Professional Documents
Culture Documents
Fluidslecture
Uploaded by
Igor Stefanet0 ratings0% found this document useful (0 votes)
49 views26 pagesOriginal Title
Fluidslecture.ppt
Copyright
© © All Rights Reserved
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
49 views26 pagesFluidslecture
Uploaded by
Igor StefanetCopyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
You are on page 1of 26
Volume, Electrolyte, and
Blood Product Replacement
W. Clay Jackson, MD, DipTh
Assistant Professor, UT Dept. of Family Medicine
Indications for Intravenous Tx
Volume replacement
Biochemical correction
Retention of RBCs
Provision of nutrition
Filtering of noxious products
Signs of Dehydration
Poor skin turgor
Tachycardia
Poor capillary refill (>3 sec)
Dry mucous membranes
Sunken eyes
Sunken fontanelles
No tears
Rehydration Solutions
Crystalloids
Distribute across ECF
Colloids
Remain intravascular
Rehydration Solutions
Crystalloids
Normal saline (NS)
Lactated Ringers (LR)
Normosol
Plasma-Lyte
NS vs. LR
154 meq Na, Cl
Often has 20 meq
KCl/L added
NEVER bolus fluid
with KCl added
pH 5.7; 308 mOsm/L
$7 / L
130 meq Na
109 meq Cl
4 meq K
3 meq Ca
28 meq lactate
pH 6.4; 273 mOsm/L
$22 / L
Cant use with blood
Normal Saline Lactated Ringers
n.b. Plasma-Lyte and Normosol approximate plasma more closely.
Rehydration Solutions
Colloids (Greek: glue)
Dextrans (anaphylaxis, bleeding)
10% Dex-40
6% Dex-70
Starch
6% Heta- (T
1/2
17 d, but oncotic 24 h)
10% Penta-
Albumin (expensive)
5%
25% (not for volume rescusc; ICF)
Rehydration
BOLUS
1-2 L (NS or LR)
MAINTENANCE
75-125 cc/hr
REPLENISH
20 meq KCl/L
BOLUS
20 cc/kg (NS or LR)
MAINTENANCE (with ?-NS)
4 cc/kg/hr (1
st
10 kg)
2 cc/kg/hr (2
nd
10 kg)
1 cc/kg/hr (additional kg)
REPLENISH
20 meq KCl/L
Adults Children
Na requirement: 3 meq/kg/d
K requirement: 2 meq/kg/d
A good heart and kidneys can
surmount all but the most
willfully incompetent of
fluid regimens.
The Whole Internists Catalog
What about D
5
W?
Poor volume expander (50 cc intravascular/L)
Poor supply of calories (170 kcal/L)
Hypertonic (278 mOsm just from dextrose)
Increased CO
2
, lactate production
NOT recommended for ill patients
EXCEPT patients with DKA
on insulin drips
Electrolyte Replacement
MS changes, szs
Must determine type
Hypovolemic
Euvolemic
Hypervolemic
Pseudo?
(+1.6 meq/L for each
100 glc above 100
mg/dL)
Treatment varies (<125)
Slow replacement (CPM)
1 meq/hr; <10 meq/24hr
Tx of underlying cause
Fluid restriction
Sodium
136-145
Electrolyte Replacement
Muscle weakness, cardiac
toxicity <3.0
Vast majority is
intracellular
Insulin pushes K into cells
Correction of acidosis
pushes K into cells
KCl or KP0
4
po (bitter)
KCl IV 10 meq/h (X 4h)
Potassium
3.5-5.1
Electrolyte Replacement
Tetany
(Chvosteks sign--cheek)
(Trousseaus sign--tourniquet)
Correction factor
(1.0 albumin : 0.8 Ca)
OsCal (CaCO
3
) po
1 amp 10% soln
(1000 mg/10 cc)
CaCl
2
Ca gluconate
Calcium
8.8-10.5
Electrolyte Replacement
Muscle weakness
Neutra-Phos or K-Phos po
Severe (<1.0 mg/dL):
0.08-0.16 mmol/kg IV
(over 6 hr)
Phosphate
2.5-4.9
Electrolyte Replacement
N/V, tetany
2-6 gm bolus
1-2 gm/hr (for 2-4 hrs)
Acidosis renders heart
arrhythmias refractory
to tx
Some advocate
amps of HCO
3
44 meq IV
Magnesium
1.8-2.4
HCO
3
21-32
William Harvey 1578-1657
University of Cambridge; University of Padua
Personal physician to Charles I
1628: Anatomical Exercises on the Motion
of the Heart and Blood in Animals
1651: Essays on the Generation of Mammals
Blood Products
Whole blood
Packed RBCs
Fresh frozen plasma (FFP)
Cryoprecipitate
Platelets
Blood is Blood, right?
Whole blood
Volume expander
35 d shelf life d
Washed RBCs
Pts with allergic
reactions to plasma
proteins
Packed RBCs
Saves volume (250 cc)
42 d shelf life
Leuko-poor RBCs
Pts with febrile, non-
hemolytic reactions to
plasma WBCs
The Compatibility Game
ABO compatibility
Recipient can only
receive ABO proteins
he/she has previously
seen
O can donate to any
recipient
O recipients can only
receive O blood
Rh compatibility
Rh- recipient
should receive Rh-
blood
Rh+ recipient can
receive Rh+ or Rh-
blood
Blood Loss:
How much is too much?
5% body wt. in
intravascular space
10% blood loss =
hypovolemic shock
1 unit blood = 500cc
(raises HCT 2-3%)
80 cc/kg in intravascular
space
20% blood loss =
hypovolemic shock
Transfuse 10 cc/kg
Adults Neonates
To transfuse or not to transfuse
HCT <30
Acute onset
Pt symptomatic
Presyncopal
Hypotensive
Tachycardic
Tachypneic
Other stressors imminent
Platelets
Danger zone: <50 K plts
Frank bleeding: <10 K plts
Each unit of plts count by 10 K
6-8 units usually transfused
Clotting Factors
Fresh frozen plasma (FFP)
All clotting factors; no
platelets
Can supplement RBCs
when whole blood not
available for exchange
transfusion
Cryoprecipitate
Initially a tx for VW
Dz, Hemophilia
Now a source of
fibrinogen in
cardiothoracic surgery,
obstetric emergencies
Doctor, Doctor!
Weve lost our IV!
Subclavian*
Internal Jugular (IJ)*
Femoral*
Umbilical Artery (UAC)
Umbilical Vein (UVC)
Intraosseus (IO)
All patients Peds only
* Utilize Seldinger technique; see handout
Femoral Line
Sir William Osler
www.utmem.edu/fpsa/
You might also like
- Fast Facts: Pyruvatkinase-Mangel für Patienten und Angehörige: Eine seltene genetische Erkrankung der roten Blutkörperchen Informationen + Mitreden-Können = Bestmöglicher VerlaufFrom EverandFast Facts: Pyruvatkinase-Mangel für Patienten und Angehörige: Eine seltene genetische Erkrankung der roten Blutkörperchen Informationen + Mitreden-Können = Bestmöglicher VerlaufNo ratings yet
- Fast Facts: Deficiencia de piruvato quinasa para pacientes y familiares: Una enfermedad genética rara que afecta a los glóbulos rojos Información + Asumir el control = El mejor resultadoFrom EverandFast Facts: Deficiencia de piruvato quinasa para pacientes y familiares: Una enfermedad genética rara que afecta a los glóbulos rojos Información + Asumir el control = El mejor resultadoNo ratings yet
- Fluid Management and Shock ResuscitationDocument35 pagesFluid Management and Shock ResuscitationAsrarudin HamidNo ratings yet
- Fluid Student 2012Document43 pagesFluid Student 2012Sara Ilyas KhanNo ratings yet
- Fluids&Lytes PediatricDocument33 pagesFluids&Lytes Pediatricnugraha_esaNo ratings yet
- Fluid ManagementDocument10 pagesFluid ManagementdradaadNo ratings yet
- Fluids and Electrolytes in Pediatrics FinalDocument41 pagesFluids and Electrolytes in Pediatrics FinalArun GeorgeNo ratings yet
- Fluidsrenalacid BasebloodDocument8 pagesFluidsrenalacid BasebloodmyscribeNo ratings yet
- Fluid Management and Shock ResuscitationDocument32 pagesFluid Management and Shock ResuscitationKhoirul Tn Antik0% (1)
- Fluid and Electrolytes 1.Document26 pagesFluid and Electrolytes 1.Ethan LimNo ratings yet
- Urgentno Zbrinjavanje Dehidracije Kod Dece EngDocument43 pagesUrgentno Zbrinjavanje Dehidracije Kod Dece EngMirko BelanNo ratings yet
- Management of DKA PresentationDocument46 pagesManagement of DKA PresentationMuhammed YesufNo ratings yet
- Parenteral Fluid TherapyDocument5 pagesParenteral Fluid TherapyAbdalrahman KhalilNo ratings yet
- Fluid and Electrolytes: Robert Mcintyre, Jr. Associate Professor of Surgery University of Colorado Health Sciences CenterDocument54 pagesFluid and Electrolytes: Robert Mcintyre, Jr. Associate Professor of Surgery University of Colorado Health Sciences CenterWilliam Yap WLNo ratings yet
- Kenzu B, (MD, Asst - Professor of Surgery)Document40 pagesKenzu B, (MD, Asst - Professor of Surgery)kenzu bedruNo ratings yet
- Body Fluids and ElectrolytesDocument42 pagesBody Fluids and ElectrolytesQusaiBadr100% (1)
- Balance Cairan Final.Document41 pagesBalance Cairan Final.Niqko Bayu PrakarsaNo ratings yet
- Diarrhea and DehydrationDocument12 pagesDiarrhea and DehydrationnikprovNo ratings yet
- Fluid and Electrolyte TherapyDocument23 pagesFluid and Electrolyte TherapyJamal ArizonaNo ratings yet
- Rhabdomyolysis Case Study WeeblyDocument18 pagesRhabdomyolysis Case Study Weeblyapi-241865788No ratings yet
- Sagraves MSfluids Lytes 2004Document59 pagesSagraves MSfluids Lytes 2004Burhan Ul HaqNo ratings yet
- Fluid Management & Shock Resuscitation KGD SMT 7 PDFDocument34 pagesFluid Management & Shock Resuscitation KGD SMT 7 PDFTikuqNyukUnyukUnyuk100% (1)
- Fluid & Electrolite Management in Surgical WardsDocument97 pagesFluid & Electrolite Management in Surgical WardsBishwanath PrasadNo ratings yet
- PPC15 FEN SlidesDocument88 pagesPPC15 FEN SlidesbrianzflNo ratings yet
- Fluid and Blood TherapyDocument84 pagesFluid and Blood Therapyjean uwakijijweNo ratings yet
- Fluid Management: Suparto Anesthesia Department Medical Faculty Christian Krida Wacana UniversityDocument61 pagesFluid Management: Suparto Anesthesia Department Medical Faculty Christian Krida Wacana UniversitygozaNo ratings yet
- Fetus Term Infant Premature Infants 1 Year of Life Puberty: 1.) Intracellular Fluid (Icf)Document49 pagesFetus Term Infant Premature Infants 1 Year of Life Puberty: 1.) Intracellular Fluid (Icf)binsky2009No ratings yet
- Fluid & Electrolytes SaurabhDocument88 pagesFluid & Electrolytes Saurabhunknownsince1986No ratings yet
- Fluid Therapy Final 2019 DR TaanoDocument39 pagesFluid Therapy Final 2019 DR TaanoCabdi WaliNo ratings yet
- HONK by AijazDocument40 pagesHONK by AijazMuhammad Imran AlamNo ratings yet
- DehydrationDocument14 pagesDehydrationReimer LaquihuanacoNo ratings yet
- Fluid & Electrolytes Balance NewDocument21 pagesFluid & Electrolytes Balance NewPamela Ria Aguinaldo HensonNo ratings yet
- Hyper Nat Re MiaDocument27 pagesHyper Nat Re MiaPankaj Kumar SinghNo ratings yet
- Hypovolemic ShockDocument27 pagesHypovolemic Shock'govamaniacs' Insave IVNo ratings yet
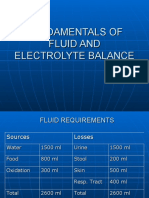
- Fundamentals of Fluid and Electrolyte BalanceDocument46 pagesFundamentals of Fluid and Electrolyte BalanceMelia Eka Rosita PharmacistNo ratings yet
- Intravenous Fluids: Composition & UsesDocument41 pagesIntravenous Fluids: Composition & UsesFathima BanuzNo ratings yet
- DkaDocument38 pagesDkaHam SotheaNo ratings yet
- Diabetic Ketoacidosis2Document2 pagesDiabetic Ketoacidosis2Venkat RamanNo ratings yet
- Internal Medicine TNDocument3 pagesInternal Medicine TNZeeshan Ahmed100% (2)
- Fluid - Electrolyte Imbalance 2012-InedDocument45 pagesFluid - Electrolyte Imbalance 2012-InedmiamuhpianNo ratings yet
- Disorders of Potassium Homeostasis: Informal Academic in ServiceDocument37 pagesDisorders of Potassium Homeostasis: Informal Academic in ServiceaqilasafikaNo ratings yet
- Pediatric NotesDocument45 pagesPediatric NoteskkkssbbNo ratings yet
- S.gaus-Management of Life-Threatening (Kuliah Sistem)Document54 pagesS.gaus-Management of Life-Threatening (Kuliah Sistem)Rusmin UsmanNo ratings yet
- Perioperative Fluid Therapy: Department of Anesthesiology &ICU KKUH. King Saud UniversityDocument47 pagesPerioperative Fluid Therapy: Department of Anesthesiology &ICU KKUH. King Saud Universityarifjo7999No ratings yet
- HyperkalemiaDocument30 pagesHyperkalemiaAyanna100% (3)
- Fluid Therapy and ElectroliteDocument36 pagesFluid Therapy and ElectroliteAriefBudimanHidayatNo ratings yet
- Fluid Resuscitation - Dita AditianingsihDocument48 pagesFluid Resuscitation - Dita AditianingsihGalih Wicaksono100% (1)
- Fluid & Electrolyte Balance: PresentedDocument30 pagesFluid & Electrolyte Balance: PresentedFathimathNo ratings yet
- Intravenous Fluid Therapy: Michael OrnesDocument27 pagesIntravenous Fluid Therapy: Michael OrnesOkto Mara Fandi HarahapNo ratings yet
- Fluid & Electrolyte TherapyDocument38 pagesFluid & Electrolyte Therapyharjuna100% (1)
- Kelly Shinkaruk, MD FRCPC HLT 123 October 17, 2009Document88 pagesKelly Shinkaruk, MD FRCPC HLT 123 October 17, 2009Hutagaol ImeldaNo ratings yet
- 120 Med Labs HyperkalaemiaDocument4 pages120 Med Labs HyperkalaemiaqurbanNo ratings yet
- Fluids & Electrolytes Acid/Bas Balance: DR Wael SadaqahDocument72 pagesFluids & Electrolytes Acid/Bas Balance: DR Wael Sadaqahdr wael sadaqaNo ratings yet
- Surgery 1.1 Fluid and Electrolyte Balance - Azares PDFDocument7 pagesSurgery 1.1 Fluid and Electrolyte Balance - Azares PDFAceking MarquezNo ratings yet
- Roumilla Mendoza, M.D. Roumilla Mendoza, M.D. Pediatric Gastroenterologist Pediatric GastroenterologistDocument59 pagesRoumilla Mendoza, M.D. Roumilla Mendoza, M.D. Pediatric Gastroenterologist Pediatric GastroenterologistYenyen DelgadoNo ratings yet
- Somchodok Chakreeyarat, MD. Endocrine Unit, Department of Medicine Bhumibol Adulyadej HospitalDocument53 pagesSomchodok Chakreeyarat, MD. Endocrine Unit, Department of Medicine Bhumibol Adulyadej HospitalLing TaerahkunNo ratings yet
- Terapi Cairan Dan Transfusi: Dr. Imam Ghozali., Span.,MkesDocument47 pagesTerapi Cairan Dan Transfusi: Dr. Imam Ghozali., Span.,MkesHelend ChildDjNo ratings yet
- UMBC CC-EMTP Class Notes, FLCC Class 2010Document93 pagesUMBC CC-EMTP Class Notes, FLCC Class 2010Marc LaBarberaNo ratings yet
- Potassium Final2Document18 pagesPotassium Final2Kholoud KholoudNo ratings yet
- Acid-Base and Electrolyte Handbook for Veterinary TechniciansFrom EverandAcid-Base and Electrolyte Handbook for Veterinary TechniciansAngela Randels-ThorpNo ratings yet
- ShockDocument21 pagesShockIgor StefanetNo ratings yet
- ShockDocument36 pagesShockMin-Joo Esther ParkNo ratings yet
- Shock and HypoperfusionDocument46 pagesShock and HypoperfusionIgor StefanetNo ratings yet
- ShockDocument28 pagesShockIgor StefanetNo ratings yet
- Shock I and IIDocument105 pagesShock I and IIIgor StefanetNo ratings yet
- Shock 4813Document18 pagesShock 4813docprashNo ratings yet
- Shock: Differential Diagnosis and Hemodynamic MonitoringDocument21 pagesShock: Differential Diagnosis and Hemodynamic MonitoringtataranyNo ratings yet
- Septic ShockDocument50 pagesSeptic ShockIgor StefanetNo ratings yet
- Lesson 5Document14 pagesLesson 5Igor StefanetNo ratings yet
- EMS Shock LexDocument60 pagesEMS Shock LexIgor StefanetNo ratings yet
- Ramphal SepsisDocument29 pagesRamphal SepsisIgor StefanetNo ratings yet
- Pharmacotherapy of ShockDocument23 pagesPharmacotherapy of ShockIgor Stefanet100% (2)
- Cardiogenic Shock - FINALDocument79 pagesCardiogenic Shock - FINALIgor StefanetNo ratings yet
- Cardiogenic ShockDocument27 pagesCardiogenic ShockIgor StefanetNo ratings yet
- 2008 Corrective Hair Transplant ArticleDocument9 pages2008 Corrective Hair Transplant ArticleIgor StefanetNo ratings yet
- Blood TherapyDocument21 pagesBlood TherapySandra Ag Ariodere KeonyediNo ratings yet
- Treatment of Venous Thrombosis and Pulmonary EmbolismDocument53 pagesTreatment of Venous Thrombosis and Pulmonary EmbolismIgor StefanetNo ratings yet
- Transplant Balding ScalpDocument8 pagesTransplant Balding ScalpIgor StefanetNo ratings yet
- 5 Big Tournament LeaksDocument17 pages5 Big Tournament LeaksIgor StefanetNo ratings yet
- Toshiba Conditioner PDFDocument73 pagesToshiba Conditioner PDFIgor StefanetNo ratings yet
- GERIAT1Document8 pagesGERIAT1Igor StefanetNo ratings yet
- 10 More Essential HoldDocument51 pages10 More Essential HoldIgor StefanetNo ratings yet
- BinionDocument75 pagesBinionIgor StefanetNo ratings yet
- Digestion Enzyme Practice TestDocument15 pagesDigestion Enzyme Practice TestJila HafiziNo ratings yet
- Anterior Cross Bites in Primary Mixed Dentition PedoDocument32 pagesAnterior Cross Bites in Primary Mixed Dentition PedoFourthMolar.comNo ratings yet
- 21 Prof Suwadi DEVIASI SEXDocument46 pages21 Prof Suwadi DEVIASI SEXdr.cintaNo ratings yet
- SIL (2011) List of Semantic DomainsDocument19 pagesSIL (2011) List of Semantic DomainsTakashi NakagawaNo ratings yet
- Atlas of Poultry Disease 2Document41 pagesAtlas of Poultry Disease 2DDurasNo ratings yet
- TugasDocument4 pagesTugasYuli Wardani OrNo ratings yet
- Editorial For December 2010 - Rare RemediesDocument4 pagesEditorial For December 2010 - Rare Remediespanniyin selvanNo ratings yet
- Pentavet Homeopathic Veterinary Medicine For AnorexiaDocument16 pagesPentavet Homeopathic Veterinary Medicine For AnorexiaLonely WolfNo ratings yet
- 7 Habits Checklist1 1 PDFDocument3 pages7 Habits Checklist1 1 PDFilsarduNo ratings yet
- Fish Poisoning (Print)Document65 pagesFish Poisoning (Print)Cristina SarinoNo ratings yet
- DLLDocument7 pagesDLLmichelle abianNo ratings yet
- Subcutaneous MycosesDocument22 pagesSubcutaneous MycosesIan MosesNo ratings yet
- Basic Cardiac Life Support 2011Document6 pagesBasic Cardiac Life Support 2011Tashfeen Bin NazeerNo ratings yet
- J 1365-2869 2012 01044 XDocument371 pagesJ 1365-2869 2012 01044 XMarco Bakker100% (1)
- Chapter 2 Body CoordinationDocument15 pagesChapter 2 Body CoordinationYatt YatiNo ratings yet
- Honk ScriptDocument48 pagesHonk ScriptTom Corcoran100% (4)
- Malaria Control BrochureDocument2 pagesMalaria Control BrochureEkwoh Okwuchukwu ENo ratings yet
- Being Afraid: Everyday WorriesDocument10 pagesBeing Afraid: Everyday Worriesdina171279No ratings yet
- 2 Medrega Cristian Gabriel enDocument1 page2 Medrega Cristian Gabriel enCristian GabrielNo ratings yet
- Anatomi Dan Fisiologi GinjalDocument32 pagesAnatomi Dan Fisiologi GinjalAlamul Huda100% (1)
- Vitamin B ComplexDocument3 pagesVitamin B Complexjoseph_delacruz20No ratings yet
- Middle Cerebral Artery DopplerDocument4 pagesMiddle Cerebral Artery DopplerHervi LaksariNo ratings yet
- PPK ParuDocument64 pagesPPK Parusri wahyuniNo ratings yet
- Health AssessmentDocument39 pagesHealth AssessmentAnnalisa TellesNo ratings yet
- Aquarium Pharmaceuticals AmmoniaDocument1 pageAquarium Pharmaceuticals AmmoniaKayyyNo ratings yet
- Sjavs 24a270 281Document12 pagesSjavs 24a270 281Ramesh BeniwalNo ratings yet
- Indian Meat Industry: Opportunities and Challenges: January 2011Document7 pagesIndian Meat Industry: Opportunities and Challenges: January 2011satyajitNo ratings yet
- TURP SyndromeDocument13 pagesTURP SyndromeWindy Ari WijayaNo ratings yet
- Topic Test: Oxfordaqa International Gcse Biology 9201Document26 pagesTopic Test: Oxfordaqa International Gcse Biology 9201Novanolo Christovori ZebuaNo ratings yet
- Horner SYndromeDocument3 pagesHorner SYndromeHendri Wijaya WangNo ratings yet