Professional Documents
Culture Documents
CPAP Slides
Uploaded by
Anusha VergheseCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
CPAP Slides
Uploaded by
Anusha VergheseCopyright:
Available Formats
CPAP
Types of CPAP
Boussignac
Oxypeep
Whisperflow Flow Generators
Emergent Products PortO2vent
CAREvent ALS + CPAP
Physiology of CPAP
Vital Terminology
Tidal Volume (Vt)
Minute Volume (Vm)
Peak Inspiratory Flow
Functional Reserve
Capacity (FRC)
Inspired Oxygen (FiO2)
Work of Breathing
(WOB)
Airway and Respiratory Anatomy and
Physiology
Pathway review
Oxygenation and Ventilation
Functional Residual Capacity
Work of breathing
Airway and Respiratory Anatomy
Pathways-
Airway and Respiratory Anatomy
Pathways-
Airway and Respiratory Physiology
The Pressure gradient!
Aveolar Air has higher content
of OXYGEN than venous
(deoxygenated) blood
Therefore oxygen transfers
from the air into the blood.
This is called the Pressure
Gradient
The higher the inspired
oxygen (FiO2) the better the
pressure gradient!
Airway and Respiratory Physiology
Oxygen Saturation Curve
Picture released into public domain by wikipedia
Airway and Respiratory Physiology FRC
Functional reserve Capacity (FRC) is the volume of air in
the lungs at the end of a normal passive expiration.
approximately 2400 ml in a 70 kg, average-sized male
FRC decreases with lying supine, obesity, pregnancy and
anaesthesia.
Important aim of CPAP is to increase functional residual
capacity (FRC)
By increasing he FRC, the surface area of the Aveoli is distended
(increased).
Greater surface area improves gas exchange (oxygenation and
ventilation)
This improves Spo2/SaO2
Airway and Respiratory Physiology
WOB
Work of breathing (WOB) is respiratory effort to effect oxygenation
and ventilation.
Important aim of CPAP is to reduce work of breathing (WOB)
Airway and Respiratory Physiology
WOB
Signs of increased WOB:
Dyspnea on Exertion (DOE)
Speech Dyspnea
Tripoding
Orthopnea
Accessory Muscle Use/Restractions
Lung Sounds
Doorway Test
Silent Chest!!!!
Airway and Respiratory Physiology
WOB
Increased WOB :
Respiratory Fatigue
Respiratory Distress
Respiratory Failure
CPAP reduces WOB
Airway and Respiratory Pathology
Airway and Respiratory Pathology
CHF
Precipitating Causes
Non Compliance with Meds and Diet
Acute MI
Arrhythmia (e.g. AF)
Increased Sodium Diet (Holiday Failure)
Pregnancy (PIH, Pre-eclampsia, Eclampsia)
Airway and Respiratory Pathology
CHF
Severe resp distress
Foamy blood tinged
sputum
Accessory muscle use
Apprehension, agitation
Speech Dyspnea
Diaphoresis
Bilateral crackles or Rhales
Orthopnea (cant lie down)
Paroxysmal nocturnal
dyspnea (PND)
Cyanosis
Pedal Edema
JVD
Chest pain (possible
co-existent AMI)
abnormal vitals (increased
B/P; rapid pulse; rapid &
labored respirations
Cardiac Asthma?
Fluid leaks into the Interstitial Space
Airways narrow
Mimics broncoconstriction seen in asthma
May actually exacerbate asthma if a co-existing PMHx
Produces Wheezing
Infiltration of Interstitial Space
mal
Micro-anatomy
Micro-anatomy
with fluid
movement.
Airway and Respiratory Pathology CHF
The following treatments should be done concurrently with CPAP, patient
condition permitting*.
High Flow Oxygen!!!
Nitroglycerin *
0.4 mg sl every 5 minutes;
0.5-2 inches transdermal
5-200 mcg/min IV Drip
Lasix *
20- 80 mg IV/IM (or double daily dose if already on Lasix)
Opiates*
Reduce Anxiety
Mild Vasodilator
2.5-5 mg q5 minutes IVP
(* = defer to local protocol or medical control)
Airway and Respiratory Pathology
Asthma and COPD
Obstructive vs Reactive airways
Bronchoconstrictive issues
Poor Gas Exchange
Accessory Muscle Use/Muscle
Tiring
CPAP is best reserved for those
patients who are refractory to
normal interventions, and have a
severe presentation.
At least TWO doses of
bronchedialtors should be
administered before the provider
initiates CPAP.
Airway and Respiratory Pathology
Asthma and COPD
The following treatments should be done concurrently with CPAP, patient
condition permitting*.
High Flow Oxygen!!!
Bronchodilators*
Albuterol 2.5 mg (0.83% in 3 cc)/ Atrovent 0.5 mg (0.02% in 2.5 cc)
nebulized.
Repeat as needed with Albuterol Only.
Do not dilute.
Magnesium Sulfate* (Asthma extremis only)
IV: 2 g given SLOWLY, diluted.
Do not give faster than 1 g/minute.
Epinephrine 1:1,1000
0.3-0.5 mg IM/SQ for severe refractory bronchospasm
Use Epinephrine with caution on patients over 65 or with cardiac
history.
Solu-medrol
IV/IM: 125 mg
(* = defer to local protocol or medical control)
Airway and Respiratory Pathology
Pneumonia
Infectious process
Often confused with, or masked by, CHF
Detailed assessment required
PMhx, Med list review
Sputum type/color
Onset of s/s
Fever
Lack of CHF/Afib Hx
Normal CHF Tx may be ineffective or detrimental
Nitroglycerine (ineffective)
Diuretics (detrimental)
Airway and Respiratory Pathology
Pneumonia
CPAP may be of minimal benefit in Pneumonia*.
High Flow Oxygen!!!
Bronchodilators*
Albuterol 2.5 mg (0.83% in 3 cc)/ Atrovent 0.5 mg (0.02% in 2.5 cc)
nebulized.
Repeat as needed with Albuterol Only.
Do not dilute.
(* = defer to local protocol or medical control)
Airway and Respiratory Pathology
Drowning
CPAP may be beneficial to the drowning/near drowning patient
Strongly consider intubation for severe s/s refractory to CPAP and
other treatments
Other uses of CPAP
ARDS
Acute Respiratory Failure
Anesthesia (Pre-Op and Post-Op)
Atelectasis
Alternative to Mechanical Ventilation
Weaning from Mechanical Ventilation
Left Ventricular Failure
Renal Failure
Sleep Apnea
Physiology of CPAP
Physiology of CPAP
Airway pressure maintained at set level
throughout inspiration and expiration
Maintains patency of small airways and alveoli
Stents small airways open
Distends aveoli
Improves delivery of bronchodilators
By up to 80%
Moves extracellular fluid into vasculature
Improves gas exchange
Reduces work of breathing
Physiology of CPAP : CPAP Mechanism
Increases pressure within
airway.
Airways at risk for collapse
from excess fluid are
stented open.
Gas exchange is maintained
Increased work of breathing
is minimized
Physiology of CPAP : Redistribution
of pulmonary edema with CPAP
Physiology of CPAP: Hypotension
CPAP increases intrathoracic pressure
This decreases cardiac output causing hypotension
Therefore hypotensive patients may have are relatively
contraindicated with CPAP...
Physiology of CPAP : Administration of
Medications by CPAP
CPAP and Nebulizers can be used together to provide better
penetration of nebulizer medications through the respiratory
tract.
Use of CPAP by EMS
Goals of CPAP use in the field
Primary Goals
Increase amount of inspired oxygen (FiO2)
Increase the SpO2 and PaO2 of the patient
Decrease the work load of breathing (WOB)
To reduce overall mortality
Secondary Goals:
Reduce the need for emergent intubations of the patient
Decrease hospital length of stay (LOS)
CPAP vs. Intubation
CPAP
Non-invasive
Easily discontinued
Easily adjusted
Use by EMT-B (in some
states)
Minimal complications
Does not (typically)
require sedation
Comfortable
Intubation
Invasive
Intubated stays
intubated
Requires highly trained
personnel
Significant complications
Can require sedation or
RSI
Potential for infection
Key Point:
This module discusses CPAP in patients >8 years
of age
CPAP has been safely used in children, infants,
and neonates in the in-hospital and critical care
settings
Local protocols may allow use in children and
infants
Appropriate sized equipment mandatory
Risk increases
Consult medical control and local protocols
Indications
For consideration (for patients <8) in moderate to severe
respiratory distress secondary to:
CHF/APE
Acute Respiratory Failure
asthma/reactive airway disease,
near drowning,
COPD,
acute pulmonary edema (cardiogenic and non cardiogenic),
pneumonia who present with any of the following:
Pulse oximetry < 88% not improving with standard therapy
ETCO2 > 50mmHg
Accessory muscle use / retractions
Respiratory rate > 25
Wheezes, rales, rhonchi
Signs of respiratory fatigue or failure
A note on misdiagnosis
There is a significant misdiagnosis rate of CHF in the field, most
commonly confused with pneumonia
CPAP still demonstrated significant improvement in other (non-
CHF/APE) respiratory emergencies
Risks are greater in non CHF/APE
CPAP Max Pressures are lower non CHF/APE
Caution is required non CHF/APE
2003 Helsinki EMS Looked at patients in Acute Severe
Pulmonary Edema (ASPE)
Study Group: 121
Confirmed CHF: 38 (32%)
Miss- DX: 83 (68%)
Non CHF Patients that got
better with CPAP: 34 (28%)
Non CPAP mortality (17.8%)
CPAP Mortality (8%)
Other Notes:
Confirmed by MNP
Treated with Low-Mid FiO2, Nitrates. No Lasix
4 intubated in field (3%)
(Kallio, T. et al. Prehospital Emergency Care. 2003. 7(2) )
Contraindications/Exclusion
Criteria
Physiologic
Unconscious, Unresponsive, or inability to protect airway.
Inability to sit up
Respiratory arrest or agonal respirations (Consider Intubation)
Persistent nausea/vomiting
Hypotension- Systolic Blood Pressure less than 90 mmHg
Inability to obtain a good mask seal
Pathologic
Suspected Pneumothorax
Shock associated with cardiac insufficiency
Penetrating chest trauma
Facial anomalies /trauma/burns
Closed Head Injury
Has active upper GI bleeding or history of recent gastric surgery
Vomiting
Cautions
History of Pulmonary Fibrosis
Claustrophobia or unable to tolerate mask (after initial
1-2 minutes)
Coaching essential
Consider mild sedation
Has failed at past attempts at noninvasive ventilation
Complains of nausea or vomiting
Has excessive secretions
Has a facial deformity that prevents the use of CPAP
Administration
CPAP is measured in
cm/H2O
Start with device in the
lowest setting, and titrate
upward.
Initial dose at 0-2 cm/H2O
Titrated up to*:
10 cm/H2O MAX for CHF or,
5 cm/H2O MAX for COPD, near
drowning, and respiratory
failure form other causes.
(* = defer to local protocol or medical control)
Complications
CPAP may drop BP due to increased intrathoracic pressure.
A patient must have a systolic BP of at least 90mmHg to be a candidate
for CPAP
Increased Intrathoracic pressure means decreased ventricular filling and
increased afterload, thus decreasing cardiac output and blood pressure.
Providers should be comfortable giving a CPAP patient NTG If they are
too hypotensive for NTG, then they are too hypotensive for CPAP.
Risk of pneumothorax
Increased intrathoracic pressure = increased risk
Higher in Asthmatics and COPD
Gastric Distention, and vomiting
Strongly consider placement of a gastric tube (if in scope of practice)
Risk of corneal drying
High volumes of air blowing at eyes, especially on long transports.
Discontinuing of CPAP
CPAP therapy needs to be continuous and should not be
removed unless the patient:
cannot tolerate the mask, success of tolerance to the treatment
increased with proper coaching by EMS crew
requires suctioning or airway intervention,
experiences continued or worsening respiratory failure,
Develops severe hypotension
or a pneumothorax is suspected.
Intermittent positive pressure ventilation and/or
intubation should be considered if patient is removed
from CPAP therapy.
Documentation
Dosage
CPAP level (10cmH2O)
FiO2 (100%)
Subjective response to therapy
Objective response to therapy
Lung Sounds,
Work of Breathing
SPO2
Nasal ETCO2
SpO2 q5 minutes
Vital Sign q5 minutes
Any adverse reactions
Justification for sedation,
intubation, or discontinuation of
CPAP. Be specific.
Documentation: Modified Borg
Scale
0-No breathlessness at all
1-Very slight
2-Slight breathlessness
3-Moderate
4-Somewhat severe
5-Severe
7-Very severe
9-Very, very severe (Almost maximum)
10-Maximum
CPAP and Intubation
Intubation will be inevitable in some patients regardless
of the use of CPAP, and the paramedic must be prepared
for rapid intervention by RSI/MAI or other means as
feasible.
Indications to proceed to ET placement are (not all
inclusive):
Deterioration of mental status
Increase of the EtCO2
Decline of SpO2
Progressive fatigue
Ineffective tidal volume
Respiratory or cardiac arrest.
You might also like
- Energy Conservation TechniquesDocument9 pagesEnergy Conservation Techniquesqwas zNo ratings yet
- Basic Principles of Mechanical Ventilation Andventilator GraphicsDocument70 pagesBasic Principles of Mechanical Ventilation Andventilator GraphicsSupriya PattnayakNo ratings yet
- ArticlesOfConfederation Constitution 3.0Document6 pagesArticlesOfConfederation Constitution 3.0ChristinaNo ratings yet
- Understanding Mechanical Ventilation: Jennifer Zanni, PT, DSCPT Johns Hopkins HospitalDocument52 pagesUnderstanding Mechanical Ventilation: Jennifer Zanni, PT, DSCPT Johns Hopkins HospitalDeepa BhattacharjeeNo ratings yet
- Lung Expansion 1Document31 pagesLung Expansion 11trindogg100% (2)
- Basics of Ventilatory SupportDocument43 pagesBasics of Ventilatory SupportAdhithya Bhat100% (1)
- Physiotherapy Management in Icu Patients: Dr.S.Ramachandran MPTDocument37 pagesPhysiotherapy Management in Icu Patients: Dr.S.Ramachandran MPTvaishnaviNo ratings yet
- DR - Kannan Nair JR - Consultant Apollo HospitalsDocument62 pagesDR - Kannan Nair JR - Consultant Apollo HospitalsKannan NairNo ratings yet
- Overview of Respiratory Failure & Use of Mechanical VentilationDocument89 pagesOverview of Respiratory Failure & Use of Mechanical VentilationsheharyarNo ratings yet
- Ventilator Weaning and Spontaneous Breathing Trials An Educational Review 2016Document7 pagesVentilator Weaning and Spontaneous Breathing Trials An Educational Review 2016Tarran PhagooNo ratings yet
- Pulsus ParadoxusDocument2 pagesPulsus ParadoxusHassan.shehriNo ratings yet
- Convention Modes of Mechanical Ventilation. DR - purwOKODocument53 pagesConvention Modes of Mechanical Ventilation. DR - purwOKOIsnia WahibNo ratings yet
- Ambulation Aids and Patterns 2018Document59 pagesAmbulation Aids and Patterns 2018venkata ramakrishnaiah100% (1)
- King Airway: Norcal Ems Training ModuleDocument13 pagesKing Airway: Norcal Ems Training Moduleandrew22No ratings yet
- 4 Weaning Ventilator-NIADocument31 pages4 Weaning Ventilator-NIAResyana Widyayani100% (1)
- Cardiopulmonary Bypass: Dr. Ravi Gadani MS, FmasDocument24 pagesCardiopulmonary Bypass: Dr. Ravi Gadani MS, FmasRaviNo ratings yet
- PAINLESS DELIVERY - PPDocument17 pagesPAINLESS DELIVERY - PPrafiaNo ratings yet
- Icu Initial Ventilator SettingsDocument40 pagesIcu Initial Ventilator SettingsantreaspetsasNo ratings yet
- Regional AnesthesiaDocument54 pagesRegional AnesthesiaIdza Fariha AfriNo ratings yet
- Airway Obstruction - Types, Causes, and SymptomsDocument6 pagesAirway Obstruction - Types, Causes, and SymptomsGilbertLiem100% (1)
- Preoperative Assessment Hairina MazlanDocument27 pagesPreoperative Assessment Hairina MazlanHairina MazlanNo ratings yet
- Cardiorespiratory AssessmentDocument7 pagesCardiorespiratory AssessmentmalarvelykNo ratings yet
- Preoperative EvaluationDocument47 pagesPreoperative EvaluationCzerwin Juales100% (2)
- Nursing Care of Patients With Pneumothorax: Prepared By: N. WadeDocument33 pagesNursing Care of Patients With Pneumothorax: Prepared By: N. WadeokaciaNo ratings yet
- Spinal Anaesthesia A Practical GuideDocument14 pagesSpinal Anaesthesia A Practical GuideNovita WulandariNo ratings yet
- Journal ClubDocument26 pagesJournal Clubysindhura23gmailcom100% (1)
- Anaesthetic Management of Joint Replacement SurgeriesDocument55 pagesAnaesthetic Management of Joint Replacement SurgeriesRaguNo ratings yet
- Airway AdjunctsDocument17 pagesAirway AdjunctsChannelGNo ratings yet
- Acute Respiratory Distress SyndromeDocument70 pagesAcute Respiratory Distress SyndromeAndrea Del Villar100% (1)
- Posterior Cranial Fossa Anesthetic ManagementDocument48 pagesPosterior Cranial Fossa Anesthetic ManagementDivya Rekha KolliNo ratings yet
- Patient Controlled AnalgesiaDocument129 pagesPatient Controlled AnalgesiamehranerezvaniNo ratings yet
- Mechanical VentilationDocument40 pagesMechanical VentilationPratik SahooNo ratings yet
- Pneumonectomy 2Document7 pagesPneumonectomy 2jeanelineNo ratings yet
- RSI For Nurses ICUDocument107 pagesRSI For Nurses ICUAshraf HusseinNo ratings yet
- CQI Presentation Feb'24Document94 pagesCQI Presentation Feb'24Neeti NayakNo ratings yet
- Premedication: by Alif Moderator: Dr. JasmineDocument45 pagesPremedication: by Alif Moderator: Dr. JasmineAlef AminNo ratings yet
- Management of Intraoperative Bronchospasm: Dr. ImranDocument49 pagesManagement of Intraoperative Bronchospasm: Dr. ImranhellodrvigneshwarNo ratings yet
- General AnaesthesiaDocument53 pagesGeneral Anaesthesiapeter singal100% (2)
- Anesthesia ManualDocument21 pagesAnesthesia ManualDocFrankNo ratings yet
- Advanced Airway Management: Leaugeay Webre, BS, CCEMT-P, Nremt-PDocument35 pagesAdvanced Airway Management: Leaugeay Webre, BS, CCEMT-P, Nremt-Pbasic100% (4)
- Agenda Bls-AclsDocument2 pagesAgenda Bls-AclsespegehNo ratings yet
- Origin & Conduction of Cardiac Impulse: Dr.S.Brinda MD Associate Professor PhysiologyDocument36 pagesOrigin & Conduction of Cardiac Impulse: Dr.S.Brinda MD Associate Professor PhysiologyAtchaya ThillainatarajanNo ratings yet
- Failed Spinal Anesthesia PDFDocument2 pagesFailed Spinal Anesthesia PDFShamim100% (1)
- Conscious Sedation: Prof - Med. Nabil H. Mohyeddin Intensive Care &anesthesiologyDocument84 pagesConscious Sedation: Prof - Med. Nabil H. Mohyeddin Intensive Care &anesthesiologyKhaled GharaibehNo ratings yet
- General Surgery: Post-Operative Care and ManagementDocument9 pagesGeneral Surgery: Post-Operative Care and ManagementMohammed Yousif AbdualjabbarNo ratings yet
- SaO2 Versus SpO2Document9 pagesSaO2 Versus SpO2jidongjc100% (1)
- Useful Formulas in Fluid TherapyDocument2 pagesUseful Formulas in Fluid TherapyPrabhakar KumarNo ratings yet
- Perioperative Fluid TherapyDocument36 pagesPerioperative Fluid TherapyUmhy GumianaNo ratings yet
- Lung SurgeriesDocument43 pagesLung SurgeriesSereinNo ratings yet
- Management of Bronchopleural Fistula: DR Grace SM Lam ICU Friday Lecture 16 January, 2009Document40 pagesManagement of Bronchopleural Fistula: DR Grace SM Lam ICU Friday Lecture 16 January, 2009Dicky SampelimbongNo ratings yet
- Bronchial Hygiene Therapy Lecture CHP 40Document18 pagesBronchial Hygiene Therapy Lecture CHP 40Ion FloreaNo ratings yet
- Thoracic Trauma: Kenyatta University LectureDocument25 pagesThoracic Trauma: Kenyatta University LectureIrene Zae MwandotoNo ratings yet
- Role of Anesthesia Nurse in Operation TheatreDocument37 pagesRole of Anesthesia Nurse in Operation TheatreZainul SaifiNo ratings yet
- Gullian Barre SyndromeDocument26 pagesGullian Barre SyndromeArslan AslamNo ratings yet
- Perioperative Fluid Management in Pediatrics: By: Karim Kamal, MDDocument33 pagesPerioperative Fluid Management in Pediatrics: By: Karim Kamal, MDMohammed AKNo ratings yet
- Lung Metabolism: Proteolysis and Antioproteolysis Biochemical Pharmacology Handling of Bioactive SubstancesFrom EverandLung Metabolism: Proteolysis and Antioproteolysis Biochemical Pharmacology Handling of Bioactive SubstancesAlain JunodNo ratings yet
- Community-Acquired Pneumonia: Strategies for ManagementFrom EverandCommunity-Acquired Pneumonia: Strategies for ManagementAntoni TorresRating: 4.5 out of 5 stars4.5/5 (2)
- A Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Endotracheal IntubationDocument1 pageEndotracheal IntubationAnusha VergheseNo ratings yet
- INDIVIDUAL CASE ANALYSIS ScribdDocument2 pagesINDIVIDUAL CASE ANALYSIS ScribdAnusha VergheseNo ratings yet
- Allergic Reactions: What To Look ForDocument2 pagesAllergic Reactions: What To Look ForAnusha VergheseNo ratings yet
- S.N o Criteria Yes No Remarks: Checklist For Intra-Hospital Transport of PatientDocument2 pagesS.N o Criteria Yes No Remarks: Checklist For Intra-Hospital Transport of PatientAnusha VergheseNo ratings yet
- CholeraDocument9 pagesCholeraAnusha VergheseNo ratings yet
- Inducing Hypothermia in Post Cardiac Arrest PatientsDocument2 pagesInducing Hypothermia in Post Cardiac Arrest PatientsAnusha VergheseNo ratings yet
- TB DiseaseDocument3 pagesTB DiseaseAnusha VergheseNo ratings yet
- Updates On Organ DonationDocument61 pagesUpdates On Organ DonationAnusha VergheseNo ratings yet
- Infection and Its Mode of TransmissionDocument33 pagesInfection and Its Mode of TransmissionAnusha Verghese100% (1)
- Leukemias Nursing ManagementDocument20 pagesLeukemias Nursing ManagementAnusha Verghese100% (5)
- Updates On Organ DonationDocument61 pagesUpdates On Organ DonationAnusha VergheseNo ratings yet
- What Is Hodgkin's Disease?: Lymphoma CancerDocument4 pagesWhat Is Hodgkin's Disease?: Lymphoma CancerAnusha VergheseNo ratings yet
- Blood Transfusion 2Document11 pagesBlood Transfusion 2Anusha VergheseNo ratings yet
- Effect of Media Violence On ChildrenDocument13 pagesEffect of Media Violence On ChildrenAnusha Verghese100% (1)
- Checklist For Emergency Incharge:: SN O Emergency Incharge Duties Done Not DoneDocument2 pagesChecklist For Emergency Incharge:: SN O Emergency Incharge Duties Done Not DoneAnusha VergheseNo ratings yet
- Ecg BSTDocument204 pagesEcg BSTAnusha Verghese100% (1)
- Argumentative Paragraph About Cars.: Click HereDocument6 pagesArgumentative Paragraph About Cars.: Click HereAnusha VergheseNo ratings yet
- Thermal (TE-411,412,413,414,511)Document25 pagesThermal (TE-411,412,413,414,511)nved01No ratings yet
- Presente Progresive TenseDocument21 pagesPresente Progresive TenseAriana ChanganaquiNo ratings yet
- Software Construction - MetaphorsDocument17 pagesSoftware Construction - MetaphorsMahmoodAbdul-Rahman0% (1)
- Disciplines, Intersections and The Future of Communication Research. Journal of Communication 58 603-614iplineDocument12 pagesDisciplines, Intersections and The Future of Communication Research. Journal of Communication 58 603-614iplineErez CohenNo ratings yet
- Customer AnalysisDocument6 pagesCustomer AnalysisLina LambotNo ratings yet
- Does Moore Succeed in Refuting IdealismDocument5 pagesDoes Moore Succeed in Refuting IdealismharryNo ratings yet
- IOSH Managing Safely Leaflet For Training ProvidersDocument6 pagesIOSH Managing Safely Leaflet For Training ProvidersShakil Ahmad AligNo ratings yet
- Cyrano de BergeracDocument209 pagesCyrano de BergeracKayleeNo ratings yet
- Personal Development: Quarter 2 - Module 2: Identifying Ways To Become Responsible in A RelationshipDocument21 pagesPersonal Development: Quarter 2 - Module 2: Identifying Ways To Become Responsible in A RelationshipTabada Nicky100% (2)
- Long Range Plans ReligionDocument3 pagesLong Range Plans Religionapi-266403303No ratings yet
- They Cried MonsterDocument13 pagesThey Cried MonstermassuroNo ratings yet
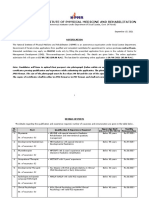
- NIPMR Notification v3Document3 pagesNIPMR Notification v3maneeshaNo ratings yet
- Autobiography of A 2nd Generation Filipino-AmericanDocument4 pagesAutobiography of A 2nd Generation Filipino-AmericanAio Min100% (1)
- CardiologyDocument83 pagesCardiologyAshutosh SinghNo ratings yet
- Project Report On Amazon vs. FlipkartDocument86 pagesProject Report On Amazon vs. FlipkartDimple100% (3)
- 3658 - Implement Load BalancingDocument6 pages3658 - Implement Load BalancingDavid Hung NguyenNo ratings yet
- Landow - The Rhetoric of HypermediaDocument26 pagesLandow - The Rhetoric of HypermediaMario RossiNo ratings yet
- Vocabulary Ladders - Grade 3 - Degree of FamiliarityDocument6 pagesVocabulary Ladders - Grade 3 - Degree of FamiliarityfairfurNo ratings yet
- The First Step Analysis: 1 Some Important DefinitionsDocument4 pagesThe First Step Analysis: 1 Some Important DefinitionsAdriana Neumann de OliveiraNo ratings yet
- Biology Chapter 23.1Document2 pagesBiology Chapter 23.1Carlos Enrique Altamar BorjaNo ratings yet
- National ScientistDocument2 pagesNational ScientistHu T. BunuanNo ratings yet
- Exam3 Buscom T F MC Problems FinalDocument23 pagesExam3 Buscom T F MC Problems FinalErico PaderesNo ratings yet
- Case Study On TQMDocument20 pagesCase Study On TQMshinyshani850% (1)
- Chiraghe Roshan Wa Amali Taweel - Nasir Khusrau PDFDocument59 pagesChiraghe Roshan Wa Amali Taweel - Nasir Khusrau PDFJuzer Songerwala100% (1)
- Microsoft Official Course: Installing and Configuring Windows Server 2012Document18 pagesMicrosoft Official Course: Installing and Configuring Windows Server 2012jttodorovNo ratings yet
- 160 LW Bending Tester v2.0Document4 pages160 LW Bending Tester v2.0Sá StrapassonNo ratings yet
- National Formulary of Unani Medicine Part Ia-O PDFDocument336 pagesNational Formulary of Unani Medicine Part Ia-O PDFMuhammad Sharif Janjua0% (1)
- A Portrayal of Gender and A Description of Gender Roles in SelectDocument429 pagesA Portrayal of Gender and A Description of Gender Roles in SelectPtah El100% (1)
- Fabre, Intro To Unfinished Quest of Richard WrightDocument9 pagesFabre, Intro To Unfinished Quest of Richard Wrightfive4booksNo ratings yet