Professional Documents
Culture Documents
Pipert Vanco
Pipert Vanco
Uploaded by
Yanina ZambranaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pipert Vanco
Pipert Vanco
Uploaded by
Yanina ZambranaCopyright:
Available Formats
Research
JAMA Pediatrics | Original Investigation
Association of Acute Kidney Injury With Concomitant
Vancomycin and Piperacillin/Tazobactam Treatment
Among Hospitalized Children
Kevin J. Downes, MD; Carter Cowden, MPH; Benjamin L. Laskin, MD, MS; Yuan-Shung Huang, MS; Wu Gong, MS, MPH; Matthew Bryan, PhD;
Brian T. Fisher, DO, MPH, MSCE; Stuart L. Goldstein, MD; Theoklis E. Zaoutis, MD, MSCE
Supplemental content
IMPORTANCE β-Lactam antibiotics are often coadministered with intravenous (IV)
vancomycin hydrochloride for children with suspected serious infections. For adults, the
combination of IV vancomycin plus piperacillin sodium/tazobactam sodium is associated with
a higher risk of acute kidney injury (AKI) compared with vancomycin plus 1 other β-lactam
antibiotic. However, few studies have evaluated the safety of this combination for children.
OBJECTIVE To assess the risk of AKI in children during concomitant therapy with vancomycin
and 1 antipseudomonal β-lactam antibiotic throughout the first week of hospitalization.
DESIGN, SETTING, AND PARTICIPANTS This retrospective cohort study focused on children
hospitalized for 3 or more days who received IV vancomycin plus 1 other antipseudomonal
β-lactam combination therapy at 1 of 6 large children’s hospitals from January 1, 2007,
through December 31, 2012. The study used the Pediatric Health Information System Plus
database, which contains administrative and laboratory data from 6 pediatric hospitals in the
United States. Patients with underlying kidney disease or abnormal serum creatinine levels on
hospital days 0 to 2 were among those excluded. Patients 6 months to 18 years of age who
were admitted through the emergency department of the hospital were included. Data were
collected from July 2015 to March 2016. Data analysis took place from April 2016 through
July 2017. (Exact dates are not available because the data collection and analysis processes
were iterative.)
MAIN OUTCOMES AND MEASURES The primary outcome was AKI on hospital days 3 to 7 and
within 2 days of receiving combination therapy. Acute kidney injury was defined using KDIGO
criteria and was based on changes in serum creatinine level from hospital days 0 to 2 through
hospital days 3 to 7. Multiple logistic regression was performed using a discrete-time failure
model to test the association between AKI and receipt of IV vancomycin plus
piperacillin/tazobactam or vancomycin plus 1 other antipseudomonal β-lactam antibiotic.
RESULTS A total of 1915 hospitalized children who received combination therapy were
identified. Of the 1915 patients, a total of 866 (45.2%) were female and 1049 (54.8%) were
male, 1049 (54.8%) were identified as white in race/ethnicity, and the median (interquartile
range) age was 56 (2.1-12.7) years. Among the cohort who received IV vancomycin plus 1 other
antipseudomonal β-lactam antibiotic, 157 patients (8.2%) had antibiotic-associated AKI. This
number included 117 of 1009 patients (11.7%) who received IV vancomycin plus
piperacillin/tazobactam combination therapy. After adjustment for age, intensive care unit
level of care, receipt of nephrotoxins, and hospital, IV vancomycin plus piperacillin/
tazobactam combination therapy was associated with higher odds of AKI each hospital day
compared with vancomycin plus 1 other antipseudomonal β-lactam antibiotic combination
(adjusted odds ratio, 3.40; 95% CI, 2.26-5.14).
Author Affiliations: Author
affiliations are listed at the end of this
CONCLUSIONS AND RELEVANCE Coadministration of IV vancomycin and piperacillin/ article.
tazobactam may increase the risk of AKI in hospitalized children. Pediatricians must be Corresponding Author: Kevin J.
cognizant of the potential added risk of this combination therapy when making empirical Downes, MD, Division of Infectious
antibiotic choices. Diseases, The Children’s Hospital of
Philadelphia, 2716 South St,
JAMA Pediatr. doi:10.1001/jamapediatrics.2017.3219 Ste 10360, Philadelphia, PA 19146
Published online October 2, 2017. (downeskj@email.chop.edu).
(Reprinted) E1
© 2017 American Medical Association. All rights reserved.
Downloaded From: by a UNIVERSITY OF ADELAIDE LIBRARY User on 10/13/2017
Research Original Investigation Acute Kidney Injury and Concomitant Vancomycin and Piperacillin/Tazobactam Treatment
H
ospitalized children commonly receive multiple
antibiotics.1,2 Although they are lifesaving in the set- Key Points
ting of severe infection and sepsis, some antibiotics
Question Is the combination of intravenous vancomycin
can result in acute kidney injury (AKI),3,4 which is associated hydrochloride and piperacillin sodium/tazobactam sodium
with an increased risk of chronic kidney disease and death in associated with the development of acute kidney injury in
children.5-8 Identifying antibiotic combinations with a de- children?
creased likelihood to cause AKI is important to reduce the nega-
Findings In this multicenter cohort study that included 1915
tive sequelae among children treated for suspected serious in- hospitalized children prescribed combination therapy, the
fection or sepsis. concomitant administration of intravenous vancomycin plus
Vancomycin hydrochloride and a broad-spectrum β-lactam piperacillin/tazobactam, compared with vancomycin plus other
antibiotic are often administered in combination to empiri- antipseudomonal β-lactam antibiotics, was significantly associated
cally treat children admitted with suspected serious bacterial with an increased risk of acute kidney injury.
infections. Vancomycin is the drug of choice for suspected se- Meaning Pediatricians must be cognizant of the potential added
rious gram-positive infection, and the β-lactam antibiotic pro- risk of this combination therapy when making empirical antibiotic
vides the necessary gram-negative coverage. Despite its ef- choices.
fectiveness, vancomycin has been associated with AKI in up
to 22% of children,9-13 a risk that may increase in the setting
of concurrent administration of other nephrotoxic agents.9-13 2016 through July 2017. (Exact dates are not available
Several adult studies have suggested that adding pipera- because the data collection and analysis processes were
cillin sodium/tazobactam sodium (TZP) to vancomycin in- iterative.)
creases the risk of AKI, compared with the use of vancomycin
alone or in combination with certain β-lactam antibiotics.14-20 Study Population
Limited data exist, however, on whether the combination of We identified children 6 months to 18 years of age who were
TZP and vancomycin is associated with increased nephrotox- admitted through the emergency department and were given
icity in children.21,22 Using a large administrative data set, we combination therapy, which consisted of IV vancomycin plus
assessed the risk of AKI in children who concomitantly re- 1 antipseudomonal β-lactam agent (ceftazidime sodium,
ceived intravenous (IV) vancomycin plus an antipseudo- cefepime hydrochloride, TZP, meropenem, or imipenem/
monal β-lactam antibiotic during the first week of hospital- cilastin sodium), on at least days 1 and 2 of hospitalization; ti-
ization. We hypothesized that the combination of vancomycin carcillin disodium/clavulanate potassium was not included be-
and TZP is associated with an increased risk of AKI in chil- cause it was given infrequently (n = 9) and not at each hospital.
dren. The results are immediately informative to clinicians ad- Because the first calendar day associated with a hospital ad-
ministering empirical antibiotics to children admitted with sus- mission is inherently less than 24 hours and antibiotics given
pected severe infection or sepsis. in the emergency department may differ from those admin-
istered when the child becomes an inpatient, the second cal-
endar day of an admission was considered hospital day 1. For
patients admitted more than once during the study period, only
Methods the first admission was included.
Study Design and Data Source We excluded patients who were hospitalized for fewer than
We conducted a retrospective cohort study of hospitalized chil- 3 days; had an International Classification of Diseases, Ninth
dren receiving IV vancomycin plus 1 antipseudomonal β-lactam Revision, Clinical Modification (ICD-9-CM) discharge diagno-
antibiotic at 6 large pediatric hospitals between January 1, 2007, sis code of kidney disease other than acute renal failure, in-
and December 31, 2012. These hospitals contribute adminis- cluding chronic kidney disease (580-583, 587, 590-2, 593.1,
trative and laboratory data to the Pediatric Health Informa- 593.3-5, 593.7-8; eTable 1 in the Supplement) or an ICD-9-CM
tion System Plus (PHIS+) database. The PHIS+ database incor- procedure code that may be associated with chronic kidney dis-
porates the clinical and financial data contained in the Pediatric ease (39.27, 39.42-3, 39.50, 39.53, 39.93-4, 55.52-4, 55.6; eTable
Health Information System (PHIS),23 augmented with labora- 1 in the Supplement); had an ICD-9-CM procedure code for di-
tory and radiology data of children seen in the ambulatory and alysis (39.95 or 54.98) during the first 3 days of hospitaliza-
inpatient departments of the 6 hospitals. The Children’s Hos- tion; or had an ICD-9-CM procedure code or charge for extra-
pital of Philadelphia Institutional Review Board has judged that corporeal membrane oxygenation (36.95) during the first 7 days
the PHIS+ database contains data that are not readily identi- of hospitalization. To reduce the potential for ascertainment
fiable, and thus its use exempts our study from the require- bias, the level of serum creatinine (SCr) had to be measured
ments for prospective review and approval. According to the (1) at least once during hospital days 0 to 2, (2) at least once
US Department of Health and Human Services Common Rule on hospital days 3 to 7, and (3) no fewer than every 4 days dur-
45 CFR 46 and the policies of The Children’s Hospital of Phila- ing the hospitalization, as validated in the literature.24,25
delphia institutional review board, our research did not meet
the definition of human subjects research, and thus no pa- Exposures
tient informed consent was obtained. Data were collected from For our primary analysis, we grouped patients on the basis of
July 2015 to March 2016. Data analysis took place from April the combination therapy they received: vancomycin plus TZP
E2 JAMA Pediatrics Published online October 2, 2017 (Reprinted) jamapediatrics.com
© 2017 American Medical Association. All rights reserved.
Downloaded From: by a UNIVERSITY OF ADELAIDE LIBRARY User on 10/13/2017
Acute Kidney Injury and Concomitant Vancomycin and Piperacillin/Tazobactam Treatment Original Investigation Research
or vancomycin plus an antipseudomonal β-lactam antibiotic (ICU) level of care each day based on resource utilization and
(ceftazidime, cefepime, meropenem, or imipenem/cilastin). Pa- any procedure associated with cardiovascular or respiratory
tients who received multiple β-lactam agents plus vancomy- support (vasopressors or mechanical ventilation).29 Physical
cin on hospital day 1 or 2 were excluded. Because the choice admission locations were not used. Patients were catego-
of antipseudomonal antibiotics may vary by hospital, the rized based on the ICU level of care received at any time on hos-
groups were chosen owing to the similarity in their spectrum pital days 0 to 2 or on any given hospital day.
of activity and clinical indications for the drugs they used. In Receipt of concomitant nephrotoxic medications (eTable
addition, children receiving non-antipseudomonal, as op- 2 in the Supplement) the preceding day was categorized as
posed to antipseudomonal, β-lactam agents likely differed at fewer than 2 vs 2 or more each day. Because the injurious out-
baseline in several ways, such as severity of illness, number comes of nephrotoxins may be summative, continuous neph-
of previous health care exposures, and underlying condi- rotoxin exposure, defined as receipt of multiple nephrotoxic
tions. Such differences could introduce bias in the compari- medications for more than 2 consecutive days, was also iden-
son of cases of AKI between patients receiving vancomycin plus tified. Intravenous contrast administration on the preceding
TZP and patients receiving vancomycin plus any β-lactam an- day was separately evaluated. Data on the first vancomycin
tibiotic. trough concentration for each patient on hospital day 1 or 2 were
also collected.
Outcomes
For each patient, the presence or absence of AKI was deter- Statistical Analysis
mined each day using SCr data from hospital day 0 through Baseline (hospital days 0 to 2) characteristics of patients
hospital day 7 (or discharge), whichever was sooner. The KDIGO with or without subsequent AA-AKI were compared using
(Kidney Disease: Improving Global Outcomes) criteria were the Wilcoxon rank sum test for continuous variables and the
used to define AKI26 as an increase in SCr level by 50% or higher χ2 tests for categorical variables. Baseline characteristics
from baseline or by 0.3 mg/dL or higher (to convert to micro- were also compared across the combination therapy groups.
moles per liter, multiply by 88.4) within 2 hospital days or Temporal trends in AA-AKI incidence were assessed using
fewer. The SCr level had to be 0.5 mg/dL to qualify as AKI if negative binomial regression to evaluate AA-AKI by each
the 50% change criterion was met. A SCr-based AKI defini- year of the study. Median vancomycin trough concentra-
tion was used because the PHIS+ database does not include tions were compared for the subset with available data, as
patient heights to allow for back calculation of the glomeru- were the proportions of patients in each combination
lar filtration rate; urine output was also not captured by the therapy group with a first vancomycin trough more than 15
PHIS+ database. Because laboratory data preceding admis- μg/mL and more than 20 μg/mL (to convert to micromoles
sion were unavailable, the baseline SCr level was calculated per liter, multiply by 0.690).
using the lowest SCr level on hospital days 0 to 2; the lowest We performed multiple logistic regression using a discrete-
level was chosen to allow for minor perturbations in the ini- time failure model to test the association between AA-AKI on
tial SCr level measurement secondary to dehydration, which any given hospital day and receipt of either vancomycin plus
can occur on presentation to care. TZP or vancomycin plus another 1 antipseudomonal β-lactam
The primary outcome was antibiotic-associated AKI (AA- antibiotic. Time was modeled using a day indicator. Patients
AKI), defined as AKI occurring on any of hospital days 3 to 7 contributed days to the model until the detection of AA-AKI,
and within 2 days of the last administration of vancomycin plus hospital day 7, or 2 days after the end of vancomycin plus an
an antipseudomonal β-lactam antibiotic combination therapy. antipseudomonal β-lactam agent combination therapy, which-
Given that the primary exposure required combination therapy ever occurred first. The association between covariates and AA-
on at least hospital days 1 and 2, AKI identified on hospital days AKI was first evaluated using a model adjusting for the com-
0 to 2 would, by definition, precede the exposure window. bination therapy group and for hospital day. Then, the final
Therefore, patients with AKI on hospital days 0 to 2 or a base- multivariable model was constructed, including ICU level of
line SCr level above the upper limit of published normal care, exposure to concomitant nephrotoxic medications, and
values27 for age and sex were excluded. hospital that admitted the patient a priori, along with other co-
variates if P < .20 or if inclusion resulted in a change in the point
Covariates estimate of the combination therapy group by 10% or more.
Demographic data, such as age, sex, and race, were collected We did not evaluate vancomycin trough concentrations be-
from the PHIS+ database. To account for variation in chronic cause we could not verify through the PHIS+ database the tim-
medical conditions, and identify patients with medical prob- ing of measurement of the preceding doses. To evaluate the
lems that precede hospitalization, complex chronic condi- potential influence of confounding by an unmeasured covar-
tion codes were derived using ICD-9-CM codes and dichoto- iate on the observed measure of association between the com-
mized as 0 to 1 or 2 or more. These codes have previously been bination therapy group and AA-AKI, we conducted a quanti-
used to detect the presence of a chronic condition in a hospi- tative sensitivity analysis (eAppendix in the Supplement).30,31
talized patient.28 In addition, we examined the influence of our definition of
Because patients may present to the hospital with vary- baseline SCr level by repeating the multivariable analysis in a
ing degrees of acuity of illness, data from the PHIS+ database subset of patients whose SCr level measurements on hospital
were leveraged to identify patients requiring intensive care unit days 0 to 2 were less than the median for age and sex.27
jamapediatrics.com (Reprinted) JAMA Pediatrics Published online October 2, 2017 E3
© 2017 American Medical Association. All rights reserved.
Downloaded From: by a UNIVERSITY OF ADELAIDE LIBRARY User on 10/13/2017
Research Original Investigation Acute Kidney Injury and Concomitant Vancomycin and Piperacillin/Tazobactam Treatment
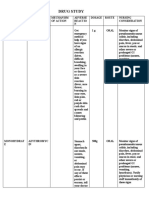
Table 1. Baseline (Hospital Days 0 to 2) Characteristics of Patients With or Without AA-AKI Who Received
Vancomycin Hydrochloride Plus 1 Antipseudomonal β-Lactam Agent
Patients, No. (%)a
Without AA-AKI With AA-AKI
Variable (n = 1758) (n = 157) P Value
Sex
Female 792 (91.5) 74 (8.6) .62
Male 966 (92.1) 83 (7.9)
Race
White 960 (91.5) 89 (8.5)
Black 144 (92.3) 12 (7.7) .88
Other, mixed race, or unknown 654 (92.1) 56 (7.9)
Ethnicity
Hispanic or Latino 143 (94.1) 9 (5.9)
.29
Not Hispanic or Latino/unknown 1615 (91.6) 148 (8.4)
Age, median (IQR), y 5.03 12.64 <.001
(1.97-11.81) (7.92-15.82)
Required ICU level of care on hospital days 0-2 497 (88.1) 67 (11.9)
<.001
Required no ICU level of care 1261 (93.3) 90 (6.7)
Had ≥2 complex or chronic conditions 932 (90.8) 95 (9.3)
.07
Had 0-1 complex or chronic conditions 826 (93.0) 62 (7.0)
Received ≥2 concomitant nephrotoxins on hospital days 0-2 319 (88.9) 40 (11.1)
.02
Received 0-1 nephrotoxin on hospital days 0-2 1439 (92.5) 117 (7.5)
Received IV contrast on hospital days 0-2 168 (87.1) 25 (13.0)
.01
Received no IV contrast 1590 (92.3) 132 (7.7)
Year of study
2007 252 (91.6) 23 (8.4)
2008 270 (93.4) 19 (6.6)
2009 267 (91.1) 26 (8.9)
.89
2010 325 (90.8) 33 (9.2)
2011 312 (92.0) 27 (8.0)
2012 332 (92.0) 29 (8.0)
PHIS hospital
1 230 (94.7) 13 (5.4) Abbreviations: AA-AKI,
antibiotic-associated acute kidney
2 541 (90.3) 58 (9.7)
injury; ICU, intensive care unit;
3 412 (90.6) 43 (9.5) IQR, interquartile range; IV,
.04
4 116 (88.6) 15 (11.5) intravenous; PHIS, Pediatric Health
Information System.
5 322 (93.6) 22 (6.4)
a
Percentages are based on the total
6 137 (95.5) 6 (4.2)
for each row.
Hospital outcomes (length of stay and in-hospital mortal- the Supplement). Of the 1915 patients, a total of 866 (45.2%) were
ity) of patients with or without AA-AKI were compared using female and 1049 (54.8%) were male, 1049 (54.8%) were identi-
the Wilcoxon rank sum test and the χ2 tests, respectively. Mul- fied as white in race/ethnicity, and the median age was 5.60 years
tiple logistic regression determined the association of AA-AKI (interquartile range [IQR], 2.12-12.65 years). In this combina-
with in-hospital mortality, adjusting for the combination tion therapy cohort, 157 patients (8.2%) developed AA-AKI within
therapy group and other baseline (hospital days 0-2) covari- the first hospital week, and 74 (47%) of these patients had
ates if P < .20 or if inclusion resulted in a change in the point KDIGO26 stage 2 AKI or higher. Table 1 displays the baseline char-
estimate of AA-AKI by 10% or more. P < .05 was considered acteristics of patients in the cohort with AA-AKI and patients in
significant, and all P values reported were 2-sided. All analy- the cohort without AA-AKI. The incidences of AA-AKI were simi-
ses were performed using Stata, version 13.1 (StataCorp LLC). lar across the years of the study, ranging from 19 (6.6%) in 2008
to 33 (9.2%) in 2010 (P = .89); no trend by study year was ob-
served (negative binomial regression P = .85). Recipients of IV
vancomycin plus a β-lactam agent who sustained AA-AKI, com-
Results pared with those who did not, were older (median age, 12.64
We identified 1915 admissions of patients who received the IV years [IQR, 7.92-15.82 years] vs 5.03 years [IQR, 1.97-11.81 years];
vancomycin plus a β-lactam agent combination therapy on at P < .001), more often required ICU level of care on hospital days
least hospital days 1 and 2 during the study period (eFigure in 0 to 2 (67/157 [42.7%] vs 497/1758 [28.3%]; P < .001), and were
E4 JAMA Pediatrics Published online October 2, 2017 (Reprinted) jamapediatrics.com
© 2017 American Medical Association. All rights reserved.
Downloaded From: by a UNIVERSITY OF ADELAIDE LIBRARY User on 10/13/2017
Acute Kidney Injury and Concomitant Vancomycin and Piperacillin/Tazobactam Treatment Original Investigation Research
Table 2. Unadjusted Frequency of AA-AKI Among Patients Who Received Combination Therapy on at Least
Hospital Days 1 and 2
Patients, No. (%)
Courses of Cumulative Incidence
Treatment of AA-AKI % Increase in SCr Level Among
β-Lactam Antibiotic (n = 1915) (n = 157) Those With AA-AKI, Median (IQR)
Piperacillin sodium/tazobactam 1009 117 (11.7) 67 (67-120)
sodium
Ceftazidime sodium 295 17 (5.8) 75 (55-200) Abbreviations: AA-AKI,
Cefepime hydrochloride 422 17 (4.0) 67 (60-120) antibiotic-associated acute kidney
injury; IQR, interquartile range;
Meropenem/imipenem 189 6 (3.2) 69 (43-133)
SCr, serum creatinine.
more often administered 2 or more nephrotoxic medications (40/ Figure. Kaplan-Meier Curves for Antibiotic-Associated Acute Kidney
157 [25.5%] vs 319/1758 [18.1%]; P = .02) or IV contrast on hos- Injury (AA-AKI)–Free Survival in Hospitalized Children
pital days 0 to 2 (25/157 [15.9%] vs 168/1758 [9.6%]; P = .01). The
AA-AKI incidences across the 6 hospitals ranged from 6 pa- 100
tients (4.2%) to 15 patients (11.5%) (P < .001).
Among recipients of any combination therapy on at least
AA-AKI–Free Survival, %
95
hospital days 1 and 2, AA-AKI was detected most often in re-
cipients of vancomycin plus TZP (117 [11.7%]; Table 2). The
90
Figure displays a Kaplan-Meier graph of AA-AKI–free sur-
vival for each combination therapy group. Baseline character- Vancomycin hydrochloride
istics of recipients of combination therapy are shown in Table 3. 85 plus 1 other antipseudomonal
β-lactam agent
The duration of combination therapy and the number of SCr
Vancomycin plus TZP
level measurements were similar among the combination
80
therapy groups. Among the subset of patients with vancomy- 0 1 2 3 4 5 6 7
cin trough concentrations available on day 1 or 2 (1177 [61.5%]), Hospital Day
No. at risk
the median initial troughs were similar between those who re- Other agents 906 906 906 906 825 536 328 219
ceived IV vancomycin plus TZP and those who received van- TZP 1009 1009 1009 1009 883 570 342 226
comycin plus 1 other antipseudomonal β-lactam agent (7.5
Combination therapy was administered to children during the first week of
μg/mL [IQR, 5.0-10.7 μg/mL] vs 7.1 μg/mL [IQR, 5.2-10.2 μg/
hospitalization. TZP indicates piperacillin sodium/tazobactam sodium.
mL]; P = .62; eTable 3 in the Supplement).
On multivariable analysis using a discrete-time failure potential for nephrotoxicity. When serious infections are sus-
model, receipt of IV vancomycin plus TZP combination therapy pected, vancomycin and a β-lactam agent are often coadmin-
was associated with increased odds of AA-AKI each hospital istered to provide appropriate empirical broad-spectrum cov-
day (adjusted odds ratio [aOR], 3.40; 95% CI, 2.26-5.14; erage until a pathogen is identified. Understanding how the
Table 4). These findings were robust for the addition of an un- nephrotoxic potential of vancomycin is altered by the choice
measured confounder to the model across a range of plau- of β-lactam agent can inform empirical antibiotic decisions that
sible clinical scenarios (eTable 4 in the Supplement). In a sen- will reduce the risk for subsequent AKI. This study demon-
sitivity analysis of patients with a baseline SCr level less than strates that AKI in children receiving vancomycin appeared to
the median SCr level for age and sex, a similar association be- be increased by coadministration of TZP compared with simi-
tween IV vancomycin plus TZP combination therapy and lar-spectrum β-lactam antibiotics. Our findings are in keep-
AA-AKI was observed (aOR, 4.14; 95% CI, 2.34-7.33). ing with several recent studies in adults.14-19
Patients who sustained AA-AKI had increased length of stay Limited pediatric data are available, but previous investi-
(median, 13 days [IQR, 6-18 days] vs 10 days [IQR, 9-26 days]; gations have suggested an association between TZP and AKI
P < .001) and increased in-hospital mortality (7 of 157 [4.5%] vs during courses of vancomycin. Knoderer and colleagues32 re-
22 of 1758 [1.3%]; P = .002), compared with patients who did ported that among children administered vancomycin for 8
not sustain AA-AKI. On multiple logistic regression analysis, days or more, a higher percentage of patients experiencing AKI
AA-AKI, ICU level of care on hospital days 0 to 2, and 2 or more received concomitant TZP (62% vs 38%), although this differ-
nephrotoxins on hospital days 0 to 2 were associated with in- ence was not significant on multivariable analyses. McQueen
creased in-hospital mortality, whereas receiving combina- and Clark21 compared the incidence of AKI between children
tion therapy was not (eTable 5 in the Supplement). who received vancomycin alone (3.8%) and children who re-
ceived vancomycin plus TZP (23.6%). This difference was sig-
nificant in bivariate analysis, but a multivariate analysis was
not conducted. To our knowledge, no pediatric studies have
Discussion described an independent association of AKI with concur-
Vancomycin is an important antibiotic for treatment of gram- rent TZP and vancomycin administration. There is a risk of con-
positive infections, but clinicians need to be cognizant of its founding by indication, but sicker patients may have been more
jamapediatrics.com (Reprinted) JAMA Pediatrics Published online October 2, 2017 E5
© 2017 American Medical Association. All rights reserved.
Downloaded From: by a UNIVERSITY OF ADELAIDE LIBRARY User on 10/13/2017
Research Original Investigation Acute Kidney Injury and Concomitant Vancomycin and Piperacillin/Tazobactam Treatment
Table 3. Characteristics of Patients Who Received Combination Therapy
Patients, No. (%)a
Vancomycin Hydrochlordie Vancomycin Plus
Plus Piperacillin Sodium/ 1 Antipseudomonal
Tazobactam Sodium β-Lactam Agent
Variable (n = 1009) (n = 906) P Value
Sex
Female 447 (44.3) 419 (46.3)
.39
Male 563 (55.7) 487 (53.8)
Race
White 568 (56.3) 481 (53.1)
Black 81 (8.0) 75 (8.3) .36
Other, mixed race, or unknown 360 (35.7) 350 (38.6)
Hispanic or Latino ethnicity 64 (6.3) 88 (9.7) .006
Age, median (IQR), y 4.42 7.07 <.001
(1.56-11.47) (2.77-13.72)
Required ICU level of care on hospital days 0-2 367 (36.4) 197 (21.7) <.001
Had ≥2 complex or chronic conditions 557 (54.2) 470 (51.9) .15
Received ≥2 concomitant nephrotoxins on hospital 225 (22.3) 134 (14.8) <.001
days 0-2
Received IV contrast on hospital days 0-2 118 (11.7) 75 (8.3) .01
PHIS hospital
1 15 (1.5) 228 (25.2)
2 384 (38.1) 215 (23.7)
3 371 (36.8) 84 (9.3) <.001
4 41 (4.1) 90 (9.9) Abbreviations: AA-AKI,
5 133 (13.2) 211 (23.3) antibiotic-associated acute kidney
injury; ICU, intensive care unit;
6 65 (6.4) 78 (8.6) IQR, interquartile range; IV,
Patients with AA-AKI 117 (11.6) 40 (4.4) <.001 intravenous; PHIS, Pediatric Health
Information System; SCr, serum
AA-AKI onset, median (IQR), d 4 (3-5) 4 (3-6) .25
creatinine.
Duration of combination therapy, median (IQR), d 4 (3-7) 4 (3-7) .69 a
Percentages are based on the total
No. of SCr level measurements on hospital days 3-7, 2 (1-4) 2 (1-3) .66 within each combination
median (IQR) therapy group.
likely to receive vancomycin plus TZP and thus were more likely tibiotics are associated with the development of other ad-
to sustain AKI. We attempted to address this by adjusting for verse events, such as Clostridium difficile infection, and anti-
differences in patient characteristics and by comparing pa- microbial resistance.
tients receiving similarly broad antibiotic coverage. Our re- The mechanism by which TZP and vancomycin cause
sults were also robust to the potential for unmeasured con- greater nephrotoxicity is unknown. Piperacillin inhibits tubu-
founding that explains the association between vancomycin lar secretion and clearance of other drugs, and an interaction
plus TZP combination therapy and AA-AKI. between piperacillin and vancomycin may contribute to toxic
The negative association of AKI with outcomes of hospi- consequences for proximal tubule cells.33,34 Rutter et al18 re-
talized children receiving vancomycin has been well ported that the incidence of AKI in adults receiving vancomy-
documented.11-13 As in our study, AKI has been associated with cin plus either TZP or cefepime increased with higher dos-
increased hospital length of stay and in-hospital mortality.11-13 ages of TZP but not of vancomycin or cefepime. This finding
Few therapeutic approaches exist to mitigate AKI secondary suggests that TZP plays an important additive or synergistic
to nephrotoxic medication exposure, aside from avoidance of role in vancomycin nephrotoxicity. However, because the
these potentially injurious agents. PHIS+ data set does not include medication dosing informa-
With limited alternatives to vancomycin for treatment of tion, we could not investigate the association between anti-
serious gram-positive infections, knowledge that concomi- biotic dosage and AKI. Future studies need to determine the
tant TZP use carries an added risk of nephrotoxicity for chil- association between vancomycin and TZP dosing and subse-
dren may help guide empirical β-lactam antibiotic selection. quent AKI in children.
When adequate substitutes to TZP exist, other broad- Higher vancomycin trough serum concentrations are as-
spectrum β-lactam antibiotics should be considered. In set- sociated with vancomycin nephrotoxicity in children.9,10,13 For
tings where TZP and vancomycin are both needed, clinicians the subset of patients with initial vancomycin trough levels
should make efforts to limit the duration of combination available in our study, trough concentrations were similar
therapy. Other β-lactam agents may less often be associated across the combination therapy groups. However, we did not
with AKI, but additional studies should evaluate how these an- incorporate trough concentrations into multivariable analy-
E6 JAMA Pediatrics Published online October 2, 2017 (Reprinted) jamapediatrics.com
© 2017 American Medical Association. All rights reserved.
Downloaded From: by a UNIVERSITY OF ADELAIDE LIBRARY User on 10/13/2017
Acute Kidney Injury and Concomitant Vancomycin and Piperacillin/Tazobactam Treatment Original Investigation Research
Table 4. Discrete-Time Failure Models of AA-AKI in Patients Who Received IV Vancomycin Hydrochloride Plus 1
Antipseudomonal β-Lactam Antibiotic
Covariate OR (95% CI)a aOR (95% CI)b
Vancomycin plus
1 other antipseudomonal β-lactam agent 1 [Reference] 1 [Reference]
Piperacillin sodium/tazobactam sodium 2.64 (1.83-3.79) 3.40 (2.26-5.14)
Female sex 1.06 (0.77-1.46)
Race
Other, mixed race, or unknown 1 [Reference]
White 1.06 (0.76-1.49)
Black 1.13 (0.60-2.13)
Hispanic or Latino ethnicity 0.77 (0.39-1.53)
Age in years 1.14 (1.12-1.17) 1.15 (1.12-1.18)
Presence of ≥2 complex or chronic conditions 1.16 (0.83-1.60)
Receipt of ≥2 concomitant nephrotoxins on hospital days 0-2 1.17 (0.81-1.70)
Receipt of ≥2 concomitant nephrotoxins on the preceding hospital day 1.12 (0.73-1.73)
Receipt of ≥2 nephrotoxins for >2 consecutive days 1.36 (0.80-2.31) 1.50 (0.87-2.16)
Receipt of IV contrast on hospital days 0-2 1.32 (0.85-2.06)
Receipt of IV contrast on the preceding hospital day 0.49 (0.12-2.00)
Requirement of ICU level of care on hospital days 0-2 1.31 (0.95-1.80)
Requirement of ICU level of care on a given day 1.42 (1.01-2.00) 1.46 (0.99-2.16)
Receipt of mechanical ventilation on a given day 1.22 (0.85-1.76)
Receipt of vasopressors on a given day 1.68 (0.98-2.88)
Year of study
2007 1 [Reference]
2008 0.71 (0.38-1.32)
2009 1.12 (0.63-1.98)
2010 1.15 (0.67-1.99) Abbreviations: AA-AKI,
2011 0.93 (0.52-1.63) antibiotic-associated acute kidney
injury; aOR, adjusted odds ratio; ICU,
2012 1.01 (0.58-1.63) intensive care unit; IV, intravenous;
PHIS hospital OR, odds ratio; PHIS, Pediatric Health
1 1 [Reference] 1 [Reference] Information System.
a
Models adjusted for combination
2 0.76 (0.39-1.45) 0.90 (0.47-1.74)
therapy group and hospital day,
3 0.59 (0.30-1.14) 0.69 (0.34-1.39) along with specific covariate being
4 1.79 (0.83-3.87) 1.88 (0.84-4.21) tested.
b
5 0.66 (0.83-3.88) 0.66 (0.31-1.34) Receipt of nephrotoxins, ICU level of
care, and PHIS hospital included in
6 0.40 (0.15-1.08) 0.40 (0.15-1.10)
the final model a priori, along with
Hospital day covariates with P < .20 or that
3 1 [Reference] 1 [Reference] caused a 10% change in the point
estimate of combination therapy
4 0.61 (0.41-0.93) 0.63 (0.41-0.98)
group. Consecutive days of
5 0.71 (0.44-1.13) 0.70 (0.43-1.14) nephrotoxin receipt were most
6 0.89 (0.53-1.50) 0.89 (0.51-1.56) strongly associated with AA-AKI
among nephrotoxin covariates and
7 0.79 (0.41-1.52) 0.76 (0.38-1.49)
were included in the final model.
ses because of the lack of information about the timing of doses emergency department and given combination therapy on
in the PHIS+ database. We do not suspect that vancomycin at least hospital days 1 and 2. Our results are not necessarily
doses or trough goals vary by β-lactam agent coadministra- generalizable to other clinical scenarios. For instance, the
tion, given that vancomycin serum trough concentrations have risk factors for AKI in patients starting antimicrobial therapy
been similar across combination therapy groups reported in later during hospitalization may be different than in
the adult literature.17,18,21 patients who are treated on admission32; such patients may
be sicker or have more comorbidities. In addition, we lim-
Limitations ited our analysis to AKI onset in the first week of hospital-
This study has several limitations. To focus on the empirical ization. The factors influencing AKI may differ in children
antibiotic decisions made on patient presentation, we with prolonged vancomycin administration, as suggested by
restricted our cohort to children admitted through the Knoderer et al.32
jamapediatrics.com (Reprinted) JAMA Pediatrics Published online October 2, 2017 E7
© 2017 American Medical Association. All rights reserved.
Downloaded From: by a UNIVERSITY OF ADELAIDE LIBRARY User on 10/13/2017
Research Original Investigation Acute Kidney Injury and Concomitant Vancomycin and Piperacillin/Tazobactam Treatment
Investigation of AKI using administrative data sets is with normal baseline kidney function and accurately cap-
challenging. Certain variables, such as vital signs and fluid tured AA-AKI on days 3 to 7 after admission.
status, are not included in the PHIS+ database. Reliance on
billing codes has low sensitivity and underestimates the
incidence of nephrotoxin-associated AKI in children.24,35 To
overcome this potential limitation, we leveraged a large
Conclusions
administrative database supplemented with laboratory data This large, multicenter study using both administrative and labo-
and applied a systematic approach to defining AKI. This ratory data found that the combination of vancomycin and TZP
method resulted in an estimated AKI incidence in our study was associated with AKI in children during the first week of hos-
that is similar to that previously reported in the pediatric lit- pitalization compared with vancomycin combined with 1 other
erature describing vancomycin nephrotoxicity. 10,36 The similar-spectrum β-lactam agent. Because of the deleterious con-
method of SCr level measurement likely differs at each of sequences of AKI, including increased length of stay and in-
the 6 hospitals in this study, but the use of an AKI definition hospital mortality, clinicians must be cognizant of the potential
based on percentage change in SCr level allows for more added risk of this combination therapy when making empirical
consistent identification of AKI cases across all hospitals. antibiotic choices. Pediatricians must limit the duration of van-
Through implementation of rigorous screening criteria, we comycin plus TZP combination therapy, as is feasible, and closely
believe that we identified a cohort of hospitalized children monitor children for whom both of these drugs are necessary.
ARTICLE INFORMATION this study) from Merck and Pfizer. Dr Fisher 7. Sutherland SM, Byrnes JJ, Kothari M, et al. AKI in
Accepted for Publication: July 27, 2017. reported receiving research support (unrelated to hospitalized children: comparing the pRIFLE, AKIN,
this study) from Pfizer, Merck, Ansun Biopharma, and KDIGO definitions. Clin J Am Soc Nephrol. 2015;
Published Online: October 2, 2017. and T2 Biosystems. Dr Zaoutis reported providing 10(4):554-561.
doi:10.1001/jamapediatrics.2017.3219 consultant services to T2 Biosystems and Nabriva 8. Akcan-Arikan A, Zappitelli M, Loftis LL,
Author Affiliations: Division of Infectious Diseases, Therapeutics. Washburn KK, Jefferson LS, Goldstein SL. Modified
The Children’s Hospital of Philadelphia, Funding/Support: Dr Laskin received support from RIFLE criteria in critically ill children with acute
Philadelphia, Pennsylvania (Downes, Fisher, the National Institute of Diabetes and Digestive and kidney injury. Kidney Int. 2007;71(10):1028-1035.
Zaoutis); Center for Pediatric Clinical Effectiveness, Kidney Diseases (grant K23-DK101600).
The Children’s Hospital of Philadelphia, 9. McKamy S, Hernandez E, Jahng M, Moriwaki T,
Philadelphia, Pennsylvania (Downes, Cowden, Role of the Funder/Sponsor: The funder had no Deveikis A, Le J. Incidence and risk factors
Fisher, Zaoutis); The Pediatric Infectious Diseases role in the design and conduct of the study; influencing the development of vancomycin
Epidemiology and Antimicrobial Stewardship collection, management, analysis, and nephrotoxicity in children. J Pediatr. 2011;158(3):
Research Group, The Children’s Hospital of interpretation of the data; preparation, review, or 422-426.
Philadelphia, Philadelphia, Pennsylvania (Downes, approval of the manuscript; and decision to submit 10. Le J, Ny P, Capparelli E, et al. Pharmacodynamic
Cowden, Fisher, Zaoutis); Department of Pediatrics, the manuscript for publication. characteristics of nephrotoxicity associated with
Perelman School of Medicine, University of Additional Contributions: Kelly Getz, PhD, MPH, vancomycin use in children. J Pediatric Infect Dis Soc.
Pennsylvania, Philadelphia (Downes, Laskin, Fisher, Children’s Hospital of Philadelphia, assisted with 2015;4(4):e109-e116.
Zaoutis); Division of Nephrology, The Children’s bias analysis. Dr Getz received no compensation for 11. Totapally BR, Machado J, Lee H, Paredes A,
Hospital of Philadelphia, Philadelphia, Pennsylvania her contribution. Raszynski A. Acute kidney injury during vancomycin
(Laskin); Healthcare Analytics Unit, The Children’s therapy in critically ill children. Pharmacotherapy.
Hospital of Philadelphia, Philadelphia, Pennsylvania REFERENCES 2013;33(6):598-602.
(Huang, Gong); Department of Biostatistics and 1. Lasky T, Ernst FR, Greenspan J, Wang S, Gonzalez
Epidemiology, Perelman School of Medicine, 12. Seixas GT, Araujo OR, Silva DC, Arduini RG,
L. Estimating pediatric inpatient medication use in Petrilli AS. Vancomycin therapeutic targets and
University of Pennsylvania, Philadelphia (Bryan, the United States. Pharmacoepidemiol Drug Saf.
Fisher, Zaoutis); Division of Nephrology and nephrotoxicity in critically ill children with cancer.
2011;20(1):76-82. J Pediatr Hematol Oncol. 2016;38(2):e56-e62.
Hypertension, Cincinnati Children’s Hospital
Medical Center, Cincinnati, Ohio (Goldstein); 2. Feudtner C, Dai D, Faerber J, Metjian TA, Luan X. 13. Knoderer CA, Nichols KR, Lyon KC, Veverka
Department of Pediatrics, University of Cincinnati Pragmatic estimates of the proportion of pediatric MM, Wilson AC. Are elevated vancomycin serum
College of Medicine, Cincinnati, Ohio (Goldstein). inpatients exposed to specific medications in the trough concentrations achieved within the first 7
USA. Pharmacoepidemiol Drug Saf. 2013;22(8): days of therapy associated with acute kidney injury
Author Contributions: Dr Downes had full access 890-898.
to all of the data in the study and takes in children? J Pediatric Infect Dis Soc. 2014;3(2):127-
responsibility for the integrity of the data and the 3. Pannu N, Nadim MK. An overview of 131.
accuracy of the data analysis. drug-induced acute kidney injury. Crit Care Med. 14. Burgess LD, Drew RH. Comparison of the
Study concept and design: Downes, Laskin, Fisher, 2008;36(4 suppl):S216-S223. incidence of vancomycin-induced nephrotoxicity in
Goldstein, Zaoutis. 4. Patzer L. Nephrotoxicity as a cause of acute hospitalized patients with and without concomitant
Acquisition, analysis, or interpretation of data: All kidney injury in children. Pediatr Nephrol. 2008;23 piperacillin-tazobactam. Pharmacotherapy.
authors. (12):2159-2173. 2014;34(7):670-676.
Drafting of the manuscript: Downes. 5. Menon S, Kirkendall ES, Nguyen H, Goldstein SL. 15. Kim T, Kandiah S, Patel M, et al. Risk factors for
Critical revision of the manuscript for important Acute kidney injury associated with high kidney injury during vancomycin and
intellectual content: Downes, Cowden, Gong, nephrotoxic medication exposure leads to chronic piperacillin/tazobactam administration, including
Laskin, Huang, Bryan, Fisher, Goldstein, Zaoutis. kidney disease after 6 months. J Pediatr. 2014; increased odds of injury with combination therapy.
Statistical analysis: Downes, Cowden, Gong, Bryan. 165(3):522-527. BMC Res Notes. 2015;8:579-589.
Administrative, technical, or material support:
Downes, Cowden, Laskin, Huang. 6. Alkandari O, Eddington KA, Hyder A, et al. Acute 16. Fodero KE, Horey AL, Krajewski MP, Ruh CA,
Study supervision: Downes, Laskin, Fisher, kidney injury is an independent risk factor for Sellick JA Jr, Mergenhagen KA. Impact of an
Goldstein, Zaoutis. pediatric intensive care unit mortality, longer length antimicrobial stewardship program on patient
of stay and prolonged mechanical ventilation in safety in veterans prescribed vancomycin. Clin Ther.
Conflict of Interest Disclosures: Dr Downes critically ill children: a two-center retrospective 2016;38(3):494-502.
reported receiving research support (unrelated to cohort study. Crit Care. 2011;15(3):R146.
E8 JAMA Pediatrics Published online October 2, 2017 (Reprinted) jamapediatrics.com
© 2017 American Medical Association. All rights reserved.
Downloaded From: by a UNIVERSITY OF ADELAIDE LIBRARY User on 10/13/2017
Acute Kidney Injury and Concomitant Vancomycin and Piperacillin/Tazobactam Treatment Original Investigation Research
17. Navalkele B, Pogue JM, Karino S, et al. Risk of variation in pediatric surgery: implications for the 30. Lash TL, Fox MP, Fink AK. Applying
acute kidney injury in patients on concomitant prioritization of comparative effectiveness Quantitative Bias Analysis to Epidemiologic Data. New
vancomycin and piperacillin-tazobactam compared research. JAMA Pediatr. 2017;171(2):e163926. York, NY: Springer; 2009.
to those on vancomycin and cefepime. Clin Infect Dis. 24. Schaffzin JK, Dodd CN, Nguyen H, 31. Lash TL, Fox MP, MacLehose RF, Maldonado G,
2017;64(2):116-123. Schondelmeyer A, Campanella S, Goldstein SL. McCandless LC, Greenland S. Good practices for
18. Rutter WC, Cox JN, Martin CA, Burgess DR, Administrative data misclassifies and fails to quantitative bias analysis. Int J Epidemiol. 2014;43
Burgess DS. Nephrotoxicity during vancomycin identify nephrotoxin-associated acute kidney injury (6):1969-1985.
therapy in combination with piperacillin- in hospitalized children. Hosp Pediatr. 2014;4(3): 32. Knoderer CA, Gritzman AL, Nichols KR, Wilson
tazobactam or cefepime. Antimicrob Agents 159-166. AC. Late-occurring vancomycin-associated acute
Chemother. 2017;61(2):e02089-16. 25. Moffett BS, Goldstein SL. Acute kidney injury kidney injury in children receiving prolonged
19. Gomes DM, Smotherman C, Birch A, et al. and increasing nephrotoxic-medication exposure in therapy. Ann Pharmacother. 2015;49(10):1113-1119.
Comparison of acute kidney injury during treatment noncritically-ill children. Clin J Am Soc Nephrol. 2011; 33. Najjar TA, Abou-Auda HS, Ghilzai NM. Influence
with vancomycin in combination with 6(4):856-863. of piperacillin on the pharmacokinetics of
piperacillin-tazobactam or cefepime. 26. Kidney International Supplements. Kidney methotrexate and 7-hydroxymethotrexate. Cancer
Pharmacotherapy. 2014;34(7):662-669. Disease: Improving Global Outcomes (KDIGO). Chemother Pharmacol. 1998;42(5):423-428.
20. Hammond DA, Smith MN, Li C, Hayes SM, KDIGO clinical practice guideline for acute kidney 34. Landersdorfer CB, Kirkpatrick CM, Kinzig M,
Lusardi K, Bookstaver PB. Systematic review and injury. http://www.kdigo.org/clinical_practice Bulitta JB, Holzgrabe U, Sörgel F. Inhibition of
meta-analysis of acute kidney injury associated _guidelines/pdf/KDIGO%20AKI%20Guideline.pdf. flucloxacillin tubular renal secretion by piperacillin.
with concomitant vancomycin and Published March 2012. Accessed May 11, 2012. Br J Clin Pharmacol. 2008;66(5):648-659.
piperacillin/tazobactam. Clin Infect Dis. 2017;64(5): 27. Pottel H, Vrydags N, Mahieu B, Vandewynckele
666-674. 35. Grams ME, Waikar SS, MacMahon B, Whelton S,
E, Croes K, Martens F. Establishing age/sex related Ballew SH, Coresh J. Performance and limitations of
21. McQueen KE, Clark DW. Does combination serum creatinine reference intervals from hospital administrative data in the identification of AKI. Clin
therapy with vancomycin and piperacillin- laboratory data based on different statistical J Am Soc Nephrol. 2014;9(4):682-689.
tazobactam increase the risk of nephrotoxicity methods. Clin Chim Acta. 2008;396(1-2):49-55.
versus vancomycin alone in pediatric patients? 36. Cies JJ, Shankar V. Nephrotoxicity in patients
28. Feudtner C, Hays RM, Haynes G, Geyer JR, Neff with vancomycin trough concentrations of 15-20
J Pediatr Pharmacol Ther. 2016;21(4):332-338. JM, Koepsell TD. Deaths attributed to pediatric μg/ml in a pediatric intensive care unit.
22. LeCleir LK, Pettit RS. Piperacillin-tazobactam complex chronic conditions: national trends and Pharmacotherapy. 2013;33(4):392-400.
versus cefepime incidence of acute kidney injury in implications for supportive care services. Pediatrics.
combination with vancomycin and tobramycin in 2001;107(6):E99.
pediatric cystic fibrosis patients. Pediatr Pulmonol. 29. Maude SL, Fitzgerald JC, Fisher BT, et al.
2017;52(8):1000-1005. Outcome of pediatric acute myeloid leukemia
23. Cameron DB, Graham DA, Milliren CE, et al. patients receiving intensive care in the United
Quantifying the burden of interhospital cost States. Pediatr Crit Care Med. 2014;15(2):112-120.
jamapediatrics.com (Reprinted) JAMA Pediatrics Published online October 2, 2017 E9
© 2017 American Medical Association. All rights reserved.
Downloaded From: by a UNIVERSITY OF ADELAIDE LIBRARY User on 10/13/2017
You might also like
- Protocols For Drug Allergy DesensitizationDocument40 pagesProtocols For Drug Allergy DesensitizationTimothy j. Sullivan, III, MD77% (13)
- Zosyn (Piperacillin/tazobactram)Document2 pagesZosyn (Piperacillin/tazobactram)E67% (3)
- Nephrotoxicity From Vancomycin Combined With Piperacillin-Tazobactam: A Comprehensive ReviewDocument13 pagesNephrotoxicity From Vancomycin Combined With Piperacillin-Tazobactam: A Comprehensive ReviewArturo ArturoNo ratings yet
- 2019 Vancomycin Associated Nephrotoxicity and Risk Factors in Critically III Children Whitout Preexisting Renal InjuryDocument5 pages2019 Vancomycin Associated Nephrotoxicity and Risk Factors in Critically III Children Whitout Preexisting Renal InjuryJeff Daniel Landauro PanayNo ratings yet
- Hammond 2016Document9 pagesHammond 2016RaffaharianggaraNo ratings yet
- Blum Er 2016Document7 pagesBlum Er 2016Vinsensius Rubin Ferreri ArismarjiantoNo ratings yet
- Blood Culture With CAPDocument10 pagesBlood Culture With CAPKaye Antonette AntioquiaNo ratings yet
- Schaefer 2017Document6 pagesSchaefer 2017hasemana hasemanaNo ratings yet
- Hoa 3Document9 pagesHoa 3ruth angelinaNo ratings yet
- 204 FullDocument10 pages204 FullJose Carlos Soto SaenzNo ratings yet
- Nac y AntibióticosDocument7 pagesNac y AntibióticosRoberto MorenoNo ratings yet
- E20161692 FullDocument11 pagesE20161692 FullWiti Triple'sNo ratings yet
- With Pneumonia Narrow Vs Broad-Spectrum Antimicrobial Therapy For Children HospitalizedDocument10 pagesWith Pneumonia Narrow Vs Broad-Spectrum Antimicrobial Therapy For Children HospitalizedanettepardedeNo ratings yet
- Journal 3Document11 pagesJournal 3margareth silaenNo ratings yet
- Leeyenaar DKK 2014Document14 pagesLeeyenaar DKK 2014Devanti EkaNo ratings yet
- The Safety of Acetaminophen and Ibuprofen Among Children Younger Than Two Years OldDocument7 pagesThe Safety of Acetaminophen and Ibuprofen Among Children Younger Than Two Years OldsastiraNo ratings yet
- CEP Fluconazole Prophylaxis For Prevention of Invasive Candidiasis in Extremely Preterm InfantsDocument2 pagesCEP Fluconazole Prophylaxis For Prevention of Invasive Candidiasis in Extremely Preterm InfantsElison J PanggaloNo ratings yet
- Jurnal Inggris TugasDocument10 pagesJurnal Inggris TugasManusia biasaNo ratings yet
- Early Use of Antibiotics Is Associated With A Lower Incidence of Necrotizing EnterocolitisDocument9 pagesEarly Use of Antibiotics Is Associated With A Lower Incidence of Necrotizing EnterocolitisRestu TriwulandaniNo ratings yet
- Metaanálisis VancoDocument26 pagesMetaanálisis VancoYanina ZambranaNo ratings yet
- Keac 372Document12 pagesKeac 372Abi ArifiNo ratings yet
- Objective Study Design: M P, MD, S B. K, MD, K L. A, P D, H S. B, MDDocument6 pagesObjective Study Design: M P, MD, S B. K, MD, K L. A, P D, H S. B, MDSY LodhiNo ratings yet
- Pneumonia in Infants and ChildrenDocument52 pagesPneumonia in Infants and ChildrenMikeyNo ratings yet
- 2 PDFDocument10 pages2 PDFkemalmiaNo ratings yet
- Acellular Pertussis Vaccine Effectiveness Over Time: ObjectivesDocument11 pagesAcellular Pertussis Vaccine Effectiveness Over Time: ObjectivesLee제노No ratings yet
- Van Puffelen 2018 Oi 180133Document11 pagesVan Puffelen 2018 Oi 180133Bunga Nur AnnisaNo ratings yet
- Ventilator-Associated PneumoniDocument15 pagesVentilator-Associated PneumoniYasminNo ratings yet
- Cir 531Document52 pagesCir 531Ana Maria Muñoz GonzalezNo ratings yet
- Acellular Pertussis Vaccine Effectiveness Over Time: ObjectivesDocument11 pagesAcellular Pertussis Vaccine Effectiveness Over Time: Objectives[JC]No ratings yet
- Well-Child Care Attendance and Risk of Asthma ExacerbationsDocument11 pagesWell-Child Care Attendance and Risk of Asthma ExacerbationsFC Mekar AbadiNo ratings yet
- Peds Pneumnoaie GuidlinesDocument56 pagesPeds Pneumnoaie GuidlinesDorji InternationalNo ratings yet
- Karsies Et Al 2014Document7 pagesKarsies Et Al 2014Quỳnh Nguyễn Thị NhưNo ratings yet
- Idsa NacDocument56 pagesIdsa NacAndresNo ratings yet
- 2011 Ispad NeumoníaDocument14 pages2011 Ispad NeumoníaAaron Nureña JaraNo ratings yet
- Refluks VuDocument10 pagesRefluks Vuwilliam sitnerNo ratings yet
- E794 FullDocument10 pagesE794 FullMaria Camila Ramírez GutiérrezNo ratings yet
- CAP in Children - IDSADocument52 pagesCAP in Children - IDSAlala liliNo ratings yet
- Vancomycin-Associated Acute Kidney Injury A Narrative Review From Pathophysiology To Clinical ApplicatioDocument14 pagesVancomycin-Associated Acute Kidney Injury A Narrative Review From Pathophysiology To Clinical ApplicatioZiRong TsengNo ratings yet
- Varicella Post-ProphylaxisDocument2 pagesVaricella Post-ProphylaxisAngelaTrinidadNo ratings yet
- 1688 FullDocument9 pages1688 FullAnonymous pYR4s37H6No ratings yet
- Luther 2017Document9 pagesLuther 2017Arturo ArturoNo ratings yet
- 431 2021 Article 4025Document9 pages431 2021 Article 4025Johan Wijaya KesitNo ratings yet
- Outcomes of Single-Dose Empirical Antibiotic Treatment in Children With Suspected Sepsis Implemented in The Emergency DepartmentDocument5 pagesOutcomes of Single-Dose Empirical Antibiotic Treatment in Children With Suspected Sepsis Implemented in The Emergency Departmentaldo saadot garcia ortizNo ratings yet
- Cir 531Document52 pagesCir 531Mario CornejoNo ratings yet
- Postvaccination Febrile Seizure Severity and OutcomeDocument11 pagesPostvaccination Febrile Seizure Severity and OutcomeGrace Malinda LimopranotoNo ratings yet
- challengesInTheDesignThea 1Document6 pageschallengesInTheDesignThea 1Zolla Verbianti SuwitaNo ratings yet
- Pediatrics 2015 Irwin 635 42Document10 pagesPediatrics 2015 Irwin 635 42Arif Pasti BisaNo ratings yet
- HHS Public AccessDocument21 pagesHHS Public AccessA AnonimyNo ratings yet
- Cir 531Document52 pagesCir 531Nubia PuNo ratings yet
- Early Evaluation of The Safety, Reactogenicity, AnDocument9 pagesEarly Evaluation of The Safety, Reactogenicity, An8px64mznmdNo ratings yet
- Can Tey 2015Document4 pagesCan Tey 2015irenesmbNo ratings yet
- NAC en NiñosDocument14 pagesNAC en NiñosAnonymous DxJyWJwtNo ratings yet
- Tamma Et Al., 2015Document7 pagesTamma Et Al., 2015Caio Bonfim MottaNo ratings yet
- ProbiotikDocument9 pagesProbiotikmasitah nasutionNo ratings yet
- Cap 2023Document9 pagesCap 2023Neonatología HGO4No ratings yet
- Piis0025619619305737 220530 065558Document11 pagesPiis0025619619305737 220530 065558Garcia Yepez Stephanie GraceNo ratings yet
- Does Nephrotoxicity Develop Less Frequently When Vancomycin Is Combined With Imipenem-Cilastatin Than With Meropenem? A Comparative StudyDocument8 pagesDoes Nephrotoxicity Develop Less Frequently When Vancomycin Is Combined With Imipenem-Cilastatin Than With Meropenem? A Comparative StudyAsma BahriNo ratings yet
- Childhood Nephrotic Syndrome: Steroid Sensitive, Steroid Resistant and BeyondDocument7 pagesChildhood Nephrotic Syndrome: Steroid Sensitive, Steroid Resistant and BeyondDorin Cristian AntalNo ratings yet
- Pneumonia GuidelinesDocument14 pagesPneumonia GuidelinesWilber Martin BaltodanoNo ratings yet
- Jurnal 1Document7 pagesJurnal 1Deski MadeNo ratings yet
- Adverse Events After Routine Immunization of Extremely Low-Birth-Weight Infants - DeMeo Et - AlDocument6 pagesAdverse Events After Routine Immunization of Extremely Low-Birth-Weight Infants - DeMeo Et - AlSY LodhiNo ratings yet
- Food Protein Induced Enterocolitis (FPIES): Diagnosis and ManagementFrom EverandFood Protein Induced Enterocolitis (FPIES): Diagnosis and ManagementTerri Faye Brown-WhitehornNo ratings yet
- DUE of PIPERACILLIN and TazobactumDocument73 pagesDUE of PIPERACILLIN and Tazobactumanup jagarlamudiNo ratings yet
- Name: - Competency Appraisal 2Document2 pagesName: - Competency Appraisal 2Matt Joseph CabantingNo ratings yet
- PiperacillinDocument3 pagesPiperacillinNicholas TagleNo ratings yet
- Zosyn Drug StudyDocument2 pagesZosyn Drug StudyAnalyn SarmientoNo ratings yet
- Antibiotic IV Administration During COVID-19Document5 pagesAntibiotic IV Administration During COVID-19David Hines LopezNo ratings yet
- Prolonged Infusions of Beta-Lactam AntibioticsDocument23 pagesProlonged Infusions of Beta-Lactam AntibioticsNhanLiNo ratings yet
- SHC Obesity Dosing GuideDocument10 pagesSHC Obesity Dosing GuideAnonymous 9dVZCnTXSNo ratings yet
- Go Piperacillin-TazobactamDocument4 pagesGo Piperacillin-TazobactamSAMANTHA T. MODESTONo ratings yet
- Zosyn Drug CardDocument1 pageZosyn Drug CardSheri490No ratings yet
- M E T H O D TEACHING PLAN Student: - Cassie WilliamsDocument4 pagesM E T H O D TEACHING PLAN Student: - Cassie WilliamsCassandra100% (1)
- PiperacillinDocument3 pagesPiperacillinMario Magtaka0% (1)
- Piperacillin+Tazobactam - TAZOCIN 4.5 G - Leaflet - PfizerDocument12 pagesPiperacillin+Tazobactam - TAZOCIN 4.5 G - Leaflet - PfizerTiaraNo ratings yet
- DS PiptazDocument1 pageDS PiptazCristel Z. GabucoNo ratings yet
- Cefepime Vs Zosyn For Empiric Sepsis CoverageDocument2 pagesCefepime Vs Zosyn For Empiric Sepsis Coveragetl drNo ratings yet
- Kee: Pharmacology, 6th Edition: Test Bank Chapter 4: Medications and Calculations Short AnswerDocument39 pagesKee: Pharmacology, 6th Edition: Test Bank Chapter 4: Medications and Calculations Short Answerthu_vu_2983% (6)
- Piptaz DSDocument4 pagesPiptaz DSArone SebastianNo ratings yet
- Drug Study Format and SampleDocument6 pagesDrug Study Format and SampleA.No ratings yet
- Piperacillin Tazobactam Drug StudyDocument5 pagesPiperacillin Tazobactam Drug StudyKathlene Boleche100% (2)
- Western Mindanao State University College of Nursing: Zamboanga CityDocument11 pagesWestern Mindanao State University College of Nursing: Zamboanga CitySHAINA ALIH. JUMAANINo ratings yet
- Weekly Nursing Care Plan 4Document13 pagesWeekly Nursing Care Plan 4api-673227957No ratings yet
- Drug Study - PiptazDocument1 pageDrug Study - PiptazMutya XDNo ratings yet
- PiptazDocument3 pagesPiptazArone SebastianNo ratings yet
- Drug Study HazDocument7 pagesDrug Study HazRichard HazNo ratings yet