageal reflux
disease (GERD) or hiatal hernia.
Blood in the stool:
This can be a sign of a serious GI disorder, such
as colorectal cancer, inflammatory bowel disease,
or hemorrhoids.
Write a note on clinical manifestation of
malignancy?
Malignancy refers to the presence of cancer cells
that have the ability to invade and spread to
surrounding tissues and organs in the body.
Clinical manifestations of malignancy can vary
depending on the location and stage of the
cancer.
Some common clinical manifestations of
malignancy include:
Fatigue:
Cancer patients often experience fatigue that is
not relieved by rest or sleep. This is due to the
body's increased energy demands as it fights the
cancer.
Weight loss:
Unexplained weight loss can be a symptom of
malignancy. This is especially true for cancers of
the digestive system.
Pain:
Cancer can cause pain in different parts of the
body, such as the bones, muscles, or organs. Pain
can be due to the pressure exerted by the tumor
or due to cancer cells spreading to other parts of
the body.
Changes in bowel or bladder habits:
Some cancers can cause changes in bowel or
bladder habits, such as frequent urination,
constipation, or diarrhea.
AS) ae meuar-lale [on
Skin changes such as new moles, changes in the
shape or color of existing moles, or skin sores
that do not heal can be a sign of skin cancer.
Difficulty swallowing:
This can be a symptom of cancers of the
esophagus or throat.
Cough or hoarseness:
A persistent cough or hoarseness can be a
symptom of lung cancer or throat cancer.
Abnormal bleeding:
Unusual bleeding, such as bleeding from the
vagina between periods or after menopause, or
bleeding from the rectum, can be a sign of
cancer.
It's important to note that these symptoms can
also be caused by other conditions, so it's
important to seek medical attention if you are
experiencing any of these symptoms. Early
detection and treatment of cancer can improve
the chances of successful treatment and
recovery.
Write a note on classification of blood disorder?
Blood disorders are conditions that affect the
components of blood, including red blood cells,
white blood cells, platelets, and plasma. These
disorders can be classified in several ways based
on the affected component, underlying cause,
symptoms, and treatment options.
Here are some of the common classifications of
blood disorders:
Anemia:
Anemia is a condition in which there are not
enough red blood cells to carry oxygen to the
body's tissues. Anemia can be caused by various
factors such as iron deficiency, vitamin
deficiency, blood loss, or genetic factors.
Bleeding disorders:
Bleeding disorders are conditions in which the
blood's ability to clot is impaired. This can result
in excessive bleeding or bruising even with minor
injuries. Hemophilia, von Willebrand disease, and
thrombocytopenia are some common bleeding
disorders.
Blood cancers:
Blood cancers are cancers that affect the blood
and bone marrow, including leukemia, lymphoma,
and myeloma. These cancers affect the
production and function of blood cells and can
cause symptoms such as fatigue, weakness, and
increased risk of infections.
Clotting disorders:
Clotting disorders are conditions in which the
blood's ability to clot is increased, leading to the
formation of blood clots. These clots can cause
serious health problems such as heart attack,
stroke, or pulmonary embolism. Deep vein
thrombosis and thrombophilia are some
common clotting disorders.
Hemoglobinopathies:
Hemoglobinopathies are a group of inherited
blood disorders that affect the production or
structure of hemoglobin, the protein that carries
oxygen in the blood. Sickle cell anemia and
thalassemia are some examples of
hemoglobinopathies.
White blood cell disorders:
White blood cell disorders affect the production,
function, or number of white blood cells, which
are responsible for fighting infections. These
disorders can cause an increased risk of
infections, autoimmune diseases, or leukemia.
Write a note on pulmonary disorder?
Pulmonary disorders refer to a group of diseases
that affect the lungs and the respiratory system.
These disorders can range from mild to severe
and can affect people of all ages.
Some of the most common pulmonary disorders
include asthma, chronic obstructive pulmonary
disease (COPD), lung cancer, pneumonia, and
pulmonary fibrosis.
Asthma:
is a chronic respiratory condition that causes the
airways to become inflamed and narrow, making
it difficult to breathe. Symptoms of asthma
include wheezing, shortness of breath, coughing,
and chest tightness. Asthma can be managed
with medication and avoiding triggers such as
allergens, smoke, and exercise.
COPD:
is a progressive lung disease that includes
chronic bronchitis and emphysema. It is caused
by long-term exposure to irritants such as
cigarette smoke, air pollution, and chemical
fumes. Symptoms of COPD include coughing,
shortness of breath, and chest tightness. There is
no cure for COPD, but it can be managed with
medication, pulmonary rehabilitation, and lifestyle
changes.
Lung cancer:
is a type of cancer that begins in the lungs and
can spread to other parts of the body. Symptoms
of lung cancer include coughing, chest pain,
shortness of breath, and weight loss. Treatment
options for lung cancer include surgery, radiation
therapy, chemotherapy, and targeted therapy.
Pneumonia:
is an infection of the lungs that can be caused by
bacteria, viruses, or fungi. Symptoms of
pneumonia include coughing, fever, chills, and
shortness of breath. Treatment for pneumonia
may include antibiotics, antiviral medication, and
oxygen therapy.
Pulmonary fibrosis:
is a lung disease that causes scarring of the lung
tissue, making it difficult to breathe. Symptoms of
pulmonary fibrosis include shortness of breath,
dry cough, and fatigue. There is no cure for
pulmonary fibrosis, but treatment can help
manage symptoms and slow down the
progression of the disease.
Write a note on Screening for Pulmonary Causes
of Shoulder Pain?
Shoulder pain is a common symptom that can be
caused by a variety of conditions, including
pulmonary causes. Screening for pulmonary
causes of shoulder pain is important, as early
detection and treatment can improve patient
outcomes.
One of the most common pulmonary causes of
shoulder pain is a pulmonary embolism, which is
a blood clot that travels to the lungs. Other
potential causes include pneumonia and pleuritis,
which is inflammation of the lining of the lungs.
Boe el(- 1m 0) IN ACr ROMS Ol elmo
healthcare providers may perform a thorough
physical exam and ask the patient about their
symptoms. They may also order diagnostic tests,
such as a chest X-ray or CT scan, to evaluate the
lungs and check for any abnormalities.
In addition, providers may also perform a blood
test to check for a specific marker known as
D-dimer, which can indicate the presence of a
blood clot. If the D-dimer test is positive, further
testing, such as a CT pulmonary angiogram, may
be necessary to confirm the presence of a
pulmonary embolism.
Overall, screening for pulmonary causes of
shoulder pain is an important step in diagnosing
and treating underlying conditions that may be
contributing to the patient's symptoms. It is
important for patients to seek medical attention if
they experience persistent or severe shoulder
pain, especially if it is accompanied by other
symptoms such as shortness of breath or chest
ry 1
Write a note on Screening for Infectious Causes
of Back Pain?
Back pain can be caused by a variety of factors,
including infections. Although infectious causes
of back pain are relatively rare, they can be
Sale Tae Wea ACen
untreated.
Therefore, it is important to screen for infectious
causes of back pain in patients who present with
back pain, especially if they have risk factors for
infection.
The first step in screening for infectious causes
of back pain is to take a detailed medical history,
including any recent travel, exposure to animals,
or history of intravenous drug use.
The physical examination should include an
assessment of the patient's vital signs, a
thorough examination of the spine, and an
evaluation for any signs of systemic infection,
such as fever, chills, or rigors.
Laboratory tests:
Laboratory tests may be ordered to screen for
infectious causes of back pain. These may
include a complete blood count (CBC),
erythrocyte sedimentation rate (ESR), C-reactive
protein (CRP), and blood cultures. These tests
can help detect signs of infection, such as an
elevated white blood cell count or increased
el Mey Maire Tan Teale h M RAT LCLCR
If an infectious cause of back pain is suspected,
imaging studies may be ordered to further
evaluate the spine and identify any abscesses or
other signs of infection. Magnetic resonance
imaging (MRI) is the imaging modality of choice
for evaluating the spine for infectious causes of
1of-to)- ae)
Treatment for infectious causes of back pain
may involve antibiotics, surgical drainage of
abscesses, or other interventions, depending on
the specific cause of the infection.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5814)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Lec 14 Screening The Head Neck and BackDocument50 pagesLec 14 Screening The Head Neck and BackEliza ButtNo ratings yet
- Chapter10 Professional Development, CompetenceDocument19 pagesChapter10 Professional Development, CompetenceEliza ButtNo ratings yet
- Chapter 1 Introduction The Physical Therapist As ProfessionalDocument42 pagesChapter 1 Introduction The Physical Therapist As ProfessionalEliza ButtNo ratings yet
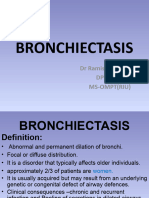
- BronchiectasisDocument21 pagesBronchiectasisEliza ButtNo ratings yet
- Integu10 Wound PainDocument13 pagesIntegu10 Wound PainEliza ButtNo ratings yet
- Integu11 Pressure UlcresDocument11 pagesIntegu11 Pressure UlcresEliza ButtNo ratings yet
- Cystic FibrosisDocument26 pagesCystic FibrosisEliza ButtNo ratings yet