Professional Documents
Culture Documents
Hemorrhoids 1
Hemorrhoids 1
Uploaded by
Nur Chapi0 ratings0% found this document useful (0 votes)
5 views24 pagesOriginal Title
HEMORRHOIDS-1.ppt
Copyright
© © All Rights Reserved
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
5 views24 pagesHemorrhoids 1
Hemorrhoids 1
Uploaded by
Nur ChapiCopyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
You are on page 1of 24
HEMORRHOIDS
ANATOMY AND CLASSIFICATION
right anterior, right posterior and left lateral
positions
those originating above the dentate line
which are termed internal
those originating below the dentate line
which are termed external.
PATHOPHYSIOLOGY
represent engorgement or enlargement of
the normal fibrovascular cushions lining the
anal canal.
chronic straining secondary to constipation
or occasionally diarrhea
fibrovascular cushions lose their attachment
to the underlying rectal wall.
PATHOPHYSIOLOGY
prolapse of internal hemorrhoidal tissue
through the anal canal.
the overlying mucosa becomes more friable
and the vasculature increases.
With overlying thinning of the mucosa and
vascular engorgement, subsequent rectal
bleeding occurs.
ANATOMY AND CLASSIFICATION
classified by history and not by physical
examination.
Grade I - bleeding without prolapse.
Grade II - prolapse with spontaneous reduction.
Grade III - prolapse with manual reduction.
Grade IV - incarcerated, irreducible prolapse.
SYMPTOMS
bright red blood per rectum or a prolapsing
anal mass.
with, or following, bowel movements, is
almost universally bright red, and very
commonly drips into the toilet water.
Blood may also be seen while wiping after
defecation.
SYMPTOMS
prolapse usually occurs in association with a
bowel movement,
may also prolapse during walking or heavy lifting
as a result of increased intra-abdominal pressure.
extreme pain, bleeding and occasionally signs of
systemic illness in case of strangulation.
PHYSICAL EXAMINATION
Patients should be examined in the left lateral
decubitus position
any rashes, condylomata, or eczematous lesions.
external sphincter function
Any abscesses, fissures or fistulae
PHYSICAL EXAMINATION
lubricated finger should be gently inserted into the
anal canal while asking the patient to bear down
the resting tone of the anal canal should be
ascertained as well as the voluntary contraction of
the puborectalis and external anal sphincter.
masses should be noted as well as any areas of
tenderness.
PHYSICAL EXAMINATION
internal hemorrhoids are generally not palpable on digital
examination.
anoscopy is performed.
The side viewing anoscope should be inserted with the
open portion in the right anterior then right posterior and
finally the left lateral position
Hemorrhoidal bundles will appear as bulging mucosa and
anoderm within the open portion of the anoscope.
EVALUATION OF RECTAL
BLEEDING
rule out rectal cancer.
young individual with bleeding associated with
hemorrhoidal disease and no other systemic
symptoms, and no family history, perhaps
anoscopy and rigid sigmoidoscopy
older individual, with either a family history of
colorectal cancer, or change in bowel habits, a
complete colonoscopy should be performed to rule
out proximal neoplasia.
TREATMENT
varies from simple reassurance to operative
hemorrhoidectomy.
Treatments are classified into three
categories:
1) Dietary and lifestyle modification.
2) Non operative/office procedures.
3) Operative hemorrhoidectomy.
DIETARY AND LIFESTYLE
MODIFICATIONS
the main goal of this treatment is to minimize
straining at stool.
achieved by increasing fluid and fiber in the diet,
recommending exercise, and perhaps adding fiber
agents to the diet such as psyllium.
if necessary, stool softeners may be added.
"you don't defecate in the library so you shouldn't
read in the bathroom".
Office Treatments
RUBBER BAND LIGATION
Grade I or Grade II hemorrhoids and, in some
circumstances, Grade III hemorrhoids.
Complications include bleeding, pain, thrombosis
and life threatening perineal sepsis.
successful in two thirds to three quarters of all
individuals with first and second degree
hemorrhoids.
Office Treatments
RUBBER BAND LIGATION
Bayer, Myslovaty, and Picovsky followed 2,934
patients banded over a 12 year period.
Seventy-nine percent required no further therapy,
while eighteen percent required repeat banding
due to recurrence.
Hemorrhoidectomy was necessary in 2.1% related
to persistent symptoms .
Office Treatments
INFRARED COAGULATION
generates infrared radiation which
coagulates tissue protein and evaporates
water from cells.
is most beneficial in Grade I and small
Grade II hemorrhoids.
Office Treatments
BICAP ELECTROCOAGULATION
It works, in theory, similar to
photocoagulation or to rubber banding.
the probe must be left in place for ten
minutes.
poor patient tolerance minimized the effect
of this procedure.
Office Treatments
SCLEROTHERAPY
injection of an irritating material into the
submucosa in order to decrease vascularity
and increase fibrosis.
Injecting agents have traditionally been
phenol in oil, sodium morrhuate, or quinine
urea.
Office Treatments
Manual anal dilatation was first described by
Lord .
Cryotherapy was used in the past with the
belief that freezing the apex of the anal
canal could result in decreased vascularity
and fibrosis of the anal cushions.
Surgical Treatment of Hemorrhoids
HEMORRHOIDECTOMY
The triangular shaped hemorrhoid is excised
down to the underlying sphincter muscle.
Wound can be closed or left open
stapled hemorrhoidectomy has been
developed as an alternative to standard
hemorrhoidectomy
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5819)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Ubc 1976 PDFDocument726 pagesUbc 1976 PDFLuisHernanGuillenC100% (3)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Asian Paints Royalee Book of ColorsDocument84 pagesAsian Paints Royalee Book of Colorskarthik_mohankumar75% (8)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Bio-Medical Waste ManagementDocument38 pagesBio-Medical Waste Managementabhishek80% (5)
- 1887667986B. St.-XIIDocument30 pages1887667986B. St.-XIIkapsicumNo ratings yet
- What Is All India Bar ExaminationDocument4 pagesWhat Is All India Bar ExaminationkapsicumNo ratings yet
- Symbiosis Law School, NOIDA: Format - BDocument1 pageSymbiosis Law School, NOIDA: Format - BkapsicumNo ratings yet
- BSZ 274265613 InhDocument3 pagesBSZ 274265613 InhkapsicumNo ratings yet
- CV Admission Process 2016Document1 pageCV Admission Process 2016kapsicumNo ratings yet
- Annexure - I Affidavit by The StudentDocument4 pagesAnnexure - I Affidavit by The StudentkapsicumNo ratings yet
- Maths Olympiad InformationDocument6 pagesMaths Olympiad InformationkapsicumNo ratings yet
- SN 3 1 3Document3 pagesSN 3 1 3kapsicumNo ratings yet
- Book AlertDocument15 pagesBook AlertkapsicumNo ratings yet
- Two Days Workshop ON Commercial Contract Drafting: Symbiosis Law School, HyderabadDocument1 pageTwo Days Workshop ON Commercial Contract Drafting: Symbiosis Law School, HyderabadkapsicumNo ratings yet
- Centralized Admissions For Law Courses From Academic Year 2016Document2 pagesCentralized Admissions For Law Courses From Academic Year 2016kapsicumNo ratings yet
- ForeverDocument3 pagesForeverkathNo ratings yet
- Kunci PT Adijaya-Paket 1Document9 pagesKunci PT Adijaya-Paket 1nasrulloh_spd100% (4)
- Valvula Sobrepresión - IN2065-08-01 - MPREC - ENDocument4 pagesValvula Sobrepresión - IN2065-08-01 - MPREC - ENSiul VegaNo ratings yet
- Samuel, Bucher & Suzuki - CAP 5, The Cambridge Handbook of Research Methods in Clinical PsychologyDocument9 pagesSamuel, Bucher & Suzuki - CAP 5, The Cambridge Handbook of Research Methods in Clinical PsychologyCarla AbarcaNo ratings yet
- Cotton Pouches SpecificationsDocument2 pagesCotton Pouches SpecificationspunnareddytNo ratings yet
- Honda XR250 R XR 250 Owners Maintenance ManualDocument88 pagesHonda XR250 R XR 250 Owners Maintenance Manualcrawdoogie100% (2)
- The Poetry of Okot Pbitek The Song of LawinoDocument8 pagesThe Poetry of Okot Pbitek The Song of LawinoThierry UhawenimanaNo ratings yet
- Novel Fingerprint Scanning Arrays Using Polysilicon TFT's On Glass and Polymer SubstratesDocument2 pagesNovel Fingerprint Scanning Arrays Using Polysilicon TFT's On Glass and Polymer SubstratesArchana TripathiNo ratings yet
- Are U Trying To Switch JobDocument5 pagesAre U Trying To Switch JobJesseNo ratings yet
- Arun Ice Cream Strategic Management Case StudyDocument18 pagesArun Ice Cream Strategic Management Case Studyvar18111989100% (1)
- DC Kit1 CarpentierDocument2 pagesDC Kit1 CarpentierErnesto KangNo ratings yet
- Non-Residential Floodproofing - Requirements and CertificationDocument17 pagesNon-Residential Floodproofing - Requirements and CertificationgrahambrasicNo ratings yet
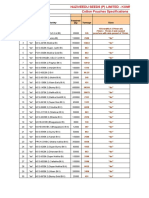
- Rates For Rate Analysis Excel FormatDocument23 pagesRates For Rate Analysis Excel FormatIswers GuptaNo ratings yet
- BS10003 Mid-Spring23 QP FinalDocument4 pagesBS10003 Mid-Spring23 QP Finalanirudhagrawal5750% (1)
- Lyoprint DaDocument4 pagesLyoprint DaLambo Sun100% (1)
- 2 - States of Matter PDFDocument26 pages2 - States of Matter PDFRisialyn ManalangNo ratings yet
- 2 Nutrient Management For Hydroponics COOKDocument33 pages2 Nutrient Management For Hydroponics COOKhyperviperNo ratings yet
- PM GB GearmotorDocument10 pagesPM GB GearmotorMulugeta Kiros GebeyehuNo ratings yet
- AN BES Murata Crystal For BT Audio IC Ver10Document11 pagesAN BES Murata Crystal For BT Audio IC Ver10Pooja Narveer RaoNo ratings yet
- Volume Changes of ConcreteDocument17 pagesVolume Changes of ConcreteAljawhara AlnadiraNo ratings yet
- Berulit GA 800Document1 pageBerulit GA 800Johan TeoNo ratings yet
- Arlegui Seminar RoomDocument1 pageArlegui Seminar RoomGEMMA PEPITONo ratings yet
- Analysis of Shaft Voltage of Large TurboDocument2 pagesAnalysis of Shaft Voltage of Large TurbohamidrezaNo ratings yet
- 194 2427 194 T Tot H H : Input OutputDocument19 pages194 2427 194 T Tot H H : Input Outputxuankhoi doanvanNo ratings yet
- Thermal Comfort SurveyDocument12 pagesThermal Comfort SurveyRahmi AndariniNo ratings yet
- ASME17-1 - Wire Rope Replacement CriteriaDocument2 pagesASME17-1 - Wire Rope Replacement Criteriaegyinspectoryahoo100% (1)
- SUMMARYDocument16 pagesSUMMARYStanley OmezieNo ratings yet
- A American Sex SurveyDocument27 pagesA American Sex SurveyRamesh RajagopalanNo ratings yet