0% found this document useful (0 votes)
43 views3 pagesRespiratory Therapy for Post-Surgical Patients
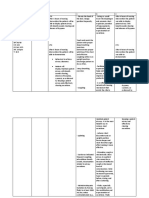
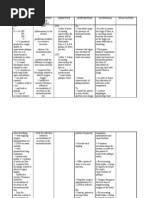
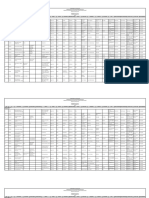
The document outlines a physiotherapy intervention plan for a patient experiencing respiratory distress, characterized by increased work of breathing, elevated respiratory rate, and ineffective cough. The plan emphasizes airway clearance techniques, breathing exercises, and functional mobility to improve respiratory function and manage fatigue. Additionally, it highlights the importance of continuous monitoring and addressing other relevant health issues impacting the patient's recovery.
Uploaded by
Dorota KabagambeCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as DOCX, PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
43 views3 pagesRespiratory Therapy for Post-Surgical Patients
The document outlines a physiotherapy intervention plan for a patient experiencing respiratory distress, characterized by increased work of breathing, elevated respiratory rate, and ineffective cough. The plan emphasizes airway clearance techniques, breathing exercises, and functional mobility to improve respiratory function and manage fatigue. Additionally, it highlights the importance of continuous monitoring and addressing other relevant health issues impacting the patient's recovery.
Uploaded by
Dorota KabagambeCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as DOCX, PDF, TXT or read online on Scribd