0% found this document useful (0 votes)
45 views38 pagesAnti-Hyperlipidemic Agents Overview
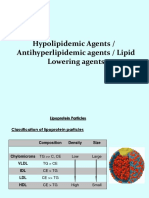
The document discusses anti-hyperlipidemic agents used to treat hyperlipidemia, a condition characterized by elevated lipid levels in the blood that increases cardiovascular disease risk. It covers various classes of medications, including statins, fibrates, bile acid sequestrants, and others, detailing their mechanisms of action and effects on cholesterol levels. Additionally, it provides information on the lipid profile, the differences between LDL and HDL cholesterol, and dietary factors influencing lipid levels.
Uploaded by
krishkoladiya152154Copyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
45 views38 pagesAnti-Hyperlipidemic Agents Overview
The document discusses anti-hyperlipidemic agents used to treat hyperlipidemia, a condition characterized by elevated lipid levels in the blood that increases cardiovascular disease risk. It covers various classes of medications, including statins, fibrates, bile acid sequestrants, and others, detailing their mechanisms of action and effects on cholesterol levels. Additionally, it provides information on the lipid profile, the differences between LDL and HDL cholesterol, and dietary factors influencing lipid levels.
Uploaded by
krishkoladiya152154Copyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PDF, TXT or read online on Scribd