Professional Documents
Culture Documents
Chorea Curs Complet
Uploaded by
Alexandra Batani0 ratings0% found this document useful (0 votes)
40 views90 pagesChorea is a borrowed Latin word that derives from the Greek khoreia, a choral dance. Levodopa-induced chorea is the most common movement disorder. Ballism or ballismus is considered a very severe form of chorea.
Original Description:
Original Title
19. Chorea Curs Complet
Copyright
© © All Rights Reserved
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentChorea is a borrowed Latin word that derives from the Greek khoreia, a choral dance. Levodopa-induced chorea is the most common movement disorder. Ballism or ballismus is considered a very severe form of chorea.
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
40 views90 pagesChorea Curs Complet
Uploaded by
Alexandra BataniChorea is a borrowed Latin word that derives from the Greek khoreia, a choral dance. Levodopa-induced chorea is the most common movement disorder. Ballism or ballismus is considered a very severe form of chorea.
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
You are on page 1of 90
Chorea
Chorea" is a borrowed Latin word that derives from the
Greek khoreia, a choral dance. The basic Greek word for
dance (written with the Roman alphabet) is khoros.
The ad hoc Committee on Classification of the World
Federation of Neurology has defined chorea as
"a state of excessive, spontaneous movements,
irregularly timed, non-repetitive, randomly distributed
and abrupt in character. These movements may vary in
severity from restlessness with mild intermittent
exaggeration of gesture and expression, fidgeting
movements of the hands, unstable dance-like gait to a
continuous flow of disabling, violent movements
Patients with chorea exhibit motor impersistence (ie, they cannot
maintain a sustained posture).
When attempting to grip an object, they alternately squeeze
and release ("milkmaid's grip"). When they attempt to protrude the
tongue, the tongue often pops in and out ("harlequin's tongue").
Patients often drop objects involuntarily. Also common are attempts
by patients to mask the chorea by voluntarily augmenting the
choreiform movements with semipurposeful movements.
Chorea involves both proximal and distal muscles. In most patients,
normal tone is noted, but, in some instances, hypotonia is present.
In a busy movement disorder center, levodopa-induced chorea is
the most common movement disorder, followed by Huntington
disease
The term athetosis comes from the Greek word athetos (not
fixed).It is a slow form of chorea. Because of the slowness, the
movements have a writhing (ie, squirming, twisting, or snakelike)
appearance. Choreoathetosis is essentially an intermediate form.
Ballism or ballismus is considered a very severe form of chorea in
which the movements have a violent, flinging quality.
In Greek, ballismos means "a jumping about or dancing."[2]
Ballism has been defined as "continuous, violent, coordinated
involuntary activity involving the axial and proximal appendicular
musculature such that the limbs are flung about."
This movement disorder most often involves only one side of
the body (ie, hemiballism or hemiballismus). Occasionally, bilateral
movements occur (ie, biballism or paraballism). Many patients with
hemiballism have choreiform movements and vice versa, and
hemiballism often evolves into hemichorea.
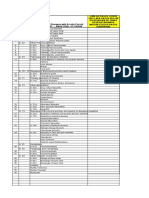
Schematic diagram of the basal ganglia circuitry. Represented are the following: inhibitory (red arrows) and excitatory (green arrows)
projections between the motor cortex, the putamen, the globus pallidus pars externa (GPe) and globus pallidus pars interna (GPi), the
subthalamic nucleus (STN), the substantia nigra pars reticulata (SNr) and substantia nigra pars compacta (SNc), and the ventrolateral
thalamus (VL). D1 and D2 indicate the direct (regulated by dopamine D1 receptors) and indirect (regulated by dopamine D2 receptors)
pathways, respectively
Pathophysiology
A simple model of basal ganglia function states that dopaminergic
and GABAergic impulses from the substantia nigra and motor
cortex, respectively, are funneled through the pallidum into the
motor thalamus and motor cortex. These impulses are modulated in
the striatum via two segregated, parallel, direct and indirect loops
through the medial pallidum and lateral pallidum/subthalamic
nucleus. Subthalamic nucleus activity drives the medial pallidum to
inhibit cortex-mediated impulses, thereby inducing parkinsonism.
Absent subthalamic nucleus inhibition enhances motor activity
through the motor thalamus, resulting in abnormal involuntary
movements such as dystonia, chorea, and tics. A classic example of
loss of subthalamic inhibitory drive is ballism
History
Patients with chorea
may not initially be aware of the abnormal movements because they
may be subtle.
can suppress the chorea temporarily and frequently camouflage
some of the movements by incorporating them into semipurposeful
activities (ie, parakinesia).
The inability to maintain voluntary contraction (ie, motor
impersistence), as is seen during manual grip (milkmaid grip) tests
or tongue protrusion, is a characteristic feature of chorea and
results in the dropping of objects and clumsiness.
Muscle stretch reflexes are often hung-up and pendular.
In severely affected patients, a peculiar dancelike gait may be noted.
Depending on the underlying cause of the chorea, other motor
symptoms include- dysarthria, dysphagia, postural instability, ataxia,
dystonia, and myoclonus.
Laboratory Studies Diagnosis of the primary choreatic conditions
history and clinical findings;
several laboratory studies are useful, especially in distinguishing the secondary forms of chorea from the
primary forms.
Huntington disease: The only laboratory study presently available to confirm HD is genetic
testing. It identifies a gene abnormality in the short arm of chromosome 4, characterized
by abnormal repetition of the trinucleotide CAG, the length of which determines the age of
onset (anticipation).
Wilson disease: A low serum ceruloplasmin level and serum copper values showing
increased urinary copper excretion corroborate the diagnosis in most cases.
Liver function test results are usually abnormal.
If the diagnosis is still uncertain, liver biopsy can help confirm the diagnosis.
Sydenham chorea : The chorea can lag behind the etiologic streptococcal infection by 1-6
months, sometimes as long as 30 years; therefore, antistreptococcal antibody titers may
no longer be elevated at presentation. Without documentation of an antecedent
streptococcal infection, the diagnosis of Sydenham chorea must be made by excluding
other causes.
Neuroacanthocytosis: The diagnosis is confirmed by the presence of spiky erythrocytes
(acanthocytes) in peripheral blood smears. The serum creatine kinase level may be
elevated.
is based on
Other laboratory studies useful in the differential diagnosis
of chorea include complement levels, antinuclear antibody titers,
antiphospholipid antibody titers, amino acid levels in serum and
urine, enzymatic studies from skin fibroblasts, thyrotropin levels,
thyroxine values, and parathormone levels.
Imaging Studies
MRI
Patients with Huntington disease (HD) and chorea-
acanthocytosis show decreased signal in the
neostriatum, caudate, and putamen. No significant
difference has been observed between these
diseases. The decreased neostriatal signal
corresponds to increased iron deposition.
Generalized atrophy, as well as focal atrophy of
the neostriatum, predominantly of the caudate, with
resulting enlargement of the frontal horns, follows the
initial findings of decreased neostriatal signal
Medical Care
Only symptomatic treatment is available for patients with
chorea.
Chorea may be a disabling symptom, leading to bruises,
fractures, and falls, and may impair the ability of patients to feed
themselves.
The most widely used agents in the treatment of chorea are the
neuroleptics. The basis of their mechanism of action is thought to
be related to blocking of dopamine receptors.
Neuroleptics can be classified as typical and atypical.
Typical neuroleptics include haloperidol and fluphenazine.
Atypical neuroleptics include risperidone, olanzapine, clozapine, and
quetiapine.
Dopamine-depleting agents, such as reserpine and
tetrabenazine, represent another option in the treatment of chorea.
GABAergic drugs, such as clonazepam, gabapentin, and valproate
, can be used as adjunctive therapy.
Coenzyme Q10 alone and in combination with minocycline have
been proposed as potential therapies
Intravenous immunoglobulin and plasmapheresis may shorten the
course of the illness and decrease symptom severity in patients with
Sydenham chorea.
Surgical Care
Deep brain stimulation is an emerging technique that
may benefit patients, at least in certain cases.
Although deep brain stimulation is not yet used routinely
for chorea, as it is for PD, exciting progress has been
made with this modality.
Cell transplantation is controversial and in early stages of
research. It has shown variable results for HD patient
participants.
Causes of Chorea
Inherited
Ataxia-telangiectasia
Benign hereditary chorea
Hallervorden-Spatz disease
Hereditary spinocerebellar ataxias
Huntington disease
Inborn errors of metabolism
Glutaric acidemia, Propionic acidemia ,Homocystinuria Phenylketonuria,Sulfite oxidase
deficiency
Mitochondrial encephalomyopathies
Neuroacanthocvtosis
Paroxysmal disorders
Paroxysmal kinesiogenic choreoathetosis
Paroxysmal nonkinesiogenic choreoathetosis
Pyruvate carboxylase deficiency
Wilson disease
Drugs Antimetabolites
Anticholinergics
Anticonvulsants (eg, phenytoin, carbamazepine, phenobarbital)
Antidopaminergic agents (eg, phenothiazines, haloperidol, metoclopramide)
Antihistamines
CNS stimulants (eg, amphetamines, methylphenidate, pemoline)
Lithium
Dopamine agonists (eg, levodopa)
Oral contraceptives
Endocrine
Hyperthyroidism
Chorea gravidarum
Hypoparathyroidism, pseudohypoparathyroidism
Immune/infectious
Behet disease
Other infections - Pertussis, diphtheria, varicella
Primary antiphospholipid antibody syndrome
Sydenham chorea
Systemic lupus erythematosus
Bacterial endocarditis
Herpes simplex encephalitis
HIV related
Infectious mononucleosis
Lyme disease
Mycoplasmal pneumonia
Viral meningoencephalitis (eg, mumps, measles, varicella)
Vascular
Arteriovenous malformation
Basal ganglia infarction or hemorrhage
Vasculopathies/vasculitis: Churg-Strauss syndrome[1] , moyamoya
Metabolic
Hypocalcemia
Hypoglycemia and hyperglycemia
Hypomagnesemia
Hyponatremia, hypernatremia, and central pontine myelinolysis
Renal failure
Miscellaneous
Cerebral palsy
Head trauma
Bronchopulmonary dysplasia (infantile chorea)
Cardiopulmonary bypass - "Postpump chorea
Neoplastic
Primary and metastatic brain tumors
Primary CNS lymphoma
Toxins CO, Mg, organophosphate
Pathophysiology and General Principles in
Treatment of Chorea
Movement disorders (particularly chorea, athetosis, and dystonia)
are thought to result from basal ganglia pathology.
Dopaminergic neurons within the substantia nigra project rostrally
to the neostriatum (caudate and putamen).
Chorea may be viewed as resulting from increased dopaminergic
activity in the projections from the substantia nigra to the striatum,
resulting in decreased GABAergic projection from the striatum to the
globus pallidus.
Most of the drugs used in symptomatic treatment of chorea act
through attenuation of dopaminergic transmission or
enhancement of GABA transmission.
Anticonvulsant drugs may suppress chorea but also may induce
chorea, especially in patients with basal ganglia dysfunction.
Rheumatic (Sydenham) Chorea
In 1684, Thomas Sydenham described the clinical syndrome that
now bears his name. Originally termed St. Vitus' dance, it now is
referred to as rheumatic chorea. Stoll first proposed a relationship
between Sydenham chorea and rheumatic fever (RF) in 1780.
In 1889, Cheadle described the full rheumatic syndrome of carditis,
polyarthritis, chorea, subcutaneous nodules, and erythema
marginatum.
Several decades later, epidemiologic and microbiologic studies
confirmed the etiological role of streptococcal infection in RF.
More recently, Sydenham chorea (SC) has been linked to numerous
neuropsychiatric disorders, including obsessive compulsive disorder
(OCD), attention deficit-hyperactivity disorder, depression and
anxiety.
Epidemiology
Sydenham chorea is the most common cause of acquired chorea in the
young. During the latter part of the twentieth century the number of
reported cases of RF in the United States increased. This resurgence
appears to be associated with strains of group A beta hemolytic
streptococcal infection that are less likely to cause symptomatic pharyngitis.
In the United States, the incidence of RF is approximately 0.5-2 per
100,000 population per year.
Chorea is a major manifestation of acute RF and
is the only evidence of RF in approximately 20% of cases.
In some outbreaks, chorea has been present in more than 30% of patients
with acute RF.
The female-to-male ratio is approximately 2:1, and most patients present
between 5-15 years of age.
Clinical features and course
SC is a major manifestation of acute rheumatic fever.
According to the 1992 modification of the Jones criteria,
chorea (or indolent carditis) alone is sufficient for diagnosis of
RF, provided other causes have been excluded.
SC typically presents with other manifestations of RF, but in
20% of cases chorea may be the presenting or sole
manifestation of RF.
The main features of SC are involuntary movements,
hypotonia, and mild muscular weakness.
Chorea can be generalized or unilateral, predominantly
involving the face, hands, and arms. Movements are present
at rest, aggravated by stress, and usually cease during sleep.
In about 20% of patients, only one side of the body may
seem to be affected (hemichorea); however, careful
examination usually reveals some involvement of the opposite
side.
The choreic movements interfere with volitional movements
and result in a clumsy gait, dropping and spilling, and
explosive bursts of dysarthric speech.
Muscular weakness leads to inability to sustain a contraction
(milkmaid's grip).
The pronator sign consists of hyperpronation of the hands,
causing the palms to face outward when the arms are held over
the head. Another sign of weakness and hypotonia is the so-
called choreic handwith the arms extended, the wrist will flex
and the metacarpophalangeal joints overextend.
Some children may have such profound weakness that they
appear paralyzed. Not uncommonly, children are restricted to
bed or are unable to attend school for the duration of the
illness. Fortunately, paralytic chorea is uncommon.
Patients with SC may also have psychiatric symptoms such as
depression, anxiety, personality changes, emotional lability,
OCD, and attention deficit disorder (ADD).
Occasionally, these symptoms precede the onset of chorea
On average, the disease resolves spontaneously in 3-6 months and
rarely lasts longer than 1 year.
Mild chorea without functional disability may be found in a small
proportion of patients up to 10 years after the initial attack of SC.
About 20% of patients experience 2-10 recurrences, usually within 2
years after the initial attack.
Pathophysiology
Immunology: Evidence suggests that SC may result from the production of
immunoglobin G antibodies that crossreact with antigens in the membrane of group A
streptococci and antigens in the neuronal cytoplasm of the caudate and subthalamic
nuclei, namely intracellular tubulin and extracellular lysoganglioside.
Antineuronal antibodies have also been found in the cerebrospinal fluid (CSF) of
patients with acute rheumatic chorea. Immunofluorescent staining has shown that
sera from approximately half of the children with SC have antibodies that react with
neuronal cytoplasmic antigens in the caudate and subthalamic nuclei.
Serum antineuronal antibody titers have been found to decrease as the chorea
improves.
In children who suffer a relapse, the increase in symptom severity correlates with a
rise in these neuronal antibodies.
Neuroimaging
MRI findings in SC are not consistent and may be
normal.
Functional neuroimaging using fluorodeoxyglucose (FDG)
positron emission tomography (PET) has demonstrated
reversible striatal hypermetaboli.
Diagnosis
Diagnosis rests on a combination of clinical manifestations that can
develop in relation to group A streptococcal pharyngitis. These
include chorea, carditis, subcutaneous nodules, erythema
marginatum, and migratory polyarthritis. Because the inciting
infection is completely treatable, attention has been refocused on
prevention.
Diagnosis
Diagnosis of SC may be difficult, because no single, established
diagnostic test is available.
SC usually develops in those aged 3-13 years and is believed to result from
a preceding streptococcal infection.
The patient may have no history of rheumatic fever, and a
preceding streptococcal infection cannot always be documented. Infections
can be subclinical and often precede the development of neurologic
symptoms by age 1-6 months.
At least 25% of patients with SC fail to have serologic evidence of
prior infection.
Chorea may be the first and only manifestation of rheumatic fever.
However, some patients may have subtle evidence of carditis by
echocardiography despite a normal clinical examination and ECG. Chorea
alone is sufficient for diagnosis providing other causes of the condition have
been excluded.
Treatment
Treatment and prevention may involve multiple fields of discipline,
including infectious diseases, cardiology, and neurology. For this
reason, several different classes of medications are used. These
include antibiotic, neuroleptic, and cardiac medications
(ethiologyc, pathogenic, symptomatic)
A.The primary goal of treating an ARF attack is to eradicate streptococcal
organisms and bacterial antigens from the pharyngeal region.
Penicillin is the drug of choice in persons who are not at risk of
allergic reaction. A single parenteral injection of benzathine benzylpenicillin
can ensure compliance.
Oral cephalosporins, rather than erythromycin, are recommended as
an alternative in patients who are allergic to penicillin. However, be
cautious of the 20% cross-reactivity of the cephalosporins with penicillin
C
SC is usually self-limited, and treatment should be limited to
patients with chorea severe enough to interfere with function.
Anticonvulsants (valproic acid and carbamazepine) have been
shown to be effective in diminishing choreic movements at doses
normally used for seizure control. In particular, valproate may be
quite helpful in children with SC.
Dopaminergic blockers (pimozide and haloperidol) are effective
and, when used in small doses, are usually well tolerated.
Neuroleptics such as haloperidol and pimozide remain an important
treatment option, especially in older children
B. Steroids have been used widely, but no controlled studies have been done
to confirm steroid efficacy in chorea.
Patients with carditis require prednisone. The goal is to decrease myocardial
inflammation. May decrease inflammation by reversing increased capillary
permeability and suppressing PMN activity. After 2-3 wk, dosage may tapered,
reduced 25% each week.
. Prednisone,
plasma exchange and intravenous immunoglobulin (IVIG) have been
shown to be effective. Case reports have suggested IVIG to be a safe,
effective option in disabling SC.
Immunologic treatment can also be effective but is expensive and may be
associated with significant side effects.
The presence of antineuronal antibodies suggests that intravenous
immunoglobulin (IVIg) and plasma exchange may be effective.
More recent reports have shown IVIG to be an effective safe option.
Because this treatment modality is quite expensive, it should be reserved
for protracted or debilitating cases.
Parents and school officials should be informed that emotional
lability is characteristic of this organic condition.
Children with SC require prophylaxis against
streptococcal infections until 18 years of age.
Chorea gravidarum
Background
Chorea gravidarum (CG) is the term given to chorea occurring
during pregnancy. This is not an etiologically or pathologically
distinct morbid entity but a generic term for chorea of any
cause starting during pregnancy.
Chorea gravidarum is regarded as a syndrome rather than a
specific disease entity.
Incidence
Willson and Preece (1932) found that the overall incidence of
chorea gravidarum was approximately 1 case per 300 deliveries.
The condition is much more rare now.
The decline is probably the result of a decline in rheumatic
fever (RF), which was a major cause of chorea gravidarum before
the use of antibiotics for streptococcal pharyngitis.
In recent times, most cases of chorea appearing during pregnancy
are caused by other diseases systemic lupus erythematosus
[SLE], Huntington disease).
In general, about half the cases are idiopathic, with rheumatic fever
and antiphospholipid syndrome (APLS) underlying most of the
remainder.
Patient profile
Most patients with chorea gravidarum are young; the
average age is 22 years.
Of initial attacks, 80% occur during first pregnancies,
and one half start during the first trimester.One third
begin in the second trimester.
Of afflicted women, 60% previously had chorea.
Recurrences may occur in subsequent pregnancies,
particularly if antiphospholipid syndrome is the cause.
Pathophysiology
Several pathogenetic mechanisms for chorea gravidarum have been offered, but none
have been proven.
Willson and Preece noted that nearly 70% of their patients gave a previous
history of either rheumatic fever or chorea.
Of patients who present with chorea and no apparent carditis,
20% may develop rheumatic heart disease after 20 years.
Interestingly, 50% of patients with oral contraceptive-induced
chorea have a past history of chorea, which in 41% of cases is of rheumatic
origin.
The suggestion is that estrogens and progestational hormones may
sensitize dopamine receptors (presumably at a striatal level) and induce
chorea in individuals who are vulnerable to this complication by virtue of
preexisting pathology in the basal ganglion.
Pathologic changes found at autopsy in chorea gravidarum include
perivascular degenerative changes in the caudate nucleus.
TREATMENT
CG is not an indication for abortion or premature interruption of
pregnancy
Indicated for patients with disabling severe chorea
Reserpine = CI
Haloperidol effective
Pimozide, valproate, carbamazepine
Discontinue the oral contraceptive pill
2/3 the choreea lasts until puerperium
Mortality 12%
21% have recurrent chorea with subsequent pregnancies
Background
is an incurable,
adult-onset,
autosomal dominant inherited disorder associated with
cell loss within a specific subset of neurons in the basal
ganglia and cortex.
HD is named after George Huntington, the physician who described it as
hereditary chorea in 1872.
Characteristic features of HD include
involuntary movements, dementia, and behavioral changes.
Huntington disease (HD)
Pathophysiology
The most striking neuropathology in HD occurs within
the neostriatum, in which gross atrophy of the caudate
nucleus and putamen is accompanied by selective
neuronal loss and astrogliosis.
Marked neuronal loss also is seen in deep layers of the
cerebral cortex. Other regions, including the globus
pallidus, thalamus, subthalamic nucleus, substantia
nigra, and cerebellum, show varying degrees of atrophy
depending on the pathologic grade.
The extent of gross striatal pathology, neuronal loss, and
gliosis provides a basis for grading the severity of HD
pathology (grades 0-4)
No gross striatal atrophy is observed in grades 0 and 1.
Grade 1 cases have neuropathologic changes that can be
detected microscopically but without gross atrophy.
In grade 2, striatal atrophy is present, but the caudate
nucleus remains convex.
In grade 3, striatal atrophy is more severe, and the
caudate nucleus is flat.
In grade 4, striatal atrophy is most severe, and the
medial surface of the caudate nucleus is concave.
is the expansion of a cysteine-adenosine-guanine (CAG) repeat
encoding a polyglutamine tract in the N-terminus of the protein
product called huntingtin.
The function of huntingtin is not known. Normally, it is located in
the cytoplasm. The association of huntingtin with the cytoplasmic
surface of a variety of organelles, including transport vesicles,
synaptic vesicles, microtubules, and mitochondria, raises the
possibility of the occurrence of normal cellular interactions that
might be relevant to neurodegeneration.
N-terminal fragments of mutant huntingtin accumulate and form
inclusions in the cell nucleus in the brains of patients with HD, as
well as in various animal and cell models of HD.
The presence of neuronal intranuclear inclusions (NIIs) initially led
to the view that they are toxic and, hence, pathogenic
The genetic basis of HD
Epidemiology
Frequency
United States
Estimates of the prevalence of HD in the United States
range from 4.1-8.4 per 100,000 people. Accurate
estimates of the incidence of HD are not available.
International
The prevalence in most European countries ranges from
1.63-9.95 per 100,000 people. The prevalence of HD in
Finland and Japan is less than 1 per 100,000 people.
Mortality/Morbidity
HD is a relentlessly progressive disorder, leading to
disability and death, usually from an intercurrent illness.
The mean age at death in all major series ranges from
51-57 years, but the range may be broader. Duration of
illness varies considerably, with a mean of approximately
19 years. Most patients survive for 10-25 years after the
onset of illness.
In a large study, pneumonia and
cardiovascular disease were the most common primary
causes of death.
Juvenile HD (ie, onset of HD in patients younger than 20 years)
accounts for approximately 5-10% of all affected patients.
Most patients with juvenile HD inherit the disease from their father,
whereas patients with onset of the disease after age 20 years are
more likely to have inherited the gene from their mother.
Inheritance through the father can lead to earlier onset through
succeeding generations, a phenomenon termed anticipation. This
is caused by greater instability of the HD allele during
spermatogenesis.
CAG repeat length correlates inversely with age of onset, and the
correlation is stronger when the onset of symptoms occurs earlier.
The length of the CAG repeat is the most important factor in
determining age of onset of HD.
Most studies show a mean age at onset ranging from 35-44 years.
Huntington Disease Clinical Presentation
The clinical features of Huntington disease (HD) include a
movement disorder, a cognitive disorder, and a behavioral
disorder. Patients may present with one or all disorders in
varying degrees.
Chorea (derived from the Greek word meaning to dance) is
the most common movement disorder seen in HD.
Initially, mild chorea may pass for fidgetiness. Severe chorea
may appear as uncontrollable flailing of the extremities (ie,
ballism), which interferes with function.
As the disease progresses, chorea coexists with and gradually
is replaced by dystonia and parkinsonian features, such as
bradykinesia, rigidity, and postural instability, which are
usually more disabling than the choreic syndrome per se.
In advanced disease, patients develop an akinetic-rigid
syndrome, with minimal or no chorea. Other late features are
spasticity, clonus, and extensor plantar responses.
Dysarthria and dysphagia are common.
Abnormal eye movements may be seen early in the disease.
Other movement disorders, such as tics and myoclonus, may be
seen in patients with HD.
Juvenile HD (Westphal variant), defined as having an age of
onset of younger than 20 years, is characterized by
parkinsonian features, dystonia, long-tract signs, dementia,
epilepsy, and mild or even absent chorea.
Cognitive decline is characteristic of HD, but the rate of
progression among individual patients can vary considerably.
Dementia and the psychiatric features of HD are perhaps the
earliest and most important indicators of functional impairment.
The dementia syndrome associated with HD includes early onset
behavioral changes, such as irritability, untidiness, and loss of
interest. Slowing of cognition, impairment of intellectual function,
and memory disturbances are seen later. This pattern corresponds
well to the syndrome of subcortical dementia, and it has been
suggested to reflect dysfunction of frontal-subcortical neuronal
circuitry.
Early stages of HD are characterized by deficits in short-term
memory, followed by motor dysfunction and a variety of cognitive
changes in the intermediate stages of dementia.[6, 7] These deficits
include diminished verbal fluency, problems with attention,
executive function, visuospatial processing, and abstract reasoning.
Language skills become affected in the final stages of the illness,
resulting in a marked word-retrieval deficit.
The behavioral disorder of HD is represented most
commonly by affective illness.
Depression is more prevalent, with a small percentage of
patients experiencing episodic bouts of mania
characteristic of bipolar disorder.
Patients with HD and persons at risk for HD may have an
increased rate of suicide.
Patients with HD also can develop psychosis, obsessive-
compulsive symptoms, sexual and sleep disorders, and
changes in personality
Tendon reflexes are variable in HD, ranging from
reduced in some patients to pathologically brisk with
clonus in other patients. The plantar response usually is
flexor, but it may be extensor in advanced stages of the
illness.
Other hyperkinesias, such as tics and myoclonus, may
be seen in HD.
Eye movement abnormalities can be seen early in the
disease.
Imaging Studies
No single imaging technique is necessary or sufficient for
diagnosis of Huntington disease (HD).
Measurement of the bicaudate diameter (ie, the distance
between the heads of the 2 caudate nuclei) by CT scan
or MRI is a reliable marker of HD.
Other Tests
Genetic testing (reported as the CAG repeat number for
each allele) is now commercially available.
Genetic testing may not be necessary in a patient with a typical
clinical picture and a genetically proven family history of HD.
In the absence of a family history of HD, patients with a suggestive
clinical presentation should undergo genetic testing to exclude or
confirm HD.
If the genetic test is negative for HD, then testing for
systemic lupus erythematosus (SLE), antiphospholipid
antibody syndrome, thyroid disease, neuroacanthocytosis,
DRPLA, Wilson disease, and other less common causes of
chorea may be reasonable, depending on the individual
case
Medication Summary
Although no therapy is currently available to delay the onset
of symptoms or prevent the progression of the disease,
symptomatic treatment of patients with Huntington disease
(HD) may improve the quality of life and prevent
complications. Symptomatic treatment for HD can be divided
into drugs to treat the movement disorder and drugs to treat
psychiatric or behavioral problems.
Therapeutic options include dopamine-depleting agents (eg,
reserpine, tetrabenazine) and dopamine-receptor antagonists
(eg, neuroleptics).
Medical Care
Depression in patients with HD is treatable and should be recognized
promptly. Selective serotonin reuptake inhibitors (SSRIs) should be
considered as first-line therapy. Other antidepressants, including bupropion,
venlafaxine, nefazodone, and tricyclic antidepressants, also can be used.
Electroconvulsive therapy (ECT) can be used in patients with refractory
depression.
Antipsychotic medications may be necessary in patients with hallucinations,
delusions, or schizophrenia-like syndromes. Newer agents, such as
quetiapine, clozapine, olanzapine, and risperidone, are preferred to older
agents because of the lower incidence of extrapyramidal side effects and the
decreased risk for tardive syndromes.
Irritability may be treated with antidepressants, particularly the SSRIs;
mood stabilizers, such as valproic acid or carbamazepine; and, if needed,
atypical neuroleptics.
Other less frequent aspects of HD that may require pharmacologic
treatment are mania, obsessive-compulsive disorder, anxiety, sexual
disorders, myoclonus, tics, dystonia, and epilepsy.
Wilson Disease
Background
Wilson disease is a rare autosomal recessive inherited
disorder of copper metabolism. The condition is
characterized by excessive deposition of copper in the liver,
brain, and other tissues.
The major physiologic aberration is excessive absorption of
copper from the small intestine and decreased excretion of
copper by the liver.
The genetic defect, localized to arm 13q, has been shown to
affect the copper-transporting adenosine triphosphatase
(ATPase) gene (ATP7B) in the liver.
Patients with Wilson disease more often initially present with
hepatic manifestations when identified in the first decade of
life as compared with more neuropsychiatric illness later,
and the latter most commonly occurs during the third
decade.
The diagnosis is established by no individual test but requires
the use of some combination of serum ceruloplasmin level,
urinary copper excretion, presence of Kayser-Fleischer rings,
and hepatic copper content when biopsy is required.
Etiology
The normal estimated total body copper content is 50-100 mg, and the
average daily intake 2-5 mg, depending on an individuals intake of legumes,
meats, shellfish, and chocolate.
Copper is an important component of several metabolic enzymes, including
lysyl oxidase, cytochrome c oxidase, superoxide dismutase, and dopamine
beta-hydroxylase.
Around 50-75% of intestinal copper is absorbed and then transported to the
hepatocytes. This pathway is intact in Wilson disease. After copper reaches
the hepatocyte, it is incorporated into copper-containing enzymes and copper-
binding proteins (CBPs), including ceruloplasmin, a serum ferroxidase.
Within the liver, the majority of in-infancy (< 6 mo) CBP granules
staining positive may be normal. After 6 months, positive staining of CBPs for
copper is almost exclusively found in association with liver diseases such as
Wilson disease, chronic biliary disorders (eg, primary biliary cirrhosis, primary
sclerosing cholangitis), cirrhosis/extensive fibrosis, and primary liver tumors
(most often fibrolamellar hepatocellular carcinoma).
Excess copper may be rendered nontoxic by forming complexes with apo-
metallothionein to produce copper-metallothionein, or it may be excreted into
bile. Normal copper balance is maintained by regulation of excretion, rather than
absorption, and the predominant route of copper excretion (approximately 95%)
is hepatobiliary in nature.
In Wilson disease, the processes of incorporation of copper into
ceruloplasmin and excretion of excess copper into bile are impaired. The
transport of copper by the copper-transporting P-type ATPase is defective in
Wilson disease secondary to one of several mutations in the ATP7B gene. By
genetic linkage studies, Bowcock and colleagues narrowed the assignment of the
Wilson disease locus to 13q14-q21.
The excess copper resulting from Wilson disease promotes
free radical formation that results in oxidation of lipids and
proteins.
Ultrastructural abnormalities in the earliest stages of
hepatocellular injury, involving the endoplasmic reticulum,
mitochondria, peroxisomes, and nuclei, have been identified.
Initially, the excess copper accumulates in the liver, leading to
damage to hepatocytes. Eventually, as liver copper levels
increase, it increases in the circulation and is deposited in
other organs.
Histologic findings
Histologic findings in the brain include the following:
Copper deposition in the basal ganglia[8]
Opalski cells - Periodic acid-Schiffpositive altered glial
cells
Cavitary degeneration
Gliosis
Neuronal loss
Epidemiology
In the United States, the carrier frequency is 1 per 90
individuals. The prevalence of Wilson disease is 1 per 30,000
individuals.
Worldwide, the incidence of Wilson disease is 10-30 million
cases, and the heterozygote carrier rate is 1 case per 100
persons, with the genetic mutation frequency varying from
0.3-0.7%.
Age-related presentations
A German study of patients with Wilson disease illustrated
that patients presenting earlier show predominantly hepatic
symptoms , while those presenting later more often present
with neurological symptoms .
The onset of neurologic symptoms
second / third decade
50% are symptomatic by age 15 years
The initial event is a deposition of copper
in the liver.
Wilson Disease Clinical Presentation
History
Consider hepatic Wilson disease in the differential diagnosis of any
unexplained chronic liver disease, especially in individuals younger than
40 years. The condition may also manifest as acute hepatitis.
Hepatic dysfunction is the presenting feature in more than half of
patients.
The 3 major patterns of hepatic involvement are as follows:
(1) chronic active hepatitis,
(2) cirrhosis,
(3) fulminant hepatic failure.
The most common initial presentation is cirrhosis
Hepatic dysfunction is the presenting feature in more than half of
patients. Although the condition may manifest as acute hepatitis,
the 3 major patterns of hepatic involvement are as follows:
Chronic active hepatitis
Cirrhosis (the most common initial presentation)
Fulminant hepatic failure
Signs of fulminant hepatic failure include the following:
Ascites and prominent abdominal veins
Spider nevi
Palmar erythema
Digital clubbing
Hematemesis
Jaundice
Neuropsychiatric features
Most patients who present with neuropsychiatric manifestations have cirrhosis.
The most common presenting neurologic feature is asymmetric tremor, which is
variable in character and may be predominantly resting, postural, or kinetic.
Frequent early symptoms include the following:
Difficulty speaking
Excessive salivation
Ataxia
Masklike facies
Clumsiness with the hands
Personality changes
Late manifestations (now rare because of earlier diagnosis and treatment) include the
following:
Dystonia
Spasticity
Grand mal seizures
Rigidity
Flexion contractures
Neurologic signs
Neurologic signs of Wilson disease include the following:
Parkinsonian symptoms - Rigidity, bradykinesia
Dysarthria
Tremor at rest or with action
Dystonia, mainly of the face
Dysdiadochokinesia
Poor handwriting
Incoordination
Abnormal eye movements ( slow saccadic movement, limitation of upgaze)
Respiratory dyskinesia, which can present as an unusual cough[3]
Polyneuropathy, which may be the initial manifestation and may be
reversible with treatment[4]
Psychiatric features (10-20% of patients) include the following:
Emotional lability
Impulsiveness
Disinhibition
Self-injurious behavior
Psychiatric abnormalities associated with Wilson disease has been
divided into the following 4 basic categories:
Behavioral
Affective
Schizophrenic-like
Cognitive
Psychiatric signs
Psychiatric signs include the following:
Hyperkinetic behavior
Irritability or anger
Emotional lability
Psychosis
Mania
Difficulty concentrating
Abnormal behavior
Personality changes
Depression
Schizophrenia
Musculoskeletal manifestations
The arthropathy of Wilson disease is a degenerative process that
resembles premature osteoarthritis
Symptomatic joint disease usually arises late in the course of the
disease, frequently after age 20 years
The arthropathy generally involves the spine and large appendicular
joints (eg, knees, wrists, hips)
Osteochondritis dissecans, chondromalacia patellae, and
chondrocalcinosis have also been described
Hematologic and renal manifestations
Coombs-negative acute intravascular hemolysis (10-15%)
Urolithiasis
Hematuria
Clinically, patients may resemble those with Fanconi syndrome,
demonstrating defective renal acidification and excess renal losses
of amino acids, glucose, fructose, galactose, pentose, uric acid,
phosphate, and calcium. The frequency of renal manifestations is
variable.
Urolithiasis, found in up to 16% of patients with Wilson disease,
may be the result of hypercalciuria or poor acidification.
Hematuria and nephrocalcinosis are reported.
OPHTALMOLOGIC SYMTOMS
Kayser-Fleischer rings
Formed by the deposition of copper in the Descemet membrane in the limbus of
the cornea
The color may range from greenish gold to brown
Well-developed rings may be readily visible to the naked eye or with an
ophthalmoscope set at +40.When not visible to the unaided eye, the rings may be
identified using slit-lamp examination or gonioscopy
Observed in up to 90% of individuals with symptomatic Wilson disease and almost
invariably present in those with neurologic manifestations
No longer considered pathognomonic of Wilson disease unless accompanied
by neurologic manifestations, as they may also be observed in patients with chronic
cholestatic disorders
Ophthalmic findings
Sunflower cataracts are brilliantly multicolored and are visible only on
slit-lamp examination.
They do not impair vision.
Other relatively uncommon ophthalmic findings include exotropic
strabismus, optic neuritis or pallor of the optic disc
Additional manifestations
Skeletal abnormalities (eg, osteoporosis, osteomalacia, rickets,
spontaneous fractures, polyarthritis)
Cardiac manifestations (eg, rhythm abnormalities, increased
autonomic tone)
Skin pigmentation and a bluish discoloration at the base of the
fingernails (azure lunulae)
Histologic findings
Histologic findings in the brain include the following:
Copper deposition in the basal ganglia[8]
Opalski cells - Periodic acid-Schiffpositive altered glial
cells
Cavitary degeneration
Gliosis
Neuronal loss
DIAGNOSIS
Approach Considerations
The presence of Kayser-Fleischer rings and ceruloplasmin levels
of less than 20 mg/dL in a patient with neurologic signs or
symptoms suggest a diagnosis of Wilson disease.
If a patient is asymptomatic, exhibits isolated liver disease, and
lacks corneal rings, the coexistence of a hepatic copper
concentration of more than 250 mg/g of dry weight and a low
serum ceruloplasmin level is sufficient to establish a diagnosis.
Therefore, in the absence of Kayser-Fleischer rings or
neurologic abnormalities, a liver biopsy for quantitative copper
determination is essential to establish the diagnosis of Wilson
disease.
Diagnosis
Considerations in the workup of Wilson disease are as follows:
Serum ceruloplasmin levels are less than 20 mg/dL (reference range, 20-40 mg/dL) in
approximately 90% of all patients with Wilson disease
The urinary copper excretion rate is greater than 100 mcg/day (reference range, < 40
mcg/day) in most patients with symptomatic Wilson disease, but it may also be elevated in
other cholestatic liver diseases
In a patient with Kayser-Fleischer rings, a serum ceruloplasmin level < 0 mg/dL and 24-hoyr
urine copper excretion >40 mcg/day establish the diagnosis of Wilson disease
Hepatic copper concentration (criterion standard) on a liver biopsy specimen is >250 mcg/g
of dry weight even in asymptomatic patients; a normal result (15-55 mcg/g) effectively
excludes the diagnosis of untreated Wilson disease, but elevation may be found in other
chronic hepatic disorders
Radiolabeled copper testing directly assays hepatic copper metabolism
Genetic testing is limited to screening of family members for an identified mutation detected
in the index patient
Brain imaging shows characteristic findings; MRI appears to be more sensitive than CT in
detecting early lesions
Abdominal imaging findings are neither sensitive nor specific
Resting ECG abnormalities include left ventricular or biventricular hypertrophy, early
repolarization, ST segment depression, T-wave inversion, and various arrhythmias
Electron microscopic detection of copper-containing hepatocytic lysosomes is helpful in the
diagnosis of the early stages of Wilson disease, in addition to the quantification of hepatic
copper by atomic absorption spectrophotometry
Genetic diagnosis
Linkage analysis has been used in family studies for presymptomatic
testing; however, the multiplicity of mutations (>200 mutations of
ATP7B have been identified) that require screening in individuals
without affected family members is large, making such analysis
impractical. Therefore, the use of molecular testing is currently limited
to screening of family members for an identified mutation detected in
the index patient.
Abdominal imaging
Computed tomography (CT) scanning, magnetic resonance imaging
(MRI), ultrasonography, and nuclear medicine studies of the liver have
been uninformative, with findings neither specific nor sensitive for
Wilson disease.
Electrocardiography
Resting electrocardiographic abnormalities include left ventricular or
biventricular hypertrophy, early repolarization, ST segment depression,
T-wave inversion, and various arrhythmias.
Serum Ceruloplasmin
Serum ceruloplasmin levels are low in newborns and gradually rise
within the first 2 years of life. Approximately 90% of all patients
with Wilson disease have ceruloplasmin levels of less than 20 mg/dL
(reference range, 20-40 mg/dL). (Ceruloplasmin is an acute phase
reactant and may be increased in response to hepatic inflammation,
pregnancy, estrogen use, or infection.)
Falsely low ceruloplasmin levels may be observed in any protein
deficiency state, including nephrotic syndrome, malabsorption,
protein-losing enteropathy, and malnutrition. Ceruloplasmin levels
may also be decreased in 10-20% of Wilson Disease gene
heterozygotes, who do not develop Wilson disease and do not
require treatment.
Urinary Copper Excretion and Hepatic Copper
Concentration
Urinary copper excretion
The urinary copper excretion rate is greater than 100 mcg/d
(reference range, < 40 mcg/d) in most patients with
symptomatic Wilson disease. The rate may also be elevated in
other cholestatic liver diseases.
Hepatic copper concentration
This test is regarded as the criterion standard for diagnosis of
Wilson disease. A liver biopsy with sufficient tissue reveals
levels of more than 250 mcg/g of dry weight even in
asymptomatic patients.
Brain MRI
MRI of the brain appears to be more sensitive than CT scanning in detecting
early lesions of Wilson disease.
MRI studies have identified focal abnormalities in the white matter, pons,
and deep cerebellar nuclei. These lesions, measuring 3-15 mm in diameter,
are typically bilateral, appearing with low signal intensity on T1-weighted
images and with high signal intensity on T2-weighted images, representing
cell loss and gliosis. Other studies describe decreased signal intensity in the
putamen and other parts of the basal ganglia, which may represent either
copper or iron ferritin deposition.
A characteristic "face of the giant panda" sign has been described, formed
by high signal intensity in the tegmentum (except for the red nucleus),
preserved signal intensity of the lateral portion of the pars reticulata of the
substantia nigra, and hypointensity of the superior colliculus.
PET Scanning
Positron emission tomography (PET) scanning reveals
a significantly reduced regional cerebral metabolic rate
of glucose consumption in the cerebellum, striatum,
and, to a lesser extent, in the cortex and thalamus.
PET scan analyses of patients with Wilson disease have
also demonstrated a marked reduction in the activity of
dopa-decarboxylase, indicative of impaired function of
the nigrostriatal dopaminergic pathway.
Management
Features of treatment of Wilson disease are as
follows:
The mainstay of therapy is lifelong use of
chelating agents (eg, penicillamine, trientine)
Symptoms, particularly neurologic ones, may worsen with initiation
of chelation
Surgical decompression or transjugular
intrahepatic shunting (TIPS) is reserved for
recurrent or uncontrolled variceal bleeding
unresponsive to standard conservative measures
Orthotopic liver transplantation is curative
Other treatments for Wilson disease include the following:
Anticholinergics, baclofen, GABA antagonists, and levodopa to treat
parkinsonism and dystonia
Antiepileptics to treat seizures
Neuroleptics to treat psychiatric symptoms
Protein restriction, lactulose, or both to treat hepatic
encephalopathy
After the initiation of therapy with a chelating agent, the
patient needs to be aware of potential adverse effects of the
agents with which he or she is being treated.
For instance, some of the concerning adverse
effects are those commonly associated with penicillamine use.
In addition, a patient must also be aware of the potential to develop
worsening of some symptoms when chelation is started; in particular,
patients with neurologic signs and symptoms can see worsening of these
with chelation, and, in some instances, therapy needs to be reduced or
stopped.
Laboratory tests in patients started on penicillamine should include
hematology and biochemical monitoring, as well as urinalysis.
With clinical progression, acute liver failure, or worsening
hepatic function, the patient must be evaluated at a center
with expertise in Wilson disease and the capability to perform
liver transplantation.
Orthotopic liver transplantation is curative treatment for
Wilson disease.
Diet
Patients should generally avoid eating foods with a high
copper content, such as liver, chocolate, nuts, mushrooms,
legumes, and shellfish (especially lobster). Drinking water
from atypical sources (eg, well water) should be analyzed for
copper content and replaced with purified water if the
copper content is greater than 0.2 parts per million.
Medication Summary
The mainstay of therapy for Wilson disease is the use of
chelating agents and
medications that block copper absorption from the
gastrointestinal (GI) tract.
Zinc and penicillamine are lifelong medications for patients with Wilson
disease. Dosages vary with the severity of the disorder.
Another chelating agent is trientine, which may be more easily tolerated
than penicillamine.[1] Patients who do not respond to zinc therapy and
who have increased activities of liver enzymes should be identified so
that chelating agents may be added to the therapeutic regimen.
Class Summary
Chelating agents bind excess copper. Ammonium tetrathiomolybdate is an investigational
chelating drug used at the University of Michigan as an initial treatment for patients who
present with neurologic or psychiatric manifestations. This drug works as a chelating agent
and as an inhibitor of copper absorption from the GI tract.[17]
Penicillamine (Cuprimine, Depen)
Penicillamine forms soluble complexes with metals excreted in urine. It was the drug of choice
before newer regimens were available. Because of extensive toxicities, alternative agents are
used. It must be administered with pyridoxine 25 mg by mouth daily.
Trientine (Syprine)
Trientine is an effective oral chelator used to induce cupruresis. It is useful for patients who
cannot tolerate penicillamine. It is indicated in Wilson disease if the initial presentation is
hepatic. It should be administered with zinc
Zinc (Galzin)
Zinc is a cofactor for more than 70 types of enzymes. It is approved for patients initially
treated with a chelating agent. It should be used for maintenance after initial chelation
therapy. Zinc acetate is the drug of choice in presymptomatic, pregnant, pediatric
populations, and in some instance for maintenance in compliant patients who have undergone
copper chelation therapy
Prognosis
Important clues for the diagnosis of Wilson disease that a
clinician must recognize are a younger patient with
hemolytic anemia, impaired hepatic synthetic function, and
normal alkaline phosphatase values.
The major complications in patients with untreated Wilson disease are those
associated with acute liver failure, chronic hepatic dysfunction with either
portal hypertension or hepatocellular carcinoma, and the sometimes-
relentless course to cirrhosis, which is characterized by a progressive
lassitude, fatigue, anorexia, jaundice, spider angiomas, splenomegaly, and
ascites. Bleeding from varices, hepatic encephalopathy, hepatorenal
syndrome, and coagulation abnormalities occur as liver failure ensues.
Death occurs, generally at age 30 years, if emergent liver transplantation is
not performed.
Complications
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Patient History and Presentation SkillsDocument4 pagesPatient History and Presentation Skillsbnarnold100% (2)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Toxicity of ToadsDocument29 pagesToxicity of ToadsAdarshBijapurNo ratings yet
- Musculoskeletal System (20000 Series) : A) 20205 B) 20206 C) 20225 D) 27324Document8 pagesMusculoskeletal System (20000 Series) : A) 20205 B) 20206 C) 20225 D) 27324JJKNo ratings yet
- Classic Radiology SignsDocument9 pagesClassic Radiology SignsJui DirDapNo ratings yet
- Pediatric Nursing GastroDocument3 pagesPediatric Nursing GastronieacatleyaNo ratings yet
- A Review of Drug-Induced Acute Angle Closure Glaucoma For Non-Ophthalmologists PDFDocument8 pagesA Review of Drug-Induced Acute Angle Closure Glaucoma For Non-Ophthalmologists PDFMeida Putri UtamiNo ratings yet
- Hepatitis EDocument7 pagesHepatitis EmdNo ratings yet
- Bac AmpicillinDocument2 pagesBac AmpicillinAnkush BiswasNo ratings yet
- Local AnestheticsDocument47 pagesLocal AnestheticsKeerthi LakshmiNo ratings yet
- Ballard Score Calculator: CalculatorsDocument1 pageBallard Score Calculator: Calculatorsbazlin syabrinaNo ratings yet
- Hemorrhage PathophysiologyDocument3 pagesHemorrhage PathophysiologyJubelle Sipalay0% (1)
- Substance Use Disorder Fact SheetDocument2 pagesSubstance Use Disorder Fact Sheetrandey92No ratings yet
- Health Benefits of Bicycle RidingDocument3 pagesHealth Benefits of Bicycle RidingPeter JohnsonNo ratings yet
- Art Therapy What Is Art Therapy?Document2 pagesArt Therapy What Is Art Therapy?rohit singhNo ratings yet
- Sialometria ClinicaDocument4 pagesSialometria ClinicaDr. JharNo ratings yet
- Patho Safe Insert 04-2020V2Document3 pagesPatho Safe Insert 04-2020V2Luciano LopezNo ratings yet
- 1.1 Background of The StudyDocument13 pages1.1 Background of The StudyJeth DayNo ratings yet
- Uk Guidelines SarcomaDocument21 pagesUk Guidelines Sarcomachu_chiang_3No ratings yet
- Henoch Schonlein Purpura GuidelineDocument12 pagesHenoch Schonlein Purpura GuidelinewenyinriantoNo ratings yet
- Management of Anembryonic Pregnancy Loss: An Observational StudyDocument6 pagesManagement of Anembryonic Pregnancy Loss: An Observational StudyAnonymous ORleRrNo ratings yet
- Hospital Setup (Equipment) - by Harleys DistributorsDocument5 pagesHospital Setup (Equipment) - by Harleys DistributorsKevinNo ratings yet
- Acid-Base Balance: Graciela Lou F. Mana-Ay, RN, ManDocument68 pagesAcid-Base Balance: Graciela Lou F. Mana-Ay, RN, ManKeshia Joyce LimNo ratings yet
- Icd-10 Oktober 2021Document9 pagesIcd-10 Oktober 2021Nia KurniawatiNo ratings yet
- Treatment of Hyperprolactinemia A.7Document4 pagesTreatment of Hyperprolactinemia A.7Leyni fanny guerrero limaNo ratings yet
- NCM312 PPT Operating Room NursingDocument132 pagesNCM312 PPT Operating Room NursingNine SoleilNo ratings yet
- Analisis Kesesuaian Penggunaan Antiinfeksi Pada Infeksi Oportunistik Pasien Hiv/Aids Rawat Inap Di Rsup Dr. Sardjito YogyakartaDocument7 pagesAnalisis Kesesuaian Penggunaan Antiinfeksi Pada Infeksi Oportunistik Pasien Hiv/Aids Rawat Inap Di Rsup Dr. Sardjito YogyakartaindahNo ratings yet
- A Survey of Cross-Infection Control Procedures: Knowledge and Attitudes of Turkish DentistsDocument5 pagesA Survey of Cross-Infection Control Procedures: Knowledge and Attitudes of Turkish Dentistsbie2xNo ratings yet
- Joint Pain Leaflet PDFDocument12 pagesJoint Pain Leaflet PDFSuaeni Kurnia Wirda100% (1)
- Resume Tatiana HajouDocument1 pageResume Tatiana Hajouapi-338525355No ratings yet
- Acute Gastrointestinal HemorrhageDocument21 pagesAcute Gastrointestinal HemorrhageWarthinNo ratings yet