Professional Documents
Culture Documents
5.chronic Inflamation
5.chronic Inflamation
Uploaded by
Bravan Alienn0 ratings0% found this document useful (0 votes)
7 views22 pagesOriginal Title
5.chronic inflamation.ppt
Copyright
© © All Rights Reserved
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
7 views22 pages5.chronic Inflamation
5.chronic Inflamation
Uploaded by
Bravan AliennCopyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
You are on page 1of 22
CHRONIC INFLAMMATION
• Inflammation of prolonged duration (weeks or
months).
In which all the following process simultaneously;
Active inflammation.
Tissue destruction.
Attempt at repair.
• Chronic inflammation may follow Acute inflation.
• But may begin insidiously as a low – grade often
asymptomatic response.
• This latter type is the cause of tissue damage in
certain disabling common condition such as ;
Rheumatoid arthritis.
Chronic lung diseases.
Tuberculosis.
Causes of chronic inflammation
• Persistent infection – e.g. TB
• Prolonged exposure to potentially toxic agent e.g.
silica.
• Autoimmunity - immune reaction against
individual’s own tissue e.g Rhaumatoid arthritis.
Mophologic Features
• Chronic inflammation is characterized by;
infiltration of mononuclear cells includes
macrophages, lymphocytes and plasma cells.
Tissue destruction
Induced by persistent of offending agents or
by inflammatory cells.
Attempt at healing by connective tissue
replacement of damage tissue.
Accomplished by proliferation of small blood
vessels (angiogenesis) and in particular Fibrosis.
Mononuclear cell infiltration
• The dominant cellular player in chronic
inflammation is macrophage
•A component of mononuclear phagocyte system
(MPS)
• MPs consist of closely related cells of bone marrow
origin
Bone Blood Tissue
Stem cell – monoblast Monocytes – Macrohages microglia(CNS)
half life I day half life month Kupffer cells
- years Alveolar
Activated macrophage
• On reaching tissue monocytes becomes
transformed into larger phagocytic cells called
Macrophages
• Macrophages may be activated by a variety of
stimuli;
cytokines (e.g. IFN – Y).
Bacterial endotoxin.
Other chemical mediators.
• Activation results
Increase in size of cell
Increase in level of Lysosomal enzymes
Greater ability to phogocytose
• Activated Macrophages secrete a wide variety of
biologically active product.
• Some product if unchecked, results in tissue injury
and fibrosis.
• Products of activated Macrophages
Serve to eliminate injurious agent e.g. microbes.
Initiate process of repair.
Are responsible for much of tissue injury in Chronic
inflammation.
• Note some of the products are toxic to microbes
and host cells e.g;
Oxygen and Nitrogen intermediates some cause influx of
other cells (cytokines and chemotactic factors).
• Other causes fibroblast proliferation and collagen
deposition
• Other agiogenesis
Other cells of Chronic Inflammation
• Lymphocytes
• Plasma cells
• Oesinophils – immune reaction mediated by IgE
e.g Parasitic infection
• Mast cells
Although neutrophils are characteristic of acute
inflammation chronic inflammation lasting for months
continue to show large numbers of neutrophils .
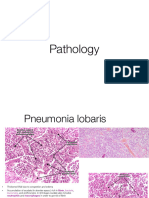
Granulomatous inflammation
• A distinct pattern of chronic inflammation
• Characterized by focal accumulation of activated macrophages
• The macrophage often develop an epitheliative pattern
(epithelioid cells)
• The aggregate of macrophages is surrounded by a collar of
mononuclear leukocytes;
Principally lymphocytes and occasionally plasma
cells.
Old granulomas develops an endosing rim of
fibroblast and connective tissue.
Frequently epithelioid cells fuse to form giant cells Fuse to
form giant cells
These giant cells are often in pheriphery but
sometimes in center of granuloma
Giant cells
Few examples exists in normal tissues.
• Osteoclast – bones.
• Trophoblast – placenta.
• Megakarycytes – Bone Marrow.
In chronic inflammation when macrophages fails
to deal with particles to be removed, they fuse
together.
• Forms giant cells.
• Giant cells have abundant cytoplasma and multiple
nuclei.
TYPES OF GIANT CELLS
Foreign body giant cells
Contains numerous nuclei (upto 100).
Nuclei size uniform.
Scattered through cytoplasm.
Seen as a result of chronic inflammation by foreign
body, also seen in infective granulomas .
Langharn’s giant cells
Seen in Tuberculosis and sarcoidosis.
Nuclei often arranged in pheriphery .
Forms horseshue pattern.
Or are clustered in two poles of cells.
Tuton giant cells
Multinucleated.
Vacuolated cytoplasm due to lipoid content.
Seen e.g. in Xanthoma.
Aschoff giant cells
Multinucleated giant cells derived from cardiac
histocytes.
Seen in rheumatic nodules.
Healing
• Healing process involves 2 distinct
processes(regeneration and repair).
Regeneration
This take place by proliferation of
parenchymal cell.
Usually results into complete restoration of
original tissue.
Repair
Take place by proliferation of connective
tissue
End result is fibrosis and scarring
NB
Both at times take place simultaneously
• Regeneration
Occurs only in when cells are able to
divide postnatally
• Repair
Its replacement of injured tissue by
fibrosis
Two process involved;
Granulation formation
Contraction of wound
Repair take place by participation of
mesenchymal cells
Fibroblasts, endothelial cells, macrophages, platelets
and parenchymal cells of injured organ
Granulation Tissue formation
Granulation tissue (‘granular and pink appearance)
• Proliferation of new small vessels
• Proliferation of fibroblast
• New vessels are covered by a thin surface of Fibroblast and
collagen hence pink colour
Contraction of wound
Achieved by myofibroblasts whose contraction
decreases size of the wound
Regeneration and repair
• Both processes are better demonstrated by
wound healing
• Healing of wound is achieved through the
following two ways ;
Healing by first intention (primary union)
Healing by second intention (secondary union)
Healing by first intention
This is defined by wound with the following
characteristics;
Clean and uninfected
Surgically incised
Minimal loss of cells and tissue
Edges approximated by surgical sutures
Sequence of events
1. Initial haemorrhage
Immediately after injury space between filled by
blood.
The blood clot covers the surface preventing
dehydration
and infection.
2. Acute inflammatory response
In 24 hours neutrophils appears from the margin
By third day replaced by macrophages.
• Epithelial changes
• Regeneration
Basal cells of epidermis of both margin start
proliferating migrates toward incision al
space “Forms epithelial spurs”.
As they migrate they lay their basement
membrane
By 48 hours a well approximated wound is
covered by a layer of epithelium
Migrated epithelium covers dermis
Separates if from overlying necrotic material
and clot “scab” which is cast off.
• Basal cells continue to divide.
• By 5th day multilayered new epidermis is formed
(stratified into layers).
REPAIR--Organization
By 3rd day granulation tissue progressively invade
the wound area.
By 5th day Neovascularization is maximal and new
collagen fibrils forming.
• Collagen deposition continues until incision is
bridged.
• By 4th week there is a scar tissue which is scantly
cellular and devoid of inflammatory cells.
Healing by second intention
•Characteristic of wound;
Open with large tissue defect.
At times infected.
Extensive loss of cells and tissue.
Wound not approximated by suture.
• Healing take place form base upward and from
margin
Epithelium starts growing from both sides.
Cannot meet because of large size.
Large granulation tissue has to form first.
• On healing there is extensive connective tissue
formation.
•End result contraction of wound.
Complication of wound healing
Infection.
Defect in scar formation.
Hypertrophied scar and keloid.
Excessive contraction.
(contractures).
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5820)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Identification of Basic Patterns - Skin - Fibrosing DermatitisDocument28 pagesIdentification of Basic Patterns - Skin - Fibrosing DermatitisBogdan CarabasNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- A Guide To Life!: - and List To Live byDocument6 pagesA Guide To Life!: - and List To Live byBravan AliennNo ratings yet
- Computer Data Storage-1Document9 pagesComputer Data Storage-1Bravan AliennNo ratings yet
- 6 ThrombosisDocument27 pages6 ThrombosisBravan AliennNo ratings yet
- Cellular Events: A Critical Function of InflammationDocument21 pagesCellular Events: A Critical Function of InflammationBravan AliennNo ratings yet
- Vascularized Tissue To Injurious Agent A Protective ResponseDocument13 pagesVascularized Tissue To Injurious Agent A Protective ResponseBravan AliennNo ratings yet
- Hemoglobinopathies (Hemoglobin Disorders)Document18 pagesHemoglobinopathies (Hemoglobin Disorders)Bravan AliennNo ratings yet
- L27 VasculitisDocument28 pagesL27 VasculitisGazarNo ratings yet
- Benign Breast DisordersDocument30 pagesBenign Breast DisordersShams Nadeem AlamNo ratings yet
- Essential of Special Patholog by DR Zair Hassan: December 2015Document271 pagesEssential of Special Patholog by DR Zair Hassan: December 2015pdf pediatriNo ratings yet
- The Histopathological Approach To Inflammatory Bowel Disease: A Practice Guide.Document18 pagesThe Histopathological Approach To Inflammatory Bowel Disease: A Practice Guide.Ana CanastraNo ratings yet
- Restrictive Lung Diseases 1Document18 pagesRestrictive Lung Diseases 1RAMNo ratings yet
- 03-Granulom Inelar Diseminat Prezentare de Caz en 262Document8 pages03-Granulom Inelar Diseminat Prezentare de Caz en 262celena8No ratings yet
- General Pathology NotesDocument29 pagesGeneral Pathology NotesMohd Syaiful Mohd ArisNo ratings yet
- Effusion Cytology 2Document6 pagesEffusion Cytology 2PranayNo ratings yet
- Fish Vaccines - Alexandra Adams 2016Document182 pagesFish Vaccines - Alexandra Adams 2016Richard TorresNo ratings yet
- Morpho - Pathology Final Summary: Chapter 1: Cellular Reactions To AggressionDocument21 pagesMorpho - Pathology Final Summary: Chapter 1: Cellular Reactions To Aggressiondjxela89No ratings yet
- Collection of University Question Papers Ii Year MBBS: 1990 - 2009 TKMC 007 BatchDocument23 pagesCollection of University Question Papers Ii Year MBBS: 1990 - 2009 TKMC 007 BatchSubramaniam KrishnamoorthiNo ratings yet
- Path Important Questions CompatibleDocument12 pagesPath Important Questions Compatiblecarol_nditaNo ratings yet
- OCTA InflammatoryEyediseaseSrivastavaDocument24 pagesOCTA InflammatoryEyediseaseSrivastavaPriyanka DocNo ratings yet
- SarcoidosisDocument7 pagesSarcoidosisJohn SmithNo ratings yet
- Benign EntitiesDocument37 pagesBenign EntitiesleartaNo ratings yet
- Textbook of Surgery For Dental Students-smile4DrDocument400 pagesTextbook of Surgery For Dental Students-smile4DrRotariu Ana Maria100% (8)
- Inflammation SeminarDocument59 pagesInflammation SeminarVinod S Vinu100% (2)
- Jurnal 2Document3 pagesJurnal 2Renita Mandalinta SitepuNo ratings yet
- Robbins & Cotran Pathologic Basis of Disease - With STUDENT CONSULT Online Access, 8e (PDFDrive - Com) - 89-105Document17 pagesRobbins & Cotran Pathologic Basis of Disease - With STUDENT CONSULT Online Access, 8e (PDFDrive - Com) - 89-105bgfhnfgNo ratings yet
- 11 Lung PathologyDocument7 pages11 Lung PathologycarlgangcaNo ratings yet
- Viva Questions AllDocument18 pagesViva Questions AllFiaz medicoNo ratings yet
- Nasal Septal PerforationDocument12 pagesNasal Septal PerforationRini RahmawulandariNo ratings yet
- Ijd 12629Document8 pagesIjd 12629Hamza RafiqNo ratings yet
- Pathology Seminar Review (Semester 1)Document26 pagesPathology Seminar Review (Semester 1)Lin AdutNo ratings yet
- Pathology Slides by Organ 2Document25 pagesPathology Slides by Organ 2Lin AdutNo ratings yet
- Tuberculosis - Knowledge at AMBOSSDocument4 pagesTuberculosis - Knowledge at AMBOSSKC Dela RosaNo ratings yet
- PATHO FALCON (Latest Edition)Document17 pagesPATHO FALCON (Latest Edition)Nikhil kumar Sangam.No ratings yet
- Tuberculosis of The Central Nervous SystemDocument17 pagesTuberculosis of The Central Nervous Systemnight.shadowNo ratings yet
- T4HSR PresentationDocument20 pagesT4HSR PresentationAnm 2123No ratings yet