Professional Documents
Culture Documents
Trisomy 18 With Multiple Congenital Anomalies A Rare Case Report-3
Uploaded by
Elna Esther0 ratings0% found this document useful (0 votes)
5 views4 pagesOriginal Title
Trisomy+18+With+Multiple+Congenital+Anomalies+A+Rare+Case+Report-3
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
5 views4 pagesTrisomy 18 With Multiple Congenital Anomalies A Rare Case Report-3
Uploaded by
Elna EstherCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 4
DOI: http://10.5281/zenodo.
6857977 JCTEI
JOURNAL OF CLINICAL TRIALS AND EXPERIMENTAL INVESTIGATIONS CASE REPORT
Trisomy 18 With Multiple Congenital
Anomalies: A Rare Case Report
Hande Gizem Özalp1
1Dicle University Faculty of Medicine, Department of Pediatrics, Diyarbakır, Turkey.
Abstract
The most common congenital anomalies, autosomal aneuploidies are
linked to a variety of metabolic diseases, hormone imbalances,
neurotransmitter abnormalities, and intellectual difficulties.
Chromosomal segregation mistakes that occur during cell division are
what cause trisomies. A number of studies have revealed that numerous
Correspondence: disrupted cellular processes are linked to uncontrolled gene expression
brought on by the triplication of chromosomes 13 and 18. Furthermore,
Özalp H.G. Dicle
University Faculty of Medicine, the occurrence of embryonic abnormalities may be linked to a disrupted
Department of Pediatrics, oxidative stress condition. These chromosomal aberrations generate
Diyarbakır, Turkey.
many congenital abnormalities such as heart defects, gastrointestinal
e-mail: defects, tracheoesophageal abnormalities, endocrine disorders, vision,
hande9193@hotmail.com and hearing disorders, and limb and nervous system anomalies.
However, there are many theories and mechanisms regarding this issue.
In this study, we aimed to present a case with multiple congenital
Specialty section:
anomalies born from a 38-year-old mother.
This article was submitted to
Pediatrics section
Keywords: Trisomy 18, Congenital anomalies, Genetic
Received: 12 June 2022
Revised: 27 June 2022
Accepted: 8 July 2022
Published: 20 July 2022 Introduction
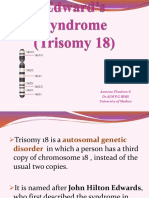
Trisomy 18 (Edward's) syndrome; is one of the most common
Copyright© 2022 Published chromosomal disorders 3 times more frequently in girls and is another
by The JCTEI. frequent autosomal aneuploidy after Trisomy 21 (T21), affecting 1/6000 to
1/8000 live-birth fetuses. [1,2]. Trisomy 18 syndrome was first described
in 1960 by Edwards, and genetic and environmental factors such as
maternal and paternal germ cell dissociation and advanced maternal age
are blamed [3-5].
T18 occurs most frequently as a result of a complete 18 trisomy
due to a maternal meiotic nondisjunction, which is the most common form
(94%) [6]. Mosaic trisomy 18 is the second cause corresponding to fewer
than 5% of occurrences, and fewer than 2% of cases are caused by an
28 JCTEI YEAR: 2022 VOLUME: 1 ISSUE: 1
additional copy of long arm chromosome 18q The patient had micrognathia (fig.1),
[7]. These chromosomal aberrations generate microphthalmia (fig.1), short mane neck, low
many congenital abnormalities such as heart ear appearance (fig.2), and left ankle was in
defects, gastrointestinal defects, extreme flexion posture (clubfoot, fig.3).
tracheoesophageal abnormalities, endocrine Detailed examination of the patient revealed
disorders, vision and hearing disorders, and an artery and a vein in the umbilical cord, left
limb and nervous system anomalies [8-10]. choanal stenosis, bilateral clenched hand
Following the complexity of existing (fig.4), and unilateral undescended testis.
comorbidities, numerical chromosomal
aberration, such as T13 and T18 are one of the
main causes of miscarriage or stillbirth [11].
However, along with improvements in clinical
management, an increased survival rate of
patients with these syndromes has been
reported [12, 13].
In this study, we aimed to present a case with
multiple congenital anomalies born from a 38-
year-old mother.
Figure 2: Short Neck and Low Ear Appearance
Case Description
A male baby born at the 33rd week of
pregnancy weighing 1850 g was intubated in A chest X-ray was taken to the patient.
the delivery room due to his poor general The radiogram was compatible with RDS. The
condition and inability to maintain his patient was treated with 1 dose of surfactant.
saturations and was admitted to our intensive And 6 hours later, the surfactant was applied
care unit with the diagnosis of neonatal again. Antimicrobial therapy was started in the
respiratory distress, prematurity, and a patient who could not differentiate between
dysmorphic baby. The patient was the 5th child RDS and congenital pneumonia.
born by cesarean section from the 6th
In the laboratory findings of the
pregnancy of a 38-year-old mother with
patient, urea: 33.6 mg/dL and creatinine: 1,03
polyhydramnios.
mg/dL. Hypocalcemia was also detected. Left
kidney could not be observed in abdominal
ultrasonography (USG) (hypoplasia). One cyst
was observed in the hepatic intrahepatic bile
ducts, not clinically significant. Asymmetrical
dilatation in the 3rd ventricle was observed in
the transfontanelle USG (Hydrocephaly?).
Positive inotropic therapy was initiated
in the patient with circulatory disorder and
cyanosis. Echocardiography revealed a double
outlet right ventricle, large Ventricular septal
defect (VSD) (subaortic), patent ductus
Figure 1: Micrognathia and Microphthalmia arteriosus (PDA), and Secundum Atrial Septal
Defect (ASD).
29 JCTEI YEAR: 2022 VOLUME: 1 ISSUE: 1
newborns with trisomy 18 were included in the
cohort of Embleton et al. Of these, an
echocardiography or post-mortem testing was
revealed [16]. Our patient was also on
mechanical ventilator support and despite
receiving 2 doses of surfactant and
antimicrobial therapy, he could not maintain
his saturation. According to the
echocardiography, double outlet right
ventricle, wide VSD, PDA, and ASD were
observed in this patient.
Figure 3: Clubfoot In the etiology of trisomy 18, increased
maternal age and faulty chromosome
distribution are the most important factors
The patient, who was followed up with [3,17]. All cases with trisomy 18 syndrome have
the diagnosis of dysmorphic baby, underwent low birth weight, characteristic facial
an eye examination. The diagnoses of right appearance, and cardiac anomaly. In addition
optic disc coloboma and Morning Plory to these findings, there are also those with
Syndrome were suspected, but a clear extremity deformity and renal anomalies [18].
diagnosis was not made. In our case, we mentioned a case with
micrognathia, microphthalmia, low ear, mane
The patient's TORCH tests were neck appearance, clubfoot deformity of the left
unremarkable. A diagnosis of trisomy 18 was foot, and bilateral clenched hand. The mother
made by performing chromosomal analysis in of our baby, who was born 1850 grams, was 38
peripheral blood. years old.
Their mortality is due to sepsis, nutritional
disorders, renal failure, and apnea due to
cardiac anomalies [19]. When monitoring this
patient with a trisomy 18 diagnosis, we have
taken into account cardiac abnormal status,
renal failure, and other grave health issues.
Trisomy 18 is a syndrome accompanied by
multiple congenital anomalies and its definitive
diagnosis is made by chromosome analysis
[11]. We performed a genetic analysis as soon
as possible.
In conclusion, As we mentioned above,
Figure 4: Clenched hand chromosome analysis should be performed in
patients with dysmorphic facial appearance,
low ear micrognathia, microphthalmia, and
Discussion mane neck. And the clinician should be alerted
to accompanying disorders.
According to earlier research, 46–100% of
newborns with trisomy 18 have some sort of Conflict of interest:
congenital heart abnormality, with samples
The authors report no conflict of interest.
ranging from 13–114 infants [14, 15]. 34
30 JCTEI YEAR: 2022 VOLUME: 1 ISSUE: 1
Funding source: Surg. 2017;103:1941–1949.
doi: 10.1016/j.athoracsur.2017.02.068.
No funding was required. 10. Roberts W., Żurada A., Zurada-Zielińska A.,
Gielecki J., Loukas M. Anatomy of trisomy
Ethical approval: 18. Clin. Anat. 2016;29:628–632.
doi: 10.1002/ca.22725.
No need for case reports 11. Morris J.K., Savva G.M. The risk of fetal loss
following a prenatal diagnosis of trisomy 13 or
trisomy 18. Am. J. Med. Genet. Part
A. 2008;146A:827–832.
doi: 10.1002/ajmg.a.32220.
Contributions
12. Anderson C.E., Punnett H.H., Huff V., De
Chadarévian J.-P. Characterization of a Wilms
Research concept and design: HGÖ
tumor in a 9-year-old girl with trisomy 18. Am.
Data analysis and interpretation: HGÖ J. Med. Genet. Part A. 2003;121A:52–55.
Collection and/or assembly of data: HGÖ doi: 10.1002/ajmg.a.20141.
13. Khan F., Jafri I. Characterization of a 16-Year-
Writing the article: HGÖ Old Long-Time Survivor of Edwards
Critical revision of the article: HGÖ Syndrome. Cureus. 2021;13:e15205.
doi: 10.7759/cureus.15205.
Final approval of the article: HGÖ
14. Rasmussen SA, Wong LY, Yang Q, May KM,
Friedman JM. 2003. Population-based analyses
of mortality in trisomy 13 and trisomy 18.
References Pediatrics 111:777–784.
15. Pont S.J., Robbins J., Bird T., Gibson J.B., Cleves
1. Jones K (Ed). Smith’sRecognizablePatterns of
M.A., Tilford J.M., Aitken M.E. Congenital
Human Malformation. Philadelphia: WB malformations among liveborn infants with
SaundersCompany; 2006: p. 13-17 trisomies 18 and 13. Am. J. Med. Genet. Part
2. Parker MJ, Budd JL, Draper ES, Young ID. A. 2006;140A:1749–1756.
Trisomy 13 andtrisomy 18 in a defined doi: 10.1002/ajmg.a.31382.
population: Epidemiological, geneticand 16. Embleton ND, Wyllie JP, Wright MJ, Burn J,
prenatal observations. PrenatDiagn 2003; 23: Hunter S. 1996. Natural history of trisomy 18.
856-860. Arch Dis Child Fetal Neonatal Ed 75:F38–F41.
3. Edwards JH, Harnden DG, Cameron AH, Crosse 17. Kelly M, Robinson BW, Moore JW. Trisomy 18 in
VM, Wolff OH. A newtrisomicsyndrome. Lancet a 20- year-old woman. Am J MedGenet 2002;
1960; 1: 787-790 112: 397–399
18. Narlı N, Satar M, Süleymanova D. Trizomi 18
4. Naguib KK, Al-Awadi SA, Bastaki L, et al.
(Edward’ssendromu): Üç olgu sunumu. Klinik
Clustering of Trisomy 18 in Kuwait:
Gelişim Dergisi 1998; 11: 486-489
Geneticpredispositionorenvironmental? 19. Nyberg DA, Kramer D, Resta RG. Prenatal
AnnSaudiMed 1999; 19: 197-200. sonographicfindings of trisomy 18: Rewiew of
5. Nussbaum RL, Mclnnes RR, Willard HF. 47 cases. J UltrasoundMed 1993; 12:103.
Principles of clinicalcytogenetics. In: McInnes
RR (Ed). ThompsonandThompson Genetics in
Medicine. Philadelphia: WB SaundersCompany;
2001: p. 140- 144.
6. Cereda A., Carey J.C. The trisomy 18
syndrome. Orphanet J. Rare Dis. 2012;7:81.
doi: 10.1186/1750-1172-7-81.
7. Balasundaram P., Avulakunta I.D. Edward
Syndrome. StatPearls Publishing; Treasure
Island, FL, USA: 2021.
8. Pont S.J., Robbins J., Bird T., Gibson J.B., Cleves
M.A., Tilford J.M., Aitken M.E. Congenital
malformations among liveborn infants with
trisomies 18 and 13. Am. J. Med. Genet. Part
A. 2006;140A:1749–1756.
doi: 10.1002/ajmg.a.31382.
9. Peterson J., Kochilas L.K., Catton K.G., Moller
J.H., Setty S.P. Long-Term Outcomes of Children
With Trisomy 13 and 18 After Congenital Heart
Disease Interventions. Ann. Thorac.
31 JCTEI YEAR: 2022 VOLUME: 1 ISSUE: 1
You might also like
- Cell Cycle: Diseases and Disorders: Shs Stem - Biology 1Document25 pagesCell Cycle: Diseases and Disorders: Shs Stem - Biology 1Emer Perez100% (3)
- Acog Practice Bullet In: Neural Tube DefectsDocument12 pagesAcog Practice Bullet In: Neural Tube DefectsSILVIA GAONANo ratings yet
- The Impact of Trisomy 18 On Quality of LifeDocument10 pagesThe Impact of Trisomy 18 On Quality of LifeJacobs Financial Services LLCNo ratings yet
- 1750 1172 7 81 PDFDocument14 pages1750 1172 7 81 PDFelisabethpriskaNo ratings yet
- Tirotoxicosis Mayo Clinic Proceedings. Harma2019Document17 pagesTirotoxicosis Mayo Clinic Proceedings. Harma2019Salome GarciaNo ratings yet
- Common Dysmorphic Syndromes in The NICUDocument12 pagesCommon Dysmorphic Syndromes in The NICUDaniel PuertasNo ratings yet
- Trisomy 13, 18, 21, Triploidy and Turner Syndrome: The 5T's. Look at The HandsDocument7 pagesTrisomy 13, 18, 21, Triploidy and Turner Syndrome: The 5T's. Look at The HandsDinar Yudistira FirdausNo ratings yet
- Peripartum Cardiomyopathy An Unforeseen CatastropheDocument3 pagesPeripartum Cardiomyopathy An Unforeseen CatastropheBIOMEDSCIDIRECT PUBLICATIONSNo ratings yet
- Tsukada 2012Document8 pagesTsukada 2012jijiNo ratings yet
- Thyrotoxicosis Diagnosis and ManagementDocument17 pagesThyrotoxicosis Diagnosis and ManagementEsteban Martin Chiotti KaneshimaNo ratings yet
- 10 31362-Patd 757219-1166081Document5 pages10 31362-Patd 757219-1166081Elna EstherNo ratings yet
- Mehnaz PDFDocument4 pagesMehnaz PDFdickyaririsandyNo ratings yet
- 2018 Article 1600Document4 pages2018 Article 1600christian roblesNo ratings yet
- Chromosome 18: Ameena Thusleen N DR - Alm P.G Ibms University of MadrasDocument19 pagesChromosome 18: Ameena Thusleen N DR - Alm P.G Ibms University of MadrasRoy EscotaNo ratings yet
- Evidence For The Oocyte Mosaicism Selection Model On The Origin of Patau Syndrome (Trisomy 13)Document7 pagesEvidence For The Oocyte Mosaicism Selection Model On The Origin of Patau Syndrome (Trisomy 13)christian roblesNo ratings yet
- Radio-Contrast Agent-Induced Hyperthyroidism: Case Report and Review of The LiteratureDocument3 pagesRadio-Contrast Agent-Induced Hyperthyroidism: Case Report and Review of The LiteratureIwan SaputeraNo ratings yet
- Di GeorgeDocument3 pagesDi Georgethresh mainNo ratings yet
- Aziz Khan 1985Document7 pagesAziz Khan 1985Eric MunNo ratings yet
- Case Reports in Clinical Practice: A 53-Year-Old Woman With Persistent Erythroderma and DyspneaDocument3 pagesCase Reports in Clinical Practice: A 53-Year-Old Woman With Persistent Erythroderma and Dyspneashinta saingNo ratings yet
- Dev Riend T 1998Document5 pagesDev Riend T 1998Sarly FebrianaNo ratings yet
- Unusual Long Survival in A Case of Heterotaxy and PolyspleniaDocument5 pagesUnusual Long Survival in A Case of Heterotaxy and PolyspleniaVicente Bruno GuimaraesNo ratings yet
- Sindrom PatauDocument12 pagesSindrom PatauIoana PaulaNo ratings yet
- Trisomy 18: Prenatal Diagnosis and Outcome in A Tertiary Care Fetal Medicine Center in South IndiaDocument13 pagesTrisomy 18: Prenatal Diagnosis and Outcome in A Tertiary Care Fetal Medicine Center in South IndiaElna EstherNo ratings yet
- Trisomy 18 Research PaperDocument4 pagesTrisomy 18 Research Paperefhwx1vt100% (1)
- Clinical and Demographic Characteristics of Cutaneous Mastocytosis in Childhood - Single-Center ExperienceDocument6 pagesClinical and Demographic Characteristics of Cutaneous Mastocytosis in Childhood - Single-Center ExperienceRubi LosoyaNo ratings yet
- Cerebral Vein Thrombosis Associated With MTHFR A1289C Mutation Gene in A Young Postpartum WomanDocument5 pagesCerebral Vein Thrombosis Associated With MTHFR A1289C Mutation Gene in A Young Postpartum WomanMauro Porcel de PeraltaNo ratings yet
- 10.7556 Jaoa.2019.032Document4 pages10.7556 Jaoa.2019.032Luana MesquitaNo ratings yet
- Sae 2Document6 pagesSae 2hardi adiyatmaNo ratings yet
- Cripe2017 2750523Document4 pagesCripe2017 2750523فرجني موغNo ratings yet
- Failure To ThriveDocument3 pagesFailure To ThrivefernandoNo ratings yet
- Chagas Therapy NEJM 2011Document8 pagesChagas Therapy NEJM 2011Ever LuizagaNo ratings yet
- European Journal of Medical GeneticsDocument6 pagesEuropean Journal of Medical GeneticsLarissa DmtNo ratings yet
- Arar0332 Jco 2021 DR RaulDocument14 pagesArar0332 Jco 2021 DR RaulLeonardo Müller RodriguesNo ratings yet
- Trisomy 18 ResearchDocument4 pagesTrisomy 18 Researchapi-524182301No ratings yet
- GastricDocument3 pagesGastricedo andriyantoNo ratings yet
- Neonatal PresenatestionDocument32 pagesNeonatal PresenatestionMerwan KemalNo ratings yet
- Sjams 22C749 751 PDFDocument3 pagesSjams 22C749 751 PDFelisabethpriskaNo ratings yet
- Cog NTDocument11 pagesCog NTFabiolaQuijaiteNo ratings yet
- Virilism: M.D., CahillDocument5 pagesVirilism: M.D., CahillQuang Huy NguyenNo ratings yet
- Journal AsliDocument7 pagesJournal AsliMeta ParamitaNo ratings yet
- Labmed36 0419 PDFDocument5 pagesLabmed36 0419 PDFRahul K. JagaNo ratings yet
- Review: Irina Bancos, Stefanie Hahner, Jeremy Tomlinson, Wiebke ArltDocument11 pagesReview: Irina Bancos, Stefanie Hahner, Jeremy Tomlinson, Wiebke Arltinterna MANADONo ratings yet
- Bhanchet 1977Document7 pagesBhanchet 1977zaki ahmadNo ratings yet
- Case Report:: Jana K, Chakraborty T, Ghosh T K, Ghosh S, Pathak SDocument3 pagesCase Report:: Jana K, Chakraborty T, Ghosh T K, Ghosh S, Pathak SivanNo ratings yet
- HSDCDocument5 pagesHSDCCelebre MualabaNo ratings yet
- University of Colorado School of Medicine University of Colorado School of Medicine and Children's Hospital ColoradoDocument2 pagesUniversity of Colorado School of Medicine University of Colorado School of Medicine and Children's Hospital ColoradoashwiniNo ratings yet
- Gross Pericardial Effusion With Tamponade In2 Trimester of PregnancyDocument3 pagesGross Pericardial Effusion With Tamponade In2 Trimester of PregnancyRobby Paguh TariganNo ratings yet
- E1199 FullDocument6 pagesE1199 FullBeatrice Joy TombocNo ratings yet
- 104 FullDocument5 pages104 FullSamNo ratings yet
- Perinatal Transient Myeloproliferative Disorder in Trisomy 21Document11 pagesPerinatal Transient Myeloproliferative Disorder in Trisomy 21Carina SuarezNo ratings yet
- 331-Book Chapter-3614-2-10-20210406Document20 pages331-Book Chapter-3614-2-10-20210406Yolla GitamayaNo ratings yet
- Cushing's Syndrome (Lancet)Document16 pagesCushing's Syndrome (Lancet)Irma OnofreNo ratings yet
- Syndactyly 2Document5 pagesSyndactyly 2AminullahNo ratings yet
- L Iggins 1961Document4 pagesL Iggins 1961ragil putra jNo ratings yet
- Etiology of Proptosis in Children Sindhu 1998Document3 pagesEtiology of Proptosis in Children Sindhu 1998Putri Wulan SukmawatiNo ratings yet
- Hirschsprung - Megacólon CongênitoDocument17 pagesHirschsprung - Megacólon CongênitoBarbara NevesNo ratings yet
- Prise en Charge Therapeutique Des Abces Du Foie A Propos de 40 Cas Au Service de Medecine Interne de Lhopital Cheikh ZayedDocument19 pagesPrise en Charge Therapeutique Des Abces Du Foie A Propos de 40 Cas Au Service de Medecine Interne de Lhopital Cheikh ZayedIJAR JOURNALNo ratings yet
- A Rare Case of Endometriosis in Turners SyndromeDocument3 pagesA Rare Case of Endometriosis in Turners SyndromeElison J PanggaloNo ratings yet
- Operative Treatment of Gynaecologic Diseases in Puberty: Seven Years of ExperienceDocument2 pagesOperative Treatment of Gynaecologic Diseases in Puberty: Seven Years of Experiencemajacokovikj.urologijaNo ratings yet
- Clinical Approach to Sudden Cardiac Death SyndromesFrom EverandClinical Approach to Sudden Cardiac Death SyndromesRamon BrugadaNo ratings yet
- MODULE 2 Scientific SelfDocument8 pagesMODULE 2 Scientific SelfAsh FellNo ratings yet
- Congenital Cytogenetic Abnormalities - UpToDateDocument34 pagesCongenital Cytogenetic Abnormalities - UpToDateIzamar RomeroNo ratings yet
- Chromosomal AbbretionsDocument6 pagesChromosomal AbbretionsSAHIL JPNo ratings yet
- Nature of GeneDocument6 pagesNature of GeneAli JuttNo ratings yet
- Mosaic Trisomy 16Document9 pagesMosaic Trisomy 16apventure trip plannerNo ratings yet
- Topic 6 - Imperfect Cause DefectDocument2 pagesTopic 6 - Imperfect Cause DefectSyaza Izzah Athirah Bt SpaieeNo ratings yet
- SasangDocument11 pagesSasangVince Cinco ParconNo ratings yet
- Introduction To Psychology NotesDocument57 pagesIntroduction To Psychology NotesRic DNo ratings yet
- Chromosomal AberrationsDocument1 pageChromosomal AberrationsDaryl StarkNo ratings yet
- Chromosomal MutationsDocument1 pageChromosomal MutationsLouise Mae LolorNo ratings yet
- Cell Cycle, Cell Death, and DiseaseDocument14 pagesCell Cycle, Cell Death, and DiseaseRose Anne ConcepcionNo ratings yet
- Chromosomal AbberationsDocument33 pagesChromosomal AbberationsMubeena MoossaNo ratings yet
- Unit 1 CytogeneticsDocument2 pagesUnit 1 CytogeneticsALEXANDRA MARIE BUNQUINNo ratings yet
- G10 5e's - Chromosomal MutationDocument5 pagesG10 5e's - Chromosomal MutationYvonne CuevasNo ratings yet
- Genetics - Chromosomal DisordersDocument3 pagesGenetics - Chromosomal DisordersSafiya JamesNo ratings yet
- Human Heredity Principles and Issues 11Th Edition Cummings Test Bank Full Chapter PDFDocument24 pagesHuman Heredity Principles and Issues 11Th Edition Cummings Test Bank Full Chapter PDFAshleyMaciasowbj100% (8)
- XXXXXXXXDocument17 pagesXXXXXXXXRicardo LazoNo ratings yet
- Recurrent Pregnancy LossDocument211 pagesRecurrent Pregnancy LossGopal Kumar Das100% (1)
- FMS I Block BookDocument34 pagesFMS I Block BookAngelique NatalieNo ratings yet
- Interphase Fluorescence in Situ Hybridization Analysis Detects A Much Higher Rate of Thyroid Tumors With Clonal Cytogenetic Deviations of The Main Cytogenetic Subgroups Than Conventional CytogeneticDocument9 pagesInterphase Fluorescence in Situ Hybridization Analysis Detects A Much Higher Rate of Thyroid Tumors With Clonal Cytogenetic Deviations of The Main Cytogenetic Subgroups Than Conventional CytogeneticRubén ManzanoNo ratings yet
- Genetic Disorders - MerwanDocument27 pagesGenetic Disorders - MerwanMerwan KemalNo ratings yet
- Human Chromosomal AbnormalitiesDocument7 pagesHuman Chromosomal Abnormalitiesrobrpassos13No ratings yet
- Chromosomal AberrationsDocument17 pagesChromosomal AberrationsHajiRab NawazNo ratings yet
- Chromosomal Listing RulesDocument55 pagesChromosomal Listing RulesVíctor PaleoNo ratings yet
- Chromosomal AberrationDocument2 pagesChromosomal Aberrationdesi_amlokiNo ratings yet
- Chromosomal AberrationsDocument20 pagesChromosomal Aberrationsvincentsharon0% (1)
- Module 1 To 4 Philo To Sexual SelfDocument38 pagesModule 1 To 4 Philo To Sexual SelfMaryjoy MorallosNo ratings yet
- Kaumarbhriya - PDF 10Document7 pagesKaumarbhriya - PDF 10Ejaj BuzrukNo ratings yet
- Naoba BiologyDocument11 pagesNaoba BiologyCEO IMPHAL SMARTCITYNo ratings yet