Professional Documents
Culture Documents
Goddard 2024 Oi 231553 1705443705.31129
Uploaded by
Sabrina NMOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Goddard 2024 Oi 231553 1705443705.31129
Uploaded by
Sabrina NMCopyright:
Available Formats
Original Investigation | Pediatrics
Prevalence, Incidence, and Reversal Pattern of Childhood Stunting
From Birth to Age 2 Years in Ethiopia
Frederick G. B. Goddard, MS, PhD; Bezawit Mesfin Hunegnaw, MD, MPH; Jonathan Luu, MS; Sebastien J. P. A. Haneuse, PhD; Mesfin Zeleke, MD, MPH;
Yahya Mohammed, BSc; Chalachew Bekele, BSc, MPH; Daniel Tadesse, BSc, MPH; Meles Solomon, BSc, MSc; Delayehu Bekele, MD, MPH; Grace J. Chan, MD, MPH, PhD
Abstract Key Points
Question What is the burden,
IMPORTANCE Although there has been a reduction in stunting (low-height-for-age and
incidence, and reversal pattern of
low-length-for-age), a proxy of malnutrition, the prevalence of malnutrition in Ethiopia is still high.
childhood stunting in Ethiopia?
Child growth patterns and estimates of stunting are needed to increase awareness and resources to
improve the potential for recovery. Findings In this cohort study that
included 3674 children, the prevalence
OBJECTIVE To estimate the prevalence, incidence, and reversal of stunting among children aged 0 of stunting at 2 years of age was 57.4%.
to 24 months. Incidence of stunting was highest
between the ages of 12 to 24 months
DESIGN, SETTING, AND PARTICIPANTS This population-based cohort study of the Birhan Maternal (51.0%) and rates of stunting reversal
and Child Health cohort in North Shewa Zone, Amhara, Ethiopia, was conducted between December were highest by 6 months of
2018 and November 2020. Eligible participants included children aged 0 to 24 months who were age (63.5%).
enrolled during the study period and had their length measured at least once. Data analysis occurred
Meaning These findings suggest that
from Month Year to Month Year.
understanding patterns of linear growth
and onset of growth faltering or
MAIN OUTCOMES AND MEASURES The primary outcome of this study was stunting, defined as
recovery serves as a critical input to
length-for-age z score (LAZ) at least 2 SDs below the mean. Z scores were also used to determine the
meet national and global targets of
prevalence, incidence, and reversal of stunting at each key time point. Growth velocity was
ending malnutrition.
determined in centimeters per month between key time points and compared with global World
Health Organization (WHO) standards for the same time periods. Heterogeneity was addressed by
excluding outliers in sensitivity analyses using modeled growth trajectories for each child. + Supplemental content
Author affiliations and article information are
RESULTS A total of 4354 children were enrolled, out of which 3674 (84.4%; 1786 [48.7%] female) listed at the end of this article.
had their length measured at least once and were included in this study. The median population-level
length was consistently below WHO growth standards from birth to 2 years of age. The observed
prevalence of stunting was highest by 2 years of age at 57.4% (95% CI, 54.8%-9 60.0%). Incidence
of stunting increased over time and reached 51.0% (95% CI, 45.3%-56.6%) between ages 12 and 24
months. Reversal was 63.5% (95% CI, 54.8%-71.4%) by age 6 months and 45.2% (95% CI, 36.0%-
54.8%) by age 2 years. Growth velocity point estimate differences were slowest compared with
WHO standards during the neonatal period (−1.4 cm/month for girls and −1.6 cm/month for boys).
There was substantial heterogeneity in anthropometric measurements.
CONCLUSIONS AND RELEVANCE The evidence from this cohort study highlights a chronically
malnourished population with much of the burden associated with growth faltering during the
neonatal periods as well as after 6 months of age. To end all forms of malnutrition, growth faltering
in populations such as that in young children in Amhara, Ethiopia, needs to be addressed.
JAMA Network Open. 2024;7(1):e2352856. doi:10.1001/jamanetworkopen.2023.52856
Open Access. This is an open access article distributed under the terms of the CC-BY License.
JAMA Network Open. 2024;7(1):e2352856. doi:10.1001/jamanetworkopen.2023.52856 (Reprinted) January 24, 2024 1/10
Downloaded from jamanetwork.com by Sabrina NM on 04/04/2024
JAMA Network Open | Pediatrics Prevalence, Incidence, and Reversal Pattern of Childhood Stunting in Ethiopia
Introduction
One central theme of the United Nations Sustainable Development Goals (SDGs) is child
development, including Goals 2 and 4, which aim to end hunger and improve education.1 Nutritional
status plays a major role in reaching these goals, because it is associated with both physical and
cognitive development.2 Malnutrition continues to be a major public health problem and is the most
important underlying factor associated with increased risk of illness and death, particularly in
low-income countries and among young children.3 An estimated 53% of all deaths in children
younger than 5 years are associated with malnutrition.4 Target 2.2. under Goal 2 of the SDGs set out
to end all forms of malnutrition by 2030, including meeting targets on stunting in children younger
than 5 years by 2025.5 Stunting is defined as low-length-for-age and low-height-for-age, and
indicates chronic undernutrition.6 Stunting is considered to be an important indicator for both child
physical and cognitive development,7 and is associated with environmental factors, such as living
conditions and nutrition.8 In 2019, an estimated 144 million children younger than 5 years (21%)
globally were stunted.9
To meet the SDGs and end all forms of malnutrition, a wealth of evidence has been generated
to understand how and when to intervene. A recent collection of research by the Ki Child Growth
Consortium10,11 that combined anthropometric data from over 100 000 children enrolled in 35
longitudinal cohorts across 15 low- and middle-income countries found that the incidence of stunting
peaks early between birth and 3 months of age. Recovery from stunting was rare, with only 5% of
children reversing their stunting status any given month.11 The prevalence of child stunting in
sub-Saharan Africa remains high, including in Ethiopia.12 Although there has been a reduction in
stunting over the last 2 decades, in 2016, an estimated 38% of children younger than 5 years in
Ethiopia were stunted.13 There is high spatial heterogeneity of stunting within Ethiopia,14 with the
highest prevalence of stunting occurring in the Amhara region.15 As part of the World Health
Assembly global nutrition targets, Ethiopia aims to reduce stunting in children younger than 5 years
to 27% by 2025 with an expected mean annual reduction rate of 6%.16,17 Current estimates show
that the country is off track following a mean annual reduction rate of only 2.4%.18
To achieve these goals, rigorous studies that not only describe the magnitude of the problem
but also the dynamics of growth and changes through childhood are imperative. Accurate depiction
of the growth process that includes analysis of growth trajectories and patterns among populations
and subgroups is critical to understanding and identifying key time points that predispose children to
growth faltering. There are limited longitudinal data on stunting, particularly from underserved
populations in low resource settings. Although the recent studies by the Ki Child Growth Consortium
included large, pooled data sets of longitudinal anthropometric data, they did not include data from
Ethiopia. Infants younger than 6 months of age are often excluded from nutrition surveys and
marginalized in nutrition programs,19 even though this time period is characterized not only by
maximal growth velocity but also by vulnerability to nutrition related events and insults. The Birhan
maternal and child health (MCH) cohort in Amhara, Ethiopia, can fill some of these gaps, with
longitudinal anthropometry data from birth until the child reaches their second birthday.20
Methods
Study Design
This cohort study was approved by the institutional review boards of St Paul’s Hospital, Ethiopia, and
Boston Children’s Hospital and followed the Strengthening the Reporting of Observational Studies
in Epidemiology (STROBE) reporting guideline. Written informed consent was obtained from
mothers prior to enrollment. This study was nested within the Birhan field site, a platform for
community and facility-based research and training that was established in 2018, with a focus on
maternal and child health.21 Nested in the site is an open cohort, the Birhan MCH cohort, which
JAMA Network Open. 2024;7(1):e2352856. doi:10.1001/jamanetworkopen.2023.52856 (Reprinted) January 24, 2024 2/10
Downloaded from jamanetwork.com by Sabrina NM on 04/04/2024
JAMA Network Open | Pediatrics Prevalence, Incidence, and Reversal Pattern of Childhood Stunting in Ethiopia
enrolls approximately 2000 pregnant women and their newborns per year with longitudinal
follow-up over the first 2 years of life and household data linked with health facility information.20
Study Population
All pregnant women and mothers (guardians) of children younger than 2 years of age residing in the
study area who provided consent were enrolled to the parent cohort. From December 2018 to
November 2020, children were enrolled through both a birth cohort (ie, enrolled at birth) and a
nonbirth cohort (ie, enrolled after birth). Children enrolled to the study were followed until they
reached 2 years of age.
Data Collection
A custom length board, standardized against the infant and child ShorrBoard (Weigh and Measure)
and Seca 417 infantometer (Seca) were used for length measurements. Length measurements were
performed by study nurses and midwives who were given lessons on theory and participated in lab
sessions on WHO standard child growth assessment procedures to measure length. Measurements
were recorded to the nearest 0.1 cm. Length was measured as single measurements (rather than
averaging repeated measures for patient acceptability) during scheduled child follow-up visits at
birth, on days 6, 28, and 42 after birth; and at 6 months, 12 months, and 24 months of age; as well as
from health facility visits (ie, outpatient visits or hospital admissions).
Outcomes
The primary outcome of the study was stunting, defined as length-for-age z score (LAZ) less than 2
SDs below the mean. We generated LAZ with length, age, and sex data using WHO growth
standards.22 Z scores were used to determine the prevalence, incidence, and reversal of stunting at
each key time point. International Fetal and Newborn Growth Consortium for the 21st Century
standards23,24 were used to generate LAZ scores at birth and during the neonatal period; the
standards were generated using data from low-income and middle-income countries, and adjust for
gestational age at birth, in contrast with WHO standards22 that assume all babies are born at 40
weeks gestation and, hence, can overestimate stunting prevalence at birth and during the neonatal
period. We excluded anthropometric measurements if (1) the Z scores fell outside the biologically
plausible range defined by the WHO (LAZ <−6 or LAZ >6) or (2) the measurements were abstracted
from facility charts after birth because these measurements were not validated by our data
collectors. We compared the median (IQR) length of children enrolled in the Birhan cohort to WHO
global growth standards22 at key time points. Growth velocity was determined in centimeters per
month between key time points and compared with global WHO standards for the same time
periods.25 We defined reversal of stunting as an LAZ no longer less than 2SDs below the mean.
Definitions of low birth weight, preterm birth, and estimation of gestational age can be found in the
eAppendix in Supplement 1.
Key time points were defined as birth, 4 weeks, 6 weeks, 6 months, 12 months, and 24 months.
Birth length measurements were defined as those that were collected within the first week of life.
For measurements at the end of the neonatal period and at 6 weeks, we included those taken at 4
weeks and 6 weeks (±1 week) after birth. For the other key time points (6 months, 12 months, and 24
months) we included measurements taken within 4 weeks of each time point.
Statistical Analysis
Empirical length measurements were stratified by sex to describe population median (IQR) length at
birth, 4 weeks (ie, the end of the neonatal period), 6 weeks, 6 months, 12 months, and 24 months
of age. Differences in medians between key time points were used to calculate monthly growth
velocity. Medians at each key time point and velocities between key time points were then compared
with WHO standards. For incidence calculations, the sample population for each time period (defined
as 2 adjoining key time points) was defined as all children that were at risk of stunting (ie, not already
JAMA Network Open. 2024;7(1):e2352856. doi:10.1001/jamanetworkopen.2023.52856 (Reprinted) January 24, 2024 3/10
Downloaded from jamanetwork.com by Sabrina NM on 04/04/2024
JAMA Network Open | Pediatrics Prevalence, Incidence, and Reversal Pattern of Childhood Stunting in Ethiopia
having stunted growth by the beginning of that time period) and have available anthropometric
Table 1. Population Summary Characteristics
measurements between 2 adjoining key time points. Similarly, for reversal, the sample population for
Participants,
each time period was defined as all children that had the chance of reversing their stunting (ie, Characteristic No./Total No. (%)
already having stunted growth by the beginning of that time period) and have available Birth cohort 2592/4354 (59.5)
anthropometric measurements at the beginning and end of the time period. To expand on our Nonbirth cohort 1762/4354 (40.5)
Children with length data 3674/4354 (84.4)
incidence and reversal analysis, we calculated incidence and reversal both sequentially (ie, comparing available
birth with 4 weeks and comparing 4 weeks with 6 weeks) and using birth as a baseline (ie, comparing Residing in rural areas 3037/3674 (82.7)
birth to 4 weeks and birth to 6 weeks). Sex
To consider potential measurement error for length in our findings, we used a mixed effects Female 1786/3670 (48.7)
model to determine potential outliers that should be removed from the analysis. Using LASSO Male 1884/3670 (51.3)
regression to determine significant covariates to include in the models, we considered 6 different Preterm births 360/2350 (15.3)
models that used a mix of fixed and random age variables and intercepts, quadratic splines, and Low birth weight 156/1732 (9.0)
Singleton births 3557/3674 (96.8)
piecewise-linear splines. Our final model included a piecewise-linear spline of age for the fixed effect,
Length measurements, 2.6 (1.6) [1-8]
and an intercept and slope of standardized age for the random effects. We determined this model mean (SD) [range]
was the best fit after comparing Akaike information criterion, Bayes information criterion, and (n = 3674)
deviance diagnostic criteria. Using the predicted outcomes and estimated standard deviation from
the model, we removed observed points that were not within 1.5 SDs of fitted trajectories. After
these measurements were removed from the data set, prevalence, incidence, and reversal estimates
were recalculated. Confidence intervals for all proportion estimates were calculated using the
Agresti-Coull method. All analyses were completed in R Version 4.2.3 (R Project for Statistical
Computing).26 Data analysis occurred from July 2021 to July 2022.
Results
We enrolled 4354 children younger than 2 years of age into the MCH cohort study, among which
3674 (84.4%; 1786 [48.7%] female) had their length measured at least once and were included in
this study (Table 1). Among children included, 3037 (82.7%) resided in rural areas and. Among 2350
children with gestational age data, 360 (15.3%) were born preterm, and among 1732 children with
birth weight data, 156 (9.0%) had low birth weight. Over the course of the study, length
measurements were taken a mean (range) of 2.6 (1-8) times for each child. Length measurements
were clustered around the scheduled follow-up visits (Figure 1). A total of 206 children whose
measurements were outside ±6 LAZ were excluded.
Median (IQR) length was lower in the study population compared with global WHO standards
at all key time points defined for this study (ie, birth, the end of the neonatal period [4 weeks], 6
weeks, 6 months, 12 months, and 24 months) (Table 2). The point estimates of the differences were
smallest at birth (−0.1 cm for girls and −0.9 cm for boys); thereafter, there was slower monthly
growth velocity point estimate differences compared with WHO standards that were most
pronounced during the neonatal period (−1.4 cm/month for girls and −1.6 cm/month for boys). After
the neonatal period, the point estimate difference in growth velocity was smaller for girls between 4
weeks and 6 weeks (−0.7 cm/month) and between 6 weeks and 6 months (−0.2 cm/month). There
was no difference in growth velocity point estimates for boys in the MCH cohort compared with
WHO standards between the end of the neonatal period and 6 weeks. Differences in growth velocity
were between −0.2 cm/month and −0.3 cm/month thereafter, resulting in the largest difference in
point estimates between median length in the MCH cohort study compared with WHO standards by
2 years of age (−6.6 cm for girls and −7.8 cm for boys).
We investigated the potential for measurement error in our data and found variation in
longitudinal length measurement for some individuals. To determine which points to exclude in a
repeated prevalence, incidence, and reversal analysis, we compared the fitted trajectories for each
individual with observed data points. Observed lengths that were 1.5 SDs away from fitted growth
trajectories for 922 measurements were removed from the modeled prevalence, incidence, and
reversal analysis (eTable in Supplement 1).
JAMA Network Open. 2024;7(1):e2352856. doi:10.1001/jamanetworkopen.2023.52856 (Reprinted) January 24, 2024 4/10
Downloaded from jamanetwork.com by Sabrina NM on 04/04/2024
JAMA Network Open | Pediatrics Prevalence, Incidence, and Reversal Pattern of Childhood Stunting in Ethiopia
Using observed data, the prevalence of stunting at birth was 16.1% (95% CI, 14.5%-17.9%) and
showed a gradual increase with a sharp rise from the age of 6 months to 24 months, reaching an
observed prevalence of 57.4% (95% CI, 54.8%-60.0%) at 24 months. Observed prevalences from
the Birhan data were higher than modeled values at birth and at 6 months, whereas prevalences
were similar at other key time points (Figure 2A).
The incidence, indicating that children were newly stunted at a given key time point compared
to the previous time point, followed a similar pattern to the prevalence except for the 6-week time
point (Figure 2B). Among 1149 newborns who were not stunted at birth, 279 (24.3%) experienced
observed incident stunting within the first month of life. The highest incidence of cases was observed
between the ages of 12 to 24 months (151 out of 296 individuals [51.0%]; 95% CI, 45.3%-56.6%)
followed by the 6 to 12 months period (192 of 591 individuals [32.5%]; 95% CI, 28.8%-36.4%).
Observed incidence estimates were, for the most part, higher than modeled. Further analysis using
birth as a common baseline time point showed a steady increase in incidence up to 2 years of age
(eFigure 1 in Supplement 1). Overall, among 531 children who were not stunted at birth, 205 (38.6%)
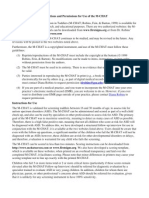
Figure 1. Distribution of Length Measurements Compared With World Health Organization (WHO) Standards
100
95
90
85
80
75
Length, cm
70
65
60
55
50
45 WHO length-for-age standard
–2 SD
40 Median
35 The figure shows the distribution of length
0 1 6 12 24
measurements for boys and girls combined.
Age, mo
Table 2. Length-for-Age and Length at Key Times Points for Girls and Boys Compared With WHO Global Standards
Girls Boys
Birth 4 wk 6wk 6 mo 12 mo 24 mo Birth 4 wk 6 wk 6 mo 12 mo 24 mo
Measurement (n = 882) (n = 787) (n = 787) (n = 825) (n = 863) (n = 688) (n = 938) (n = 775) (n = 778) (n = 830) (n = 906) (n = 733)
Length-for-age
Birhan z score, 0.00 −0.64 −0.55 −0.62 −1.17 −2.11 −0.19 −0.79 −1.07 −1.21 −1.63 −2.54
median (IQR) (−1.04 to (−1.74 to (−1.60 to (−1.79 to (−2.42 to (−3.17 to (−1.22 to (−2.05 to (−2.15 to (−2.20 to (−2.85 to (−3.70 to
1.17 0.70) 0.71) 0.40) −0.21) −1.10) 0.80 0.43) 0.34) −0.15) −0.72) −1.57)
Birhan 49.0 52.0 53.4 64.0 71.0 79.8 49.0 52.0 53.8 65.0 72.0 80.0
median (IQR) (47.3 to (50.0 to (51.5 to (61.5 to (68.0 to (76.4 to (47.5 to (50.0 to (52.0 to (62.5 to (69.0 to (76.6 to
cm 50.2) 54.0) 55.6) 66.2) 73.5) 83.0) 50.5) 54.3) 56.0) 67.0) 74.0) 83.0)
WHO standard, 49.1 53.4 55.1 65.7 74.0 86.4 49.9 54.4 56.2 67.6 75.7 87.8
cm
Birhan vs WHO −0.1 −1.4 −1.7 −1.7 −3.0 −6.6 −0.9 −2.4 −2.4 −2.6 −3.7 −7.8
difference, cm
Growth velocity,
cm/mo
Birhan NA 3.3 3.0 2.3 1.2 0.7 NA 3.3 3.9 2.4 1.2 0.7
WHO standard NA 4.7 3.7 2.5 1.4 1.0 NA 4.9 3.9 2.6 1.4 1.0
Birhan vs WHO NA −1.4 −0.7 −0.2 −0.2 −0.3 NA −1.6 0 −0.2 −0.2 −0.3
difference
Abbreviations: NA, not applicable; WHO, World Health Organization.
JAMA Network Open. 2024;7(1):e2352856. doi:10.1001/jamanetworkopen.2023.52856 (Reprinted) January 24, 2024 5/10
Downloaded from jamanetwork.com by Sabrina NM on 04/04/2024
JAMA Network Open | Pediatrics Prevalence, Incidence, and Reversal Pattern of Childhood Stunting in Ethiopia
had incident stunting at 1 year of age and 331 of 585 children with data (56.6%) had new onset
stunting by 2 years of age.
The marked difference in incidence between the 2 time points compared with difference in
prevalence among these same time points indicates the presence of a dynamic incidence and
reversal process through time. Rates of reversal (both sequentially when compared to a prior time
point and using birth as baseline) were highest by 6 months of age (Figure 2C and eFigure 2 in
Supplement 1). Among children who were already stunted at birth and thus had a chance to reverse
stunting later in life, 80 of 126 children with data (63.5%; 95% CI, 54.8%-71.4%) were able to do so
by 6 months of life and 59 of 96 children with data (61.5%; 95% CI, 51.5%-70.6%) reversed stunting
by the end of the first year of life (eFigure 2 in Supplement 1). By the age of 2 years, 47 of 104 children
with data (45.2%; 95% CI, 36.0%-54.8%) who were stunted at birth no longer had stunted growth.
Discussion
Our findings in this cohort study provide evidence that median population-level length among
children in our study sample are consistently below global standards from birth to 2 years of age.
Monthly growth velocity was slowest compared with global standards during the neonatal period
before stabilizing until the child reached 6 months of age, and then slowing again thereafter.
Incidence of stunting followed a similar trajectory, suggesting an increasing incidence of children with
newly stunted growth over time. Reversal of stunting was a frequent observation with the highest
rate of reversal occurring between birth and 6 months of age.
Figure 2. Prevalence, Incidence, and Reversal of Stunting
A Estimated prevalence of stunting B Estimated incidence of stunting (sequential)
80 80
Model
Observed
60 60
Prevalence, (95% CI), %
Incidence, (95% CI), %
40 40
20 20
0 0
Birth 28 d 42 d 6 mo 12 mo 24 mo 28 d 42 d 6 mo 12 mo 24 mo
Age Age
C Estimated incidence of reversal (sequential)
80
60
Reversal, (95% CI), %
40
20
0
28 d 42 d 6 mo 12 mo 24 mo
Age
JAMA Network Open. 2024;7(1):e2352856. doi:10.1001/jamanetworkopen.2023.52856 (Reprinted) January 24, 2024 6/10
Downloaded from jamanetwork.com by Sabrina NM on 04/04/2024
JAMA Network Open | Pediatrics Prevalence, Incidence, and Reversal Pattern of Childhood Stunting in Ethiopia
These findings suggest that among this study population, most loss in potential linear growth
occurred during the neonatal period, and then again, after 6 months of age. An elevated burden in
malnutrition after 6 months was also documented in the 2016 Ethiopia Demographic and Health
survey (EDHS),13 and may be associated with household food insecurity, poor infant and young child
feeding practices, lack of food diversity and frequency, as well as an increased exposure to enteric
pathogens and infectious diseases.27-29 The prevalence of stunting at 2 years of age in our study was
higher than the 2016 EDHS, which found a 47.2% prevalence of stunting among children aged 0 to
59 months in the same region.15
Our stunting prevalence findings are consistent with those from the Ki Child Growth
Consortium, which combined longitudinal anthropometric data from multiple cohorts, (but did not
include data from Ethiopia) where a steady increase was observed in the prevalence of stunting until
2 years of age.11 However, in contrast with findings from the Ki Child Growth Consortium, we found
that incidence of stunting in this population did not peak during the first 3 months of life, but rather
continued to increase throughout the first 2 years of life. Stunting reversal was much higher in our
study population, particularly early in life from birth to 6 months and 12 months of age. This finding
may be reflective of the impact of various initiatives in place throughout the country to reduce
stunting, which include nutritional interventions (particularly predominant breastfeeding in the first
6 months of life), improved health care access, sanitation, and education.30 Additionally, the infancy
period is also marked by the greatest potential increment in linear growth, thereby presenting higher
likelihood of favorable interventions associated with reversal changes. However, the high prevalence
and incidence of stunting suggests that even when stunting status is reversed, a substantial number
of children relapse.
This study also found evidence of within-child heterogeneity in longitudinal length
measurements that may be due to measurement error. Challenges associated with measuring length
among newborns, infants, and toddlers have been well documented.31,32 In this study, we excluded
measurements that were not biologically plausible as defined by WHO standards. We also developed
modeled trajectories with previously validated methodologies using linear spline multilevel models
that have knots at key time points,33-35 to validate the observed prevalence, incidence and reversal
findings. Excluding outliers did not substantially alter prevalence, incidence, or reversal findings.
Observed values were slightly higher than modeled estimates, especially in the earlier ages, implying
that our observations may have overestimated the outcome, which may possibly be associated with
difficulty in measuring length in the younger ages.
Limitations
The findings of this study should be interpreted with its limitations in mind. We saw heterogeneity of
length measurements for individual children, both at the same time point and across 2 time points.
We were also limited in the number of measurements we had per child and each child contributed a
different number of observations to this analysis due to late enrollments in the non-birth cohort,
intermittently missed scheduled visits, differences in the prevalence of unscheduled health care-
seeking visits, or missing data from the pausing of data collection due to COVID-19. We also recognize
that incidence and reversal events or relapses may occur within a single, longer study time frame,
which may have been identified with shorter time windows especially in the post infancy period.
However, this study provides several important contributions to the literature. It outlines longitudinal
evidence on the burden, onset and reversal of growth faltering in Amhara, Ethiopia, the region
identified by the 2016 EDHS as having the highest burden of malnutrition in the country.13 This study
also provides evidence of linear growth at birth and during the neonatal period, where available data
are more limited.
JAMA Network Open. 2024;7(1):e2352856. doi:10.1001/jamanetworkopen.2023.52856 (Reprinted) January 24, 2024 7/10
Downloaded from jamanetwork.com by Sabrina NM on 04/04/2024
JAMA Network Open | Pediatrics Prevalence, Incidence, and Reversal Pattern of Childhood Stunting in Ethiopia
Conclusion
There is growing recognition that growth faltering is a dynamic process with the burdens of
undernutrition not limited to those that pass the threshold for stunting at a defined point in time.6
Instead, it is worth noting, that the evidence from this study suggests that this population is
chronically malnourished compared with global standards. To meet the United Nations SDGs and end
all forms of malnutrition, growth faltering in populations such as that in children younger than 2 years
in the North Shewa Zone of Amhara, Ethiopia, needs to be addressed.
ARTICLE INFORMATION
Accepted for Publication: December 3, 2023.
Published: January 24, 2024. doi:10.1001/jamanetworkopen.2023.52856
Open Access: This is an open access article distributed under the terms of the CC-BY License. © 2024 Goddard
FGB et al. JAMA Network Open.
Corresponding Author: Grace J. Chan, MD, MPH, PhD, Department of Pediatrics, Boston Children’s Hospital,
Harvard Medical School, 677 Huntington Ave, Boston, MA 02115 (grace.chan@childrens.harvard.edu).
Author Affiliations: Department of Epidemiology, Harvard T. H. Chan School of Public Health, Boston,
Massachusetts (Goddard, D. Bekele, Chan); Department of Pediatrics and Child Health, St Paul’s Hospital
Millennium Medical College, Addis Ababa, Ethiopia (Hunegnaw, Chan); Department of Biostatistics, Harvard T. H.
Chan School of Public Health, Boston, Massachusetts (Luu, Haneuse); HaSET, St Paul’s Hospital Millennium Medical
College, Addis Ababa, Ethiopia (Zeleke, Mohammed, C. Bekele, Tadesse); Maternal, Child and Adolescent health
lead executive office, Federal Ministry of Health, Ethiopia (Solomon); Department of Obstetrics and Gynecology, St
Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia (D. Bekele); Department of Pediatrics, Boston
Children’s Hospital, Harvard Medical School, Boston, Massachusetts (Chan).
Author Contributions: Dr Chan had full access to all of the data in the study and takes responsibility for the
integrity of the data and the accuracy of the data analysis. Drs Goddard and Hunegnaw contributed equally as co-
first authors.
Concept and design: Goddard, Hunegnaw, Haneuse, C. Bekele, D. Bekele, Chan.
Acquisition, analysis, or interpretation of data: Goddard, Hunegnaw, Luu, Haneuse, Zeleke Hunegnaw,
Mohammed, Tadesse, Solomon, Chan.
Drafting of the manuscript: Goddard, Hunegnaw, Luu.
Critical review of the manuscript for important intellectual content: Hunegnaw, Haneuse, Zeleke Hunegnaw,
Mohammed, C. Bekele, Tadesse, Solomon, D. Bekele, Chan.
Statistical analysis: Goddard, Luu, Haneuse, Mohammed, Chan.
Obtained funding: D. Bekele, Chan.
Administrative, technical, or material support: Hunegnaw, C. Bekele, Solomon, D. Bekele, Chan.
Supervision: Hunegnaw, Zeleke Hunegnaw, C. Bekele, Tadesse, D. Bekele, Chan.
Conflict of Interest Disclosures: None reported.
Funding/Support: This study has been supported by the Bill & Melinda Gates Foundation (Grant Nos. INV-010382
and INV-003612).
Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection,
management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and
decision to submit the manuscript for publication.
Disclaimer: Dr Haneuse is a statistical editor of JAMA Network Open, but was not involved in any of the decisions
regarding review of the manuscript or its acceptance.
Data Sharing Statement: See Supplement 2.
Additional Contributions: The authors thank all mothers and children who participated in the study; the
community of the Birhan field site; the Ministry of Health; St. Paul’s Hospital Millennium Medical College; Amhara
Regional Health Bureau, North Shewa Zone Office; Angolela Tera and Kewet and Shewa Robit Woreda Health
Offices and catchment health facilities; and the data collectors, supervisors, coordinators, and the HaSET team for
their contributions.
JAMA Network Open. 2024;7(1):e2352856. doi:10.1001/jamanetworkopen.2023.52856 (Reprinted) January 24, 2024 8/10
Downloaded from jamanetwork.com by Sabrina NM on 04/04/2024
JAMA Network Open | Pediatrics Prevalence, Incidence, and Reversal Pattern of Childhood Stunting in Ethiopia
REFERENCES
1. United Nations Department of Economic and Social Affairs. Transforming our world: the 2030 agenda for
sustainable development. October 21, 2015. Accessed December 15, 2023. https://sdgs.un.org/2030agenda
2. Nyaradi A, Li J, Hickling S, Foster J, Oddy WH. The role of nutrition in children’s neurocognitive development,
from pregnancy through childhood. Front Hum Neurosci. 2013;7:97. doi:10.3389/fnhum.2013.00097
3. Müller O, Krawinkel M. Malnutrition and health in developing countries. CMAJ. 2005;173(3):279-286. doi:10.
1503/cmaj.050342
4. Bryce J, Boschi-Pinto C, Shibuya K, Black RE; WHO Child Health Epidemiology Reference Group. WHO
estimates of the causes of death in children. Lancet. 2005;365(9465):1147-1152. doi:10.1016/S0140-6736(05)
71877-8
5. United Nations Department of Economic and Social Affairs. THE 17 GOALS | sustainable development. Accessed
December 15, 2023. https://sdgs.un.org/goals
6. Wells JCK, Briend A, Boyd EM, et al. Beyond wasted and stunted-a major shift to fight child undernutrition.
Lancet Child Adolesc Health. 2019;3(11):831-834. doi:10.1016/S2352-4642(19)30244-5
7. Grantham-McGregor S, Cheung YB, Cueto S, Glewwe P, Richter L, Strupp B; International Child Development
Steering Group. Developmental potential in the first 5 years for children in developing countries. Lancet. 2007;
369(9555):60-70. doi:10.1016/S0140-6736(07)60032-4
8. Reinhardt K, Fanzo J. Addressing chronic malnutrition through multi-sectoral, sustainable approaches: a review
of the causes and consequences. Front Nutr. 2014;1:13. doi:10.3389/fnut.2014.00013
9. UNICEF. Levels and trends in child malnutrition: key findings of the 2020 edition UNICEF, WHO, and the World
Bank Group joint child malnutrition estimates. March 2020. Accessed December 15, 2023. https://www.unicef.org/
reports/joint-child-malnutrition-estimates-levels-and-trends-child-malnutrition-2020
10. Mertens A, Benjamin-Chung J, Colford JM Jr, et al; Ki Child Growth Consortium. Child wasting and concurrent
stunting in low- and middle-income countries. [published correction appears in Nature. 2023
Nov;623(7985):E1]. Nature. 2023;621(7979):558-567. doi:10.1038/s41586-023-06480-z
11. Benjamin-Chung J, Mertens A, Colford JM Jr, et al; Ki Child Growth Consortium. Early-childhood linear growth
faltering in low- and middle-income countries. [published correction appears in Nature. 2023 Nov;623(7985):E2].
Nature. 2023;621(7979):550-557. doi:10.1038/s41586-023-06418-5
12. Akombi BJ, Agho KE, Hall JJ, Wali N, Renzaho AMN, Merom D. Stunting, wasting and underweight in
sub-Saharan Africa: a systematic review. Int J Environ Res Public Health. 2017;14(8):863. doi:10.3390/
ijerph14080863
13. Central Statistical Agency [Ethiopia]. Ethiopia demographic and health survey. 2016. Accessed December 15,
2023. https://dhsprogram.com/pubs/pdf/FR328/FR328.pdf
14. Local Burden of Disease Child Growth Failure Collaborators. Mapping child growth failure across low- and
middle-income countries. Nature. 2020;577(7789):231-234. doi:10.1038/s41586-019-1878-8
15. Hailu BA, Bogale GG, Beyene J. Spatial heterogeneity and factors influencing stunting and severe stunting
among under-5 children in Ethiopia: spatial and multilevel analysis. Sci Rep. 2020;10(1):16427. doi:10.1038/
s41598-020-73572-5
16. Ethiopian Public Health Institute. Reducing stunting in Ethiopia: “from promise to impact:” an evidence-
informed policy brief. 2019. Accessed December 15, 2023. https://ephi.gov.et/wp-content/uploads/2014/04/B-
Stunting-policy-brief-full-report-05-23-19.pdf
17. Laillou A, Baye K, Meseret Z, Darsene H, Rashid A, Chitekwe S. Wasted children and wasted time: a challenge
to meeting the nutrition sustainable development goals with a high economic impact to Ethiopia. Nutrients. 2020;
12(12):3698. doi:10.3390/nu12123698
18. World Health Organization. Global targets tracking tool. Accessed December 15, 2023. https://www.who.int/
tools/global-targets-tracking-tool
19. Munirul Islam M, Arafat Y, Connell N, et al. Severe malnutrition in infants aged <6 months-outcomes and risk
factors in Bangladesh: A prospective cohort study. Matern Child Nutr. 2019;15(1):e12642. doi:10.1111/mcn.12642
20. Chan GJ, Hunegnaw BM, Van Wickle K, et al. Birhan maternal and child health cohort: a study protocol. BMJ
Open. 2021;11(9):e049692. doi:10.1136/bmjopen-2021-049692
21. Bekele D, Hunegnaw BM, Bekele C, et al. Cohort profile: The Birhan health and demographic surveillance
system. Int J Epidemiol. 2022;51(2):e39-e45. doi:10.1093/ije/dyab225
JAMA Network Open. 2024;7(1):e2352856. doi:10.1001/jamanetworkopen.2023.52856 (Reprinted) January 24, 2024 9/10
Downloaded from jamanetwork.com by Sabrina NM on 04/04/2024
JAMA Network Open | Pediatrics Prevalence, Incidence, and Reversal Pattern of Childhood Stunting in Ethiopia
22. WHO.WHO child growth standards: length/height-for-age, weight-for-age, weight-for-length, weight-for-
height and body mass index-for-age: Methods and development. November 11, 2006. Accessed December 15,
2023. https://www.who.int/publications/i/item/924154693X
23. Villar J, Cheikh Ismail L, Victora CG, et al; International Fetal and Newborn Growth Consortium for the 21st
Century (INTERGROWTH-21st). International standards for newborn weight, length, and head circumference by
gestational age and sex: the newborn cross-sectional study of the INTERGROWTH-21st Project. Lancet. 2014;384
(9946):857-868. doi:10.1016/S0140-6736(14)60932-6
24. Villar J, Giuliani F, Bhutta ZA, et al; International Fetal and Newborn Growth Consortium for the 21(st) Century
(INTERGROWTH-21(st)). Postnatal growth standards for preterm infants: the preterm postnatal follow-up study
of the INTERGROWTH-21(st) Project. Lancet Glob Health. 2015;3(11):e681-e691. doi:10.1016/S2214-109X(15)
00163-1
25. WHO. Length velocity. Accessed January 27, 2022. https://www.who.int/tools/child-growth-standards/
standards/length-velocity
26. The R Foundation. The R project for statistical computing. Accessed December 15, 2023. https://www.r-
project.org/
27. Psaki S, Bhutta ZA, Ahmed T, et al; for MALED Network Investigators. Household food access and child
malnutrition: results from the eight-country MAL-ED study. Popul Health Metr. 2012;10(1):24. doi:10.1186/1478-
7954-10-24
28. Singh A, Singh A, Ram F. Household food insecurity and nutritional status of children and women in Nepal.
Food Nutr Bull. 2014;35(1):3-11. doi:10.1177/156482651403500101
29. Paudel R, Pradhan B, Wagle RR, Pahari DP, Onta SR. Risk factors for stunting among children: a community
based case control study in Nepal. Kathmandu Univ Med J (KUMJ). 2012;10(39):18-24.
30. Tasic H, Akseer N, Gebreyesus SH, et al. Drivers of stunting reduction in Ethiopia: a country case study. Am J
Clin Nutr. 2020;112(suppl 2):875S-893S. doi:10.1093/ajcn/nqaa163
31. Perumal N, Namaste S, Qamar H, Aimone A, Bassani DG, Roth DE. Anthropometric data quality assessment in
multisurvey studies of child growth. Am J Clin Nutr. 2020;112(suppl 2):806S-815S. doi:10.1093/ajcn/nqaa162
32. Daymont C, Ross ME, Russell Localio A, Fiks AG, Wasserman RC, Grundmeier RW. Automated identification of
implausible values in growth data from pediatric electronic health records. J Am Med Inform Assoc. 2017;24(6):
1080-1087. doi:10.1093/jamia/ocx037
33. Howe LD, Tilling K, Matijasevich A, et al. Linear spline multilevel models for summarising childhood growth
trajectories: a guide to their application using examples from five birth cohorts. Stat Methods Med Res. 2016;25
(5):1854-1874. doi:10.1177/0962280213503925
34. Grajeda LM, Ivanescu A, Saito M, et al. Modelling subject-specific childhood growth using linear mixed-effect
models with cubic regression splines. Emerg Themes Epidemiol. 2016;13(1):1. doi:10.1186/s12982-015-0038-3
35. Anderson C, Hafen R, Sofrygin O, Ryan L; members of the HBGDki Community. Comparing predictive abilities
of longitudinal child growth models. Stat Med. 2019;38(19):3555-3570. doi:10.1002/sim.7693
SUPPLEMENT 1.
eAppendix. Definitions of Low Birth Weight (LBW), Preterm Birth and Estimation of Gestational Age
eReferences
eTable 1. Number of Observations
eFigure 1. Estimated Incidence of Stunting (Common Baseline–Birth)
eFigure 2. Estimated Incidence of Reversal (Common Baseline–Birth)
SUPPLEMENT 2.
Data Sharing Statement
JAMA Network Open. 2024;7(1):e2352856. doi:10.1001/jamanetworkopen.2023.52856 (Reprinted) January 24, 2024 10/10
Downloaded from jamanetwork.com by Sabrina NM on 04/04/2024
You might also like
- Worldwide Timing of Growth Faltering: Implications For Nutritional InterventionsDocument7 pagesWorldwide Timing of Growth Faltering: Implications For Nutritional InterventionsAdebetris AmigiaNo ratings yet
- Stunting Inj Childhood An Overview of Global Burden, Trends, Determinants, and Driver of DeclinesDocument15 pagesStunting Inj Childhood An Overview of Global Burden, Trends, Determinants, and Driver of DeclinesMichimichi 78No ratings yet
- Bab 2Document15 pagesBab 2Its4peopleNo ratings yet
- Relationships Between Wasting and Stunting and Their Concurrent Occurrence in Ghanaian Preschool ChildrenDocument13 pagesRelationships Between Wasting and Stunting and Their Concurrent Occurrence in Ghanaian Preschool ChildrenRahmi DzulhijjahNo ratings yet
- Rakotomanana Et Al-2017-Maternal & Child NutritionDocument10 pagesRakotomanana Et Al-2017-Maternal & Child Nutritionsunino ninoNo ratings yet
- 08 AntrocomDocument8 pages08 AntrocombarauNo ratings yet
- Child Wasting and Concurrent Stunting in Low - and Middle-Income CountriesDocument29 pagesChild Wasting and Concurrent Stunting in Low - and Middle-Income CountriesDyah WulaningsihNo ratings yet
- OpftdDocument18 pagesOpftdgyztantika patadunganNo ratings yet
- Breastfeeding and Mortality Under 2 Years of Age in Sub-Saharan AfricaDocument11 pagesBreastfeeding and Mortality Under 2 Years of Age in Sub-Saharan AfricaMuhammad Arief SaputraNo ratings yet
- Ana Riandari (152221039) Tugas Penelitian Kebidanan 2 (Dosen Isfaizah, S.si.T.,MPH)Document12 pagesAna Riandari (152221039) Tugas Penelitian Kebidanan 2 (Dosen Isfaizah, S.si.T.,MPH)Ana RiandariNo ratings yet
- Nutrients 11 01818Document15 pagesNutrients 11 01818curly13blackNo ratings yet
- Oup-Accepted-Manuscript-2019Document10 pagesOup-Accepted-Manuscript-2019Ena EppirtaNo ratings yet
- Nigeria PDFDocument16 pagesNigeria PDFrima weniNo ratings yet
- Sema 2019Document9 pagesSema 2019Adib FraNo ratings yet
- Trends and Determinants of Stunting Among Under 5s Evidence From The 1995 2001 2006 and 2011 Uganda Demographic and Health SurveysDocument14 pagesTrends and Determinants of Stunting Among Under 5s Evidence From The 1995 2001 2006 and 2011 Uganda Demographic and Health SurveysMichimichi 78No ratings yet
- Determinants of Exclusive Breastfeeding in NigeriaDocument9 pagesDeterminants of Exclusive Breastfeeding in Nigeriainggrid28 syaputriNo ratings yet
- Case ControlDocument13 pagesCase ControlririsNo ratings yet
- Research ArticleDocument9 pagesResearch ArticleMukhammad FakhriNo ratings yet
- Determinants of Stunting and Severe Stunting Among Under-Fives: Evidence From The 2011 Nepal Demographic and Health SurveyDocument15 pagesDeterminants of Stunting and Severe Stunting Among Under-Fives: Evidence From The 2011 Nepal Demographic and Health SurveyNIRMALANo ratings yet
- Determinants of Undernutrition Among Young Children in EthiopiaDocument18 pagesDeterminants of Undernutrition Among Young Children in EthiopiaElijah IbsaNo ratings yet
- Heliyon: Ahmed Hossain, Bhupendra Niroula, Sangita Duwal, Shakil Ahmed, Md. Golam KibriaDocument6 pagesHeliyon: Ahmed Hossain, Bhupendra Niroula, Sangita Duwal, Shakil Ahmed, Md. Golam KibriaMariaCamilaPerezGuzmanNo ratings yet
- Berat Badan Lahir Bayi 2Document8 pagesBerat Badan Lahir Bayi 2Adib FraNo ratings yet
- Bulan Madu Ala IslamDocument7 pagesBulan Madu Ala IslamAsror El-RomlyNo ratings yet
- Prevalence of Contraceptive Use Among Married Women of Reproductive Age Groups in A Rural Area of BangladeshDocument7 pagesPrevalence of Contraceptive Use Among Married Women of Reproductive Age Groups in A Rural Area of BangladeshindragazaliNo ratings yet
- Effectiveness of Nutrient Mixture On The Level of Haemoglobin Among The Adolescent Girls With AnemiaDocument5 pagesEffectiveness of Nutrient Mixture On The Level of Haemoglobin Among The Adolescent Girls With AnemiaEditor IJTSRDNo ratings yet
- Ijpedi2021 5005365Document8 pagesIjpedi2021 5005365KimberlyjoycsolomonNo ratings yet
- OddoDocument8 pagesOddoariniNo ratings yet
- Stunting, Prevalence, Associated Factors, Wondo Genet, EthiopiaDocument14 pagesStunting, Prevalence, Associated Factors, Wondo Genet, EthiopiaJecko BageurNo ratings yet
- Remaja 2Document18 pagesRemaja 2rhamozaNo ratings yet
- Growth in HIV-infected Children On Long-Term Antiretroviral TherapyDocument11 pagesGrowth in HIV-infected Children On Long-Term Antiretroviral TherapyChristian Alexis Loza CorderoNo ratings yet
- Practice of Exclusive Breastfeeding and Its Associated Factors in A Suburban Area in Angola: A Cross-Sectional StudyDocument10 pagesPractice of Exclusive Breastfeeding and Its Associated Factors in A Suburban Area in Angola: A Cross-Sectional StudyfahubufezNo ratings yet
- Acta Paediatrica - 2019 - Svefors - Stunting Recovery From Stunting and Puberty Development in The MINIMat CohortDocument27 pagesActa Paediatrica - 2019 - Svefors - Stunting Recovery From Stunting and Puberty Development in The MINIMat CohortYaumil FauziahNo ratings yet
- Applied Nutritional Investigation Spatial Variation and Determinants ofDocument10 pagesApplied Nutritional Investigation Spatial Variation and Determinants ofrezky_tdNo ratings yet
- Nutritional Status and Associated Factors in Under-Five Children of RawalpindiDocument5 pagesNutritional Status and Associated Factors in Under-Five Children of RawalpindiMarya Fitri02No ratings yet
- Factors Associated With Stunting Among Children of Age 24 To 59 Months in Meskan District, Gurage Zone, South Ethiopia: A Case-Control StudyDocument7 pagesFactors Associated With Stunting Among Children of Age 24 To 59 Months in Meskan District, Gurage Zone, South Ethiopia: A Case-Control Studyfio rentiniNo ratings yet
- Socioeconomic Determinants of Child Malnutrition EDocument24 pagesSocioeconomic Determinants of Child Malnutrition Eyrgalem destaNo ratings yet
- 1 s2.0 S2214109X16303552 MainDocument9 pages1 s2.0 S2214109X16303552 MainVIRGINA PUTRINo ratings yet
- Korelasi Life Expectancy Dan StuntingfDocument10 pagesKorelasi Life Expectancy Dan StuntingfHaqqul AminNo ratings yet
- Analysis of Breastfeeding Practice, Infection Diseases and Sosiodemographic Factor With Children Linear Growth in Indralaya, Ogan IlirDocument9 pagesAnalysis of Breastfeeding Practice, Infection Diseases and Sosiodemographic Factor With Children Linear Growth in Indralaya, Ogan IlirNur SulistiyaningsihNo ratings yet
- Jurnal Gizi Klinik Indonesia: Low Birth Weight To The Incidence of Stunting in Children Aged 6-24 MonthsDocument7 pagesJurnal Gizi Klinik Indonesia: Low Birth Weight To The Incidence of Stunting in Children Aged 6-24 Monthskesekamak980No ratings yet
- Jurnal Internasional Tema 1Document15 pagesJurnal Internasional Tema 1MinartiNo ratings yet
- Determinan Faktor JurnalDocument7 pagesDeterminan Faktor Jurnalhilan sasewaNo ratings yet
- Predictors of StuntingDocument12 pagesPredictors of Stuntingrezky_tdNo ratings yet
- The Biopsychosocial Determinants of Stun 6df91c01Document14 pagesThe Biopsychosocial Determinants of Stun 6df91c01Endang PitrianiNo ratings yet
- The Stunting Syndrome in Developing Countries - CompressedDocument16 pagesThe Stunting Syndrome in Developing Countries - CompressedYumaizar FitriaNo ratings yet
- 6 Nutrisi LBNDocument7 pages6 Nutrisi LBNRizalMarubobSilalahiNo ratings yet
- Chapter IDocument51 pagesChapter IAdhish khadkaNo ratings yet
- Carmen M. Siagian and Merry Halisitijayani PDFDocument12 pagesCarmen M. Siagian and Merry Halisitijayani PDFsatra yunolaNo ratings yet
- Nutritional Status and Associated Factors in Under-Five Children of RawalpindiDocument6 pagesNutritional Status and Associated Factors in Under-Five Children of Rawalpindizahfira edwardNo ratings yet
- A Survey of Undernutrition in Children Under Three Years of Age in Rural Western ChinaDocument10 pagesA Survey of Undernutrition in Children Under Three Years of Age in Rural Western ChinaCherryNo ratings yet
- 2 PDFDocument17 pages2 PDFnoerNo ratings yet
- Prevalence and Determinants of Stunting and Overweight in 3-Year-Old Black South African Children Residing in The Central Region of Limpopo Province, South AfricaDocument8 pagesPrevalence and Determinants of Stunting and Overweight in 3-Year-Old Black South African Children Residing in The Central Region of Limpopo Province, South AfricaVina SoumokilNo ratings yet
- Jurnal Kesehatan Masyarakat: Health, Food Consumption, Social Economy, and Stunting Inci-Dency in Timor LesteDocument9 pagesJurnal Kesehatan Masyarakat: Health, Food Consumption, Social Economy, and Stunting Inci-Dency in Timor LesteYubeth LedohNo ratings yet
- JCurrMedResPract7117-1973431 052854Document5 pagesJCurrMedResPract7117-1973431 052854maudinaa_lisaNo ratings yet
- HHS Public Access: Determinants of Undernutrition and Overnutrition Among Adolescents in Developing CountriesDocument21 pagesHHS Public Access: Determinants of Undernutrition and Overnutrition Among Adolescents in Developing CountriesKhalida FauziaNo ratings yet
- Challenges in The Management of HIV 2019Document2 pagesChallenges in The Management of HIV 2019Naili Bourhane Aboudou RahimeNo ratings yet
- Nutritional Status of Infants and Some Related Risk Factors in Shahroud, IranDocument6 pagesNutritional Status of Infants and Some Related Risk Factors in Shahroud, IranGiovanni MartinNo ratings yet
- JPaediatrNursSci 3 3 73 761Document4 pagesJPaediatrNursSci 3 3 73 761vaideeswari kumarNo ratings yet
- Acta 92 168 PDFDocument12 pagesActa 92 168 PDFnah indoNo ratings yet
- Social Determinants of Health and Knowledge About Hiv/Aids Transmission Among AdolescentsFrom EverandSocial Determinants of Health and Knowledge About Hiv/Aids Transmission Among AdolescentsNo ratings yet
- Multi-Country Analysis of The Effects of Diarrhoea On Childhood StuntingDocument15 pagesMulti-Country Analysis of The Effects of Diarrhoea On Childhood StuntingSabrina NMNo ratings yet
- 2023-Non-Sequencing Based Molecular Bacterial Typing As An Affordable Tool For Outbreak Investigation in Low-Income CountriesDocument11 pages2023-Non-Sequencing Based Molecular Bacterial Typing As An Affordable Tool For Outbreak Investigation in Low-Income CountriesSabrina NMNo ratings yet
- 2020-E-Outbreak PlatformDocument7 pages2020-E-Outbreak PlatformSabrina NMNo ratings yet
- Cardiorespiratory Fitness and Physical Activity in Pediatric Diabetes - A Systematic Review and Meta AnalysisDocument15 pagesCardiorespiratory Fitness and Physical Activity in Pediatric Diabetes - A Systematic Review and Meta AnalysisSabrina NMNo ratings yet
- Modified Paq-CDocument4 pagesModified Paq-CSabrina NMNo ratings yet
- Clinic Director Operations Healthcare in Chicago IL Resume Kivaughn SheltonDocument3 pagesClinic Director Operations Healthcare in Chicago IL Resume Kivaughn SheltonKivaughnSheltonNo ratings yet
- Financial Enabling For Rural Women Via Ict - Malaysian ExperienceDocument22 pagesFinancial Enabling For Rural Women Via Ict - Malaysian ExperienceShahnaz ShahizanNo ratings yet
- 01 1 PDFDocument8 pages01 1 PDFpravikumar1989No ratings yet
- Clinical Optometry Primary Eye CareDocument3 pagesClinical Optometry Primary Eye CareDanielle SangalangNo ratings yet
- Urban Liveability in The Context of Sustainable Development: A Perspective From Coastal Region of West BengalDocument15 pagesUrban Liveability in The Context of Sustainable Development: A Perspective From Coastal Region of West BengalPremier PublishersNo ratings yet
- Patient Satisfaction With Nursing Care in An Emergency ServiceDocument10 pagesPatient Satisfaction With Nursing Care in An Emergency ServicenasimhsNo ratings yet
- Dental Negligence in Clinical PracticeDocument18 pagesDental Negligence in Clinical PracticeLutfun NessaNo ratings yet
- Swine Infectious Gastrointestinal DiseasesDocument6 pagesSwine Infectious Gastrointestinal DiseasesnessimmounirNo ratings yet
- Oxygen AdministrationDocument29 pagesOxygen Administrationjembut300100% (2)
- Libs 2804 Assignment 1 Fall 2021Document2 pagesLibs 2804 Assignment 1 Fall 2021api-537166164No ratings yet
- Certicate For CaregiversDocument3 pagesCerticate For CaregiversconsultantNo ratings yet
- Circle DietDocument171 pagesCircle DietΧΤ90% (10)
- Predicting Physiological Capacity of Human Load Carriage - A ReviewDocument10 pagesPredicting Physiological Capacity of Human Load Carriage - A ReviewlnarimotoNo ratings yet
- A Clear Label Strategy For Food AdditivesDocument6 pagesA Clear Label Strategy For Food AdditivesJerome DiazNo ratings yet
- M ChatDocument2 pagesM Chatballad3100% (2)
- Russian Current Shiva Sarari 1Document25 pagesRussian Current Shiva Sarari 1Sharma MukeshNo ratings yet
- Residents Self Assessment FormDocument5 pagesResidents Self Assessment Formapi-245673459No ratings yet
- Trigeminal NeuralgiaDocument18 pagesTrigeminal NeuralgiaKaran KohliNo ratings yet
- Unit 2 - UHVDocument65 pagesUnit 2 - UHVSrihari PuttaNo ratings yet
- Approach Considerations: Nita V Bhatt, MD, MPH Clinical Instructor, Resident Physician, Department ofDocument7 pagesApproach Considerations: Nita V Bhatt, MD, MPH Clinical Instructor, Resident Physician, Department ofHiLmy ZakiyahNo ratings yet
- Advent-Health SWOT AnalysisDocument9 pagesAdvent-Health SWOT Analysisholly100% (1)
- Resident Services DirectoryDocument121 pagesResident Services Directoryapi-349654123No ratings yet
- Gpas 2015 10 PaediatricsDocument14 pagesGpas 2015 10 PaediatricsZack TaylorNo ratings yet
- Food Related Dissertation TopicsDocument6 pagesFood Related Dissertation TopicsPaperWritingServicesLegitimateCanada100% (1)
- Relationship of Self-Regulation, Stress, and Life Satisfaction Among Middle School Students of Ekamai International School, Bangkok, ThailandDocument27 pagesRelationship of Self-Regulation, Stress, and Life Satisfaction Among Middle School Students of Ekamai International School, Bangkok, ThailandFrederick Edward FabellaNo ratings yet
- Principles of Autonomy & JusticeDocument30 pagesPrinciples of Autonomy & JusticeDr. Liza Manalo100% (1)
- Fathers' Experiences in Caring For A Young Child With Autism Spectrum DisorderDocument33 pagesFathers' Experiences in Caring For A Young Child With Autism Spectrum DisorderlauraNo ratings yet
- Health7 Q3 Module7Document18 pagesHealth7 Q3 Module7Joams artsNo ratings yet
- Psition Paper - Salupare - Ervin - DDocument2 pagesPsition Paper - Salupare - Ervin - DErvin SalupareNo ratings yet
- Activated Charcoal in Resource Poor Settings Reviewing The EvidenceDocument5 pagesActivated Charcoal in Resource Poor Settings Reviewing The EvidenceCarlos Laureano Martinez FloresNo ratings yet