Professional Documents
Culture Documents
Histology Exam IV Review Part 1
Uploaded by
ashdmb217Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Histology Exam IV Review Part 1
Uploaded by
ashdmb217Copyright:
Available Formats
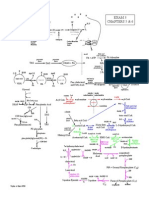
Respiratory
Olfactory Epithelium
Serous glands (secrete fluid)
Bipolar neurons
Immotile cilia with olfactory receptors
Respiratory Epithelium
Ciliated columnar cells: ciliated cells have a basal body
Goblet cells: secrete mucus
Brush cells: microvilli
Neuroendocrine (Kulchitskys) cells
Basal reserve cells
The Larynx
Stratified Squamous Epithelium
Only in the area of the vocal
cord is there wear and tear
which is why there is Stratified
Squamous Epithelium
C-shaped cartilage rings
Trachealis muscle holds together
Trachea 2
Hyalin cartilage
Trachea
Separation artifacts
Lumen ciliated epithelium
Submucosa glands
Serous glands
Hyalin cartilage
CT
No smooth muscle = trachea
Trachea
Submucosa
Submucosa glands
Connective Tissue
Respiratory epithelium
Missing band
of smooth
muscle
Hyalin Cartilage
Subdivisions of the Lungs
Lobes: right (3) left (2) containing
secondary bronchi
Bronchopulmonary segments containing
tertiary segmental bronchi
Acinus (Terminal Respiratory Unit)
Secondary lobules
Primary lobules
Airway and artery
Intrapulmonary Bronchus
Arises from subdivisions of primary bronchi
Muscosa (pseudostratified with goblet)
Muscularis
Mucosa
Cartilage
Islands
Intrapulmonary Bronchus
REP
Submucosal
glands
Muscularis mucosae
Hyaline
cartilage
Pulmonary
artery
Trachea
Submucosa glands
Fibroelastic lamina propia
No smooth muscle
Hyalin cartilage
Broncus
Cartilage arranged in islands
Submucosa glands
Smooth muscle present
Bronchiole
Loose cartilage, glands,
mucous producing cells
Submucosa increases
Clara cells present
Gas exchange airways
Hybrid: brochiole to a respiratory
bronchiole (bronchiole function and
also gas exchange)
Progresses into alveolar
Gartner 12-4-4 Bronchioles
Brochioles: No glands; No cartilage
Juinqueira 17-12 Clara cells
Found in epithelium in bronchioles
Have morphology of a protein secreting cell
Secrete bronchiole fluid to decrease surface
tension and also to detoxify
Bronchiole
Clara cells
have a dome
shaped apex
(causes them
to stick out
into the
lumen)
Pulmonary
artery (travels
with the
conducting
airway); carries
deoxygenated
blood
As you go further down the division, the walls become
thinner and less complicated
Respiratory ep.
Ciliated cells
The Respiratory Portion
Respiratory bronchiole: similar to terminal bronchiole, but wall
is interrupted by alveoli; contains ciliated, goblet, and clara cells
As R.B. divide, the number of alveoli increases, goblet
cells become absent, and cilias cells decrease in number
Alveolar duct
Alveolar sac
Alveolus
c
o
n
d
u
c
tin
g
re
s
p
ira
to
ry
conducting
respiratory
*
Elastic fibers
Respiratory bronchiole
Terminal bronchiole Alveolus Respiratory bronchiole
Bronchi, Bronchioles, Acini
Lobule = terminal
bronchiole and
everything attached
Acini = respiratory
bronchiole and the alveolar
sacs and alveoli attached;
multiple acini per lobule
Juinqueira 17-13 Terminal bronchiole
Terminal bronchiole
Last part of conducting passage before
respiratory system
Bronchiole. Alveolar duct, alveoli
Alveolar duct
Alveolar
Sac
Bronchiole: Alveolar duct, alveoli
Alveolar Cells
Type I: 97% of alveolar surface
Type II: Secretes surfactant which is packaged into
multilamellar bodies and reduces surface tension at air-
blood interface; contains lamellar bodies (lipid +
protein); have mitotic capacity
Pulmonary Defense Mechanisms
Secretions from the goblet cells, seromucous glands,
Clara cells, immune cells
Mucociliary clearance mechanism
Alveolar macrophages
Immune / Inflammatory Cells in the Interstitium
Macrophagesl Lymphocytes; Plasma cells etc.
Alveolar Wall
Type I and Type II Cells
Type II cells: make
surfactant
Dust cells:
alveolar
macrophages
Type I cells:
participate in
formation of air-
blood barrier
(stretch thin)
Air Blood Barrier
Air exchange
Gas exchange
Dust Cells
Lymphatics: Thin Walled Structure with dust cells and Macrophages
Pleura
Cubodial epithelium: gives
support but is not thick
BLOOD VESSELS OF THE LUNG
Pulmonary Arteries
Arise from the pulmonary trunk; leave the heart
Carry deoxygenated blood
**Run with conducting airways**
Low pressure, low resistance system
Thin walled
End as capillary networks
Pulmonary Veins
Run by themselves, not connected to conducting airway
Carry oxygenated blood
Goes back to the heart
Airway and blood vessels
Airway
Intrapulmonary Bronchiole Pulmonary artery
shares the connective
tissue
Pulmonary vein:
by itself;
swimming in a
sea of alveoli
Airway and artery
Airway
Artery
Pulmonary Artery
Pulmonary vein
Pulmonary Vein: swimming in a sea of alveoli
Vein
NUTRITIVE BLOOD VESSELS IN THE
LUNG
Bronchial Arteries & Veins
Start from thoracic aorta or posterior
intercostal arteries
Arteries carry oxygenated blood
Veins carry deoxygenated blood
Found within the walls of the
bronchial tree
Also supply the pleura
Urinary System
removal of waste products from blood
excretion of metabolic waste products in urine
regulation of ion concentration (Na
+
, K
+
, etc.)
regulation of acid-base balance
regulation of blood pressure (renin secretion)
regulation of erythrocyte production
(erythropoietin)
vitamin D metabolism & storage (parathyroid
hormone)
regulation of calcium levels (parathyroid
hormone)
heme bilirubin urobilin
Renal
artery
Interlobular
artery
Arcuate
artery
Interlobar
artery
RP
caylx
Renal
pelvis
M
Medullary
rays
C
lobules
Renal
pyramid
(lobe)
Segmental
artery
Renal
column (Bertin)
renal corpuscle =
glomerulus + Bowmans capsule
nephron =
renal corpuscle + tubule
(2 million/kidney)
uriniferous tubule =
nephron + collecting duct
(50 miles)
juxtamedullary
nephron
cortical
nephron
interlobar artery
interlobular
artery
efferent arteriole
afferent arteriole
arcuate artery
Bowman's capsule
proximal
convoluted
tubule
distal
convoluted
tubule
collecting duct
lo
b
u
le
lobule
cortex
medulla
glomeruli
lobule
Renal Corpuscles
only found in cortex;
contains the
glomerulus in the
center
*
*
lobule
medullary
ray
renal
corpuscle
interlobular artery
medullary
ray
medullary
ray
Afferent arteriole
Efferent arteriole
Cells:
-podocytes
-mesangial cells
-endothelial cells
Glomerulus
Bowmans capsule &
space (plasma from the
blood enters this space)
Mesangial cells:middle vessel
Support; phagocytosis; repair; contractile; EPO
synthesis (extraglomerular mesangial cells =
lacis cells)
GBM ~68,000 Kd allowed to pass:
podocyte
processes
combined basal
lamina
endothelial cell
fenestrations
capillary lumen
urinary space
-type IV collagen network
-laminin network
-proteoglycans
Glomerular filtration
Bowmans space
Most of the resorption of nutrients:
PCT small intestine
*most tubules are proximal convoluted
Resorption is a two-step process:
1) pump into extracellular space
2) pass into capillary lumen
Most of resorption of water:
DCT large intestine
Proximal
convoluted
Tubule
cell
Active
resorption:
Na
+
/K
+
-ATPase
pumps
water
Cl-
basal
infoldings
peritubular
capillary
Na+
amino acids
sugars
polypeptides
Passive
resorption:
enzyme-rich
glycocaylx
endocytic
vesicles
Resorption:
Distal
convoluted
Tubule
cell
Na
+
/K
+
-ATPase
(aldosterone sensitive)
active: Na
+
passive: water
peritubular
capillary
Renal Cortex
Renal corpuscles
DCT
PCT with
a brush
border
and filled
lumen
Renal
corpuscle
PCT and DCT
Medullary Rays
give circular profiles
Renal Cortex
PCT
DCT
DCT
DCT
VP
UP
Intralobular
(afferent)
arteriole enters
the vascular
pole
Urinary pole
collects into the
proximal conv.
tubule
Large amount of microvilli
Collecting Duct
Received partially concentrated urine at the distal end of the DCT
ADH (antidiuretic hormone) from pituitary: causes aquaporin
channels to open up, letting water move from lumen into
interstitum
Cells of the C.D. are impermeable to water in the absence
of ADH
Beer acts to negate ADH release
Diabetes (Gr. A siphon)
Diabetes insipidus:
inability to make or respond to ADH CD remain
impermeable to water
Diabetes mellitus:
insulin deficiency (osmotic diuresis); results in high
glucose in blood; offsets osmotic gradient resulting
in high water excretion
Ducts of bellini: ends of the collecting ducts
Collecting Ducts
Thick and thin parts of loop of henle
Vasa
recta
T thin loop of Henle
A Ascending thick limb of loop of Henle
V vasa recta
CD collecting duct
Blood Pressure Regulation
juxtaglomerular (JG) cells respond to arterial
pressure(baroreceptors); found in the wall of afferent
arteriole
Low pressure signals to JG cells to release renin to
increase BP
macula densa: responds to low salt
conc.(chemoreceptors); specialized cells of the DCT;
signal nearby JG cells to release renin
N
a
To increase blood pressure:
adrenal
cortex
Renin cleaves angiotensinogen
Angiotensin II is a potent
vasoconstrictor; also
increases sodium
resorption which increases
water resorption and thus
also BP
Transitional epithelium (urothelium)
stretched
relaxed
Pseudostratified epithelium
Cells larger at lumen surface; umbrella
shaped; may be binucleated
Cells
transition
and
become
more
stretched
out
Urinary bladder
Lined with transitional epithelium
Layers of
unorganized
muscle
Urinary Abbreviations to Know
PCT
DCT
JG cells/apparatus
ADH
ACE
Endocrine System
Ductless glands
Usually secrete hormones into bloodstream
Generally have systemic effects
Endocrine tissue exists in many "non-endocrine" organs:
mesangial & JG cells (EPO & renin) in kidney
enteroendocrine cells in gut, lung
Functions of hormones:
regulation of metabolism and energy balance
regulation of smooth and cardiac muscle contraction
regulation of glandular secretions
regulation of growth and development
regulation of 'flight or fight" responses and reproduction
Types of hormones:
Protein: prolactin, growth hormone, etc.
Peptide: ADH, calcitonin, etc.
water-soluble: bind to cell surface receptors, activate 2
nd
messengers etc.
Lipid-derived:
from cholesterol: steroid hormones (estrogen, glucocorticoids, etc.)
from eicosanoids: prostaglandins
lipid-soluble: diffuse through cell/nuclear membranes, bind to nuclear receptors to effect gene
expression
Monoamine:
derived from: phenylalanine, tyrosine, tryptophan thyroxine, melatonin, catecholamines, etc.
Pituitary portal system
(hypothalamic-hypophyseal portal system)
releasing
or
inhibitory TRH
(TSHRH)
From hypothalamus
thyrotropes
TSH made
and
released
from pituitary
this regulatory system affects primarily anterior pituitary cells
Portal system =
capillary bed
connected via veins to
another capillary bed
posterior lobe
unmyelinated axons &
supporting cells
Pituitary Anterior Pituitary
Much more cellular
3 distinct cell types
Poster Pituitary
Mostly axons
Herring bodies store
Neurosecretion: releases
a transmitter into a space
which then goes into the
blood
Pars intermedia
Residual of
rathkes pocket
pars distalis
Pars
intermedia
pars nervosa
Posterior Pituitary Anterior Pituitary
Rathkes pouch separates the
pars distalis from pars intermedia
Intermediate lobe (pars intermedia)
minimal/absent in humans
cysts
(remnants of
Rathke's pouch
Basophils
pars intermedia
posterior pituitary anterior pituitary
Acidophiles:
-somatotropes (50%, growth hormone growth of muscle, cartilage)
-lactotropes/mammotropes (15%)
(prolactin: mammary gland development, milk production, hypertrophy in multiparous women)
Basophils:
tropic hormones: act on other (distal) endocrine organs
-corticotropes (15%)
(adrenocorticotropic hormone, ACTH)
-thyrotropes (5%)
(thyroid stimulating hormone,TSH)
-gonadotropes (10%)
(follicle stimulating hormone, FSH &
leutinizing hormone, LH)
Chromophobes
-degranulated acidophils/basophils
-folliculostellate cells
-stem cells?
Anterior Pituitary Cell Types
Acidophils
Basophils
Chromophobes
Anterior Pituitary Cell Types
Brilliant Crystal Scarlet, Aniline Bl, Martius yellow
Anterior pituitary fenestrated capillaries
B
C
H & E
Chromophils: have an affinity for dye; either acidophils
(appear red) or basophils
Chromophobs: appear clear
Nerve terminals with
oxytocin-NI & ADH-NII
posterior pituitary
-hormones are coupled to neurophysin I & II
-axons terminate near blood vessels
(fenestrated capillaries)
-calcium release stimulates exocytosis
-one axon may have thousands of nerve terminals
-hormone product can be stored in Herring body
right above the nerve terminal
Neurosecretion
Hormones RELEASED:
oxytocin
1) smooth m. contraction
(uterus)
2) myoepithelial cell- cell
contraction (mammary gland)
ADH (vasopressin)
increases collecting duct
permeability
No ADH = diabetes incipits
Herring
bodies
Retina
Hypothalamus
& sympathetic
nervous system
Pineal
inhibition
light-stimulated
nerve impulse
norepinephrine
(darkness promotes hormone [melatonin] production)
melatonin functions:
-participates in circadian rhythms (sleep cycles)
-disregulation jet lag & SAD (treat with bright light)
-role in puberty ~possibly resulting inprecocious development
-powerful antioxidant
Pinealocyte
m
e
l
a
t
o
n
i
n
L L D D
tryptophan
fenestrated
capillary
Melatonin elevated
during sleep
(darkness) pineal
gland stimulated
Make
Melatonin
Thyroid
Lots of circular structures with homogenous
staining due to colloid (storage form of
precursor hormone thyroglobulin)
Only endocrine organ that stores its
hormone on outside of the cell
Homogeneous staining with dark staining
around indicating follicular epithelium
(single layer surrounding each follicle)
Setpa of CT divide into lobes
Thyroglobulin
iodinated glycoprotein
comprises the major colloid
component; extracellular storage
form of inactive thyroid hormone
colloid
follicular
cells
fenestrated
capillaries
Thyroid Gland Homogenous Staining
Colloid surrounded by single layer of follicular cells (flattened cubodial epithelium)
Production of thyroid hormone
follicular epithelium
capillaries
colloid
TSH (from pituitary) causes follicular cells
to synthesize Thyrogloblin in their RER,
which will be shuttled to and stored in the
colloid mass
Follicular cells also take up Iodide (I-)
from the blood stream into the cell
Storage form is iodinated tyrosine
Conjugation mechanism in colloid
T1 = general storage form
T3 = active thyroid hormone; can be
made in cells outside the thyroid
T4 = thyroxin = precursor molecule
that can only be made in the thyroid
Hyperthyroidism:
-due to Graves' disease:
-autoantibodies against TSH receptor
-weight loss, muscle weakness, sweating, increased apatite
-due to follicular adenoma (cancer) or pituitary adenoma (thyrotropes)
exophthalmos
Hypothyroidism:
-due to iodine deficiency, autoimmune, low pituitary TSH release
-poor muscle tone, fatigue, cold intolerance, weight gain
Iodine-deficiency Goiter
low thyroxine
increased
TSHRH from
hypothalamus
increased TSH
from pituitary
hypertrophy &
hyperplasia of
thyroid cells &
increased colloid
Enlarged lakes of colloid
Thyroid Gland Parathyroid Gland
Parathyroid Gland Thyroid Gland
Lakes of colloid; storage of precursor
(thyroglobulin) molecule for thyroid hormone
Thyroid Gland
Parathyroid Gland
Colloid
Lake
Dense CT capsule separates
Parathyroid from Thyroid
Fibroblast
nuclei
Parathyroid Gland
Oxiphil cells: dark central nucleus;
homogeneous pink staining cytoplasm
Fat
infiltration
THYROID: Parafollicular (C) cells
Clear cells on the side of the follicular; lies within the
epithelium but makes contact only with the basal surface
and blood vessels
Makes calcitonin
Lowers blood calcium levels by:
Decreasing osteoclast activity
Decreasing calcium absorption
Stimulates calcium deposition in bone
oxyphil
cells
oxyphil
cells
chief
cells
chief
cells
Parathyroid Gland
Mostly chief cells (making
parathyroid hormone)
Oxyphil cells: round, dark staining nucleus
and pink homogenous cytoplasm; found only
in the parathyroid and only appear at puberty
PARATHYROID: Chief Cells
Parathyroid hormone (PTH)
Stimulated by falling blood Ca levels
Increases blood calcium by:
Increasing osteoclast activity
Stimulating Vitamin D activation in kidney
Vitamin D stimulates Ca resorption in GI tract
and kidney
PTH opposes action of calcitonin, but only PTH is VITAL
Zona Glomerulosa
Round balls of cells surrounded by capillary beds
Thick clumps of cells not surrounded by a basement membrane
Thinnest
of the 3
cortex
layers
Beginning of the
Zona Fasiculata
With lipid droplets
Zona Fasiculata
Big cells, simple nucleus, lots of lipid droplets
Endothelial cell nuclei of blood vessels
Zona Fasiculata
Zona Reticularis
Eosinophilic cells with no
lipid droplet accumulation
Adrenal Gland
Supradrenal Gland
Zona Glomerulosa: under control of
Angiotensin II
Zona Fasciculita: responsive
to ATCH
Zona Reticularis: produces
gonadocorticoids
Medulla: modififed postganglionic
neurons that secrete epi & norepi into
the blood (modified neurosecretion);
norepi to epi change stimulated by
glucocortoids from cortex
Adrenal Gland
Adipocytes outside
of CT capsule
Dense CT Capsule
Zona Glomerulosa
Round balls of cells surrounded
by capillary beds
Part of the
Zona
Fasiculata
Adrenal Gland
Zona Reticularis
Zona Reticularis
Medulla
Large Veins with
longitudinally running
smooth muscle
ADRENAL CORTEX Hormone Production
Zona glomerulosa: mineralocorticoids (aldosterone)
Na2+ resorption in kidney, increases b.p.
controlled by Na+ & K+ levels, ACTH, and angiotensin II
promotes Na+ resorption & K+ excretion
Zona fasciculata: glucocorticoids (cortisol)
glucose metabolism (e.g. gluconeogenesis)
anti-inflammatory agent
controlled by ACTH
Zona reticularis: androgens (gonadicorticoids)
precursors for M & F sex hormones (DHEA
dehydroepiandrosterone converted to estrogen and
testosterone in ovaries & testes)
controlled by ACTH
ADRENAL MEDULLA Hormone Production
Chromaffin Cells
80% Epinephrine (adrenaline) [lighter cell]
20% Norepinephrine (noradrenaline) [darker cell]
Neuroendocrine cell derived from neural crest
Stimulated by endocrine system to release hormones
Target organ
adrenergic
(adrenaline, noradrenaline)
cholinergic
(acetylcholine)
Ch
adrenaline,
noradrenaline
(20:1)
Released directly into blood
1
st
1
st
2
nd
cholinergic
(acetylcholine)
Sympathetic neurons
(two-neuron chain):
( heart rate
blood pressure
-dilate bronchioles
-dilate coronary
arteries)
chromaffin
cell = postsynaptic neuron
Endocrine Abbreviations to Know
ACTH
ADH
FSH
GH
LH
PRL
PTH
T3/T4
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Brain 3Document3 pagesBrain 3Nurse Betty100% (1)
- Nurse Brain Sheet Telemetry Unit SBARDocument1 pageNurse Brain Sheet Telemetry Unit SBARashdmb217No ratings yet
- Room: - Name: - Code Status: - AllergiesDocument2 pagesRoom: - Name: - Code Status: - Allergiesashdmb217No ratings yet
- Room: - Name: - Code Status: - AllergiesDocument2 pagesRoom: - Name: - Code Status: - Allergiesashdmb217No ratings yet
- Student Clinical Report SheetDocument2 pagesStudent Clinical Report SheetMike100% (4)
- Maxwell Quick Medical Reference PDFDocument35 pagesMaxwell Quick Medical Reference PDFAnonymous fj68Ms100% (10)
- Clinical Experience "Tips"Document5 pagesClinical Experience "Tips"ashdmb217No ratings yet
- Adventitious Breath SoundsDocument1 pageAdventitious Breath Soundsashdmb217No ratings yet
- Medical TerminologyDocument13 pagesMedical Terminologyashdmb217No ratings yet
- SymbolsDocument1 pageSymbolsashdmb217No ratings yet
- Useful Spanish Words and PhrasesDocument32 pagesUseful Spanish Words and Phrasesashdmb217No ratings yet
- Nursing Management of The Perioperative PatientDocument16 pagesNursing Management of The Perioperative Patientashdmb217No ratings yet
- HCP FormDocument8 pagesHCP FormMarkNo ratings yet
- Information Regarding Family History DocumentDocument9 pagesInformation Regarding Family History Documentashdmb217No ratings yet
- Vitamin Chart.2Document3 pagesVitamin Chart.2ashdmb217No ratings yet
- Nutrition Review 2.3Document10 pagesNutrition Review 2.3ashdmb217No ratings yet
- Critical Care PhysiologyDocument287 pagesCritical Care Physiologyashdmb217100% (7)
- AbbreviationsDocument5 pagesAbbreviationsashdmb217No ratings yet
- Starting Out - New in The ICUDocument30 pagesStarting Out - New in The ICUashdmb217100% (1)
- Nutrition Review1.2Document12 pagesNutrition Review1.2ashdmb217No ratings yet
- Histology Exam IV Review Part 2Document26 pagesHistology Exam IV Review Part 2ashdmb217No ratings yet
- Histology Exam 3 ReviewDocument7 pagesHistology Exam 3 Reviewashdmb217No ratings yet
- Histology Exam 2 Review.1Document18 pagesHistology Exam 2 Review.1ashdmb217No ratings yet
- Exam IV ReviewDocument39 pagesExam IV Reviewashdmb217No ratings yet
- Exam 1 Study Guide.2Document52 pagesExam 1 Study Guide.2ashdmb217No ratings yet
- Exam 3 PathwaysDocument1 pageExam 3 Pathwaysashdmb217No ratings yet
- Exam 4 PathwaysDocument1 pageExam 4 Pathwaysashdmb217No ratings yet
- Biochem Exam III Review.2Document24 pagesBiochem Exam III Review.2ashdmb217No ratings yet
- Biochem Exam 2 Review.2Document31 pagesBiochem Exam 2 Review.2ashdmb217No ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hard Gainer Project XDocument98 pagesHard Gainer Project XShano Bartik100% (2)
- Endocrine SystemDocument52 pagesEndocrine Systemnurshuhada zainuddinNo ratings yet
- Case Presentation and Literature Review of Adrenal MassesDocument50 pagesCase Presentation and Literature Review of Adrenal MassesAnas Mk HindawiNo ratings yet
- Chapter 16Document23 pagesChapter 16Richard RichardsNo ratings yet
- Endocrine Study GuideDocument4 pagesEndocrine Study GuideNursingSchoolNotes100% (1)
- Pharmacology Exam 3 Pharmacology Exam 3Document44 pagesPharmacology Exam 3 Pharmacology Exam 3LillabinNo ratings yet
- Astro Diagnosis Libra Part ADocument26 pagesAstro Diagnosis Libra Part AOvn MurthyNo ratings yet
- Pex 04 04Document4 pagesPex 04 04Erwin SetiawanNo ratings yet
- Lecture10 CommunicationIII 1Document30 pagesLecture10 CommunicationIII 1Liana Rose MeregildoNo ratings yet
- Adrenal Disorders in ChildrenDocument39 pagesAdrenal Disorders in ChildrenCorina OngNo ratings yet
- Dulutalias - Chapter18-THE ENDOCRINE SYSTEMDocument10 pagesDulutalias - Chapter18-THE ENDOCRINE SYSTEMGwen Valerie DulutaliasNo ratings yet
- Manajemen ShockDocument47 pagesManajemen ShockPutry RizqiaNo ratings yet
- 6 - Clinical Biochemistry - 1001411Document14 pages6 - Clinical Biochemistry - 1001411bsmallahNo ratings yet
- 4 - Endocrinology Tiki TakaDocument32 pages4 - Endocrinology Tiki TakaHemaNo ratings yet
- BB Training Tests Med Physiology 2nd Sem - Answ 120 OrderDocument19 pagesBB Training Tests Med Physiology 2nd Sem - Answ 120 OrderGandam SwadeepNo ratings yet
- Non Chordates - ChordatesDocument4 pagesNon Chordates - Chordateschetanbhagat7No ratings yet
- Cushing-Syndrome SyndromeDocument16 pagesCushing-Syndrome SyndromeVanetNo ratings yet
- CH 52 Assessment and Management of Patients With Endocrine DisordersDocument15 pagesCH 52 Assessment and Management of Patients With Endocrine Disordersfiya33No ratings yet
- Endocrine SystemDocument41 pagesEndocrine SystemMerrin EncarnacionNo ratings yet
- ReviewerDocument20 pagesReviewerYang MolosNo ratings yet
- Egyankosh..Unit 2..influencing FactorsDocument9 pagesEgyankosh..Unit 2..influencing FactorsAnshita SharmaNo ratings yet
- Principles of Molecular Medicine - J. Larry Jamenson - Humana Press - 1998Document1,144 pagesPrinciples of Molecular Medicine - J. Larry Jamenson - Humana Press - 1998BOC100% (1)
- AnatomyDocument286 pagesAnatomyAbbyramy NNo ratings yet
- Noor Endocrinologybase. FINALDocument62 pagesNoor Endocrinologybase. FINALschool adressNo ratings yet
- Physiology MCQ - EndocrineDocument8 pagesPhysiology MCQ - EndocrineSana Almosawi100% (2)
- Diagnostic Tests For Cushing'sDocument6 pagesDiagnostic Tests For Cushing'sChristine ParrillaNo ratings yet
- Endocrine System: QuestionsDocument15 pagesEndocrine System: QuestionsJeane Irish Paller EgotNo ratings yet
- Endocrine Case StudiesDocument36 pagesEndocrine Case StudiesaagarwalmdNo ratings yet
- Adrenal EctomyDocument26 pagesAdrenal EctomyMemburu Ma'rifah IlahiNo ratings yet
- Facts About CAH (Congenital Adrenal Hyperplasia) : What Are The Adrenal Glands?Document5 pagesFacts About CAH (Congenital Adrenal Hyperplasia) : What Are The Adrenal Glands?TheGardenPixy100% (1)