Professional Documents
Culture Documents
Jurnal Reading Hepatitis B
Uploaded by
Anonymous 6Ml6e2GmCo0 ratings0% found this document useful (0 votes)
39 views15 pagespresent and future therapies from hepatitis B.
Original Title
Jurnal Reading hepatitis B
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentpresent and future therapies from hepatitis B.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
39 views15 pagesJurnal Reading Hepatitis B
Uploaded by
Anonymous 6Ml6e2GmCopresent and future therapies from hepatitis B.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 15
Jurnal Reading
Present and Future Therapies of
Hepatitis B: From
Discovery to Cure
Preseptor: dr Ihsanil Husna, Sp.PD
Background
Hepatitis B virus (HBV) is a significant global
pathogen, infecting more than 240 million
people worldwide.
Moreover, the actual number of persons who
are chronically infected is estimated to have
increased slightly from 223 million to 240
million during this same period.
Natural history of chronic hepatitis B
The course of chronic HBV infection has been
grouped into four phases:
The immune tolerant phase
The immune active/hepatitis B e antigen
(HBeAg)positive chronic hepatitis phase,
The HBeAg-negative inactive phase
The immune active/HBeAg-negative chronic
hepatitis phase.
HBV Replication
Current therapies of hepatitis B and
mechanism of action
There are currently two classes of drugs
approved for the treatment of hepatitis B:
nucleos(t)ide reverse transcriptase inhibitors
(NRTIs) and interferon-a (IFN-a).
The first-line antiviral HBV medications include
a nucleoside analogue, entecavir; a nucleotide
analogue, tenofovir; and pegylated IFN-a
(PEG-IFN-a), used as monotherapy.
The second generation NRTIs such as
entecavir and tenofovir can potently suppress
the DNA synthesis step of HBV replication,
they have a little effect on the level and
activity of cccDNA, which has a long half life
and can persist for decades in the infected
liver despite successful antiviral treatment.
Entecavir and tenofovir can decrease the level
of HBV DNA by 6 logs within 1 year of
treatment and have low rates of antiviral drug
resistance.
For patients who do not have cirrhosis or do
not require immunosuppresive therapy,
profesional society guidelinesrecommend
treating those in the immune active phase.
Combination Studies of Current Therapies
Combinaton of PEG-IFN with an NRTI would be
more likely to result in synergy because the
drugs have different mechanism of action, the
concept being that inhibition of viral
replication with an NRTI may augment the
immune effect of PEG-IFN.
Patients receiving PEG-IFN and tenofovir had a
higher rate of HBsAg loss than those receiving
either drug along. They represent a small
increase (6%) in HBsAg loss over PEG-IFN
monotherapy.
HBV Entry Inhibitors
In particulr, small molecules and antibody
based treatments are quite effective in
treating acute viral infections.
Myrcludex B, cyclosporin A and other
substrate analogues inhibit bile salt transport
by NTCP.
Preliminary results suggested that Myrcludex
B is safe and well tolerated in HBsAg positive
patients with or without HDV coinfection.
HBV Capsid Inhibitors
They function to dysregulate or selectively
inhibit either pregenomic RNA encapsidation
or nucleocapsid assembly or both. The first of
these were the phenylpropenamide
derivatives AT-61 and AT-130.
The second group is the
heteroaryldihydropyrimidines.
In vitro studies have demonstrated strong
synergy when these inhibitors are used in
combination with currently approved NRTIs.
HBV Nonspesific Immunomodulatory
Agents
TLR Agonists
PDI and othe Coinhibitory Blockers
Therapeutic Vaccines
Induce sufficient anti HBV immune responses
to eliminate and/or cure infected heaptocytes
without undue host cell damage, prevent viral
spread to new heaptocytes and promote long
term viral control.
HBsAg based Vaccine
Cytotoxic T-Lymphocyte Epitope Vaccine
DNA Vaccination with or without
Immunomodulators
Other Therapeutic Vaccine Trials
Therapeutic pipeline and Conclusion
To achieve a more sustained and effective
control of HBV Infection , a combination of the
existing HBV therapies and one or more of the
above modalities, either small molecules
drugs or biologics will be necessary.
With growing interest in developing and
efforts to develop more effectie therapies for
HBV the challenging goal of a cure may be
well within reach in the near future.
You might also like
- JurnalDocument11 pagesJurnalAnonymous 6Ml6e2GmCoNo ratings yet
- Anes 10Document8 pagesAnes 10Fuchsia ZeinNo ratings yet
- Nejmoa1304369 PDFDocument13 pagesNejmoa1304369 PDFAnonymous 6Ml6e2GmCoNo ratings yet
- Tugas Radiologi Part 3Document10 pagesTugas Radiologi Part 3rachma30No ratings yet
- ICD10Volume2 en 2010Document201 pagesICD10Volume2 en 2010Ai NurfaiziyahNo ratings yet
- JNC 8 Guideline Algorithm for Treating HypertensionDocument2 pagesJNC 8 Guideline Algorithm for Treating HypertensionTaradifaNurInsi0% (1)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Client Centered TherapyDocument3 pagesClient Centered TherapyDavender VashistNo ratings yet
- NHS Tayside Flowchart For Systemic HRT Prescribing: AbbreviationsDocument2 pagesNHS Tayside Flowchart For Systemic HRT Prescribing: AbbreviationspiNo ratings yet
- 0907 MigraineheadachesDocument2 pages0907 Migraineheadachesrena_psNo ratings yet
- Pengadaan Maret 2023Document2 pagesPengadaan Maret 2023Endah Masmulia NNo ratings yet
- WS 4 - Risani Andalasia Putri, M.Farm., Apt - PAIN MANAGEMENTDocument66 pagesWS 4 - Risani Andalasia Putri, M.Farm., Apt - PAIN MANAGEMENTMuhammad HabibieNo ratings yet
- Daftar Harga FAHRENHEIT - 2019 2Document18 pagesDaftar Harga FAHRENHEIT - 2019 2Stephen SatigiNo ratings yet
- HeadacheDocument2 pagesHeadacheBeck TumangNo ratings yet
- Atls Indonesia: Download NowDocument4 pagesAtls Indonesia: Download NowGyidian UpaNo ratings yet
- Complete Products ListDocument20 pagesComplete Products ListHina Tina100% (1)
- Wisconsin Amphetamine Rule PDFDocument2 pagesWisconsin Amphetamine Rule PDFBrian HarrisNo ratings yet
- Art Therapy EbookDocument10 pagesArt Therapy EbookJean Dolores Mena50% (12)
- DRUG STUDY (Dextromethorphan)Document2 pagesDRUG STUDY (Dextromethorphan)Avianna CalliopeNo ratings yet
- MSD Tender Numbers Closing On 10 09 2019Document6 pagesMSD Tender Numbers Closing On 10 09 2019Sanjeev JayaratnaNo ratings yet
- ADHD Medication Conversion ChartDocument4 pagesADHD Medication Conversion ChartThaíse FontanaNo ratings yet
- Medicinal-Chemistry Mcqs 1Document5 pagesMedicinal-Chemistry Mcqs 1Abera Lemma100% (1)
- OTC and POMDocument23 pagesOTC and POMShannelle CaballeroNo ratings yet
- Module 2Document14 pagesModule 2Muskaan BindalNo ratings yet
- B. Pharm.2nd 3rd 4th 2016-17Document8 pagesB. Pharm.2nd 3rd 4th 2016-17Mukesh TiwariNo ratings yet
- 18 JL 7Document15 pages18 JL 7Irma SihotangNo ratings yet
- BiopharmaceuticsDocument21 pagesBiopharmaceuticsSilvy100% (1)
- Paracetamol A Review of Three Routes of AdministrationDocument3 pagesParacetamol A Review of Three Routes of AdministrationMohd MiqdamNo ratings yet
- 〈7〉 LABELINGDocument8 pages〈7〉 LABELINGSiska Rotua Uli SihombingNo ratings yet
- Oxaliplatin For Injection (Preservative-Free) 50 MG Per Vial and 100 MG Per Vial Package Leaflet - Taj PharmaDocument1 pageOxaliplatin For Injection (Preservative-Free) 50 MG Per Vial and 100 MG Per Vial Package Leaflet - Taj PharmaTAJ PHARMA — A Health Care ProviderNo ratings yet
- Kidney 1Document26 pagesKidney 1Zainurain Zainal AbidinNo ratings yet
- Nursing Record: Student Name: Student IDDocument5 pagesNursing Record: Student Name: Student IDHaneenNo ratings yet
- Group 1 - BREAST CANCER - Case StudyDocument29 pagesGroup 1 - BREAST CANCER - Case StudyCONTRERAS, ALIANNA IRISHNo ratings yet
- Method For IV Heparin CalculationDocument3 pagesMethod For IV Heparin CalculationDerricka CrosbyNo ratings yet
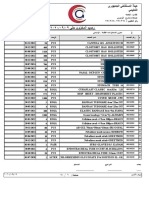
- رصيد المستهلاكات حتى - 9Document20 pagesرصيد المستهلاكات حتى - 9ahmad aliNo ratings yet
- PNDFvol1ed7 2008Document315 pagesPNDFvol1ed7 2008Wilma de LeonNo ratings yet
- X ReportDocument12 pagesX ReportILHAM 'K FOR ALLNo ratings yet