0% found this document useful (0 votes)
108 views4 pagesMental Status Examination
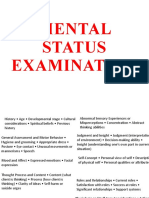
The Mental Status Examination (MSE) is a systematic assessment of an individual's psychological functioning, covering aspects such as appearance, behavior, thoughts, mood, speech, and cognition. It serves as a crucial tool in evaluating a person's mental state and determining the need for psychiatric follow-up, especially in cases of suicidal or homicidal ideation. The MSE includes various components that provide insights into a person's emotional state, thought processes, and overall mental health.
Uploaded by
kritikarajeswariCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as DOCX, PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
108 views4 pagesMental Status Examination
The Mental Status Examination (MSE) is a systematic assessment of an individual's psychological functioning, covering aspects such as appearance, behavior, thoughts, mood, speech, and cognition. It serves as a crucial tool in evaluating a person's mental state and determining the need for psychiatric follow-up, especially in cases of suicidal or homicidal ideation. The MSE includes various components that provide insights into a person's emotional state, thought processes, and overall mental health.
Uploaded by
kritikarajeswariCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as DOCX, PDF, TXT or read online on Scribd