Professional Documents
Culture Documents
12 Cranial Nerves and Assessment
Uploaded by
Rella QuelOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
12 Cranial Nerves and Assessment
Uploaded by
Rella QuelCopyright:
Available Formats
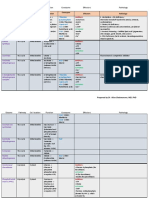
12 Cranial Nerves and Assessment 1)Nerve:Olfactory( I ) Type:Sensory Function:Sense of smell Test: Youll need three substances with distinctive
but familiar odors; for example, coffee, tobacco, and cloves. Ask your patient to close his or her eyes, and occlude her left nostril with her finger. Hold one of these substances under his / her right nostril, and ask her to identify the odor. Follow the same procedure with the other two substances. Then, repeat the entire test on the other nostril. Normal findings: Patient detects and correctly identifies all three odors. Possible causes of abnormalities: Temporary impairment from common cold; head trauma resulting in Parosmia (perversion of sense of smell); compression of Olfactory bulb by meningiomas or anterior fossa aneurysm; tumor infiltration in frontal lobe; or temporal lobe lesions, resulting in Olfactory hallucinations. 2)Nerve:Optic( II ) Type:Sensory Function:Vision Test: Visual acuity Use Snellen chart or an E chart to test your patients visual acuity. Normal Findings:Patients vision fields should be approximately the same as your own ( provided your own vision is normal ). Test: Internal eye structure Examine your patients eyes with an opthalmoscope. Normal Findings:Optic disc appears yellowish-pink and is round or oval, with clearly defined edges. Fundus appears uniformly orange, with optic disc located one side. Blood vessels extend outward from optic disc along borders of the fundus. Possible causes of abnormalities: Optic neuritis, toxic substances ( fro example, alcohol abuse ), head trauma, chronic nephritis, Diabetes mellitus, anemia, nutritional deficiencies, multiple sclerosis, chronic hypertension, intracranial tumors or aneurysms, or increased intracranial pressure.
(2 ) 3)Nerve/s: Oculomotor( III ) Type: Motor
Trochlear( IV ) Abducens( VI )
Function: Oculomotor:Innervates extrinsic eyemuscles and ciliary muscle Trochlear :Innervates superior oblique muscle Abducens :Innervates external rectus muscle Important:These three (3) nerves operate as a unit and should be tested and evaluated together. Test: Extrinsic Eye muscles Ask the patient to open his or her eyes. Instruct him or her to focus on a point directly in front of him / her. Observe her ability to focus on one point effectively. Normal Findings:Lower edges of lids meet bottom edges of irises; upper lids cover approximately 2mm of irises. Test: Direct papillary response Carefully note each pupils size. Darken the room, and check your patients eyes with a penlight. To do this, shine the light directly into one of your patients pupils, as she keeps his / her other eye closed. Note the pupils reaction. Then, check the other eye. Normal Findings:Pupils constrict and remain constricted with light; pupils dilate when light is removed. Test: Consensual papillary responses Darken the room, but make sure your patient keeps both eyes open. Position the penlight directly in front of his / her right eye. Turn the penlight ON, and observe the reaction of his or her left pupil. Then, check the other eye. Normal Findings:Pupils constrict bilaterally and remain constricted with light. Test: Extraocular eye movement Begin by familiarizing yourself with the six cardinal fields of gaze. As you know each of these fields corresponds to one of your patients extraocular muscles. Check the field separately. First, hold a pencil 12 (30 cm.) in front of your patients nose. Ask your patient to hold his / her head still and follow the pencils movement with his / her eyes. Then, slowly move the pencil to your right side, then to your left, then, when the pencils approximately 24 ( 60 cm) from your starting point, or your patients eye movement stops ( in either or both eyes ), hold the pencil still. Note the position of theiris in relation to each eyes midline. Repeat this procedure, checking each vision field separately. (3) Normal Findings:Eyes move smoothly and bilaterally in six cardinal fields of gaze. Test: Accommodation and Convergence First, hold a pencil approximately 18 ( 45 cm ) in front of your patients nose. Then, ask her to watch the pencil as you move it. Instruct him or her to keep his / her head and eyes stationary
throughout the examination. Then, slowly move the pencil toward the bridge of his / her nose. If everythings OK, both your patients eyes will converge on the pencil at the same level and distance. At that point, expect his / her pupils to constrict and remain constricted. When the pencils 2 to 3 ( 5 to 7.6 cm.) from the bridge of his / her nose, your patient should be able to comfortably hold her gaze. Document all findings in your nurses notes. Normal Findings:Both eyes converge on pencil at same level and distance. Patient maintains gaze on pencil when its held 2 to 3 ( 5 to 7.6 cm.) from the bridge of his / her nose. When your patients eyes converge, both of her pupils constrict and remain constricted. Abnormal findings in Oculomotor ( III ) nerve damage: Lid ptosis, with inability to completely open eye; eyeball deviated outward and slightly downward; pupil dilated and unreactive to light; nystagmus, and accommodation power lost. Abnormal findings in Trochlear ( IV ) nerve damage: Inability to turn eye downward or outward. Abnormal findings in Abducens ( VI ) nerve damage: Eyeball deviated inward, diplopia, paralysis of lateral gaze. Possible causes of abnormalities: Trauma, multiple sclerosis, tumor or aneurysm at base of skull, increased intracranial pressure, botulism, or lead poisoning. 4)Nerve:Trigeminal( V ) Type:Motor; Sensory Function:Chewing movements by innervation of masseter, temporal, and pterygoid muscles; corneal and sneezing reflexes; and sensations of face, scalp, and teeth. Test: Masseter muscle strength Instruct your patient to clench her teeth tightly. As he or she does,locate and palpate the masseter muscle bulges at his / her right andleft jaw joints. Compare them. (4 ) Normal Findings:Patient can clench teeth tightly. Masseter muscles bulge when teeth are clenched. On palpation, both masseter muscles feel equal in size and strength. Test: Temporal muscle strength Instruct your patient to clench his or her teeth tightly. As he or shedoes, locate and palpate the temporal muscles at his or her temples.Compare them. Normal Findings:Patient can clench his / her teeth tightly. On palpation, temporal muscles feel equal in size and strength. Test: Pterygoid Muscle strength
Instruct your patient to clench his or her teeth. Ask your patient to resist your efforts to open his or her jaws. Then, grasp his or her lower jaw with one hand, and pull downward. Normal Findings:Patient keeps teeth tightly clenched, despite your efforts. Test: Corneal reflex Instruct your patient to look up. Gently touch a cotton wisp to her right cornea. Repeat the test on her left cornea. Note: if your patient wears contact lenses, her corneal reflexes may be diminished. Normal Findings:Patient blinks and his or her eyes tear when corneas touched. Test: Facial sensation Instruct your patient to close her eyes. Gently touch the point of a pin to one side of his or her forehead. Ask him or her to tell you what she feels, and when and where she feels it. Wait about 2 seconds, then repeat the test on the opposite side of the forehead. Next, repeat the test, using the blunt end of the pin. Finally, try the entire test ( both ends of pin ) on both sides of your patients cheeks and jaw. Compare all findings. Normal Findings:Patient identifies the same sensation bilaterally, and tells when and where she feels it. Test: Temperature sensation To test your patients hot / cold perception, to do this, fill one test tube ( or bottle ) withhot water and another test tube ( or bottle ) with cold water. Then, touch the one filled with hot water to your patients face. Hold it there for about 1 second. Then, touch the cold one to his or her face for about 1 second. (5 ) As you do, ask your patient to tell you what temperature she feels and where she feels it. Note any difficulty she has distinguishing hot from cold. Using the same technique, alternately test his or her other body parts, varying test locations. Be sure to document test location, test performed, and the result. Normal Findings:Patient identifies the same sensation bilaterally, and tells when and where she feels it. Possible causes of abnormalities: Trauma, tic douloureux ( Trigeminal Neuralgia ), intracranial tumor, menigeal infection, intracranial aneurysm; when only
descending tract is affected, syringobulbia ( cavities in medulla oblongata ) and multiple sclerosis. Also, pons lesion produces masticatory muscle paralysis and light touch sensation loss in face. Medulla lesion affecting descending tract causes pain and produces loss of temperature sensation and corneal reflex. 5)Nerve:Facial( VII ) Type:Motor Function: Facial expression, taste ( anterior 2/3 of the tongue ), and salivary and lacrimal gland innervation. Test: Lower portion of the facial nerve Observe your patients face at rest and during conversation. Instruct him or her to purse his or her lips, smile, and frown. Normal Findings:Symmetrical facial contours, lines, wrinkles; symmetrical facial movement. Test: Lower portion of the facial nerve Instruct your patient to puff out his or her cheeks and resist your efforts to collapse them. Normal Findings:Patient retains puffed cheeks despite your efforts to collapse them. Test: Upper portion of the facial nerve Ask your patient to close her eyes and resist your efforts to open them. Normal Findings:Patient resists efforts to open her eyes. (6 ) Test: Taste sensation on anterior 2/3 of tongue Wet cotton swabs in each of the following solutions: sugar (sweet), lemon juice ( sour ), saline ( salty ), quinine ( bitter ). Ask your patient to stick out her tongue. In turn, touch each swab to the front of her tongue, and ask her to identify the taste. Instruct your patient to rinse her mouth with water between tastes. Normal Findings:Patient correctly identifies sweet, sour, salty, and bitter tastes. Note: Remember, ability to taste may be inhibited by loss of sense of smell. Possible causes of abnormalities: Trauma to peripheral nerve branches, mastoid surgery complication, temporal bone fracture, intracranial tumor or aneurysm, meningitis, herpes zoster, Pagets disease ( a chronic disease of bones occurring in the elderly and most frequently affecting the skull, back bone, pelvis, and long bones. Affected bones becomes thickened and their structure disorganized: X-ray reveal patchy sclerosis. Severe continuous pain may result, which relieved by a prolonged course of Thyrocalcitonin injections.), and Bells Palsy. 6)Nerve:Acoustic( VIII ) Type:Sensory
Function:Hearing and sense of balance. Test: Air and bone conduction 1.Youll need a tuning fork in the C-Octave. Using a 256-Hertz tuning fork to perform the Weber, Rinne, Schwabach tests. By studying the results of these tests, a trained health-care professional can differentiate between a patient with normal hearing and a patient with a conductive or sensori-neural hearing loss. To ensure accurate results, you should perform each of these tests three separate times with 256-, 512-, and 1,024-Hertz tuning forks. However, this may not always be possible. 2.Before you begin a test, explain the testing procedure to your patient. Then, practice vibrating the tuning fork. Youll get the most accurate testing tone by gently hitting the fork against your fist, OR you may also get a tone by pinching the forks prongs together, OR by stroking the prongs upward. 3.To perform WEBER test. Begin by holding a vibrating 256Hertz tuning fork between your thumb and index finger. Touch the base of the tuning fork to your patients forehead. Then, ask your patient to describe the tone in each ear. If all is well, your patient will hear the same tone ( volume and intensity ) in each ear. In that case, youd document the result as Weber negative (7 ) If your patient hears the tone louder in one ear, ask him or her to point to the ear in which she hears the louder tone. Document the result Weber right or Weber left . 4.Next, youll perform the RINNEs test to evaluate your patients hearing by both bone and air conduction. First, ask your patient to mask the hearing in her left ear byrapidly moving his or her left fingertip in and out of his or herleft ear canal. To test your patients hearing by bone conduction, place the vibrating 256-Hertz fork against his or her right mastoid process. Your patient should hear the tone immediately. Ask him or her to tell you when she no longer hears the tone. Note the length of time she heard the tone. 5.Then, test his or her hearing by air conduction. Quickly (without re-vibrating the fork), place the prongs ( 1.3 cm.) from his or her right external ear canal, as the nurse is doing here. Make sure the prongs are in front but not touching the ear canal.
Ask your patient to tell you when she no longer hears the tone. Note the length of time she heard the tone. If everythings OK, your patient will hear the tone carried by air conduction twice as long as the tone carried by bone conduction. In this case, document the result as +R ( Rinne Positive ). Repeat the same procedure on your patients left ear. 6.Youll perform the Schwabach test to compare your hearing by bone conduction with your patients hearing by bone conduction. But remember, make sure your hearing is normal before you begin or the test wont be accurate. Ask your patient to mask the sound in her left ear, then, place a vibrating 256-Hertz tuning fork on his or her right mastoid process until she says she hears the sound. If alls well, she should say she hears the sound immediately. 7.Then, immediately mask the sound in yourleft ear, and place the fork on your right mastoid process. Listen for the sound. Continue to alternate the tuning fork between your patients mastoid process and your mastoid process. When either you or your patient stops hearing the tone, count the seconds the other continues to hear it. If both of you have normal hearing, youll stop hearing the tone at the same time. Repeat the test on your patients left mastoid process. If you suspect your patient has a hearing deficit, recommend she get an audiogram for a more accurate assessment. Always document the type of test you performed, the result, and the kind of tuning fork used, in your nurses notes. (8 ) Normal Findings:Equal hearing in both ears. Air conducted tone heard twice long in both ears as bone-conducted tone. Possible causes of abnormalities: Inflammation; intracranial tumor; drug toxicity, particularly from Aspirin, Quinine, or Streptomycin; middle fossa skull fracture. 7)Nerve/s: Glossopharyngeal( IX ) Vagus( X ) Types:Motor ; Sensory Function: Swallowing movements and saliva secretion. Gag and swallow reflexes. Sensation in the pharynx and larynx, as well as taste on posterior 1/3 of tongue. Also, autonomic innervation of heart, lungs, esophagus, and stomach. Important: these two nerves operate as a unit and should be tested and evaluated together. Test: Throat movement
Instruct your patient to open his or her mouth and say Ah. As he or she does, observe his or her uvula and soft palate. Normal Findings:When patient speaks, his or her uvula and soft palate move straight up. Test: Gag reflex Instruct your patient to open his or her mouth. As you depress his or her tongue with a tongue depressor, touch a cotton swab to either side of his or her pharynx. Normal Findings:Patient gags. However, remember that a weak gag reflex may be normal in an elderly patient. Test: Vocalization Ask your patient to speak or cough. Normal Findings:Patients voice clear and strong. Cough strong.. Possible causes of Glossopharyngeal ( IX ) nerve damage: Intracranial tumor or infection. Possible causes of Vagus ( X ) nerve damage: Acute anterior poliomyelitis, intramedullary lesions; syringobulbia, vascular lesions, amyotrophic lateral sclerosis, multiple sclerosis 8)Nerve:Spinal Accessory( XI ) Type:Motor Function:Innervates sternocliedomastoid and trapezius muscles. Test: Shoulder movement Stand facing your patient. Place your hands on his or her shoulders. Ask him or her to lift his or her shoulders as you apply moderate downward pressure.. Normal Findings:Patient lifts shoulder despite your downward pressure.. Test: Neck muscle strength Stand facing your patient. Place your left hand on the right side of your patients face. Instruct him or her to turn her head toward his or her right side, against your hands pressure. Repeat the procedure on the left side of her face. Normal Findings:Firm jaw pressure against your hand. Possible causes of abnormalities: Extrasmedullary tumors, occipital bone necrosis, inflammation, syringobulbia, amyotrophic lateral sclerosis, demyelinating diseases of the medulla. 9)Nerve:Hypoglossal( XII ) Type:Motor Function:Innervates tongue muscle. Test: Tongue movement Ask your patient to open his or her mouth, and observe his or her tongue at rest. Normal Findings:Tongue is motionless and centered on mouth floor. Test:
Tongue Movement Instruct your patient to stick out her tongue. Normal Findings:Protruding tongue appears centered between lips. Expect slight tongue movement. Test: Tongue strength Instruct your patient to press his or her tongue against one cheekwall. Apply fingertip pressure to outside of cheek as patient usestongue to resist pressure. Repeat test on other cheek. Normal Findings:Patient exerts firm tongue pressure against your fingertips. ( 10 ) Test: Tongue Movement Instruct your patient to dart his or her tongue in and out quickly. Then, ask him or her to stick his or her tongue out and move it from side to side as quickly as possible. Normal Findings:Fast, smooth tongue movement. Possible causes of abnormalities: Syringobulbia, amyotrophic lateral sclerosis, alcoholism, or CVA
You might also like
- Cranial Nerve Functions and Assessment MethodsDocument7 pagesCranial Nerve Functions and Assessment MethodsNewb TobikkoNo ratings yet
- 12 Cranial Nerves and AssessmentDocument10 pages12 Cranial Nerves and Assessmentapollo100% (17)
- Cranial Nerve AssessmentDocument8 pagesCranial Nerve AssessmentAllean Sarmiento Apolinario100% (1)
- Cranial Nerves Assessment: Prepared By: Eloisa M. Bonus, RN MANDocument56 pagesCranial Nerves Assessment: Prepared By: Eloisa M. Bonus, RN MANsarooah1994No ratings yet
- Examination of The Cranial Nerves: I OlfactoryDocument6 pagesExamination of The Cranial Nerves: I Olfactorygolagani praveenkumarNo ratings yet
- Assessment of The Nervous SystemDocument49 pagesAssessment of The Nervous Systemnovita100% (1)
- Neurological AssessmentDocument7 pagesNeurological AssessmentSharon LawrenceNo ratings yet
- HEENT Exam Teaching DocketDocument10 pagesHEENT Exam Teaching DocketJonah R. MeranoNo ratings yet
- Neuro ExamDocument25 pagesNeuro ExamkamalNo ratings yet
- Cranial NervesDocument65 pagesCranial Nervessarguss14100% (13)
- ASSESSMENT OF THE NERVOUS SYSTEM (230 NursDocument72 pagesASSESSMENT OF THE NERVOUS SYSTEM (230 Nursriya priyaNo ratings yet
- CRANIALDocument11 pagesCRANIALDemianaNo ratings yet
- Neurological ExaminationDocument58 pagesNeurological ExaminationMartin Ogbac100% (2)
- Neurological Assessment2Document14 pagesNeurological Assessment2Hana F. BarakatNo ratings yet
- HEENT ExamDocument7 pagesHEENT Examnz0ptkNo ratings yet
- Neurological AssessmentDocument13 pagesNeurological AssessmentJamaica Manuel IglesiasNo ratings yet
- Neuro Exam ReviewDocument6 pagesNeuro Exam ReviewDianne Flores100% (2)
- Kumuthamalar Cranial Nerve Examination (PCM)Document4 pagesKumuthamalar Cranial Nerve Examination (PCM)Andrew MaNo ratings yet
- Eye MethodsDocument28 pagesEye MethodsWaqar Ul HaqNo ratings yet
- Exercise 3 - Neuro, Cranial NervesDocument3 pagesExercise 3 - Neuro, Cranial NervesAubrey SungaNo ratings yet
- Neurological AssessmentDocument23 pagesNeurological AssessmentNavjot BrarNo ratings yet
- Neuro CN ScriptDocument7 pagesNeuro CN ScriptRay ChangNo ratings yet
- Sensory Examination and CoordinationDocument7 pagesSensory Examination and CoordinationFatimah Alsultan100% (1)
- Clinical Exam For OphthalmologyDocument6 pagesClinical Exam For Ophthalmologynuuraaisya50% (2)
- Checklist Eye ExaminationDocument7 pagesChecklist Eye ExaminationDiane100% (1)
- Canas, Patricia Gan, Razel Ruelo, Vanessa Aquino, Camile Guillano, Christabelle BSN IiiDocument73 pagesCanas, Patricia Gan, Razel Ruelo, Vanessa Aquino, Camile Guillano, Christabelle BSN IiiGan BangNo ratings yet
- Health Assessment ChecklistDocument14 pagesHealth Assessment ChecklistLindy JaneNo ratings yet
- Module 2 Physical AssessmentDocument8 pagesModule 2 Physical AssessmentEsvinch EsvinchNo ratings yet
- 06 EENT AssessmentDocument36 pages06 EENT AssessmentHerlinaNababanNo ratings yet
- Head and NeckkkkkkDocument7 pagesHead and NeckkkkkkJoey A. RumbaoaNo ratings yet
- (Murag Ga Tinan - Away Ra Ta Ani Na Part From # 1-4) : Appearance and BehaviourDocument3 pages(Murag Ga Tinan - Away Ra Ta Ani Na Part From # 1-4) : Appearance and BehaviourKaissa GomezNo ratings yet
- Neurological ExaminationDocument240 pagesNeurological Examinationramadan0% (1)
- Professional Skills Review Central Nervous System (CNS)Document25 pagesProfessional Skills Review Central Nervous System (CNS)Noora AlmuailiNo ratings yet
- Cranial Nerve ExaminationDocument9 pagesCranial Nerve ExaminationKorina AngelaNo ratings yet
- Neurologic Disorder: By: Sandot, Alfrien BDocument25 pagesNeurologic Disorder: By: Sandot, Alfrien BAlfrien Ivanovich LarchsonNo ratings yet
- See Also: Rinne/Webber With Left-Ear DeafnessDocument19 pagesSee Also: Rinne/Webber With Left-Ear DeafnessSri Sri WahNo ratings yet
- Cranial Nerve Exam RoutineDocument9 pagesCranial Nerve Exam Routine5kqmn798rfNo ratings yet
- Neurologic ExaminationDocument116 pagesNeurologic ExaminationMikylla OrdanielNo ratings yet
- Assessment of EyeDocument34 pagesAssessment of Eyeraima ayazNo ratings yet
- Eye AssessmentDocument7 pagesEye AssessmentPuviyarasiNo ratings yet
- Neuro PEDocument36 pagesNeuro PEkhaderbasha2020No ratings yet
- Lab Manual Human physiology-IIDocument32 pagesLab Manual Human physiology-IIAKASHDEEP SINGHNo ratings yet
- Cranial-Nerve-Examination Copy Copy-1Document27 pagesCranial-Nerve-Examination Copy Copy-1cvmqx7yppdNo ratings yet
- Assignment of Neurology (Repaired) .Docx - 1494344936467Document24 pagesAssignment of Neurology (Repaired) .Docx - 1494344936467Amrit Preet KaurNo ratings yet
- Cranial Nerve Examination 1Document17 pagesCranial Nerve Examination 1Salsabeel SalamahNo ratings yet
- Cranial Nerve StepsDocument5 pagesCranial Nerve StepsRonaldoNo ratings yet
- Ophtha PEDocument4 pagesOphtha PEChristian Edward MacabaliNo ratings yet
- Ophthalmology Osce Exam - PPTX PP by Abel - 230170110143Document86 pagesOphthalmology Osce Exam - PPTX PP by Abel - 230170110143Chefera Aga100% (1)
- MRCP Paces ManualDocument47 pagesMRCP Paces ManualAli AlisonNo ratings yet
- Neurologic Disorder: By: Sandot, Alfrien BDocument117 pagesNeurologic Disorder: By: Sandot, Alfrien BAlfrien Ivanovich LarchsonNo ratings yet
- Neurologic Disorder: By: Sandot, Alfrien BDocument118 pagesNeurologic Disorder: By: Sandot, Alfrien BNeirfla WassabiNo ratings yet
- Examination of Cranial NervesDocument61 pagesExamination of Cranial NerveshelenthongNo ratings yet
- Cranial Nerve AssessmentDocument5 pagesCranial Nerve AssessmentBAdz TanNo ratings yet
- CNS Cranial NervesDocument4 pagesCNS Cranial Nervesdenise joyce19No ratings yet
- Anatomy of The Eye EYE: Extaocular StructuresDocument5 pagesAnatomy of The Eye EYE: Extaocular StructuresfLOR_ZIANE_MAENo ratings yet
- Cranial Nerve ExaminationDocument6 pagesCranial Nerve ExaminationAlthea Aubrey AgbayaniNo ratings yet
- Heart of the Field "Refresher & Nha Certification Quick Notes"From EverandHeart of the Field "Refresher & Nha Certification Quick Notes"No ratings yet
- OHNS--Otolaryngology; Head and Neck surgery: pocket field guideFrom EverandOHNS--Otolaryngology; Head and Neck surgery: pocket field guideNo ratings yet
- 44transboundary Environmental Issues Intra-ASEANZoonotic Diseases Affecting TDocument4 pages44transboundary Environmental Issues Intra-ASEANZoonotic Diseases Affecting Ttanmaya_purohitNo ratings yet
- PCV Vaccine ProfileDocument6 pagesPCV Vaccine ProfileLhemmuel FiestaNo ratings yet
- Module 6 - Case Study Exercise Gastroenteritis at A College: Learning ObjectivesDocument9 pagesModule 6 - Case Study Exercise Gastroenteritis at A College: Learning ObjectivesdlsajdlkasNo ratings yet
- Physicians Desk Reference 2016 UnicityDocument6 pagesPhysicians Desk Reference 2016 UnicityJey BautistaNo ratings yet
- MGA VACCINE NA SAKOP NG NIP: BCG Birth Dose, Hepatitis B Birth Dose, OralDocument3 pagesMGA VACCINE NA SAKOP NG NIP: BCG Birth Dose, Hepatitis B Birth Dose, OralVanessa AbboudNo ratings yet
- Adolescent History and Physical Examination FormDocument10 pagesAdolescent History and Physical Examination Formjosephtimbol123No ratings yet
- Ileus ObstructionDocument22 pagesIleus ObstructionfitrahNo ratings yet
- Oral Manifestation of Systemic DiseaseDocument137 pagesOral Manifestation of Systemic DiseaseJeff Burgess100% (4)
- ECG - NotesDocument33 pagesECG - NotesNaveen ChandanNo ratings yet
- Iji2013 151028Document8 pagesIji2013 151028Kershaun MathewNo ratings yet
- Ecologic Model - PTBDocument2 pagesEcologic Model - PTBGio_Bueno_7488No ratings yet
- Geriatric Dentistry-An Overview: April 2016Document4 pagesGeriatric Dentistry-An Overview: April 2016surya saputraNo ratings yet
- Ebook Shafers Textbook of Oral Pathology PDF Full Chapter PDFDocument67 pagesEbook Shafers Textbook of Oral Pathology PDF Full Chapter PDFmargaret.harrell973100% (25)
- BMLE Course (Pediatrics)Document52 pagesBMLE Course (Pediatrics)fasmekbakerNo ratings yet
- Important EnzymesDocument15 pagesImportant EnzymesErin HillNo ratings yet
- Glucose Tolerance TestDocument3 pagesGlucose Tolerance TestdechychyNo ratings yet
- 100 PhobiasDocument2 pages100 PhobiasD RICENo ratings yet
- Hip Fractures in Elderly - Shanojan ThiyagalingamDocument26 pagesHip Fractures in Elderly - Shanojan ThiyagalingamDr. Shanojan Thiyagalingam, FRCPC FACPNo ratings yet
- NatureCeuticals 2020 ProspectusDocument10 pagesNatureCeuticals 2020 ProspectusJamall EllisNo ratings yet
- Bowflex Xtreme 2 SE Home Gym ManualDocument92 pagesBowflex Xtreme 2 SE Home Gym ManualBest Home Gym100% (1)
- USMLE Preparatory Online Resource_ Effective Biochemistry and Genetics Teaching Relatively Short Time_Dr Kumar Ponnusamy Urea Cycle & Nitrogen Metabolism_ST Matthew's University School of Medicine 2010Document185 pagesUSMLE Preparatory Online Resource_ Effective Biochemistry and Genetics Teaching Relatively Short Time_Dr Kumar Ponnusamy Urea Cycle & Nitrogen Metabolism_ST Matthew's University School of Medicine 2010Dr Kumar Ponnusamy100% (1)
- Uterine ProlapseDocument17 pagesUterine ProlapseChe AinNo ratings yet
- Shoulder DystociaDocument9 pagesShoulder DystociaRorschach VargasNo ratings yet
- RhinosinusitisDocument45 pagesRhinosinusitisMuhammad Ade RahmanNo ratings yet
- Jurnal IDocument8 pagesJurnal II Gusti Ayu Agung YuliantiNo ratings yet
- From Pro-Inflammatory Molecules To The Brain's Resting-State Connectivity The Future of Clinical Diagnosis of DepressionDocument36 pagesFrom Pro-Inflammatory Molecules To The Brain's Resting-State Connectivity The Future of Clinical Diagnosis of DepressiondgavrileNo ratings yet
- Implementing Clinical Decision Support System Using Naïve Bayesian ClassifierDocument6 pagesImplementing Clinical Decision Support System Using Naïve Bayesian ClassifierEditor IJRITCCNo ratings yet
- Case Study FormatDocument11 pagesCase Study FormatDemecillo, NoelleNo ratings yet
- Clinical Classification of Cerebral PalsyDocument23 pagesClinical Classification of Cerebral PalsymiNo ratings yet
- Chapter 14 NotesDocument4 pagesChapter 14 NotesRhianon Annie McDowellNo ratings yet