Professional Documents
Culture Documents
Wound Healing and An Approach To Dressings
Uploaded by
yosuemvOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Wound Healing and An Approach To Dressings
Uploaded by
yosuemvCopyright:
Available Formats
Wound Healing
and an
Approach to Dressings
By
Daniel Nagase
Introduction
Wound Trauma to any of the tissues of the body,
causing interruption of tissue continuity.
Wound Healing A combination of regeneration and
repair, involving hemostasis, extracellular matrix
synthesis, wound contraction, and epithelialization,
leading to the restoration of form and function of the
injured tissue.
NORMAL WOUND HEALING
PHASES OF WOUND HEALING
INFLAMMATORY
PROLIFERATIVE
REMODELLING
PHASES OF WOUND HEALING
Inflammatory
Hemostasis - Clotting factors activated by
exposed basement membrane proteins
and collagen
Clotting Cascade results in Fibrin
Traps Platelets and RBCs forming a platelet Plug
Inflammatory
Platelet Aggregation and Activation :
- PDGF
- TGF-
- IGF-1
- VWF
- Also release serotonin, which causes
vasodilation and increased vascular
permeability
Inflammatory
Neutrophils : 6-48 hrs
Kill Bacteria
Debride tissue proteases degrade damaged
ECM
Secrete cytokines to cause inflammation
Inflammatory
Monocytes : 48-72 hrs
Attracted to wound by cytokines (eg. TGF- )
Extravasate and turn into Macrophages
Secrete more cytokines to initiate proliferative
phase
Lymphocytes
Modulate extent of inflammation
Proliferative
Begins day 2-3 after wounding
Lasts 2-4 weeks
Angiogenesis
Fibroplasia
Epithelialization
Proliferative
Angiogenesis - necessary to support a wound environment that can
repair the injury
Macrophage derived growth factors stimulate angiogenesis
FGF
TGF-, TGF-
TNF-
Also stimulated by hypoxia, fibronectin and hyaluronic acid, which are found
in the wound matrix
Endothelial cells proliferate, neovascularity visible through epithelium =
pink appearance
Supplies Oxygen and nutrients for fibroblast proliferation and production
of wound matrix
Proliferative
Fibroblasts migrate into wound on fibrin skeleton left
behind from hemostasis
Macrophage derived growth factors stimulate
proliferation of fibroblasts
Collagen synthesized at an accelerated rate
Collagen levels rise for 3 weeks (Type I : III ratio increases to Normal
4:1)
As levels rise, number of fibroblasts diminishes
When Rate of collagen synthesis = rate of degredation
Collagen Homeostasis
Proliferative
Epithelialization
Cells in basal layer at wound edge flatten
Dedifferentiation
Pseudopod formation
Migrate across wound - integrin receptors in underlying
extracellular matrix
Cells along margin divide to reform mature, multilayered
epithelium
For surgical wound : complete wound coverage in 24-48 hrs.
Proliferative
Epithelialization
Process compromised by:
Bacteria
Protein exudate from leaky capillaries
Necrotic debris
Delayed epithelialization = prolonged & profound
inflammatory process
Facilitated by clean moist wound
Remodeling
3 weeks - 1 year
Supranormal rates of collagen synthesis and
degradation during remodeling. No change in
collagen content
Tensile strength gradually increases as random
collagen fibrils form intermollecular bonds
Collagen fibrils align in longitudinal direction as
dictated by stress placed on wound
Scars never reach degree of order in normal skin
Achieve 70% - 80% of strength of unwounded skin
NORMAL WOUND HEALING
Inflammatory Phase
If low bacterial contamination, macrophages
promptly replace PMNs
Macrophages complete process of removing all
material not necessary for ensuing steps of
wound healing
Macrophages not just phagocytic
Macrophages source of >30 growth factors &
cytokines
NORMAL WOUND HEALING
Inflammatory Phase
Fibroblast Endothelial cell
proliferation proliferation
(ANGIOGENESIS)
MACROPHAGE
Extracellular matrix Recruitment of
production additional macrophages
NORMAL WOUND HEALING
TYPES OF WOUND HEALING
1
st
Intention (Primary) Healing
2
nd
Intention (Secondary) Healing
3
rd
Intention (Tertiary) Healing
= Delayed Primary Closure
Partial Thickness Wounds
NORMAL WOUND HEALING
TYPES OF WOUND HEALING
1
st
INTENTION (Primary) HEALING
Wound closed within 24 hours
Prior to formation of granulation tissue
Fastest healing
Generally best cosmetic result
Treatment of choice for non-infected wound
Time!! Infection Rate Time since wounding
Golden Period vs. individual evaluation
NORMAL WOUND HEALING
TYPES OF WOUND HEALING
2
nd
INTENTION (Secondary) HEALING
Open wound allowed to close by
Contraction & Epithelialization
Contraction by myofibroblasts
Myofibroblasts disappear as contraction
completed
Direct correlation between number of
myofibroblasts and extent of wound contraction
NORMAL WOUND HEALING
TYPES OF WOUND HEALING
3
rd
INTENTION (Tertiary) HEALING
= DELAYED PRIMARY CLOSURE
Contaminated, left open to prevent infection
Normal host defenses debride wound
After 3-4 days, local phagocytes and
inflammatory cells recruited and angiogenesis
Wound edges approximated
Collagen metabolism undisturbed
Tensile strength develops as if primary closure
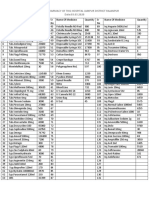
TABLE 3 -- AGENTS THAT PROMOTE EPIDERMAL RESURFACING
Dressing Relative Rate of Healing (%)
DuoDerm +36
Blisterfilm +33
Benzoyl peroxide (20%) +33
Bacitracin zinc +30
Silvadene +28
Neosporin +28
Polysporin +25
J&J First Aid Cream +20
Bioclusive +20
Op-Site +18
From Alvarez O: Moist environment: Matching the dressing to the wound.
Ostomy/Wound Manage 12:64-83, 1988, with permission.
TABLE 4 -- AGENTS THAT DELAY EPIDERMAL RESURFACING
Dressing Relative Rate of Healing (%)
Neomycin sulfate -5
Dakin solution (1%) -6
Hibiclens -7
Hydrogen peroxide (3%) -8
Povidone-iodine solution -10
Wet-to-dry gauze -15
Liquid detergent -28
Furacin -30
Triamcinalone acetonide (0.1%) -34
From Alvarez O: Moist environment: Matching the dressing to the wound.
Ostomy/Wound Manage 12:64-83, 1988; with permission.
Principles
1) Protection
2) Absorption
3) Compression
4) Immobilization
5) Aesthetics
TABLE 20-7 -- Burn Wound Dressings
Burn Wound Dressings Advantages and Disadvantages
Antimicrobial Salves
Silver sulfadiazine (Silvadine) Broad-spectrum antimicrobial; painless and easy to use; does not penetrate eschar; may leave black
tattoos from silver ion; mild inhibition of epithelialization
Mafenide acetate (Sulfamyalon) Broad-spectrum antimicrobial; penetrates eschar; may cause pain in sensate skin; wide application may
cause metabolic acidosis; mild inhibition of epithelialization
Bacitracin Ease of application; painless; antimicrobial spectrum not as wide as the above agents
Neomycin Ease of application; painless; antimicrobial spectrum not as wide
Polymyxin B Ease of application; painless; antimicrobial spectrum not as wide
Nystatin (Mycostatin) Effective in inhibiting most fungal growth; cannot be used in combination with Sulfamyalon
Mupirocin (Bactroban) More effective staphylococcal coverage; does not inhibit epithelialization, expensive
Antimicrobial Soaks
0.5% silver nitrate Effective against all microorganisms; stains contacted areas; leaches sodium from wounds; may cause
methemoglobinemia
5% mafenide acetate Wide antibacterial coverage; no fungal coverage; painful on application to sensate wound; wide
application associated with metabolic acidosis
0.025% sodium hypochlorite (Dakins solution) Effective against almost all microbes, particularly gram-positive organisms; mildly inhibits
epithelialization
0.25% acetic acid Effective against most organisms, particularly gram-negative organisms; mildly inhibits
epithelialization
Synthetic Coverings
OpSite Provides a moisture barrier; inexpensive; decreased wound pain; use complicated by accumulation of
transudate and exudate requiring removal; no antimicrobial properties
Biobrane Provides a wound barrier; associated with decreased pain; use complicated by accumulation of exudate
risking invasive wound infection; no antimicrobial properties
Transcyte Provides a wound barrier; decreased pain; accelerated wound healing; use complicated by accumulation
of exudate; no antimicrobial properties
Integra Provides complete wound closure and leaves a dermal equivalent; sporadic take rates; no antimicrobial
properties
Biologic Coverings
Xenograft (pig skin) Completely closes the wound; provides some immunologic benefits; must be removed or allowed to
slough
Allograft (homograft, cadaver skin) Provides all the normal functions of skin; can leave a dermal equivalent; epithelium must be removed or
allowed to slough
Dressings
Dressing
Derived from French word drecier, which
means to make straight, to make right, and
to put in proper order
Pare (1510-1590)
I dressed the wound and God healed it.
Winter (1962)
Moist wounds heal better than those
exposed to air
Dressings
Moist wound healing
Achieved by occluding the wounds such that
the bodys own fluids accumulate at the
wound-dressing interface and prevent
dehydration and dessication
Occlusive dressings do not cause infection
Ideal Dressing
Removes exudate and toxic components
Maintains high humidity at interface
Allows gaseous exchange
Insulates thermally
Protects from secondary infection
Allows removal without trauma
Dressing Based on Exudate
Minimal to mild
Hydrocolloid (duoderm)
Polyurethane (tegaderm)
Saline gauze
Moderate to Heavy
Alginate (sorbsan)
Stomal collection bag
Hypertonic saline gauze (Mesalt)
Dressing based on wound color
Red (granulation) or pink (epithelialization)
Keep clean, moist
Cover with tegaderm, hydrocolloid
Polysporin, jelonet
Yellow
Debride
Absorbant dressing or saline gauze (change bid or
tid)
Hydrocolloid changed every 7 days
Black
Debridement, dressings as for yellow wound
Dressings for Pressure Sores
Grade I
Polyurethane or hydrocolloid dressing for
protection
Grade II or III
Clean ulcer: saline gauze, wetmoist;
polyurethane; hydrocolloid; hydrogel
Infected ulcer:topical antiseptic; saline gauze
wetdry (avoid use >5days)
Dressings for Pressure Sores
Grade IV
Clean ulcer: saline gauze, wetmoist;
hydrocolloid; hydrogel
Infected ulcer: topical antiseptic; saline gauze,
wetdry
Marjolins Ulcer
1828: Marjolin described a tumor in a chronic
wound
Dupuytren noted it was malignant
Marjolins ulcer describes a carcinoma arising
in a chronic wound
Usually SCC
Aggressive, poor survival rate
Metastatic rate 61% vs 34% for Marjolins
ulcer in burn scars
Treatment- wide excision to clear margins
Wound VAC
Exposure of wound bed to negative
pressure in a closed system
Benefits
Removes edema fluid from extravascular
space
Stimulates cellular proliferation
Improves blood flow
Maggot Therapy
Beneficial effects of maggots in
suppurative wounds first noted by
Ambroise Pare in the 16th century
Also described by Fabricius (1634) and
Larrey, a surgeon in Napoleans army
Baer (1917)- two soldiers with compound
femur fractures, untreated for 7 days,
found to be infested with thousands of
maggots!
Healthy granulation tissue beneath!
Standard treatment of the day produced
a mortality rate of 75%
Maggot Therapy
Mumcuoglu et al. Int. J. Dermatology, 1999
25 patients with chronic leg ulcers and sacral
pressure sores that failed standard therapy were
treated using maggots of Phaenicia sericata
wounds present 1-90 months
sterile maggots (50-1000) applied to wound 2-5 times
weekly and replaced every 1-2 days
88% complete debridement
7% significant debridement
5 patients initially referred for amputation had limb
salvaged
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Top 70 Microbiology RegulationsDocument3 pagesThe Top 70 Microbiology RegulationsRudra RahmanNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- CR FormatDocument4 pagesCR FormatSri HariNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Available Medicine at Pharmacy of THQ Hospital Jampur District Rajanpur Date:03.03.2020Document2 pagesAvailable Medicine at Pharmacy of THQ Hospital Jampur District Rajanpur Date:03.03.2020Kashif AhmadNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Malocclusion (2nd Concept Map)Document4 pagesMalocclusion (2nd Concept Map)Stephanie Joy EscalaNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Mason 2021 Feasibility and Acceptability of ADocument9 pagesMason 2021 Feasibility and Acceptability of AjorgeNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Navrekar - LWM PPT For Workshop 16 JulyDocument40 pagesNavrekar - LWM PPT For Workshop 16 JulyQudratullah ShaikNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Introduction To Community Health NursingDocument20 pagesIntroduction To Community Health NursingKrishnaveni MurugeshNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Research Paper: Coaching and Counseling - What Can We Learn From Each Other?Document11 pagesResearch Paper: Coaching and Counseling - What Can We Learn From Each Other?International Coach AcademyNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- PsyHx and MSEDocument25 pagesPsyHx and MSERazel AnneNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- Patient Warfarin Education Review 2005Document6 pagesPatient Warfarin Education Review 2005Mano cempakaNo ratings yet
- Botulinum Toxin Treatment in Clinical Medicine PDFDocument309 pagesBotulinum Toxin Treatment in Clinical Medicine PDFjesussalvadorsuaza100% (1)
- Beta-Blockers: Friend or Foe in Asthma?: International Journal of General Medicine DoveDocument7 pagesBeta-Blockers: Friend or Foe in Asthma?: International Journal of General Medicine DoveastriedamaliaamanatNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- SystemOne 60 Series REMstar Auto User ManualDocument28 pagesSystemOne 60 Series REMstar Auto User Manualmanojsingh4allNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- AmpicillinDocument1 pageAmpicillinMichael KuzbytNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Pancreas functions in digestion and glucose metabolismDocument4 pagesPancreas functions in digestion and glucose metabolismClayton VerBerkmösNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- UNANSWERED Past Plab 1700 McqsDocument260 pagesUNANSWERED Past Plab 1700 McqsHassaan Imtiaz100% (5)
- Myers 7th Edition Psychology: Chapter 17 OutlineDocument6 pagesMyers 7th Edition Psychology: Chapter 17 OutlineHockeyboy41100% (3)
- Integrated Management of Childhood IllnessDocument2 pagesIntegrated Management of Childhood Illness지창욱No ratings yet
- ALDAHOL OLYMPUS CompatibilityDocument6 pagesALDAHOL OLYMPUS CompatibilityMaria TorresNo ratings yet
- National Minimum Prevention MPPI GuideDocument20 pagesNational Minimum Prevention MPPI GuideEmmanuel Umo EffiongNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Salient Features of Water ActDocument4 pagesSalient Features of Water Actparth sarthi100% (2)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Manaois - Drug STUDY (Lorazepam)Document2 pagesManaois - Drug STUDY (Lorazepam)Dan Dan ManaoisNo ratings yet
- Ap Psychology Unit 8 Overview 2015Document5 pagesAp Psychology Unit 8 Overview 2015api-262090199No ratings yet
- Qualitative Research InterviewsDocument8 pagesQualitative Research InterviewsDaniel Fancis Amabran BarrientosNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Precancerous Lesions of The Gynecologyc Tract - 2016 PDFDocument324 pagesPrecancerous Lesions of The Gynecologyc Tract - 2016 PDFCésar Garavito Quijaite50% (2)
- Assessment Diagnosis Rationale Planning Interventions Rationale EvaluationDocument3 pagesAssessment Diagnosis Rationale Planning Interventions Rationale EvaluationJharene BasbañoNo ratings yet
- The Residency Towers: 15 - 16 SeptemberDocument10 pagesThe Residency Towers: 15 - 16 SeptembervamshidhNo ratings yet
- Outcomes of Percutaneous Endoscopic Gastrostomy in ChildrenDocument7 pagesOutcomes of Percutaneous Endoscopic Gastrostomy in ChildrenHenry BarberenaNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Pic Heart Talk Final Programme (19-10-13)Document4 pagesPic Heart Talk Final Programme (19-10-13)usman9117563No ratings yet
- Doctor-Patient Communication A ReviewDocument6 pagesDoctor-Patient Communication A ReviewWagiono SuparanNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)