Professional Documents
Culture Documents
Hema 2 Lec - M3
Hema 2 Lec - M3
Uploaded by
Lancer BlazeOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hema 2 Lec - M3
Hema 2 Lec - M3
Uploaded by
Lancer BlazeCopyright:
Available Formats
HEMATOLOGY 2 (LECTURE) PRELIMS
MODULE 3 – DISORDERS OF PRIMARY HEMOSTASIS
TOPIC OUTLINE
A. VASCULAR DEFECTS B. QUANTITATIVE PLATELET DISORDERS C. QUALITATIVE PLATELET DISORDERS
a. Connective tissue defects a. Thrombocytopenia a. Inherited Thrombocytopathy
I. Hereditary I. Decreased production I. Adhesion defects
II. Acquired II. Increased loss or destruction II. Aggregation defects
b. Alterations of vessel wall structure i. Non-immunologic III. Release defects
I. Hereditary ii. Immunologic IV. Storage pool diseases
II. Acquired III. Platelet / Splenic sequestration V. Granule-release defects
c. Vascular damage b. Thrombocytosis b. Acquired Thrombocytopathy
I. Infectious purpura I. Primary Chronic Thrombocytosis I. Drugs
II. Autoimmune vascular purpura II. Reactive II. Diet
d. Miscellaneous abnormalities causing purpura secondary to vessel damage III. Diseases
A. VASCULAR DEFECTS
VASCULAR DEFECTS
Categorized into HEREDITARY and ACQUIRED DEFECTS causing bleeding secondary to vascular abnormalities of different types
CONNECTIVE TISSUE DEFECTS (Refer to Table 2A)
o Found in all three layers of the vessel wall; thus, hereditary connective tissue defects affect vessels in all three layers of their structure
TABLE 1. VASCULAR DEFECTS
ABNORMALITY HEREDITARY ACQUIRED
Connective tissues (Refer to Table 2A) Ehlers-Danlos Syndrome Vitamin C deficiency (Scurvy)
Pseudoxanthoma Elasticum Senile purpura
Corticosteroid purpura
Cushing disease
Altered blood vessel wall structure (Refer to Table 2B) Hemorrhagic telangiectasia Diabetes mellitus
Cavernous hemangioma (Kasabach-Merritt Syndrome) Amyloidosis
Vascular damage Infectious purpura
Autoimmune vascular purpura
Miscellaneous abnormalities causing purpura secondary to BV damage Waldenstrom’s macroglobulinemia
Kaposi’s sarcoma
Certain skin disease
Hemochromatosis
Snake venom
TABLE 2A. CONNECTIVE TISSUE DEFECTS
HEREDITARY CONNECTIVE TISSUE DEFECTS
CONDITION INHERITANCE DESCRIPTION CAUSE MANIFESTATIONS DX / Pr / Tx / Lab results
Ehlers-Danlos Autosomal Problem: DEFECTIVE Gene alterations: (discussion) Hypermobile joints (image A) and Dx:
Syndrome dominant (AD) COLLAGEN SYNTHESIS o Problems with the production of fibrillar hyperextensible skin (C, D)
Affects the CT of the skin, collagen / collagen fibrils o Can be stretched much s/s
Autosomal vasculature, and bones lead o Collagen-modifying or collagen-processing more than normal skin, Results of physical examination
non-sex genes to lack of structural tissue enzymes but returns to normal on Genetic testing (checking for
support and great tissue Digesting, rearranging of collagen in release alterations)
Dominant fragility order for them to be biologically active o Increase in tissue
needs only a Enzymes that modify GAGs within elasticity Pr & Tx:
single copy from the ECM Hemorrhagic tendencies (skin or
mucous membranes) No known therapy / cure
BANIÑA, NJ “Nothing worth having comes easy” 1
HEMATOLOGY 2 (LECTURE) PRELIMS
either of the Brought about by defects that lie in: (module) o Skin ecchymoses Most have normal lifespan
parent o PEPTIDASE ENZYME converts procollagen o Hematomas
to collagen o Bleeding from the
o PROCOLLAGEN itself gums
o CROSS-LINKING OF MATURE COLLAGEN Excessive postpartum
bleeding
GIT bleeding
Prone to bruise formation
Higher tendency to scar (B)
o Wound healing requires
functional collagen
Raynaud’s phenomenon (image on the right)
o Distal part of the hands are pale due to decreased blood flow
and BV dilation
o From pale (A) blue (B) red (C)
Pseudoxanthoma Autosomal The ELASTIC FIBERS of the Mutations in ABCC6 gene Common manifestation: Easy Dx:
Elasticum recessive (AR) skin are abnormal causes the o ABCC6: synthesis of elastin (elastin fiber bruisability and hemorrhagic episodes
skin to lax abnormal) (tendency for the BV to become easily s/s
aka Gronblad- Recessive CT elastic fibers in small damaged) Results of physical examination
Strandberg requires copy arteries: Most common causes of death: Results of skin biopsy
Syndrome from both o Calcified Subarachnoid and GIT bleeding Eye examination
parents in order o Structurally and Ectopic mineralization and fragmented
for it to be functionally abnormal elastic fibers of the CT of the skin, Pr & Tx:
apparent retina, and vascular walls
o Deposition of minerals, oftentimes calcium, in abnormal places Lab tests do not provide
in the body diagnosis
o Mineralization is also present in the eyes (retina) No known therapy / cure
o BV calcification Complications may limit lifespan
BV stiffens difficulty in constriction and dilation
Affected areas of the body: neck, axillary, groin
o Skin usually thickens, loose, grooved, inflexible (image on the
right)
ACQUIRED CONNECTIVE TISSUE DEFECTS
CONDITION DESCRIPTION CAUSE MANIFESTATIONS DX / Pr / Tx / Lab results
Vitamin C VITAMIN C Dietary deficiency of Vitamin C (ascorbic acid) Gingival (gum) bleeding (C) Tx:
Deficiency In the absence of Vit C: o Visibly thicken
(Scurvy) Required for the formation of intact, stable collagen, o There is deficiency of the intercellular cement o Red-purple coloration Administration of ascorbic
particularly in BVs substances that holds endothelial cells together Coiled hairs acid
o Hydroxylation of PROLINE and LYSINE o “cork-screw” o Usually brings the
cannot take place no collagen production appearance plasma level of Vit C
o Collagen cannot be formed properly Bleeding tendencies and the vascular
Causes fragility and serious bleeding o Ecchymoses and integrity back to
problems purpura normal
Other conditions that may cause scurvy: o Hemorrhage into o Rapidly eliminates the
o Pregnancy subcutaneous tissues hemorrhagic
o Breastfeeding and muscles manifestations
o An overactive thyroid gland o Petechiae (often
(hyperthyroidism) develop on the thighs Lab results:
o Prolonged diarrhea and buttocks, particularly around the hair follicles
BT and coagulation tests
o Surgery (PERIFOLLICULAR PETECHIAE)) (A, B, D)
usually normal
o Burns o Large hemorrhagic areas may develop just below the eyes,
o Smoking particularly in affected infants Tests for plt function
sometimes abnormal
Senile Purpura Senile: relates to all age Progressive degeneration and loss of collagen, Red to purple ecchymotic spots on the
Benign, acquired, and chronic disorder of the elderly elastin, and subcutaneous fat due to aging forearm and on the back of the hands, and
There may also be a defective cross-linking of collagen neck (secondary to loss of skin and vascular
elasticity)
o The hemorrhage resolves but the
area retains a permanent brownish
color
This is possibly because
the Hgb is not properly
removed by the aging
macrophage system
(degenerated)
BANIÑA, NJ “Nothing worth having comes easy” 2
HEMATOLOGY 2 (LECTURE) PRELIMS
Steroid / Atrophy of collagen fibers due to chronic steroid Chronic exposure to steroids
Corticosteroid use
Purpura STEROIDS
o Inhibits response of macrophages
o Bleeding cannot be engulfed by
macrophages
Cushing Disease Involves the endocrine system: pituitary gland Adrenals overproduce corticosteroids Skin becomes thin
affects adrenal gland Bruises easily
Heals poorly when bruised or cut
Striae (image on the right)
o Differentiate if it is caused by
Cushing disease or
pregnancy
Check first if the px
is pregnant
Check hormonal panel
TABLE 2B. ALTERATIONS OF VESSEL WALL STRUCTURE
HEREDITARY ALTERATIONS OF VESSEL WALL STRUCTURE
CONDITION INHERITANCE DESCRIPTION CAUSE MANIFESTATIONS DX / Pr / Tx / Lab results
Hereditary AD Gr. Telangiectasia: telos end; Genetic mutations that involve signaling of TGF-β LESIONS Tx:
Hemorrhagic angeion BVs; ektasis o A transformative / transforming group factor o Pinpoint (0.3 mm)
Telangectasia dilation or widening o Affects cell cycle, apoptosis, certain cell o Red to violet Given only based on symptoms
o Small widened BVs signaling processes, and proliferation of certain o Raised or flat Iron therapy
aka “Osler-Weber- Characterized by bleeding that cells o Round or spider-like (1st Therapeutic drugs and
Rendu Syndrome” occurs from TELANGECTASIAS image) surgical techniques (may be
–vascular malformations of o May bleed spontaneously required to stop or prevent
thin, dilated small vessels in or from minor trauma bleeding episodes)
the skin and mucosae o Appear most commonly on
The small blood vessels are the face, lips, tongue,
focally disorganized and mucous membranes of
dilated throughout the body, their the mouth and nose,
wall support is poor, and their ears, conjunctivae, and
ability to contract is diminished palms of the hands and
o Thus, any trauma to the soles of the feet
vessels causes them to o Permanent
bleed readily and for a o Number increases with advancing age
prolonged period Most common symptoms: Epistaxis and alimentary bleeding
May be detected in childhood Iron deficiency
Bleeding usually begins during anemia (if
the 2nd or 3rd decade chronic)
Dilated
capillaries on
skin and
mucosal
membrane
Arteriovenous
alterations
Cavernous AD Cavernous cave-like; hema Spontaneous Cavernous or “strawberry” (red-blue color) The tumor requires surgical
Hemangioma blood; oma swelling hemangioma (1st image) removal
Tumor
aka Kasabach- o A tumor that encloses large vascular
Merritt Syndrome spaces and it is partly or completely
filled with blood (2nd image)
o Present at birth or soon thereafter
o Composed of soft
vascular
malformations
that commonly
swell and bleed
at the surface
o Size: small to
enormous
lesions that protrude from the skin surface
BANIÑA, NJ “Nothing worth having comes easy” 3
HEMATOLOGY 2 (LECTURE) PRELIMS
o Formation of fibrin clots, plt consumption, and red cell
destruction secondary to vascular obstruction occur at the
site of the tumor
Thrombocytopenia
Microangiopathic Hemolytic Anemia (MAHA)
o Involves smallest BVs
o Destruction of RBCs
Consumptive coagulopathy
o Decrease in fibrinogen concentration (hypofibrinogenemia)
Presence of endothelial cells, spindle cells, and abnormal lymphatic
tissues
ACQUIRED ALTERATIONS OF VESSEL WALL STRUCTURE
CONDITION DESCRIPTION
Atherosclerosis Under DYSLIPIDEMIA build-up of lipids, especially cholesterol, in the BVs (arteries)
Plaque eventually becomes ATHEROMA that will slough off and will block the heart
Diabetes mellitus Metabolic disorder that affects how glucose will be taken into the cell
Involvement of inflammatory mediators affects the integrity of the BVs may lead to thrombosis, fibrosis, and bleeding tendencies
Large BVs become ATHEROSCLEROTIC and the capillary basement membrane may thicken blocking the normal blood flow
Amyloidosis There is abnormal deposition of FIBRILLAR PROTEINS (AMYLOID) obstruct the function of many organs including the vascular system
Weakens the vessels and causes hemorrhaging
B. QUANTITATIVE PLATELET DISORDERS
a. THROMBOCYTOPENIA
Defined as a plt count less than 140x109/L and occurs whenever the plt production is insufficient to meet the need
2 MAJOR CAUSES:
o Rate of production is decreased
o Rate of plt loss is increased
The severity of bleeding is related to the degree of thrombocytopenia (Refer to Table 3)
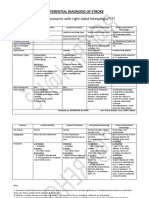
TABLE 3. SEVERITY OF BLEEDING AND DEGREE OF THROMBOCYTOPENIA
PLATELET COUNT / FUNCTION DEGREE OF THROMBOCYTOPENIA
Less than 100x109/L Bleeding time is INVERSELY PROPORTIONAL to the platelet count
Above 50x109/L; plt fxn is normal Pxs will have no hemorrhagic symptoms unless subjected to trauma or surgery
Less than above 50x109/L Referred to as SEVERE THROMBOCYTOPENIA
Less than 20x109/L Spontaneous bleeding occurs
Normal plt fxn The template BT is usually within the normal range as long as plt counts are greater than 100x109/L (when the plt count falls below
this, the degree to which BT is prolonged is INVERSELY PROPORTIONAL to the decrease in plt count);
Plt aggregation studies should be normal
Below 60x109/L Clot retraction is usually abnormal
DEGREE OF THROMBOCYTOPENIA
NORMAL 150-400 x109/L
MILD 100-150 x109/L
MODERATE 50-99 x109/L
SEVERE <50 x109/L
BANIÑA, NJ “Nothing worth having comes easy” 4
HEMATOLOGY 2 (LECTURE) PRELIMS
TABLE 4. LABORATORY MEASUREMENT OF PLATELET COUNT
AUTOMATED HEMATOLOGY CELL ANALYZER ERRORS (SPURIOUS CELL COUNTS)
Coulter principle Sample clotting problem with specimen collection
Manual counting is still needed for plt estimation Spontaneous plt agglutination
o Cold Autoimmune Hemolytic Anemia
MARROW ASPIRATE OR BIOPSY o Platelet Satellitosis
Plt binds to surface of WBC (neutrophils)
Aspirate: BM cells in the bone Pseudothrombocytopenia
Biopsy: fragment of bones Use citrate or heparin
Purpose: assess plt production or destruction HOW TO KNOW: establish thrombocytopenia, validate the results of blood smear by blood film, recollect
Check for hematopoietic disease processes and evaluate the number and appearance of megakaryocytes if using different anticoagulant
o Binding to WBCs
TABLE 5. CLASSIFICATION OF THROMBOCYTOPENIA
Megakaryocyte hypoproliferation: Aplastic anemia, Drug toxicity, Alocohol toxicity, Viral infection, Congenital states
DECREASED PRODUCTION: Ineffective thrombopoiesis: Megaloblastic anemia, Paroxysmal Nocturnal Hemoglobinuria (PNH), Thrombopoietin deficiency, Ethanol abuse without malnutrition, Severe iron-deficiency anemia, Viral
(Refer to Table 6A) infection
Marrow replacement: Leukemia, Plasma-cell dyscrasia, Metastatic carcinoma, Myelofibrosis, Lymphoma, Granulomatous infections
Non-immunologic (due to intravascular coagulation and Loss: Severe hemorrhage, Extensive transfusion
increased platelet clearance) Consumption: DIC, HUS, TTP, Foreign surface, Thermal injury, Sepsis without DIC
INCREASED LOSS OR DESTRUCTION: (Refer to
Isoimmune: NATP, PTP, Refractory to platelet syndrome
Table 6B)
Immunologic Autoimmune: ITP, Disease-associated
Viral infection
SPLENIC SEQUESTRATION (Refer to Table 6C)
TABLE 6A. THROMBOCYTOPENIA: DECREASED PLATELET PRODUCTION
INHERITED MEGAKARYOCYTIC HYPOPLASIA
CONDITION INHERITANCE DESCRIPTION CAUSE MANIFESTATIONS DX / Pr / Tx / Lab results
Fanconi Anemia AR Characterized by marked DEFECTIVE dsDNA REPAIR Most notable skeletal deformities: absent or
(FA) hypomegakaryocytic Most common cause of inherited BM failure hypoplastic thumbs and short stature
thrombocytopenia, Pancytopenia
skeletal deformities, and Microcephaly small brain and head
sexual and mental Prone to dislocated hips
retardation
Thrombocytopeni AR Not well established Transient thrombocytopenia
a with Absent Neonates with TAR present at birth with severe thrombocytopenia and normal RBC and
Radius (TAR) WBC count
Defect exists at the stem cell level and involves early progenitors of all cell lines
Most evident abnormality: bilateral absence of the forearm bones (radius)
The defect affects only the megakaryocyte progenitor cells
Up to 90% of the neonates with TAR die in the 1st year of life
o There is a possibility that the plt count will be close to normal by 5-6 years of age
Mental retardation occurs in about 7% of the TAR neonates associated with
INTRACRANIAL HEMORRHAGE
Cow’s milk intolerance exacerbates thrombocytopenia when px drinks cow’s milk
Amegakaryocytic Differs from TAR in that the
Thrombocyto- thrombocytopenia
penia (AMT) persists and the px
deteriorates
In some cases, there is
complete failure of the
marrow affects all
hematopoietic cell lines
BANIÑA, NJ “Nothing worth having comes easy” 5
HEMATOLOGY 2 (LECTURE) PRELIMS
ACQUIRED MEGAKARYOCYTIC HYPOPLASIA
(MARROW DAMAGE failure in plt production; possible that all aspects of normal hematopoiesis are decreased MARROW APLASIA)
(RADIATION THERAPY, CHEMOTHERAPY, EXPOSURE TO TOXIC CHEMICALS AND ALCOHOL, COMPLICATION OF VIRAL INFECTION reduction in marrow megakaryocyte)
CONDITION DESCRIPTION
Aplastic anemia Can be a consequence of toxic chemical or physical agents
o IONIZING RADIATION and CHEMOTHERAPEUTIC AGENTS produce a dose-dependent suppression of cells at the stem cell level
Viral infections implicated in bone marrow hypoplasia
Drugs: CHLOROTHIAZIDE, CISPLATIN and CARBOPLATIN, and ANAGRELIDE directly suppress megakaryocyte production
Myelophthisic Refers to the crowding out of megakaryocytic precursors by space-occupying lesions in the marrow
Thrombocytopenia Invasion of the marrow by non-megakaryocytic tissues occurs in many conditions such as:
o Myelofibrosis
o Metastatic tumor
o Leukemia
o Hodkin and non-Hodgkin lymphomas
o Microangiopathic Hemolytic Anemia (MAHA)
o Osteopetrosis
Prolonged Hypoxia Reduces the pool of megakaryocytic thrombocytopenia by reducing the pool of committed megakaryocyte progenitor cells by means of a greatly expanded erythroid progenitor pool
INHERITED INEFFECTIVE THROMBOPOIESIS
CONDITION INHERITANCE DESCRIPTION CAUSE MANIFESTATIONS Dx / Pr / Tx / Lab results
May-Hegglin AD Characterized by Dohle bodies Mutation in a gene causing defective Often symptomatic Degree of
Anomaly within leukocytes, a variable megakaryocytic maturation thrombocytopenia:
9
degree of thrombocytopenia and 20-120x10 /L
giant plts MPV: 15-20 fL
Thrombocytopenia is attributed to Plt fxn: normal
ineffective thrombocytosis with
the possibility of an immune
involvement of destruction
Bernard Soulier AR Causes plt adhesion defect Larger DMS in megakaryocytes abnormally large
Syndrome leads to bleeding problems in proplatelet tips
affected individuals
Deficiency of the
GLYCOPROTEIN Ib/IX in plts
Wiskott-Aldrich An immunodeficiency syndrome Mutation in the WASP gene Small plts
Syndrome Characterized by severe Thrombocytopenia
thrombocytopenia and Decreased α-granules and dense bodies
excessively small plts lead to Eczema
bleeding Recurrent infections
Paris-Trousseau Characterized by Skull dysmorphism Although plts in
Syndrome thrombocytopenia due to Developmental delay peripheral circulation
ineffective thrombopoiesis and Multiple organ abnormalities have normal life
production of span, 15% of the plts
micromegakaryocytes in the BM in peripheral blood
show giant α-
granules resulting
from the fusion of α-
granules
BANIÑA, NJ “Nothing worth having comes easy” 6
HEMATOLOGY 2 (LECTURE) PRELIMS
ACQUIRED INEFFECTIVE THROMBOPOIESIS
Normal to increased number of certain BM cells; BM cells are dysplastic; generalized cytopenia; associated with Vitamin B12 deficiency (megaloblastic anemia) possibility of increased apoptosis of developing megakaryocyte
CONDITION DESCRIPTION CAUSE MANIFESTATIONS Dx / Pr / Tx / Lab results
Ethanol abuse Suppresses thrombopoiesis at the level of the Defective formation and decreased lifespan
maturing megakaryocyte decreases the plt
lifespan
Plt counts usually start to increase after 2-5 days of
abstinence from alcohol
Vitamin B12 or Results in an impairment of DNA synthesis leads to Due to short lifespan of plts, Vit B12-deficient pxs present with mild thrombocytopenia
Folate Deficiency dyspoiesis and megaloblastic transformation of cells before the RBC megaloblastic changes are seen
in the myeloid series
Paroxysmal Affects the hematopoietic stem cells Thrombocytopenia is primarily caused by Presence of Hgb in urine
Nocturnal Cells have enhanced susceptibility to complement ineffective thrombopoiesis
Hemoglobinuria binding and lysis Megakaryocyte progenitors have
(PNH) decreased proliferative activity
Viruses Invade megakaryocytes leads to decreased plt
production
They can impair megakaryopoiesis by interacting at
the cell surface or thru viral entry and intracellular
replication
Viruses known to invade megakaryocytes include the ff:
o Hepatitis C
o Herpes simplex
o HIV
o Colorado tick fever
TABLE 6B. THROMBOCYTOPENIA: INCREASED LOSS OR DESTRUCTION
NON-IMMUNE PLATELET DESTRUCTION: PLATELET CONSUMPTION
CONDITION DESCRIPTION CAUSE MANIFESTATIONS LAB RESULTS
Disseminated Toxins or conditions that trigger procoagulant Massive tissue damage Thrombocytopenia
Intravascular release G-septicemia Schistocytes
Coagulation (DIC) Obstetric complications 1 or 2 clotting factors and
Three major
Organ destruction inhibitors
conditions
Severe transfusion reactions FDPs
characterized by
tumors D-dimer
non-immune
thrombocytopenia
due to increased
Hemolytic Uremic In the early stages of HUS, thrombi formation Damage to endothelium Hematologic studies
plt consumption
Syndrome (HUS) is primarily intraglomerular Thrombotic microangiopathy Hemolytic workup
and shortened plt
Common manifestations: renal RBC fragmentation UA
lifespan
dysfunction, proteinuria, and hematuria
Thrombocytopenia Both HUS and TTP
results from either have a common
Thrombotic Can be congenital w/ unknown etiology (1/3-1/2, PENTAD (FATRN) Considered sufficient for dx:
acute or chronic pathomechanisms Thrombus formation is diffuse and affects
Thrombocytopenic most) o F Fever
activation of the involving endothelial many organs
Purpura (TTP) Can be pregnancy-related o A Anemia (MAHA) Anemia and
coagulation cell damage Increase levels of vWF multimers T Thrombocytopenia thrombocytopenia
system and the Can be a result of marrow transplantation o
causes plt thrombi to accumulate in the plasma for unknown
Can be a result of drug therapy- as an effect of o R Renal pathology (oliguria, Schistocytosis
generation of form: reasons
inhibitor mediated cleaving protease deficiency; hematuria, ESRD) Increased LDH
thrombin As the severity of TTP progresses, these o N Neurological symptoms
tacrolimus, cyclosporine; quinine
large multimers disappear and the plt
Secondary to plt activation, aggregation, and (hemiplegia, aphasia,
count decreases paresthesia, visual disturbance)
thrombus formation
HELLP Syndrome HEMOLYSIS, ELEVATED LIVER ENZYMES, AND LOW PLATELETS (HELLP) SYNDROME Result from microvascular endothelial activation Coagulation studies:
and cell injury normal PT, 50% may
have prolonged APTT
Hemolytic workup (PBS)
BANIÑA, NJ “Nothing worth having comes easy” 7
HEMATOLOGY 2 (LECTURE) PRELIMS
NON-IMMUNE PLATELET DESTRUCTION: MISCELLANEOUS
CAUSE DESCRIPTION
Dilutional Loss Severe thrombocytopenia is a common occurrence following massive blood transfusions
o Degree of thrombocytopenia is DIRECTLY PROPORTIONAL to the number of units transfused
The number of functional plts in blood that have been stored for more than a few days is close to zero
o Thus, the pxs requiring extensive transfusions develop thrombocytopenia by acute blood loss, plt consumption, and dilution of their own plt pool
Artificial Surfaces Plt contact with artificial surface such as vascular prosthetic devices, artificial organs, prosthetic vascular grafts, and dialysis membranes is associated with quantitative and qualitative changes in plt function
Drugs Drug-induced plt clumping can result in thrombocytopenia
Among the drugs implicated in this mechanism are RISTOCETIN and HEPARIN
Infections SEPSIS-INDUCED THROMBOCYTOPENIA can result from the direct interaction betw the organism and plts, resulting in lysis or phagocytosis by the RES
IMMUNE PLATELET DESTRUCTION: ISOIMMUNE THROMBOCYTOPENIA
CONDITION DESCRIPTION CAUSE MANIFESTATION LABS
Neonatal PLATELET-SPECIFIC Homologous to HDFN, Measurement of mother’s plasma
Alloimmune ALLOANTIGEN HPA-1a except that plt is the Specificity for neonate’s plts
Thrombocytopenic target of the maternal
Purpura (NATP) The most IgG
antigenic of the plt
alloantigens
Post-transfusion Associated with A sudden, profound, Alloimmunization Sudden, severe thrombocytopenia after 5-10 days
(Isoimmune) NATP and PTP and self-limited against platelet
Purpura (PTP) thrombocytopenia antigens
caused by sensitization
of Ab response by an
alloantigen located on
the membrane
glycoprotein IIIa
Refractory to Platelet Pxs refractory to plt transfusion develop thrombocytopenia by not producing sustained increase in plt count
Syndrome Among pxs with APLASTIC ANEMIA or ACUTE LEUKEMIA who have received long-term plt support, plt alloimmunization causes a rapid destruction of transfused plts
IMMUNE PLATELET DESTRUCTION: AUTOIMMUNE THROMBOCYTOPENIA
CONDITION DESCRIPTION / CAUSE MANIFESTATIONS Dx / Pr / Tx / Lab results
Primary IMMUNE THROMBOCYTOPENIC PURPURA (ITP) ACUTE ITP ACUTE ITP
Autoimmune o haracterized by the destruction of antibody-coated plts in the RES and by normal to increased megakaryocytic
Thrombocytopenia production Affects adults of age 20-40 Plt count: less than 20x109/L
o Loss of immunological tolerance to autoantigens on px’s own plts (IIb-IIIa and Ib-IX) o Manifestations: Tx: IV immunoglobulin (Anti-D antibody), interferon, and
o Cause is related to drugs and infection hypermenorrhagia, cyclosporin
o Purpura, menorrhagia, epistaxis, gingival bleeding, retinal hemorrhages, bruising tendency easy bruising,
Autoantibodies target membrane glycoproteins IIb-IIIa and Ib-IX petechiae, purpura, CHRONIC ITP
o The binding of autoantibodies to plts can cause phagocytosis by the immune system by an Fc receptor mechanism and or prolonged
activation of the complement pathway allows more efficient phagocytosis bleeding from Plt count: 30-80x109/L
superficial skin Tx:
cuts o Steroids and IV immunoglobulin (initial therapy)
o Splenectomy most effective management
CHRONIC ITP among pxs who do not respond to initial tx
Affects older adults
Secondary Refers to thrombocytopenia that is secondary to another disease process
Autoimmune Disease that lead to thrombocytopenia include the ff:
Thrombocytopenia o Lymphoproliferative disorders (e.g., chronic lymphocytic leukemeia (CLL), and Hodgkin disease)
o Miscellaneous conditions (e.g., rheumatoid arthritis, SLE, and Chron’s disease)
o Infectious diseases caused by bacterial infections, HIV, and other viruses
BANIÑA, NJ “Nothing worth having comes easy” 8
HEMATOLOGY 2 (LECTURE) PRELIMS
IMMUNE PLATELET DESTRUCTION: DRUG-INDUCED
CONDITION DESCRIPTION / CAUSE MANIFESTATIONS Dx / Pr / Tx / Lab results
Drug-induced Drugs implicated to cause immune thrombocytopenia include: Common manifestations: Plt count returns to normal limit 7-10 days after drug is
Immune o Quinidine o Sudden onset of discontinued
Thrombocytopenia o Quinine petechiae
o Gold salts o Ecchymoses Dx:
o Sulfonamides and their derivatives o Blood-filled blisters
o Chloroquine in the mouth 1) exposure to the candidate drug preceded
o Rifampicin o Mucosal bleeding thrombocytopenia
The Ab is directed against either a drug-platelet complex or a drug-plasma protein complex that binds to the plt, or there could 2) recovery from thrombocytopenia was complete and
also be a drug-induced synthesis of plt autoantibody sustained after discontinuing the candidate drug
3) other causes for thrombocytopenia were excluded
TABLE 6C. THROMBOCYTOPENIA: SPLENIC SEQUESTRATION
Platelet SPLEEN responsible for thrombocytopenia by increased phagocytosis and destruction of damaged plts or by increased sequestration of normal, undamaged plts
Sequestration This happens in HYPERSPLENISM caused by the ff:
o Gaucher disease
o Sarcoidosis
o Felty Syndrome
b. THROMBOCYTOSIS
Defined as an increase in plts above 450x109/L
Classified into 2: reactive and essential (Refer to Table 5)
TABLE 7. CLASSIFICATION OF THROMBOCYTOSIS
REACTIVE THROMBOCYTOSIS ESSENTIAL THROMBOCYTOSIS
Caused by a stimulus (e.g., neoplasma, inflammatory conditions, iron deficiency, major trauma, post-splenectomy, post- A condition characterized by extensive thrombocytosis due to increased megakaryocyte production with persistent and
surgery, epinephrine injection, or recovery from thrombocytopenia) massive elevation in plt count
Increased plt count is temporary, and is less than 1000x109/L and is not associated with any clinical problems
THROMBOCYTHEMIA
A term that refers to increased plt counts associated with chronic myeloproliferative disorders (CMPD)
BANIÑA, NJ “Nothing worth having comes easy” 9
HEMATOLOGY 2 (LECTURE) PRELIMS
REACTIVE: PRIMARY CHRONIC THROMBOCYTOSIS:
Physiologic Essential thrombocythemia
Iron Deficiency Anemia Polycythemia vera
Rapid Blood Regeneration: Acute blood loss, Hemolytic anemia, Rebound Postoperative Chronic granulomatous leukemia
Infections and inflammatory diseases Myelofibrosis with myeloid metaplasia
o Chronic Disorders: Tuberculosis, Ulcerative colitis, sprue, rheumatoid arthritis, osteomyelitis
o Acute Infections
Neoplasms: Carcinoma, Hodgkin disease
TABLE 8. TYPES OF THROMBOCYTOSIS
CONDITION DESCRIPTION CAUSE
Can be caused by essential thrombocythemia, polycythemia vera, and chronic myelocytic leukemia
Primary Uncontrolled, malignant proliferation of plts
Thrombocytosis
Secondary Increased plt production Chronic and acute inflammatory disease
Thrombocytosis Plt count is elevated, but <1000x109/L Iron deficiency: Iron regulates thrombopoiesis by inhibiting thrombopoietin; deficiency causes increased TPO
Rapid blood regeneration due to hemolytic anemia and acute blood loss
Exercise
Other conditions: Cytotoxic drug withdrawal
Neoplasms
C. QUALITATIVE PLATELET DISORDERS
TABLE 9A. QUALITATIVE PLATELET DISORDERS: INHERITED THROMBOCYTOPATHY
ADHESION DEFECTS
Extremely rare
Defect in the Ib molecule: receptor sites for thrombin mediates adhesion of platelets to the BV wall by binding vWF
CONDITION DESCRIPTION CAUSE MANIFESTATIONS Dx / Pr / Tx / Lab results
Bernard-Soulier Abnormal bleeding occurs because plts lack Mild to moderate thrombocytopenia (not very common) MPV of giant plts: 12.5 fL
Syndrome (BSS) the vWF adhesion receptor GP Ib-V-IX that Marked anisocytosis of plts (evident) majority of them being as big BT: excess of 20 minutes
is necessary for binding as lymphocytes Decreased plt retention by glass bead
Plt lifespan shortened to 4 days columns
Epistaxis Plt count: very low to low normal
Gingival bleeding Plt aggregation studies: reduced
Cutaneous bleeding Abnormal ristocetin plt agglutination
Hemorrhage associated with trauma
Platelet-type Aka PSEUDO VON WILLEBRAND DISEASE BT: prolonged
(Pseudo) von Characterized by abnormally enhanced binding of Plts show hypersensitivity to ristocetin
Willebrand Disease vWF to the plt GP Ib-V-IX membrane receptor
results to the loss of vWF from the plasma and the
removal of vWF-bound plts from the circulation
AGGREGATION DEFECTS
Glanzmann A thrombocytopathy associated with a defect in the GP Inability of fibrinogen to bind w/ plts Plts are normal in number, size,
Thrombasthenia IIb-IIIa complex Lack of thrombasthenin/actomyosin morphology and prolonged
(GT) causes clot retraction defect Plts do not aggregated with ADP,
TYPE I GT epinephrine, collagen, or thrombin,
but will react with ristocetin
Lacks the GP IIb-IIIa as well as intraplatelet fibrinogen
thus, plts cannot perform clot retraction
TYPE II GT
Plts contain subnormal levels of fibrinogen and
decreased amounts of GP IIb/IIIa (15% only)
BANIÑA, NJ “Nothing worth having comes easy” 10
HEMATOLOGY 2 (LECTURE) PRELIMS
RELEASE DEFECTS: STORAGE POOL DISEASES (characterized by abnormal release of ADP secondary to lack of α- or dense-granules; there may also be a deficient quantity of ADP stored within the granules)
Gray Platelet α-granules are lacking Lifelong history of mild bleeding, easy bruising, moderate Wright-stained PBS: plts appear to be
Syndrome thrombocytopenia, and abnormal plt morphology larger and gray to blue-gray in color
Tests for the constituents of α-
granules are abnormal
Wiskott-Aldrich An immunodeficiency disorder The profound thrombocytopenia is brought Prone to hemorrhage and recurrent infections Plts are significantly small, almost 2/3
Syndrome Characterized by small plts and the TRIAD OF: about by rapid plt turnover and ineffective of the normal size
o THROMBOCYTOPENIA production MPV: significantly reduced
o RECURRENT INFECTIONS Abnormal cellular membranes (due to
o ECZEMA lack of surface proteins)
Decreased α-granules and dense bodies
Hermansky-Pudlack Characterized by a TRIAD OF:
Syndrome o TYROSINASE-POSITIVE
OCULOCUTANEOUS ALBINISM
o ACCUMULATION OF CEROID-LIKE
PIGMENT IN MACROPHAGES
o BLEEDING TENDENCY ASSOCIATED WITH
ABNORMAL PLT FXN
Associated with the lack is dense bodies, while the
number of α-granules is normal
RELEASE DEFECTS: GRANULE-RELEASE DEFECTS (characterized by impaired secretion of normal granule contents, referred to as ASPIRIN-LIKE DEFECT)
Deficiency of Platelet Include deficiencies in the cyclooxygenase and
Prostaglandin abnormal TXA2 activity leads to abnormal plt
Enzymes aggregation
Cyclooxygenase Mild bleeding disorder Pxs are advised to avoid anti-platelet
Deficiency drugs
TABLE 9B. QUALITATIVE PLATELET DISORDERS: ACQUIRED THROMBOCYTOPATHY
DRUGS
DRUG CAUSE AND EFFECT
Aspirin Pxs taking aspirin have abnormal aggregation due to the inhibition of cyclooxygenase
Indomethacin, Have the same effects as to aspirin
Ibuprofen,
Butazolidine
Carbenicillin Affects plt function by interacting with glycoproteins on the surface of the platelet causes reduced response to aggregating agents
Alcohol Prolonged exposure to alcohol impairs PF3 release and reduces aggregation due to the inhibition of TXA2
Dipyridamole Can increase plt cAMP concentration inhibit plt function
IV Dextran and Reduce plt function because of the plt surface coating action of these expanders
related plasma
expanders
DIET
Fish Significant amounts of fish in the diet can decrease plt function
This is brought about by the replacement of arachidonic acid production with the fatty acids present in fish oils and the production of inactive prostaglandin
BANIÑA, NJ “Nothing worth having comes easy” 11
HEMATOLOGY 2 (LECTURE) PRELIMS
Herbs Herbs used in Szechwan cooking decreases plt release reaction
Onions, garlic, and Contain substances that can inhibit plt aggregation
related plants
Vitamin B12 or May lead to qualitative plt defects as well as thrombocytopeni
Folate Deficiencies
Large amounts of Affect plt lipids through peroxidation with resulting defects in prostaglandin synthesis
Vitamin E
DISEASES
Myeloproliferative Malignant myeloproliferative disorders are associated with large, hypogranular platelets that can be defective in any or all functions that reflect fundamental defects in megakaryocyte maturation
Disorders
Uremia An increase in BUN is associated with qualitative plt defects that can be corrected with dialysis
Presentations include decreased adhesion, aggregation and defective release caused by the metabolites of urea – GUANIDOSUCCINIC ACID and PHENOLIC ACID inhibit platelet aggregation
Some patients exhibit defective factor VIII/vWF complexes
DIC Prematurely activated plts release granules causing an acquired platelet SPD
The fibrin(ogen) degradation products that circulate in DIC interact with platelet membranes inhibit adhesion or aggregation
Immunoglobulin Antibody binding to plts accelerates platelet destruction and inhibits platelet function
Production The reduced platelet aggregation using collagen, ADP, and epinephrine seen in SLE and ITP has been associated with increased levels of immunoglobulins
Antibodies such as anti-HPA-1a which binds to GP IIIa can bind to membrane receptors and inhibit platelet function while some can affect the uptake of substances into the platelet granules during megakaryopoiesis
Dx: diagnosis
Pr: prognosis
Tx: treatment
BANIÑA, NJ “Nothing worth having comes easy” 12
You might also like
- Blair Upper CervicalDocument4 pagesBlair Upper Cervicallopezhectora100% (1)
- Classification of AnemiaDocument4 pagesClassification of AnemiaEna PaparićNo ratings yet
- Chapter 11 Blood Vessels 8th Ed NotesDocument7 pagesChapter 11 Blood Vessels 8th Ed NotesKyle Christopher SiaNo ratings yet
- Renal - PathologyDocument38 pagesRenal - Pathologyjmosser3102100% (2)
- Neuro HackingDocument2 pagesNeuro HackingAnonymous HQuX2LUsDNo ratings yet
- CHRA 1st Reprint 2018 PDFDocument149 pagesCHRA 1st Reprint 2018 PDFMohd Jamalil Azam MustafaNo ratings yet
- Promoting The Conservation and Use of Under Utilized and Neglected Crops. 08 - ChayoteDocument58 pagesPromoting The Conservation and Use of Under Utilized and Neglected Crops. 08 - ChayoteEduardo Antonio Molinari NovoaNo ratings yet
- Role of Blood Vessels in Hemostasis: Villa, M.D. MLS 4CDocument10 pagesRole of Blood Vessels in Hemostasis: Villa, M.D. MLS 4CMarianne Dennesse100% (1)
- AnemiaDocument8 pagesAnemiasibanah menor100% (1)
- Earth and Life Science ExamDocument9 pagesEarth and Life Science ExamMa WiNo ratings yet
- HEMA 2 - Midterm Topic 3 - Anemia of Bone Marrow DisorderDocument10 pagesHEMA 2 - Midterm Topic 3 - Anemia of Bone Marrow DisorderLowenstein JenzenNo ratings yet
- Anemia - SFFTDocument5 pagesAnemia - SFFTShikha UpadhyayNo ratings yet
- MODULE 3 Disorders of Primary HemostasisDocument13 pagesMODULE 3 Disorders of Primary HemostasisLancer BlazeNo ratings yet
- Meng GitDocument60 pagesMeng GitGary SisiputNo ratings yet
- HEMA2 GroupNo.1 AnemiaofBoneMarrowDisordersDocument13 pagesHEMA2 GroupNo.1 AnemiaofBoneMarrowDisordersLowenstein JenzenNo ratings yet
- QuizletDocument67 pagesQuizletnaimNo ratings yet
- Anemia of Iron Abnormal Metabolism: DR Bidasari Lubis, Sp. A (K) Bagian Ilmu Kesehatan Anak RSU Haji Adam Malik MedanDocument40 pagesAnemia of Iron Abnormal Metabolism: DR Bidasari Lubis, Sp. A (K) Bagian Ilmu Kesehatan Anak RSU Haji Adam Malik Medanalfat22No ratings yet
- Anemia of Iron Abnormal Metabolism: Blue Ocean 1Document40 pagesAnemia of Iron Abnormal Metabolism: Blue Ocean 1Sukhrian MuhdaNo ratings yet
- Vasculitis by VinhDocument4 pagesVasculitis by VinhTovin NguyenNo ratings yet
- Blood Loss 2. Increased Destruction 3.impaired Red Cell ProductionDocument4 pagesBlood Loss 2. Increased Destruction 3.impaired Red Cell Productionjehangir zuberiNo ratings yet
- COURSE OUTLINE Heam 2019Document3 pagesCOURSE OUTLINE Heam 2019Edna Uneta RoblesNo ratings yet
- Prelim 118 NotesDocument6 pagesPrelim 118 NotesMicah Huns San JuanNo ratings yet
- Seco Ndar Y HEM Osta SIS (Coa Gula Tion Fact OR) : Mucocutaneous - PetechiaeDocument7 pagesSeco Ndar Y HEM Osta SIS (Coa Gula Tion Fact OR) : Mucocutaneous - Petechiaea a r o n b a u t i s t aNo ratings yet
- Boards - Gen PathDocument12 pagesBoards - Gen PathJoyce EbolNo ratings yet
- Classification of AnaemiaDocument14 pagesClassification of AnaemiaAbdallah AlasalNo ratings yet
- F.04 Diseases of The HeartDocument7 pagesF.04 Diseases of The HeartPAUL ALINGKAYONNo ratings yet
- IM - Cardiomyopathy and MyocarditisDocument9 pagesIM - Cardiomyopathy and MyocarditisElisha BernabeNo ratings yet
- ISSVA Ijms-23-02358Document13 pagesISSVA Ijms-23-02358Henrique PeresNo ratings yet
- Transes HemaDocument4 pagesTranses HemaJainee Chen JavillonarNo ratings yet
- Renal Diseases NotesDocument4 pagesRenal Diseases NotesJanine CabreraNo ratings yet
- Unit Exam #1: Blood Vessels: B.) Advanced Glycation End ProductsDocument85 pagesUnit Exam #1: Blood Vessels: B.) Advanced Glycation End ProductsCherry RahimaNo ratings yet
- Krull 1985Document8 pagesKrull 1985Heba VerebceanNo ratings yet
- Pseudomonas: Situs Inversus, Due ToDocument12 pagesPseudomonas: Situs Inversus, Due ToAmulya ThotambailuNo ratings yet
- Pseudomonas: Situs Inversus, Due ToDocument12 pagesPseudomonas: Situs Inversus, Due ToAmulya ThotambailuNo ratings yet
- 2020 Pathology Compilation Questions by TopicsDocument7 pages2020 Pathology Compilation Questions by Topicsrupertgrint2000No ratings yet
- F.05 The HeartDocument7 pagesF.05 The HeartPAUL ALINGKAYONNo ratings yet
- Dilated Cardiomyopathy Notes AtfDocument15 pagesDilated Cardiomyopathy Notes AtfSingha ChangsiriwatanaNo ratings yet
- TID Dr. Lu 2014Document4 pagesTID Dr. Lu 2014MACATANGAY, GAELLE LISETTENo ratings yet
- Congenital Heart DefectsDocument6 pagesCongenital Heart DefectsJohiarra Madanglog TabigneNo ratings yet
- Cvspa02 Haemorrhage and ShockDocument6 pagesCvspa02 Haemorrhage and ShockRobert So JrNo ratings yet
- Chapter 147:: Vascular Malformations:: Laurence M. Boon, Fanny BallieuxDocument33 pagesChapter 147:: Vascular Malformations:: Laurence M. Boon, Fanny BallieuxJhauharina RfNo ratings yet
- Chest Radio 8 Widening of The MediastinumDocument14 pagesChest Radio 8 Widening of The Mediastinumlonsilord17No ratings yet
- Nutritional DisordersDocument3 pagesNutritional Disordersmanar.alaneziNo ratings yet
- Rheumatology Quiz.8Document1 pageRheumatology Quiz.8Ali salimNo ratings yet
- Atherosclerosis WanDocument7 pagesAtherosclerosis WanEliud Florentino MolinaNo ratings yet
- ATHEROSCLEROSISDocument4 pagesATHEROSCLEROSISMARYHAN M MUKHALALATINo ratings yet
- Hema 2 - Prelim Topic 3 - Platelet Disorders and Laboratory TestsDocument8 pagesHema 2 - Prelim Topic 3 - Platelet Disorders and Laboratory TestsLowenstein JenzenNo ratings yet
- Cancer BulletsDocument3 pagesCancer Bulletsraquel maniegoNo ratings yet
- 04 SST Hemodynamic DerangementsDocument1 page04 SST Hemodynamic DerangementsFranz LibreNo ratings yet
- Renal Tubular Acidosis: BY DR/ Mohammad Hassan Mostafa Ass - Prof. Internal Medicine & NephrologyDocument34 pagesRenal Tubular Acidosis: BY DR/ Mohammad Hassan Mostafa Ass - Prof. Internal Medicine & NephrologyYoussef Refaat RaoofNo ratings yet
- Differential Diagnosis of StrokeDocument2 pagesDifferential Diagnosis of StrokeAnonymous 7dsX2F8nNo ratings yet
- Blood & HaematologyDocument12 pagesBlood & HaematologySagor DeyNo ratings yet
- Errata PathomaDocument1 pageErrata PathomaKumar ShivamNo ratings yet
- MBR 2019 - Pathology HandoutsDocument98 pagesMBR 2019 - Pathology HandoutsRgm UyNo ratings yet
- Patho Magnus May 2023Document46 pagesPatho Magnus May 2023CC Samson, Caesar AnthonyNo ratings yet
- 1 s2.0 S1578219008703275 MainDocument10 pages1 s2.0 S1578219008703275 Mainavnish sharmaNo ratings yet
- Pancytopenia and BicytopeniaDocument12 pagesPancytopenia and BicytopeniaRonny DoankNo ratings yet
- Definition of Stroke: Risk FactorsDocument12 pagesDefinition of Stroke: Risk FactorsNik Fatnin YusoffNo ratings yet
- Hydro CortisoneDocument3 pagesHydro Cortisonepaninay17No ratings yet
- Cardiomiopatia HEARTDocument6 pagesCardiomiopatia HEARTSofia SimpertigueNo ratings yet
- PLT DisordersDocument3 pagesPLT DisordersAudreySlitNo ratings yet
- Renal Pathology - 012) Nephrotic Syndrome (Notes)Document10 pagesRenal Pathology - 012) Nephrotic Syndrome (Notes)hasanatiya41No ratings yet
- Cryoglobulinaemia Occlusive Vasculopathy From Multiple MyelomaDocument3 pagesCryoglobulinaemia Occlusive Vasculopathy From Multiple MyelomaWei Sheng ChongNo ratings yet
- Ciulla HemastasisDocument12 pagesCiulla HemastasisLancer BlazeNo ratings yet
- Para Pre 2 Merged 1 1Document87 pagesPara Pre 2 Merged 1 1Lancer BlazeNo ratings yet
- Ciulla HemastasisDocument12 pagesCiulla HemastasisLancer BlazeNo ratings yet
- QUIZ 1 TO 4 RECALLS CombinedDocument13 pagesQUIZ 1 TO 4 RECALLS CombinedLancer BlazeNo ratings yet
- Laboratory Manual in Parasitology 2021Document62 pagesLaboratory Manual in Parasitology 2021Lancer BlazeNo ratings yet
- Para Extension RecallsDocument9 pagesPara Extension RecallsLancer BlazeNo ratings yet
- MLS 322 INTRO TO HEMOSTASIS STUDENT COPY - MegakaryopoeisisDocument25 pagesMLS 322 INTRO TO HEMOSTASIS STUDENT COPY - MegakaryopoeisisLancer BlazeNo ratings yet
- Hema 2 Lec - M2 Updated 01Document12 pagesHema 2 Lec - M2 Updated 01Lancer BlazeNo ratings yet
- CH 10Document1 pageCH 10Lancer BlazeNo ratings yet
- Gesc 112Document10 pagesGesc 112Kalpavriksha1974No ratings yet
- 01 Abstract ArgaDocument1 page01 Abstract ArgateranagargaNo ratings yet
- Osmosis: The Condition Is NormalDocument4 pagesOsmosis: The Condition Is NormalVince RetutaNo ratings yet
- NCERT Short Notes - Science & TechnologyDocument38 pagesNCERT Short Notes - Science & Technologyvishal.may256No ratings yet
- Student Exploration: MeiosisDocument8 pagesStudent Exploration: MeiosisAshtyn CurnowNo ratings yet
- Complete blood count, CBC With Diff. and blood lm: B10845383 International Medical Center 20.5.2021 2:28 ًءﺎﺴﻣDocument6 pagesComplete blood count, CBC With Diff. and blood lm: B10845383 International Medical Center 20.5.2021 2:28 ًءﺎﺴﻣNizar AlharbiNo ratings yet
- Materi 2 - Prof. Dr. Amin Soebandrio, PH.D., SP - MKDocument27 pagesMateri 2 - Prof. Dr. Amin Soebandrio, PH.D., SP - MKChristina100% (1)
- Cases of CherubismDocument7 pagesCases of CherubismSadia GullNo ratings yet
- Research PaperDocument13 pagesResearch Paperapi-608512616No ratings yet
- 91155-2 3 ExemplarsDocument16 pages91155-2 3 Exemplarsapi-324594246No ratings yet
- Journal of Bodywork & Movement TherapiesDocument6 pagesJournal of Bodywork & Movement TherapiesGabrielDosAnjosNo ratings yet
- Chapter - Iv Conceptual Background On Customers PerceptionDocument27 pagesChapter - Iv Conceptual Background On Customers PerceptionMatachi MagandaNo ratings yet
- Lab Practical Exam 2 InstructionsS21Document14 pagesLab Practical Exam 2 InstructionsS21jashanpreetNo ratings yet
- Biotechnology in Healthcare - An Introduction To Biopharmaceuticals (PDFDrive)Document249 pagesBiotechnology in Healthcare - An Introduction To Biopharmaceuticals (PDFDrive)AddicoNo ratings yet
- Dissertation EpigeneticsDocument5 pagesDissertation EpigeneticsSomeoneWriteMyPaperWashington100% (1)
- Robotics SyllabusDocument52 pagesRobotics SyllabusManoj Kumar100% (1)
- Biochemical Changes in Raw FoodDocument39 pagesBiochemical Changes in Raw FoodBinardo AdisenoNo ratings yet
- Bs Merged SearchableDocument90 pagesBs Merged SearchableShomak BakshiNo ratings yet
- Cell Quiz 1Document8 pagesCell Quiz 1CHRISTOPHER SCALENo ratings yet
- Chapter 2 - AntigenDocument6 pagesChapter 2 - AntigenAngelica Joy GonzalesNo ratings yet
- Endosymbiotic Theory Reference - Martin Et Al, 2015 PDFDocument18 pagesEndosymbiotic Theory Reference - Martin Et Al, 2015 PDFsoham deolankarNo ratings yet
- Age, Gender, and Muscular Strength - Ben F. HurleyDocument4 pagesAge, Gender, and Muscular Strength - Ben F. HurleyOz FalchiNo ratings yet
- RocheCARDIACTroponinT 07007302190 V2 CAN ENDocument3 pagesRocheCARDIACTroponinT 07007302190 V2 CAN ENPrince KatariyaNo ratings yet
- G11 Bio2 WS1 Inheritance PatternsDocument1 pageG11 Bio2 WS1 Inheritance PatternsArlance Sandra Marie MedinaNo ratings yet