Professional Documents
Culture Documents
Radiological Findings in Moyamoya Disease: P.N. Jayakumar M.K. Vasudev S.G. Srikanth
Uploaded by
Sudha RaniOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Radiological Findings in Moyamoya Disease: P.N. Jayakumar M.K. Vasudev S.G. Srikanth
Uploaded by
Sudha RaniCopyright:
Available Formats
RADIOLOGICAL FINDINGS IN MOYAMOYA DISEASE
P.N. Jayakumar M.K. Vasudev S.G. Srikanth
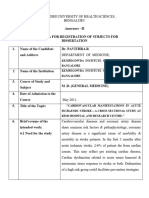
ABSTRACT The clinical, angiographic and computed tomographic features in eight children with Moyamoya disease were evaluated. The CT Scan findings were correlated with the angiographic features and the stage of the vascular disease. Stenosis/occlusion of the supraclinoid internal carotid artery (ICA) and the proximal parts of the anterior (ACA) and middle cerebral arteries (MCA) were the commonest angiographic findings". The cervical ICA was narrow in four patients, lnfarcts (100%), abnormal enhancement patterns (63%) and cerebral atrophy (88%) were the frequent CT scan findings. Although the CT scan findings did not correlate entirely with the angiographic and clinical findings, they were more frequently abnormal in later stages of the disease. The volume of Moyamoya increased progressively upto stage 3 of the disease only to decrease with further progression. The etiology of Moyamoya disease in Indian children is not clear. However, the clinical and radiological features are similar to that in the Japanese. Key words: Moyamoya disease, Computed tomography, Angiography, Brain infarction, Brain atrophy. From the Department of Neuraradiology, National Institute of Mental Health and Neurosciences, Bangalore 560 029. Reprint requests: Dr. P.N. Jayakumar, Department of Neuroradiology, NIMHANS, Bangalore 560 029. Received for publication: April 19, 1994; Accepted: October 12,1994
Moyamoya disease (MMD) has been reported frequently in the Japanese(l-6) with a few reports in non-Japanese populations(7-10). Moyamoya disease in children has been suggested to be distinct from that in adults(ll). The radiological features of MMD in children outside Japan are relatively undescribed(12). Moyamoya disease is an unknown cause of stroke in Indian children. Of a prospective study of 43 children with strokes from this institution, only 6 had Moyamoya disease(13). We report the angiographic and computed tomographic (CT) features in 8 Indian children with Moyamoya disease, seen at our centre over a period of six years. Material and Methods Angiograms and CT scans in 8 children with MMD were analyzed. Transfemoral selective serial external and' internal carotid angiography was done in 6 patients and two patients underwent direct antegrade puncture of the common carotid artery. Their ages ranged from 2 to 17 (mean = 7.5) years. The age at onset of the disease ranged from 1 to 11 (mean = 6.1) years. Detailed investigations including CSF analysis, blood sugar, VDRL, Lipid profile, rheumatoid factor and antinuclear factor were performed. Two patients underwent echocardiograms. The angiographic data from a total of 14 sides of the anterior circulation was analyzed. Each side was classified into 5 stages depending upon the degree of stenosis of the internal carotid artery (TCA) and proximal portions of the anterior (ACA) and middle cerebral arteries (MCA) (Table J)(2). They were also clas-
JAYAKUMAR ET AL.
RADIOLOGY IN MOYAMOYA DISEASE
sified into 6 stages of MMD depending upon the type and degree of collateral circulation (Table 7J)(12). The feeders to the basal Moyamoya disease were classified into those from the internal carotid artery (ICA) and the external carotid artery (ECA). The size of the Moyamoya blush was measured on the anteroposterior and lateral projections of the angiograms. The volume of the blush or abnormal network volume (ANV) was calculated as the product of the maximum dimensions of length, breadth and height. The CT scans were done on CGR ND-8000 scanner (4 patients) and Seimen's Somatom DR3 (4 patients). Section thickness varied between 5 mm to 10 mm depending upon the region of interest. Contrast scan was done after intravenous bolus injection of 2 ml/kg body weight of meglumine iothalamate
TABLE I-Progress of Stenosis of Moyamoya Disease (Suzuki and Takaku, 1989) Stage Stenotic/Occlusive features 1. 2. 3. 4. 5. Slight to moderate stenosis of TCA bifurcation Severe stenosis of ICA bifurcation Occlusion of ICA or MCA Occlusion of ICA or ACA and MCA, with partial retention of trunk of ACA/MCA Occlusion of ICA or ACA & MCA. Main trunk of ACA & MCA are not seen.
immediately prior to the scan. The scans were analyzed for infarcts, atrophy and abnormal enhancement. The CT and angiographic features were correlated with each other. The stage of ICA stenosis was correlated with the volume of abnormal vascular network on the same side. Results The clinical and radiological findings are shown in Table III. All the 8 patients showed cortical infarcts; the infarcts were bilateral in 6 and unilateral in 2. Deep ganglionic or white matter infarcts were seen in 5 patients (Fig. 1). The frontal, parietal and temporal lobes were commonly affected, while the occipital lobe was spared. Considering the hemispheres individually, 11 showed atrophy, either cortical, subcortical or both and 4 were normal. In one patient with an acute infarct, the presence and degree of the atrophy could not be assessed on the infracted hemisphere (Patient 2). Infarction on CT scan and
TABLE II- Classification of Basal Moyamoya
(Modified from Suzuki and
Kodama, 1983)
Stage 1. 2. 3. 4. 5. 6.
Angiographic features Narrowing of bifurcation of the internal carotid artery Initiation of basal Moyamoya Increase of Moyamoya. Obvious Moyamoya vessels at base of brain Decrease of Moyamoya Cross education of Moyamoya. All the main cerebral arteries are missing Disappearance of Moyamoya. Cerebral blood flow is only from external carotid artery
ICA- Internal carotid artery. ACA-Anterior cerebral artery. MCA-Middle cerebral artery. ICA Bifurcation--First portions of ICA, ACA and MCA
462
INDIAN PEDIATRICS
VOLUME 32-APRIL 1995
TABLE III - Clinical and Radiological Features in Mayamaya Disease Pt. No. 1 Age (Yr) 3 Sex F Duration of illness 2 weeks Clinical features Right hemiparesis 2 16 F 5 yr Quadriparesis
RCA
Angiographic findings
Angiographic stage stenosis 3 1 5 3 4 4
CT findings Infarcts both hem ipsheres; left cortical atrophy Infarcts both hemispheres Infarcts left hemisphere; bilateral subcortical atrophy Infarcts both hemispheres; bilateral cerebral atrophy Infarcts both hemispheres; right hem ispheric atrophy Infarcts both hem ispheres; bilateral cerebral atrophy Infarct left hem isphere; right cortical atrophy Infarcts both hem ispheres; bilateral cerebral atrophy
CI
LCA-
M2 occulusion stenosis
RCA - C1 occlusion
LCA
Al occlusion C1 stenosis
2 yr
M1 stenosis Left facio- RCA- C1 occlusion brachial M2 occlusion weakness LCA- C1 occlusion M2 occlusion Left hemi- RCAplegia and LCAaphasia C1 stenosis C1 occlusion M2 occlusion
17
12 yr
3 4
6mo
Quadriparesis
RCA - C1 occlusion
M1 stenosis LCA- C1 stenosis Ml occlusion RCA- C1 occlusion M1 stenosis LCA- C1 occlusion M2 occlusion RCA- Not done LCA- Cl stenosis M2 occlusion RCA- Cl stenosis LCA- Not done
4 4 5 5
10
4 yr
ParapMMis
2 days
Right hemiparesis Quadriparesis
3 2 -
6mo
RCA - Right carotid angiogram;
LCA
- Left carotid angiogram.
463
JAYAKUMAR ET AL
clinical deficits did not correlate in 2 patients (Patients 1 and 3). One patient had bilateral infarctions with unilateral deficits and the other had unilateral clinical deficits and ipsilateral infarction. A total of fourteen angiographic sides were analyzed and all of them, were abnormal. Of them, four sides were in angiographic stage 3, three sides were in stage 4 and three were in stage five (Figs. 2 & 3). The cervical ICA was narrow in 4 patients (8 sides). The stenosis of the ICA extended from the cervical to the supraclinoid portion (Fig. 4). Of the 8 patients with narrow ICAs, 7 patients had severe degree of basal Moyamoya. Collateral circulation was from both the ICA and ECA systems. Of the ICA collaterals, anterior falcine artery, ethmoidal branches and recurrent branches of the ophthalmic artery were the most frequent and seen in 65 to 75% of the patients. Predominent ECA collaterals were the anterior and posterior branches of the
VOLUME 32-APRIL 1995
angiographic stenosis Stages of IV and V showed infarction. Enhancement of the superficial cortex was seen across various stages of the disease (Stages II to V). However, abnormal intense enhancement of the basal ganglia was seen only in 2 patients in later stages of the disease (Stages IV and V). There was a distinct difference in the type of cerebral atrophy seen in different stages of the disease. While cortical atrophy (6 patients) was seen in patients from Stages I to V, subcortical atrophy (8 patients) was overwhelmingly seen in patients in Stages IV and V (75%). Involvement of the posterior circulation was seen in only 3 patients and in none of them was the CT scan demonstrative of any infarctions in the vertebrobasilar territory. Discussion The angiographic features which are previously described in children with MMD were corraborated in this study. They include narrowing/occlusions of the supraclinoid ICA and MCA with development of Moyamoya vessels in the base of the brain(2). Some of the features as yet unexplained include bilateral involvement of ICA, unpredictable rate of progression of the disease and spontaneous regression in later life(12). Though all the patients in the present study had evidence of bilateral disease on angiogram, the stage/severity of disease did not correlate with the scan in many patients. This disparity is probably due to the slow, asymmetric progression of the stenotic processes with development of extensive collaterals via the posterior and external carotid circulations.
465
middle meningeal artery and the superficial temporal artery and seen in 50 to 65% of the patients. The number and extent of collateral participation increased progressively with the severity of the disease. Correlating the scan abnormalities with the angiographic stage of the disease, the frequency of abnormalities on scan increased progressively with the stage of the disease. All the cerebral brain hemispheres with corresponding
JAYAKUMAR ET AL.
RADIOLOGY IN MOYAMOYA DISEASE
Reports of abnormal enhancement in the region of the basal ganglia are variable(4,14,15). Although differences in the technique of administration of contrast medium could be 3 factor(16), the severity of the disease is perhaps an important determinent. The fact that all of our patients with enhancement of the basal ganglia were in angiographic Stages IV and V, is suggestive. The volume of the Moyamoya (ANV) when correlated with the degree of stenosis of the ICA, showed progressive increase of both (upto Stage III). With further progression of the stenosis of the TCA (Stages IV and V), the volume of the Moyamoya dropped. ANV has been reported to be more extensive in children as compared to the adults(2). Results of the present as well as previous studies have shown ANV to be maximal in Stage III and to decrease with further progression of the disease(2,7,11,12,15). An interesting feature of our study was the presence of narrowing of both cervical ICAs in 4 patients. All these patients were in angiographic Stages IV and V. Since involvement of cervical ICA has not been described easier as feature of childhood MMD, it is possible that MMD as it occurs in the native Indian population may be different from that described in the Japanese(12). It is not clear from the present study but likely that the disease starts in the terminal part of the ICA and subsequently progresses distally to involve, the ACA and MCA and proximally to involve the cervical ICA. This is partly substantiated by the angiographic evidence of frequent and earlier involvement of the terminal part of ICA as compared to its
466
cervical part. There was no evidence of any systemic or cranial infection in any of our patients. CSF analyses and chest X-rays were normal and rheumatoid and antinuclear factors were negative. The presence of multiple cortical/ subcortical infarcts, abnormal enhancement of the basal ganglia on a background of supratentorial cerebral atrophy suggests MMD. The present study shows some degree of correlation between the angiographic stage of the disease and CT findings though neither correlates with the clinical stage of the disease. However, once the disease starts, the gross arterial changes suggest a progressive response of the intracranial vascular system to the underlying etiopathogenetic cause. Morphologically, there is no difference between the Japanese and the Indian children.
REFERENCES 1. Mishimoto 'A, Takeuchi S. Abnormal cerebrovascular network related to the internal carotid arteries. J Neurosurg 1968, 29: 255-260. Suzuki J, Takaku A. Cerebrovascular "Moyamoya" disease. Disease showing abnormal net-like vessels in the brain. Arch Neurol 1969, 20: 288-299. Takahashi M. Magnification angiography in Moyamoya Disease. Radiology 1980,136: 379-386. Takeuchi S, Kobayashi K, Tsuchida T, Imamura H, Tanaka R, Ito J. Computed tomography in Moyamoya disease. J Comp Axial Tomogr 1982, 6: 24-32. Miyamoto S, Kikuchi H, Karasawa J, Nagata I, Ikota T. Takeuchi S. Study of the posterior circulation in Moyamoya disease. Clinical and neuroradiological evaluation. J Neurosurg 1984, 61: 1032-1037.
2.
3.
4.
5.
INDIAN PEDIATRICS
VOLUME 32-APRIL 1995
6. Handa J, Handa H. Progressive cerebral arterial occlusive disease: Analysis of 27 cases. Neuroradiology 1972, 3:119-133. 7. Krayanbuhl HA. The Moyamoya syndrome and the neurosurgeon. Surg Neurol 1975, 4: 353-360. 8. Taveras JM. Multiple progressive intracranial arterial occlusions. A syndrome of children and young adults. Am J Roentgenol 1969,106: 235-268. 9. Lee MLK, Cheung EMT. Moyamoya disease as a cause of subarachnoid hemorhhage in Chinese. Brain 1973, 96: 623-628. 10. Meriwether RP, Barnett HG, Echos DH. Moyamoya disease as a cause of subarachnoid hemorrhage in a Negro patient. J Neurosurg 1976, 44: 620-622. 11. Satoh S, Shibuya H, Matsumisha Y, Suzuki S. Analysis of the angiographic findings in cases of childhood Moyamoya disease. Neuroradiology 1988, 30:111-119.
12. Suzuki J, Xadama N. Moyamoya diseaseA review. Stroke 1983, 14: 104-109. 13. Nagaraja D, Verma A, Taly AB, Veerendrakumar M, Jayakumar PN. Stroke in children. Acta Neurol Scand 1994, 90: 251-255. 14. Handa J, -Handa H, Nakano Y, et al. Computed tomography in Moyamoya: Analysis of 16 cases. Comp Axial Tomogr 1977,1:165-174. 15. Takahashi M, Miyauchi T, Kowada M. Computed tomography of Moyamoya disease, demonstration of occluded arteries and collateral vessels as important diagnostic signs. Radiology 1980, 134: 671-676. 16. Asari S, Satoh T, Sakurai M, Yamamoto Y, Sadomoto K. The advantage of coronal scanning in cerebral computed angiotomography for diagnosis of Moyamoya disease. Radiology 1982,142: 709-711.
467
You might also like
- Coronary Vasomotion AbnormalitiesFrom EverandCoronary Vasomotion AbnormalitiesHiroaki ShimokawaNo ratings yet
- MDCT Angiography Imaging Presentation of ALCAPA in Adults: Qinyi Dai, Biao LV, Zhaoqi ZhangDocument6 pagesMDCT Angiography Imaging Presentation of ALCAPA in Adults: Qinyi Dai, Biao LV, Zhaoqi ZhangRajesh SharmaNo ratings yet
- Articol Medico Legal Aspects AVMDocument9 pagesArticol Medico Legal Aspects AVMVoicu AndreiNo ratings yet
- F QRSDocument9 pagesF QRSaisyah hamzakirNo ratings yet
- 35fcthrombotic Occlusion of The Common Carotid Artery 1233912120856263 2Document19 pages35fcthrombotic Occlusion of The Common Carotid Artery 1233912120856263 2Ye HtunNo ratings yet
- Kang2008 ACA Infarction Patterns and ClinicsDocument8 pagesKang2008 ACA Infarction Patterns and ClinicsAlex DimanceaNo ratings yet
- Spontaneous Vertebral Artery Dissection: Report of 16 Cases: Original ArticleDocument7 pagesSpontaneous Vertebral Artery Dissection: Report of 16 Cases: Original ArticleAyu Yoniko CimplukNo ratings yet
- Short-And Long-Term Outcomes of Acute Upper Extremity Arterial ThromboembolismDocument4 pagesShort-And Long-Term Outcomes of Acute Upper Extremity Arterial ThromboembolismWilhelm HeinleinNo ratings yet
- Moya Moya DiseaseDocument87 pagesMoya Moya DiseaseDilip Kumar MNo ratings yet
- The Thoracic Anterior Spinal Cord Adhesion SyndromeDocument7 pagesThe Thoracic Anterior Spinal Cord Adhesion Syndromepaulina_810100% (1)
- Synopsis For DissertationDocument9 pagesSynopsis For DissertationahmedNo ratings yet
- 226-Article Text-717-3-10-20141213Document5 pages226-Article Text-717-3-10-20141213jasleen.jk92No ratings yet
- 1 s2.0 S0022510X13013646 MainDocument2 pages1 s2.0 S0022510X13013646 Mainfakhrusy rizqyNo ratings yet
- BMC NeurologyDocument8 pagesBMC NeurologyTarun MathurNo ratings yet
- Cortical Laminar NecrosisDocument4 pagesCortical Laminar NecrosisSulaiman Al SheikhNo ratings yet
- Cardiac ValveDocument9 pagesCardiac Valveikbal rambalinoNo ratings yet
- The Pattern and Prevalence of Vertebral Artery Injury in Patients With Cervical Spine FracturesDocument4 pagesThe Pattern and Prevalence of Vertebral Artery Injury in Patients With Cervical Spine FracturesFrontiersNo ratings yet
- Giant Coronary Artery Aneurysms in Kawasaki Disease Detected by Multi Detector Computed TomographicDocument3 pagesGiant Coronary Artery Aneurysms in Kawasaki Disease Detected by Multi Detector Computed TomographicVigoNo ratings yet
- Case Reports of Left Atrial Myxoma in Elderly and ChildrenDocument5 pagesCase Reports of Left Atrial Myxoma in Elderly and Childrenbri bugelNo ratings yet
- The Variations in The Circle of Willis On 64-Multislice Spiral Computed TomographyDocument7 pagesThe Variations in The Circle of Willis On 64-Multislice Spiral Computed TomographyTuNo ratings yet
- 586 2007 Article 345Document6 pages586 2007 Article 345pipitingesNo ratings yet
- Ctangiographyincomplexupperextremity Reconstruction: Keywords: CT Angiography, Upper Extremity ReconstructionDocument5 pagesCtangiographyincomplexupperextremity Reconstruction: Keywords: CT Angiography, Upper Extremity ReconstructionIrinel BuscaNo ratings yet
- Jurnal 20Document7 pagesJurnal 20Zella ZakyaNo ratings yet
- DEXTROCARDIADocument4 pagesDEXTROCARDIAamalia elisene mondoñedo sanchezNo ratings yet
- Hemimegalencephaly: A Study of Abnormalities Occurring Outside The Involved HemisphereDocument5 pagesHemimegalencephaly: A Study of Abnormalities Occurring Outside The Involved Hemisphereapi-148100258No ratings yet
- Nikus 2006Document5 pagesNikus 2006Robby Paguh TariganNo ratings yet
- Carotid JCPSP WaDocument4 pagesCarotid JCPSP Washakil11No ratings yet
- Disseccao Tipo b2Document6 pagesDisseccao Tipo b2coopervascba.diradmNo ratings yet
- HSDC CBC 2015Document5 pagesHSDC CBC 2015Bob sponjaNo ratings yet
- 1 s2.0 S0002870322002721 MainDocument12 pages1 s2.0 S0002870322002721 MainJuan ManuelNo ratings yet
- Acs 33 241Document9 pagesAcs 33 241Ratna AyieNo ratings yet
- Fatehihassanabad 2019Document4 pagesFatehihassanabad 2019Anna Sofía ParedesNo ratings yet
- Coronary Artery EcstasiaDocument4 pagesCoronary Artery EcstasiaAnestis FilopoulosNo ratings yet
- ECG in PneumoniaDocument5 pagesECG in PneumoniaDiah Rachmania ThalibNo ratings yet
- 182 FullDocument3 pages182 FullViona ApriliaNo ratings yet
- CME Article January 2017 PDFDocument7 pagesCME Article January 2017 PDFsheila dewantyNo ratings yet
- Outcome of Unroofing Procedure For Repair of Anomalous Aortic Origin of Left or Right Coronary ArteryDocument8 pagesOutcome of Unroofing Procedure For Repair of Anomalous Aortic Origin of Left or Right Coronary ArteryKrupa KarnikNo ratings yet
- Clinical and Imaging Outcomes After Stroke With Normal AngiogramsDocument4 pagesClinical and Imaging Outcomes After Stroke With Normal AngiogramsAgustina 'tina' HartutiNo ratings yet
- Coronary Slow FlowDocument8 pagesCoronary Slow FlowradiomedicNo ratings yet
- SCA Et Maladie de KawasakiDocument10 pagesSCA Et Maladie de KawasakiMame fatou DaboNo ratings yet
- Pseudonormalization: Clinical, Electrocardiographic, Echocardiographic, and Angiographic CharacteristicsDocument3 pagesPseudonormalization: Clinical, Electrocardiographic, Echocardiographic, and Angiographic CharacteristicspavithranmbbsNo ratings yet
- CazuriDocument4 pagesCazuriIbănescu Iulia AndreeaNo ratings yet
- Clinical Cases: Ischaemic Heart DiseaseDocument4 pagesClinical Cases: Ischaemic Heart DiseaseLADY JOWAHER ALLASNo ratings yet
- Brain/awq009 PDFDocument8 pagesBrain/awq009 PDFWafae TouchaNo ratings yet
- Pi Is 0003497505012002Document5 pagesPi Is 0003497505012002Tri RachmadijantoNo ratings yet
- Aicardi-Goutie'res Syndrome: Neuroradiologic Findings and Follow-UpDocument6 pagesAicardi-Goutie'res Syndrome: Neuroradiologic Findings and Follow-UpclaypotgoldNo ratings yet
- Chiari Malformations in Adults: A Single Centre Surgical Experience With Special Emphasis On The Kinetics of Clinical ImprovementDocument25 pagesChiari Malformations in Adults: A Single Centre Surgical Experience With Special Emphasis On The Kinetics of Clinical ImprovementBruno NdoumouNo ratings yet
- 2013 Adjustment of The Surgical Plan in Repair of Congenital Heart Disease - The Power of Cross-Sectional Imaging and Three-Dimensional VisualizationDocument6 pages2013 Adjustment of The Surgical Plan in Repair of Congenital Heart Disease - The Power of Cross-Sectional Imaging and Three-Dimensional Visualizationccvped3dNo ratings yet
- ICA AneurismDocument6 pagesICA AneurismnaimNo ratings yet
- Right Ventricular Function in Inferior Wall Myocardial Infarction: Case StudyDocument3 pagesRight Ventricular Function in Inferior Wall Myocardial Infarction: Case StudyIOSRjournalNo ratings yet
- Hemangiomas of The Head, Neck, and Chest With Associated Vascular and Brain Anomalies: A Complex Neurocutaneous SyndromeDocument11 pagesHemangiomas of The Head, Neck, and Chest With Associated Vascular and Brain Anomalies: A Complex Neurocutaneous SyndromeSILVA SINTIANo ratings yet
- Patients With St-Elevation Acute Coronary Syndrome in Young Aged PersonsDocument5 pagesPatients With St-Elevation Acute Coronary Syndrome in Young Aged PersonsCentral Asian StudiesNo ratings yet
- 34 DiscssionuDocument4 pages34 Discssionupokharelriwaj82No ratings yet
- Usefulness of Stent Implantation For Treatment ofDocument19 pagesUsefulness of Stent Implantation For Treatment ofAngel YapNo ratings yet
- 1 s2.0 S1010518216000652 Main PDFDocument9 pages1 s2.0 S1010518216000652 Main PDFRoberto AmayaNo ratings yet
- Inggris PDFDocument6 pagesInggris PDFChimul Lavigne 'L'No ratings yet
- BR Heart J 1985 Hartnell 392 5Document5 pagesBR Heart J 1985 Hartnell 392 5phng77No ratings yet
- Research On Post Reversible Encephalopathy Due To Blood TransfusionsDocument7 pagesResearch On Post Reversible Encephalopathy Due To Blood TransfusionsAnkit AgarwalNo ratings yet
- Kim 2019Document7 pagesKim 2019Edison Chiriboga OrtegaNo ratings yet
- Karnofsky Performance Status Scale - Karnofsky Performance Status ScaleDocument2 pagesKarnofsky Performance Status Scale - Karnofsky Performance Status ScaleNungkiNo ratings yet
- 2004 Yucha-Gilbert Evidence Based Practice BFDocument58 pages2004 Yucha-Gilbert Evidence Based Practice BFdiego_vega_00No ratings yet
- AcuteExpertSystem PDFDocument3 pagesAcuteExpertSystem PDFMMHMOONNo ratings yet
- Pediatric Head Trauma: PathophysiologyDocument5 pagesPediatric Head Trauma: Pathophysiologyherman76No ratings yet
- Oral SURGERY REVALIDA1Document27 pagesOral SURGERY REVALIDA1Bea Y. Bas-ongNo ratings yet
- Diagnosis and Management of Atypical Preeclampsia-Eclampsia: Obstetric Anesthesia Digest March 2010Document8 pagesDiagnosis and Management of Atypical Preeclampsia-Eclampsia: Obstetric Anesthesia Digest March 2010Fedrik Monte Kristo LimbongNo ratings yet
- Degloving Injuries of The Extremities and TorsoDocument20 pagesDegloving Injuries of The Extremities and TorsoRommy Shandy Saputra100% (1)
- DFP40182 Software Requirement and DesignDocument3 pagesDFP40182 Software Requirement and DesignTiyah BahariNo ratings yet
- TuberculosisDocument4 pagesTuberculosisHadish BekuretsionNo ratings yet
- s8. Partograph. ExerciseDocument44 pagess8. Partograph. ExerciseAngel ReyesNo ratings yet
- Sample Proposal 1 - DengueDocument8 pagesSample Proposal 1 - Dengueazliothman100% (1)
- AHA Scientific StatementDocument42 pagesAHA Scientific StatementepraetorianNo ratings yet
- Program and Proceedings - 11th International Regional "Stress and Behavior" Neuroscience and Biopsychiatry Conference (North America), June 22-24, 2017, Miami Beach, FL, USADocument49 pagesProgram and Proceedings - 11th International Regional "Stress and Behavior" Neuroscience and Biopsychiatry Conference (North America), June 22-24, 2017, Miami Beach, FL, USAISBS_SocietyNo ratings yet
- Acute Poststreptococcal GlomerulonephritisDocument58 pagesAcute Poststreptococcal GlomerulonephritisALI MUMTAZNo ratings yet
- The Reconstruction of Pink and White Esthetics: ClinicalDocument4 pagesThe Reconstruction of Pink and White Esthetics: ClinicalPreventiva HRACNo ratings yet
- Wellness Massage Q1 Mod 4Document21 pagesWellness Massage Q1 Mod 4Jea Caderao AlapanNo ratings yet
- Birth Plan TemplateDocument3 pagesBirth Plan TemplateCherry Savannah AbenojarNo ratings yet
- Head TraumaDocument4 pagesHead TraumaDinarkram Rabreca EculNo ratings yet
- Bl4ck - S4lve (Balm of Gilead)Document12 pagesBl4ck - S4lve (Balm of Gilead)Panther PantherNo ratings yet
- 603ca5b18c1d9 PANE Written - Sample QuestionsDocument11 pages603ca5b18c1d9 PANE Written - Sample QuestionsFazal ShahNo ratings yet
- Effects of Sexual AbuseDocument5 pagesEffects of Sexual AbuseFREEZIENo ratings yet
- Infection Control & Hospital EpidemiologyDocument7 pagesInfection Control & Hospital EpidemiologyJonNo ratings yet
- OligohydramniosDocument4 pagesOligohydramniossalamredNo ratings yet
- 12TH Postgraduate Course Program PDFDocument2 pages12TH Postgraduate Course Program PDFOliver VirataNo ratings yet
- MOH-National Antimicrobial GuidelinesDocument65 pagesMOH-National Antimicrobial GuidelinesHamada Hassan AlloqNo ratings yet
- Moh Cimu April 2020Document9 pagesMoh Cimu April 2020ABC News GhanaNo ratings yet
- Maternal Serum Alpha-Fetoprotein (MSAFP)Document2 pagesMaternal Serum Alpha-Fetoprotein (MSAFP)Shaells JoshiNo ratings yet
- Drug Study..Document4 pagesDrug Study..Micah SalesNo ratings yet
- Va Inspector Report 3Document100 pagesVa Inspector Report 3Jeff MorrisNo ratings yet
- Zyrtec: Tablet Core: Tablet CoatingDocument5 pagesZyrtec: Tablet Core: Tablet CoatingDwi WirastomoNo ratings yet