Professional Documents
Culture Documents
Hemolytic-Uremic Syndrome 06.11.2014
Uploaded by
Emily EresumaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hemolytic-Uremic Syndrome 06.11.2014
Uploaded by
Emily EresumaCopyright:
Available Formats
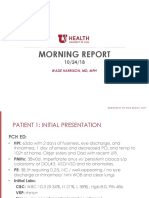
EDWARD FI SHER, MD PGY- 3
JUNE 1 1 , 201 4
Morning Report
5 yo boy with cough and fever
Presents with cough and fever x5 days, up to 103.5 F
Dx with viral illness at PCP 2 days prior to admission
Intermittent emesis, poor PO intake
Brought to PCH ED for worsening sx
5 yo boy with cough and fever
PMH: Healthy, no surgeries
No meds, NKDA
Imms: Up to date
FH: Older brother died at home at 15 months of
pneumonia/strep pneumo bacteremia (was fully
immunized, prior to PCV 13). Lots of pneumonia
on paternal side?
SH: Lives with parents, older brother, no tobacco
exposure
5 yo boy with cough and fever
T 37.3, HR 163, RR 36, 94% on RA
Gen: pale but well-appearing, tachypneic, NAD
HEENT: normal
CV: Tachycardic, no murmurs, good pulses
Resp: Diminished breath sounds on L with
crackles. No retractions
Abd: soft, NT/ND, normal BS
Skin: normal
Neuro: normal
In the ED
Due to history of poor PO, bolused 40 mL/kg
WBC 10.6 (22% bands), Hct 36.6, Plts 164
Blood cx sent
CXR: LLL pneumonia with effusion
Not hypoxic
Admit to RTU, IV ampicillin
In the RTU
Worsening work of breathing, tachypnea, increasing
effusion on CXR
As he is being transferred, blood culture turns
positive @16 hrs, DNA for S pneumo detected
Ampicillin --> ceftriaxone
On the floor
Worsening effusion --> chest tube placement
Mild hyponatremia (SIADH?)
Not hypoxic
Subsequent blood cultures negative
Overnight
Called to evaluate pt ~2300
Worsened tachycardia (130s --> 170s)
Looks more pale/yellow, more swollen
Nurse is concerned he looks bad, and wants to call a
rapid response
Overnight
T 37.6, HR 167, RR 40, BP 107/62, 88% on RA
Gen: pale/yellow/greenish, not wanting to interact
HEENT: very pale conjunctiva
CV: Tachycardic, no murmurs, good pulses, cap
refill hard to elicit
Resp: Diminished breath sounds on L with
crackles. No retractions. Chest tube in place
Abd: soft, NT/ND, normal BS, no HSM
Skin: normal
Neuro: normal
Differential diagnosis
Heme
Blood loss (Chest tube,
hemothorax, abdomen, GI
bleed)
Hemolysis
Anemia of inflammatory
state
DIC
TTP
Rheum
Vasculitis
Renal
HUS
Labs
WBC 17.6 (23% bands), Hgb 3.9, Hct 11.1, Plts 46
Smear 2+ schistocytes
Na 136, K 4.7, Cl 113, bicarb 17, BUN 33, creat
0.71, gluc 121, alb 2.1, bili 2.1, ALT 26, AST 213
PT/INR 15.4/1.2, PTT 48, fibrinogen 633
D-dimer 4467
Hemolytic-Uremic Syndrome
Microangiopathic hemolytic anemia
Thrombocytopenia
Acute kidney injury
HUS Classifications
Diarrhea positive/negative
Primary (complement gene mutations, antibodies to
complement factor B)
Secondary (usually infectious)
Epidemiology
STEC: 90% of HUS cases
Pneumococcus: ~5% (40% of non-STEC cases)
HUS in ~0.5% of pneumococcal infections
Pathogenesis (?)
Certain serotypes of strep
pneumo expose Thomsen-
Friedenreich (T) antigen
(serotype 19A)
Preformed host IgM bind
T antigen
Cascade of events lead to
HUS
Alternative complement-
mediated pathway?
Management
Treat underlying pneumococcal infection -
empirically if necessary
Consider rates of resistance
HUS therapy largely supportive
RBCs and platelets
STOP nephrotoxic drugs
Nephrology involvement (dialysis?)
Avoid FFP, plasmapheresis (theoretical)
Risk Factors and Outcome
Generally more severe than STEC HUS
Mortality higher (5-10% vs 12%)
More likely to require dialysis (67-80%)
Need more transfusions (PRBs and plts)
Death usually due to infection
Biggest risk factor: meningitis (88% of deaths in the largest
review)
~10% evolve to ESRD requiring dialysis
References
Banerjee R et al. Streptococcus pneumoniae-associated hemolytic
uremic syndrome among children in North America. Pediatr Infect Dis
J 30:736, 2011
Copelovitch L, Kaplan BS. Streptococcus pneumoniae-associated
hemolytic uremic syndrome. Pediatr Nephrol 23:1951-56, 2008
Copelovitch L, Kaplan BS. Streptococcus pneumoniae-associated
hemolytic uremic syndrome: classification and the emergence of
serotype 19A. Pediatrics 125:174-182, 2010
Geary DF. Hemolytic uremic syndrome and Streptococcus
pneumoniae: improving our understanding. J Pediatr 151:113, 2007
Spinale JM et al. Update on Streptococcus pneumoniae-associated
hemolytic uremic syndrome. Curr Opin Pediatr 25:203-8, 2013
You might also like
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Pediatric Hypertension Noon Conference 03.20.2019Document44 pagesPediatric Hypertension Noon Conference 03.20.2019Emily EresumaNo ratings yet
- Board Prep Metabolics Feb 2019Document23 pagesBoard Prep Metabolics Feb 2019Emily EresumaNo ratings yet
- Morning Report Case Presentation: APRIL 1, 2019Document14 pagesMorning Report Case Presentation: APRIL 1, 2019Emily EresumaNo ratings yet
- Investing 101 For Residents: RJ Nemeyer MDDocument12 pagesInvesting 101 For Residents: RJ Nemeyer MDEmily EresumaNo ratings yet
- Food Challenge 03.20.2019Document17 pagesFood Challenge 03.20.2019Emily EresumaNo ratings yet
- Case Presentation: Tad MiyaDocument41 pagesCase Presentation: Tad MiyaEmily EresumaNo ratings yet
- Tachycardia How To Keep Your Patient Alive in The Middle of The NightDocument30 pagesTachycardia How To Keep Your Patient Alive in The Middle of The NightEmily Eresuma100% (1)
- Board Prep GI Jan 2019Document32 pagesBoard Prep GI Jan 2019Emily EresumaNo ratings yet
- Somatization 01.28.2019Document28 pagesSomatization 01.28.2019Emily EresumaNo ratings yet
- Dangers of Vaping 03.15.2019Document23 pagesDangers of Vaping 03.15.2019Emily EresumaNo ratings yet
- Bells Palsy or Stroke 02.06.2019Document19 pagesBells Palsy or Stroke 02.06.2019Emily EresumaNo ratings yet
- Chronic Granulomatous Disease 01.23.2019Document10 pagesChronic Granulomatous Disease 01.23.2019Emily EresumaNo ratings yet
- Cah 10.01.2018Document26 pagesCah 10.01.2018Emily EresumaNo ratings yet
- MysteryCase 10.22.18Document10 pagesMysteryCase 10.22.18Emily EresumaNo ratings yet
- Morning Report: Melanie Nelson, PGY-2Document25 pagesMorning Report: Melanie Nelson, PGY-2Emily EresumaNo ratings yet
- Pertussis 01.14.2019Document29 pagesPertussis 01.14.2019Emily EresumaNo ratings yet
- Limping 12.10.2018Document32 pagesLimping 12.10.2018Emily Eresuma100% (1)
- Jaundice 11.28.2018Document13 pagesJaundice 11.28.2018Emily EresumaNo ratings yet
- Board Prep Emergency Ingestions Dec.2018Document46 pagesBoard Prep Emergency Ingestions Dec.2018Emily EresumaNo ratings yet
- Pediatric Urology Topics Relating To Infants & Toddlers: Danielle Brady, Pgy-2Document35 pagesPediatric Urology Topics Relating To Infants & Toddlers: Danielle Brady, Pgy-2Emily EresumaNo ratings yet
- Morning Report: Lindsey Gakenheimer-Smith MD PGY3Document20 pagesMorning Report: Lindsey Gakenheimer-Smith MD PGY3Emily EresumaNo ratings yet
- Halloween Safety: Dominique ChevalierDocument21 pagesHalloween Safety: Dominique ChevalierEmily EresumaNo ratings yet
- Foster Care in Utah: Marlayna DespresDocument11 pagesFoster Care in Utah: Marlayna DespresEmily EresumaNo ratings yet
- Board Prep 08.07.2018 CommonPediatricsDocument42 pagesBoard Prep 08.07.2018 CommonPediatricsEmily EresumaNo ratings yet
- Morning Report: Wade Harrison, MD, MPHDocument13 pagesMorning Report: Wade Harrison, MD, MPHEmily EresumaNo ratings yet
- Morning Report 9/5/18: Adam Cardullo, MD Pgy - 2Document22 pagesMorning Report 9/5/18: Adam Cardullo, MD Pgy - 2Emily EresumaNo ratings yet
- BehaviorDocument30 pagesBehaviorEmily Eresuma100% (1)
- Advocacy: Early Literacy: Nate Riechers Pgy1 8/16/2018Document32 pagesAdvocacy: Early Literacy: Nate Riechers Pgy1 8/16/2018Emily EresumaNo ratings yet
- Jeffrey Barratt, MDDocument27 pagesJeffrey Barratt, MDEmily EresumaNo ratings yet
- Syncope 08.29.2018Document16 pagesSyncope 08.29.2018Emily EresumaNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Advanced Diagnostic TechniquesDocument19 pagesAdvanced Diagnostic TechniquesSunkara Musalaiah0% (1)
- Nursing Profession: The United States and Quickly Advanced With The Rise of Trainings For NursesDocument3 pagesNursing Profession: The United States and Quickly Advanced With The Rise of Trainings For NursesMoureneGasperszNo ratings yet
- Soluvit NinfDocument4 pagesSoluvit NinfNurkholis AminNo ratings yet
- Dedham Transcript Jan. 5, 2012 Ready To Share Memories?Document2 pagesDedham Transcript Jan. 5, 2012 Ready To Share Memories?AndreaECalvinNo ratings yet
- Notes For PMLSDocument3 pagesNotes For PMLSAlliah LorioNo ratings yet
- Implementation Toolkit For Clinical Handover ImprovementDocument60 pagesImplementation Toolkit For Clinical Handover ImprovementKhanh LeNo ratings yet
- DR Anuj Raj BijukchheDocument95 pagesDR Anuj Raj BijukchheMUHAMMAD JAWAD HASSANNo ratings yet
- Sirosis HepatisDocument54 pagesSirosis HepatisaprillyaNo ratings yet
- The 8 D's of Stroke CareDocument3 pagesThe 8 D's of Stroke Caremuhammad fahrizaNo ratings yet
- Strattera PDFDocument5 pagesStrattera PDFToronto StarNo ratings yet
- 1-Medical Gases Systems. The First Lecture.Document18 pages1-Medical Gases Systems. The First Lecture.Fireproof Sistemas Electromecánicos100% (1)
- Kelly Timmons ResumeDocument3 pagesKelly Timmons Resumeapi-300946292No ratings yet
- 7172.ALL CardioQuickGuide 9Document95 pages7172.ALL CardioQuickGuide 9jan.headley9915No ratings yet
- NCPDocument7 pagesNCPJo Chiko FlorendoNo ratings yet
- Anesthesia in Day Care SurgeryDocument143 pagesAnesthesia in Day Care SurgeryGmkmcNo ratings yet
- Borang Helth ConnectDocument1 pageBorang Helth Connectklinik hafiz Putra perdanaNo ratings yet
- 4 10 18 306 Transcultural PaperDocument6 pages4 10 18 306 Transcultural Paperapi-488513754No ratings yet
- In Service Exam For Breast DR Paul BalisiDocument11 pagesIn Service Exam For Breast DR Paul BalisiAmiel Francisco ReyesNo ratings yet
- Informatics HYPERLINK Gypsy Kaye PinedaDocument73 pagesInformatics HYPERLINK Gypsy Kaye PinedaRaquel JavierNo ratings yet
- UW ObjectivesDocument220 pagesUW ObjectivesRaymond Bernatowicz100% (2)
- PRUBSN Heatlh Enrich PlusDocument2 pagesPRUBSN Heatlh Enrich PlusMalik TaufiqNo ratings yet
- Naturalpath Intake Form - ADULTDocument5 pagesNaturalpath Intake Form - ADULTcms_gcoles100% (1)
- Managing Motor Speech DisordersDocument54 pagesManaging Motor Speech DisordersTashi WangmoNo ratings yet
- Quality Improvement Paper FinalDocument11 pagesQuality Improvement Paper Finalapi-291740538No ratings yet
- Gemba Overview - Sheena Butts - IIESHS - WEBINAR v1Document35 pagesGemba Overview - Sheena Butts - IIESHS - WEBINAR v1Bryan OrdialesNo ratings yet
- Vonlays: A Conservative Esthetic Alternative To Full-Coverage CrownsDocument6 pagesVonlays: A Conservative Esthetic Alternative To Full-Coverage CrownsDavid Gomez0% (1)
- Acute Viral HepatitisDocument43 pagesAcute Viral HepatitisFatimah Az-zahra100% (2)
- PCS HMCG - Docx CS - Docx 2ndDocument1 pagePCS HMCG - Docx CS - Docx 2ndJane Imperial LitcherNo ratings yet
- Emergency Management of AnaphylaxisDocument1 pageEmergency Management of AnaphylaxisEugene SandhuNo ratings yet
- Establishing Priorities in The Supervision HourDocument7 pagesEstablishing Priorities in The Supervision HourDianaSantiagoNo ratings yet