0% found this document useful (0 votes)
15 views59 pagesLec 23
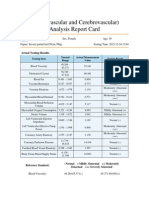
This lecture covers antihypertensive drugs, their classification, pharmacological properties, and effective management of hypertension. It discusses the pathogenesis and types of hypertension, including primary and secondary causes, as well as various classes of antihypertensive medications such as diuretics, beta-blockers, ACE inhibitors, and calcium channel blockers. The lecture also highlights the clinical uses, side effects, and contraindications of these medications.
Uploaded by
goopabbas94Copyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
15 views59 pagesLec 23
This lecture covers antihypertensive drugs, their classification, pharmacological properties, and effective management of hypertension. It discusses the pathogenesis and types of hypertension, including primary and secondary causes, as well as various classes of antihypertensive medications such as diuretics, beta-blockers, ACE inhibitors, and calcium channel blockers. The lecture also highlights the clinical uses, side effects, and contraindications of these medications.
Uploaded by
goopabbas94Copyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PDF, TXT or read online on Scribd