Professional Documents
Culture Documents
Jurding Yessica+Julian
Uploaded by
JulianNathanael0 ratings0% found this document useful (0 votes)
21 views16 pages-
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Document-
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
21 views16 pagesJurding Yessica+Julian
Uploaded by
JulianNathanael-
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 16
Sue Langham1* , Jen Lewis1, Nick Pooley1, Nina Embleton1, Julia Langham1,
MeiLan K. Han2 and
James D. Chalmers3
Yessica Viona Rahadi/ 42180244
Julian Nathanael/ 42180245
For the smoking
status subgroup,
there was a strong
trend for a higher
reduction in the
For overall For the eosinophil rate of moderate
populations, the subgroup, in the and severe
rate of moderate TRINITY, TRIBUTE,
or severe exacerbations in
IMPACT and ex-smokers
exacerbations KRONOS studies compared to
was generally there was a higher smokers (IMPACT,
significantly lower For the prior
for triple exacerbation reduction in the
TRILOGY)
therapy than the frequency rate of moderate reduction in the
comparators. subgroup, triple and severe rate of
therapy exacerbations in
exacerbations
demonstrated a patients with wasgreater for
higher reduction higher eosinophil smokers.
in the rate of counts (TRIBUTE,
moderate and TRINITY)
severe
exacerbations
Across all the studies quality of life
was assessed using
the St. George’s Respiratory
Questionnaire (SGRQ), In the three
studies that assessed the single-
inhaler triple therapy resulted in
greater improvement
In the TRINITY, TRILOGY and in SGRQ total score compared with
IMPACT studies the time to first TIO, LABA/ICS and LAMA/LABA
moderate or severe exacerbation
was significantly extended with Across all the studies, SAEs were
triple therapy compared with comparable between
LAMA/LABA, LABA/ICS and LAMA Lung Function
triple therapy triple therapy and comparators.
KRONOS study, the time to first resulted in a Triple therapy was associated
moderate or severe significant with a similar percentage of
change from patients who experienced SAEs
exacerbation was extended with baseline than compared with TIO LABA/ICS
triple therapy; the improvement LABA/LAMA, and LAMA/LABA
LABA/ICS, TIO
Pneumonia was defined as an
was significant with LAMA/LABA
adverse event (AE) by the
(hazard investigator in each of these
studies (defined as an AE of
ratio [HR]: 0.59; p < 0.0001 [Cox special interest with supporting
regression] radiography)
Our analysis of single-inhaler triple therapy trials suggests
that in the patient populations included in these studies
• 25–50 patients would need to be treated with single-inhaler
triple therapy to prevent one patient from having a
moderate or severe exacerbation over one year compared
with dual therapy, with an NNH for the pneumonia AE of
around 33 and upwards.
• This emphasizes that we must weigh benefits and risks of
ICS in individual patients.
• Our analyses suggest benefit appears to be greatest in
patients with higher eosinophil counts, greater historical
frequency of exacerbations, and ex-smokers. This must be
balanced against the increased risk for AEs including
pneumonia.
The six studies included in this review had enrolled 19,658
participants with COPD of single-inhaler triple therapy, patients from
all the studies were required to have a baseline COPD assessment test
(CAT) score
We identified 523 records, of which 15 reports/abstracts from six RCTs were
included
The initial search returned 523 references after deduplication. From these,
we identified 105 as potentially relevant. A full-text analysis led to the
removal of 90, leaving 15 records (seven abstracts/posters) belonging to
six studies
All of the included studies were multinational, randomised, double-blind,
parallel-group trials.
In the study that assessed single-inhaler triple therapy with a LAMA (GLY/ FOR/BDP
versus tiotropium [TIO]), triple therapy resulted in a RR of 0.80 (95% CI: 0.69, 0.92;
20% difference; p = 0.0025), with a patient-based NNT of around 25 and an event-
based NNT of 9.
All of the outcome was considered, primary and secondary outcome
You might also like
- Jurding IpdDocument32 pagesJurding IpdJulianNathanaelNo ratings yet
- Rui Zeng (Eds.) - Graphics-Sequenced Interpretation of ECG-Springer Singapore (2016) PDFDocument173 pagesRui Zeng (Eds.) - Graphics-Sequenced Interpretation of ECG-Springer Singapore (2016) PDFJulianNathanaelNo ratings yet
- Curriculum VitaeDocument2 pagesCurriculum VitaeJulianNathanaelNo ratings yet
- OsdiDocument2 pagesOsdiFairuz PaiNo ratings yet
- Kasus JeheDocument16 pagesKasus JeheJulianNathanaelNo ratings yet
- Agama CDocument1 pageAgama CJulianNathanaelNo ratings yet
- QuoteDocument30 pagesQuoteJulianNathanaelNo ratings yet
- QuoteDocument30 pagesQuoteJulianNathanaelNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Nursing Care Plan and Diagnosis For Substance AbuseDocument87 pagesNursing Care Plan and Diagnosis For Substance AbuseZohrahLiaqatNo ratings yet
- Conversation Nonvegetarian Vs A Vegetarian Diet ConversationDocument1 pageConversation Nonvegetarian Vs A Vegetarian Diet ConversationLaura GPNo ratings yet
- History of MicrobiologyDocument23 pagesHistory of MicrobiologyISRAELNo ratings yet
- Group WorkDocument19 pagesGroup WorkSoumya Ranjan ParidaNo ratings yet
- 3 Biological Macromolecules: Chapter OutlineDocument35 pages3 Biological Macromolecules: Chapter OutlineMarkus EvanNo ratings yet
- Abnormal Perception PDFDocument5 pagesAbnormal Perception PDFsugarmelodies100% (1)
- Nut Ric ScoreDocument1 pageNut Ric ScoreClaudia M FernandezNo ratings yet
- Ticagrelor Vs Aspirin in Acute Stroke or Transient Ischemic AttackDocument28 pagesTicagrelor Vs Aspirin in Acute Stroke or Transient Ischemic AttacklucasNo ratings yet
- Resultados SaludDignaDocument2 pagesResultados SaludDignaAdriana RamosNo ratings yet
- Sindromul - De.epuizare (Bourn-Out) La Medici. F Matache. Full PDFDocument10 pagesSindromul - De.epuizare (Bourn-Out) La Medici. F Matache. Full PDFCosmin BurleanuNo ratings yet
- NCMC103 Prelims ReviewerDocument13 pagesNCMC103 Prelims ReviewerVeronica ShaneNo ratings yet
- Peripheral Blood SmearDocument46 pagesPeripheral Blood SmearAris ResurreccionNo ratings yet
- NCP - Ineffective Airway ClearanceDocument4 pagesNCP - Ineffective Airway ClearanceKen RegalaNo ratings yet
- 2020-21 Big Game Status BookDocument200 pages2020-21 Big Game Status BookAaron Meier0% (1)
- Hornsby Girls High School: Trial HSC Examination 2019 HSC BiologyDocument29 pagesHornsby Girls High School: Trial HSC Examination 2019 HSC BiologyDrewNo ratings yet
- Kode Icd X Spesialistik FixDocument2 pagesKode Icd X Spesialistik FixPuskesmas CipicungNo ratings yet
- CKD MBD GuidelineDocument65 pagesCKD MBD GuidelineCitra DessyNo ratings yet
- Lighting in Nursing Homes - The Unmet Need Noell-Waggoner, Eunice, LC, IesnaDocument6 pagesLighting in Nursing Homes - The Unmet Need Noell-Waggoner, Eunice, LC, IesnagrovelharderNo ratings yet
- Strangles and GlandersDocument26 pagesStrangles and Glandersanil regmiNo ratings yet
- Steroid AbuseDocument7 pagesSteroid Abuseapi-400575655No ratings yet
- MCQs VTEDocument7 pagesMCQs VTEMUHAMMADNo ratings yet
- 1-23 Field Ex JIDocument9 pages1-23 Field Ex JIblakeobrien2006No ratings yet
- Cardiovascular Diagnostic Tests and ProceduresDocument27 pagesCardiovascular Diagnostic Tests and ProceduresSajjal JohnsonNo ratings yet
- Definition:: Pleural EffusionDocument4 pagesDefinition:: Pleural EffusionGetom NgukirNo ratings yet
- Gambaran Peran Tenaga Kesehatan SebagaiDocument10 pagesGambaran Peran Tenaga Kesehatan SebagaiNur Rahmy OktavianiNo ratings yet
- Formulation and Evaluation of Floating Microspheres of Metformin HydrochlorideDocument10 pagesFormulation and Evaluation of Floating Microspheres of Metformin HydrochlorideBaru Chandrasekhar RaoNo ratings yet
- Endodontic Management of Mandibular Premolar With Two RootsDocument3 pagesEndodontic Management of Mandibular Premolar With Two RootsJitender ReddyNo ratings yet
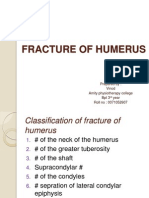
- Fracture of HumerusDocument56 pagesFracture of HumerusDr. Vinod Gupta100% (2)
- DR Ayano Final-Impacts of Sustainable Development Goals On Economic Growth in NigeriaDocument39 pagesDR Ayano Final-Impacts of Sustainable Development Goals On Economic Growth in NigeriaAyano DavidNo ratings yet
- Rabbies Health Talk NewDocument10 pagesRabbies Health Talk NewAmit Ranjan100% (1)